Professional Documents
Culture Documents
The Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose Diet
Uploaded by
Sasa AprilaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose Diet
Uploaded by
Sasa AprilaCopyright:
Available Formats
Journal of Diabetes Mellitus, 2018, 8, 160-170
http://www.scirp.org/journal/jdm
ISSN Online: 2160-5858
ISSN Print: 2160-5831
The Effect of Cortex Lycii on Rattus norvegicus’
Blood Glucose Level Using a High Glucose Diet
Hongping Tan, Cristian Vinanzaca
John Bowne High School, Flushing, NY, USA
How to cite this paper: Tan, H.P. and Abstract
Vinanzaca, C. (2018) The Effect of Cortex
Lycii on Rattus norvegicus’ Blood Glucose One of the primary problems in the United States is diabetes. Cortex Lycii is
Level Using a High Glucose Diet. Journal of an herb from Asia mostly used in traditional Chinese medicine. Although its
Diabetes Mellitus, 8, 160-170.
main purpose is not for lowering blood glucose levels, there are studies on
https://doi.org/10.4236/jdm.2018.84016
Cortex Lycii with other substances which have proven it can lower glucose
Received: May 21, 2018 level in type 2 diabetes rat. Unlike other experiments, this experiment only
Accepted: November 16, 2018 used Cortex Lycii as a single unit to see if there was any effect on blood glu-
Published: November 19, 2018
cose level. Also an observation was done on if Cortex Lycii could reduce
Copyright © 2018 by authors and blood glucose level after ingesting a high glucose diet. Rattus norvegicus was
Scientific Research Publishing Inc. used in this project and in order for the subject to consume Cortex Lycii, the
This work is licensed under the Creative
herb was boiled and the liquid was given for consumption. In order to in-
Commons Attribution International
License (CC BY 4.0). crease the rats’ glucose levels, corn syrup and white sugar were added to the
http://creativecommons.org/licenses/by/4.0/ mixture. The data showed significant decrease of blood glucose when Cortex
Open Access Lycii liquid was ingested. This research has shown that Cortex Lycii can be a
potential treatment for hyperglycemia or diabetes. With further research,
there can be an alternative treatment rather than injecting external hormones
(Insulin).
Keywords
Cortex Lycii, Diabetes, Blood Glucose Level, Health, Hyperglycemia
1. Introduction
Currently, diabetes is one of the top 10 causes of leading deaths in United States.
The most common sign of having diabetes is hyperglycemia. Hyperglycemia is
described as having abnormally high blood glucose level. Over time, having
hyperglycemia can lead to organ damage. The reason behind type 2 diabetes and
hyperglycemia is the body not producing enough insulin for glucose intake.
When human takes foods, the foods are broken down into glucose. When glu-
DOI: 10.4236/jdm.2018.84016 Nov. 19, 2018 160 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
cose enters the bloodstream, the pancreas secretes insulin to keep the glucose
level down. Insulin is a hormone that signals the cells that lack energy to accept
glucose into their cell wall. When not enough insulin hormones are produced,
glucose is unable to diffuse cells and causes the bloodstream to have high levels
of glucose. Since the cells are not getting enough glucose, they are weakened.
Blood glucose level can be tested using a glucometer. Small amounts of blood
can be collected using a lance and a test strip. The current treatment for hyper-
glycemia is injecting insulin into bloodstream.
This study has the potential to find alternative treatment for hyperglycemia to
combat diabetes. Using Rattus norvegicus as test subject is the most efficient way
to test a treatment without using human as test subjects. Giving rats a high glu-
cose diet will cause them to have hyperglycemia. Then feeding them cortex lycii
liquid and comparing it with the control group without cortex lycii will show the
effects of cortex lycii on blood glucose. Rat’s blood can also be tested using hu-
man glucometer. If rats from the experimental group show lower glucose level
than the control group when both of them consume high glucose diet, then it
will prove Cortex Lycii can stimulate higher insulin production.
This experiment was designed to find an alternative treatment for hypergly-
cemia. The findings from this experiment can be followed up with further stu-
dies on diabetes. Another objective of this study was to observe the effect of high
glucose diet on Rattus norvegicus. Since many researches have found the con-
nection between unhealthy diets with diabetes, this experiment could show cor-
tex lycii having a diabetes prevention effect. Last objective of this study was to
observe if there are side effects of using cortex lycii. Based on other research, this
herb has shown no side effects [1].
2. Materials
Items Subtotal
Large Rat Cages at John Bowne
4 Plastic Large Rat Cages 20 × 16 × 8 High School Agriculture department
$0.00
Rats were provided by John Bowne
8 Rats (Rattus norvegicus)
High School Agriculture department
Provided by John Bowne
Rat Food 50 Lb Mazon: Rat Pallets
$0.00
Provided by John Bowne
Hot Plate
$0.00
Provided by John Bowne
Pot
$0.00
Provided by John Bowne
580 mL Water Bottles
$0.00
Bayer Contour Meter, 50 Contour Test Strips,
Amazon
100 Slight Touch 30 Gauge Lancets,
$40.00
1 Lancing Device, 100 Alcohol Prep Pads.
DOI: 10.4236/jdm.2018.84016 161 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
Continued
Provided by John Bowne
2 Cartel Corn Syrup
$13.00
Supermarket
Domino Sugar
$4.00
Provided by John Bowne
Measuring Cup (1 liter)
$0.00
Provided by John Bowne
Digital Weighing Scale
$0.00
Chinese herbal store
3 Lb of Cortex lycii herb
$24.00
Total cost: $81.00
3. Methodology
3.1. Blood Testing
1) Use alcohol wipes to disinfect the tail of the rat.
2) Use lancet to prick a small visible amount of blood from the rat’s tail.
3) Use test strip to collect the blood sample and wait for the glucometer to give
a reading.
4) Repeat the blood test for all 8 rats.
5) Record down the data for each group of 4 rats.
6) Compare the blood glucose level of Cortex Lycii group with the normal water
group.
7) Repeat for 3 trials.
3.2. Feeding
1) Soak 50 grams of Cortex Lycii in 1 liter of water for 10 minutes, then boil for
30 minutes.
2) After Cortex Lycii liquid cool down to room temperature, it is poured into
580 mL water bottle mixed in with sugar and high fructose corn syrup.
3) For experimental group, the Cortex Lycii bottle is given to 4 Rattus norvegi-
cus along with their 3 pellets/animal of food.
