Professional Documents
Culture Documents
Subacromial Decompression Protocol: Anatomy and Biomechanics
Uploaded by
Ioana PiticarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Subacromial Decompression Protocol: Anatomy and Biomechanics
Uploaded by
Ioana PiticarCopyright:
Available Formats
Subacromial Decompression Protocol
Anatomy and Biomechanics
The shoulder is a wonderfully complex joint that is made up of the ball and socket connection between
the humerus (ball) and the glenoid portion of the
scapula (socket). The socket portion of the joint is not
naturally deep. For this reason, the shoulder is the most
mobile joint in the body. Due to the lack of boney
coverage the shoulder’s proper function and stability is
largely dependent on the soft tissues that surround it.
The shoulder joint is extremely important when the arm
is used during activities that involve lifting, pushing and
pulling, but especially when the arm is repetitively placed
overhead. Over time with continual repetitive activity
the soft tissues and joint surfaces of the shoulder are
subject to wear and tear and degeneration. The soft
tissue around the joint can become irritated and
inflamed and excess bone (spurs) can form as a result. These inflammatory or degenerative changes
often leave the shoulder feeling achy and sore during everyday activities.
Treatment Options
Regardless of nature or extent of the degeneration in the shoulder your physician will work with you to
determine what the best course of treatment will be. In many cases the pain and dysfunction associated
with degenerative changes can be successfully treated with rest, anti-inflammatory measures, activity
modification and Physical Therapy. When these conservative measures are unsuccessful in restoring
function your physician may recommend that you undergo arthroscopic surgery to remove the irritated,
degenerative tissue in the shoulder.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 1
in Clinical Collaboration with South Shore Orthopedics
Surgery
The subacromial decompression procedure involves removing tissue
from the front part of the shoulder. This part of the shoulder is
referred to as the subacromial space, as it is located below the
outcropping of bone on the scapula (shoulder blade) know as the
acromian process. During the procedure the end of the acromian
process and any inflamed tissue including the subacromial bursa is
debrided. This creates more room in the front of the shoulder so
that the tendons of the rotator cuff can move freely without getting
irritated or pinched. The procedure is performed arthroscopically
and is, in most cases an outpatient day surgery. This means that it
is very rare to have to spend the night in the hospital.
Recovery/Time off Work
Before undergoing subacromial decompression surgery your doctor will discuss the recovery process
with you. It is very important that the patient knows that the recovery process is fairly difficult and time
consuming. He or she must be an active participant during this process, performing daily exercises to
ensure there is proper return of the shoulder’s range of motion and strength. There is a large amount of
variability in the time it takes to fully recover from this procedure and is typically dependant on the
extent of the damage that needs to be fixed. It is usually estimated that it will take at least 3-4 months
to feel as though you have completely regained the use of your arm. Some cases may take as long as 6-
9 months to make a full recovery. People with desk jobs should plan to take at least 1 week off from
work. Those with jobs that require physical activity and lifting will likely be out of work for at least 3
months. Recovery is different in each case. Your individual time table for return to activities and work
will be discussed by your surgeon during post operative office visits.
Post Operative Visits
Your first post-op visit to the doctor’s office will be approximately 7-10 days after the operation. At this
visit any stitches you have will be removed and you will review the surgery with the doctor or his
assistant. At this time you will most likely be cleared to make an appointment to begin Physical Therapy.
You should also plan to check in with your surgeon at 6 and 12 weeks after the operation. The surgeon
may create a different timetable for postoperative office visits if your case warrants it.
At Home
You may remove your post-op dressing 2 days after the operation and replace it as needed. Do not
remove the tape (steri-strips) that is across your incisions. Allow them to fall off on their own. You may
shower after 2 days, but use a water-tight dressing until your sutures are removed. Bathing without
getting the shoulder wet or sponge baths are a good alternative. You may wash under the affected arm
by leaning forward and letting the arm dangle. You may move your arm in front of your body, but not
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 2
in Clinical Collaboration with South Shore Orthopedics
out to the side until your doctor allows you. You may remove your sling several times a day and gently
move your hand, wrist and elbow and perform shoulder pendulum exercises.
