Professional Documents
Culture Documents
Radiopaque Periapical Lesion Variances
Uploaded by
Sasa AprilaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Radiopaque Periapical Lesion Variances
Uploaded by
Sasa AprilaCopyright:
Available Formats
64
DENTINO
JURNAL KEDOKTERAN GIGI
Vol IV. No 1. Maret 2019
THE VARIANCE OF RADIOPAQUE IMAGES COMMONLY FOUND IN
PERIAPICAL LESION USING PERIAPICAL RADIOGRAPHIC TECHNIQUE (Review
article)
Indra G1, Ria F2, Lusi E, Azhari2
1
Residence at Oral and Maxillofacial Radiology Specialist Programme, Faculty of Dentistry,
Padjadjaran University, Bandung, Indonesia
2
Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, Padjadjaran
University Bandung, Indonesia
ABSTRACT
Background: Two pathological views are presented in radiographic imaging: radiolucency and radiopacity. In
radiographic examination, radiopaque lesions are reported as the most common manifestation to be found.
Opaque lesions are displayed into various depictions thus more specific examination is required to distinguish
respective lesions. Objectives: Investigate radiopacity aspect of periapical lesions using literature review to aid
dental practitioners obtain final diagnosis, differential diagnosis, and identification of each periapical opaque
lesion. Discussion: Assessing respective matter about lucent and opaque lesion images in periapical tissue, this
review resulted in the identification of elusive characterization in each opaque lesion. Conclucion:
Radiographically, each diagnosis possesses particular characteristic which differ each periapical opaque lesion
from another.
Keyword: Opaque lesion characteristic, periapical opaque lesion, periapical radiograph
Correspondence: Indra Gunawan, c/o: Residence of Oral and Maxillofacial Radiology Specialist Programme,
Faculty of Dentistry, Padjadjaran University, JL Sekeloa Selatan 1 Bandung, Indonesia. e-mail:
indragunawandrg290376@gmail.com
INTRODUCTION For many radiologists, radiopaque lesion of
jaw bone is known as terra incognita, the Latin term
Inflammatory lesion in periapical region is a for "unknown land". Jaw lesions mostly depict
local response of bone surrounding dental apex to radiolucent appearance, such as periapical
periapical tissue destruction which induced by the (radicular) cyst, folicular (dentigerous) cyst,
expansion of periodontal disease. Infectious agents
ceratocyst odontogenic tumor (previously known as
from necrotized pulp spread via root apex to promote
odontogenic keratocyst), and ameloblastoma; which
inflammatory reaction in surrounding bone.1 This are well-explained in radiological literatures. Yet
frequently affects alveolar bone in periapical region radiopaque presentations of jaw lesion are
or surrounding teeth.2 This periapical lesion is continuously gained less attention. Radiological
identified as an abnormality around root apex, diagnosis of periapical and jaw lesions are obtained
periodontal membrane and alveolar bone.2,3,4 through several imaging aspects such as attenuation,
Commonly began with inflammation or necrosis of margination (narrow or wide transition zone) and the
the pulp, this condition then progressively circulate
interrelation with adjacent teeth.6
inflammatory mediators through apical foramen to
initiate the development of periapical lesion.2,5 Causing resorption in periapical bone
Traditionally, periapical radiograph has been structure, progressive phase of inflammatory
clinically used to diagnose periapical pathology.18 condition can be identified by radiolucent lesion in
Indra G: The Variance Of Radiopaque Images Commonly 65
radiographic examination.19 Radiopaque lesion may osseus dysplasia usually progresses in the anterior of
also be identified near dental apices and should be mandibula and merely includes one or several teeth.
discerned, as it is possibly progressed from Other restricted manifestation occured in posterior
endodontic and non-endodontic problem.20 region of the jaw, commonly affects molar tooth, is
entitled as focal cemento-osseus dysplasia.
The purpose of this review is to discuss about Cemento-osseus dysplasia itself typically involves
radiopacity aspect of periapical lesion through two or more jaw quadrants.
