Professional Documents
Culture Documents
JDM 2018111414202615 PDF
Uploaded by
Sasa AprilaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JDM 2018111414202615 PDF
Uploaded by
Sasa AprilaCopyright:
Available Formats
Journal of Diabetes Mellitus, 2018, 8, 152-159
http://www.scirp.org/journal/jdm
ISSN Online: 2160-5858
ISSN Print: 2160-5831
Marked Improvement in Glycemic Control
with Exenatide on Addition to Metformin,
Sulfonylurea and Insulin Glargine in Type 2
Diabetes Mellitus, a Real World Experience
Salina Esmail1, Sonal Banzal2, Udaya M. Kabadi2,3*
1
University of Iowa, Iowa City, IA, USA
2
MGM College of Medicine, Indore, India
3
Broadlawns Medical Center, Des Moines, IA, USA
How to cite this paper: Esmail, S., Banzal, S. Abstract
and Kabadi, U.M. (2018) Marked Improve-
ment in Glycemic Control with Exenatide on Background: The major effect of Exenatide is attributed to lowering of
Addition to Metformin, Sulfonylurea and post-prandial glycemia, whereas insulin glargine mainly improves fasting
Insulin Glargine in Type 2 Diabetes Mellitus,
glycemia [FPG]. Objective: Therefore, we assessed effect of Exenatide
a Real World Experience. Journal of Diabetes
Mellitus, 8, 152-159. administration at 6 months and for at 1 year on glycemic control, lipids, body
https://doi.org/10.4236/jdm.2018.84015 weight [BW], daily insulin dose and hypoglycemic events. Methods: Records
of 164 subjects, 126 men and 38 women administered Exenatide between
Received: August 27, 2018
Accepted: November 12, 2018
January 2011 and December 2013 are included in this report. Exenatide was
Published: November 15, 2018 initiated at 5 mcg subcutaneously twice daily [BID] in obese subjects, BMI >
30 kg/m2, with C-peptide > 1 ng/d, and HbA1c 7.5% - 9.5%, while receiving
Copyright © 2018 by authors and
daily metformin 2000 mg, Sulfonylurea Glimepiride 8 mg and insulin Glar-
Scientific Research Publishing Inc.
This work is licensed under the Creative gine [GLAR]. Exclusion criteria were creatinine > 1.5 mg/dL and liver en-
Commons Attribution International zymes > 2.5 times upper limit of normal. Indices of glycemic control include
License (CC BY 4.0). fasting plasma glucose levels and HbA1c. Lipids include serum concentra-
http://creativecommons.org/licenses/by/4.0/
tions of total, LDL and HDL cholesterol. Other endpoints are body weight,
Open Access
daily insulin dose and number of hypoglycemic events per patient during 4
weeks prior to initiation of Exenatide, at 6 months and 1 year of therapy. Re-
sults: In 37 subjects, Exenatide was discontinued within 1 - 3 weeks; 29 due to
onset of nausea and vomiting. Seven of these also complained of abdominal
pain and in these, serum amylase and lipase were elevated indicating presence
of acute pancreatitis. One subject discontinued because of chest pain. Fasting
plasma Glucose remained unchanged following Exenatide administration.
However, HbA1c declined significantly denoting improvement in overall
glycemic control without significant changes in body weight, daily insulin
DOI: 10.4236/jdm.2018.84015 Nov. 15, 2018 152 Journal of Diabetes Mellitus
S. Esmail et al.
dose and hypoglycemic events. Lipid panel improved as well. Conclusion:
Exenatide may be an appropriate adjuvant option in obese subjects with Type
2 diabetes mellitus with lack of desirable glycemic control while receiving
therapy with Metformin, Glimepiride, and insulin Glargine. Moreover, im-
provement in glycemic control is likely to be secondary to lowering of post
prandial hyperglycemia induced by Exenatide.
Keywords
Type 2 Diabetes Mellitus, Glycemic Control, Insulin Glargine, Metformin,
Sulfonylurea, Exenatide
1. Introduction
Exenatide is an incretin mimetic, having glucoregulatory activities similar to
those of naturally occurring mammalian hormone GLP-1 secreted by L cells lin-
ing the ileum and jejunum in response to meal [1] [2] [3]. GLP1 enhances glu-
cose-dependent insulin secretion by beta cells while simultaneously inhibiting
glucagon release by alpha cells both residing in pancreatic islets [2]-[7]. Moreo-
ver, exenatide delays gastric emptying [2]-[7]. Finally, data in animal models as
well as humans indicate that both native GLP1 and GLP1 receptor agonists cause
weight loss by reducing food intake via stimulation of satiety center [8]-[14].
However, Exenatide has a greater potency and a longer duration of action in
comparison to the native GLP-1 when administered subcutaneously [4].
The major effect of Exenatide in improving glycemic control in subjects with
type 2 diabetes is attributed to lowering of post-prandial glucose [PPG] concen-
tration [9]-[17]. Therefore, we examined the effect of administration of Exena-
tide on indices of glycemic control in subjects with type 2 diabetes with desirable
fasting plasma glucose levels, but still elevated HbA1c concentrations while re-
ceiving insulin Glargine, Glimepiride and Metformin.
