Professional Documents
Culture Documents
Electronic Medical Handover: Towards Safer Medical Care
Uploaded by
Luminita StoleruOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Electronic Medical Handover: Towards Safer Medical Care
Uploaded by
Luminita StoleruCopyright:
Available Formats
H EA L T H C A R E
Electronic medical handover: towards safer medical care
Lean-Peng Cheah, Debbie H Amott, James Pollard and David A K Watters
J unior doctors in hospitals cannot work 24 hours a day, 7 days
a week. When they go off-duty, some form of information
handover to the relieving team is necessary to ensure continu-
ity of care. With the moves to reduce junior doctors’ working
ABSTRACT
• As the working hours of junior doctors decrease, adequate
handover of patients becomes more important to maintain
hours, the number of handovers is increasing. However, the continuity of care and avoid errors caused by information
quality of handovers can be poor.1 Lack of information when a gaps.
patient needs urgent and often unexpected care is a clinical risk. In • A minimum dataset for surgical handover should include the
addition, as on-call periods are often busy, a handover system that patient’s name, location (ward and bed number), date of
identifies the patients most in need of review and the required admission, diagnosis, procedure (with date), complications
decisions and progress, management plan, resuscitation plan,
The would
Medicalassist doctors
Journal in setting
of Australia priorities.
ISSN: 0025-
Suggestions to improve the quality of handovers include elec- consultant availability (and instructions if not available),
729X 3 October
2,3 2005 183 7 369-372
tronic©The
handovers,
Medical and the development
Journal of Australiaof2005
guidelines for hand- expected need for review, and name of doctor completing
4 handover and date to confirm that information is current.
overs.www.mja.com.au
Guidelines are also endorsed by the Australian Safety and
Quality Carein Health Care.5
Council
Health • An electronic handover system is a potential solution, but our
In our hospital, the impetus to document and improve hand- survey shows that free-text entry into such systems may be
overs arose from a root-cause analysis of a surgical adverse event in inadequate; prompts or predefined fields for handover
late 2003. A patient died of septicaemia complicating peritonitis content are possible solutions.
caused by a leaking large-bowel anastomosis. The cause of the MJA 2005; 183: 369–372
patient’s deteriorating condition was not initially recognised, and
the patient died despite a late repeat laparotomy. The deterioration
occurred over a weekend when communication between the on- • Allow patients from other specialties (eg, a medical unit) for
call doctors and the specialist responsible for care could have been whom consultations have been requested to appear in the
improved. Although our hospital, like many others, assumed that “patients-to-review” list.
handovers take place, there were no formal policies or guidelines
about what information should be included in handover.
Developing an electronic handover system
We describe the process of developing an improved, electronic
handover system for junior doctors at our hospital, a regional Many of the required data were already present in the two
teaching hospital with 400 beds. electronic information systems in use in the hospital. The CORDis
system (Correspondence, Operation notes, Reports and Discharge
summaries) was used hospital-wide to generate discharge summa-
Developing a minimum dataset for handover ries, clinic letters, operation notes, audit reports and drug prescrip-
In early 2004, we reviewed handover procedures for surgical tions. CORDis (http://www.cordisehr.com.au) was developed by
patients at the hospital. In consultation with junior and senior Dynamic Solutions (Melbourne, Vic; www.dynamic.net.au) in
doctors and the Clinical Risk Management Committee, we deter- association with Barwon Health, and introduced in 2001, with the
mined the data and functions required for electronic handover and Pharmaceutical Benefits Scheme prescribing function added in
handback. Handover needs to inform about the patient’s location early 2002.
and unit, the consultant normally responsible for care, diagnosis, In addition, the review of handover procedures coincided with
length of stay, procedures, and plan or instructions for the the roll-out of a second information system, the BOSS (Core
handover period (Box 1). Medical Solutions, Adelaide, SA; www.coremedicalsolutions.com).