Medication
Your surgeon will prescribe pain medicine for you after the operation. Please call the doctor’s office if
you have any questions regarding medication.
Ice
You must use ice on your shoulder after the operation for management of pain and swelling. Ice should
be applied 3-5 times a day for 10-20 minutes at a time until the postoperative inflammation has
resolved. Always maintain one layer between ice and the skin. Putting a pillow case over your ice pack
works well for this.
Sling
You will be provided with a sling to wear after the operation. Remove it when bathing/showering, or to
do your exercises. You should remove the sling several times a day to perform pendulum exercises as
instructed. Wear the sling most of the time (especially when out in public) until you see your doctor for
your first post op visit. Most patients use their sling for about 2 weeks. If your case is atypical your
doctor may have custom guidelines for you regarding use of the sling.
Sleeping
You may sleep with a pillow propped under your arm to keep it slightly away from the body if you need
to. For many patients lying flat is uncomfortable at first. It is generally easier to sleep propped up for a
short period of time after the operation. Do not attempt to sleep on your operated shoulder for at least
6 weeks.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 3
in Clinical Collaboration with South Shore Orthopedics
Rehabilitation
**The following is an outlined progression for rehab. Time tables are approximate. Advancement
from phase to phase, as well as specific exercises performed, should be based on each individual
patient’s case and sound clinical judgment on the part of the rehab professional. **
Phase 1 (0-2 Weeks) ROM Phase
Goals
Control Pain and Swelling
Protect Healing Tissue
Begin to Restore Range of Motion
Precautions
Do not actively use your arm for reaching, especially overhead.
Do not lift anything with your arm.
Recommended Exercises
Pendulums
Standing Scapular Mobility (no resistance)
Supine or Standing Passive External Rotation
Supine, Seated or Standing Passive Shoulder Flexion (elevation)
Passive Internal Rotation
Passive Horizontal Adduction
Guidelines
Perform these exercises 3-5 times a day. Do 1-2 sets of 10-20 repetitions of each exercise.
Phase 2 (2-6 Weeks) Active ROM Phase
Goals
Continued protection of healing tissue
Continue to improve ROM
Initiate gentle peri-scapular and rotator cuff strengthening
Begin using your arm for daily activities in front of body
Precautions
Discontinue use of sling if you have not already
Be careful with raising your arm, especially overhead, and away from your body
Continue to avoid lifting or carrying anything
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 4
in Clinical Collaboration with South Shore Orthopedics
Recommended Exercises
ROM
Continue passive ROM with physical therapist
Pendulums
Supine Stick Flexion
Table Slides with progression to Wall Slides
Supine or Standing Passive External Rotation with gentle progression of abduction angle
Passive Internal Rotation
Gentle supine or standing cross body stretch
AROM Against Gravity
Prone Row
Prone Extension
Prone Horizontal Abduction
Sidelying External Rotation
Guidelines
Perform all exercises once a day. Do 2-3 sets of 15-20 repetitions.
Phase 3 (6-12 Weeks) Strengthening Phase
Goals
Continue to acquire normal ROM (both passive and active)
Progressive strengthening of rotator cuff and shoulder blade muscle groups
Begin limited use arm for daily activities in all planes
Precautions
No lifting away from your body or overhead greater than 1 or 2 pounds
Caution with repetitive use of arm especially overhead
Stop activity if it causes pain in shoulder
Recommended Exercises
Range of Motion
Continue passive ROM with physical therapist as needed
Continue ROM exercises from phase 2 until ROM is normalized
Strengthening (Resistance Band or Dumbell)
Row
Prone Extension
Prone Horizontal Abduction
Standing/Prone Scaption
Internal Rotation
External Rotation
Dynamic Strengthening
Manual Resistance Rythmic Stabilization
Proprioceptive Drills (90⁰ of Elevation or Below)
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 5
in Clinical Collaboration with South Shore Orthopedics
Guidelines
Perform ROM and stretching exercises once a day until normal ROM is achieved. Do 2 sets of 15-20
Reps. Once normal ROM is achieved continue exercises to maintain ROM 3-5 times a week.