2. Subjects and Methods
Data was collected retrospectively by examining the records of 164 obese sub-
jects, 126 men and 38 women with type 2 diabetes attending diabetes clinics at 2
academic medical centers during a period of 6 years between January 2011 and
December 2016. The study protocol was approved by Institutional Review
Boards at both medical centers. The major inclusion criterion was the records of
subjects in whom therapy with Exenatide was initiated because of failure in at-
taining desirable HbA1c levels < 7.0% as recommended by American Diabetes
Association [18] despite achieving desirable fasting plasma glucose concentra-
tions, 90 - 130 mg/dl while receiving p maximum daily dose of Glimepiride, 8
mg; Metformin 1000 - 2000 mg as tolerated and insulin Glargine administered
subcutaneously in AM. The other inclusion criteria were obesity with BMI > 30
kg/m2, C-peptide > 1 ng/dl, HbA1c levels ranging between 7.5% - 9.0% at initia-
DOI: 10.4236/jdm.2018.84015 153 Journal of Diabetes Mellitus
S. Esmail et al.
tion and minimum duration of 1 year while receiving combination therapy. This
range of HbA1c was chosen because post prandial glycemia is documented to be
a major contributor to this range of HbA1c levels [19]. Moreover, fasting plasma
glucose in the desirable range of 80 - 130 mg/ dl confirms the contribution of
post prandial hyperglycemia to elevated HbA1c levels in subjects included in this
study. Exclusion criteria were serum creatinine levels > 1.5 mg/dL and liver en-
zymes > 2.5 times upper normal limit.
Adjunctive therapy with Exenatide was elected because the major effect of
Exenatide is well established to lower post prandial hyperglycemia [9]-[17]. Ex-
enatide was administered subcutaneously with initial dose, 5 mcg twice daily
prior to breakfast and supper. The dose was increased to 10 mcg twice daily after
2 - 4 weeks if the initial dose was tolerated without nausea, vomiting, diarrhea or
abdominal pain. Concomitant therapy with same oral agents; metformin, Gli-
mepiride and insulin Glargine was continued for at least one year. The daily
dose of insulin Glargine was adjusted as required on onset of hypoglycemia as
documented by presence of symptoms accompanied by blood glucose level < 60
mg/dl determined by self blood glucose monitoring. Data includes indices of
glycemic control e.g. HbA1c, fasting plasma glucose levels as well as serum con-
centrations of total, LDL and HDL cholesterol, urea nitrogen, creatinine and liv-
er enzymes. Daily insulin dose, body weight and all other parameters were de-
termined prior to initiation of Exenatide and again at 6 months and 1 year.
Number of hypoglycemic events during 4 weeks prior to initiation of Exenatide
and at the end of 1 year of therapy is reported as well. Comparisons between
glycemic and other outcomes prior to initiation of exenatide and at 6 months
and 1 year following the adjunctive therapy were conducted by statistical analys-
es using Student’s “t” test and analysis of variance.
3. Results
Population comprised 164 adult subjects, 126 men and 38 women with ages, 34 -
72 years. Diagnosis of type 2 Diabetes was established by documentation of de-
sirable glycemic control while receiving oral agents for several years as well as
fasting c-peptide concentration > 1 ng/dl. Duration of diabetes ranged between 8
- 20 years. 127 subjects were noted to complete a year of combination therapy
(77%) whereas in 37 subjects (23%), Exenatide was discontinued within 1 - 3
weeks; in 36 subjects because of onset of abdominal pain and/or nausea and/or
vomiting. In 7 of these subjects, further evaluation revealed elevated serum
amylase and lipase levels indicating presence of acute pancreatitis. One subject
discontinued because of chest pain. Thus, Exenatide was withdrawn soon after
initiation because of onset of adverse event.
Fasting plasma glucose concentrations remained between 80 - 130 mg/dl in all
subjects (Table 1). However, HbA1c levels declined in all subjects by 6 months
and lower concentrations were maintained at 1 year (Table 1). Desirable HbA1c
concentration < 7% was attained and maintained in 87% of subjects while re-
maining subjects achieved HbA1c levels below 7.6%.
DOI: 10.4236/jdm.2018.84015 154 Journal of Diabetes Mellitus
S. Esmail et al.
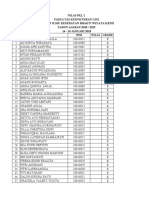
Table 1. Fasting Plasma Glucose (FPG), HbA1c, lipid panel, body weight, daily insulin
dose and hypoglycemic events per patient during 4 weeks prior to initiation (pre Rx) and
again at 6 months and 1 year after (post Rx ) treatment with Exenatide.
PostRx Post Rx
PreRx
6 months 1 year
FPG (mg/dl ) 112 ± 6 105 ± 5 109 ± 8
HbA1c (%) 8.1 ± 0.2 6.7 ± 0.1* 6.8 ± 0.1*
Total Cholesterol (mg/dL) 152 ± 12 129 ± 10 125 ± 9†
Triglycerides (mg/dL) 269 ± 41 205 ± 38 198 ± 36*
HDL (mg/dL) 35 ± 2 38 ± 3 37 ± 3
LDL (mg/dL) 80 ± 16 75 ± 11 81 ± 10
Body weight (kg) 134 ± 7 138 ± 8. 135 ± 9
Insulin (units/day) 101 ± 22 93 ± 19 96 ± 18
Hypo G/patient 2.3 ± 0.4 1.9 ± 0.6 2.1 ± 0.5
*p < 0.01 vs Pre Rx, †p < 0.05 vs Pre Rx.
Serum cholesterol and triglyceride levels declined by 6 months with im-
provement being maintained at 1 year while no significant alterations were do-
cumented in LDL and HDL cholesterol concentrations (Table 1).
Mean body weights prior to initiation of Exenatide and at 6 months and 1 year
following therapy were not significantly different (Table 1). However, the change
in body weight was not consistent with a weight gain 1 - 3 kg noted in 56 sub-
jects and a weight loss of 0.8 - 2.2 kg in the remaining 72 subjects. Finally, mean
daily insulin glargine dose appeared to decline on addition of Exenatide (Table
1). However, daily doses at initiation of Exenatide and at 6 months and 1 year
following treatment were not significantly different (Table 1). Finally, hypogly-
cemic events during last 4 weeks of both phases of treatment, prior to initiation
of Exenatide and at the end of 1 year were not significantly different (p > 0.10).
4. Discussion
This study documented exenatide withdrawal due to onset of established adverse
effects of intolerable abdominal pain, nausea or vomiting in 22.6% of subjects.