In addition, we defined the required functions for an electronic This system was used for reporting results of laboratory investiga-
handover system. The system should be able to: tions, and through linking to the radiology reporting system it
• Print a patient list for the specialty or units being covered; provided a common system for reporting all investigation results.
• Sort the list by ward and bed number, by consultant, by unit, or The BOSS system also includes a free-text window for recording
by need for review; handover information if desired. The system creates lists of
• Allow handover information to be entered efficiently (ideally patients with location, diagnosis, length of stay, recent results and
with a single mouse click); and any content inserted in the free-text window (Box 2).
In 2004, neither system was able to provide all the required
handover information. In devising a solution, our guiding princi-
University of Melbourne and Barwon Health, Geelong, VIC. ples were to avoid duplication of data entry and to ensure that
Lean-Peng Cheah, MB BS(Hons), MRCS, Advanced Surgical Trainee;
currently, St Vincent’s Hospital, Melbourne, VIC; Debbie H Amott,
information viewed was accurate and up-to-date. Our initial
MB BS(Hons), Advanced Surgical Trainee; James Pollard, MB BS, approach was to build fields for the minimum dataset into
Medical Registrar; David A K Watters, FRCS, FRACS, Professor and CORDis, as we had easy access to its developers. We did not
Director of Surgery. attempt to replicate the transmission of investigation results into
Reprints will not be available from the authors. Correspondence: CORDis, as this would have been complex and expensive. The
Professor David A K Watters, Department of Surgery, Geelong Hospital, handover system was available in CORDis with more predefined
Geelong, VIC 3220. davidw@barwonhealth.org.au
fields for content (Box 1) but without investigation results, and in
MJA • Volume 183 Number 7 • 3 October 2005 369
H EA L T H C A R E
doctor was responsible, and the number of patients with no
1 A minimum data set for handover
handover information entered.
Generated automatically from hospital information system In addition, we conducted a prospective survey of registrars and
Patient (name, UR no.) residents receiving handovers and those receiving handback on
Patient age seven consecutive weekends and public holidays between Decem-
Date of admission/day of stay ber 2004 and February 2005. For each handover, the on-call
Patient location (ward and bed number) registrar and resident were interviewed by one of the authors
Consultant responsible for care (D A K W) and given an evaluation form to complete. This form
Treating unit
asked about the completeness and usefulness of the handover
information. Results from the registrar, as the team leader, were
Current diagnosis
scored, except in the case of opinions about the desirability of
Results of recent investigations
electronic handover. The registrars receiving handback were also
To be entered by junior doctor going off duty interviewed about events, discharges and discharge summaries and
Handover note (free text) any problems.
Update current diagnosis Results are shown in Box 3. On average, completing the
Recent procedure(s) and date(s) handover information took 10 minutes, for seven to eight patients
Desirable (or required in a free-text note) per unit, while completing handback information took 2 minutes
Consultant availability per event for 2–3 events per unit during the on-call period (2
Insurance status* discharges and 0–1 other event).
Need for and urgency of review† The need for handovers and the value of a documented
Patient’s condition‡
handover was universally accepted by junior doctors. Doctors
volunteered that they were particularly pleased with the ability of
Condition trend§
the BOSS to include results of recent laboratory tests on a
Management plan¶
handover sheet, which encouraged use of the system.
Resuscitation plan** We found that the system reliably identified patients and their
Investigations pending/required locations. However, the free-text entry, although helpful, was often
Name of doctor completing handover information deficient in particular information, such as decisions that needed
Date of handover update to be made in ward rounds and consultant availablity. In addition,
* Insurance status (private or public) to help determine whether changes in
handback information was not completed consistently, particularly
patient’s condition should be reported to the patient’s private consultant when patients were discharged or transferred to another unit (eg,
rather than the on-call team. from a surgical to a medical unit). We found a documented
† We recommend a drop down menu with choices: frequently, necessary, handback in only half the patients with significant events. While
desirable, as required.
almost 80% of doctors returning to duty were informed of patients
‡ We recommend a drop down menu with choices: critical (unstable), stable,
for palliation.
