Professional Documents
Culture Documents
Administration of Oral Medication: Practical Procedures
Uploaded by
Nom NomOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Administration of Oral Medication: Practical Procedures
Uploaded by
Nom NomCopyright:
Available Formats
PRACTICAL PROCEDURES
Administration of
oral medication
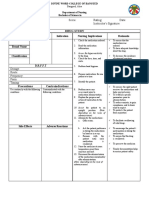
AUTHOR Andy Ferguson, RN, is The prescription should be
registered nurse, emergency care, legible and unambiguous and
Birmingham Children’s Hospital. should be signed and dated by
the prescribing practitioner.
Administration of medication is The prescription chart should be
more than a task to be done in labelled with the patient’s name,
compliance with a prescription date of birth and hospital
(NMC, 2004). It requires nurses to identification number. It should
understand the prescription and also clearly state whether the
to have knowledge of common patient has any known allergies. Fig 1. Check the information on the prescription
indications, dosages and side- Good practice states that the
effects of the medications. patient’s weight be recorded on
Should any error occur during the prescription sheet for any
the procedure the practitioner has weight-related dosages, such as
a professional responsibility to therapeutic doses for low
report this in accordance with molecular weight heparin or for
local risk management procedures. medicines for children.
Ultimately, the practitioner is
responsible for ensuring the Checking the medication
correct patient, dose, drug, time Policies regarding the appropriate
and route. practitioner and number of
practitioners needed to check oral
Preparing to administer medication may vary. Exceptions
All equipment required to to this include controlled drugs
administer the medication should and medicines for children, both
be gathered before the procedure. of which need to be checked by
This may include: two registered nurses.
● Any necessary keys; The nurse should check, as
Fig 2. Select the medication and check the expiry date
● Prescription charts; a minimum:
● Clean dispensing pots; ● The generic name of the drug;
● Drug reference books. ● The dose required;
Gathering equipment prior to ● The time for administration;
the procedure reduces ● That the drug has not already
interruptions and the risk of error been given (or taken by
associated with these. the patient);
Thorough handwashing should ● That the prescription is legible,
be performed. Hands should be signed and dated;
cleansed between patients to ● The expiry date of the drug;
reduce the risk of cross-infection. ● That the patient does not have
any known allergy or sensitivity
The prescription to the drug.
Local policies vary slightly on the
requirements for legitimate Patient identity
prescription. As a minimum the The practitioner must verify that
prescription should include: the patient receiving the medicine
● The generic name of the drug is the patient for whom it is
(not the trade name); prescribed. The most common Fig 3. Check the patient’s identity using their hospital name band
● The dose to be given; and convenient way to do this is
● The time for administration; to check that the details on the
SPL
● The route of administration. patient’s hospital identification
24 NT 8 November 2005 Vol 101 No 45 www.nursingtimes.net
KEYWORDS ■ Medication ■ Drug administration ■ Risk management
band match those on the REFERENCES
prescription chart.
If the patient does not have an Morris, H. (2005) Administering
identification band, or for patients drugs to patients with swallowing
in areas such as A&E, it is difficulties. Nursing Times;
necessary to verbally confirm the 101: 39, 28–29.
identity of patients by asking
them to state their name and Nursing and Midwifery Council
date of birth. (2004) Guidelines for the
Administration of Medicines.
London: NMC.
Administration
Medicines should be dispensed
into a clean, dry and preferably
disposable container.
Where liquid preparations are
used, these should be measured
using syringes specifically
Fig 4. To avoid touching the medication, empty the prescribed dose into the designed for this purpose.
lid of the bottle then into a clean dispensing container Informed consent should be
sought and this will involve
assessing the patient’s knowledge
of the medication and providing
information where necessary.
Patients have the right to refuse
medication. If this occurs it should
be correctly documented and
reported to the prescribing health
care professional.
The patient should be helped
into a comfortable position and
assisted if necessary.
If the patient is not present
when the medication is due or
does not wish to take it then, the
practitioner should return later.
Medicines should never be left out
Fig 5. Liquid medication should be measured in a specialist oral syringe and
administered immediately for the patient to take later.
Medication must be given in
the prescribed manner and
tablets should not be crushed
(Morris, 2005).
Documentation
The practitioner should sign the PROFESSIONAL
prescription to verify that the RESPONSIBILITIES
medication has been administered. All nurses who administer
Only when the patient has taken medication must have
the medication should the chart be undertaken a programme of
signed. It is not acceptable to sign education and demonstrated
the chart when the medication is competence under supervision.
placed into the container. The practitioner is responsible
The effectiveness of the for ensuring that her or his
medication should be documented. practice is compliant with the
Following the procedure, the NMC guidelines (NMC, 2004).