4) For control group, the other 4 Rattus norvegicus are given normal water with
sugar and syrup along with the same food.
5) Wait for 2 days for food consumption.
6) For trial 1 only 25 grams of syrup was given. For trial 2 and 3, 25 gram of sy-
rup and 25 gram of sugar was given.
7) Compare the rise in blood glucose when higher glucose diet was given.
3.3. Literature Review
Currently based on statistics provided by the CDC (National Center for Chronic
Disease Prevention and Health Promotion), more than 30.3 million Americans
have diabetes which is more than 9% of the population [2]. In an experiment
conducted on Diabetes epidemic by Mokdad, Bowman, Ford, Vinicor, Marks
DOI: 10.4236/jdm.2018.84016 162 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
and Koplan, it was explained that diabetes is one of the leading causes of death
in the United States. The two types of diabetes (type 1 and type 2) both can be
treated with insulins [3]. They have similar results on the body, however, type 2
diabetes can be caused by weight gain and physical inactivity [4]. Physical inac-
tivity is defined as not getting recommended level of physical exercises. The
β-cell apoptosis occurs when the body becomes inactive. However, type 1 is
mostly inherited through genetic [5]. Based on a research on type 2 diabetes, the
amount of patients is expected to double by 2030 [6].
The only medical treatment currently available for diabetic patients is insulin
treatment. Due to β-cell not producing enough insulin, injection of insulin is
used as a treatment. Patient can take the insulin injection, when they have high
blood glucose. Insulin is used to combat hyperglycemia [7] [8]. Hyperglycemia is
an abnormal blood glucose level. There are other treatments, however, many of
them have insufficient research to support their effects [9].
Testing the effect of Cortex Lycii on high blood glucose rats could lead to a
new breakthrough in the field of agriculture. Agriculture is the cultivation of
animal and plants to benefit more humans. The result of this experiment could
lead to more production of the herb Cortex Lycii and enhancing diabetic re-
searches. Finding new treatments for hyperglycemia could lead to less people
suffering from the symptoms of diabetes.
Cortex Lycii is an herb that is used in traditional Chinese herbal medicine
formulas [10]. It is not well known in western treatments and little research has
been done on this herb. In the experiment by Chan, Lam, Leung, Che, and Fung
tested a formula labeled SR10 was tested on type 2 diabetic mice. In SR10 one of
the content listed was Cortex Lycii. The results showed it lowered blood glucose
level and the SR10 did not exhibit any toxic effect to the mice. Another experi-
ment conducted by different scientists on diabetic patients with different symp-
toms. The patients were given an herbal treatment with Cortex Lycii included as
part of its content. The result showed some of the symptoms were being relieved
[11]. Further research was done on Cortex Lycii by Ye, Huang, Ni, and Wang
where the scientists compared the effectiveness of aqueous extracts to ethanol
extracts of Cortex Lycii in elevating insulin sensitivity [12]. There is currently no
found research done on the testing Cortex Lycii as a single unit on diabetic pa-
tients. Most research on Cortex Lycii is mixing this herb with many other sub-
stances to view their combined effect. Cortex Lycii has more benefits than just a
treatment for diabetes. Research done by Li, Hu, Huang, Han, and Cheung, con-
cluded that Cortex Lycii extract contained a chemical compound that was effec-
tive in preventing cell damage [13]. In the few other researches, the chemical
compounds of cortex lycii were further broken down [12] [14]. The compound
Kukoamine B found in the herb has antibacterial effects. The compound lyci-
mins A and B was also found to have Anti-ACE effect. ACE is an angiotensin
converting enzyme which raises blood pressure. Lyciminis A and B are types of
ACE inhibitor. ACE inhibitors can reduce heart failures [15].
DOI: 10.4236/jdm.2018.84016 163 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
Diabetes can cause other vascular diseases. Since diabetes cause abnormal
metabolism of triglyceride-rich lipoproteins, diabetic patients have increased
risk of atherosclerosis [16]. Cortex Lycii also has a suppression effect on atheros-
clerosis. Atherosclerosis is a buildup of fat and cholesterol that causes blockage
in blood flow. Cortex Lycii has an effect on slowing blood cell hemolysis and
LDL (low-density lipoprotein) oxidation which can lessen the risk of atheroscle-
rosis [17].
Although research on Cortex Lycii is limited, there has been other research on
testing different substances on diabetes [18]. Tsuneki, Ishizuka, Wu, Sasaoka,
and Kimura conducted a research on green tea effects on diabetic mice. After
letting the diabetic mice ingest green tea, blood glucose levels were tested after 2
- 6 hours. The result shows their blood glucose levels were lowered. Similar tests
could be done on the rats with Cortex Lycii replacement of green tea [19]. There
are other herbs that researchers have tested for diabetes treatments. Panax gin-
seng was tested on type 2 diabetic mice and resulted in enhancing insulin sensi-
tivity. By improving insulin, the blood glucose level was also lowered [20]. In
another experiment Corni Fructus and Lycii Radicis Cortex were combined and
tested on diabetic rats. The results also showed improvement in blood glucose
levels [21]. Codonopsis javanica root is also used in Chinese traditional medi-
cine, and was tested on fructose-fed insulin resistant rats. The finding was that
fructose intake can damage cell function and this herb can significantly improve
the antioxidant enzyme activities [22]. In 2005, an experiment with Mangiferin
on diabetic rats was done. The drugs showed significant effect on lowering
plasma glucose level. This drug is extracted from the plant Mangifera indica
[23]. This means that future research in developing new drugs, plants can also be
part of the research.
Lastly, in order to successfully test blood glucose levels, research on blood
drawing procedures was done. There are few ways to draw small amounts of
bloods from rats. Some locations where blood can be collected are saphenous
vein, dorsal pedal vein, and tail vein [24] However, this research mostly shows
the collection of large amount of blood sample. In a glucose test, the glucometer
only requires 0.5 μl. For minimal stress to the rat drawing blood from the tail is
the most ideal [25]. To increase blood flow rats can be placed in warm water
[26]. Based on IACUC blood sample guidelines, rats should not have more than
2.0 mL of blood drew in 24-hour time period [27]. To keep this experiment con-
stant, only male rats were used. Identifying the sex of the rat was done by look-
ing at the anogenital distance. Male rats have a longer a longer anogenital than
females [28]. Diabetic male rats tend to show increasing blood glucose more
early on than female [14]. Also male rats show early symptom of body weight
and are more susceptible to early symptoms of diabetes [29].
