0% found this document useful (0 votes)
89 views7 pagesCoronary Artery Bypass Grafting Overview
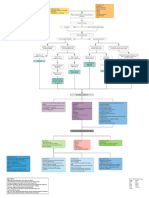
This document provides information on coronary artery bypass grafting (CABG) surgery, including definitions, indications, nursing care considerations, and postoperative assessments. CABG is performed to relieve angina and reduce coronary artery disease risk by grafting arteries or veins around narrowed coronary arteries. Postoperative nursing care focuses on monitoring the patient's recovery in the intensive care unit while on a ventilator before moving to a step-down unit. Assessments after surgery center on pain management and respiratory, cardiac, and renal function.
Uploaded by
flipside22Copyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
89 views7 pagesCoronary Artery Bypass Grafting Overview
This document provides information on coronary artery bypass grafting (CABG) surgery, including definitions, indications, nursing care considerations, and postoperative assessments. CABG is performed to relieve angina and reduce coronary artery disease risk by grafting arteries or veins around narrowed coronary arteries. Postoperative nursing care focuses on monitoring the patient's recovery in the intensive care unit while on a ventilator before moving to a step-down unit. Assessments after surgery center on pain management and respiratory, cardiac, and renal function.
Uploaded by
flipside22Copyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd