Professional Documents
Culture Documents
Identification of COVID-19 Clinical Phenotypes by Principal Component Analysis-Based Cluster Analysis
Uploaded by
noor khairaniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Identification of COVID-19 Clinical Phenotypes by Principal Component Analysis-Based Cluster Analysis
Uploaded by
noor khairaniCopyright:
Available Formats
ORIGINAL RESEARCH
published: 12 November 2020
doi: 10.3389/fmed.2020.570614
Identification of COVID-19 Clinical
Phenotypes by Principal Component
Analysis-Based Cluster Analysis
Wenjing Ye 1† , Weiwei Lu 2† , Yanping Tang 3† , Guoxi Chen 4† , Xiaopan Li 5,6† , Chen Ji 7 ,
Min Hou 8 , Guangwang Zeng 3 , Xing Lan 4 , Yaling Wang 4 , Xiaoqin Deng 4 , Yuyang Cai 8*† ,
Hai Huang 4*† and Ling Yang 3*†
1
Department of Respiratory Medicine, Xinhua Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China,
Edited by: 2
Department of Emergency, Xinhua Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China,
Marc Jean Struelens, 3
Department of Geriatrics, Xinhua Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China,
Université Libre de Bruxelles, Belgium 4
Department of Tuberculosis Ward 2, Wuhan Pulmonary Hospital, Wuhan, China, 5 Center for Disease Control and
Reviewed by: Prevention, Shanghai, China, 6 Fudan University Pudong Institute of Preventive Medicine, Shanghai, China, 7 Warwick Clinical
Aruni Wilson, Trials Unit, Warwick Medical School, Coventry, United Kingdom, 8 School of Public Health, Shanghai Jiao Tong University
Loma Linda University, United States School of Medicine, Shanghai, China
John Hay,
University at Buffalo, United States
*Correspondence:
Background: COVID-19 has been quickly spreading, making it a serious public health
Yuyang Cai threat. It is important to identify phenotypes to predict the severity of disease and design
caiyuyang@sjtu.edu.cn
an individualized treatment.
Hai Huang
1220775601@qq.com Methods: We collected data from 213 COVID-19 patients in Wuhan Pulmonary Hospital
Ling Yang
yangling01@xinhuamed.com.cn
from January 1 to March 30, 2020. Principal component analysis (PCA) and cluster
analysis were used to classify patients.
† These authors have contributed
equally to this work Results: We identified three distinct subgroups of COVID-19. Cluster 1 was the largest
group (52.6%) and characterized by oldest age, lowest cellular immune function, and
Specialty section:
albumin levels. 38.5% of subjects were grouped into Cluster 2. Most of the lab results in
This article was submitted to
Infectious Diseases - Surveillance, Cluster 2 fell between those of Clusters 1 and 3. Cluster 3 was the smallest cluster (8.9%),
Prevention and Treatment, characterized by youngest age and highest cellular immune function. The incidence of
a section of the journal
Frontiers in Medicine respiratory failure, acute respiratory distress syndrome (ARDS), heart failure, and usage
Received: 08 June 2020
of non-invasive mechanical ventilation in Cluster 1 was significantly higher than others (P
Accepted: 13 October 2020 < 0.05). Cluster 1 had the highest death rate of 30.4% (P = 0.005). Although there were
Published: 12 November 2020
significant differences in age between Clusters 2 and 3 (P < 0.001), we found that there
Citation:
was no difference in demand for medical resources.
Ye W, Lu W, Tang Y, Chen G, Li X,
Ji C, Hou M, Zeng G, Lan X, Wang Y, Conclusions: We identified three distinct clusters of the COVID-19 patients. The results
Deng X, Cai Y, Huang H and Yang L
(2020) Identification of COVID-19
show that age alone could not be used to assess a patient’s condition. Specifically,
Clinical Phenotypes by Principal management of albumin, and immune function are important in reducing the severity
Component Analysis-Based Cluster
of disease.
Analysis. Front. Med. 7:570614.
doi: 10.3389/fmed.2020.570614 Keywords: COVID-19, phenotype, treatment, principal component analysis, cluster analysis
Frontiers in Medicine | www.frontiersin.org 1 November 2020 | Volume 7 | Article 570614
Ye et al. Identification of COVID-19 Clinical Phenotypes
INTRODUCTION virus from the sputum, pharyngeal swab, or lower respiratory
tract samples.
Since December 2019, pneumonia cases with unknown cause The National Health Commission of the People’s Republic of
have been reported in Wuhan (1). It has been identified as an China affirmed that data collection and analysis of cases and
acute respiratory infection caused by a novel coronavirus, later close contacts are part of ongoing investigations into outbreaks of
named COVID-19 by the World Health Organization (2). Since public health events and are therefore exempt from the approval
that time, COVID-19 has been quickly spreading in China and requirements of the institutional review board.
other countries, making it a serious global public health threat
(3). It is important for health professionals to take coordinated,
timely, and effective actions to help prevent additional cases or Data Collection
poor health outcomes. Clinical data include demographic information (gender, age,
The entire population is generally susceptible to the virus. comorbidities), laboratory tests (routine blood test, coagulation
Confirmed cases need to be treated in designated hospitals with test, infection markers, liver and kidney function, and markers
effective isolation and protection conditions. Critical cases should of myocardial injury), and outcomes (survival or death at
be admitted to the ICU as soon as possible (3). Mechanical hospital discharge).
ventilation, blood purification, and extracorporeal membrane
oxygenation (EMCO) should be applied cautiously in severe
COVID-19 patients (2). Beyond these invasive rescue methods, Statistical Analysis
doctors hope to find ways to prevent disease progress from the The main factors with the highest loading in 18 variables
early stage in the clinic. (including all the laboratory tests) were selected using principal
Cluster analysis is one of the unsupervised learning methods component analysis (PCA) at baseline. K-means cluster analysis
which has been successfully applied in medical research (4). (6), one of the most widely adopted clustering algorithms, was
Cluster generation involves merging samples into larger clusters carried out to classify COVID-19 patients into different groups
to minimize the within-cluster variations amongst patients and to using clinical data based on the PCA results.