In summary of all these studies conducted on diabetes, the current insulin
treatment is not the only way to treat hyperglycemia. Many herbs that were
tested for their effectiveness against diabetic patients, showed a positive effect.
Cortex Lycii is one of the herbs that showed up several of different studies. This
DOI: 10.4236/jdm.2018.84016 164 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
could mean Cortex Lycii is one of the key factors of lowering blood glucose.
Further experiments and researches should be done on this herb to support or
reject this theory. If it is supported, then a new treatment for diabetes could be
discovered in the near future.
4. Discussion
Trial 1 of the experiment was used to compare the blood glucose of the control
group with the experimental group (Table 1). The rats’ diet included 25 grams
of corn syrup mixed in their water. The control group received 25 grams of corn
syrup with normal water in a 580 mL water bottle. The experimental group re-
ceived 25 grams of corn syrup with Cortex Lycii liquid in 580 mL water bottle.
When the trial ended, the results showed that the control group had a higher
blood glucose level than the experimental group. However, the result didn’t
show enough differences in the blood glucose level. To view the effect of Cortex
Lycii on blood glucose, more significant changes in glucose levels were needed.
Therefore, in trial 2, white sugar was added to both control and experimental
group to increase their glucose intake (Table 2). Within the increase of glucose
in the rats’ diet, the data presents the control group had a significant increase to
their blood glucose levels. Due to the increase of blood glucose in the control
group, the data shows rats in the experimental group had significantly lower
blood glucose levels compared to the control group. With the increase of glucose
intake, only the rats that drank Cortex Lycii showed no significant increase to
their blood glucose levels. To confirm that the data collected from trial 2 was
accurate, trial 3 was conducted with the same variable (Table 3). As shown in
Figure 1, the average differences between experimental group and control group
of trial 2 and 3 are similar. With the same diet of 25 grams of white sugar and 25
grams of corn syrup, both rats’ blood glucose levels from trial 2 and 3 increased
similarly from trial 1. This proves that white sugar can increase blood glucose
levels significantly when added to a diet. Since the data from trial 2 and 3 are
constant, it indicated the trials were run accurately (Figure 2).
Table 1. Trial 1 with 25 grams of syrup mixed into rats’ drinking water.
Control group Experimental group
Rat 1: 143 mg/dL Rat 1: 124 mg/dL
Rat 2: 110 mg/dL Rat 2: 85 mg/dL
Rat 3: 117 mg/dL Rat 3: 113 mg/dL
Rat 4: 127 mg/dL Rat 4: 99 mg/dL
Table 2. Trial 2 with 25 grams of syrup and 25 grams of white sugar in drinking water.
Control group Experimental group
Rat 1: 255 mg/dL Rat 1: 116 mg/dL
Rat 2: 146 mg/dL Rat 2: 103 mg/dL
Rat 3: 143 mg/dL Rat 3: 120 mg/dL
Rat 4: 141 mg/dL Rat 4: 119 mg/dL
DOI: 10.4236/jdm.2018.84016 165 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
Table 3. Trial 3 with 25 grams of syrup and 25 grams of white sugar in drinking water.
Control group Experimental group
Rat 1: 135 mg/dL Rat 1: 103 mg/dL
Rat 2: 144 mg/dL Rat 2: 92 mg/dL
Rat 3: 155 mg/dL Rat 3: 111 mg/dL
Rat 4: 178 mg/dL Rat 4: 114 mg/dL
Figure 1. This graph represents the difference of blood glucose level (mg/dL) over 3
trials.
Figure 2. This graph shows average blood glucose level of both subject groups over the 3
trials.
Research done by Chan, Lam, Leung, Che, and Fung, proved that Cortex Lycii
with other herbs can stimulate insulin production. The experiment done by
them was on type 2 diabetic rats with a dysfunctional pancreas. The data pro-
DOI: 10.4236/jdm.2018.84016 166 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
vided by this research also supports their hypothesis of Cortex Lycii that can
stimulate pancreas β-cells production of insulin. By increasing the production of
insulin, this would cause blood glucose levels to decrease. This experiment was
able to test the effect of Cortex Lycii by testing blood glucose levels. Since type 2
diabetes means the body is not producing enough insulin to keep blood glucose
levels normal, and Cortex Lycii can increase insulin production, then with fur-
ther research Cortex Lycii has the potential for type 2 diabetes treatment. At the
end of the research, no rats from the experimental group showed any signs of
lethargy or intoxicated behaviors. This also supports the experiment done by re-
searchers, Chan, Lam, Leung, Che, and Fung which has discussed Cortex Lycii
does not have any toxic effects [2]. One observation of the 8 rats is the difference
in sizes of the control group compared to the experimental group. The rats that
did not receive the Cortex Lycii and only high glucose diet were significantly
larger in size, close to being obese. This result was similar to the experiment
done by other scientist who showed that Cortex Lycii helps prevent obesity [30].
The rats that received Cortex Lycii and also had the same high glucose diet were
smaller in size and similar to an average rat. Because the nature of this experi-
ment is on blood glucose, no weighing test was done on the rats.
One challenge faced in this experiment is the small sample size. Due to time
limitation, this experiment was only able to test 8 rats per trial over 3 trials.
However, with the trials that were conducted, the data presented was highly
constant and showed a significant difference of blood glucose levels to reach a
conclusion. A minor problem faced in this experiment was the difficulties of
collecting blood sample from the rats. The lancet in the blood glucose kit was
meant for human use, so the needle was not able to prick through the skin of the
rats’ tough tail. After some few failures, the cap of the pen was removed to in-
crease the depth of the lancet. This method of collecting blood was then used for
rest of the trials.
The main purpose in studies of agriculture is to benefit people through the use
of plants and animals. This research can benefit the agriculture field due to the
potential medical advancement on diabetic treatment. Since current treatment
for lack of insulin is to inject body with more insulin, with further research Cor-
tex Lycii could be an alternative treatment due to its ability to stimulate pancreas
to produce its own insulin rather than injecting external hormone. This could be
a potential market for growers to become a part. Growing the Cortex Lycii herb
can increase jobs, as well as profit for farmers and plant producers.
