Professional Documents
Culture Documents
Accuracy of 3D Printed Implant Casts Versus Stone Casts: A Comparative Study in The Anterior Maxilla
Uploaded by
Dhinesh KumarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Accuracy of 3D Printed Implant Casts Versus Stone Casts: A Comparative Study in The Anterior Maxilla
Uploaded by
Dhinesh KumarCopyright:
Available Formats
Accuracy of 3D Printed Implant Casts Versus Stone Casts: A
Comparative Study in the Anterior Maxilla
Ayman Banjar, BDS, MS,1,2 Yo-wei Chen, DDS, MS, FACP ,2 Aikaterini Kostagianni, DDS, MS ,2
Matthew Finkelman, PhD,3 Aikaterini Papathanasiou, DDS, MS,2 Konstantinos Chochlidakis, DDS, MS,
FACP ,4 & Panos Papaspyridakos, DDS, MS, PhD 2,4
1
Department of Restorative Dentistry, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia
2
Department of Prosthodontics, Tufts University School of Dental Medicine, Boston, MA
3
Department of Public Health and Community Service, Tufts University School of Dental Medicine, Boston, MA
4
Department of Prosthodontics, University of Rochester Eastman Institute for Oral Health, Rochester, NY
Correspondence Abstract
Panos Papaspyridakos DDS, MS, PhD,
Associate Professor, Department of
Purpose: To conduct an in vitro comparison of the amount of three-dimensional
Prosthodontics, Tufts University School of (3D) deviation of 3D printed casts generated from digital implant impressions with
Dental Medicine, One Kneeland Street, an intraoral scanner (IOS) to stone casts made of conventional impressions.
Boston, MA, 02111. Material and Methods: A maxillary master cast with partially edentulous anterior
E-mail: panpapaspyridakos@gmail.com area was fabricated with two internal connection implants (Regular CrossFit, Strau-
mann). Stone casts (n = 10) that served as a control were fabricated with the splinted
Disclosure Statement: The authors do not open-tray impression technique. Twenty digital impressions were made using a white
have any financial interest in the companies light IOS (TRIOS, 3shape) and the Standard Tesselation Language (STL) files ob-
whose materials are included in this article. tained were saved. Based on the STL files, a digital light processing (DLP) and a
Accepted January 14, 2021
stereolithographic (SLA) 3D printer (Varseo S and Form 2) were used to print casts
(n = 10 from each 3D printer). The master cast and all casts generated from each
doi: 10.1111/jopr.13335
group were digitized using the same IOS. The STL files obtained were superimposed
on the master cast STL file (reference) to evaluate the amount of 3D deviation with in-
spection software using the root mean square value (RMS). The independent-samples
Kruskal-Wallis test and Dunn’s test with Bonferroni correction (for post hoc compar-
isons) were used for statistical analyses.
Results: The Varseo S group had the lowest median RMS value [77.5 µm (IQR =
91.4-135.4)], followed closely by the Conventional group [77.7 µm (IQR = 61.5-
93.4)]. The Form 2 had the highest mean value [98.8 µm (IQR = 57.6-87.9)]. The
independent-samples Kruskal-Wallis test revealed a significant difference between
the groups (p = 0.018). Post hoc testing revealed a significant difference between
Varseo S and Form 2 (p = 0.009).
Conclusion: The casts generated from the Varseo S 3D printer had better 3D ac-
curacy than did those from the Form 2 3D printer. Both the Varseo S group and the
conventional stone casts groups had similar 3D accuracy.
An accurate impression is a prerequisite to produce an error- tient suffocation are among the drawbacks of conventional
free stone cast, which contributes to the fabrication of a impressions.6–8 The use of intraoral scanners (IOS) for tak-
definitive restoration with accurate fit.1,2 Several factors im- ing digital scans has emerged as an alternative approach to
pact the three-dimensional (3D) accuracy of implant impres- the conventional impression technique for both partially and
sions: the properties of the impression material, the type of fully edentulous patients.9–20 The IOSs produce standard tes-
impression coping, the impression technique, the implant an- sellation language (STL) files that can be utilized to fabri-
gulation, and the connection type.3–5 According to a system- cate casts and/or dental restorations through computer-aided
atic review by Papaspyridakos et al, the splinted implant im- designing/computer-aided manufacturing (CAD/CAM).9–20
pression was reported to be the most accurate, regardless The STL files are sent and stored electronically, improv-
of the impression material used and the selected tray tech- ing efficiency. This technology offers simple, comfortable,
nique for both partially and completely edentulous cases.4 and time-effective treatment workflow for the dentist and the
However, patient gagging, taste irritation and risk of pa- patient.
Journal of Prosthodontics 0 (2021) 1–6 © 2021 by the American College of Prosthodontists 1
Accuracy of 3D Printed Casts for Partially Edentulous Anterior Maxilla Banjar et al
Until recently, subtractive manufacturing has always been as- Materials and Methods
sociated with the CAM element of the digital workflow. In this
approach, the object is created by milling it from a prefabri- A partially edentulous maxillary master cast was fabricated
cated block of the material desired. The limitations of the sub- with two bone-level internal connection implants (Bone Level
tractive technique include: the inability to create fine details, as RC, Straumann) to simulate a clinical scenario of a partially
it is highly dependent on the milling burs’ smallest radius, con- edentulous anterior maxilla that would be restored with a 4-
siderable waste of material associated with the milling, which unit implant-supported fixed dental prosthesis. The two im-
can reach 90%, and the limited number of objects that can be plants were within 5° angulation to each other simulating ideal
produced per milling session.21,22 implant placement. Four locating notches were made on the
Additive manufacturing (AM) also referred to as 3D print- master cast to standardize the process by which conventional
ing, is a process by which an object is constructed one layer impressions were made.