Moreover, acute pancreatitis occurred in 7 of 127 subjects. Both these observa-
tions are consistent with previous data in several studies [11]-[17] [20].
This study also demonstrates that in subjects with type 2 diabetes, addition of
exenatide to background therapy consisting of Metformin, Sulfonylurea and
basal insulin glargine leads to marked improvement in glycemic control as ex-
pressed by a significant lowering in HbA1c (Table 1). This finding is consistent
with previous data in the literature including several clinical trials [11]-[17]. Im-
provement in glycemic control with lowering of HbA1c may be attributed to re-
duction in post prandial hyperglycemia since fasting plasma glucose concentra-
tions were unchanged. Moreover, major physiologic effect of exenatide in lo-
wering post prandial glycemia via stimulating insulin secretion and inhibiting
DOI: 10.4236/jdm.2018.84015 155 Journal of Diabetes Mellitus
S. Esmail et al.
glucagon release is well established [2]-[7]. Finally, the role of lowering of post
prandial hyperglycemia in the decline in HbA1c is also consistent with previous
documentation of post prandial glycemia being the major contributor to HbA1c
levels noted in subjects prior to initiation of exenatide in this study [19].
This study documents mixed results in terms of the lipid panel; a significant
reduction in total cholesterol and triglyceride levels with no significant altera-
tions in LDL and HDL cholesterol concentrations. These results are apparently
analogous to two other prospective studies [12] [14], although in contrast to
another study, it documented decline in the HDL levels following treatment with
exenatide [8]. Lowering of total cholesterol and triglyceride levels may be attri-
buted to improvement in glycemic control as previously documented [21] [22]
[23] [24] [25].
In this study, significant change in body weight was not documented in sub-
jects as a group. Insignificant weight gain in some subjects and similar weight
loss in others may have contributed to this finding. However, this observation is
consistent with the data regarding body weight in the original pre-marketing
clinical trial [12]. In this trial, marked weight loss documented in subjects con-
tinuing exenatide despite experiencing adverse side effects may have contributed
to significant decline in mean body weight as minimal change in body weight
was evident in other subjects tolerating the drug. Similar significant weight loss
was noted in subjects using exenatide in another study [11]. However, data
lacked detailed information regarding body weights in individual subjects. The
differences in changes in body weights observed in some other studies as well
[12] [13] [14] [15]. This inconsistent findings regarding changes in body weights
may be attributed to the different times during the day at which exenatide was
administered coupled with various other factors, such as lack of exercise or se-
dentary lifestyle. Another potential reason for lack of significant changes in body
weight in subjects in this study is the lack of requirement of bed time snack due
to almost negligible onset of nocturnal hypoglycemia secondary to administra-
tion of insulin Glargine U100 or insulin Glargine U300 in AM as opposed to
bedtime documented in previous studies [26] [27] [28] [29]. Weight gain no-
ticed in subjects receiving insulin glargine at bedtime may be due to a consump-
tion of a snack following insulin administration because of the concern of noc-
turnal hypoglycemia on part of both patients and providers alike especially be-
cause of a fairly large dose required by most obese subjects with type 2 Diabetes.
Finally, lower daily insulin dose on addition of exenatide noted in this and other
studies may contribute to lack of weight gain as well [11]-[17].
In final analysis, in patients with type 2 DM with poorly controlled glycemic
levels while receiving combination treatment with insulin glargine, metformin
and Glimepiride , addition of exenatide induced a marked reduction in HbA1c,
serum cholesterol and triglyceride levels. Moreover, this improvement occurred
without both the weight gain and a significant rise in hypoglycemia, a distinct
advantage over administration of rapid acting insulin to lower post prandial
hyperglycemia. Therefore, addition of exenatide or another GLP 1 receptor
DOI: 10.4236/jdm.2018.84015 156 Journal of Diabetes Mellitus
S. Esmail et al.
agonist may be preferred to use of rapid acting insulin in subjects with type 2
diabetes with lapse of glycemic control while receiving metformin, Glimepiride
and basal insulin Glargine.
However, this study has several limitations including retrospective observa-
tional nature, lack of comparisons with either placebo or other oral agents e.g.
DPP4 inhibitors or injectable rapid acting insulin, well established strategies for
lowering postprandial hyperglycemia. However, the findings are important since
use of ezenatide or other GLP1 receptor agonist may be preferential to rapid
acting insulin, especially in obese subjects with diabetes because of their benefi-
cial effect on body weight and hypoglycemia. This beneficial effect in terms of
hypoglycemia is distinctly crucial in elderly because of frequent presence of hy-
poglycemia unawareness rendering onset of hypoglycemia detrimental to well
being resulting in a seizure, a stroke, acute coronary event, arrhythmia and even
death.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this pa-
per.
References
[1] Chen, Y.E. and Drucker, D. (1997) Tissue-Specific Expression of Unique mRNAs
that Encode Pro-Glucagon-Derived Peptides or Exendin-4 in the Lizard. The Jour-
nal of Biological Chemistry, 272, 4108-4115.
[2] Drucker, D.J. (1998) Glucagon-Like Peptides. Diabetes, 47, 159-169.
https://doi.org/10.2337/diab.47.2.159
[3] Young, A.A., Gedulin, B.R., Bhavsar, S., Bodkin, N., Jodka, C., Hansen, B. and De-
naro, M. (1999) Glucose-Lowering and Insulin-Sensitizing Actions of Exendin-4:
Studies in Obese Diabetic (ob/ob, dbh/db) Mice, Diabetic Fatty Zucker Rats, and
Diabetic Rhesus Monkeys (Macaca mulatta). Diabetes, 48, 1026-1034.
https://doi.org/10.2337/diabetes.48.5.1026
[4] Parkes, D.G., Pittner, R., Jodka, C., Smith, P. and Young, A. (2001) Insulinotropic
Actions of Exendin-4 and Glucagon-Like Peptide-1 in Vivo and in Vitro. Metabol-
ism, 50, 583–589. https://doi.org/10.1053/meta.2001.22519
[5] Nielsen, L.L. and Baron, A.D. (2003) Pharmacology of Exenatide (Synthetic Exen-
din-4) for the Treatment of Type 2 Diabetes. Current Opinion in Investigational
Drugs, 4, 401-405.