Acknowledgements
The John Bowne agriculture department provided funding and animals for this
experiment. Both authors Hongping Tan and Cristian Vinanzaca were the main
experimenters and did all the actions listed in the procedure. Both authors wrote
in this manuscript and research data. Some assistance was provided by Raj Patel
and Sebastian Wirawan for recording some of data in the glucometer while
DOI: 10.4236/jdm.2018.84016 167 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
blood sample was being collected. Erika Asitimbay and Karen Cruz cleaned the
rat’s cages when time was limited. Chelsea Aviles assisted in boiling Cortex lycii
for the rats. Karla Bunay assisted with restraining the rats while collecting blood
sample from the rats from time to time. Ms. Weinstein assisted by breeding the
amount of rats needed for the project. Ms. Jamiolkowska assisted by purchasing
the materials needed for the project and edited this paper. There is no conflict of
interest in this experiment, as everyone was credited for their attribution. Ms
Jamiolkowska, the instructor of this experiment, will be the guarantor of this
work, as such, had full access to all the data in the study and takes responsibility
for the integrity of the data and the accuracy of the data analysis.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this pa-
per.
References
[1] Chan, J.Y., Lam, F., Leung, P., Che, C. and Fung, K. (2008) Antihyperglycemic and
Antioxidative Effects of a Herbal Formulation of Radix Astragali, Radix Codonopsis
and Cortex Lycii in a Mouse Model of Type 2 Diabetes Mellitus. Phototherapy Re-
search, 23, 658-665. http://onlinelibrary.wiley.com/doi/10.1002/ptr.2694/full
[2] National Diabetes Statistics Report, 2017. (2017)
https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.
pdf
[3] Mokdad, A.H., Bowman, B.A., Ford, E.S., Vinicor, F., Marks, J.S. and Koplan, J.P.
(2001) The Continuing Epidemics of Obesity and Diabetes in the United States.
JAMA, 286, 1195-1200. https://doi.org/10.1001/jama.286.10.1195
[4] Lee, I.M., Shiroma, E.J., Lobelo, F., Puska, P., Blair, S.N., Katzmarzyk, P.T., Lancet
Physical Activity Series Working Group. (2012) Effect of Physical Inactivity on Ma-
jor Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and
Life Expectancy. Lancet, 38, 219-229.
https://www.ncbi.nlm.nih.gov/pubmed/22818936
[5] Tuomi, T. (2005) Type 1 and Type 2 Diabetes.
http://diabetes.diabetesjournals.org/content/54/suppl_2/S40
[6] Vijan, S. (2010) Type 2 Diabetes.
http://annals.org/aim/article-abstract/745650/type-2-diabetes
[7] Garvey, W.T., Olefsky, J.M., Griffin, J., Hamman, R.F. and Kolterman, O.G. (1985)
The Effect of Insulin Treatment on Insulin Secretion and Insulin Action in Type II
Diabetes Mellitus. Diabetes, 34, 222-234.
http://diabetes.diabetesjournals.org/content/34/3/222.short
[8] Kasuga, M. (2006) Insulin Resistance and Pancreatic β Cell Failure. Journal of Clin-
ical Investigation, 116, 1756-1760. https://doi.org/10.1172/JCI29189
[9] Ghorbani, A. (2014) Clinical and Experimental Studies on Polyherbal Formulations
for Diabetes: Current Status and Future Prospective. Journal of Integrative Medi-
cine, 12, 336-345.
http://www.sciencedirect.com/science/article/pii/S2095496414600315?via%3Dihub
[10] Gao, J., Liu, Z.J., Chen, T. and Zhao, D. (2014) Pharmaceutical Properties of Caly-
DOI: 10.4236/jdm.2018.84016 168 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
cosin, the Major Bioactive Isoflavonoid in the Dry Root Extract of Radix astragali.
Pharmaceutical Biology, 52, 1217-1222.
http://www.tandfonline.com/doi/full/10.3109/13880209.2013.879188
[11] Su, K., Zhu, F., Guo, L., Zhu, Y., Li, W. and Xiong, X. (2013) Retrospective Study on
Professor Zhongying Zhou’s Experience in Traditional Chinese Medicine Treat-
ment on Diabetic Nephropathy. Journal of Traditional Chinese Medicine, 33,
262-267.
http://www.sciencedirect.com/science/article/pii/S0254627213601375?via%3Dihub
[12] Yahara, S., Shigeyama, C., Nohara, T., Okuda, H., Wakamatsu, K. and Yasuhara, T.
(1989) Structures of Anti-Ace and -Renin Peptides from Lyciiradicis Cortex. Tetra-
hedron Letters, 30, 6041-6042.
http://www.sciencedirect.com/science/article/pii/S0040403901938493
[13] Li, Y., Hu, S., Huang, Y., Han, Y. and Cheung, H. (2015) Preventing H2O2-Induced
Toxicity in Primary Cerebellar Granule Neurons via Activating the PI3-K/Akt/
GSK3β Pathway by Kukoamine from Lycii Cortex. Journal of Functional Foods, 17,
709-721. http://www.sciencedirect.com/science/article/pii/S1756464615003230#
[14] Liu, X., Zheng, X., Long, Y., Cao, H., Wang, N., Lu, Y., et al. (2011) Dual Targets
Guided Screening and Isolation of Kukoamine B as a Novel Natural Anti-Sepsis
Agent from Traditional Chinese Herb Cortex Lycii. International Immunopharma-
cology, 11, 110-120.
http://www.sciencedirect.com/science/article/pii/S1567576910003449
[15] Yusuf, S., et al. (2000) Effects of an Angiotensin-Converting–Enzyme Inhibitor,
Ramipril, on Cardiovascular Events in High-Risk Patients. New England Journal of
Medicine, 342, 145-153.