literature review and assist dental practitioner obtain
final diagnosis, differential diagnosis, and In radiographic presentation, initial lesion
identification of each periapical opaque lesion. manifests as a lucent area which developed into a
combination of lucent and opaque lesion and
This article elucidates four common lesions frequently with central calcified area. Initial lesion
frequently found in dental practice, comprised of: (lucent) may be confounded by periapical
cementoblastoma, cemento-osseus dysplasia, inflammatory lesions like cyst, granuloma, and
condensing osteitis/periapical sclerosing osteitis and abscess. Differ from other inflammatory lesions,
hypercementosis. These lesions are reported as the cemento-osseus dysplasia/cementoma is usually
most common lesion to be found in periapical associated with unrestored vital teeth, intact
region.6 periodontal ligament and lamina dura, and visible
Cementoblastoma calcified epicenter.8
Cementoblastoma frequently occurs among
adolescent and children under age 20 (50%) and
under 30 (75%). The incident varies from less than
1% to 6.2% among other odontogenic tumors. More
than 75% cementoblastomas are developed in
mandibula where 90% progressed in mandibular first
molar or second premolar area. Radiographically,
cementoblastoma appeared as sclerotic periapical Figure 2. Progression of cemento-osseus dysplasia
lesion with clear and sharp border surrounded by (left to right)
round radiolucency which attached closely to dental
root.6 Lesion progression is comprised of three
phases, where initial phase presented as
radiolucency, followed by radiolucent image with
patchy opacity inside radiolucent structure. The last
stage is depicted by compact radiopaque lesion
surrounded by thin radiolucent line.9
Cemento-osseus dysplasia possesses a strong
tendency in race and sexes, where most lesions occur
among Black and Asian females in fourth or five
decade of life. Only focal variant frequently reported
Figure 1. Round sclerosing and opaque lesion in in White female. Cemento-osseus dysplasia often
dental periapical region with clear and sharp border manifests with no noticeable symptoms yet it
surrounded by round radiolucent area. manifests with blunt pain. This lesion can also be
mystified by osteomyelitis and drainage of necrotic
Cemento-osseus dysplasia bone debris in oral cavity or skin surface through
osteocutan sinus.6
Cemento-osseus dysplasia is hamartomatosed
process which frequently related with dental apex.
Presented in many clinical variations, respective
terminology becomes quite confusing. Cemento-
66 Dentino (Jur. Ked. Gigi), Vol IV. No 1. Maret 2019 : 64-68
Condensing osteitis/periapical condensing osteitis Condensing osteitis/periapical sclerosing
osteitis occurs in child and adolescent, frequently in
Condensing osteitis (CO), known as focal mandibular premolar and molar. This is a localized
sclerosing osteomyelitis, is a persistent, form of osteitis and reactive sclerosis which
asymptomatic, pathological change in bone structure surrounds dental apex persisted with pulpitis or pulp
which considered as a response upon long-term necrosis. Adjacent tooth commonly present the
inflammatory stimulus and low-grade stage of widening in periodontal ligament or the presence of
inflamed or necrotized pulp.10 periapical inflammatory lesion (like granuloma, cyst
or abscess). In radiographic image, condensing
osteitis/periapical sclerosing osteitis appears as non-
expansive, uni or multifocal periapical sclerotic
lesion, with ill-defined margin related to dental
caries.6
Biopsy is not required to diagnose CO. It is
assessed based on clinical manifestations and
radiographic image where root canal treatment is
considered as selected treatment.11
Hypercementosis
Hypercementosis is an excessive non-
neoplastic cementum deposition blend with normal
root cementum.12 In most cases, etiologic factor
remains unknown. The lesion progressed in supra-
erupted teeth as the consequence of antagonist tooth
loss. Another cause of hypercementosis is
inflammation, which commonly induced by
scleroting ostetitis. This lesion is sometimes
Figure 3. Condensing osteitis (CO): CBCT exposed associated with hyper-occlusion or tooth fracture .1
a diffuse radiopaque lesion in the apex of mandibular
molar (arrow) (D), adjacent to inflammatory Hypercementosis generally requires no
periapical lesion (arrow) (E). treatment. Any dental intervention therapy, be it tooth
extraction, endodontic or orthodontic therapy, will
demand adequate preventive measure to avoid further
complication generated from this condition.21
Figure 4. Presentation of ill-defined border with
progressive transition from condensed (short arrow)
to normal trabecula near alveolar crest (long arrow)
Indra G: The Variance Of Radiopaque Images Commonly 67
varied in size, 2-3 mm in diameter. Internal structure
presents radiopaque image surrounded by thin
radiolucent. It is located in the apical of mandibular
first permanent molar and sometimes in the
premolar. Large attachment in dental root may cause
localized extension of cortical plate. The incident
occurs between age 8 and 44 with average age of 20.
Cemento-osseus dysplasia is presented as
round, small-sized unilocular lesion in vital teeth,
around 5-6 mm. Internal structure is divided into 3
stages: radiolucent, patchy opacity in radiolucent,
and radiopaque surrounded with radiolucent.
Common location is in the apical of vital lower
incisiv. It does not generate reposition of adjacent
tissue. The incidence commonly found in middle-
aged adult.
Scleroting/condensing osteitis occurs in
Figure 5. Enlarged root surrounded by radiolucent
non-vital teeth (large caries) in irregular form.
in PDL space and adjoining intact lamina dura. This
Internal structure expresses irregular and diffuse
enlargement may possibly progressed as
radiopaque, located commonly in mandibula
cementoblastoma
premolar and molar. It is typically found in adult in
DISCUSSION three to seven decade without any difference in sex
predilection.