[6] Nielsen, L.L., Young, A.A. and Parkes, D. (2004) Pharmacology of Exenatide (Syn-
thetic Exendin-4): A Potential Therapeutic for Improved Glycemic Control of Type
Diabetes. Regulatory Peptides, 117, 77-88.
https://doi.org/10.1016/j.regpep.2003.10.028
[7] Bunck, M.C., Diamant, M., Cornér, A., Eliasson, B., Malloy, J.L., Shaginian, R.M.,
Deng, W. and Kendall, D.M. (2009) One-Year Treatment With Exenatide Improves
β-Cell Function, Compared with Insulin Glargine, in Metformin-Treated Type 2
Diabetic Patients. Diabetes Care, 32, 762-768. https://doi.org/10.2337/dc08-1797
[8] Szayna, M., Doyle, M.E., Betkey, J.A., Holloway, H.W., Spencer, R.G.S., Greig, N.H.
and Egan, J.M. (2000) Exendin-4 Decelerates Food Intake, Weight Gain, and Fat
DOI: 10.4236/jdm.2018.84015 157 Journal of Diabetes Mellitus
S. Esmail et al.
Deposition in Zucker Rats. Endocrinology, 141, 1936-1941.
https://doi.org/10.1210/endo.141.6.7490
[9] Edwards, C.M., Stanley, S.A., Davis, R., Brynes, A.E., Frost, G.S., Seal, L.J., Ghatei,
M.A. and Bloom, S.R. (2001) Exendin-4 Reduces Fasting and Postprandial Glucose
and Decreases Energy Intake in Healthy Volunteers. American Journal of Physiolo-
gy-Endocrinology and Metabolism, 281, E155-E161.
https://doi.org/10.1152/ajpendo.2001.281.1.E155
[10] Poon, T., Nelson, P., Shen, L., Mihm, M., Taylor, K., Fineman, M. and Kim, D.
(2005) Exenatide Improves Glycemic Control and Reduces Body Weight in Subjects
with Type 2 Diabetes: A Dose-Ranging Study. Diabetes Technology & Therapeutics,
7, 467-477.
[11] DeFronzo, R.A., Ratner, R.E., Han, J., Kim, D.D., Fineman, M.S. and Baron, A.D.
(2005) Effects of Exenatide (Exendin-4) on Glycemic Control and Weight over 30
Weeks in Metformin-Treated Patients with Type 2 Diabetes. Diabetes Care, 28,
1092-1100. https://doi.org/10.2337/diacare.28.5.1092
[12] Blonde, L., Klein, E.J., Han, J., Zhang, B., Mac, S.M., Poon, T.H., Taylor, K.L.,
Trautmann, M.E., Kim, D.D. and Kendall, D.M. (2006) Interim Analysis of the Ef-
fects of Exenatide Treatment on A1C, Weight and Cardiovascular Risk Factors over
82 Weeks in 314 Overweight Patients with Type 2 Diabetes. Diabetes, Obesity and
Metabolism, 8, 436–447. https://doi.org/10.1111/j.1463-1326.2006.00602.x
[13] Ratner, R.E., Maggs, D., Nielsen, L.L., Stonehouse, A.H., Poon, T., Zhang, B., Bic-
sak, T.A., Brodows, R.G. and Kim, D.D. (2006) Long-Term Effects of Exenatide
Therapy over 82 Weeks on Glycaemic Control and Weight in Over-Weight Met-
formin-Treated Patients with Type 2 Diabetes Mellitus. Diabetes, Obesity and Me-
tabolism, 8, 419-428. https://doi.org/10.1111/j.1463-1326.2006.00589.x
[14] Klonoff David, C., Buse John, B., Nielsen Loretta, L., Guan, X.S., Bowlus
Christopher, L., Holcombe, J.H., Wintle Matthew, E. and Maggs, D.G. (2008) Ex-
enatide Effects on Diabetes, Obesity, Cardiovascular Risk Factors and Hepatic Bio-
markers in Patients with Type 2 Diabetes Treated for at Least 3 Years, Current
Medical Research and Opinion, 24, 275-286.
https://doi.org/10.1185/030079908X253870
[15] Kolterman, O.G., Buse, J.B., Fineman, M.S., Gaines, E., Heintz, S., Bicsak, T.A.,
Taylor, K., Kim, D., Aisporna, M., Wang, Y. and Baron, A.D. (2003) Synthetic Ex-
endin-4 (Exenatide) Significantly Reduces Postprandial and Fasting Plasma Glucose
in Subjects with Type 2 Diabetes. The Journal of Clinical Endocrinology & Meta-
bolism, 88, 3082-3089. https://doi.org/10.1210/jc.2002-021545
[16] Buse, J.B., Henry, R.R., Han, J., Kim, D.D., Fineman, M.S. and Baron, A.D., Exena-
tide-113 Clinical Study Group (2004) Effects of Exenatide (Exendin-4) on Glycemic
Control over 30 Weeks in Sulfonylurea-Treated Patients with Type 2 Diabetes. Di-
abetes Care, 27, 2628-2635. https://doi.org/10.2337/diacare.27.11.2628
[17] John, L.E., Kane, M.P., Busch, R.S. and Hamilton, R.A. (2007) Expanded Use of
Exenatide in the Management of Type 2 Diabetes. Diabetes Spectrum, 20, 59-63.
https://doi.org/10.2337/diaspect.20.1.59
[18] American Diabetes Association (2018) Glycemic Targets: Standards of Medical Care
in Diabetes. Diabetes Care, 43, S55-S64.