Fig 6. Document that the medication has been given on the prescription practitioner should ensure that all The practitioner should also
chart, according to local policy equipment is replaced and that all ensure that she or he is familiar
medicines are stored in with local trust policies.
compliance with local policy. ■
NT 8 November 2005 Vol 101 No 45 www.nursingtimes.net 25
You might also like
- Medication Pathway (Prescription) PDFDocument162 pagesMedication Pathway (Prescription) PDFChristine Annmarie TapawanNo ratings yet
- Medication Error 2017Document51 pagesMedication Error 2017Christina100% (1)
- Administering Oral Medication (Print)Document5 pagesAdministering Oral Medication (Print)Binoy Serino100% (1)
- 12 Rights of Administering MedicationDocument2 pages12 Rights of Administering Medicationlilcheeza77% (74)
- Medication SafetyDocument54 pagesMedication SafetyJuwitaASih100% (2)
- 10 Rights of Drug Administration With Nursing ImplicationsDocument3 pages10 Rights of Drug Administration With Nursing ImplicationsJet Bautista100% (6)
- Medications OSCE Criteria 2011-12Document3 pagesMedications OSCE Criteria 2011-12Kim GuevarraNo ratings yet
- 5 PlasterDocument3 pages5 PlasterMuhammad AgungNo ratings yet
- Module 3 Pharma Safety and Quality of Drug Administration Final PDFDocument10 pagesModule 3 Pharma Safety and Quality of Drug Administration Final PDFMichelle HutamaresNo ratings yet
- Guide To Good Dispensing PracticeDocument7 pagesGuide To Good Dispensing PracticeGizelle Mae Pasiol-MacayanNo ratings yet
- Coefficient of Thermal ExpansionDocument6 pagesCoefficient of Thermal ExpansionemiljuchiacNo ratings yet
- What A Plant Smells PDFDocument4 pagesWhat A Plant Smells PDFCarlos Javier TejadaNo ratings yet
- Good Dispensing PracticeDocument59 pagesGood Dispensing Practicechalii100% (1)
- Module 4 - Nursing Process and Administration-PharmaDocument13 pagesModule 4 - Nursing Process and Administration-PharmaKelsey MacaraigNo ratings yet
- Pharma Nursing ApplicationDocument53 pagesPharma Nursing ApplicationRiegne Chiara Fay AcuzarNo ratings yet
- 03 Rights in Giving MedicationsDocument4 pages03 Rights in Giving MedicationsJAN CAMILLE LENONNo ratings yet
- CH 03Document18 pagesCH 03Emmanuel GaliciaNo ratings yet
- Nur 1208 2021 Prep of MedsDocument38 pagesNur 1208 2021 Prep of MedsDannielle EvangelistaNo ratings yet
- Prin - of Drug AdministrationDocument4 pagesPrin - of Drug AdministrationAzhly AntenorNo ratings yet
- Administering Medication Via Small-Volume Nebulizer DefinitionDocument5 pagesAdministering Medication Via Small-Volume Nebulizer DefinitionNessy Nicholle SatruionNo ratings yet
- Procedures RationaleDocument3 pagesProcedures RationaleJamaica Leslie NovenoNo ratings yet
- Concepts and Principles of Pharmacology To Ensure Safe and Proper Use of DrugsDocument21 pagesConcepts and Principles of Pharmacology To Ensure Safe and Proper Use of DrugsBea Bianca CruzNo ratings yet
- Module 3.1 - Safety in Medication AdministrationDocument29 pagesModule 3.1 - Safety in Medication AdministrationAkio OzaragaNo ratings yet
- Module 3.1 - Safety in Medication AdministrationDocument29 pagesModule 3.1 - Safety in Medication AdministrationAkio OzaragaNo ratings yet
- Role of Pharmacist in Rational DispensingDocument6 pagesRole of Pharmacist in Rational DispensingGohar MalikNo ratings yet
- Contiunuity of Care SlidesDocument31 pagesContiunuity of Care SlidesYovi pransiska JambiNo ratings yet
- 1-Guidelines For Safe Medication Adminstration (Non Parentral Medication Adminstration)Document6 pages1-Guidelines For Safe Medication Adminstration (Non Parentral Medication Adminstration)onco learnNo ratings yet
- Administration of MedicationDocument10 pagesAdministration of MedicationYeesha Palacio BalmesNo ratings yet
- 12 Rights of Administering Medication PDF Dose (Biochemistry) ChemistryDocument1 page12 Rights of Administering Medication PDF Dose (Biochemistry) ChemistryTina Michelle DazaNo ratings yet