Tooth-associated lesion can be found in
periapical (around dental apex), interapical (between Hypercementosis demonstrates an
apex of two adjacent teeth), or pericoronal (around enlargement image around affected root. The tooth
dental crown) area. Pericoronal lesions are originated may be vital or non-vital with different size and form
from ectoderm-derived component of enamel organ adjusting the root shape. Internal structure presents
(ameloblast). Periapical lesions generally progress radiopaque area with well-defined border located in
from endodontal or periodontal or ectodermal of affected root cementum. Hypercementosis are
dental papilla (odontoblast) or follicle (cementoblast, mostly found in Indian population and usually
fibroblast and osteoblast) of inflammatory disease related with one or more local and systemic factors.
The incident of hypercementosis based on race and
area.6,13
population are not yet able to determine. Mandibular
Inflammatory changes in periapical bone molar is the most frequent tooth to be affected,
structure are the consequence of root canal system followed by mandibular second premolar, upper first
infection and the result of osteoclastic or osteoblastic premolar and lower first premolar. 22 Clinical aspect
activity. These changes are identified by like pulp sensibility and vitality test mostly assist the
radiographic examination in the presence of assessment of periapical change originated from
radiolucent or radiopaque image.14 Changes in bone inflammatory or non-inflammatory causes. 23
structure may be presented in inflammatory,
There are several variances used to guide the
neoplastic, displastic, and metabolic lesions. 15-17
assessment of clinical and radiological findings which
Radiolucent area is frequently identified with root
is remarkably convenient in daily practice as a dentist.
canal infection yet radiopaque lesion may also be
Cone-Beam Computed Tomography (CBCT) is also a
induced by similar causation hence equal concern
should be given to prevent misdiagnosis. significant tool for diagnosis in dentistry, 24 which
enable the detection of periapical lesion with high
Cementoblastoma commonly resembles a accuracy compared to periapical and panoramic
golf ball attached on the root of vital tooth which technique. CBCT characteristics and overall
68 Dentino (Jur. Ked. Gigi), Vol IV. No 1. Maret 2019 : 64-69
interpretation strategy enhance a comprehensive 11. Miloglu O, Yalcin E, Buyukkurt MC,
multi-dimensional examination thus clarify accurate Acemoglu H. The frequency and characteristics of
location of periapical lesion, bone resoprtion or bone idiopathic osteosclerosis and condensing osteitis lesions in
formation characteristic and accurate detection of a Turkish patient population. Med Oral Patol Oral Cir
Bucal. 2009;14(12):e640-5.
any regressive lesion.25 From this review, it can be https://doi.org/10.4317/medoral.14.e640.
concluded that each radiographic image expressed [ Links ]
particular characteristic which distinguish one 12. Brad W. Neville, Douglas D. Damm, Carl
periapical opaque lesion from the others. M. Allen, Angela C. Chi. Oral and Maxillofacial
Pathology, 4th Ed, 2016, Elsevier, Canada, p. 88.
REFERENCE 13. Morgan PR. Odontogenic tumors: a review.
Periodontol 2000, 2011;57(1):160–176.
1. White and Paroah. Oral Radiology 14. Brunno Santos Freitas Silva, Mike
Principles and Intrepretation 7nd ed, 2017. ,
Reis Bueno Fernanda P. Yamamoto-Silva,
Mosby. Elsevier.Inggris, p. 315.
Ricardo Santiago Gomez, Ove
2. AO Akinyamoju, SO Gbadebo, and BF
Adeyemi, Periapical Lesion of The Jaws : A review Andreas Peters, Carlos Estrela. Differential
of 104 Cases in Ibadan, Ann Ibd. Pg. Med 2014; diagnosis and clinical management of
12(2):115-119 periapical radiopaque/hyperdense jaw
lesions, 2017:31, p.17.
3. Ramanpreet B, Simarpreet SV, Rajat B,
15. Fang Z, Jin S, Zhang C, Wang L, He Y.
Amandeep B, Shruti G. Histopathological insight
Misdiagnosis of osteosarcoma as
into periapical lesions: an institutional study from
cementoblastoma from an atypical
Punjab. Int J Oral Maxillofac Pathol 2012; 3(3):2-7.
mandibular swelling: a case report. Oncol
4. Safi L, Adl A, Azar MR, Akbary R. A
Lett. 2016;11(6):3761-5.
Twentyyear sur vey of pathologic reports of two
https://doi.org/10.3892/ol.2016.4433
common types of chronic periapical lesions in Shiraz
[ Links ]
Dental School. J Dent Res Dent Clin Dent Prospects
16. Lerman MA, Do C, Gunaratnam L,
2008; 2(2): 63-67.