maximize the between-cluster variations. Using cluster analysis, PCA analysis was performed using the following variables:
we can take advantage of in-depth phenotyping to reveal unique D-Dimer, fibrinogen (FIB), activated partial thromboplastin
patterns of association among phenotypic variables (5), which time (APTT), prothrombin time (PT), c-reactive protein (CRP),
may allow health professionals to develop specialized and more procalcitonin (PCT), white blood cell (WBC), neutrophil count,
effective therapeutic strategies for the treatment of COVID- lymphocyte count, monocyte count, alanine aminotransferase
19 patients. (ALT), aspartate aminotransferase (AST), albumin (Alb), helper
We hypothesized that COVID-19 comprises discrete clusters T lymphocyte count, cytotoxic T lymphocyte count, creatinine
of patients with different clinical characteristics associated with (Cr), troponin I (TNI), and N-terminal pro-Brain Natriuretic
different outcomes. To test this hypothesis, we used cluster Peptide (NT-proBNP). In order to select the number of
analysis to identify COVID-19 subgroups and then determined important principal components, we chose values with an
the disease severity among subgroups. We demonstrate that this eigenvalue >1. The Oblimin method was used in the square
unbiased clustering approach could predict the severity of disease rotation. The similarity of data was calculated using the
in patients and thus reveal the key variables clinicians could principal factors that were identified by PCA-transformed data.
consider when evaluating patients. Kaiser–Meyer–Olkin (KMO) and the Bartlett’s test of Sphericity
assessed the adaptive validity of PCA analysis. The representative
variables of principal components were chosen based on their
MATERIALS AND METHODS factor loading.
We performed a K-means cluster analysis in this study.
Study Design and Participants The main steps were as follows: First, the initial cluster center
We conducted a retrospective, single centered and observational was selected with the number of K. Second, cluster steps were
study in Wuhan Pulmonary Hospital, Hubei Province, China (a repeated until cluster membership stabilized. Third, each point
COVID-19-designated hospital in the epidemic outbreak) and was assigned to its closest cluster center. Finally, the new cluster
collected clinical data from the patients diagnosed with COVID- centers were computed.
19 between January 1 and March 30, 2020. Patients with missing SPSS version 24.0 (IBM Corp, Armonk, NY) was used for
clinical data were excluded. statistical analysis. Qualitative and quantitative variables were
The diagnosis and treatment of COVID-19 complied with the summarized using mean and standard deviation (SD), median
“new coronary pneumonia diagnosis and treatment plan” issued and inter-quartile range (IQR), and number and percentage,
by the health commission of the People’s Republic of China. respectively. Differences between clusters in qualitative variables
Laboratory diagnosis of COVID-19 was confirmed by viral were analyzed using the Chi-squared test. Differences in the
nucleic acid test (NAT) using high-throughput sequencing or quantitative variables were analyzed using the t-test. In the
real-time reverse-transcriptase–polymerase-chain-reaction (RT- case of non-normally distributed variables, the non-parametric
PCR), which can amplify the open reading frame 1ab (ORF1ab) Mann–Whitney test was used. A P < 0.05 was considered
and nucleocapsid protein (NP) gene fragments of COVID-19 statistically significant.
Frontiers in Medicine | www.frontiersin.org 2 November 2020 | Volume 7 | Article 570614
Ye et al. Identification of COVID-19 Clinical Phenotypes
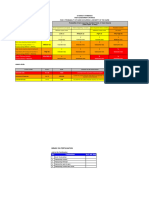
TABLE 1 | Baseline characteristics and laboratory tests of 213 patients.
Characteristics Count (%) or Mean
(SD) or Median
(IQR)
Gender (Male, %) 116 (54.5%)
Age (years) 61.7 (14.7)
D-Dimer (mg/L) 0.5 (0.2–1.7)
FIB (g/L) 4.2 (1.4)
APTT (s) 35.8 (32.5–39.7)
PT (s) 13.1 (12.5–14.3)
WBC (×109 /L) 6.7 (5.1–9.2)
Neutrophil count (×109 /L) 5.0 (3.2–7.6)
Lymphocyte count (×109 /L) 0.9 (0.6–1.5)
Monocyte coun t (×109 /L) 0.4 (0.2)
Alanine aminotransferase (µ/L) 27 (16–41)
FIGURE 1 | Selection of the study patients.
Aspartate aminotransferase (µ/L) 25 (17.5–42)
Albumin (g/L) 36.0 (5.4)
Creatinine (µmol/L) 68 (56–83)
RESULTS Helper T lymphocyte count (n/µl) 258.3 (23.1–525.6)
Cytotoxic T lymphocyte count (n/µl) 145.4 (72.9–313.0)
Demographics and Baseline CRP (mg/L) 32.4 (3.4–81.7)
Characteristics of Patients With COVID-19 PCT (ng/ml) 0.0 (0.0–0.1)
There were 431 confirmed COVID-19 patients admitted to TNI (ng/ml) 0.0 (0.0–0.0)
Wuhan Pulmonary Hospital between January 1 and March NT-proBNP (pg/ml) 144 (34–558)
30, 2020 and 218 (52.8%) were excluded due to missing Death (n, %) 46 (21.6%)
clinical data (Figure 1). Two hundred and thirteen patients were Ventilator (n, %) Invasive mechanical ventilation 33 (15.5%)
ultimately enrolled with a mean age of 61.85 ± 14.72 years, Non-invasive mechanical ventilation 49 (23%)
and 116 (54.50%) of them were males. 167 (78.40%) patients Comorbidity (n, %) Respiratory failure 37 (17.4%)
survived, while 46 (21.60%) died. Demographic characteristics, ARDS 34 (16%)
laboratory tests, and comorbidities of all patients are shown Heart failure 50 (23.5%)
in Table 1. AKI 12 (5.6%)
Diabetes mellitus 42 (19.7%)
Principal Component Analysis and Cluster
ARDS, acute respiratory dyspnea syndrome; AKI, acute kidney injury; CRP, C-reactive
Analysis for the Identification of COVID-19 protein; PCT, procalcitonin; NT-proBNP, N-terminal pro brain natriuretic peptide; TNI,
Clusters troponinI; FIB, fibrinogen; APTT, anginal partial thromboplastin time; PT, prothrombin time;
WBC, white blood cell.
The KMO value was 0.676, and the p-value of Bartlett’s
test of sphericity was <0.001. Six components were
retained using the PCA analysis. These six components
significantly contributed to explaining the relationships the highest CRP and neutrophil count, the lowest lymphocyte
among the 18 variables and accounted for 73.18% of the count and cellular immune function and albumin level, and the
information. The following representative variables were highest NT-proBNP.
chosen based on relatively high factor loading: factor 1, 38.5% of subjects (n = 82) were grouped into Cluster
CRP and neutrophil counts; factor 2, WBC and monocyte 2. This cluster had the middle age with mean age of 54.1
counts; factor 3, ALT and AST; factor 4, PCT and Fib; factor ± 5.8 years. NT-proBNP, cytotoxic T lymphocyte count,
5, TNI and D-Dimer; and factor 6, Alb and NT-proBNP helper T lymphocyte count, AST, and lymphocyte count fell
(Table 2). between those of Clusters 1 and 3. CRP, Alb, and D-Dimer
of Cluster 2 had a significant difference between Cluster
Baseline Characteristics of COVID-19 1. Clusters 2 was characterized by middle age and general
Clusters basic situation.
