Professional Documents
Culture Documents
Alikhan I 2014
Alikhan I 2014
Uploaded by
WahyunitadotokaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alikhan I 2014
Alikhan I 2014
Uploaded by
WahyunitadotokaCopyright:
Available Formats
Jundishapur J Microbiol. 2014 January; 7(1): e8888.
DOI: 10.5812/jjm.8888
Published online 2014 January 1. Research Article
Antimicrobial Resistance Patterns and Prevalence of blaPER-1 and blaVEB-1
Genes Among ESBL-producing Pseudomonas aeruginosa Isolates in West of
Iran
1 1 1 2
Mohammad Yousef Alikhani ; Zahra Karimi Tabar ; Fatemeh Mihani ; Enayat Kalantar ;
1 3 4 5,*
Pegman Karami ; Mahnaz Sadeghi ; Shiva Ahdi Khosroshahi ; Safar Farajnia
1Department of Microbiology, Faculty of Medicine, Hamadan University of Medical Sciences, Hamadan, IR Iran
2Department of Microbiology, School of Medicine, Alborz University of Medical Sciences, Alborz, IR Iran
3Tuberculosis and Lung Research Center, Tabriz University of Medical Sciences, Tabriz, IR Iran
4Biotechnology Research Center, Tabriz University of Medical Sciences, Tabriz, IR Iran
5Drug Applied Research Center, Tabriz University of Medical Sciences, Tabriz, IR Iran
*Corresponding author: Safar Farajnia, Drug Applied Research Center, Tabriz University of Medical Sciences, Daneshgah Ave., Postal Code: 51656-65811, Tabriz, IR Iran. Tel: +98-
9143018589, Fax: +98-4113363231, E-mail: farajnias@tbzmed.ac.ir
Received: November 15, 2012; Revised: January 23, 2013; Accepted: March 14, 2013
Background: Pseudomonas aeruginosa is a leading cause of nosocomial infections worldwide. Resistance of P. aeruginosa strains to the
broad-spectrum cephalosporins may be caused by extended-spectrum β-lactamases (ESBLs).
Objectives: The aim of this study was to determine the antimicrobial resistance patterns and prevalence of PER-1 and VEB-1 type genes
among ESBL producing strains of P. aeruginosa.
Material and Methods: A total of 106 P. aeruginosa isolates were collected from two university hospitals in Hamadan, Iran, during a7-
month study (2009). The antimicrobial susceptibility of isolates was determined by disc diffusion method and interpreted according to
the clinical and laboratory standards institute (CLSI) recommendations. Production of ESBL was determined by combined disk test and
presence of PER-1 and VEB-1 type ESBL genes was identified by PCR.
Results: The resistance against broad-spectrum cephalosporins and monobactames were: cefepime (97%), cefotaxime (92.5%) ceftazidime
(51%), and aztreonam (27%). Ciprofloxacin (91.5%), imipenem (84.9%) and meropenem (82.1%) were the most effective anti-pseudomonas
agents in this study. The results revealed that 88.7% of the isolates were multidrug resistant, 58.25% of those were ESBL positive. Sixteen
(26.6%), 9 (15%) and 3 (5%) strains among ESBL-producing strains contained blaPER-1, blaVEB and blaPER-1-blaVEB, respectively.
Conclusions: This study highlighted the need to establish antimicrobial resistance surveillance networks for P. aeruginosa to determine
the appropriate empirical treatment regimens. The high prevalence of multidrug resistance and production of ESBLs in P. aeruginosa
isolates confirms the necessity of protocols considering these issues in the hospitals.
Keywords: Pseudomonas aeruginosa; Antimicrobial Drug Resistance; Beta-lactamase
1. Background some difficulties, because this bacterium not only has an
inducible AmpC enzyme but also has an efflux-mediated
Pseudomonas aeruginosa is an important cause of noso-
resistance and a higher degree of impermeability than
comial infections, including pneumonia, burn infection,
Enterobacteriaceae (10, 11). The PER-1 and VEB-1 type ESBLs
urinary tract infections, meningitis and bacteremia. The
belong to class A of β- lactamases and is associated with
infections can be particularly develop to a severe form in
high level of resistance to cephems, monobactams and
immune deficient patients (1). Antibiotics have been used
ceftazidime (12, 13).
successfully for several decades, but resistance genes
have emerged and disseminated particularly in the last 2. Objectives
few years (2).
Extended-spectrum β-lactamases (ESBLs) mediate resis- The aim of this study was to determine the antibacterial
tance to various broad-spectrum cephalosporins, includ- resistance patterns and prevalence of PER-1 and VEB type
ing cefotaxime, ceftriaxone, ceftazidime, and aztreonam ESBLs among P. aeruginosa isolated from patients in west
(3). These enzymes originally collected from Klebsiella of Iran.
pneumoniae and Escherichia coli and recently from P. ae- 3. Materials and Methods
ruginosa (4-7). Most of the methods for detection of ESBLs
are used in bacterial species such as Klebsiella and E. coli
3.1. Bacterial Isolates
lacking chromosomal β-lactamase activity (8, 9), Howev-
er, the detection of ESBL production in P. aeruginosa has A total of 106 isolates of P. aeruginosa recovered from
Implication for health policy/practice/research/medical education:
This study highlights the need for an antimicrobial resistance surveillance network for P. aeruginosa to monitor the trends and new types of resistance
mechanism emerging.
Copyright © 2014, Ahvaz Jundishapur University of Medical Sciences; Published by Kowsar Corp. This is an open-access article distributed under the terms of the Cre-
ative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Alikhani MY et al.