Kulkarni C, Tucker K, Woo SB. Localized mandibular
5. Soares JA, Leonardo MR, da Silva LAB,
enlargement in end-stage renal disease: two case reports
Filho TM, Ito IY. Histomicrobiologic aspects of the and a review of the literature. Oral Surg Oral Med Oral
root canal system and periapical lesions in dogs’ Pathol Oral Radiol .2012;113(3):384-390.
teeth after rotary instrument and intracanal dressing
https://doi.org/10.1016/j.tripleo.2011.04.03 9 [ Links ]
with Ca(OH)2 pastes. J Appl Oral Sci 2006; 14: 355-
364. 17. Estrela C, Decurcio DA, Silva JA, Batista
AC, Lima NCS, Silva BSF et al. Immune-inflammatory
6. Joel K. Curé, MD, Surjith Vattot, Ritu
cell profile and receptor activator of nuclear factor kappa B
Shah. Radiopaque Jaw Lesions: An Approach to the
Differential Diagnosis. ligand/osteoprotegerin expression in
2012. RSNA RadioGraphics. Vol. 32:1909– persistent apical periodontitis after root
1925. Published online
canal retreatment failure. J Endod. 2016 ;
42(3) : 439-46.
10.1148/rg.327125003
https://doi.org/10.1016/j.joen.2015.11.012 [
7. Slootweg PJ. Lesions of the jaws.
Links ]
Histopathology 2009;54(4):401–418.
18. Paula-Silva FWG, Wu M, Leonardo MR,
8. Resnick CM, Novelline RA. Cemento-
Bezerra da Silva L, Wesselink PR. Accuracy of Periapical
osseous dysplasia, a radiological mimic of periapical
Radiography and Cone-Beam Computed Tomography
dental abscess. Emerg Radiol 2008;15(6):367–374.
Scans in Diagnosing Apical Periodontitis Using
9. Whaites E, Drage N. Essentials of Dental
Histopathological Findings as a Gold Standard. J Endod.
Radiography and Radiology , Fifth Ed, 2013,
2009;35(7):1009–1012.
Churchill Livingstone, Elsevier, Inggris, p. 356.
19. Nair PNR. Biology and pathology of apical
10. Green TL, Walton RE, Clark JM, Maixner
periodontitis. In: Estrela C. Endodontic science. 2nd ed.
D. Histologic examination of condensing osteitis in
São Paulo: Artes Médicas; 2009. p. 285-347.
cadaver specimens. J Endod. 2013;39(8):977-
9.https://doi.org/10.1016/j.joen.2013.02.002
[ Links ].
69
20. Bueno MR, De Carvalhosa AA, Castro PHS, Pereira KC, Borges FT, Estrela C. Mesenchymal
chondrosarcoma mimicking apical periodontitis. J Endod 2008; 34(11):1415-9.
https://doi.org/10.1016/j.joen.2008.08.016.
21. Pappen FG, Fagonde CD, Martos J et al.
Hypercementosis: a challenge for
endodontic therapy. RSBO 2011;8:321–8.
22. Consolaro A, Consolaro RB, Francischone LA. Cementum, apical morphology and hypercementosis: a
probable adaptive response of the periodontal support tissues and potential orthodontic implications. Dental Press
J Orthod 2012;17:21–30.
23. Bruno KF, Barletta FB, Felippe WT, Silva JA, Alencar AHG, Estrela C. Oxygen saturation in the dental
pulp of permanent teeth: a critical review. J Endod.
2014;40(8):1054-7. ht
tps://doi.org/10.1016/j.joen.2014.04.01.
24. Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam
computed tomography. J Endod. 2008;34(11):1325-31. https://doi.org/10.1016/j.joen.2008.08.013
25. Nunes CA, Guedes OA, Alencar AH, Peters AO, Estrela CR, Estrela C. Evaluation of periapical lesions
and their association with maxillary sinus abnormalities on cone-beam computed tomographic images. J Endod.