[16] Tomkin, G.H. (2010) Atherosclerosis, Diabetes and Lipoproteins. Expert Review of
Cardiovascular Therapy, 8, 1015-1029. https://doi.org/10.1586/erc.10.45
http://www.tandfonline.com/doi/abs/10.1586/erc.10.45
[17] Chan, J.Y., Koon, J.C., Leung, P., Che, C. and Fung, K. (2011) Suppression of
Low-Density Lipoprotein Oxidation, Vascular Smooth Muscle Cell Proliferation
and Migration by a Herbal Extract of Radix astragali, Radix codonopsis and Cortex
lycii. BMC Complementary and Alternative Medicine, 11, 32.
https://bmccomplementalternmed.biomedcentral.com/articles/10.1186/1472-6882-1
1-32
https://doi.org/10.1186/1472-6882-11-32
[18] He, K., Li, X., Chen, X., Ye, X., Huang, J., Jin, Y. and Shu, H. (2011) Evaluation of
Antidiabetic Potential of Selected Traditional Chinese Medicines in STZ-Induced
Diabetic Mice. Journal of Ethnopharmacology, 137, 1135-1142.
http://www.sciencedirect.com/science/article/pii/S0378874111005095?via%3Dihub#
fig0025
https://doi.org/10.1016/j.jep.2011.07.033
[19] Tsuneki, H., Ishizuka, M., Wu, J., Sasaoka, T. and Kimura, I. (2004) Effect of Green
Tea on Blood Glucose Levels and Serum Proteomic Patterns in Diabetic (db/db)
Mice and on Glucose Metabolism in Healthy Humans. BMC Pharmacology, 4, 18.
https://bmcpharma.biomedcentral.com/articles/10.1186/1471-2210-4-18
https://doi.org/10.1186/1471-2210-4-18
[20] Yeo, J., Kang, Y., Cho, S. and Jung, M. (2011) Effects of a Multi-Herbal Extract on
Type 2 Diabetes. Chinese Medicine, 6, 10. https://doi.org/10.1186/1749-8546-6-10
https://cmjournal.biomedcentral.com/articles/10.1186/1749-8546-6-10
[21] Oh, T.W., Kang, S.Y., Kim, K.H., Song, M. and Park, Y. (2013) Anti-Diabetic Effect
DOI: 10.4236/jdm.2018.84016 169 Journal of Diabetes Mellitus
H. P. Tan, C. Vinanzaca
of Medicinal Plants Used for Lower Wasting-Thirst in Streptozotocin-Induced Di-
abetic Rats. The Korea Journal of Herbology, 28, 53-60.
http://koreascience.or.kr/article/ArticleFullRecord.jsp?cn=DHBCBU_2013_v28n5_
53
https://doi.org/10.6116/kjh.2013.28.5.53
[22] Chen, K., Peng, W., Hou, C., Chen, C., Chen, H., Kuo, C. and Korivi, M. (2013)
Codonopsis javanica Root Extracts Attenuate Hyperinsulinemia and Lipid Peroxi-
dation in Fructose-Fed Insulin Resistant Rats. Journal of Food and Drug Analysis,
21, 347-355. http://www.jfda-online.com/article/S1021-9498(13)00048-3/fulltext
https://doi.org/10.1016/j.jfda.2013.08.001
[23] Muruganandan, S., Srinvasan, K., Gupta, S., Gupta, P. and Lal, J. (2005) Effect of
Mangiferin on Hyperglycemia and Atherogenicity in Streptozotocin Diabetic Rats.
Journal of Ethnopharmacology, 97, 497-501.
http://www.sciencedirect.com/science/article/pii/S0378874105000097
https://doi.org/10.1016/j.jep.2004.12.010
[24] Parasuraman, S., Raveendran, R. and Kesavan, R. (2010) Blood Sample Collection in
Small Laboratory Animals. Journal of Pharmacology and Pharmacotherapeutics, 1,
87-93. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3043327/
https://doi.org/10.4103/0976-500X.72350
[25] Lee, G. and Goosens, K.A. (2015) Sampling Blood from the Lateral Tail Vein of the
Rat. Journal of Visualized Experiments, No. 99, Article No. 52766.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4542852/
https://doi.org/10.3791/52766
[26] Stewart, K. and Schroeder, V.A. (2018) Blood Withdrawal I.
https://www.jove.com/science-education/10246/blood-withdrawal-i
[27] Office of Animal Resources Institutional Animal Care and Use Committee (n.d.).
https://animal.research.uiowa.edu/iacuc-guidelines-blood-collection
[28] Quesenberry, K.E., Donnelly, T.M. and Mans, C. (2012) Chapter 22 Biology, Hus-
bandry, and Clinical Techniques of Guinea Pigs and Chinchillas. In: Quesenberry,
K.E. and Carpenter, J.W., Eds., Ferrets, Rabbits, and Rodents: Clinical Medicine and
Surgery, Elsevier, Amsterdam, 279-294.
https://www.sciencedirect.com/science/article/pii/B9781416066217000221
https://doi.org/10.1016/B978-1-4160-6621-7.00022-1
[29] Cortright, R.N., Collins, H.L., Chandler, M.P., Lemon, P.W. and Dicarlo, S.E. (1999)
Diabetes Reduces Growth and Body Composition More in Male than in Female
Rats. Physiology & Behavior, 60, 1233-1238.