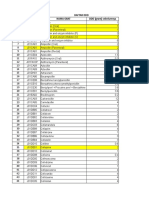
various clinical specimens (Table 1) in Beasat Teaching ing combine disk test (CDT) as CLSI recommendations.
Hospital at the Hamadan University of Medical Scienc- CDT were performed on ceftazidime, cefotaxime, ce-
es during a 7-month study in 2009. The identification fepime and aztreonam resistant strains by placing disks
were carried out by colonial morphology, positive of ceftazidime, and cefotaxime (30 µg each) at a 20 mm
oxidase test, pigment formation; growth test at 42ºC distance from a disk containing ceftazidime-clavulanic
on nutrient agar, Gram staining and motility test. acid (30/10 µg), cefotaxime-clavulanic acid (30/10µg) and
cefepime-clavulanic acid (30/10 µg) (16). ESBL production
Table 1. Distribution of P. seudomonas aeruginosa by Site of was inferred when the cephalosporin inhibitory zones
Isolation were expanded by the clavulanate.
Source Isolates, No. (%)
3.4. PCR Amplification
Burn wounds 55 (51.9)
PCR amplifications were done using specific primers
Trashes 20 (18.9) for the β-lactamases PER-1, and VEB-1 genes, as described
Urine 12 (11.3) previously (17). PCR was performed for all ESBL-producers
Blood 7 (6.6) which their resistance to cephalosporins and phenotypic
Feces 6 (5.7)
was identified by confirmatory tests. DNA was extracted
by the boiling method as previously described (17). The
Sputum 5 (4.7)
DNA amplification program consisted of an initial de-
CSFa 1 (0.9) naturation (94 °C, 5 minutes) followed by 35 cycles of
Total 106 (100) denaturation (94 °C, 60 seconds), annealing (50 °C for
a Abbreviation: CFS, Cerebral spinal fluid PER-1 and 55 °C for VEB-1, 60 seconds), extension (72 °C,
45 seconds) and a single final extension for 5 minutes at
72 °C. Reaction mixtures for PCR contained 1.5mM MgCl2,
3.2. Antibiotic Susceptibility Test 0.5 mM of each primer, 0.2 mM of dNTPs, 1 U of Taq poly-
Antibiotic susceptibility of the isolates was determined merase, 1X PCR buffer and 2 µL of DNA. Primers PER-F
by standard disk diffusion method (14). The following an- (5-AATTTGGGCTTAGGGCAGAA-3') and PER-R (5'-ATGAAT-
tibiotics were used: gentamicin (30 µg), aztreonam (30
GTCATTATAAAAGC-3') were used for blaPER-1; and VEB-F
µg), meropenem (10 µg), imipenem (10 µg), amikacin (30
(5'-CGACTTCCATTTCCCGATGC-3') and VEB-R (5'-GGACTCT-
µg), tobramycin (30 µg), piperacillin (30 µg), ceftazidime
GCAACAAAT AC GC-3') were used for blaVEB-1 amplifica-
(30 µg), ciprofloxacin (5 µg), ofloxacin (5 µg), cefepime (30
tion.
µg) and cefotaxime (30 µg) (Himedia, India). P. aeruginosa
ATCC 27853 was used as control. The results were inter- 4. Results
preted according to the clinical and laboratory standards
institute (CLSI) (15).
4.1. Antimicrobial Susceptibility Test
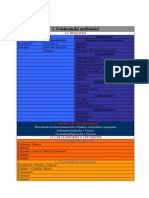
3.3. Phenotypic Detection of Beta-Lactamase Table 2 shows the antimicrobial susceptibility pattern
The isolates were tested for the ESBLs production by us- of P. aeruginosa strains. Ciprofloxacin (91.5%), imipenem
Table 2. Antimicrobial Susceptibility Pattern of P. aeruginosa Strains
Antimicrobials Resistance, No. (%) Sensitive, No. (%) Intermediate, No. (%)
Amikacin 32 (30.2) 70 (66) 4 (3.8)
Ceftazidime 54 (51) 40 (37.7) 12(11.3)
Aztreonam 29 (27.4) 70 (66) 7 (6.6)
Cefepime 103 (97.2) 1 (0.9) 2 (1.9)
cefotaxime 53 (50) 10 (9.4) 43 (40.6)
Ciprofloxacin 5 (4.7) 97 (91.5) 4 (3.8)
Gentamicin 39 (36.8) 55 (51.9) 12 (11.3)
Imipenem 8 (7.5) 90 (84.9) 8 (7.5)
Meropenem 14 (13.2) 87 (82.1) 5 (4.7)
Ofloxacin 31 (29.2) 72 (67.9) 3 (2.8)
Piperacillin 99 (93.4) 7 (6.6) 0
Tobramycin 39 (36.8) 67 (63.2) 0
2 Jundishapur J Microbiol. 2014;7(1):e8888
Alikhani MY et al.
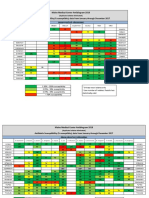
(84.9%) and meropenem (82.1%) were the most active an- ESBL Production: Among 106 isolates, 94 (88.7%) were
timicrobial agents followed by ofloxacin (67.9% suscepti- multidrug resistant and 60(58.3%) were putative ESBL pro-
bility). Aztreonam, a monobactam, and amikacin showed ducers using phenotypic confirmatory tests (Table 3). Six-
antibiotic activity against 66% of the strains. Susceptibil- teen (26.6%), 9 (15%) and 3 (5%) strains among 60 ESBL-pro-
ity to the cephalosporins was reduced to 37.7% for ceftazi- ducing strains had blaPER-1 (Figure 1), blaVEB-1 (Figure 2),
dime, followed by cefotaxime (9.4%) and Cefepime (0.9%). and blaPER-1- blaVEB related genes, respectively (Table 4).