- PN-Chapter 1-Introduction To PharmacologyDocument14 pagesPN-Chapter 1-Introduction To PharmacologymysNo ratings yet
- Unit 4-InpatientDocument38 pagesUnit 4-InpatientSharmila LamisharNo ratings yet
- Administering Medication Via A Metered Dose InhalerDocument7 pagesAdministering Medication Via A Metered Dose InhalerGio TalomiaNo ratings yet
- Medication Safety: Mita Restinia, M.Farm, AptDocument57 pagesMedication Safety: Mita Restinia, M.Farm, Apt094DNORMINo ratings yet
- Module 2 - Preparation of Standard Patient Scripting, Incident Reporting and Usual Company Policies and RegulationsDocument41 pagesModule 2 - Preparation of Standard Patient Scripting, Incident Reporting and Usual Company Policies and RegulationsCharles DapitoNo ratings yet
- 2018 Pharm Good-Prescribing-PracticeDocument4 pages2018 Pharm Good-Prescribing-PracticeOlivia StevensNo ratings yet
- Drug Study NCP Template 2Document2 pagesDrug Study NCP Template 2Janico Lanz BernalNo ratings yet
- Principles of Medication AdministrationDocument10 pagesPrinciples of Medication AdministrationEarl BenedictNo ratings yet
- Mindanao State University - Iligan Ins Tute of Technology College of NursingDocument4 pagesMindanao State University - Iligan Ins Tute of Technology College of NursingNessy Nicholle SatruionNo ratings yet
- Administering Medication Via A SmallDocument6 pagesAdministering Medication Via A SmallAndrea Bayaga WaganNo ratings yet
- Safety and QualityDocument24 pagesSafety and QualityPaula Janine BarrogaNo ratings yet
- RUD Dispensers - July 22, NKDocument43 pagesRUD Dispensers - July 22, NKAbdul MutholibNo ratings yet
- Microsoft Word - SOP ON DispensingDocument4 pagesMicrosoft Word - SOP ON DispensingPalawan Baptist HospitalNo ratings yet
- Pharamacology Notes 3Document7 pagesPharamacology Notes 3Martinet CalvertNo ratings yet
- Med Brought Into Hospital3Document5 pagesMed Brought Into Hospital3Nina JuanNo ratings yet
- Developing A Measure For The Appropriateness of Prescribing in General PracticeDocument5 pagesDeveloping A Measure For The Appropriateness of Prescribing in General Practiceujangketul62No ratings yet
- M5 Continuation Dispensing ProcessDocument32 pagesM5 Continuation Dispensing Processcbun22222No ratings yet
- DISPENSINGDocument1 pageDISPENSINGJENSEL CLOUIE C. REGLOSNo ratings yet
- Ceftriaxone, IndiaDocument5 pagesCeftriaxone, IndiaTya ALditsa SadegaNo ratings yet
- Administering Nasal MedicationsDocument4 pagesAdministering Nasal MedicationsNessy Nicholle SatruionNo ratings yet
- Medicine Use Evaluation: A Guide To ImplementationDocument26 pagesMedicine Use Evaluation: A Guide To ImplementationmrboredguyNo ratings yet
- Learning Activity 2 Philosophy in NursingDocument9 pagesLearning Activity 2 Philosophy in NursingJoseph AbangNo ratings yet
- Pharmacology (DNPC 4122) : Nur Adilah Rasyadah Binti Suhaimi 3042191093Document12 pagesPharmacology (DNPC 4122) : Nur Adilah Rasyadah Binti Suhaimi 3042191093Suhaimi ShafieNo ratings yet
- Rectal Suppository Procedure With Rationale 1Document5 pagesRectal Suppository Procedure With Rationale 1yuuki konnoNo ratings yet
- Rights of Drug AdministrationDocument4 pagesRights of Drug AdministrationAnusha VergheseNo ratings yet
- Pharma Part 3Document6 pagesPharma Part 3Bee LeriosNo ratings yet
- Review of Pharmaceutical Care Services Provided by The PharmacistsDocument3 pagesReview of Pharmaceutical Care Services Provided by The PharmacistsellianaeyNo ratings yet
- Unit 3-OutpatientDocument38 pagesUnit 3-OutpatientSharmila LamisharNo ratings yet
- Challenges To Effective Drug TherapyDocument5 pagesChallenges To Effective Drug TherapyAlyssaGrandeMontimorNo ratings yet
- Five Essential Rights in Administering Medication: Jay Mark M. ArizabalDocument3 pagesFive Essential Rights in Administering Medication: Jay Mark M. ArizabalAriz J M KingNo ratings yet
- ID Checklist RATIONALEDocument42 pagesID Checklist RATIONALEAT4-11 HUMSS 2 CEDRICK ILAONo ratings yet
- Lucy MallowDocument18 pagesLucy MallowbutiljohnnemradNo ratings yet