http://www.sciencedirect.com/science/article/pii/S0031938496002223
https://doi.org/10.1016/S0031-9384(96)00222-3
[30] Ye, Z., Huang, Q., Ni, H.X. and Wang, D. (2008) Cortex Lycii Radicis Extracts Im-
prove Insulin Resistance and Lipid Metabolism in Obese-Diabetic Rats. Phytothe-
rapy Research, 22, 1665-1670. https://doi.org/10.1002/ptr.2552
http://onlinelibrary.wiley.com/doi/10.1002/ptr.2552/full
DOI: 10.4236/jdm.2018.84016 170 Journal of Diabetes Mellitus
You might also like
- Magic DustDocument29 pagesMagic DustKeyur ShahNo ratings yet
- Obesity - 2012 - Sampey - Cafeteria Diet Is A Robust Model of Human Metabolic Syndrome With Liver and Adipose InflammationDocument10 pagesObesity - 2012 - Sampey - Cafeteria Diet Is A Robust Model of Human Metabolic Syndrome With Liver and Adipose InflammationRodrigoNo ratings yet
- Edr2010 289614Document10 pagesEdr2010 289614FawwaziNo ratings yet
- Original Article Evidence of Anti-Obesity Effects of The Pomegranate Leaf Extract in High-Fat Diet Induced Obese MiceDocument7 pagesOriginal Article Evidence of Anti-Obesity Effects of The Pomegranate Leaf Extract in High-Fat Diet Induced Obese MiceAisy Savira anizarNo ratings yet
- EndocrineDocument203 pagesEndocrineSeli WondaleNo ratings yet
- Diabetes & Metabolism: Hypoglycemic Effect of Kyllinga Triceps in STZ Induced Diabetic RatsDocument3 pagesDiabetes & Metabolism: Hypoglycemic Effect of Kyllinga Triceps in STZ Induced Diabetic RatsSujith KuttanNo ratings yet
- Chavez Et Al - Final PaperDocument9 pagesChavez Et Al - Final PaperJed BellenNo ratings yet
- Increased Hydration Can Be Associated With Weight Loss: Simon N. ThorntonDocument8 pagesIncreased Hydration Can Be Associated With Weight Loss: Simon N. ThorntonS Dian RNo ratings yet
- MIRA KESUMA - Tugas Resume Jurnal - TEBDocument9 pagesMIRA KESUMA - Tugas Resume Jurnal - TEBksm vlogNo ratings yet
- Peperomia Pellucida in Diets Modulates Hyperglyceamia, Oxidative Stress and Dyslipidemia in Diabetic RatsDocument6 pagesPeperomia Pellucida in Diets Modulates Hyperglyceamia, Oxidative Stress and Dyslipidemia in Diabetic RatsMahati UlfahNo ratings yet
- My FinalDocument33 pagesMy FinalBhoj RajNo ratings yet
- ResponseConsensusReportAntipsychoticsMetabolicIssuesLetter CITROME DiabCare2004Document5 pagesResponseConsensusReportAntipsychoticsMetabolicIssuesLetter CITROME DiabCare2004Leslie CitromeNo ratings yet
- In Vivo Sorbus Decora: Original ArticleDocument8 pagesIn Vivo Sorbus Decora: Original ArticleSophea Ananoria MissionaNo ratings yet
- Case Study DM TYPE IIDocument16 pagesCase Study DM TYPE IIrose_avy200975% (4)
- IDDMDocument19 pagesIDDMZam PeaceNo ratings yet
- Coffee and Caffeine Improve Insulin Sensitivity and Glucose Tolerance in C57BL 6J Mice Fed A High Fat DietDocument8 pagesCoffee and Caffeine Improve Insulin Sensitivity and Glucose Tolerance in C57BL 6J Mice Fed A High Fat DietIdaNo ratings yet
- 2022 Anti Dia Be TecDocument15 pages2022 Anti Dia Be TecHilda SarahNo ratings yet
- Diabetes Mellitus Triggers Oxidative Stress in The Liver of Alloxan-Treated Rats: A Mechanism For Diabetic Chronic Liver DiseaseDocument7 pagesDiabetes Mellitus Triggers Oxidative Stress in The Liver of Alloxan-Treated Rats: A Mechanism For Diabetic Chronic Liver DiseaseKarina Winda BessufiNo ratings yet
- Enzyme Technology CHAPLINDocument3 pagesEnzyme Technology CHAPLINSharan GayathrinathanNo ratings yet
- Effect of Ocimum Sanctum (Tulsi) Powder On Hyperlipidemic and Hyperglycemic Male PatientsDocument7 pagesEffect of Ocimum Sanctum (Tulsi) Powder On Hyperlipidemic and Hyperglycemic Male PatientsEditor IJTSRDNo ratings yet
- Indian Medicinal Plants in DiabetesDocument6 pagesIndian Medicinal Plants in DiabetesDr Dushyant Kamal DhariNo ratings yet
- Induction of Diabetes by Streptozotocin in RatsDocument5 pagesInduction of Diabetes by Streptozotocin in RatsJusty GuavaNo ratings yet
- Akbarzadeh 2007 Induksi STZ Diabetic PDFDocument5 pagesAkbarzadeh 2007 Induksi STZ Diabetic PDFPutri MauraNo ratings yet
- Jurnal Fartoks KunyitDocument11 pagesJurnal Fartoks Kunyitrambutan0408No ratings yet
- Badyal, 2003 - Animal Models of Hypertension and Effect of DrugsDocument14 pagesBadyal, 2003 - Animal Models of Hypertension and Effect of DrugsHo Yoke MeiNo ratings yet
- Evaluation of Anti-Diabetic Potentials of Albiza Zygia (DC) Stem Barks in Alloxan-Induced Diabetic RatsDocument8 pagesEvaluation of Anti-Diabetic Potentials of Albiza Zygia (DC) Stem Barks in Alloxan-Induced Diabetic RatsOnyekachi OnyekwereNo ratings yet
- (1479683X - European Journal of Endocrinology) Diet-Induced Weight Loss Alters Hepatic Glucocorticoid Metabolism in Type 2 Diabetes MellitusDocument11 pages(1479683X - European Journal of Endocrinology) Diet-Induced Weight Loss Alters Hepatic Glucocorticoid Metabolism in Type 2 Diabetes MellitusDeltaphierhoNo ratings yet
- RESEARCHDocument19 pagesRESEARCHJeremiah BautistaNo ratings yet
- Jpfarmasigg 160035Document6 pagesJpfarmasigg 160035nikomang ayuNo ratings yet
- Onion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsDocument8 pagesOnion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsRizky Agustian HadiNo ratings yet
- Effect of Honey Bee Venom Apis Mellifera On Hyperglycemia and Hyperlipidemia in Alloxan Induced Diabetic Rabbits 2155 6156.1000507Document4 pagesEffect of Honey Bee Venom Apis Mellifera On Hyperglycemia and Hyperlipidemia in Alloxan Induced Diabetic Rabbits 2155 6156.1000507Solongo GanboldNo ratings yet
- Herbs Against DiabtiesDocument10 pagesHerbs Against DiabtiesSobia NoreenNo ratings yet