who had been discharged, only 13% knew whether a discharge
§ We recommend a drop down menu with choices: improving, deteriorating, summary had been done.
unchanged. The BOSS handover procedure was also used on an ad-hoc basis
¶ Management plan (eg, remove drain tube, discharge, resume normal diet). by junior doctors in other clinical services. Handover for medical
**Resuscitation plan (eg, full resuscitation, not for life support, MET patients could take twice as long as for surgical patients, as they
[medical emergency team] calls only, not for resuscitation). ◆
often have multiple problems, each problem with its own thera-
peutic intervention, instead of a single procedure.
the BOSS with a free-text field for data entry. The inclusion of
Discussion
laboratory results on the tasklists generated by the BOSS meant
that it became the preferred system for junior doctors to use during We found that that free-text entries in an electronic system were
ward rounds and handover. not adequate to convey all the information required for a thorough
patient handover. Handover information needs to identify a list of
patients and their location, to highlight their priority for review,
Evaluating the BOSS handover system and indicate the availability of the treating specialist. A system to
As junior doctors preferred to use the BOSS system for handovers, provide this information is relatively simple to develop if a clinical
we investigated the adequacy of the BOSS free-text entries for information system is already in place. However, it is more
communicating the minimum dataset for general surgery patients. complex to ensure that the system updates, while also retaining a
Our hospital has four general surgical units and one vascular unit, copy of “who, what and when” entered the handover information
each staffed on weekdays by one registrar and one resident medical should it ever be necessary to review the information conveyed. A
officer. On weekends and public holidays, responsibility for all five further challenge is to ensure that any system being developed is
units is handed over to one on-call registrar and one resident, the used. If a handover system is to be successfully implemented, it
latter changing on the second and any subsequent days. needs to be seen as advantageous by its users — simple, informa-
We reviewed the BOSS general surgery on-call handover sheets tive, time-saving and practical.
(comprising the combined lists of the four general surgical and one In our hospital, the information required for handovers by
vascular unit) for 14 weekends and public holidays in 2004 and junior doctors originated in two separate electronic systems. The
between December 2004 and February 2005. The aim was to situation is probably similar in many other Australian hospitals. To
determine the total number of patients for whom the on-call junior be simple and effective, and to avoid duplication of data entry, all
370 MJA • Volume 183 Number 7 • 3 October 2005
H EA L T H C A R E
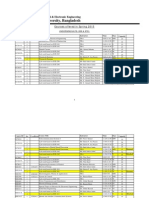
2 The BOSS electronic system with free-text handover 3 Survey of the adequacy of the BOSS free-text
handover system
Question Response
Handover
Average number of patients to hand over (n = 14) 7–8
Average time taken to fill in handover information 10
(min) (n = 14)
Is it a good idea to fill in a formal electronic 7/7 (100%)
handover? (Yes [%])
The weekend round
Average number of patients doctor is responsible 40
for (n = 7)
Average number with incomplete handover 8 (20%)
information (n = 7)
Did you know where your patients were? (Yes [%]) 7/7 (100%)
Screen shot from the BOSS handover system showing the free-text Did you know what was wrong with your patients? 5/7 (71%)
field used to enter a handover note. This field is brought up by (Yes [%])
clicking on the patient row. Did you know what decisions had to be made? 4/7 (57%)
(Yes [%])
Did the handover list help remind you of key 6/7 (85%)
investigations to do/results to review? (Yes [%])
Was information about consultants’ availability 3/7 (41%)
adequate? (Yes [%])
Is an electronic handover system desirable?* (Yes [%]) 14/14 (100%)
Handback
Were the handover data updated over the weekend 7/14 (50%)
for handback? (Yes [%])
Does the handover system identify significant events 8/13 (61%)†
that happened while you were off-duty? (Yes [%])
Do you know who was discharged or died while you 11/14 (79%)
were away? (Yes [%])
Screen shot showing the “Print a tasklist” format which contains the Do you know if the discharge summaries were done? 2/14 (13%)
handover information (central section), laboratory results (right hand (Yes [%])
section) and patient name, age, length of stay, diagnosis and * Denominator was 14 as replies were scored from both registrar and resident.