Perform strengthening exercises 3-5 times a week. Do 2-3 sets of 15-20 Reps. Strict attention must be
paid to scapulohumeral rhythm with completion of all strengthening exercises.
Phase 4 (12 Weeks +) Sport Specific and Return to Activity Phase
Goals
Achieve normal ROM and strength
Continue to encourage progressive use of arm for functional daily activity
Precautions
Encourage return to full use of arm for daily activities
Pay particular attention to scapulohumeral rhythm especially with abduction and overhead activity
Discuss return to sport and activity plan with physician
Recommended Exercises
ROM and Stretching
Continue ROM and stretching exercises from phase 2-3 as needed
Strengthening
Continue strengthening exercises from phase 3
IR/ER strengthening at 90 deg of abduction
May begin supervised weight training pending surgeons clearance
Dynamic Strengthening
Progress manual resistance patterns
Progress proprioceptive drills to include rhythmic stabilization
Slowly progress to overhead proprioceptive and plyometric drills
Push up progression
Guidelines
Perform ROM and stretching program 1-3 times a week to maintain normal ROM. Do 1-2 sets of 15-20
Reps. Perform ROM and stretching more frequently in any planes of motion that are still deficient
Perform strengthening 3 times a week. Do 2-3 sets of 15-20 Reps.
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 6
in Clinical Collaboration with South Shore Orthopedics
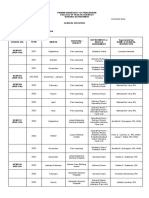
Recommended
Time Focus Range of Motion Precautions
Exercises
Phase 1 *Tissue Healing *PROM with PT as Passive/Active ROM *Sling 0-2
0-2 Weeks *Decrease Pain tolerated in all Pendulums Weeks or per
and planes Scapular Mobility MD Instruction
Inflammation *Avoid AROM in Passive External Rotation *Limit Active
*Start Early Coronal Plane Passive Flexion ROM
Passive ROM Passive Internal Rotation *Limit Use of
with Attention to Passive Horizontal Adduction Arm, Especially
Restrictions Overhead and
in Abduction
Phase 2 *Continue to *Continue Passive Passive ROM *No Resisted
2-6 Weeks Decrease Pain ROM as tolerated. Continue PROM Exercises Activity/Lifting
and *Slowly Encourage Active Assisted ROM *Avoid
Inflammation Pain Free Active Supine to Standing Flexion Repetitive
*Improve Passive ROM Cross-body Adduction Motion
and Active ROM Progress Abd angle with ER Especially
Active ROM Against Gravity Overhead
Sidelying ER *Must have
Prone Row good Scapular
Prone Extension Control with
Prone Horizontal Abduction Active ROM
Against Gravity
Phase 3 *Progressive *Passive and Passive ROM *No Heavy or
6-12 Strengthening Active ROM as Continue as Needed Repetitive
Weeks *Continued tolerated in all Active Assisted/Active ROM Overhead
Attention to planes and Stretching Lifting/Reaching
ROM if Still Continue Phase 2 Exercises *Dynamic
Deficient Strengthening (Dumbbell/T- Progressions if
*Establish Proper band) Pain Free/Full
Scapulohumeral Row ROM with all
Rhythm Prone Extension ROM and
*Enhance Prone Horizontal Abduction Strengthening
Proprioception Standing/Prone Scaption Exercises
Internal Rotation
External Rotation
“W” (Row/ER)
Bicep Curl
Dynamic Progressions
Rhythmic Stabilization