Table 3. Susceptibility Pattern to Antimicrobial Agents in ESBLs and non ESBLs-producing P. aeruginosa Strains
ESBL Positive (n=60) ESBL Negative (n=46)
Antimicrobials Resistant, No. Susceptible, Intermediate, Resistant, No. Susceptible, Intermediate,
(%) No. (%) No. (%) (%) No. (%) No. (%)
Amikacin 29 (48.3) 30 (50) 1 (1.7) 4 (9.3) 37 (86) 2 (4.7)
Ceftazidime 40 (66.7) 18 (30) 2 (3.3) 13 (28.3) 24 (55.2) 6 (13)
Aztreonam 25 (41.7) 32 (53.3) 3 (5) 3 (6.97) 39 (90.69) 1 (2.32)
Cefepime 58 (96.7) 0 2 (3.3) 42 (97.67) 1 (2.32) 0
cefotaxime 41 (68.3) 6 (10) 13 (21.7) 12 (27.90) 3 (6.97) 28 (65.11)
Ciprofloxacin 5 (8.3) 50 (83.3) 5 (8.3) 0 42 (97.67) 1 (2.32)
Gentamicin 32 (53.3) 28 (46.7) 0 7 (16.27) 36 (83.72) 0
Imipenem 7 (11.7) 45 (75) 8 (13.3) 1 (2.32) 41 (95.34) 1 (2.32)
Meropenem 13 (21.7) 44 (73.3) 3 (5) 2 (4.65) 39 (90.69) 2 (4.65)
Ofloxacin 30 (50) 29 (48.3) 1 (1.7) 4 (9.30) 37 (86.04) 2 (4.65)
Piperacillin 54 (90) 6 (10) 0 41 (95.34) 2 (4.65) 0
Tobramycin 31 (51.6) 28 (46.7) 1 (1.7) 4 (9.30) 39 (90.69) 0
Table 4. Association of Antimicrobial Resistance Pattern and ESBL Genotypes
PER-1:16 (26.6%) VEB: 9 (15%)
Antimicrobials Resistant, No. Susceptible, Intermediate, Resistant, No. Susceptible, Intermediate,
(%) No. (%) No. (%) (%) No. (%) No. (%)
Amikacin 10 (62.5) 5 (31.25) 1(6.25) 5 (55.5) 2 (22.2) 2 (22.2)
Ceftazidime 12 (75) 4 (25) 0 9 (100) 0 0
Aztreonam 10 (62.5) 4 (25) 2 (12.5) 9 (100) 0 0
Cefepime 16 (100) 0 0 9 (100) 0 0
cefotaxime 87.5 (14) 0 2 (12.5) 9 (100) 0 0
Ciprofloxacin 2 (12.5) 13 ( 81.25) 1 (6.25) 2 (22.2) 6 (66.6) 1 (11.11)
Gentamicin 10(62.5) 6 ( 37.5 ) 0 6 (66.6) 3 (33.3) 0
Imipenem 5 (31.25) 5 (31.25) 6 (37.5) 1 (11.11) 6 (66.6) 2 (22.2)
Meropenem 7 ( 43.75) 8 (50) 1 (6.25) 6 (66.6) 2 (22.2) 1 (11.11)
Ofloxacin 11 (68.8) 5 (31.25) 0 8 (88.8) 1 (11.11) 0
Piperacillin 16 (100) 0 0 9 (100) 0 0
Tobramycin 10 (62.5) 6 ( 37.5 ) 0 6 (66.6) 3 (33.3) 0
Jundishapur J Microbiol. 2014;7(1):e8888 3
Alikhani MY et al.
sistant to ≥ 3 different antibiotic classes) (20-25).
Figure 1. PCR Amplification of blaPER-1 Gene
The prevalence of ESBL- producing P. aeruginosa iso-
lates in this study was also higher than other investiga-
tions (5, 20, 26, 27). Among 60 ESBL-positive strains, 16
(26.6%), 9 (15%) and 3 (5%) contained PER-1, VEB-1 and PER-1-
VEB-1 genes, respectively. These results indicated that the
prevalence of VEB-1 gene in our area, is higher than Turkey
and Korea, but the prevalence of VEB-1 and PER-1 genes, is
lower than in Thailand (94.44% blaVEB-1) and Italy (34.61%
blaPER-1) (5, 13, 26). Data on the prevalence of ESBL- pro-
ducing P. aeruginosa strains in our area is limited. In the
1000 bp study performed by Shahcheraghi and colleges on P. ae-
900 bp
800 bp ruginosa isolates in Tehran, the rate of blaVEB and blaPER
700 bp ESBLs were reported 24% and 17%, respectively, that was
600 bp
500 bp similar to our results (28). The high prevalence of PER-
400 bp 1 and VEB-1 indicated the high resistance to penicillins,
300 bp ceftazidime and cefotaxime, as reported by other studies
200 bp
100 bp (26, 29).