[19] Louis, L.M., Lapinski, H. and Claude, C. (2003) Contributions of Fasting and Post-
prandial Plasma Glucose Increments to the Overall Diurnal Hyperglycemia of Type
2 Diabetic Patients. Diabetes Care, 26, 881-885.
https://doi.org/10.2337/diacare.26.3.881
DOI: 10.4236/jdm.2018.84015 158 Journal of Diabetes Mellitus
S. Esmail et al.
[20] Sonal, B. and Udaya, K. (2017) Eleavated Pancreatic Enzymes and Acute Pancreati-
tis in Subjects with Type 2 Diabetes Treated with Exenatide. Advanced Research in
Gastroenterology and Hepatology, 1, 1-4.
[21] Kabadi, U.M. and Kabadi, M.U. (2001) Improvement in Lipids with Glimepiride in
Type 2 Diabetes Mellitus. Diabetes Research, 35, 155.
[22] Kabadi, U.M. (2004) Weight Gain, Improvement in Metabolic Profiles and Immu-
nogenicity with Insulin or Sulfonylurea Administration in AIDS. Clinical Drug In-
vestigation, 24, 287-294. https://doi.org/10.2165/00044011-200424050-00005
[23] Kabadi, U.M. (2006) Comparative Efficacy of Glimepiride and/or Metformin with
Insulin in Type 2 Diabetes. Diabetes Research & Clinical Practice, 72, 265-270.
https://doi.org/10.1016/j.diabres.2005.10.024
[24] Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein, H.C.,
Miller, M.E., Byington, R.P., Goff Jr., D.C., Bigger, J.T., Buse, J.B., Cushman, W.C.,
Genuth, S., Ismail-Beigi, F., Grimm Jr., R.H., Probstfield, J.L., Simons-Morton, D.G.
and Friedewald, W.T. (2008) Effects of Intensive Glucose Lowering in Type 2 Di-
abetes. The New England Journal of Medicine, 358, 2545-2559.
[25] Esmail, R. and Kabadi U.M. (2016) Improvement in Cardiovascular Risk Markers
with Glimepiride in Non Obese Subjects with Pre Diabetes: Similar to Obese Cohort
Treated with Metformin. British Journal of Medicine & Medical Research, 18, 1-6.
[26] Fritsche, A., Schweitzer, M.A., Häring, H.U., 4001 Study Group (2003) Glimepiride
Combined with Morning Insulin Glargine, Bedtime Neutral Protamine Hagedorn
Insulin, or Bedtime Insulin Glargine in Patients with Type 2 Diabetes: A Rando-
mized, Controlled Trial. Annals of Internal Medicine, 138, 952-959.
https://doi.org/10.7326/0003-4819-138-12-200306170-00006
[27] Standl, E., Maxeiner, S., Raptis, S., Karimi-Anderesi, Z., Schweitzer, M.A.,
HOE901/4009 Study Group (2005) Good Glycemic Control with Flexibility in
Timing of Basal Insulin Supply: A 24-Week Comparison of Insulin Glargine Given
Once Daily in the Morning or at Bedtime in Combination with Morning Glimepi-
ride. Diabetes Care, 28, 419-420. https://doi.org/10.2337/diacare.28.2.419
[28] Kabadi, U.M. (2016) Better Glycemic Control with Lesser Hypoglycemia on Transi-
tion of Insulin Glargine Administration at Bedtime to Morning in Type 2 Diabetes
Mellitus. Diabetes Research and Metabolism, 1, 1-7.
[29] Hampton, N., Exley, S., Robbins, S. and Kabadi, U.M. (2018) Lower Daily Dose with
Better Outcomes with Oral Agents and AM Insulin Toujeo Administration than
Lantus While Attaining Desirable Glycemic Control in Type 2 Diabetes. European
Journal of Pharmaceutical and Medical Research, 5, 555-563.
DOI: 10.4236/jdm.2018.84015 159 Journal of Diabetes Mellitus
You might also like
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- The Effect of Glimepiride On Glycemic Control and Fasting Insulin LevelsDocument3 pagesThe Effect of Glimepiride On Glycemic Control and Fasting Insulin Levelszahrosofi ahmadahNo ratings yet
- Eficiencia y Tolerabilidad Glimepirida y MetfomrinaDocument7 pagesEficiencia y Tolerabilidad Glimepirida y MetfomrinaMarioA.VelascoCórdobaNo ratings yet
- Mitigating Effects of Vildagliptin in Experimental Diabetes With Metabolic SyndromeDocument9 pagesMitigating Effects of Vildagliptin in Experimental Diabetes With Metabolic Syndromerajesh sumanNo ratings yet
- Sitagliptin vs. Pioglitazone As Add-On Treatments in Patients With Uncontrolled Type 2 Diabetes On The Maximal Dose of Metformin Plus SulfonylureaDocument9 pagesSitagliptin vs. Pioglitazone As Add-On Treatments in Patients With Uncontrolled Type 2 Diabetes On The Maximal Dose of Metformin Plus SulfonylureaFebi FernandaNo ratings yet
- Saxagliptin and Metformin in Fixed Combination For The Treatment of Type 2 Diabetes in AdultsDocument11 pagesSaxagliptin and Metformin in Fixed Combination For The Treatment of Type 2 Diabetes in AdultsLaura MelatiNo ratings yet
- s13300-020-00981-0Document15 pagess13300-020-00981-0Lilian Aracely Gaspar caceresNo ratings yet
- Tirzepatide Versus Semaglutide Once Weekly in Patients With Type 2 DiabetesDocument13 pagesTirzepatide Versus Semaglutide Once Weekly in Patients With Type 2 Diabetesmanish chaudharyNo ratings yet