consultant in charge (left hand section). ◆ † Denominator was 13 as no significant events occurred on one weekend. ◆
hospital systems need to be linked so that all necessary informa- tronic systems and to devise a local solution for presenting it in a
tion can be presented in one handover list. We considered two single screen or patient list.
potential solutions: Continuity of care is important to patients but must be
• To replicate what was wanted from one of the systems into the balanced against junior doctors’ working hours and the dangers
other (a short-term, interim solution). of fatigue. Recent studies have shown that reducing working
• To develop a web browser that could access both systems and hours decreases attentional failures and medical errors.7,8 In
build handover preferences on an HTML page (a longer-term Australia, the average working week has dropped from over 100
solution). A web-based system could be introduced in two phases: hours to under 70 hours in recent times, as errors caused by
a first read/print-only phase; and a second phase permitting data fatigue have become unacceptable.9,10 A surgical registrar is now
entry. rarely on a 1 day in 2 on-call roster, with 1 day in 4 or 5 being
We are currently developing the second solution. The ability to the norm. Thus, handover information must be provided on
view handover information on a personal digital assistant would 75%–80% of working days. Senior staff are also becoming
also be a significant attraction of such a system.6 In the meantime, increasingly less available — particularly on weekends — as
we have developed a “handover wizard” in the BOSS system to they arrange cover through group practices or take long week-
prompt for required handover information from junior doctors end breaks.
who choose to use it (Box 4). Similar changes are being implemented overseas. In the United
Other hospitals can use the dataset we have identified (Box 1) to Kingdom, the European Working Time Directive limits doctors in
develop their own handover solutions. Each hospital needs to training to 48 hours’ work a week.11,12 This weekly limit is being
determine where the necessary information resides in their elec- implemented in stages, with an interim average 58-hour working
MJA • Volume 183 Number 7 • 3 October 2005 371
H EA L T H C A R E
2003. Available at: http://www.rcseng.ac.uk/service_provision/ewtd/serv-
4 The BOSS “wizard” for electronic handover ices/publications/publications/pdf/wtd_policy.pdf (accessed Dec 2004).
12 British Medical Association. Time’s up 1 August 2004. A guide on the
EWTD for junior doctors. London: BMA, 2004. Available at: http://
www.bma.org.uk/ap.nsf/Content/TimesUp/$file/T imesUp2.pdf
(accessed Dec 2004).
13 NHS Modernisation Agency. The hospital at night. Report and recom-
mendations of the hospital at night project. Available at: http://
www.modern.nhs.uk/workingtime/17048/WhatisHospitalatNight/1_1.pdf
(accessed Feb 2005).
14 MacDonald R, Eccles S. The hospital at night. BMJ Career Focus 2004;
328: 19; doi:10.1136/bmj.328.7431.s19. Available at: http://careerfo-
cus.bmjjournals.com/cgi/content/full/328/7431/s19 (accessed Mar 2005).
15 Common program requirements (resident duty hours). Chicago: Accredi-
tation Council for Graduate Medical Education, 2003. Available at: http://
www.acgme.org/acWebsite/dutyHours/dh_dutyHoursCommonPR.pdf
(accessed Dec 2004).
(Received 21 Dec 2004, accepted 11 Aug 2005) ❏
Screen shot from the BOSS handover system showing the “wizard”
prompt for content of the handover note. Clicking on the patient
row brings up the handover note window. ◆
week. A “hospital at night” project is looking at specific issues in
regard to the increased number of shifts, competency and hand-
over.13,14 In the United States, the Accreditation Council for
Graduate Medical Education has also recently limited duty hours
for medical residents to 80 hours per week.15
We believe further research and evaluation are required to fine
tune the format of handover for different medical specialties and to
demonstrate the effectiveness of introducing formal handover
systems into other hospitals.