Proprioceptive Drills
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 7
in Clinical Collaboration with South Shore Orthopedics
Phase 4 *Progress *Continue ROM/Stretch * Return to
12 Weeks + strengthening Stretching Continue Phase 3 As Needed Gym Lifting per
*Regain use of Program as Strengthening MD Approval
arm for all daily needed. Continue T-band and *Avoid
activities. Dumbbell Progressions from Activities that
*Prepare for Phase 3 Cause Shoulder
Return to Sport Progress to Diagonal Patterns Pain
and Physical IR/ER at 90⁰ Abd *Begin
Activity May Begin Limited Weight Progressive
Training Return to
Dynamic Progressions Sports and
Pushup Progression Physical Activity
Continue Proprioceptive Drills Program After
Plyometrics/Rebounder MD Evaluation
Progress to Overhead
Rhythmic Stabilization
Manual Resistance Patterns
*Reviewed by Michael Geary, MD
South Shore Hospital Orthopedic, Spine and Sports Therapy Page 8
in Clinical Collaboration with South Shore Orthopedics
You might also like
- Tips for Everyday Life and Sports With an Artificial Joint: Expert guidebook for dealing with a prosthesis for patients with a new hip or knee jointFrom EverandTips for Everyday Life and Sports With an Artificial Joint: Expert guidebook for dealing with a prosthesis for patients with a new hip or knee jointNo ratings yet
- Total Shoulder ReplacementDocument11 pagesTotal Shoulder ReplacementNeicu VladNo ratings yet
- If they could talk about walking again: Canine Cruciate Surgery Rehabilitation Program: A 10 week detailed program of specific approaches, exercises, massage, and restoring balance to get the best results after your pet has undergone surgery for cruciate ligament repair. Tracking sheets for each week.From EverandIf they could talk about walking again: Canine Cruciate Surgery Rehabilitation Program: A 10 week detailed program of specific approaches, exercises, massage, and restoring balance to get the best results after your pet has undergone surgery for cruciate ligament repair. Tracking sheets for each week.No ratings yet
- Knee Arthroscopy Meniscectomy Recovery GuideDocument9 pagesKnee Arthroscopy Meniscectomy Recovery Guidebayan salahNo ratings yet
- Resistance Band Workouts for Bad Posture and Back PainFrom EverandResistance Band Workouts for Bad Posture and Back PainRating: 3.5 out of 5 stars3.5/5 (4)
- National Hospital (Shoulder-Arthroplasty Rehab-Protocol)Document14 pagesNational Hospital (Shoulder-Arthroplasty Rehab-Protocol)muhammad umarNo ratings yet
- Total Hip Arthroplasty (THA) Rehabilitation ProtocolDocument11 pagesTotal Hip Arthroplasty (THA) Rehabilitation ProtocoldvenumohanNo ratings yet
- Total Hip Arthroplasty (THA) Rehabilitation ProtocolDocument11 pagesTotal Hip Arthroplasty (THA) Rehabilitation ProtocolSherly L WaromiNo ratings yet
- Ortho Services Sports Rehab Clavicle Fracture Protocol Non SurgicalDocument17 pagesOrtho Services Sports Rehab Clavicle Fracture Protocol Non SurgicalKattamedhi Krishnachaitanya KumarreddyNo ratings yet
- Frozen Shoulder - Adhesive Capsulitis - OrthoInfo - AAOSDocument6 pagesFrozen Shoulder - Adhesive Capsulitis - OrthoInfo - AAOSpempekplgNo ratings yet