This is the first report about the presence of these en-
zymes in P. aeruginosa isolates from west of Iran. It has
shown that ESBL production in strains of P. aeruginosa can
L: 100 bp DNA ladder, C-: negative control, C+: positive control, N: PER-1
negative strains, 1–3: PCR products from PER-1positive strains.
greatly complicate the clinical management of infection
if advanced care is not taken. However, further studies
are needed to determine other ESBL- types in P.aeruginosa
Figure 2. PCR Amplification of blaVEB-1 Gene strains in this area and their role in resistance to other
antibiotic classes. The results of this study emphasizes
on the need for a surveillance network to monitor the
trends and emerge of new resistance mechanism in P.
aeruginosa from different geographic regions. Therefore,
the improvement in antibiotic prescription policies and
infection control programs are of high necessity to pre-
vent the spread of such resistant infectious agents.
Acknowledgements
1000 bp
No Acknowledgments.
500 bp
Authors’ Contribution
All authors contributed in the research equally.
100 bp
L: 100 bp DNA ladder, C-: negative control, C+: positive control, N: negative
Financial disclosure
strain, 1–4: PCR products fromVEB-1 positive strains. There is not any financial interest.
Funding/Support
5. Discussion
This work was financially supported by Hamadan and
P. aeruginosa has a high resistance to antibiotics and is Tabriz University of Medical Sciences.
a common cause of morbidity and mortality in hospital-
ized and immunocompromised patients (18). Treatment
References
of P. aeruginosa infections is complicated by the inhered
1. Pagani L, Mantengoli E, Migliavacca R, Nucleo E, Pollini S, Spalla
and acquired resistance to the most of commonly used M, et al. Multifocal detection of multidrug-resistant Pseudomo-
antimicrobial agents (19). The results from this study nas aeruginosa producing the PER-1 extended-spectrum beta-
showed the high resistance of P. aeruginosa to most of lactamase in Northern Italy. J Clin Microbiol. 2004;42(6):2523–9.
2. Isturiz RE, Carbon C. Antibiotic use in developing countries. In-
used antimicrobial agents. It was also demonstrated that
fect Control Hosp Epidemiol. 2000;21(6):394–7.
the prevalence of antibiotic resistance of the isolates was 3. Livermore DM, Brown DF. Detection of beta-lactamase-mediated
very high in comparison to other studies and most of P. resistance. J Antimicrob Chemother. 2001;48 Suppl 1:59–64.
aeruginosa isolates (88.7%) were multi-drug resistant (re- 4. Ben-Mahrez Kamel, Rejiba Samia, Belhadj Cherifa, Belhadj Om-
rane. β-lactamase-mediated resistance to extended spectrum
4 Jundishapur J Microbiol. 2014;7(1):e8888
Alikhani MY et al.
cephalosporins among clinical isolates of Pseudomonas aerugi- A, et al. Prevalence of OXA-type beta-lactamases among Acineto-
nosa. Res Microbiol. 1999;150(6):403–406. bacter baumannii isolates from Northwest of Iran. Microb Drug
5. Lee S, Park YJ, Kim M, Lee HK, Han K, Kang CS, et al. Prevalence Resist. 2012;18(4):385–9.
of Ambler class A and D beta-lactamases among clinical isolates 18. Todar Kenneth. Todar's online textbook of bacteriology.: University
of Pseudomonas aeruginosa in Korea. J Antimicrob Chemother. of Wisconsin-Madison Department of Bacteriology; 2006.
2005;56(1):122–7. 19. Hauser AR, Sriram P. Severe Pseudomonas aeruginosa infec-
6. Poirel L, Lebessi E, Castro M, Fevre C, Foustoukou M, Nordmann tions. Tackling the conundrum of drug resistance. Postgrad Med.
P. Nosocomial outbreak of extended-spectrum beta-lactamase 2005;117(1):41–8.
SHV-5-producing isolates of Pseudomonas aeruginosa in Athens, 20. Chayakulkeeree M, Junsriwong P, Keerasuntonpong A, Tribud-
Greece. Antimicrob Agents Chemother. 2004;48(6):2277–9. dharat C, Thamlikitkul V. Epidemiology of extended-spectrum
7. Weldhagen GF. Rapid detection and sequence-specific differen- beta-lactamase producing gram-negative bacilli at Siriraj Hos-
tiation of extended-spectrum beta-lactamase GES-2 from Pseu- pital, Thailand, 2003. Southeast Asian J Trop Med Public Health.
domonas aeruginosa by use of a real-time PCR assay. Antimicrob 2005;36(6):1503–9.
Agents Chemother. 2004;48(10):4059–62. 21. Kaushik Robin, Kumar Sandeep, Sharma Rajeev, Lal Pawanin-
8. Essack SY. Laboratory detection of extended-spectrum dra. Bacteriology of burn wounds — the first three years in
β-lactamases (ESBLs)—The need for a reliable, reproducible meth- a new burn unit at the Medical College Chandigarh. Burns.
od. Diag Microbiol Infect Dis. 2000;37(4):293–295. 2001;27(6):595–597.
9. Jacoby GA, Han P. Detection of extended-spectrum beta-lacta- 22. Mirsalehian A, Feizabadi M, Nakhjavani FA, Jabalameli F, Goli
mases in clinical isolates of Klebsiella pneumoniae and Esch- H, Kalantari N. Detection of VEB-1, OXA-10 and PER-1 genotypes
erichia coli. J Clin Microbiol. 1996;34(4):908–11. in extended-spectrum beta-lactamase-producing Pseudomo-
10. Poirel L, Menuteau O, Agoli N, Cattoen C, Nordmann P. Outbreak nas aeruginosa strains isolated from burn patients. Burns.
of extended-spectrum beta-lactamase VEB-1-producing isolates 2010;36(1):70–4.
of Acinetobacter baumannii in a French hospital. J Clin Microbiol. 23. Nikbin VS, Abdi-Ali A, Feizabadi MM, Gharavi S. Pulsed field gel
2003;41(8):3542–7. electrophoresis & plasmid profile of Pseudomonas aeruginosa at
11. Wolska MK, Bukowski K, Jakubczak A. [Occurrence of beta-lacta- two hospitals in Tehran, Iran. Indian J Med Res. 2007;126(2):146–51.
mase type ESBL and IBL in Pseudomonas aeruginosa rods]. Med 24. Ozumba UC, Jiburum BC. Bacteriology of burn wounds in Enugu,
Dosw Mikrobiol. 2001;53(1):45–51. Nigeria. Burns. 2000;26(2):178–180.