Three distinct subgroups were identified using the cluster Cluster 3 was the smallest cluster (n = 19; 8.9% of subjects).
analysis (Table 3). Differences between Clusters 2 and 3 are It was characterized by youngest age with mean (SD) age of 31.4
shown in Supplementary Table 1. (12.2) years and highest cytotoxic T lymphocyte count.
In total, 52.6% of subjects (n = 112) were grouped into Cluster There was no significant difference in fibrinogen, activated
1. This cluster was characterized by the oldest age with mean age APTT, PT, WBC, monocyte count, ALT, creatinine, and PCT
of 72.7 ± 6.7 years, most obvious inflammatory reaction with among the three clusters.
Frontiers in Medicine | www.frontiersin.org 3 November 2020 | Volume 7 | Article 570614
Ye et al. Identification of COVID-19 Clinical Phenotypes
TABLE 2 | Correlations of the 18 original variables with the six main factors derived from the principal component analysis.
Factor 1 Factor 2 Factor 3 Factor 4 Factor 5 Factor 6
Eigenvalue 4.388 2.539 1.673 1.629 1.136 1.076
% variance explained 25.812 14.934 9.840 9.581 6.683 6.328
APTT 0.139 0.304 0.409 −0.751 −0.119 0.077
PT 0.197 0.280 0.201 −0.815 −0.113 −0.130
WBC 0.423 0.743 −0.154 0.203 −0.315 −0.043
Monocyte count −0.254 0.646 0.033 0.242 −0.285 −0.309
Lymphocyte count −0.696 0.514 0.261 0.028 0.058 0.072
Neutrophil count 0.603 0.592 −0.196 0.175 −0.293 −0.046
Alb −0.707 0.068 0.146 0.018 0.017 0.174
CRP 0.747 0.014 0.232 −0.012 −0.212 0.310
ALT 0.232 −0.098 0.709 0.315 0.099 −0.369
AST 0.485 −0.047 0.705 0.218 0.295 −0.119
Cr 0.275 0.038 0.003 −0.082 0.257 −0.288
TNI 0.401 0.418 −0.084 −0.009 0.416 −0.146
PCT 0.379 0.139 0.313 0.232 0.029 0.712
Helper T lymphocyte count −0.768 0.418 0.174 0.080 0.147 0.075
Cytotoxic T lymphocyte count −0.761 0.425 0.182 0.105 0.039 0.065
NT-proBNP 0.473 0.368 −0.105 0.039 0.295 0.186
Fib 0.283 −0.223 0.201 0.205 −0.511 −0.130
D-Dimer 0.426 0.323 −0.282 −0.002 0.517 −0.021
CRP, C-reactive protein; PCT, procalcitonin; NT-pro BNP, N-terminal pro brain natriuretic peptide; TNI, troponinI; FIb, fibrinogen; APTT, anginal partial thromboplastin time; PT, prothrombin
time; WBC, white blood cell; Cr, creatinine; Alb, albumin; ALT, Alanine aminotransferase; AST, Aspartate aminotransferase.
TABLE 3 | Baseline characteristics of three clusters.
Cluster 1 (n = 112) Cluster 2 (n = 82) Cluster 3 (n = 19) P
Gender (Male, %) 63 (56.3%) 43 (52.4%) 10 (52.6) 0.620
Age (years) 72.7 (6.7) 54.1 (5.8) 31.4 (12.2) <0.001
D-Dimer (mg/L) 0.9 (0.4–3.5) 0.3 (0.2–0.6) 0.3 (0.1–0.6) <0.001
FIB (g/L) 4.1 (1.4) 4.3 (1.6) 4.1 (1.2) 0.773
APTT (s) 36.3 (23.6–40.6) 34.5 (31.8–37.2) 35.6 (33.4–41.8) 0.082
PT (s) 13.2 (12.5–14.4) 13.0 (12.4–13.9) 12.9 (12.5–13.7) 0.220
WBC (×109 /L) 6.7 (5.2–9.3) 6.8 (4.8–9.3) 6.3 (5.2–9.1) 0.771
Neutrophil count (×109 /L) 5.1 (3.7–8.0) 5.0 (3.0–7.8) 3.7 (2.8–4.9) 0.029
Lymphocyte count (×109 /L) 0.8 (0.5–1.3) 1.0 (0.6–1.7) 1.5 (0.9–2.3) 0.001
Monocyte count (×109 /L) 0.4 (0.2) 0.4 (0.2) 0.4 (0.1) 0.293
Alanine aminotransferase (µ/L) 26.5 (16.3–43.8) 28.5 (17–40.5) 19 (11–32) 0.16
Aspartate aminotransferase (µ/L) 29 (20–44.8) 23.5 (16–40.2) 19 (14–32) 0.009
Albumin (g/L) 34.8 (5.2) 37.3 (5.1) 37.9 (6.6) 0.002
Creatinine (µmol/L) 70 (58–89) 66.5 (53.8–78) 73 (52–78) 0.205
Helper T lymphocyte count (n/µl) 237.0 (85.2–422.5) 262.4 (142.7–652.7) 366.0 (274.4–696.8) 0.003
Cytotoxic T lymphocyte count (n/µl) 115.4 (51.0–239.8) 189.9 (97.8–387.8) 316.4 (164.3–498.8) <0.001
CRP (mg/L) 44.4 (15.0–85.1) 22.6 (1.0–83.0) 19.5 (1.0–31) 0.002
PCT (ng/ml) 0.0 (0.0–0.1) 0.0 (0.0–0.1) 0.0 (0.0–0.1) 0.065
TNI (ng/ml) 0.0 (0.0–0.0) 0.0 (0.0–0.0) 0.0 (0.0–0.0) 0.015
NT-proBNP (pg/ml) 390 (94.8–875.6) 48.5 (15–188) 15 (15–292) <0.001
CRP, C-reactive protein; PCT, procalcitonin; NT-pro BNP, N-terminal pro brain natriuretic peptide; TNI, troponinI; FIB, fibrinogen; APTT, anginal partial thromboplastin time; PT, prothrombin
time; WBC, white blood cell.