- Bristow Latarjet ProcedureDocument7 pagesBristow Latarjet ProcedurebigwhaledorkNo ratings yet
- Clavicle Fracture Protocol Non SurgicalDocument17 pagesClavicle Fracture Protocol Non SurgicalAlbert MarcuNo ratings yet
- A Patient's Guide To Adhesive CapsulitisDocument6 pagesA Patient's Guide To Adhesive Capsulitisamal sehat100% (1)
- Frozen ShoulderDocument6 pagesFrozen ShoulderanumolNo ratings yet
- Reverse Total Shoulder Arthroplasty Rehab ProtocolDocument12 pagesReverse Total Shoulder Arthroplasty Rehab Protocol張水蛙No ratings yet
- Rotator Cuff Impingement/Tendinopathy Rehab GuideDocument8 pagesRotator Cuff Impingement/Tendinopathy Rehab GuidemadaleenNo ratings yet
- TKR PDFDocument6 pagesTKR PDFKaribeños San JavierNo ratings yet
- Treatment: Home TreatmentsDocument3 pagesTreatment: Home TreatmentsDhimas Reyhan Putra SayudhaNo ratings yet
- Achilles Tendon Rupture 0Document15 pagesAchilles Tendon Rupture 0Usman JabbarNo ratings yet
- Total Shoulder Arthroplasty Tsa 2Document15 pagesTotal Shoulder Arthroplasty Tsa 2api-550365743No ratings yet
- ACL Non-Operative ManagmentDocument10 pagesACL Non-Operative ManagmentHammad -ullahNo ratings yet
- Information For Patients Following Knee Arthroscopy: Therapies DirectorateDocument6 pagesInformation For Patients Following Knee Arthroscopy: Therapies Directoratepecson1No ratings yet
- Arthroscopic Bankart Repair1Document14 pagesArthroscopic Bankart Repair1Rinkle KateNo ratings yet
- Post SPINAL - FUSION GuidelinesDocument7 pagesPost SPINAL - FUSION GuidelineskapilphysioNo ratings yet
- TKA Rehab Guide for Fast RecoveryDocument11 pagesTKA Rehab Guide for Fast RecoveryCamille DelageNo ratings yet
- Physiotherapy Goals and Techniques for Burn PatientsDocument15 pagesPhysiotherapy Goals and Techniques for Burn PatientsPraneetha NouduriNo ratings yet
- Signs and TestsDocument4 pagesSigns and TestsKathryn RedNo ratings yet
- Acl Physio ProtocolDocument6 pagesAcl Physio ProtocolAna MorenoNo ratings yet
- ACL Reconstruction ProtocolDocument23 pagesACL Reconstruction ProtocolRoberto Tommasini100% (2)
- Lumbar Spinal Fusion Exercises - Jan20Document4 pagesLumbar Spinal Fusion Exercises - Jan20TrisnadewiNo ratings yet
- Arthroscopic Labrum Repair of The Shoulder (SLAP) : AnatomyDocument16 pagesArthroscopic Labrum Repair of The Shoulder (SLAP) : AnatomyDruga Danut100% (1)
- Rotator Cuff Repair EbookDocument31 pagesRotator Cuff Repair EbookJohnPaulBascoNo ratings yet
- SLAP Lesion Repair Operation: A Guide For PatientsDocument12 pagesSLAP Lesion Repair Operation: A Guide For PatientsCiro AlbuquerqueNo ratings yet
- Cast CareDocument4 pagesCast CareRogelyn PatriarcaNo ratings yet
- Lumbar Laminectomy Relief for SciaticaDocument3 pagesLumbar Laminectomy Relief for SciaticaIndah ChristyNo ratings yet
- After Surgery Rehabilitation Program MPFL ReconstructionDocument12 pagesAfter Surgery Rehabilitation Program MPFL ReconstructionNedelcu NicolaeNo ratings yet
- Anterior Labral (Bankart) RepairsDocument13 pagesAnterior Labral (Bankart) RepairsChris CarmenNo ratings yet
- Post-Operative Exercise Program: Knee Joint Replacement SurgeryDocument16 pagesPost-Operative Exercise Program: Knee Joint Replacement SurgeryRamses DagoyNo ratings yet
- Shoulder Post-Operative Rehabilitation ProtocolsDocument6 pagesShoulder Post-Operative Rehabilitation ProtocolsShrutiNo ratings yet
- Total Elbow Arthroplasty and RehabilitationDocument5 pagesTotal Elbow Arthroplasty and RehabilitationMarina ENo ratings yet
- Adhesive Capsulitis or Frozen SholderDocument24 pagesAdhesive Capsulitis or Frozen Sholdersanalcrazy100% (1)
- Knee Arthroscopy ProgramDocument26 pagesKnee Arthroscopy ProgramDavid StoevskiNo ratings yet
- Post-operative and Pre-Prosthetic Management for AmputeesDocument38 pagesPost-operative and Pre-Prosthetic Management for AmputeesTanzeelah RajawNo ratings yet
- Rehab Bankart RepairDocument20 pagesRehab Bankart RepairtaingsNo ratings yet
- Shoulder Protocol Bankart Information: How The Shoulder WorksDocument4 pagesShoulder Protocol Bankart Information: How The Shoulder WorksKartick PaiNo ratings yet
- Acl Rehab ProtocolDocument18 pagesAcl Rehab Protocolapi-256259376No ratings yet
- ACL ReconstructionDocument24 pagesACL Reconstructionsamabdelaal2000No ratings yet
- Clavicle Fracture Protocol After Surgical RepairDocument20 pagesClavicle Fracture Protocol After Surgical RepairNicoGeorgescuNo ratings yet
- Anterior Cervical Diskectomy and Fusion (ACDF) : What Is Done During The Surgery? What Are The Risks of The Surgery?Document3 pagesAnterior Cervical Diskectomy and Fusion (ACDF) : What Is Done During The Surgery? What Are The Risks of The Surgery?Adi KNo ratings yet
- Role of Physiotherapy in Management of Burns-HshDocument25 pagesRole of Physiotherapy in Management of Burns-HshChristopher Chibueze Igbo100% (1)
- Physiotherapy InformationDocument16 pagesPhysiotherapy InformationAlejandro SanchezNo ratings yet
- ACL Reconstruction Rehabilitation Protocol GuideDocument18 pagesACL Reconstruction Rehabilitation Protocol GuiderajadigitalNo ratings yet
- Slap Tears-Orthoinfo - AaosDocument6 pagesSlap Tears-Orthoinfo - Aaosapi-228773845No ratings yet
- Post-Op Knee Arthroscopy InstructionsDocument4 pagesPost-Op Knee Arthroscopy InstructionsTusan SidhartaNo ratings yet
- NHS UK Rotator Cuff RepairDocument5 pagesNHS UK Rotator Cuff RepairmertNo ratings yet
- Rotator Cuff RepairDocument5 pagesRotator Cuff RepairAdhitya TaslimNo ratings yet
- Freeletics Workout PlanDocument5 pagesFreeletics Workout PlanMiguel OrdoñezNo ratings yet
- Safety TipsDocument16 pagesSafety TipsAnonymous do9rmemPDNo ratings yet
- Lumbar Disc HerniationDocument8 pagesLumbar Disc Herniationandra_scooterNo ratings yet
- Arthroscopic Shoulder Anterior Stabilisation Rehabilitation Protocol by TENDAYI MUTSOPOTSI MSc. ORTHO-MEDDocument8 pagesArthroscopic Shoulder Anterior Stabilisation Rehabilitation Protocol by TENDAYI MUTSOPOTSI MSc. ORTHO-MEDPhysiotherapy Care SpecialistsNo ratings yet
- FNCP OutputDocument6 pagesFNCP OutputRenz AnggoyNo ratings yet
- Paramedian Forehead Flap Nasal Reconstruction Surgical TechniqueDocument10 pagesParamedian Forehead Flap Nasal Reconstruction Surgical Techniquetegegnegenet2No ratings yet
- ChepalotomaDocument14 pagesChepalotomarosaNo ratings yet