12. Aubert D, Poirel L, Chevalier J, Leotard S, Pages JM, Nordmann P. 25. Song Wonkeun, Lee Kyu Man, Kang Hee Jung, Shin Dong Hoon,
Oxacillinase-mediated resistance to cefepime and susceptibility Kim Dong Kun. Microbiologic aspects of predominant bacteria
to ceftazidime in Pseudomonas aeruginosa. Antimicrob Agents isolated from the burn patients in Korea. Burns. 2001;27(2):136–
Chemother. 2001;45(6):1615–20. 139.
13. Endimiani A, Luzzaro F, Pini B, Amicosante G, Rossolini GM, To- 26. Celenza G, Pellegrini C, Caccamo M, Segatore B, Amicosante G,
niolo AQ. Pseudomonas aeruginosa bloodstream infections: risk Perilli M. Spread of bla(CTX-M-type) and bla(PER-2) beta-lacta-
factors and treatment outcome related to expression of the PER-1 mase genes in clinical isolates from Bolivian hospitals. J Antimi-
extended-spectrum beta-lactamase. BMC Infect Dis. 2006;6:52. crob Chemother. 2006;57(5):975–8.
14. Bauer AW, Kirby WM, Sherris JC, Turck M. Antibiotic susceptibil- 27. Chanawong A, M'Zali FH, Heritage J, Lulitanond A, Hawkey PM.
ity testing by a standardized single disk method. Am J Clin Pathol. SHV-12, SHV-5, SHV-2a and VEB-1 extended-spectrum beta-lacta-
1966;45(4):493–6. mases in Gram-negative bacteria isolated in a university hospital
15. Wayne PA. Performance standards for antimicrobial susceptibil- in Thailand. J Antimicrob Chemother. 2001;48(6):839–52.
ity testing. Ninth informational supplement NCCLS document M100- 28. Shahcheraghi F, Nikbin VS, Feizabadi MM. Prevalence of ESBLs
S9. National Committee for Clinical Laboratory Standards. 2008. genes among multidrug-resistant isolates of Pseudomonas ae-
16. Yousefi S, Farajnia S, Nahaei MR, Akhi MT, Ghotaslou R, Soroush ruginosa isolated from patients in Tehran. Microb Drug Resist.
MH, et al. Detection of metallo-beta-lactamase-encoding genes 2009;15(1):37–9.
among clinical isolates of Pseudomonas aeruginosa in north- 29. Tsakris A, Vatopoulos AC, Tzouvelekis LS, Legakis NJ. Diversity of
west of Iran. Diagn Microbiol Infect Dis. 2010;68(3):322–5. resistance phenotypes and plasmid analysis in multi-resistant
17. Sohrabi N, Farajnia S, Akhi MT, Nahaei MR, Naghili B, Peymani 0:12 Pseudomonas aeruginosa. Eur J Epidemiol. 1992;8(6):865–70.
Jundishapur J Microbiol. 2014;7(1):e8888 5
Copyright of Jundishapur Journal of Microbiology is the property of Kowsar Corporation and
its content may not be copied or emailed to multiple sites or posted to a listserv without the
copyright holder's express written permission. However, users may print, download, or email
articles for individual use.
You might also like
- Adult Therapy Guide-9020-7705 PDFDocument62 pagesAdult Therapy Guide-9020-7705 PDFbogdan.tomosNo ratings yet
- Antimicrobial Resistance and Molecular Characterization of Gene Cassettes From Class 1 Integrons in Pseudomonas Aeruginosa S PDFDocument7 pagesAntimicrobial Resistance and Molecular Characterization of Gene Cassettes From Class 1 Integrons in Pseudomonas Aeruginosa S PDFValentina RondonNo ratings yet
- 5 Psae Egypt 2014Document9 pages5 Psae Egypt 2014Khoa Vi Sinh BVCRNo ratings yet
- Relation Between Resistance To Antipseudomonal Β-Lactams And And Mexc Genes Of Pseudomonas AeruginosaDocument7 pagesRelation Between Resistance To Antipseudomonal Β-Lactams And And Mexc Genes Of Pseudomonas Aeruginosajack osmanNo ratings yet
- Zahra 2014Document6 pagesZahra 2014WahyunitadotokaNo ratings yet
- Molecular Characterization of Clinical Multidrug-Resistant Klebsiella Pneumoniae IsolatesDocument5 pagesMolecular Characterization of Clinical Multidrug-Resistant Klebsiella Pneumoniae IsolatesSamman zakaNo ratings yet
- Trabajo 2Document7 pagesTrabajo 2Juan Martín VargasNo ratings yet
- Development and Evaluation of A Loop-Mediated Isothermal Ampliication (LAMP) Assay For Rapid Detection of ActinobacillusDocument4 pagesDevelopment and Evaluation of A Loop-Mediated Isothermal Ampliication (LAMP) Assay For Rapid Detection of ActinobacillusLuis Ernesto Mena ZapataNo ratings yet
- Ref 05Document8 pagesRef 05truong.nguyen.19.12.92No ratings yet
- Idr 14 1517Document10 pagesIdr 14 1517Sherwan HusseinNo ratings yet
- Cortes Lara, 2021Document7 pagesCortes Lara, 2021Gabriela Chichón de la FuenteNo ratings yet