Frontiers in Medicine | www.frontiersin.org 4 November 2020 | Volume 7 | Article 570614
Ye et al. Identification of COVID-19 Clinical Phenotypes
TABLE 4 | Disease severity of three clusters.
Cluster 1 (n = 112) Cluster 2 (n = 82) Cluster 3 (n = 19) P
Invasive mechanical ventilation 22 (19.6%) 10 (12.2%) 1 (5.3%) 0.056
Non-invasive mechanical ventilation 31 (27.7%) 18 (22%) 0 (0%) 0.017
Respiratory failure 30 (26.8%) 6 (7.3%) 1 (5.3%) <0.001
ARDS 24 (21.4%) 9 (11%) 1 (5.3%) 0.019
Heart failure 36 (32.6%) 13 (15.9%) 1 (5.3%) <0.001
AKI 9 (8%) 3 (3.7%) 0 (0%) 0.087
Death 34 (30.4%) 9 (11%) 3 (15.8%) 0.005
ARDS, acute respiratory dyspnea syndrome; AKI, acute kidney injury.
COVID-19 Clusters and Disease Severity other two clusters in our study. Therefore, it is also important to
The disease severity of COVID-19 in the current patient pay attention to the albumin level in elderly patients.
population was compared across the clusters (Table 4). Our cluster analysis suggests that immunological parameters
Differences between Clusters 2 and 3 are shown in (helper T lymphocyte count and cytotoxic T lymphocyte count)
Supplementary Table 2. The incidence of respiratory failure, and serum albumin level are important in determining prognosis
acute respiratory distress syndrome (ARDS), and heart failure in and the vulnerability to developing comorbidities, including
Cluster 1 was significantly higher than the other two clusters (P respiratory failure, ARDS, and heart failure. Improving the
< 0.05). The proportion of non-invasive mechanical ventilation immune status and albumin level of patients may be a potential
usage in Cluster 1 was 27.7%, which was significantly higher than measures to prevent disease progression.
other clusters (P = 0.017). Cluster 1 also had the highest death The mortality rate was higher in elderly patients (7, 8).
rate of 30.4% (P = 0.005). We found that the mortality rate of Cluster 3, which was
characterized by the youngest mean age, was not significantly
DISCUSSION different from middle-aged patients who grouped in Cluster
2. This result aroused our attention. In previous studies, it
COVID-19 is a novel, rapidly spreading, viral illness that was mentioned that some COVID-19 patients showed immune
represents an emergent global health threat. Mortality rate is imbalance and a cytokine storm, which could be responsible
higher in elderly and intensive care unit (ICU) COVID-19 for further lung injury (15–17). Young patients in Cluster 3
patients, reaching 17–38% in recent reports (7, 8). Progressive had the highest T lymphocyte count, and most likely had a
lymphocytopenia was often found in severe cases (9–11). In cytokine storm. Thus, is the implication to clinicians that if a
this study, we identified three distinct subgroups of COVID- younger patient presents with COVID-19, they should check T
19 through a cluster analysis of 213 patients. Cluster 1 was lymphocyte counts because those with very high levels may be
characterized by oldest age, highest mortality rate (30.36%), and at risk of developing severe disease despite a younger age. This
significantly lower lymphocyte count. This result was consistent needs further pathological research to validate.
with previous reports (7, 8). D-Dimer is a degradation product that is produced in
The immune system of a host controls invading pathogens and hydrolysis of fibrin (18). Studies have reported increase in D-
thereby determines the prognosis of patients with any infectious Dimer levels in patients with pneumonia, has an indication of
disease, including pneumonia (12). As immune deficiency is the presence of thrombosis and the blood hypercoagulable state
closely tied to mortality, evaluating the immune condition could (19, 20). High D-Dimer is likely to be associated with persistent
be an important companion to monitoring a patient’s general clotting disorders, microthrombotic formation, pulmonary
condition in order to estimate prognosis (13). We found that embolism and acute myocardial infarction in long-stay patients
helper T lymphocyte count and cytotoxic T lymphocyte count or death patients, which may cause refractory hypoxemia,
in Cluster 1 were significantly lower than those of the other two respiratory failure, disseminated intravascular coagulation or
clusters. This suggested more impaired immune function in the even death. Our previous study found that COVID-19 patients
Cluster 1 patients. Treating the immune deficiency at the early with higher initial and peak D-Dimer value tended to have a
stage of disease may reduce the risk of disease deterioration and higher risk of death (21). In this study, we found that D-Dimer
improve patient prognosis. Therefore, more attention to immune of Cluster 1 was significantly higher than other two clusters.
function is required in the elderly, severely ill patients instead of Cluster 1 also had the highest death rate of 30.4%, which was
focusing on invasive treatment only. consistent with previous studies. These patients were likely to
Low albumin can lead to hypoproteinemia, and it can cause have myocardial infarction and/or pulmonary embolism, and it
a range of diseases, such as serous effusion, pulmonary edema, might also explain the difference of myocardial enzymes (TNI
heart failure, and more. Timely correction of hypoproteinemia and AST) among the three clusters. This might suggest the
could effectively prevent the incidence of complications (14). importance of early anticoagulant intervention.
Therefore we compared the albumin differences between three Neutrophil count and lymphocyte count were found to have
clusters. Albumin of Cluster 1 was significantly lower than the great prognostic power in community-acquired pneumonia. The
Frontiers in Medicine | www.frontiersin.org 5 November 2020 | Volume 7 | Article 570614
Ye et al. Identification of COVID-19 Clinical Phenotypes
increase of neutrophils often indicates that the patients have the immune function and pay attention to the underlying
bacterial infection and the infection is aggravated. The decrease health conditions in the elderly patients. D-Dimer, lymphocyte
of lymphocyte means that the immune function is poor (22, 23). count, neutrophil count, NT-proBNP, T lymphocyte count,
At the early stage of COVID-19, the total number of leukocytes and serum albumin should be paid attention to. This might
is normal or decreases, while the lymphocyte count decreases remind us that correction of these abnormal lab results in time
(3). We found that Cluster 1 had the lowest lymphocyte count can be useful in preventing the corresponding complications
and the highest neutrophil count. There was no difference in and reducing the mortality rate. Age alone could not be
Neutrophil count and lymphocyte count between Cluster 2 and used to assess a patient’s condition; cluster assessment may be
3. Our previous study found that COVID-19 patients with more reliable.
high neutrophil-lymphocyte Count Ratio might have a poor
prognosis, even a risk of death (21). Those might suggest that the DATA AVAILABILITY STATEMENT
aggravated condition and the infection is difficult to control in
Cluster 1. The original contributions presented in the study are included
According to our clustering results in disease severity, patients in the article/Supplementary Materials, further inquiries can be
in Cluster 1 had a high incidence of respiratory failure, ARDS, directed to the corresponding author/s.