at a time.23,24 Several categories are available for AM: Vat Ten open tray splinted implant level impressions were made
polymerization, material jetting binder jetting, material extru- with polyether impression material (Impregum, 3M ESPE). To
sion, power bed fusion, sheet lamination, and direct energy de- standardize the procedure, implant impression copings were
position. Essentially, in Vat polymerization 3D printing, the splinted with urethane dimethacrylate-based visible light-cured
printer’s software slices the STL file of an object into multi- resin bars (Triad gel) at standardized dimensions. The bars
ple two-dimensional (2D) layers in the X and Y planes. Next, were sectioned with thin discs and then attached to the impres-
the printer begins building up the layers on top of each other sion copings with a minimum amount of Triad gel.9 The open
successively until the object is formed completely. Using this tray impressions were made with polyether impression mate-
technology allows minimal material waste and produces ob- rial in the fabricated custom tray. The impression copings were
jects with highly detailed geometries.21–27 screwed into the implant replicas, and the impressions were
Vat polymerization 3D printers utilize different printing tech- poured with type IV stone (Resin Rock, Whipmix Corp).
nologies; for example, stereolithography (SLA) and digital Subsequently, scan bodies made of poly(etheretherketone)
light processing (DLP) are those used most commonly for den- (PEEK) (CARES Mono Scan Body, Straumann) were tight-
tal applications.21 Largely, SLA and DLP printers use the same ened to the implants on the master cast with the 10Ncm torque.
process for printing, but they differ in the way they deliver the Twenty digital scans were made from the master cast using a
curing light to the resin. Stereolithography is the oldest and white light IOS (TRIOS, 3shape) following the manufacturer’s
most common method used for 3D printing. This method in- recommendation and STL files were exported. Prior to digi-
volves projecting a rapidly moving ultraviolet (UV) laser beam tal scanning, the scanner tip was calibrated using the calibra-
into a tank filled with light-sensitive liquid resin to draw the tion tip provided from the manufacturer. Additionally, one cal-
details of each layer of an object. The cured layer is attached ibrated operator performed all digital scans. Calibration was
to the printer’s building platform rather than to the resin tank. achieved prior to the initiation of the study after performing 20
Once a layer is complete, the building platform rises slightly, trial scans.
a new layer is formed on top of the previous one, and this pro- The STL files obtained from the TRIOS scanner were im-
cess continues to repeat until the object is formed fully. Digital ported into CAD software and processed by an experienced
light processing is an alternative method to deliver light in 3D laboratory technician. Twenty casts were printed using two dif-
printers. Rather than using a laser beam to scan one layer at a ferent 3D printers. In Group 2, ten casts were printed with the
time, DLP printers project a silhouette of an entire layer simul- Varseo S DLP printer (Varseo S 3D printing system, BEGO).
taneously and cure it with curing light, which permits relatively In Group 3, another ten casts were printed with the Form 2
faster printing.24–27 SLA printer (Form 2 3D printer, Formlabs). The casts were
Dental casts for fixed and implant prosthodontics derived positioned at 45° angulation to the build platform and a layer
from digital scans and constructed through 3D printing are thickness resolution of 100 µm was selected for both printers.
becoming popular. Although an IOS can offer the clinician a The Varseo S printer allows only one cast to be printed at a
complete digital workflow without the need for a physical cast, time, while the Form 2 printer can print up to eight casts at a
some complex prosthodontic procedures, especially in the an- time. In this study, two casts were 3D printed at a time with
terior maxilla, may still require physical casts. To the authors’ the Form 2 printer. All printed casts were cleaned with 99.9%
knowledge, there are no studies evaluating the accuracy of 3D isopropyl alcohol in an ultrasonic bath for 15 minutes and then
printed implant casts generated from digital scans using IOS in postcured in a curing unit (Metalight trend, Primotec® ) with
the partially edentulous anterior maxilla. Hence, the purpose of ultraviolet light of 405 nanometer wavelength for 60 minutes.
this in vitro study was to compare the accuracy of 3D printed Subsequently, implant analogs (Straumann digital reposition-
casts generated from one SLA and one DLP 3D printer to stone able analogs) were retrofitted into the printed casts so they
casts made out of conventional implant impression for the sce- could be used as working casts from the digital pathway.
nario of a partially edentulous anterior maxilla with two im- The same IOS (TRIOS) was used to scan and digitize the
plants. The hypothesis was that the stone casts fabricated using stone and the 3D printed casts from the three groups, in order to
conventional impressions have less 3D deviation compared to eliminate the effect of the scanner (Fig. 1). Prior to each scan,
casts generated from the two 3D printers. On the other hand, polymer scan bodies (CARES Mono Scan Body, Straumann)
the 3D accuracy of the printed casts generated from the two were tightened with the 10Ncm torque on the first test cast and
3D printers would be the same. The null hypothesis was that then scanned with the digital scanner. The scan bodies were
the groups have equal 3D deviation. transferred from the first cast to the second cast for scanning.
2 Journal of Prosthodontics 0 (2021) 1–6 © 2021 by the American College of Prosthodontists
Banjar et al Accuracy of 3D Printed Casts for Partially Edentulous Anterior Maxilla
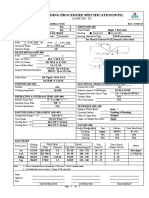
Figure 1 Casts digitization procedure. (A) SLA cast printed with Form 2 3D printer, (B) conventional stone cast, (C) DLP cast printed with Varseo S 3D
printer.
was used to test for significant differences among the three
groups. Dunn’s test with the Bonferroni correction (p < 0.05/3
≈ 0.0167) was used for the post hoc comparisons. A statistical
software program (IBM SPSS Statistics, v25; IBM Corp) was
used in the analysis.
Results
Descriptive statistics are illustrated in Table 1. The median
RMS error was 77.7 µm [IQR = (61.5, 93.4)]) for the con-
ventional group, 77.5 µm [IQR = (91.4, 135.4)] for the Varseo
S group, and 98.8 µm [IQR = (57.6, 87.9)] for the Form 2
printer group. The assumption of normality was assessed us-
ing Shapiro-Wilk test and was significant (p < 0.05 in both 3D
printed cast groups). The independent-samples Kruskal-Wallis
test revealed a significant difference (p = 0.018).