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceFrom EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceRating: 3 out of 5 stars3/5 (1)
- Drug Administration in Nursing: A Comprehensive Guide to Drug Administration and Calculation in NursingFrom EverandDrug Administration in Nursing: A Comprehensive Guide to Drug Administration and Calculation in NursingNo ratings yet
- Improving The Vase Life of Cut Gerbera Flower With Silver NanoparticlesDocument4 pagesImproving The Vase Life of Cut Gerbera Flower With Silver NanoparticlesThanhTung NguyenNo ratings yet
- 5L@35m Hydro - Multi-B - E - 2 - CR - 20-3Document5 pages5L@35m Hydro - Multi-B - E - 2 - CR - 20-3lilama45-1No ratings yet
- Material Steel StandardsDocument25 pagesMaterial Steel StandardssamadhankadamNo ratings yet
- Scientific Validation of Standardization of Narayana Chendrooram (Kannusamy Paramparai Vaithiyam) Through The Siddha and Modern TechniquesDocument12 pagesScientific Validation of Standardization of Narayana Chendrooram (Kannusamy Paramparai Vaithiyam) Through The Siddha and Modern TechniquesBala Kiran GaddamNo ratings yet
- Himatanthus DrasticusDocument6 pagesHimatanthus Drasticusdavidlopesdasilva2No ratings yet
- Tensar Basetex Technical Info (April 2003)Document4 pagesTensar Basetex Technical Info (April 2003)sandycastleNo ratings yet
- CX ISOMILL 331 - TDS - EN - 2018 - 03 - 16 v1Document1 pageCX ISOMILL 331 - TDS - EN - 2018 - 03 - 16 v1Rafael Obusan IINo ratings yet
- Experimental Techniques For Measuring Sewing Needle TemperatureDocument8 pagesExperimental Techniques For Measuring Sewing Needle TemperatureATLASNo ratings yet
- 8 2 7Document19 pages8 2 7Hussain AbouelkhairNo ratings yet
- CND 4.medication & Dispensing ErrorDocument32 pagesCND 4.medication & Dispensing Errorlisnawati farmasicbthNo ratings yet
- CryopreservationDocument18 pagesCryopreservationgaurav saxenaNo ratings yet
- Stone Patina. A Controversial Concept of Relevant Importance in ConservationDocument13 pagesStone Patina. A Controversial Concept of Relevant Importance in ConservationdelagaugljevikNo ratings yet
- CBSE Class X Science Acids Bases and Salts Important Questions Paper 2012Document5 pagesCBSE Class X Science Acids Bases and Salts Important Questions Paper 2012MahenderGoelNo ratings yet
- The Role of Titanite (CaTiSiO ) in PCD ExplorationDocument9 pagesThe Role of Titanite (CaTiSiO ) in PCD ExplorationMarco Augusto Robles AncajimaNo ratings yet
- Biochem AnswersDocument3 pagesBiochem AnswersPat FerrerNo ratings yet
- Enhanced Tribological Properties of Wind Turbine Engine Oil Formulated With Flower-Shaped MoS2 Nano-AdditivesDocument10 pagesEnhanced Tribological Properties of Wind Turbine Engine Oil Formulated With Flower-Shaped MoS2 Nano-AdditivesZoubir SaidiNo ratings yet
- EN-Genano-350 Datasheet LowresDocument2 pagesEN-Genano-350 Datasheet LowresLeader Healthcare Power CafeNo ratings yet
- Citrosteril Disinfectant 101Document2 pagesCitrosteril Disinfectant 101Darnel Perino CabañingNo ratings yet
- Summarized Research PresentationDocument4 pagesSummarized Research PresentationDaryl A. Dela CruzNo ratings yet
- Rocks PDFDocument5 pagesRocks PDFfatwa27No ratings yet
- DP1SL Redox UT VCDocument6 pagesDP1SL Redox UT VCmarilee huntNo ratings yet
- Pt. Tekenomiks Indonesia: Fuel Analysis ReportDocument1 pagePt. Tekenomiks Indonesia: Fuel Analysis Reportfirman manaluNo ratings yet
- Gönen, Turan-Modern Power System Analysis-CRC Press (2013)Document47 pagesGönen, Turan-Modern Power System Analysis-CRC Press (2013)Anand KalNo ratings yet
- Reactions and Stoichiometry Cheat Sheet: by ViaDocument3 pagesReactions and Stoichiometry Cheat Sheet: by ViaNeia De JesusNo ratings yet
- Bonga University Instrumental Analysis II: (Chem.2052)Document56 pagesBonga University Instrumental Analysis II: (Chem.2052)ashenafiNo ratings yet
- 186 Soldering Flux MSDSDocument5 pages186 Soldering Flux MSDSNicolae ChirilaNo ratings yet
- Maraging Steel - WikipediaDocument5 pagesMaraging Steel - WikipediaVysakh VasudevanNo ratings yet