- Incretin Mimetics and Dipeptidyl Peptidase-4 Inhibitors: Innovative Treatment Therapies For Type 2 DiabetesDocument11 pagesIncretin Mimetics and Dipeptidyl Peptidase-4 Inhibitors: Innovative Treatment Therapies For Type 2 DiabetesRidha Surya NugrahaNo ratings yet
- VildagliptinDocument7 pagesVildagliptinwanburyNo ratings yet
- Co-Formulations As The First Injectable in Type 2 Diabetes A Review of Efficacy, Safety, and Implications in Clinical PracticeDocument13 pagesCo-Formulations As The First Injectable in Type 2 Diabetes A Review of Efficacy, Safety, and Implications in Clinical PracticeRIKANo ratings yet
- Ajhp 140168Document12 pagesAjhp 140168cherrygems99No ratings yet
- Joi 160014Document10 pagesJoi 160014Rush32No ratings yet
- Comparison of Vildagliptin-Metformin and Glimepiride-Metformin Treatments in Type 2 Diabetic PatientsDocument7 pagesComparison of Vildagliptin-Metformin and Glimepiride-Metformin Treatments in Type 2 Diabetic PatientsGregory VeintimillaNo ratings yet
- Skugor TreatmentofdiabetesmellitusDocument5 pagesSkugor TreatmentofdiabetesmellitusyomiboyNo ratings yet
- Dipeptidyl Peptidase IV (DPP IV) : A Novel Emerging Target For The Treatment of Type 2 DiabetesDocument8 pagesDipeptidyl Peptidase IV (DPP IV) : A Novel Emerging Target For The Treatment of Type 2 DiabetesGREESTYNo ratings yet
- BIOS LIFE - Diabetes in Control Study #1 by Steven Freed and David JoffeDocument1 pageBIOS LIFE - Diabetes in Control Study #1 by Steven Freed and David JoffeHisWellnessNo ratings yet
- Appropriate Timing of Glimepiride Administration in Patients With Type 2 Diabetes MillitusDocument5 pagesAppropriate Timing of Glimepiride Administration in Patients With Type 2 Diabetes MillitusMilie RadcliffeNo ratings yet
- Tan, 2022Document8 pagesTan, 2022Mirilláiny AnacletoNo ratings yet
- New Practice in Semaglutide On Type-2 Diabetes and Obesity: Clinical Evidence and ExpectationDocument8 pagesNew Practice in Semaglutide On Type-2 Diabetes and Obesity: Clinical Evidence and ExpectationBoris ThielmannNo ratings yet
- Alogliptin - A Review of Its Use in Patients With Type 2 Diabetes MellitusDocument20 pagesAlogliptin - A Review of Its Use in Patients With Type 2 Diabetes Mellitus13201940No ratings yet
- Semaglutide Added To Basal Insulin in Type 2 Diabetes (SUSTAIN 5) : A Randomized, Controlled TrialDocument11 pagesSemaglutide Added To Basal Insulin in Type 2 Diabetes (SUSTAIN 5) : A Randomized, Controlled TrialIvan Dario Hernandez ErazoNo ratings yet
- Effects of growth hormone treatment on obese NIDDM patientsDocument1 pageEffects of growth hormone treatment on obese NIDDM patientsamritaryaaligarghNo ratings yet
- Pharmacologic Approaches To Glycemic Treatment Standards of Medical Care in Diabetes-2018Document13 pagesPharmacologic Approaches To Glycemic Treatment Standards of Medical Care in Diabetes-2018ferrossanchezNo ratings yet
- Clinical Efficacy Evaluation and Longterm Prognosis of Glucagonlike Peptide1 Combined With Sodium Glucose CotransportersDocument9 pagesClinical Efficacy Evaluation and Longterm Prognosis of Glucagonlike Peptide1 Combined With Sodium Glucose CotransportersvinayNo ratings yet
- Semaglutide 1.0 mg More Effective for Glycemic Control & Weight Loss Than Liraglutide 1.2 mgDocument10 pagesSemaglutide 1.0 mg More Effective for Glycemic Control & Weight Loss Than Liraglutide 1.2 mgIvan Dario Hernandez ErazoNo ratings yet
- NauckDocument8 pagesNauckIqaNo ratings yet
- Administration of Resveratrol For 5 WK Has No Effect On Glucagon-Like Peptide 1 Secretion, Gastric Emptying, or Glycemic Control in Type 2 Diabetes: A Randomized Controlled TrialDocument5 pagesAdministration of Resveratrol For 5 WK Has No Effect On Glucagon-Like Peptide 1 Secretion, Gastric Emptying, or Glycemic Control in Type 2 Diabetes: A Randomized Controlled TrialAmanda TeacaNo ratings yet
- Gliclazide Metformin Study Type 2 Diabetes PatientsDocument7 pagesGliclazide Metformin Study Type 2 Diabetes PatientsLyka MahrNo ratings yet
- Original Paper: World Nutrition JournalDocument9 pagesOriginal Paper: World Nutrition JournalcutthaNo ratings yet
- Comparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic PatientsDocument6 pagesComparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic Patientsthomas albertNo ratings yet
- The Effects of Licogliflozin, A Dual SGLT12 Inhibitor, On BodyDocument11 pagesThe Effects of Licogliflozin, A Dual SGLT12 Inhibitor, On BodyJose Mario HoyosNo ratings yet
- Efficacy and Safety of Biosimilar Glargine-IMGDocument8 pagesEfficacy and Safety of Biosimilar Glargine-IMGSiddiq MohammedNo ratings yet
- Reducing Hba1C in Type 2 Diabetes Using Digital Twin Technology-Enabled Precision Nutrition: A Retrospective AnalysisDocument12 pagesReducing Hba1C in Type 2 Diabetes Using Digital Twin Technology-Enabled Precision Nutrition: A Retrospective Analysisa hNo ratings yet