Figure 2 Superimposition of STL files of master cast and printed cast Post hoc testing via Dunn’s test with Bonferroni correction
generated from the digital scan. showed a significant difference between Varseo S and Form 2
printers (p = 0.009). The difference between conventional and
the Form 2 printer group (p = 0.024) would have been sig-
This process was repeated for all ten casts of the three groups, nificant at a significance level of 0.05, but was not significant
in order to eliminate the effect of the scan bodies. when using the more stringent Bonferroni correction.
Finally, the master cast was digitally scanned with the same
polymer scan bodies tightened on the implants in order to cre- Discussion
ate a reference STL file. All scanning procedures were com-
pleted by one calibrated operator. The STL file of each cast The objective of this in vitro study was to compare the 3D
from the control and the test groups were superimposed to the accuracy of conventional stone casts with 3D printed implant
STL file of the master cast in the 3D inspection software (Ge- casts generated from two printers with different printing tech-
omagic Control X, version 2018.1.1; 3D Systems) using the nologies. The null hypothesis was rejected in part, as the stone
best-fit alignment algorithm (Fig. 2). The software was utilized casts and 3D printed casts had similar accuracy only with the
to calculate the 3D deviation of each cast by the use of the root Varseo S printer, which demonstrated better accuracy than did
mean square (RMS) error. the Form 2 printer.
The statistical software package nQuery Advisor (Version The findings of this study showed that the least amount of
7.0) was used to perform a sample size calculation. Based on 3D deviation, when expressed as the median of RMS error,
the results of Alshawaf et al22 the anticipated means (SDs) was found in the Varseo S group, followed closely by the con-
were 53.49 (9.47) µm for the conventional group and 108.09 ventional stone cast group, while the Form 2 group had the
(9.59) µm for the digital groups. Under these assumptions, the highest amount of 3D deviation. The Varseo S printer did not
sample size calculation found that a sample size of n = 10 print the casts reliably when compared to the Form 2 printer,
per group would be adequate to achieve a power greater than as the Varseo S group had a total of eight misprints, while the
99% alongside a Type I error rate of 0.05. Descriptive statistics Form 2 printer had no misprints. Further, the Varseo S printer
(mean, median, standard deviation, interquartile range, min- failed to initiate the printing process on five occasions. Never-
imum, and maximum) were calculated for each group. The theless, the findings of this in vitro study indicated that Varseo
Shapiro-Wilk test was used to assess the normality of the data. S performed better than did the Form 2 at a printing layer
Accordingly, the nonparametric Kruskal-Wallis test (p < 0.05) thickness of 100 µm. This finding is consistent with that in
Journal of Prosthodontics 0 (2021) 1–6 © 2021 by the American College of Prosthodontists 3
Accuracy of 3D Printed Casts for Partially Edentulous Anterior Maxilla Banjar et al
Table 1 Mean, median, standard deviation (SD), interquartile range (IQR), minimum, and maximum 3D deviations (μm)
Mean Median SD IQR Min. Max. p
Conventional 85.9 77.7 30.2 (61.5, 93.4) 55.8 157.4 0.018∗
Form 2 111.8 98.8 26.1 (91.4, 135.4) 87.7 153.8
Varseo S 89.5 77.5 55.1 (57.6, 87.9) 42.5 238.1
*
p-Value from Kruskal-Wallis test. In post hoc comparisons (Dunn’s test with Bonferroni correction), the level of significance was 0.05/3≈0.0167. The difference
between Form 2 and Varseo S was statistically significant (p = 0.009), but the differences between conventional and Varseo S (p = 0.722) and conventional and
Form 2 (p = 0.024) were not statistically significant when using the Bonferroni correction.
Revilla-León et al’s28 study, which evaluated the positional ac- slices the object for printing. This can affect the mechanical
curacy of implants in casts printed with different 3D printing properties, quality, and time required for printing significantly.
technologies. Their study found that the DLP 3D printer can Thus, the build angle must be managed carefully to avoid any
produce definitive implant casts with accuracy comparable to deviation in the printed object.31 In a study conducted by Al-
the conventional method. With respect to SLA printing, Bohner harbi et al,32 it was found that the build angle affected the 3D
et al’s29 results are also consistent with this study’s findings. specimens’ accuracy significantly. The authors reported that
Their investigation also compared implant SLA 3D printed 135° (45°) and 210° build angles had the lowest RMS error,
casts to conventional stone casts, and they found no signifi- in which the former was more favorable.32 However, no study
cant differences in the linear measurements of the entire cast in the literature has reported the most appropriate build angle
area. It must be highlighted that although the difference be- for dental casts. In this investigation, all of the 3D printed casts
tween the 3D printed cast groups in this investigation was sta- were printed at 45°, which allowed the implant platform’s po-
tistically significant from the nominal point of view, this differ- sition to be parallel to the build platform. This was based on
ence may not be clinically relevant. According to the literature, the printing trials performed before the study, which showed
the reported clinically acceptable threshold of misfit lies below consistent outcomes with no deviations. Further, the addition
150 to 200 µm.12–14 This suggests that the printed casts from of sufficient supporting structures was important to brace the
each group tended to be clinically acceptable for restoration printing and avoid distortions within the cast. However, we did
fabrication. not test these parameters and observations in this study and
An attempt to compare the findings of this in vitro study further investigation is needed for dental casts.