References
1 Roughton VJ, Severs MP. The junior doctor handover: current practices
and future expectations. J R Coll Physicians Lond 1996; 30: 213-214.
2 Volpp KGM, Grande D. Residents’ suggestions for reducing errors in
teaching hospitals. N Engl J Med 2003; 348: 851-855.
3 Young RJ, Horsley SD, McKenna M. The potential role of IT in supporting
the work of junior doctors. J R Coll Physicians Lond 2000; 34: 366-370.
4 Junior Doctors Committee. Annual report 2004. London: British Medical
Association, 2004. Available at: http://www.bma.org.uk/ap.nsf/Content/
jdcannualreport2004 (accessed Mar 2005).
5 Australian Safety and Quality Council in Health Care. Safe staffing —
discussion paper. Canberra: Safety and Quality Council, 2003. Available
at: http://www.safetyandquality.org/articles/Publications/SafeStaffing_
web.pdf (accessed Dec 2004).
6 Wilcox RA, La Tella RR. The personal digital assistant: a new medical
instrument for the exchange of clinical information at the point of care.
Med J Aust 2001; 175: 659-662.
7 Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns’ weekly
hours on sleep and attentional failures. N Engl J Med 2004; 351: 1829-
1837.
8 Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’
work hours on serious medical errors in intensive care units. N Engl J
Med 2004; 351: 1838-1848.
9 Australian Medical Association (Victoria). Australian Medical Association
(Victoria) Hospital Medical Officer Certified Agreement 2002. Melbourne:
AMA, 2002.
10 Nocera A, Khursandi DS. Doctors’ working hours: can the medical
profession afford to let the courts decide what is reasonable? Med J Aust
1998; 168: 616-618.
11 Phillips H, Morris PJ. The Royal College of Surgeons of England and the
European Working Time Directive – a policy statement. London: RCS,
372 MJA • Volume 183 Number 7 • 3 October 2005
View publication stats
You might also like
- Last Boat Not Least - An Unofficial Adventure For Fallout 2d20Document14 pagesLast Boat Not Least - An Unofficial Adventure For Fallout 2d20Veritas Veritati100% (3)
- Newman's Certified Electronic Health Records Technician Study GuideFrom EverandNewman's Certified Electronic Health Records Technician Study GuideNo ratings yet
- Online Patients Record Platform Using PHPDocument31 pagesOnline Patients Record Platform Using PHPAmaan B EydreesNo ratings yet
- Language and The Pursuit of Hap - Chalmers BrothersDocument1,184 pagesLanguage and The Pursuit of Hap - Chalmers BrothersGeorge Adrian Oprea100% (2)
- Route TrainingDocument14 pagesRoute Trainingjohn100% (1)
- All About Immanuel KantDocument20 pagesAll About Immanuel KantSean ChoNo ratings yet
- Critical Care ApplicationsDocument35 pagesCritical Care ApplicationsrdelmoroNo ratings yet
- Computerized Patient Information SystemDocument12 pagesComputerized Patient Information SystemChristianNo ratings yet
- Electrical Engineering Portal Com Electrical Thumb Rules You Must Follow Part 1Document10 pagesElectrical Engineering Portal Com Electrical Thumb Rules You Must Follow Part 1m khNo ratings yet
- Electronic Medical RecordDocument5 pagesElectronic Medical RecordSujatha J Jayabal100% (3)
- Hand Off CommunicationDocument6 pagesHand Off CommunicationALELAW100% (1)
- Patient Management System (New Reviewed)Document39 pagesPatient Management System (New Reviewed)Ajewole Eben Tope100% (1)
- Funda Finals Lec NotesDocument20 pagesFunda Finals Lec NotesPauline AñesNo ratings yet