2016:42(1):42-46. https://doi.org/10.1016/j.joen.2015.09.014
You might also like
- Oral Medicine & Pathology from A-ZFrom EverandOral Medicine & Pathology from A-ZRating: 5 out of 5 stars5/5 (9)
- Radiopaque Periapical Lesion CharacteristicsDocument6 pagesRadiopaque Periapical Lesion CharacteristicsAgum Nila Sari IINo ratings yet
- Classification of Periradicular Pathosis:: 4-Acute Apical AbscessDocument7 pagesClassification of Periradicular Pathosis:: 4-Acute Apical AbscessOmar MohamedNo ratings yet
- Zebra XX, Part 2 PDFDocument3 pagesZebra XX, Part 2 PDFRamona MateiNo ratings yet
- Differential Diagnosis of Periapical Radiolucencies and RadiopacitiesDocument27 pagesDifferential Diagnosis of Periapical Radiolucencies and RadiopacitiesDerya İçözNo ratings yet
- Cystic Lesions of MandibleDocument18 pagesCystic Lesions of MandibleRahul ShindeNo ratings yet
- Radiographic Appearance of Common Dental Diseases: Asst. Prof. Sana'a JamalDocument23 pagesRadiographic Appearance of Common Dental Diseases: Asst. Prof. Sana'a JamalRmz AlfaizNo ratings yet
- ANTICANCER RESEARCH 34: 2533-2536 (2014Document4 pagesANTICANCER RESEARCH 34: 2533-2536 (2014CindyNo ratings yet
- Radio Graphical Approach To Jaw LesionsDocument13 pagesRadio Graphical Approach To Jaw Lesionsdr_marinaNo ratings yet
- Quistes OdontogénicosDocument15 pagesQuistes OdontogénicosYsabel GutierrezNo ratings yet
- Benign Non Odontogenic Lesions - 6Document97 pagesBenign Non Odontogenic Lesions - 6Thaer ZabenNo ratings yet
- Lesion DescriptionDocument53 pagesLesion DescriptionLames Ali Sayed Ahmed AttiaNo ratings yet
- William L. Chung Kurt Summersgill Mark Ochs: OdontogenicDocument18 pagesWilliam L. Chung Kurt Summersgill Mark Ochs: OdontogenicyosephineninaNo ratings yet
- Dentigerous Cysts With Diverse Radiological Presentation Highlighting Diagnostic ChallengesDocument14 pagesDentigerous Cysts With Diverse Radiological Presentation Highlighting Diagnostic ChallengesDSS.JORGE ALBERTO PÉREZ HERNÁNDEZNo ratings yet
- A Radiolucency Is The Darker Area Within A Bone On A Conventional RadiographDocument83 pagesA Radiolucency Is The Darker Area Within A Bone On A Conventional Radiographkabir shaikhNo ratings yet
- Gambar Radiologi Semester 5Document15 pagesGambar Radiologi Semester 5Faidhi Rahman HafizhNo ratings yet
- Benign and MalignantDocument16 pagesBenign and MalignantRSU DUTA MULYANo ratings yet
- Imaging of Odontogenic InfectionsDocument14 pagesImaging of Odontogenic InfectionsMaria Corena100% (1)
- Sclerotic Lesions of The JawDocument9 pagesSclerotic Lesions of The JawGalgalo GarbichaNo ratings yet
- Fibrous Dysplasia of The Anterior Mandible A Rare HDocument6 pagesFibrous Dysplasia of The Anterior Mandible A Rare HyesikaichaaNo ratings yet
- Periapical Cemento-Osseous Dysplasia Case ReportDocument13 pagesPeriapical Cemento-Osseous Dysplasia Case ReportDha Dina SevofrationNo ratings yet
- A solitary mixed periapical lesion seen at the apex of tooth 47Document35 pagesA solitary mixed periapical lesion seen at the apex of tooth 47AmitaNo ratings yet
- Cementoblastoma and Periapical Cemento-Osseous DysplasiaDocument15 pagesCementoblastoma and Periapical Cemento-Osseous DysplasiaHessa AloliwiNo ratings yet
- Infection of The JawDocument51 pagesInfection of The JawMutia Safitri0% (1)
- Cysts of The JawsDocument26 pagesCysts of The JawsPranay NeemaNo ratings yet
- Fibro-Osseous Lesions A ReviewDocument4 pagesFibro-Osseous Lesions A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Dental Radiology Image InterpretationDocument12 pagesDental Radiology Image Interpretationمحمد العراقيNo ratings yet
- How Can We Diagnose and Treat Osteomyelitis of The Jaws As Early As PossibleDocument11 pagesHow Can We Diagnose and Treat Osteomyelitis of The Jaws As Early As Possiblebucomaxilofacial.hfiNo ratings yet