with those of research published previously was not feasible Studies that have evaluated the accuracy of 3D printed den-
because of the paucity of such research. Previous studies that tal casts have seldom discussed resolution. Simply stated, it
have evaluated the accuracy of 3D printed and/or milled im- can be defined as the printer’s ability to reproduce the smallest
plant casts are limited, and there was great variability in the fine detail.25 In 3D printing, resolution becomes more complex
clinical scenarios and methods of testing used, as well as con- as it involves three dimensions: the 2D horizontal plane, X, Y,
flicting results.22,23 In an in vitro study by Alshawaf et al30 the and the vertical Z plane, which represents the layer’s thickness,
authors compared the accuracy of 3D printed casts (also us- and this feature is preset by the manufacturer; hence, the selec-
ing the Varseo S printer) generated from digital scans to stone tion of the printer must be based on its performance in all three
casts generated from conventional impressions. The authors re- planes (X, Y, and Z). The XY resolution is the factor that influ-
ported that 3D printed casts had more 3D deviations than the ences the 3D printing quality and accuracy most, and it varies
conventional stone casts.30 In contrast, this study found that based on the printing technology the printer uses.25,26 In DLP
printed casts from the Varseo S printer had 3D accuracy sim- printing, this feature is already fixed by the minimal pixel size
ilar to that of stone casts with two implants placed in the an- relative to the build area.21 On the other hand, in SLA printing,
terior maxilla. Another in vitro study by Lin et al5 compared the laser beam’s diameter determines the XY resolution.21–26
the accuracy of milled definitive casts made from digital scans Hence, it can be inferred that SLA technology can offer bet-
to conventional stone casts. The authors stated that the digital ter resolution than DLP, as its laser beam runs throughout the
workflow produced less accurate casts compared to the con- cross-section and draws the layer’s detail, rather than project-
ventional method when the implant divergence was at 0° and ing light on certain areas on the resin. In this investigation, the
15°.5 Although direct comparison cannot be made because of DLP printer did, in fact, perform better than the SLA printer
the difference in the fabrication method (milling vs printing), did, and the fact that the Varseo S has an XY resolution of
this study found that 3D printed casts produced in the digital 60 µm, which is better than that of Form 2 (150 µm), might
workflow had comparable accuracy to the conventional stone explain this result.25 One of the limitations of using the RMS
casts with two implants placed at 5° divergence. error to assess accuracy is its inability to determine the dis-
Many factors involved in 3D printing can affect the accuracy placement’s direction.30 Therefore, further study is required
of this approach: build angle and direction of printing, print- to analyze the cause of the discrepancies between the two
ers’ resolution, degree of support, type of resin, laser speed technologies.
and intensity, and postcuring process.31 Build angle refers to One of the principal challenges in this in vitro study was
the printing orientation, which determines the way the software determining the master cast’s true dimensions. The use of
4 Journal of Prosthodontics 0 (2021) 1–6 © 2021 by the American College of Prosthodontists
Banjar et al Accuracy of 3D Printed Casts for Partially Edentulous Anterior Maxilla
industrial computed tomography, extraoral scanners and coor- References
dinate measurement machine has been described previously in 1. Karl M, Taylor TD: Bone adaptation induced by non-passively
the literature.28,33-39 Another in vitro study used industrial com- fitting implant superstructures: a randomized clinical trial. Int J
puted tomography to validate the extraoral scanner’s accuracy Oral Maxillofac Implants 2016;31:369-375
and digital scans obtained from it were superimposed onto a 2. Chen CJ, Papaspyridakos P, Guze K, et al: Effect of misfit of
scan obtained from the industrial scanner.33 In this study, in or- cement-retained implant single crowns on crestal bone changes.
der to eliminate the effect of the scanner, the same IOS scanner Int J Prosthodont 2013;26:135-137
was used for digitization of the master cast and printed casts. 3. Jemt T, Book K. Prosthesis misfit and marginal bone loss in
In addition, the possible effect of scan bodies was minimized edentulous implant patients. Int J Oral Maxillofac Implants
1996;11:620-625
by using the same scan bodies for scanning all casts. Scan bod-
4. Papaspyridakos P, Vazouras K, Chen YW, et al: Digital vs
ies were transferred from one implant in the first cast to the conventional implant impressions: a systematic review and
same implant in the other ten casts of each group. Potential meta-analysis. J Prosthodont 2020;29:660-678
distortion of the screw might occur due to the small size, and 5. Lin WS, Harris BT, Elathamna EN, et al: Effect of implant
it might compromise the stability of the scan bodies. However, divergence on the accuracy of definitive casts created from
the scan bodies used had a titanium base interface, which is traditional and digital implant-level impressions: an in vitro
resistant to deformation. comparative study. Int J Oral Maxillofac Implants
The use of an intraoral scanner in an extraoral setting is one 2015;30:102-109
of the main limitations in this present study. In such a setting, 6. Joda T, Ferrari M, Gallucci GO, et al: Digital technology in
intraoral factors such as saliva, soft tissues, limited space and fixed implant prosthodontics. Periodontol 2000
2017;73:178-192
location of the tooth, which are all known to affect the accuracy
7. Papaspyridakos P, Chen YW, Gonzalez-Gusmao I, et al:
of the digital scan, were absent. In addition, the method used Complete digital workflow in prosthesis prototype fabrication
by the IOS to scan also contributes to the accuracy of the dig- for complete-arch implant rehabilitation: a technique. J Prosthet
ital scan. Some authors stated that video-based scanners may Dent 2019;122:189-192
demonstrate better accuracy due to the continuous streaming of 8. Chochlidakis KM, Papaspyridakos P, Geminiani A, et al: Digital
the images with large overlapping areas.40 The scanner used in versus conventional impressions for fixed prosthodontics: a