- Nursing Information SystemDocument20 pagesNursing Information SystemShahad Hakimuddin100% (1)
- System 9898XT Service ManualDocument398 pagesSystem 9898XT Service ManualIsai Lara Osoria100% (3)
- Electronic Health Record: 3.1 Application of Health Informatics in Clinical PracticeDocument3 pagesElectronic Health Record: 3.1 Application of Health Informatics in Clinical Practicepamela rasmoNo ratings yet
- The Mayo ClinicDocument13 pagesThe Mayo ClinicRuchi AvdhaniNo ratings yet
- ArticleDocument5 pagesArticleJay StoneNo ratings yet
- BHA-FPX4106 - Nadhirah Lutchminarain - Assignment 1Document11 pagesBHA-FPX4106 - Nadhirah Lutchminarain - Assignment 1Nadhirah De WetNo ratings yet
- Hospital Management SystemDocument6 pagesHospital Management SystemYohannes KefyalewNo ratings yet
- Topic 2 (Informatics - Communication Technologies in The Critical Care Units)Document2 pagesTopic 2 (Informatics - Communication Technologies in The Critical Care Units)Ghianx Carlox PioquintoxNo ratings yet
- Lesson 9 HIS Hospital Information SystemDocument36 pagesLesson 9 HIS Hospital Information SystemKauline Joseph C. BrionesNo ratings yet
- Emergency Department Overcrowding and Access Block: Caep P S N DDocument12 pagesEmergency Department Overcrowding and Access Block: Caep P S N DKomang Ayu Eka WijayantiNo ratings yet
- Using Electronically Available Inpatient Hospital Data For ResearchDocument8 pagesUsing Electronically Available Inpatient Hospital Data For ResearchSamNo ratings yet
- Triple Handoff: Spotlight Case September 2006Document28 pagesTriple Handoff: Spotlight Case September 2006Lakshay GuptaNo ratings yet
- Clinical Medicine Generic Standards Published PaperDocument4 pagesClinical Medicine Generic Standards Published PaperstarzpredoNo ratings yet
- Handouts 1Document15 pagesHandouts 1jamaica gutierrezNo ratings yet
- Perioperative Nursing Assessments Made Simple: Ew Nurse NotesDocument2 pagesPerioperative Nursing Assessments Made Simple: Ew Nurse NotesAbigail OclaritNo ratings yet
- The Electronic Medical Record: DR - Vishal SuryawanshiDocument40 pagesThe Electronic Medical Record: DR - Vishal SuryawanshiVishal SuryawanshiNo ratings yet
- f3d3 PDFDocument40 pagesf3d3 PDFSiti QamariaNo ratings yet
- NSQHS Standards Fact Sheet Standard 6Document2 pagesNSQHS Standards Fact Sheet Standard 6Annette LowryNo ratings yet
- Research 2Document10 pagesResearch 2Christie TirolNo ratings yet
- DRG AssignmentDocument12 pagesDRG Assignmentavpnqvfng100% (1)
- Bari 11Document104 pagesBari 11etsabayomiNo ratings yet
- Journal of Biomedical Informatics: Joshua Frisby, Vernon Smith, Stephen Traub, Vimla L. PatelDocument8 pagesJournal of Biomedical Informatics: Joshua Frisby, Vernon Smith, Stephen Traub, Vimla L. PatelLorenzo GarciaNo ratings yet
- NCM110 Applications of Nursing Informatics BSN3Document52 pagesNCM110 Applications of Nursing Informatics BSN3bryanmaranan173No ratings yet
- Arpa.2013 0712 SoDocument10 pagesArpa.2013 0712 SoIsti Dina NurulNo ratings yet
- Timely Simple DischargeDocument52 pagesTimely Simple DischargeDesti Setyaningrum100% (1)
- Sisteme Informatice de Spital. Fişa Electronică A Pacientului (E-Health Record - Ehr)Document18 pagesSisteme Informatice de Spital. Fişa Electronică A Pacientului (E-Health Record - Ehr)cata86_mailNo ratings yet