heart failure, and high utilization rate of non-invasive mechanical
ventilation. The demand for medical resources of these patients ETHICS STATEMENT
is significantly higher than other clusters. Thus, we suggest
that Cluster 1 needs a comprehensive treatment plan, or may The studies involving human participants were reviewed
even need to stay in the intensive care unit. Although there and approved by The National Health Commission of
were significant differences in age between Clusters 2 and the People’s Republic of China. Written informed consent
3, we also found that there was no significant difference in for participation was not required for this study in
demand for medical resources between these two clusters. It accordance with the national legislation and the institutional
could be interpreted that doctors should pay the same clinical requirements. Written informed consent was not obtained
attention to middle-aged and young patients. Age alone could from the individual(s) for the publication of any potentially
not be used to assess a patient’s condition, we must correct the identifiable images or data included in this article. Informed
misunderstanding that young patients should always be assumed consent was exempted with the approval of Medical Ethics
to have relatively mild disease in COVID-19. Committee of Xinhua Hospital Affiliated to Shanghai
There are some potential limitations in our study. First, this Jiaotong University School of Medicine, Shanghai, China
was a single center retrospective study. All of the data were (No. XHEC-D-2020-052).
collected from patients in Wuhan Pulmonary Hospital. Most of
the patients in this hospital were symptomatic, severe or even AUTHOR CONTRIBUTIONS
critical. As a result, the proportion of young and mild disease
patients in the study was relatively low. Second, only 213 out of YC, HH, and LY designed the current study and revised the
413 patients were enrolled in our study. The exclusion of patients manuscript. YT, GC, XLi, CJ, MH, GZ, XLa, YW, and XD
with missing clinical data might cause some bias in our analysis. collected data. WY and WL wrote the manuscript and revised the
Our results could be more representative if we are able to collect manuscript. All authors contributed to the article and approved
these data in the future. Finally, our data may be subjected to the submitted version.
recall bias and selection bias due to the nature of our study.
For example, the record of patients’ comorbidities might not be FUNDING
accurate and complete, considering the unprecedented pressure
during admission and treatment. This work was supported by Zhejiang University special scientific
Further studies with more detailed and representative data are research fund for COVID-19 prevention and control [grant
needed. In particular, a long-term follow up of the patients will number 2020XGZX065].
allow us to further explore the differences between phenotypes.
SUPPLEMENTARY MATERIAL
CONCLUSIONS
The Supplementary Material for this article can be found
We identified three distinct subclasses of COVID-19 patients in online at: https://www.frontiersin.org/articles/10.3389/fmed.
Wuhan Pulmonary Hospital. It might be necessary to improve 2020.570614/full#supplementary-material
REFERENCES coronavirus (COVID-19). Int J Surg. (2020) 76:71–6. doi: 10.1016/j.ijsu.2020.
02.034
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus 3. Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, et al. A
from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727– rapid advice guideline for the diagnosis and treatment of 2019
33. doi: 10.1056/NEJMoa2001017 novel coronavirus (2019-nCoV) infected pneumonia (standard
2. Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World version). Mil Med Res. (2020) 7:4. doi: 10.1186/s40779-020-
Health Organization declares global emergency: a review of the 2019 novel 0233-6
Frontiers in Medicine | www.frontiersin.org 6 November 2020 | Volume 7 | Article 570614
Ye et al. Identification of COVID-19 Clinical Phenotypes
4. Tzeng CR, Chang YC, Chang YC, Wang CW, Chen CH, Hsu MI. Cluster 17. Zhang Y, Fan L, Xi R, Mao Z, Shi D, Ding D, et al. Lethal concentration
analysis of cardiovascular and metabolic risk factors in women of reproductive of perfluoroisobutylene induces acute lung injury in mice mediated via
age. Fertil Steril. (2014) 101:1404–10. doi: 10.1016/j.fertnstert.2014. cytokine storm, oxidative stress and apoptosis. Inhal Toxicol. (2017) 29:255–
01.023 65. doi: 10.1080/08958378.2017.1357772
5. Ahmad T, Pencina MJ, Schulte PJ, O’Brien E, Whellan DJ, Piña IL, et al. 18. Gorjipour F, Totonchi Z, Gholampour Dehaki M, Hosseini S, Tirgarfakheri
Clinical implications of chronic heart failure phenotypes defined by cluster K, Mehrabanian M, et al. Serum levels of interleukin-6, interleukin-8,
analysis. J Am Coll Cardiol. (2014) 64:1765–74. doi: 10.1016/j.jacc.2014. interleukin-10, and tumor necrosis factor-α, renal function biochemical
07.979 parameters and clinical outcomes in pediatric cardiopulmonary bypass
6. Sd C, Commandeur JJ, Frank LE, Heiser WJ. Effects of group size and lack of surgery. Perfusion. (2019) 34:651–9. doi: 10.1177/0267659119842470
sphericity on the recovery of clusters in K-means cluster analysis. Multivariate 19. Guo SC, Xu CW, Liu YQ, Wang JF, Zheng ZW. Changes in plasma
Behav Res. (2006) 41:127–45. doi: 10.1207/s15327906mbr4102_2 levels of thrombomodulin and D-dimer in children with different types of
7. Wang D, Hu B, Hu C, Zhu FF, Liu X, Zhang J, et al. Clinical characteristics of Mycoplasma pneumoniae pneumonia. Zhongguo Dang Dai Er Ke Za Zhi.