the present study was a white light IOS (TRIOS), which uses systematic review and meta-analysis. J Prosthet Dent
optical confocal microscopy technology to create an image of 2016;116:184-190
the teeth. In contrast to the video-based systems, this scanner 9. Joda T, Bragger U, Zitzmann NU. CAD/CAM implant crowns
captures several images at a time and stitches them together in a digital workflow: five-year follow-up of a prospective
clinical trial. Clin Implant Dent Relat Res 2019;21:169-174
in order to create the final image.40 This may create some
10. Jiang X, Lin Y, Cui HY, et al: Immediate loading of multiple
errors during the scanning and virtual data acquisition. How- splinted implants via complete digital workflow: a pilot clinical
ever, the digital scans in the present study were completed by study with 1-year follow-up. Clin Implant Dent Relat Res
a single calibrated operator and following the manufacturer’s 2019;21:446-453
recommendation. 11. Alsharbaty MHM, Alikhasi M, Zarrati S, et al: A clinical
In the present study, only one clinical scenario was tested. comparative study of 3-dimensional accuracy between digital
It would be beneficial to evaluate different clinical scenarios and conventional implant impression techniques. J Prosthodont
with implants placed at different levels and angulations in fu- 2019;28:e902-e908
ture studies. Also, there are no studies assessing the accuracy 12. Papaspyridakos P, Chochlidakis K, Kang K, et al: Digital
of framework fit directly fabricated from 3D printed casts. workflow for implant rehabilitation with double full-arch
monolithic zirconia prostheses. Journal of Prosthodontics
The fabrication of prosthesis prototypes or frameworks derived
2020;29:460-465
from the digital workflow and fitting them into the 3D printed 13. Basaki K, Alkumru H, De Souza G, et al: Accuracy of digital vs
casts or stone casts is the ideal way of clinically relating 3D conventional implant impression approach: a three-dimensional
accuracy and clinical fit acceptability. This will allow measur- comparative in vitro analysis. Int J Oral Maxillofac Implants
ing the amount of prototype or framework misfit and deter- 2017;32:792-799
mine whether it falls within the clinically acceptable range or 14. Chia VA, Esguerra RJ, Teoh KH, et al: In vitro
not. For future study, it is also recommended to utilize printers three-dimensional accuracy of digital implant impressions: the
with another type of printing technology and different printing effect of implant angulation. Int J Oral Maxillofac Implants
angulation. 2017;32:313-321
15. Chew AA, Esguerra RJ, Teoh KH, et al: Three-dimensional
accuracy of digital implant impressions: effects of different
Conclusions scanners and implant level. Int J Oral Maxillofac Implants
2017;32:70-80
Casts generated from the Varseo S printer had better 3D accu- 16. Marghalani A, Weber HP, Finkelman M, et al: Digital versus
racy than the Form 2 printer. Comparing the Varseo S printer conventional implant impressions for partially edentulous
group to the conventional stone casts, both groups had sim- arches: an evaluation of accuracy. J Prosthet Dent
ilar 3D accuracy. This indicates that 3D printed casts might 2018;119:574-579
be clinically acceptable and can potentially be used to fab- 17. Papaspyridakos P, Gallucci GO, Chen CJ, et al: Digital versus
ricate implant-supported, fixed dental prostheses in a digital conventional implant impressions for edentulous patients:
workflow. accuracy outcomes. Clin Oral Implants Res 2016;27:465-472
Journal of Prosthodontics 0 (2021) 1–6 © 2021 by the American College of Prosthodontists 5
Accuracy of 3D Printed Casts for Partially Edentulous Anterior Maxilla Banjar et al
18. Papaspyridakos P, Hirayama H, Chen CJ, et al: Full-arch casts from conventional implant impressions: a comparative in
implant fixed prostheses: a comparative study on the effect of vitro study. Clin Oral Implants Res 2018;29:835-842
connection type and impression technique on accuracy of fit. 31. Puebla K, Arcaute K, Quintana R, et al: Effects of
Clin Oral Implants Res 2016;27:1099-1105 environmental conditions, aging, and build orientations on the
19. Menini M, Setti P, Pera F, et al: Accuracy of multi-unit implant mechanical properties of ASTM type I specimens manufactured
impression: traditional techniques versus a digital procedure. via stereolithography. Rapid Prototyp J 2012;18:374-388
Clin Oral Investig 2018;22:1253-1262 32. Alharbi N, Osman R, Wismeijer D. Effects of build direction on
20. Chochlidakis K, Papaspyridakos P, Tsigarida A, et al: Digital the mechanical properties of 3D-printed complete coverage
versus conventional full-arch implant impressions: a prospective interim dental restorations. J Prosthet Dent 2016;115:760-
study on 16 edentulous maxillae. J Prosthodont 767
2020;29:281-286 33. Al-Imam H, Gram M, Benetti A, et al: Accuracy of
21. Kessler A, Hickel R, Reymus M. 3D Printing in Dentistry-State stereolithography additive casts used in a digital workflow. J
of the Art. Oper Dent 2020;45:30-40 Prosthet Dent 2018;119:580-585
22. Joerg RS, E Dianne R, Siegbert W. Computer-aided design and 34. Jang Y, Sim JY, Park JK, et al: Accuracy of 3-unit fixed dental
fabrication of dental restorations: current systems and future prostheses fabricated on 3D-printed casts. J Prosthet Dent
possibilities. J Am Dent Assoc 2006;137:1289-1296 2020;123:135-142
23. Dawood A, Marti Marti B, Sauret-Jackson V, et al: 3D printing 35. Papaspyridakos P, Chen YW, Alshawaf B, et al: Digital
in dentistry. Br Dent J 2015;219:521-529 workflow: in vitro accuracy of 3D printed casts generated from
24. Barazanchi A, Chen Li K, Al-Amleh B, et al: Additive complete-arch digital implant scans. J Prosthet Dent
technology: update on current materials and applications in 2020;124:589-593.
dentistry. J Prosthodont 2017;26:156-163 36. Rungrojwittayakul O, Kan JY, Shiozaki K, et al: Accuracy of
25. Revilla-Leon M, Ozcan M. Additive manufacturing 3D printed models created by two technologies of printers with
technologies used for processing polymers: current status and different designs of model base. J Prosthodont 2020;29:124-
potential application in prosthetic dentistry. J Prosthodont 128
2019;28:146-158 37. Nestler N, Wesemann C, Spies BC, et al: Dimensional accuracy
26. Quan H, Zhang T, Xu H, et al: Photo-curing 3D printing of extrusion- and photopolymerization-based 3D printers: in
technique and its challenges. Bioact Mater 2020;5:110-115 vitro study comparing printed casts. J Prosthet Dent