- Comparative Study of Cefoperazone Ceftazidime CeftDocument3 pagesComparative Study of Cefoperazone Ceftazidime CeftAdityaNo ratings yet
- Babol Jbums v17n8p19 enDocument8 pagesBabol Jbums v17n8p19 enTendi SulaksoNo ratings yet
- Trabajo 2Document7 pagesTrabajo 2Juan Martín VargasNo ratings yet
- New Delhi metallo-β-lactamase-1-producing Klebsiella pneumoniae isolates in hospitalized patients in Kashan, IranDocument5 pagesNew Delhi metallo-β-lactamase-1-producing Klebsiella pneumoniae isolates in hospitalized patients in Kashan, IranSubhecchha BaidyaNo ratings yet
- Art 5 PDFDocument10 pagesArt 5 PDFpaola lopezNo ratings yet
- Genetic and Antibiotic Susceptibility Profiles of Drug - Resistant Acinetobacter Baumannii From Various Parts of LebanonDocument9 pagesGenetic and Antibiotic Susceptibility Profiles of Drug - Resistant Acinetobacter Baumannii From Various Parts of LebanonInternational Medical PublisherNo ratings yet
- Epidermidis Carrying Biofilm Formation GenesDocument5 pagesEpidermidis Carrying Biofilm Formation GenesLini MaliqisnayantiNo ratings yet
- Piocianic EsblDocument15 pagesPiocianic EsblMari FereNo ratings yet
- Mr. Kamaraju Gadda Naveen M.SC - Medical Microbiology III Year, Dept. of Microbiology SRM MCH & RC GUIDE:-Dr - Subha Sundarmorthy Associate ProfessorDocument22 pagesMr. Kamaraju Gadda Naveen M.SC - Medical Microbiology III Year, Dept. of Microbiology SRM MCH & RC GUIDE:-Dr - Subha Sundarmorthy Associate ProfessorChockalingam MeenakshisundaramNo ratings yet
- Current Senerio of Antimicrobial Resistance Patterns of Pseudomonas Aeruginosa Clinical Isolates in East Uttar Pradesh, IndiaDocument4 pagesCurrent Senerio of Antimicrobial Resistance Patterns of Pseudomonas Aeruginosa Clinical Isolates in East Uttar Pradesh, IndiaPraveen GautamNo ratings yet
- Arnot PLOS GeneticsDocument3 pagesArnot PLOS GeneticsSahalS MNo ratings yet
- Alvi 2021Document8 pagesAlvi 2021Strik3rNo ratings yet
- RAPD AcinetoDocument8 pagesRAPD AcinetokiflyNo ratings yet
- Ijmicro2021 2145176Document5 pagesIjmicro2021 2145176cereb24567No ratings yet
- Tmp945e TMPDocument10 pagesTmp945e TMPFrontiersNo ratings yet
- Prevalence of Class 1 Integron Among Multidrug-Resistant Acinetobacter Baumannii in Tabriz, Northwest of IranDocument4 pagesPrevalence of Class 1 Integron Among Multidrug-Resistant Acinetobacter Baumannii in Tabriz, Northwest of IranDrashua AshuaNo ratings yet
- Molecular Mechanisms and Epidemiology of Carbapenem-Resistant Enterobacter Cloacae Complex Isolated From Chinese Patients During 2004-2018Document12 pagesMolecular Mechanisms and Epidemiology of Carbapenem-Resistant Enterobacter Cloacae Complex Isolated From Chinese Patients During 2004-2018Mayang WulanNo ratings yet
- Evaluation of Antibiotic Susceptibilities of Ehrlichia Canis, Ehrlichia Chaffeensis, and Anaplasma Phagocytophilum by Real-Time PCRDocument7 pagesEvaluation of Antibiotic Susceptibilities of Ehrlichia Canis, Ehrlichia Chaffeensis, and Anaplasma Phagocytophilum by Real-Time PCRyudhi arjentiniaNo ratings yet
- Pattern of Antimicrobial Drug Resistance of Salmonella Typhi and Paratyphi A in A Teaching Hospital in IslamabadDocument5 pagesPattern of Antimicrobial Drug Resistance of Salmonella Typhi and Paratyphi A in A Teaching Hospital in IslamabadDevita RamadaniNo ratings yet
- Madhavan 1999Document7 pagesMadhavan 1999KAREN GARZA NEVAREZNo ratings yet
- Tmp9e56 TMPDocument6 pagesTmp9e56 TMPFrontiersNo ratings yet
- 9,1,3Document6 pages9,1,3Aashish DhakalNo ratings yet
- Alternatives To Ciprofl Oxacin Use For Enteric Fever, United KingdomDocument2 pagesAlternatives To Ciprofl Oxacin Use For Enteric Fever, United Kingdomcharm_stormNo ratings yet
- 2002 Identification of A Conserved Plasmodium Falciparum Var Gene Implicated in Malaria in PregnancyDocument5 pages2002 Identification of A Conserved Plasmodium Falciparum Var Gene Implicated in Malaria in PregnancySethawud ChaikitgosiyakulNo ratings yet
- Cefpirome Literature PDFDocument8 pagesCefpirome Literature PDFTya ALditsa SadegaNo ratings yet
- Prevalence of Extended-Spectrum Beta-Lactamases Among Isolated Isolated From Blood Culture in A Tertiary Care HospitalDocument4 pagesPrevalence of Extended-Spectrum Beta-Lactamases Among Isolated Isolated From Blood Culture in A Tertiary Care HospitalMohammad K AlshomraniNo ratings yet