- Healthcare HXZEAL2 ZD8Document42 pagesHealthcare HXZEAL2 ZD8FMTech ConsultsNo ratings yet
- IRJET Doctors EMateDocument5 pagesIRJET Doctors EMateKRISHNA RAJ JNo ratings yet
- Design and Implementation of A Hospital Database Management System (HDMS) For Medical DoctorsDocument6 pagesDesign and Implementation of A Hospital Database Management System (HDMS) For Medical DoctorsAbhishek shendeNo ratings yet
- A Computerised Hospital Management System - Chapter 1Document5 pagesA Computerised Hospital Management System - Chapter 1Jbee TrendsNo ratings yet
- A Primer On Endoscopic Electronic Medical RecordsDocument6 pagesA Primer On Endoscopic Electronic Medical RecordsAceNo ratings yet
- Modeling and Simulation of Patient Flow in Hospitals For Resource UtilizationDocument10 pagesModeling and Simulation of Patient Flow in Hospitals For Resource UtilizationIndra GunawanNo ratings yet
- Special Requirements of Electronic Medical Record Systems in Obstetrics and GynecologyDocument4 pagesSpecial Requirements of Electronic Medical Record Systems in Obstetrics and GynecologysayansambitNo ratings yet
- BI Lecture Mod 1Document53 pagesBI Lecture Mod 1Risheel ChhedaNo ratings yet
- EvaluacionDocument4 pagesEvaluacionJhan ZitoNo ratings yet
- Design and Implementation of A Hospital Database Management System (HDMS) For Medical DoctorsDocument6 pagesDesign and Implementation of A Hospital Database Management System (HDMS) For Medical DoctorsTrần Minh HiếuNo ratings yet
- Crit Care Nurse-2007-Thomas-20-7 PDFDocument10 pagesCrit Care Nurse-2007-Thomas-20-7 PDFMr. BamsNo ratings yet
- The PACT Project: Improving Communication at Handover: Clinical Handover: Critical CommunicationsDocument3 pagesThe PACT Project: Improving Communication at Handover: Clinical Handover: Critical CommunicationssuharyaniNo ratings yet
- Nursing Informatics - Computers and NursingDocument5 pagesNursing Informatics - Computers and NursingAllia Rae Diaz GuiaoNo ratings yet
- Group 8 Reportinng PDFDocument2 pagesGroup 8 Reportinng PDFBonnie MAGHUYOPNo ratings yet
- 20190614175936skilled Nursing FacilitiesDocument5 pages20190614175936skilled Nursing Facilitiescaleb mwanziaNo ratings yet
- 10 1016@j Cnur 2019 04 003Document11 pages10 1016@j Cnur 2019 04 003zchekireb97No ratings yet
- Sepsis Screen Treatment AlgorithmDocument66 pagesSepsis Screen Treatment AlgorithmcindythungNo ratings yet
- Communication: Improving Patient Safety With SbarDocument7 pagesCommunication: Improving Patient Safety With Sbarria kartini panjaitanNo ratings yet
- The Addition of A Nurse Practitioner To An Inpatient Surgical Team Results in Improved Use of ResourcesDocument7 pagesThe Addition of A Nurse Practitioner To An Inpatient Surgical Team Results in Improved Use of Resourcesericc949432No ratings yet
- Fmea in Organ TransplantDocument8 pagesFmea in Organ TransplantVinay GargNo ratings yet
- Predicting Hospital Capacity and EfficiencyDocument9 pagesPredicting Hospital Capacity and EfficiencyManager HR Hijaz HospitalNo ratings yet
- Evaluation of A Computerized Problem OriDocument9 pagesEvaluation of A Computerized Problem OriYuli LestariNo ratings yet
- Predicting Hospital Length of Stay For Accident and Emergency AdmissionsDocument14 pagesPredicting Hospital Length of Stay For Accident and Emergency AdmissionsRABIATUL ADAWIYAHNo ratings yet