- The Genetic Landscape of Diabetes PDFDocument135 pagesThe Genetic Landscape of Diabetes PDFSC NgNo ratings yet
- Antihypertensive Effect of Allicin in Dexamethasone-Induced Hypertensive RatsDocument6 pagesAntihypertensive Effect of Allicin in Dexamethasone-Induced Hypertensive Ratsonetwo35826No ratings yet
- Diabetes ManuscriptDocument26 pagesDiabetes Manuscriptjoseph ikhenobaNo ratings yet
- UNIT-V PharmacologyofDrugsactingonRenalsystem AntidiuerticsDocument10 pagesUNIT-V PharmacologyofDrugsactingonRenalsystem AntidiuerticsMisganaw Abate AbateNo ratings yet
- Original Article Apelin Inhibits Diet-Induced Obesity by Enhancing Lymphatic and Blood Vessel IntegrityDocument46 pagesOriginal Article Apelin Inhibits Diet-Induced Obesity by Enhancing Lymphatic and Blood Vessel IntegrityAnupam BhardwajNo ratings yet
- Research Article: Antidiabetic Activity of Ethanolic Extract of Hyperglycaemic RatsDocument6 pagesResearch Article: Antidiabetic Activity of Ethanolic Extract of Hyperglycaemic RatsUmmu Ghodah ZurrahmiNo ratings yet
- Diabetes Mellitus-Pathophysiology & Herbal Management: Pharmaceutical and Biosciences Journal September 2017Document10 pagesDiabetes Mellitus-Pathophysiology & Herbal Management: Pharmaceutical and Biosciences Journal September 2017Siti AnisaNo ratings yet
- Recent Studies On Phytomedicine Used in Diabetic DisorderDocument14 pagesRecent Studies On Phytomedicine Used in Diabetic DisorderSabrina JonesNo ratings yet
- Sugar - How Much Is Too Much (2011 Fayerman)Document3 pagesSugar - How Much Is Too Much (2011 Fayerman)Hugh Ell - auNo ratings yet
- Biochem Lec Term Paper HypoglycemiaDocument8 pagesBiochem Lec Term Paper Hypoglycemiaapi-318284296No ratings yet
- Effect of Chickpea On GlucoseDocument7 pagesEffect of Chickpea On GlucoseMia DragostinNo ratings yet
- R2Document24 pagesR2Nomer SenadorNo ratings yet
- Annaardium (2016) PDFDocument7 pagesAnnaardium (2016) PDFPutri Mustika PratiwiNo ratings yet
- Pharmacodynamic Study of Jerusalem Artichoke Particles in Type I and II Diabetic Rat ModelsDocument7 pagesPharmacodynamic Study of Jerusalem Artichoke Particles in Type I and II Diabetic Rat ModelsPremier PublishersNo ratings yet
- Allium Cepa, Sani 2016 PDFDocument7 pagesAllium Cepa, Sani 2016 PDFDjati Wulan KusumoNo ratings yet
- Jurnal Ekstrak MethanolicDocument6 pagesJurnal Ekstrak MethanolicMoses FernandoNo ratings yet
- Diabetes Mellitus: The Honeyed Siphon: Past, Present, and FutureDocument7 pagesDiabetes Mellitus: The Honeyed Siphon: Past, Present, and FutureRoderick RichardNo ratings yet
- Antidiabetic and Antihyperlipidemic Effect of Alstonia Scholaris Linn Bark in Streptozotocin Induced Diabetic RatsDocument7 pagesAntidiabetic and Antihyperlipidemic Effect of Alstonia Scholaris Linn Bark in Streptozotocin Induced Diabetic RatsShaik ShoaibNo ratings yet
- Evaluation of Hypolipidemic Activity of Leaf Juice of Catharanthus Roseus (Linn.) G. Donn. in Guinea PigsDocument9 pagesEvaluation of Hypolipidemic Activity of Leaf Juice of Catharanthus Roseus (Linn.) G. Donn. in Guinea PigsyogiapNo ratings yet
- Reinvestigation of Lactose Intolerant Children LacDocument7 pagesReinvestigation of Lactose Intolerant Children Laccool_smartyom28@yahoo.co.inNo ratings yet
- Anderson 2015Document5 pagesAnderson 2015Jhon Fernando NiñoNo ratings yet
- Bartlett 2016Document7 pagesBartlett 2016Camilla Cristina SilvaNo ratings yet
- Vete 4305 - Group 2 Case Study - Cat With DiabetesDocument19 pagesVete 4305 - Group 2 Case Study - Cat With Diabetesapi-242607157No ratings yet
- Antidiabetic Effect of Fermented (Millet) Supplement in Alloxan Induced Hyperglycemic Wistar RatsDocument4 pagesAntidiabetic Effect of Fermented (Millet) Supplement in Alloxan Induced Hyperglycemic Wistar Ratsmaster apotNo ratings yet
- Diabetes AssignmentDocument8 pagesDiabetes AssignmentMildred Obeng AgyeiwaaNo ratings yet
- Jcinvest00248 0177 PDFDocument11 pagesJcinvest00248 0177 PDFluis morales garzaNo ratings yet
- A Systematic Review and Meta-Analysis On Bolton's Ratios: Normal Occlusion and MalocclusionDocument26 pagesA Systematic Review and Meta-Analysis On Bolton's Ratios: Normal Occlusion and MalocclusionSasa AprilaNo ratings yet
- Clinical Manifestation of Oral TuberculosisDocument6 pagesClinical Manifestation of Oral TuberculosisSasa AprilaNo ratings yet
- Anterior RBDocument6 pagesAnterior RBSasa AprilaNo ratings yet
- Type 2 Diabetes Mellitus Disease Diagnosis and Treatment 2155 6156 1000533Document6 pagesType 2 Diabetes Mellitus Disease Diagnosis and Treatment 2155 6156 1000533Sasa AprilaNo ratings yet
- JDM 2018111414202615 PDFDocument8 pagesJDM 2018111414202615 PDFSasa AprilaNo ratings yet
- SK 6 BL 9Document4 pagesSK 6 BL 9Sasa AprilaNo ratings yet
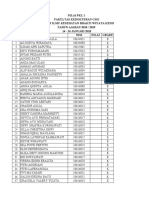
- Nilai PKL 1 Fakultas Kedokteran Gigi Institut Ilmu Kesehatan Bhakti Wiyata Kediri TAHUN AJARAN 2018 / 2019 14 - 26 JANUARI 2018 NO Nama NIM Nilai GradeDocument10 pagesNilai PKL 1 Fakultas Kedokteran Gigi Institut Ilmu Kesehatan Bhakti Wiyata Kediri TAHUN AJARAN 2018 / 2019 14 - 26 JANUARI 2018 NO Nama NIM Nilai GradeSasa AprilaNo ratings yet
- A Case Report of A Tongue Ulcer Presented As The First Sign of Occult TuberculosisDocument5 pagesA Case Report of A Tongue Ulcer Presented As The First Sign of Occult TuberculosisSasa AprilaNo ratings yet
- Erythema Multiforme Major: Case Report and Review of LiteratureDocument6 pagesErythema Multiforme Major: Case Report and Review of LiteratureSasa AprilaNo ratings yet