- Begum 2013Document4 pagesBegum 2013WahyunitadotokaNo ratings yet
- DISSEMINATIONDocument8 pagesDISSEMINATIONAbbireddy SairamNo ratings yet
- Discussion: Mac Faddin, 1976Document8 pagesDiscussion: Mac Faddin, 1976Salma MohamedNo ratings yet
- Molecular Detection of Extended Spectrum B-Lactamases, MetalloDocument7 pagesMolecular Detection of Extended Spectrum B-Lactamases, MetalloValentina RondonNo ratings yet
- Yamano 2006 Occurrence of PER-1Document6 pagesYamano 2006 Occurrence of PER-1WahyunitadotokaNo ratings yet
- Biology 10 00373Document16 pagesBiology 10 00373Imas-hendryNo ratings yet
- Generating Aptamers For Recognition of Virus-Infected Cells:: The Development of Molecular ProbesDocument10 pagesGenerating Aptamers For Recognition of Virus-Infected Cells:: The Development of Molecular Probesapi-19973331No ratings yet
- Efficacy of Practised Screening Methods For Detection of Cephalosporin-Resistant EnterobacteriaceaeDocument4 pagesEfficacy of Practised Screening Methods For Detection of Cephalosporin-Resistant EnterobacteriaceaeCoquelicot Éphémère ÉphémèreNo ratings yet
- Jurnal NCBIDocument6 pagesJurnal NCBIPutri Nilam SariNo ratings yet
- Pandrug-Resistant Causing Nosocomial Infections in A University Hospital, TaiwanDocument6 pagesPandrug-Resistant Causing Nosocomial Infections in A University Hospital, TaiwanNaufal AndaluNo ratings yet
- Emergence of Plasmid-Mediated Quinolone-Resistant SalmonellaTyphi Clinical Isolates From Punjab, PakistanDocument1 pageEmergence of Plasmid-Mediated Quinolone-Resistant SalmonellaTyphi Clinical Isolates From Punjab, Pakistanali zohaibNo ratings yet
- Detection OF IN Carbapenem-Resistant Isolated From Clinical Samples in Wasit Province HospitalsDocument15 pagesDetection OF IN Carbapenem-Resistant Isolated From Clinical Samples in Wasit Province HospitalsZainab SattarNo ratings yet
- Paterson Et Al., 2021Document3 pagesPaterson Et Al., 2021Caio Bonfim MottaNo ratings yet
- Molecular Epidemiologic Analysis of Enterococcus FaecalisDocument8 pagesMolecular Epidemiologic Analysis of Enterococcus FaecalisoinkNo ratings yet
- ESBLDocument2 pagesESBLCla ValenciaNo ratings yet
- Caracterizacion Con AntibodyDocument6 pagesCaracterizacion Con AntibodyRobert Larry Cordova DiazNo ratings yet
- JCM 44 1 119-123 2006Document5 pagesJCM 44 1 119-123 2006HArdik NegiNo ratings yet
- Fosfomycin and Comparator Activity Against Select Enterobacteriaceae, Pseudomonas, and Enterococcus Urinary Tract InfectionDocument11 pagesFosfomycin and Comparator Activity Against Select Enterobacteriaceae, Pseudomonas, and Enterococcus Urinary Tract InfectionNawwal NaeemNo ratings yet
- Potential Development of Temephos Resistance in Aedes Aegypti Related To Its Mechanism and Susceptibility To Dengue VirusDocument6 pagesPotential Development of Temephos Resistance in Aedes Aegypti Related To Its Mechanism and Susceptibility To Dengue VirusMichael KevinNo ratings yet
- VaccineDocument7 pagesVaccineyudhi arjentiniaNo ratings yet
- Antimicrobial Agents and Chemotherapy-2015-Pöppel-2508.fullDocument7 pagesAntimicrobial Agents and Chemotherapy-2015-Pöppel-2508.fullEEDIEB Prof. Millton Marques CurvoNo ratings yet
- Current Trends in the Identification and Development of Antimicrobial AgentsFrom EverandCurrent Trends in the Identification and Development of Antimicrobial AgentsNo ratings yet
- Chaudhari 2013Document4 pagesChaudhari 2013WahyunitadotokaNo ratings yet
- Zahra 2014Document6 pagesZahra 2014WahyunitadotokaNo ratings yet
- Metallo Gen e ColiDocument5 pagesMetallo Gen e ColiWahyunitadotokaNo ratings yet
- Lactamases Updated Functional Classification Of: 2010, 54 (3) :969. DOI: Karen Bush and George A. JacobyDocument9 pagesLactamases Updated Functional Classification Of: 2010, 54 (3) :969. DOI: Karen Bush and George A. JacobyWahyunitadotokaNo ratings yet
- Tielen 2011Document11 pagesTielen 2011WahyunitadotokaNo ratings yet
- Begum 2013Document4 pagesBegum 2013WahyunitadotokaNo ratings yet
- Yamano 2006 Occurrence of PER-1Document6 pagesYamano 2006 Occurrence of PER-1WahyunitadotokaNo ratings yet