- Design and Implementation of Web Base Hospital Management SystemDocument36 pagesDesign and Implementation of Web Base Hospital Management SystemMikel KingNo ratings yet
- 144 First DraftDocument4 pages144 First DraftBianca AsisNo ratings yet
- OBM752 HM Unit-IV NotesDocument34 pagesOBM752 HM Unit-IV NotesRajanNo ratings yet
- Teaching Learning Activities (TLA)Document10 pagesTeaching Learning Activities (TLA)Kristil ChavezNo ratings yet
- The Differences Between OHS Management System StandardsDocument27 pagesThe Differences Between OHS Management System StandardsRommel100% (2)
- The Journal of The Acoustical Society of AmericaDocument12 pagesThe Journal of The Acoustical Society of Americadr01dNo ratings yet
- Deiparine, Jr. vs. Court of Appeals, 221 SCRA 503, G.R. No. 96643 April 23, 1993Document9 pagesDeiparine, Jr. vs. Court of Appeals, 221 SCRA 503, G.R. No. 96643 April 23, 1993CherNo ratings yet
- COMSOL WebinarDocument38 pagesCOMSOL WebinarkOrpuzNo ratings yet
- Anaphy Lec 1Document2 pagesAnaphy Lec 1Kiana SanchezNo ratings yet
- HW 3Document10 pagesHW 3Hande ÖzerNo ratings yet
- 7th NisssDocument9 pages7th NisssVedang PandeyNo ratings yet
- 2 Wheel Drive Forklift For Industry WarehousesDocument5 pages2 Wheel Drive Forklift For Industry WarehousesSuyog MhatreNo ratings yet
- Maintain Training Facilities: Michigan English Assessments Inc. CBLM On Cookery NC Ii Date Developed: February 2017Document8 pagesMaintain Training Facilities: Michigan English Assessments Inc. CBLM On Cookery NC Ii Date Developed: February 2017Joebie delos reyesNo ratings yet
- Improve Basic Visualization SkillDocument29 pagesImprove Basic Visualization Skillpatrick.schoenkaesNo ratings yet
- Wood Support-Micro Guard Product DataDocument13 pagesWood Support-Micro Guard Product DataM. Murat ErginNo ratings yet
- 1570-Article Text-4693-1-10-20190709Document18 pages1570-Article Text-4693-1-10-20190709Innocent PhiriNo ratings yet
- Technical DescriptionDocument6 pagesTechnical DescriptionJigar MehtaNo ratings yet
- Courses Offered in Spring 2015Document3 pagesCourses Offered in Spring 2015Mohammed Afzal AsifNo ratings yet
- Gereatric Depression ScaleDocument8 pagesGereatric Depression ScaleKheista Prima NurmalaNo ratings yet
- Contoh Implementasi QMSDocument8 pagesContoh Implementasi QMSIINNo ratings yet
- IMPRSDocument11 pagesIMPRSridho kusumaNo ratings yet
- Contoh Teks HortatoryDocument4 pagesContoh Teks HortatoryZonia AlqanitaNo ratings yet
- Weekly Science Report 29th July 2022Document12 pagesWeekly Science Report 29th July 2022John SmithNo ratings yet
- Topic 1: Introduction To Telecommunication: SPM1012: Telecommunication and NetworkingDocument22 pagesTopic 1: Introduction To Telecommunication: SPM1012: Telecommunication and Networkingkhalfan athmanNo ratings yet
- PH G12 S1Document9 pagesPH G12 S1mahmoudNo ratings yet
- Technical Manual Organizational, Direct Support, and General Support Maintenance Repair Parts and Special Tools Lists (Including Depot Maintenance Repair Parts and Special Tools)Document30 pagesTechnical Manual Organizational, Direct Support, and General Support Maintenance Repair Parts and Special Tools Lists (Including Depot Maintenance Repair Parts and Special Tools)Henry PalNo ratings yet
- Economics (Micro and Macro Economics)Document13 pagesEconomics (Micro and Macro Economics)aagampreet99No ratings yet
- Mud Motor DV826Document1 pageMud Motor DV826CAMILO ALFONSO VIVEROS BRICEÑONo ratings yet