- Differential Diagnosis of Pericoronal RadiolucenciesDocument30 pagesDifferential Diagnosis of Pericoronal RadiolucenciesakNo ratings yet
- Extensive Radicular Cyst of The Mandible: A Rare Case ReportDocument5 pagesExtensive Radicular Cyst of The Mandible: A Rare Case ReportTheodora Elena BulaiNo ratings yet
- S SunilDocument4 pagesS SunileditorompjNo ratings yet
- Odonto MaDocument5 pagesOdonto MaashariNo ratings yet
- 11 Fibro Osseous LesionsDocument22 pages11 Fibro Osseous Lesionsفراس الموسويNo ratings yet
- COF4Document4 pagesCOF4ton viet nguyenNo ratings yet
- Min 2018Document7 pagesMin 2018CindyNo ratings yet
- 5 - Odontogenic KeratocytesDocument8 pages5 - Odontogenic KeratocytesRandolph Allan Lopez BalladaNo ratings yet
- Dafpus 1Document8 pagesDafpus 1Winda WidhyastutiNo ratings yet
- Odontogenic Cysts and TumorsDocument52 pagesOdontogenic Cysts and TumorsJuliett González CerdánNo ratings yet
- Radiographic Interpretation of Tumors of The Jaws: Drg. Shanty Chairani, M.SiDocument82 pagesRadiographic Interpretation of Tumors of The Jaws: Drg. Shanty Chairani, M.SiDini Dwi PuspitaNo ratings yet
- BCR 2013 200316Document4 pagesBCR 2013 200316ay lmaoNo ratings yet
- Inflammatory Lesions of The JawsDocument54 pagesInflammatory Lesions of The JawsAi Rafikah Nurpratiwi100% (1)
- tmpB15C TMPDocument5 pagestmpB15C TMPFrontiersNo ratings yet
- Ohns 3 182Document8 pagesOhns 3 182kalixinNo ratings yet
- Oral Pathology - Case Study 1 - FinalDocument5 pagesOral Pathology - Case Study 1 - Finalapi-262534732No ratings yet
- Diagnostic Imaging in Oral IntechDocument27 pagesDiagnostic Imaging in Oral Intechjamal100% (1)
- Odontogenic Keratocyst: - Jayalakshmi Preetha Meyyanathan CRIDocument48 pagesOdontogenic Keratocyst: - Jayalakshmi Preetha Meyyanathan CRIJayalakshmi PreethaNo ratings yet
- Managing Dental Issues in Cleidocranial DysplasiaDocument7 pagesManaging Dental Issues in Cleidocranial DysplasiaVesna AmbarkovaNo ratings yet
- Article-PDF-Vajendra Joshi Kalwa Pavan Kumar Shalini Joshi Sujatha Gopal-177Document3 pagesArticle-PDF-Vajendra Joshi Kalwa Pavan Kumar Shalini Joshi Sujatha Gopal-177sagarjangam123No ratings yet
- CA LS Bướu Nhiều Hốc - Multilocular Radiolucency in the Body of MandibleDocument4 pagesCA LS Bướu Nhiều Hốc - Multilocular Radiolucency in the Body of MandibleThành Luân NguyễnNo ratings yet
- Giant Cell Lesions of Oral CavityDocument4 pagesGiant Cell Lesions of Oral CavityPreetam PatnalaNo ratings yet
- Craniofacial FeaturesDocument6 pagesCraniofacial FeaturesDaliz Ü RuizNo ratings yet
- Oral Pathology: 2-Mesenchymal Origin Tumors A - Odontogenic FibromaDocument4 pagesOral Pathology: 2-Mesenchymal Origin Tumors A - Odontogenic Fibromaعلي صادق جعفرNo ratings yet
- Fibrous DysplasiaDocument2 pagesFibrous DysplasiaGus SwanjayaNo ratings yet
- TOOTH ANKYLOSIS AND ITS ORTHODONTIC IMPLICATIONSDocument4 pagesTOOTH ANKYLOSIS AND ITS ORTHODONTIC IMPLICATIONSjesuNo ratings yet
- 7 OsteosarcomaDocument4 pages7 OsteosarcomaDodNo ratings yet
- Radiograf Idiopathic Osteosclerosis Gigi Molar Ketiga Impaksi Pada Cone Beam Computed TomographyDocument6 pagesRadiograf Idiopathic Osteosclerosis Gigi Molar Ketiga Impaksi Pada Cone Beam Computed Tomographyapril perdaniNo ratings yet
- Bone Lesion Guide: Fibro-Osseous ConditionsDocument16 pagesBone Lesion Guide: Fibro-Osseous Conditionsjack jonNo ratings yet
- Palatal SwellingsDocument6 pagesPalatal Swellingsopi akbarNo ratings yet
- Complications in UveitisFrom EverandComplications in UveitisFrancesco PichiNo ratings yet
- A Systematic Review and Meta-Analysis On Bolton's Ratios: Normal Occlusion and MalocclusionDocument26 pagesA Systematic Review and Meta-Analysis On Bolton's Ratios: Normal Occlusion and MalocclusionSasa AprilaNo ratings yet
- Clinical Manifestation of Oral TuberculosisDocument6 pagesClinical Manifestation of Oral TuberculosisSasa AprilaNo ratings yet
- Medoralv22 I5 p586Document9 pagesMedoralv22 I5 p586DivaNo ratings yet