138 hospitalized patients with 2019. Novel Coronavirus-Infected Pneumonia (2013) 15:619–22.
in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.202 20. Inoue Arita Y, Akutsu K, Yamamoto T, Kawanaka H, Kitamura M, Murata H,
0.1585 et al. A fever in acute aortic dissection is caused by endogenous mediators that
8. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological influence the extrinsic coagulation pathway and do not elevate procalcitonin.
and clinical characteristics of 99 cases of 2019 novel coronavirus Intern Med. (2016) 55:1845–52. doi: 10.2169/internalmedicine.5
pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 5.5924
395:507–13. doi: 10.1016/S0140-6736(20)30211-7 21. Ye W, Chen G, Li X, Lan X, Ji C, Hou M, et al. Dynamic changes of D-
9. Li G, Fan Y, Lai Y, Han TT, Li ZH, Zhou PW, et al. Coronavirus infections and dimer and neutrophil-lymphocyte count ratio as prognostic biomarkers
immune responses. J Med Virol. (2020) 92:424–32. doi: 10.1002/jmv.25685 in COVID-19. Respir Res. (2020) 21:169. doi: 10.1186/s12931-020-
10. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of 01428-7
patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 22. Celikbilek M, Dogan S, Ozbakir O, Zararsiz G, Kücük H, Gürsoy S,
(2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5 et al. Neutrophil-lymphocyte ratio as a predictor of disease severity in
11. Han Q, Lin Q, Jin S, You L. Coronavirus 2019-nCoV: a brief perspective from ulcerative colitis. J Clin Lab Anal. (2013) 27:72–6. doi: 10.1002/jcla.
the front line. J Infect. (2020) 80:373–7. doi: 10.1016/j.jinf.2020.02.010 21564
12. Lee KY. Pneumonia, acute respiratory distress syndrome, and early immune- 23. Huang H, Wan X, Bai Y, Bian J, Xiong J, Xu Y, et al. Preoperative neutrophil-
modulator therapy. Int J Mol Sci. (2017) 18:388. doi: 10.3390/ijms180 lymphocyte and platelet-lymphocyte ratios as independent predictors of T
20388 stages in hilar cholangiocarcinoma. Cancer Manag Res. (2019) 11:5157–
13. Guo L, Wei D, Zhang X, Wu Y, Li Q, Zhou M, et al. Clinical features predicting 5162. doi: 10.2147/CMAR.S192532
mortality risk in patients with viral pneumonia: the MuLBSTA score. Front
Microbiol. (2019) 10:2752. doi: 10.3389/fmicb.2019.02752 Conflict of Interest: The authors declare that the research was conducted in the
14. Senoo T, Ishida S, Ohta K, Inaba Y, Takagi M, Yoshioka H, et al. absence of any commercial or financial relationships that could be construed as a
Hypoproteinemia as an precipitating factor of congestive heart failure in potential conflict of interest.
hypertensive heart disease (author’s transl). Nihon Ronen Igakkai Zasshi.
(1980) 17:527–32. doi: 10.3143/geriatrics.17.527 Copyright © 2020 Ye, Lu, Tang, Chen, Li, Ji, Hou, Zeng, Lan, Wang, Deng,
15. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. Cai, Huang and Yang. This is an open-access article distributed under the terms
COVID-19: consider cytokine storm syndromes and immunosuppression. of the Creative Commons Attribution License (CC BY). The use, distribution or
Lancet. (2020) 395:1033–4. doi: 10.1016/S0140-6736(20)30628-0 reproduction in other forums is permitted, provided the original author(s) and the
16. Wu D, Yang XO. TH17 responses in cytokine storm of COVID-19: an copyright owner(s) are credited and that the original publication in this journal
emerging target of JAK2 inhibitor Fedratinib. J Microbiol Immunol Infect. is cited, in accordance with accepted academic practice. No use, distribution or
(2020) 53:368–70. doi: 10.1016/j.jmii.2020.03.005 reproduction is permitted which does not comply with these terms.
Frontiers in Medicine | www.frontiersin.org 7 November 2020 | Volume 7 | Article 570614
You might also like
- Bagpipe LV 1-5Document228 pagesBagpipe LV 1-5Sathia Kdms100% (2)
- Theoretical CyclesDocument49 pagesTheoretical CyclesMariaEzzaSyUyNo ratings yet
- Filipino Construction TermsDocument6 pagesFilipino Construction TermsAdrian Perez75% (4)
- Asteroids Prospective EnergyDocument710 pagesAsteroids Prospective EnergySlavica Otovic100% (1)
- Notes Transfer of Thermal EnergyDocument12 pagesNotes Transfer of Thermal Energymahrosh mamoon100% (2)
- F24 60manual (New)Document14 pagesF24 60manual (New)Robert CumpaNo ratings yet
- Gaffin, Biblical Theology and Westminster StandardsDocument16 pagesGaffin, Biblical Theology and Westminster StandardstheoarticlesNo ratings yet
- Dynamic Interleukin-6 Level Changes As A Prognostic Indicator in Patients With COVID-19Document11 pagesDynamic Interleukin-6 Level Changes As A Prognostic Indicator in Patients With COVID-19dariusNo ratings yet
- Clinical Characteristics of Coronavirus Disease 2019 in ChinaDocument13 pagesClinical Characteristics of Coronavirus Disease 2019 in ChinaprimaNo ratings yet
- Gender Differences in Patients With COVID-19: Focus On Severity and MortalityDocument6 pagesGender Differences in Patients With COVID-19: Focus On Severity and MortalityCamila Miranda LlanesNo ratings yet
- Coronavirus Disease 2019 Related Clinical Studies: A Cross-Sectional AnalysisDocument8 pagesCoronavirus Disease 2019 Related Clinical Studies: A Cross-Sectional AnalysisMARY JANE BERMUDONo ratings yet
- Nejmoa 2002032Document13 pagesNejmoa 2002032Juan Antonio LópezNo ratings yet
- Clinical Characteristics of CoronavirusDocument13 pagesClinical Characteristics of Coronavirusleonardo almeidaNo ratings yet
- Covid 19 Patients' Clinical Characteristics, Discharge Rate, and Fatality Rate of Meta AnalysisDocument7 pagesCovid 19 Patients' Clinical Characteristics, Discharge Rate, and Fatality Rate of Meta AnalysisDelfina RubioNo ratings yet
- Luo2020 Article CanChineseMedicineBeUsedForPreDocument8 pagesLuo2020 Article CanChineseMedicineBeUsedForPreHesbon MomanyiNo ratings yet
- NEJM. COVID CHINA. 10.1056@NEJMoa2002032Document13 pagesNEJM. COVID CHINA. 10.1056@NEJMoa2002032Boris CabreraNo ratings yet
- Fimmu 11 00827Document7 pagesFimmu 11 00827yangxiao9511No ratings yet
- Title Authors:: Snarain@northwell - EduDocument17 pagesTitle Authors:: Snarain@northwell - EduPaola A. Zeña HuancasNo ratings yet
- Association of Procalcitonin Levels With The Progression and Prognosis of Hospitalized Patients With COVID-19Document9 pagesAssociation of Procalcitonin Levels With The Progression and Prognosis of Hospitalized Patients With COVID-19Dian Putri NingsihNo ratings yet
- Clinical Characteristics of Coronavirus Disease 2019 in ChinaDocument13 pagesClinical Characteristics of Coronavirus Disease 2019 in ChinaAzuraa DarmawanNo ratings yet
- D-Dimer As A Prognostic Indicator in Critically Ill Patients Hospitalized With COVID-19 in Leishenshan Hospital, Wuhan, ChinaDocument9 pagesD-Dimer As A Prognostic Indicator in Critically Ill Patients Hospitalized With COVID-19 in Leishenshan Hospital, Wuhan, ChinadariusNo ratings yet
- Liu DKK (2020)Document11 pagesLiu DKK (2020)Pinj BlueNo ratings yet
- Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, ChinaDocument7 pagesDysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, Chinacika daraNo ratings yet
- Ferritin in The Coronavirus Disease 2019 (COVID-19) : A Systematic Review and Meta-AnalysisDocument18 pagesFerritin in The Coronavirus Disease 2019 (COVID-19) : A Systematic Review and Meta-AnalysisRina ErlinaNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang Download 2024 Full ChapterDocument32 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang Download 2024 Full Chaptervito.lyons426100% (9)
- Fpubh 08 567395Document17 pagesFpubh 08 567395Healthcare Pro LearningNo ratings yet
- Covid19 - Consecuencias A 6 MesesDocument13 pagesCovid19 - Consecuencias A 6 MesesSMIBA MedicinaNo ratings yet
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument14 pagesJournal Pre-Proof: International Journal of Infectious DiseasesKenya EspinozaNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang 2 Download 2024 Full ChapterDocument32 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang 2 Download 2024 Full Chaptervito.lyons426100% (10)
- Fonc 12 857076Document10 pagesFonc 12 857076meenakshi.r.agrawalNo ratings yet
- Clinicopathological Characteristics of 8697 Patients With COVID-19 in China A Meta-AnalysisDocument11 pagesClinicopathological Characteristics of 8697 Patients With COVID-19 in China A Meta-AnalysisBenaya PhNo ratings yet
- Dong J - Prediction For Progression Risk in Patients With COVID - 19 Pneumonia The CALL ScoreDocument7 pagesDong J - Prediction For Progression Risk in Patients With COVID - 19 Pneumonia The CALL ScoreMercedes Ah CardenasNo ratings yet
- Diagnostic Utility of Clinical Laboratory Data Determinations For Patients With The Severe COVID-19Document18 pagesDiagnostic Utility of Clinical Laboratory Data Determinations For Patients With The Severe COVID-19Carla CANo ratings yet
- Estudo DiabetesDocument9 pagesEstudo DiabetesFulano de TalNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan, ChinaDocument11 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan, ChinaRENTI NOVITANo ratings yet
- Covid 19Document9 pagesCovid 19MonicaNo ratings yet
- Henry2020Document8 pagesHenry2020TisaNo ratings yet
- 6-Month Consequences of COVID-19 in Patients Discharged From Hospital: A Cohort StudyDocument13 pages6-Month Consequences of COVID-19 in Patients Discharged From Hospital: A Cohort StudyPAULA FERNANDA MONCADA CAMACHONo ratings yet
- Clinical Characteristic Covid ChildrenDocument8 pagesClinical Characteristic Covid ChildrenEstirahayuNo ratings yet
- Clinical Characteristics and Immune Responses of 137 Deceased Patients With COVID-19: A Retrospective StudyDocument12 pagesClinical Characteristics and Immune Responses of 137 Deceased Patients With COVID-19: A Retrospective StudyYogi Sampe PasangNo ratings yet
- 1.clinical Characteristics of 28 PatientsDocument7 pages1.clinical Characteristics of 28 PatientsTeguh WibowoNo ratings yet
- Liu2020 Article ClinicalAndBiochemicalIndexesFDocument11 pagesLiu2020 Article ClinicalAndBiochemicalIndexesFGabriel Ibarra TrujilloNo ratings yet
- ClinicalfeaturesDocument11 pagesClinicalfeaturesHeidiNo ratings yet
- !6-Month Consequences of COVID-19 in Patients Discharged From Hospital - A Cohort StudyDocument14 pages!6-Month Consequences of COVID-19 in Patients Discharged From Hospital - A Cohort StudyCARLA CRISTINA DE ARAUJONo ratings yet
- DDR 21762Document20 pagesDDR 21762mohammad kazem HajianiNo ratings yet
- Jurnal 7 TridaraDocument9 pagesJurnal 7 TridaraLuckyNawaNo ratings yet
- Clinical Characteristics and Diagnostic Challenges of Pediatric COVID-19: A Systematic Review and Meta-AnalysisDocument8 pagesClinical Characteristics and Diagnostic Challenges of Pediatric COVID-19: A Systematic Review and Meta-AnalysisArina Al-KhaqNo ratings yet
- Clinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province A Multicenter Descriptive StudyDocument23 pagesClinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province A Multicenter Descriptive StudyAna Maria Romero IbagonNo ratings yet
- InternacionalDocument9 pagesInternacionalbryan ronaldNo ratings yet
- Diagnostic Utility of Clinical Laboratory Data Determinationsfor Patients With The Severe COVID 19Document6 pagesDiagnostic Utility of Clinical Laboratory Data Determinationsfor Patients With The Severe COVID 19junior rodriguesNo ratings yet
- S014067362305663 PDFDocument9 pagesS014067362305663 PDFfenixNo ratings yet
- Traditional Chinese and Western Medicines Jointly Beat COVID-19 PandemicDocument2 pagesTraditional Chinese and Western Medicines Jointly Beat COVID-19 PandemicHugo GaunaNo ratings yet
- Clinical Studies On The Treatment of Novel Coronavirus Pneumonia With Traditional Chinese Medicin-A Literature AnalysisDocument15 pagesClinical Studies On The Treatment of Novel Coronavirus Pneumonia With Traditional Chinese Medicin-A Literature AnalysisSadia AfrinNo ratings yet