- Emerging Treatments Improve Diabetes ControlDocument10 pagesEmerging Treatments Improve Diabetes ControlAyman AleemNo ratings yet
- JDM20120200002 37731682Document5 pagesJDM20120200002 37731682Raissa Andi SoekrisnoNo ratings yet
- Efficacy and Safety Comparison of Liraglutide, Glimepiride, and Placebo, All in Combination With Metformin, in Type 2 DiabetesDocument7 pagesEfficacy and Safety Comparison of Liraglutide, Glimepiride, and Placebo, All in Combination With Metformin, in Type 2 DiabetesOzi ThingkingandactionNo ratings yet
- Diabetes MellitusDocument31 pagesDiabetes MellitusElenaCondratscribdNo ratings yet
- Efficacy of Vildagliptin and Metformin Combination in Type II Diabetes Mellitus PatientsDocument4 pagesEfficacy of Vildagliptin and Metformin Combination in Type II Diabetes Mellitus PatientsDR.P.KALAI SELVINo ratings yet
- Semaglutida DiarioDocument12 pagesSemaglutida Diariomelousa23No ratings yet
- Ajcpath112 0665Document10 pagesAjcpath112 0665RiyanNo ratings yet
- JOURNAL CLUB Presentation: Presented by Phatcharaporn Dangtongdee 583150152-4 Section 3Document21 pagesJOURNAL CLUB Presentation: Presented by Phatcharaporn Dangtongdee 583150152-4 Section 3Phatcharaporn DangtongdeeNo ratings yet
- Effect of A High-Protein, Low-Carbohydrate Diet On Blood Glucose Control in People With Type 2 DiabetesDocument8 pagesEffect of A High-Protein, Low-Carbohydrate Diet On Blood Glucose Control in People With Type 2 DiabetesFajar AgNo ratings yet
- Scheen 2010Document10 pagesScheen 2010Lyka MahrNo ratings yet
- 306 1164 1 PB PDFDocument6 pages306 1164 1 PB PDFDini RizkyNo ratings yet
- Insulin Therapy Patterns in Type 2 Diabetes PatientsTITLE Study of Insulin Use in Type 2 Diabetes at Negara Hospital TITLE Analysis of Insulin Regimens for Type 2 Diabetes OutpatientsDocument6 pagesInsulin Therapy Patterns in Type 2 Diabetes PatientsTITLE Study of Insulin Use in Type 2 Diabetes at Negara Hospital TITLE Analysis of Insulin Regimens for Type 2 Diabetes Outpatientssafdara tikaNo ratings yet
- Recent Advances in Incretin-Based Pharmacotherapies For The Treatment of Obesity and DiabetesDocument3 pagesRecent Advances in Incretin-Based Pharmacotherapies For The Treatment of Obesity and DiabetesAndrés ChávezNo ratings yet
- (20493614 - Endocrine Connections) Incretin-Based Therapies For Patients With Type 1 Diabetes - A Meta-AnalysisDocument12 pages(20493614 - Endocrine Connections) Incretin-Based Therapies For Patients With Type 1 Diabetes - A Meta-AnalysisIntan OktapiaNo ratings yet
- Smith 2011Document7 pagesSmith 2011sari putriNo ratings yet
- DapaglifozinDocument21 pagesDapaglifozinChiyaanVikramNo ratings yet
- Nutrition in DMDocument33 pagesNutrition in DMkero R.habibNo ratings yet
- Insulin Therapy Diabetes Mellitus: Divisi Pendidikan PeridaDocument23 pagesInsulin Therapy Diabetes Mellitus: Divisi Pendidikan PeridaElisabethHutajuluNo ratings yet
- 2 Modern Sulfonylureas - A Balanced Perspective - 15!09!2022Document30 pages2 Modern Sulfonylureas - A Balanced Perspective - 15!09!2022Lalrin ChhanaNo ratings yet
- Bo Ahr En, Susan L. Johnson, Murray Stewart, Deborah T. Cirkel, Fred Yang, Caroline Perry, and Mark N. Feinglos, For The HARMONY 3 Study GroupDocument8 pagesBo Ahr En, Susan L. Johnson, Murray Stewart, Deborah T. Cirkel, Fred Yang, Caroline Perry, and Mark N. Feinglos, For The HARMONY 3 Study GroupTari SehatiNo ratings yet
- HbA1c As A Screening Tool For Type 2 DiabetesDocument22 pagesHbA1c As A Screening Tool For Type 2 DiabetesJay RubyNo ratings yet
- Incretin PharmDocument3 pagesIncretin PharmSlim SaaryNo ratings yet
- PMC4020327-jdi 12214Document11 pagesPMC4020327-jdi 12214anca irinaNo ratings yet
- Effect of The GLP-1 Receptor Agonist Lixisenatide On Counter-Regulatory Responses To Hypoglycemia in Subjects With Insulin-Treated Type 2 DiabetesDocument8 pagesEffect of The GLP-1 Receptor Agonist Lixisenatide On Counter-Regulatory Responses To Hypoglycemia in Subjects With Insulin-Treated Type 2 DiabetestarietarooNo ratings yet
- Role of Voglibose in Managing Post-Meal Blood Sugar SpikesDocument5 pagesRole of Voglibose in Managing Post-Meal Blood Sugar SpikesNimesh ModiNo ratings yet
- Improving Glucagon-Like Peptide-1 Dynamics in Patients With Type 2 Diabetes MellitusDocument5 pagesImproving Glucagon-Like Peptide-1 Dynamics in Patients With Type 2 Diabetes MellitusscribdNo ratings yet
- Radiopaque Periapical Lesion VariancesDocument6 pagesRadiopaque Periapical Lesion VariancesSasa AprilaNo ratings yet