- Business Continuity: The Ultimate Guide ToDocument35 pagesBusiness Continuity: The Ultimate Guide ToKhairul Nazmi Zainol AriffinNo ratings yet
- S7bamgx79xjgvxnzusoeav94b@2020 - 12 - 25.json 2Document1 pageS7bamgx79xjgvxnzusoeav94b@2020 - 12 - 25.json 2Sasa AprilaNo ratings yet
- Type 2 Diabetes Mellitus Disease Diagnosis and Treatment 2155 6156 1000533Document6 pagesType 2 Diabetes Mellitus Disease Diagnosis and Treatment 2155 6156 1000533Sasa AprilaNo ratings yet
- Diabetes Mellitus: The Epidemic of The Century: Akram T Kharroubi, Hisham M DarwishDocument19 pagesDiabetes Mellitus: The Epidemic of The Century: Akram T Kharroubi, Hisham M DarwishAna Cristine Silva Pires TomeNo ratings yet
- Classification Pathophysiology Diagnosis and Management of Diabetesmellitus 2155 6156 1000541Document9 pagesClassification Pathophysiology Diagnosis and Management of Diabetesmellitus 2155 6156 1000541AldaniaNo ratings yet
- JDM 2018111414202615 PDFDocument8 pagesJDM 2018111414202615 PDFSasa AprilaNo ratings yet
- BJSTR MS Id 001574 PDFDocument4 pagesBJSTR MS Id 001574 PDFSasa AprilaNo ratings yet
- Definition Classification and Diagnosis of Diabetes Prediabetes and Metabolic SyndromeDocument6 pagesDefinition Classification and Diagnosis of Diabetes Prediabetes and Metabolic SyndromeJianhua ShiNo ratings yet
- Diabetes Mellitus A Devastating Metabolic DisorderDocument5 pagesDiabetes Mellitus A Devastating Metabolic DisorderDaniela Mădălina GhețuNo ratings yet
- The Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose DietDocument11 pagesThe Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose DietSasa AprilaNo ratings yet
- JDM 2018111414202615 PDFDocument8 pagesJDM 2018111414202615 PDFSasa AprilaNo ratings yet
- The Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose DietDocument11 pagesThe Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose DietSasa AprilaNo ratings yet
- Definition Classification and Diagnosis of Diabetes Prediabetes and Metabolic SyndromeDocument6 pagesDefinition Classification and Diagnosis of Diabetes Prediabetes and Metabolic SyndromeJianhua ShiNo ratings yet
- BJSTR MS Id 001574 PDFDocument4 pagesBJSTR MS Id 001574 PDFSasa AprilaNo ratings yet
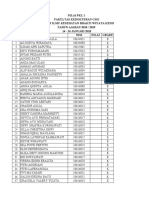
- Nilai PKL 1 Fakultas Kedokteran Gigi Institut Ilmu Kesehatan Bhakti Wiyata Kediri TAHUN AJARAN 2018 / 2019 14 - 26 JANUARI 2018 NO Nama NIM Nilai GradeDocument10 pagesNilai PKL 1 Fakultas Kedokteran Gigi Institut Ilmu Kesehatan Bhakti Wiyata Kediri TAHUN AJARAN 2018 / 2019 14 - 26 JANUARI 2018 NO Nama NIM Nilai GradeSasa AprilaNo ratings yet
- Erythema Multiforme Major: Case Report and Review of LiteratureDocument6 pagesErythema Multiforme Major: Case Report and Review of LiteratureSasa AprilaNo ratings yet
- Diabetes Mellitus A Devastating Metabolic DisorderDocument5 pagesDiabetes Mellitus A Devastating Metabolic DisorderDaniela Mădălina GhețuNo ratings yet
- SK 6 BL 9Document4 pagesSK 6 BL 9Sasa AprilaNo ratings yet
- D 023Document5 pagesD 023Ummu ZaFaNo ratings yet
- Jurnal-6-Naskah 7 JURNAL PDGI Vol 61 No 1Document6 pagesJurnal-6-Naskah 7 JURNAL PDGI Vol 61 No 1Nayda FitrinaNo ratings yet
- Erythema Multiforme Major: Case Report and Review of LiteratureDocument6 pagesErythema Multiforme Major: Case Report and Review of LiteratureSasa AprilaNo ratings yet
- 48 95 1 SMDocument6 pages48 95 1 SMMahesa DiantariNo ratings yet
- Scientific Dental Journal: Pigmented Oral Lichen Planus: A Case ReportDocument6 pagesScientific Dental Journal: Pigmented Oral Lichen Planus: A Case ReportSasa AprilaNo ratings yet
- BPJ Vol 11 No 1 P 167-170Document5 pagesBPJ Vol 11 No 1 P 167-170Retno Arienta SariNo ratings yet
- Orofacial Pain Conditions: Pain and Oral Mucosa: Berbagai Kondisi Nyeri Orofasial: Nyeri Dan MukosaDocument5 pagesOrofacial Pain Conditions: Pain and Oral Mucosa: Berbagai Kondisi Nyeri Orofasial: Nyeri Dan MukosaAlvionita AnggrainyNo ratings yet