- Detecting Hemoperitoneum: Limitations of Repeat FAST ExamsDocument123 pagesDetecting Hemoperitoneum: Limitations of Repeat FAST ExamsSinisa Ristic50% (2)
- Kimia Farma Per 30 September ZRMM076Document271 pagesKimia Farma Per 30 September ZRMM076SriyatiNo ratings yet
- Gerson Therapy Handbook-5th-Revision PDFDocument118 pagesGerson Therapy Handbook-5th-Revision PDFCelia Steiman100% (1)
- BupropionDocument23 pagesBupropiontheintrovNo ratings yet
- Increased Intracranial Pressure NCLEX ReviewDocument8 pagesIncreased Intracranial Pressure NCLEX ReviewAnia JuanNo ratings yet
- Amniotic MembraneDocument8 pagesAmniotic Membraneapi-481789048No ratings yet
- Aubf MergeDocument164 pagesAubf MergeVia Gail CanlasNo ratings yet
- Anatomy of The Hepatobiliary System MaranDocument18 pagesAnatomy of The Hepatobiliary System Maransgod34No ratings yet
- 2 Pathophysiology EpidemiologyDocument36 pages2 Pathophysiology EpidemiologyYosefina CindyNo ratings yet
- Discharge Plan: Alawan Tate NiversityDocument2 pagesDischarge Plan: Alawan Tate NiversityLenieGracePascoNo ratings yet
- Rose Geranium in Sesame Oil NasalDocument3 pagesRose Geranium in Sesame Oil NasalHolly JonesNo ratings yet
- A Model To Predict Short-Term Death or Readmission After Intensive Care Unit DischargeDocument10 pagesA Model To Predict Short-Term Death or Readmission After Intensive Care Unit DischargeInnani Wildania HusnaNo ratings yet
- Ahlskog Et Al. Mayo Clin Proc 2011Document9 pagesAhlskog Et Al. Mayo Clin Proc 2011Thais AmandaNo ratings yet
- Angioedema 4Document18 pagesAngioedema 4Venosha GunasekaranNo ratings yet
- Clinical RotationDocument2 pagesClinical RotationDarwin QuirimitNo ratings yet
- Recurrent/Persistent Pneumonia Among Children in Upper EgyptDocument14 pagesRecurrent/Persistent Pneumonia Among Children in Upper EgyptLaila Ninda ShofiaNo ratings yet
- Psychiatric Case Write Up on Brief Psychotic DisorderDocument10 pagesPsychiatric Case Write Up on Brief Psychotic DisorderBen Man JunNo ratings yet
- Cerebrovascular AccidentDocument62 pagesCerebrovascular AccidentJaydee DalayNo ratings yet
- The Voice of PLC 1101Document6 pagesThe Voice of PLC 1101The Plymouth Laryngectomy ClubNo ratings yet
- Infectious Bronchitis and Its Effect On Egg Production and Egg QualityDocument2 pagesInfectious Bronchitis and Its Effect On Egg Production and Egg QualityPrima Puji RaharjoNo ratings yet
- Ent Bcqs 2Document22 pagesEnt Bcqs 2Ghazi Uddin Ahmed100% (1)
- Pathophysiology A Clinical Approach 2nd Edition Braun Anderson Test BankDocument36 pagesPathophysiology A Clinical Approach 2nd Edition Braun Anderson Test Bankbeswikemysteryy6rpNo ratings yet
- JCDP 22 310Document6 pagesJCDP 22 310Anand MohattaNo ratings yet
- Inflammatory Bowel Disease and Carcinogenesis: Hiroko Nagao Kitamoto Sho Kitamoto Nobuhiko KamadaDocument16 pagesInflammatory Bowel Disease and Carcinogenesis: Hiroko Nagao Kitamoto Sho Kitamoto Nobuhiko KamadaDiego Fernando Ortiz TenorioNo ratings yet
- Informed Consent For Lasik SurgeryDocument2 pagesInformed Consent For Lasik SurgeryMoerieda RinquestNo ratings yet
- H. PyloriDocument5 pagesH. PyloriWaleed El SaidNo ratings yet
- Surat Dental 181Document15 pagesSurat Dental 181deva nesanNo ratings yet