- Cardiovascular Emergency: Cardiac ArrestDocument12 pagesCardiovascular Emergency: Cardiac ArrestWahyunitadotokaNo ratings yet
- Balazs 2008 PRINTDocument9 pagesBalazs 2008 PRINTWahyunitadotokaNo ratings yet
- Penyakit Paru Obstruktif Kronik (PPOK) : Fakultas Kedokteran Universitas Sultan Khairun (Unkhair)Document53 pagesPenyakit Paru Obstruktif Kronik (PPOK) : Fakultas Kedokteran Universitas Sultan Khairun (Unkhair)WahyunitadotokaNo ratings yet
- Gambaran Patologi Anatomik Kelainan Sistem PernapasanDocument49 pagesGambaran Patologi Anatomik Kelainan Sistem PernapasanWahyunitadotokaNo ratings yet
- HypertensionDocument52 pagesHypertensionWahyunitadotokaNo ratings yet
- Bacterial Infection in Gastrointestinal TractDocument30 pagesBacterial Infection in Gastrointestinal TractWahyunitadotokaNo ratings yet
- Embryologi & Normal Structure of Cardiovascular System, Dr. Hasan NyambeDocument61 pagesEmbryologi & Normal Structure of Cardiovascular System, Dr. Hasan NyambeWahyunitadotokaNo ratings yet
- CV ExampleDocument2 pagesCV ExampleWahyunitadotokaNo ratings yet
- LPDFIXDocument147 pagesLPDFIXanastasiaNo ratings yet
- Daftar Atc DDD Antibiotik Who 2018Document12 pagesDaftar Atc DDD Antibiotik Who 2018APOTEKER RSUMMNo ratings yet
- CLSI Pak-Antibiotic Sensitivity Panels Feb 2017-NasrullahDocument18 pagesCLSI Pak-Antibiotic Sensitivity Panels Feb 2017-NasrullahIhtisham Ul HaqNo ratings yet
- Amprahan PICU Sabtu, 20 Feb 2021Document6 pagesAmprahan PICU Sabtu, 20 Feb 2021muhammadrikiNo ratings yet
- Pharm I - Abx ChartDocument4 pagesPharm I - Abx ChartNicole BerryNo ratings yet
- Antimicrobial Agent Classes and SubclassesDocument5 pagesAntimicrobial Agent Classes and SubclassesAnonymous A2E2jLTNo ratings yet
- Antimicrobial SusceptibilityDocument45 pagesAntimicrobial SusceptibilityMarcelo Andrés Ortiz BentoNo ratings yet
- Contoh Perhitungan DDD Excell - IRNADocument8 pagesContoh Perhitungan DDD Excell - IRNAMaya DamanikNo ratings yet
- Comparison of Drugs in MSTGDocument2 pagesComparison of Drugs in MSTGShoaib BiradarNo ratings yet
- Lab Report 12494079 20230410023410Document5 pagesLab Report 12494079 20230410023410raymondNo ratings yet
- AntibiotikDocument3 pagesAntibiotikFeny OktariaNo ratings yet
- SS-Laktamski Antibiotici: Peroralni Parenteralni Penicilaza Rezistentni PeniciliniDocument5 pagesSS-Laktamski Antibiotici: Peroralni Parenteralni Penicilaza Rezistentni PeniciliniMali PrstNo ratings yet
- AntibioticsDocument2 pagesAntibioticsSaeed HasanNo ratings yet
- 03 Mei 2023 PDFDocument34 pages03 Mei 2023 PDFRomandaniNo ratings yet
- 2018 MMC AntibiogramDocument2 pages2018 MMC Antibiogramaman570570No ratings yet
- mcq ثانيDocument4 pagesmcq ثانيمحمدأميندماج100% (1)
- Mechanism of Action of Penicillin & CephalosporinDocument7 pagesMechanism of Action of Penicillin & CephalosporinshahabahmadNo ratings yet
- The 50th Anniversary of The Discovery of 6-Aminopenicillanic Acid (6-APA)Document6 pagesThe 50th Anniversary of The Discovery of 6-Aminopenicillanic Acid (6-APA)Estanislao Amadeo AvogadroNo ratings yet
- Doctors Order Form D4Document1 pageDoctors Order Form D4Marielle ChuaNo ratings yet
- For Diluti (ADULT)Document8 pagesFor Diluti (ADULT)Arwin DigoNo ratings yet
- David Paterson Session 1Document30 pagesDavid Paterson Session 1ADINo ratings yet
- Antibiotic Susceptibilities in Intensive Care: Gram Positive Gram NegativeDocument2 pagesAntibiotic Susceptibilities in Intensive Care: Gram Positive Gram NegativeMai Anh NguyenNo ratings yet
- CephalosporinsDocument35 pagesCephalosporinslakshmiuniq100% (1)
- Contoh Peta Pola KumanDocument1 pageContoh Peta Pola KumanAgustina Tri SetyaningtyasNo ratings yet
- Inhibit Classification AntibioticsDocument5 pagesInhibit Classification AntibioticsNurnaningsi Tajuddin ThalibNo ratings yet
- List of Cephalosporins + Uses, Types & Side EffectsDocument5 pagesList of Cephalosporins + Uses, Types & Side EffectsMd. Sabit Ahsan SarkerNo ratings yet
- 5 Sar CephalosporinsDocument17 pages5 Sar CephalosporinsGitasetya NingrumNo ratings yet
- Betalactam I-Dai Hoc-Janvier 2012.SVDocument67 pagesBetalactam I-Dai Hoc-Janvier 2012.SVsinhnocNo ratings yet
- Production Schedule of 25.06.2021 & 26.06.2021Document5 pagesProduction Schedule of 25.06.2021 & 26.06.2021Nazimuzzaman KhanNo ratings yet