27. Buda M, Bratos M, Sorensen JA. Accuracy of 3-dimensional 2021;125:103-110.
computer-aided manufactured single-tooth implant definitive 38. Koretsi V, Kirschbauer C, Proff P, et al: Reliability and
casts. J Prosthet Dent 2018;120:913-918 intra-examiner agreement of orthodontic model analysis with a
28. Revilla-León M, G-M Ó, Pérez López J, et al: Position accuracy digital caliper on plaster and printed dental models. Clin Oral
of implant analogs on 3D printed polymer versus conventional Investig 2019;23:3387-3396
dental stone casts measured using a coordinate measuring 39. Park ME, Shin SY. Three-dimensional comparative study on the
machine. J Prosthodont 2018;27:560-567 accuracy and reproducibility of dental casts fabricated by 3D
29. Bohner L, Hanisch M, De Luca Canto G, et al: Accuracy of printers. J Prosthet Dent 2018;119:861.e1-861.e7
casts fabricated by digital and conventional implant impressions. 40. Patzelt SB, Bishti S, Stampf S, et al: Accuracy of
J Oral Implantol 2019;45:94-99 computer-aided design/computer-aided
30. Alshawaf B, Weber HP, Finkelman M, et al: Accuracy of printed manufacturing-generated dental casts based on intraoral scanner
casts generated from digital implant impressions versus stone data. J Am Dent Assoc 2014;145:1133-1140
6 Journal of Prosthodontics 0 (2021) 1–6 © 2021 by the American College of Prosthodontists
You might also like
- GaugesDocument33 pagesGaugesUsman ansarNo ratings yet
- Geotecnical Limit State AustralianDocument6 pagesGeotecnical Limit State Australianprashanth c.nNo ratings yet
- A Modified Functionally Generated Path Technique FGP For Making Posterior Unit Metal Ceramic Crown PDFDocument8 pagesA Modified Functionally Generated Path Technique FGP For Making Posterior Unit Metal Ceramic Crown PDFDrRanjeet Kumar ChaudharyNo ratings yet
- 3d Printing in Fixed ProsthodonticsDocument5 pages3d Printing in Fixed ProsthodonticsCherifNo ratings yet
- Welding Procedure Specification (WPS) : (Asme Sec. Ix)Document1 pageWelding Procedure Specification (WPS) : (Asme Sec. Ix)Ahmed Lepda100% (1)
- Start DateDocument2 pagesStart DateHussainNo ratings yet
- Digital Dentistry and Digital ImpressionsDocument117 pagesDigital Dentistry and Digital ImpressionsAnonymous 0pg1qSpONo ratings yet
- Clinical Applications of Digital Dental TechnologyFrom EverandClinical Applications of Digital Dental TechnologyRadi MasriNo ratings yet
- Soil Testing Report 20170711 PDFDocument82 pagesSoil Testing Report 20170711 PDFvijayarajrameshNo ratings yet
- Comparacion Del Ajuste MarginalDocument6 pagesComparacion Del Ajuste MarginalXiomara Reyes palominoNo ratings yet
- Impresion CerámicaDocument15 pagesImpresion Cerámicacarlos andres giraldoNo ratings yet
- Articulo Medit 2023Document6 pagesArticulo Medit 2023Nancy LópezNo ratings yet
- Impresiones 3DDocument9 pagesImpresiones 3DDeyvi Emerson Rivas ZarateNo ratings yet
- JCM 09 03984Document8 pagesJCM 09 03984Zaharia NedealcovNo ratings yet
- Ing. Serag M. A Comparative Study of The Accuracy of Dies Made From Digital IntraDocument6 pagesIng. Serag M. A Comparative Study of The Accuracy of Dies Made From Digital IntraBavilonia K PaolaNo ratings yet
- Ear ProsthesisDocument6 pagesEar ProsthesisSkAliHassan100% (1)
- 3D Printing - An Alternative of Conventional Crown Fabrication A Case ReportDocument7 pages3D Printing - An Alternative of Conventional Crown Fabrication A Case ReportBalavigneshwaran bt18ipf04No ratings yet
- Evaluation of The Accuracy of Digital and 3d-Printed Casts Compared With Conventional Stone CastsDocument7 pagesEvaluation of The Accuracy of Digital and 3d-Printed Casts Compared With Conventional Stone CastsAlfred OrozcoNo ratings yet
- Comparison of Accuracy Between A Conventional and Two Digital Intraoral Impression TechniquesDocument7 pagesComparison of Accuracy Between A Conventional and Two Digital Intraoral Impression TechniquesDiego LopezNo ratings yet
- 1 s2.0 S0022391322006904 MainDocument8 pages1 s2.0 S0022391322006904 MainceramicameoNo ratings yet
- 1 s2.0 S002239132030562X MainDocument4 pages1 s2.0 S002239132030562X MainDANTE DELEGUERYNo ratings yet
- Sim 2018Document7 pagesSim 2018Bear BunnyNo ratings yet
- 2020 JPDDocument5 pages2020 JPDLuis Felipe SchneiderNo ratings yet
- CAD CAM Hybrid Hyrax, AJO - PDF - BenedictDocument6 pagesCAD CAM Hybrid Hyrax, AJO - PDF - BenedictCassiana SilvaNo ratings yet
- Trueness of CADCAM Digitization With ADocument14 pagesTrueness of CADCAM Digitization With ABedah Mulut dan Maksilofasial 2023No ratings yet
- Case Report Implant Planning SurgeryDocument8 pagesCase Report Implant Planning SurgeryPrita HapsariNo ratings yet
- 25 Gianetti2022Document8 pages25 Gianetti2022jessicajacovetti1No ratings yet
- 1 s2.0 S0300571223000684 MainDocument8 pages1 s2.0 S0300571223000684 MainFlávia de Souza BastosNo ratings yet
- Comparing The Accuracy Trueness and Precision of Models of Fixed Dental Prostheses Fabricated by Digital and Conventional Workflows 2019Document6 pagesComparing The Accuracy Trueness and Precision of Models of Fixed Dental Prostheses Fabricated by Digital and Conventional Workflows 2019ANDREA LOZANO CAMPOSNo ratings yet