- Scientific Dental Journal: Pigmented Oral Lichen Planus: A Case ReportDocument6 pagesScientific Dental Journal: Pigmented Oral Lichen Planus: A Case ReportSasa AprilaNo ratings yet
- A Case Report of A Tongue Ulcer Presented As The First Sign of Occult TuberculosisDocument5 pagesA Case Report of A Tongue Ulcer Presented As The First Sign of Occult TuberculosisSasa AprilaNo ratings yet
- Dentistry: A Case of Drug - Induced Xerostomia and A Literature Review of The Management OptionsDocument4 pagesDentistry: A Case of Drug - Induced Xerostomia and A Literature Review of The Management OptionsSasa AprilaNo ratings yet
- Section Odontology: MedicineDocument9 pagesSection Odontology: MedicineSasa AprilaNo ratings yet
- Porphyromonas Gingivalis: An: Overview of Periodontopathic Pathogen Below The Gum LineDocument14 pagesPorphyromonas Gingivalis: An: Overview of Periodontopathic Pathogen Below The Gum LineSasa AprilaNo ratings yet
- 9602 19106 1 SM PDFDocument8 pages9602 19106 1 SM PDFSasa AprilaNo ratings yet
- 19 Musculoskeletal System DR - FallerDocument27 pages19 Musculoskeletal System DR - FallerFranz Earl Niño AlbesaNo ratings yet
- DZ117A-CON - ADA Control SetDocument1 pageDZ117A-CON - ADA Control SetLễ Phan ThịNo ratings yet
- Retinal DetachmentDocument16 pagesRetinal DetachmentCandice Lim Swee LingNo ratings yet
- Medical Terminology For Health Care Professionals A Word Building Approach 9th Edition Rice Test BankDocument33 pagesMedical Terminology For Health Care Professionals A Word Building Approach 9th Edition Rice Test Bankjamesbyrdcxgsaioymf100% (15)
- Disfunctional Vascular Endothelium As A Driver of Atherosclerosis - Emergind Insights Into Pathogenesis and Treatment 2021Document18 pagesDisfunctional Vascular Endothelium As A Driver of Atherosclerosis - Emergind Insights Into Pathogenesis and Treatment 2021Camila VidigalNo ratings yet
- Vaccine: Greg G. WolffDocument5 pagesVaccine: Greg G. WolffRennan Lima M. CastroNo ratings yet
- Definition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDateDocument18 pagesDefinition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDatePaloma GBNo ratings yet
- URI Case (2 Lab Lecture) Patient Presentation: Chief ComplaintDocument2 pagesURI Case (2 Lab Lecture) Patient Presentation: Chief ComplaintMOHANNADNo ratings yet
- Advantages and Disadvantages of Aphakics Correction, Types of Aphakic Correction, Problems of Newly Corrected AphakicsDocument78 pagesAdvantages and Disadvantages of Aphakics Correction, Types of Aphakic Correction, Problems of Newly Corrected AphakicsTika100% (1)
- Equality, Diversity and RightsDocument36 pagesEquality, Diversity and RightsDoodah2100% (5)
- Sample I-Search Paper: Living With AsthmaDocument7 pagesSample I-Search Paper: Living With AsthmaputriNo ratings yet
- The Five Level Model A New Approach To Organizing Body Composition ResearchDocument10 pagesThe Five Level Model A New Approach To Organizing Body Composition ResearchGabriel FagundesNo ratings yet
- Tropical Veterinary Science: Ready Today For TomorrowDocument8 pagesTropical Veterinary Science: Ready Today For TomorrowEsdinawan Carakantara SatrijaNo ratings yet
- Sri Ramachandra University SRMC & Ri Department OF Obstetrics AND Gynaecology List OF Equipments AND Instruments (AS PER Mci)Document6 pagesSri Ramachandra University SRMC & Ri Department OF Obstetrics AND Gynaecology List OF Equipments AND Instruments (AS PER Mci)ValarmathiNo ratings yet
- Guidelines For Ritm Integrated National External Quality Assurance Scheme Neqas - Final2 24 22 PDFDocument8 pagesGuidelines For Ritm Integrated National External Quality Assurance Scheme Neqas - Final2 24 22 PDFAlexa InocNo ratings yet
- Jurnal Case Control UTS (Idrus) 2Document9 pagesJurnal Case Control UTS (Idrus) 2Reny NapitupuluNo ratings yet
- Pressure Ulcer How To Reduce The RiskDocument5 pagesPressure Ulcer How To Reduce The Riskmanu choudharyNo ratings yet
- Inborn Errors of MetabolismDocument12 pagesInborn Errors of Metabolismmichelle octavianiNo ratings yet
- Acute Lymphoblastic Leukemia: Differential DiagnosisDocument6 pagesAcute Lymphoblastic Leukemia: Differential DiagnosisIma OhwNo ratings yet
- Case Based Discussion: Sindy Helda PutriDocument30 pagesCase Based Discussion: Sindy Helda PutriSindyputri HeldaNo ratings yet
- RhabdomyolysisDocument4 pagesRhabdomyolysisEyz PabloNo ratings yet
- Procedure For Eye Irrigation To Treat Ocular Chemical InjuryDocument3 pagesProcedure For Eye Irrigation To Treat Ocular Chemical InjuryDwi Kartika RukmiNo ratings yet
- CB Insights - Digital Health 150 2020Document15 pagesCB Insights - Digital Health 150 2020nikhil karthikeyanNo ratings yet
- Sf8 Nutritional-Stat-Baseline 6 Pearl 2022Document8 pagesSf8 Nutritional-Stat-Baseline 6 Pearl 2022Dante Maligsa BautistaNo ratings yet
- Energy Balance WorksheetDocument3 pagesEnergy Balance Worksheetsara wilsonNo ratings yet
- Motor System ExaminationDocument57 pagesMotor System ExaminationSoma wahidNo ratings yet
- Holy Name University College of Health and Science Department of NursingDocument37 pagesHoly Name University College of Health and Science Department of NursingZarrick AmielNo ratings yet
- MCU PACKAGE PTVI Contractor (Operational Area) SentDocument1 pageMCU PACKAGE PTVI Contractor (Operational Area) Sentmuh.hasbi asbukNo ratings yet
- Basic Training Logbook HKCCCNDocument19 pagesBasic Training Logbook HKCCCNSANTOSH KUMAR BHASKARNo ratings yet
- English Argumentative EssayDocument2 pagesEnglish Argumentative EssayKaren BannaNo ratings yet