- 6 ErythemaMultiformeClassificationandImmunopathogenesisDocument8 pages6 ErythemaMultiformeClassificationandImmunopathogenesisRandilufti SantosoNo ratings yet
- Australian Dental Journal - 2009 - Evans - The Caries Management System An Evidence Based Preventive Strategy For DentalDocument9 pagesAustralian Dental Journal - 2009 - Evans - The Caries Management System An Evidence Based Preventive Strategy For DentalHarjotBrarNo ratings yet
- Hybrid Hyrax Distalizer JO PDFDocument7 pagesHybrid Hyrax Distalizer JO PDFCaTy ZamNo ratings yet
- VITA en Viktor Fuergut Broschuere Screen enDocument8 pagesVITA en Viktor Fuergut Broschuere Screen enHamidNo ratings yet
- 4 Intraoral Radiographic TechniquesDocument35 pages4 Intraoral Radiographic TechniquesDan 04100% (1)
- The EnamelDocument27 pagesThe EnamelYousef KhallafNo ratings yet
- Chotu PerioDocument18 pagesChotu PerioKhushi DesaiNo ratings yet
- Krasner and Rank Ow Joe 2004Document13 pagesKrasner and Rank Ow Joe 2004Eva MuNo ratings yet
- Prosthetic tooth articulation concepts for denturesDocument4 pagesProsthetic tooth articulation concepts for denturesRaluca MarinNo ratings yet
- Ijcmr - 1761Document2 pagesIjcmr - 1761Mukarram FaridiNo ratings yet
- The Center of The Incisive Papilla For The Selection of Complete Denture MaDocument6 pagesThe Center of The Incisive Papilla For The Selection of Complete Denture MaAndreea-Paula PădureNo ratings yet
- 2 Full-Cusp Class II Malocclusion With BilateralDocument20 pages2 Full-Cusp Class II Malocclusion With BilateralJULIAN ANDRES CAICEDO RIVERANo ratings yet
- Functional Occlusion: Presented By-Dr. Ruchi Saxena Dept. of OrthodonticsDocument186 pagesFunctional Occlusion: Presented By-Dr. Ruchi Saxena Dept. of OrthodonticsDrkishore Reddy0% (1)
- Functional Occlusion and OrthodonDocument9 pagesFunctional Occlusion and OrthodonAlberto DeodatoNo ratings yet
- CementumDocument10 pagesCementumAshish BisaneNo ratings yet
- RadioDocument9 pagesRadioMohammed JabrNo ratings yet
- Orthodontic Management of Impacted CanineDocument7 pagesOrthodontic Management of Impacted CanineplsssssNo ratings yet
- OrthoDocument22 pagesOrthosivaleela gNo ratings yet
- A) Multiple Choice Questions/: Stomatology ExamsDocument14 pagesA) Multiple Choice Questions/: Stomatology ExamsNJIOJOP TSAGOP CHRISTIANNo ratings yet
- The Relationship Between Dentin Microhardness and Tubule DensityDocument5 pagesThe Relationship Between Dentin Microhardness and Tubule DensitySitiKhadijahNo ratings yet
- Class III High Angle Malocclusion Treated With Orthodontic Camouflage (MEAW Therapy)Document24 pagesClass III High Angle Malocclusion Treated With Orthodontic Camouflage (MEAW Therapy)Beatriz ChilenoNo ratings yet
- Compre Ortho PedoDocument11 pagesCompre Ortho PedoPatricia L.No ratings yet
- Seltzer and Benders Dental Pulp 2012Document120 pagesSeltzer and Benders Dental Pulp 2012Izabella Efremnko100% (2)
- Biomechanical Principles of PreparationsDocument369 pagesBiomechanical Principles of PreparationsDr. Lil BaEisNo ratings yet
- 3-Molar Distalization With Modified Palatal DistalizerDocument8 pages3-Molar Distalization With Modified Palatal DistalizerJunaid Israr - OrthodonticsNo ratings yet
- Wa0006.Document2 pagesWa0006.blessy winsletNo ratings yet
- Occlusion in FPDDocument108 pagesOcclusion in FPDVishal ReddyNo ratings yet
- Home Economics Chapter on Personal Hygiene and GroomingDocument24 pagesHome Economics Chapter on Personal Hygiene and GroomingFrancisco C. ArianNo ratings yet
- Guidelines For The Orthodontic Management of The Traumatised ToothDocument8 pagesGuidelines For The Orthodontic Management of The Traumatised ToothSaumya SinghNo ratings yet
- Principles of OrthodonticsDocument75 pagesPrinciples of OrthodonticshappymeluckymeNo ratings yet
- Occlusal CorrectionDocument5 pagesOcclusal CorrectionTejas KhaireNo ratings yet