- Tocilizumab CovidDocument15 pagesTocilizumab CovidAponte MaríaNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan, ChinaDocument11 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan, Chinapbl4bkeceNo ratings yet
- Clinical Microbiology and InfectionDocument6 pagesClinical Microbiology and InfectionMiguel AngelNo ratings yet
- A Novel Severity Score To Predict Inpatient Mortality in COVID 19 PatientsDocument8 pagesA Novel Severity Score To Predict Inpatient Mortality in COVID 19 PatientsanscstNo ratings yet
- Jiang Et Al-2020-Journal of General Internal Medicine1Document6 pagesJiang Et Al-2020-Journal of General Internal Medicine1Farida MurtianiNo ratings yet
- Jamainternal Liang 2020 Oi 200032Document9 pagesJamainternal Liang 2020 Oi 200032Veloz RedNo ratings yet
- Jkms 35 E383Document21 pagesJkms 35 E383IraNo ratings yet
- 10 1001@jamainternmed 2020 2033Document9 pages10 1001@jamainternmed 2020 2033Rodrigo Ehécatl Torres NevárezNo ratings yet
- New Insights of Emerging Sars-Cov-2: Epidemiology, Etiology, Clinical Features, Clinical Treatment, and PreventionDocument22 pagesNew Insights of Emerging Sars-Cov-2: Epidemiology, Etiology, Clinical Features, Clinical Treatment, and PreventionWendi IochNo ratings yet
- Quarantine, Isolation and Lockdown: in Context of COVID-19Document10 pagesQuarantine, Isolation and Lockdown: in Context of COVID-19jay n shahNo ratings yet
- WNL 0000000000009673 Full1Document20 pagesWNL 0000000000009673 Full1Veloz RedNo ratings yet
- Effects of Non-Drug Interventions On Depression, Anxiety and Sleep in COVID-19 Patients: A Systematic Review and Meta-AnalysisDocument10 pagesEffects of Non-Drug Interventions On Depression, Anxiety and Sleep in COVID-19 Patients: A Systematic Review and Meta-Analysistriwinda sariNo ratings yet
- 415 2022 Article 11052Document13 pages415 2022 Article 11052Achilles Fkundana18No ratings yet
- Diagnostic Imaging of Novel Coronavirus PneumoniaFrom EverandDiagnostic Imaging of Novel Coronavirus PneumoniaMinming ZhangNo ratings yet
- HIRARC On Fertilisation - SI - 2022Document6 pagesHIRARC On Fertilisation - SI - 2022noor khairaniNo ratings yet
- 2008 - Good Practice Guidelines For High Conservation Value Asseement PDFDocument48 pages2008 - Good Practice Guidelines For High Conservation Value Asseement PDFMarcelo HernandezNo ratings yet
- Environmental Protection Sabah 2002Document37 pagesEnvironmental Protection Sabah 2002noor khairaniNo ratings yet
- Akta 446 - Feb2021Document41 pagesAkta 446 - Feb2021Khairulanwar RahmatNo ratings yet
- Pipoc 2019Document20 pagesPipoc 2019noor khairaniNo ratings yet
- 01-Act 447 - Electricity Supply Act 1990Document68 pages01-Act 447 - Electricity Supply Act 1990Mat Kamil AwangNo ratings yet
- Evaluation of Selected Bacterial Endophytes For BiDocument8 pagesEvaluation of Selected Bacterial Endophytes For Binoor khairaniNo ratings yet
- Duitnow / Transfer Money Acknowledgement: SuccessfulDocument1 pageDuitnow / Transfer Money Acknowledgement: SuccessfulWAN MOHD QhoziNo ratings yet
- Average FFB Yield of Oil Palm Estates JAN-JUNE 2022 & 2021 (TONNES/HECTARE)Document1 pageAverage FFB Yield of Oil Palm Estates JAN-JUNE 2022 & 2021 (TONNES/HECTARE)noor khairaniNo ratings yet
- Solar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power GeneratorDocument4 pagesSolar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power Generatorluis fernandoNo ratings yet
- Earth Science Essential Learning Competencies 2020Document5 pagesEarth Science Essential Learning Competencies 2020Charry CervantesNo ratings yet
- Reading Part 2Document14 pagesReading Part 2drama channelNo ratings yet
- FactSet London OfficeDocument1 pageFactSet London OfficeDaniyar KaliyevNo ratings yet
- Airport Security Post 9-11Document7 pagesAirport Security Post 9-11lewisNo ratings yet
- DIVAR IP All-In-One 7000 3U Datasheet 51 en 66297110155Document5 pagesDIVAR IP All-In-One 7000 3U Datasheet 51 en 66297110155Javier RochaNo ratings yet
- Aquaculture Scoop May IssueDocument20 pagesAquaculture Scoop May IssueAquaculture ScoopNo ratings yet
- Comparative Study On Serial and Parallel Manipulators - ReviewDocument23 pagesComparative Study On Serial and Parallel Manipulators - ReviewShaik Himam SahebNo ratings yet
- TheBasicsofBrainWaves - RS PDFDocument4 pagesTheBasicsofBrainWaves - RS PDFOnutu Adriana-LilianaNo ratings yet
- Diagnostic Imaging of The Pharynx and Esophagus: Key PointsDocument33 pagesDiagnostic Imaging of The Pharynx and Esophagus: Key PointsChutcharwan JintasoponNo ratings yet
- Us Navy To Evaluate Anti Submarine Warfare Training SystemDocument2 pagesUs Navy To Evaluate Anti Submarine Warfare Training SystemVictor PileggiNo ratings yet
- Free Electron TheoryDocument8 pagesFree Electron TheoryNeelam KapoorNo ratings yet
- Asme Code Sec Ix Ma Appe 2004Document3 pagesAsme Code Sec Ix Ma Appe 2004Guillermo CamachoNo ratings yet
- Case AnalysisDocument2 pagesCase AnalysisJessa San PedroNo ratings yet
- 988611457NK448908 Vehicle Scan ReportDocument5 pages988611457NK448908 Vehicle Scan ReportVictor Daniel Piñeros ZubietaNo ratings yet
- ff2023 Web 0 0Document2 pagesff2023 Web 0 0khaing khantNo ratings yet
- Resume: Satyam KumarDocument3 pagesResume: Satyam KumarEr Satyam Kumar KrantiNo ratings yet
- Practice For Mounting Buses & Joints-374561Document11 pagesPractice For Mounting Buses & Joints-374561a_sengar1No ratings yet
- Raneem AlbazazDocument33 pagesRaneem AlbazazGordana PuzovicNo ratings yet
- Manuscript FsDocument76 pagesManuscript FsRalph HumpaNo ratings yet
- Atomic St. Package PDFDocument28 pagesAtomic St. Package PDFSatvik RaoNo ratings yet
- 3 Curvilinear MotionDocument50 pages3 Curvilinear Motiongarhgelh100% (1)
- G-3 L-17 Internal QuestionsDocument4 pagesG-3 L-17 Internal QuestionsActivity MLZS BarhNo ratings yet