- Fabricating Complete Dentures With CAD/CAM Technology: A B C DDocument5 pagesFabricating Complete Dentures With CAD/CAM Technology: A B C DPaulusMetehNo ratings yet
- Precision and Accuracy of A Digital Impression Scanner in Full-Arch Implant RehabilitationDocument5 pagesPrecision and Accuracy of A Digital Impression Scanner in Full-Arch Implant Rehabilitationgeorgios031No ratings yet
- Ijp 4835Document8 pagesIjp 4835Vishal SharmaNo ratings yet
- Jced 13 E487Document6 pagesJced 13 E487Rafaela VillamaguaNo ratings yet
- Intraoral Scanning To Fabricate Complete Dentures With Functional Borders: A Proof-Of-Concept Case ReportDocument7 pagesIntraoral Scanning To Fabricate Complete Dentures With Functional Borders: A Proof-Of-Concept Case ReportVeronica Regina RosselleNo ratings yet
- Comparison of Repeatability Between Intraoral Digital Scanner and Extraoral Digital Scanner An Invitro Study.Document7 pagesComparison of Repeatability Between Intraoral Digital Scanner and Extraoral Digital Scanner An Invitro Study.Alex BurdeNo ratings yet
- Mafe AnexoDocument7 pagesMafe AnexoGABRIELA NIETO GONZALEZNo ratings yet
- 10 1016@j Prosdent 2016 08 036Document7 pages10 1016@j Prosdent 2016 08 036José Carlos Herrera IbarraNo ratings yet
- Materials 14 01550Document13 pagesMaterials 14 01550marcela fajardoNo ratings yet
- APRD - 2 (2) - 33-36 (B)Document4 pagesAPRD - 2 (2) - 33-36 (B)Nur Syfa MufidhahNo ratings yet
- 10 1016@j Prosdent 2017 06 019-2Document6 pages10 1016@j Prosdent 2017 06 019-2Paulina Vargas DíazNo ratings yet
- Evaluation of Fit For 3d-Printed Retainers Compared With Thermoform RetainersDocument8 pagesEvaluation of Fit For 3d-Printed Retainers Compared With Thermoform RetainersDr.Prakher SainiNo ratings yet
- Digital Versus Conventional Impressions in Fixed Prosthodontics: A ReviewDocument7 pagesDigital Versus Conventional Impressions in Fixed Prosthodontics: A Reviewruthy arias anahuaNo ratings yet
- Piedra 2018 Digitalworkflowforthedesignandadditivelymanufactureofasplintedframeworkandcustomtrayfortheimpressionofmultipleimplants Adentaltechnique JPDDocument8 pagesPiedra 2018 Digitalworkflowforthedesignandadditivelymanufactureofasplintedframeworkandcustomtrayfortheimpressionofmultipleimplants Adentaltechnique JPDUmesh ChauhanNo ratings yet
- Guth Et Al 2013Document8 pagesGuth Et Al 2013João BotelhoNo ratings yet
- Trueness Analysis of Zirconia Crowns Fabricated With 3d PrintingDocument7 pagesTrueness Analysis of Zirconia Crowns Fabricated With 3d PrintingAlex BurdeNo ratings yet
- Virtual Evaluation For CAD-CAM-fabricated Complete DenturesDocument6 pagesVirtual Evaluation For CAD-CAM-fabricated Complete DenturesDanny Eduardo RomeroNo ratings yet
- CAD-CAM Milled Versus Rapidly Prototyped (3d-Printed) Complete Dentures: An in Vitro Evaluation of TruenessDocument7 pagesCAD-CAM Milled Versus Rapidly Prototyped (3d-Printed) Complete Dentures: An in Vitro Evaluation of TruenessAkshayaa BalajiNo ratings yet
- 784 2009 Article 291Document8 pages784 2009 Article 291EddieLee VeraNo ratings yet
- CAD/CAM Produces Dentures With Improved FitDocument7 pagesCAD/CAM Produces Dentures With Improved FitAkshayaa BalajiNo ratings yet
- Digital Work Ow For Image-Guided Immediate Implant Placement by Using The Socket-Shield Technique and Custom Abutment in The Esthetic AreaDocument5 pagesDigital Work Ow For Image-Guided Immediate Implant Placement by Using The Socket-Shield Technique and Custom Abutment in The Esthetic AreaEduin GiraldoNo ratings yet
- Accuracy of CAD-CAM-fabricated Removable Partial Dentures: Research andDocument7 pagesAccuracy of CAD-CAM-fabricated Removable Partial Dentures: Research andHelena VenanteNo ratings yet
- Precision and Trueness of Dental Models Manufactured With Different 3-Dimensional Printing TechniquesDocument10 pagesPrecision and Trueness of Dental Models Manufactured With Different 3-Dimensional Printing TechniquesMonojit DuttaNo ratings yet
- Uso de Sistemas de Impresion Digital Con Scaners Intraorales para Fabricacion de Protesis FijaDocument7 pagesUso de Sistemas de Impresion Digital Con Scaners Intraorales para Fabricacion de Protesis FijaPaola Alexandra LaguadoNo ratings yet
- Art 2Document6 pagesArt 2Florin Eugen ConstantinescuNo ratings yet
- Are Different Generations of CAD/CAM Milling Machines Capable To Produce Restorations With Similar Quality?Document6 pagesAre Different Generations of CAD/CAM Milling Machines Capable To Produce Restorations With Similar Quality?Deyvi Emerson Rivas ZarateNo ratings yet
- Van Der Meer-2012-Application of Intra-Oral de PDFDocument8 pagesVan Der Meer-2012-Application of Intra-Oral de PDFAdinaBicaNo ratings yet
- Creacion de Un Archivo de Dentadura Total Digital, Una Tecnica DentalDocument5 pagesCreacion de Un Archivo de Dentadura Total Digital, Una Tecnica DentalPaola Alexandra LaguadoNo ratings yet
- Dynamic Designing of Dental Prostheses: International Design Conference - Design 2016Document6 pagesDynamic Designing of Dental Prostheses: International Design Conference - Design 2016Nenad BojceticNo ratings yet
- Accuracy in The Digital Work Ow: From Data Acquisition To The Digitally Milled CastDocument6 pagesAccuracy in The Digital Work Ow: From Data Acquisition To The Digitally Milled Castmarianaduque82No ratings yet
- Journal of Prosthodontic Research: Hirotaka Nishiyama, Asuka Taniguchi, Shinpei Tanaka, Kazuyoshi BabaDocument6 pagesJournal of Prosthodontic Research: Hirotaka Nishiyama, Asuka Taniguchi, Shinpei Tanaka, Kazuyoshi BabaPriscilia YovianiNo ratings yet
- PAPER BY DR CKB NAIR Dental BarsDocument8 pagesPAPER BY DR CKB NAIR Dental BarsDr CKB NairNo ratings yet
- Comparison of Denture Base Adaptation Between CAD/CAM and Conventional Fabrication TechniquesDocument8 pagesComparison of Denture Base Adaptation Between CAD/CAM and Conventional Fabrication TechniquesVictor LappostNo ratings yet
- 10 1016@j Joen 2018 11 006 PDFDocument5 pages10 1016@j Joen 2018 11 006 PDFVijithNo ratings yet
- Three-Dimensional Assessment of Virtual Bracket Removal For Orthodontic Retainers: A Prospective Clinical StudyDocument10 pagesThree-Dimensional Assessment of Virtual Bracket Removal For Orthodontic Retainers: A Prospective Clinical StudyAndré DrumondNo ratings yet
- Direct Mechanical Data Acquisition of Dental Impressions For The Manufacturing of CAD-CAM RestorationsDocument6 pagesDirect Mechanical Data Acquisition of Dental Impressions For The Manufacturing of CAD-CAM RestorationsAlex BurdeNo ratings yet
- 65 - JPR - D - 20 - 00169 - 1Document7 pages65 - JPR - D - 20 - 00169 - 1Gt SolarcNo ratings yet
- Tutorial 5 - Flexural Members - Lateral Torsional BucklingDocument32 pagesTutorial 5 - Flexural Members - Lateral Torsional BucklingChan Keng ChunNo ratings yet
- ITC Johnston Complete Family Pack Font ListDocument2 pagesITC Johnston Complete Family Pack Font ListSenthuTu0% (1)
- Mouthwash, PEG, Sulfate, Betaine FreeDocument2 pagesMouthwash, PEG, Sulfate, Betaine FreerekhilaNo ratings yet
- 4aa4 1063enwDocument8 pages4aa4 1063enwHenderson and SantosNo ratings yet
- Catalogue of Jumbo: Jumbo Power Technology Co.,LimitedDocument20 pagesCatalogue of Jumbo: Jumbo Power Technology Co.,LimitedJosé Daniel Interventoria AP MocoaNo ratings yet
- A Study On Customer Awareness and Satisfaction Towards Flipkart Shopping - With Special Reference To Pollachi TalukDocument4 pagesA Study On Customer Awareness and Satisfaction Towards Flipkart Shopping - With Special Reference To Pollachi TalukMukul SomgadeNo ratings yet
- Endodontic and Restorative Management of A Lower Molar With A Calcified Pulp Chamber.Document7 pagesEndodontic and Restorative Management of A Lower Molar With A Calcified Pulp Chamber.Nicolas SantanderNo ratings yet
- Reasearch ProposalDocument9 pagesReasearch Proposalamel amoulaNo ratings yet
- Rocna and Vulcan Anchor DimensionsDocument2 pagesRocna and Vulcan Anchor DimensionsJoseph PintoNo ratings yet
- Unit II Evolution of TQMDocument36 pagesUnit II Evolution of TQMsbmallurNo ratings yet
- Ebook Sobotta Atlas of Anatomy Vol 1 General Anatomy and Musculoskeletal System English Latin16Th Ed PDF Full Chapter PDFDocument68 pagesEbook Sobotta Atlas of Anatomy Vol 1 General Anatomy and Musculoskeletal System English Latin16Th Ed PDF Full Chapter PDFkarren.brown188100% (25)
- Pedagogy MCQsDocument85 pagesPedagogy MCQsPrasanna KumarNo ratings yet
- LP Science2 q2w5Document7 pagesLP Science2 q2w5Gaila Mae Abejuela SanorjoNo ratings yet
- Case-Friedland Timbers CompanyDocument2 pagesCase-Friedland Timbers Companytalented guy0% (1)
- CFA Level I - Timetable (August 2021 Exam) (V2)Document1 pageCFA Level I - Timetable (August 2021 Exam) (V2)Via Commerce Sdn BhdNo ratings yet
- Revealed Comparative AdvantageDocument5 pagesRevealed Comparative AdvantageiamrahulkumarNo ratings yet
- Simulación de Eventos Discretos Eduardo García Dunna May 4, 2015Document22 pagesSimulación de Eventos Discretos Eduardo García Dunna May 4, 2015Andrea GutierrezNo ratings yet
- Delta Background-Group AssignmentDocument2 pagesDelta Background-Group AssignmentTinashe100% (2)
- OTPBank Securities SI 20210217Document6 pagesOTPBank Securities SI 20210217bdsourav0No ratings yet
- AION 7.9 Part2 PatchNotes ENDocument10 pagesAION 7.9 Part2 PatchNotes ENRosaArandaNo ratings yet
- International Journal of Transportation Science and TechnologyDocument11 pagesInternational Journal of Transportation Science and TechnologyIrvin SmithNo ratings yet
- Tesla - Tunguska Explosion 1908 PDFDocument9 pagesTesla - Tunguska Explosion 1908 PDFMircea Gabriel BalanNo ratings yet
- Panasonic SC BT200Document60 pagesPanasonic SC BT200Mark CoatesNo ratings yet
- Plains Cotton Coop Ass'n V Goodpasture Computer Service, Inc, 807 F 2d 1256Document9 pagesPlains Cotton Coop Ass'n V Goodpasture Computer Service, Inc, 807 F 2d 1256gesmerNo ratings yet