- S7bamgx79xjgvxnzusoeav94b@2020 - 12 - 25.json 2Document1 pageS7bamgx79xjgvxnzusoeav94b@2020 - 12 - 25.json 2Sasa AprilaNo ratings yet
- Diabetes Mellitus: The Epidemic of The Century: Akram T Kharroubi, Hisham M DarwishDocument19 pagesDiabetes Mellitus: The Epidemic of The Century: Akram T Kharroubi, Hisham M DarwishAna Cristine Silva Pires TomeNo ratings yet
- A Systematic Review and Meta-Analysis On Bolton's Ratios: Normal Occlusion and MalocclusionDocument26 pagesA Systematic Review and Meta-Analysis On Bolton's Ratios: Normal Occlusion and MalocclusionSasa AprilaNo ratings yet
- Business Continuity: The Ultimate Guide ToDocument35 pagesBusiness Continuity: The Ultimate Guide ToKhairul Nazmi Zainol AriffinNo ratings yet
- Clinical Manifestation of Oral TuberculosisDocument6 pagesClinical Manifestation of Oral TuberculosisSasa AprilaNo ratings yet
- Type 2 Diabetes Mellitus Disease Diagnosis and Treatment 2155 6156 1000533Document6 pagesType 2 Diabetes Mellitus Disease Diagnosis and Treatment 2155 6156 1000533Sasa AprilaNo ratings yet
- JDM 2018111414202615 PDFDocument8 pagesJDM 2018111414202615 PDFSasa AprilaNo ratings yet
- Diabetes Mellitus A Devastating Metabolic DisorderDocument5 pagesDiabetes Mellitus A Devastating Metabolic DisorderDaniela Mădălina GhețuNo ratings yet
- Definition Classification and Diagnosis of Diabetes Prediabetes and Metabolic SyndromeDocument6 pagesDefinition Classification and Diagnosis of Diabetes Prediabetes and Metabolic SyndromeJianhua ShiNo ratings yet
- Definition Classification and Diagnosis of Diabetes Prediabetes and Metabolic SyndromeDocument6 pagesDefinition Classification and Diagnosis of Diabetes Prediabetes and Metabolic SyndromeJianhua ShiNo ratings yet
- BJSTR MS Id 001574 PDFDocument4 pagesBJSTR MS Id 001574 PDFSasa AprilaNo ratings yet
- Medoralv22 I5 p586Document9 pagesMedoralv22 I5 p586DivaNo ratings yet
- The Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose DietDocument11 pagesThe Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose DietSasa AprilaNo ratings yet
- The Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose DietDocument11 pagesThe Effect of Cortex Lycii On Rattus Norvegicus' Blood Glucose Level Using A High Glucose DietSasa AprilaNo ratings yet
- Classification Pathophysiology Diagnosis and Management of Diabetesmellitus 2155 6156 1000541Document9 pagesClassification Pathophysiology Diagnosis and Management of Diabetesmellitus 2155 6156 1000541AldaniaNo ratings yet
- BJSTR MS Id 001574 PDFDocument4 pagesBJSTR MS Id 001574 PDFSasa AprilaNo ratings yet
- Nilai PKL 1 Fakultas Kedokteran Gigi Institut Ilmu Kesehatan Bhakti Wiyata Kediri TAHUN AJARAN 2018 / 2019 14 - 26 JANUARI 2018 NO Nama NIM Nilai GradeDocument10 pagesNilai PKL 1 Fakultas Kedokteran Gigi Institut Ilmu Kesehatan Bhakti Wiyata Kediri TAHUN AJARAN 2018 / 2019 14 - 26 JANUARI 2018 NO Nama NIM Nilai GradeSasa AprilaNo ratings yet
- Erythema Multiforme Major: Case Report and Review of LiteratureDocument6 pagesErythema Multiforme Major: Case Report and Review of LiteratureSasa AprilaNo ratings yet
- Diabetes Mellitus A Devastating Metabolic DisorderDocument5 pagesDiabetes Mellitus A Devastating Metabolic DisorderDaniela Mădălina GhețuNo ratings yet
- SK 6 BL 9Document4 pagesSK 6 BL 9Sasa AprilaNo ratings yet
- D 023Document5 pagesD 023Ummu ZaFaNo ratings yet
- Jurnal-6-Naskah 7 JURNAL PDGI Vol 61 No 1Document6 pagesJurnal-6-Naskah 7 JURNAL PDGI Vol 61 No 1Nayda FitrinaNo ratings yet
- Erythema Multiforme Major: Case Report and Review of LiteratureDocument6 pagesErythema Multiforme Major: Case Report and Review of LiteratureSasa AprilaNo ratings yet
- 48 95 1 SMDocument6 pages48 95 1 SMMahesa DiantariNo ratings yet
- Scientific Dental Journal: Pigmented Oral Lichen Planus: A Case ReportDocument6 pagesScientific Dental Journal: Pigmented Oral Lichen Planus: A Case ReportSasa AprilaNo ratings yet
- BPJ Vol 11 No 1 P 167-170Document5 pagesBPJ Vol 11 No 1 P 167-170Retno Arienta SariNo ratings yet
- Orofacial Pain Conditions: Pain and Oral Mucosa: Berbagai Kondisi Nyeri Orofasial: Nyeri Dan MukosaDocument5 pagesOrofacial Pain Conditions: Pain and Oral Mucosa: Berbagai Kondisi Nyeri Orofasial: Nyeri Dan MukosaAlvionita AnggrainyNo ratings yet
- 6 ErythemaMultiformeClassificationandImmunopathogenesisDocument8 pages6 ErythemaMultiformeClassificationandImmunopathogenesisRandilufti SantosoNo ratings yet
- Insulin-Like Growth Factor-I (IGF-I) and Clinical Nutrition: Callum LIVINGSTONEDocument16 pagesInsulin-Like Growth Factor-I (IGF-I) and Clinical Nutrition: Callum LIVINGSTONEYafanita IzzatiNo ratings yet
- Structure and Function of The Endocrine SystemDocument53 pagesStructure and Function of The Endocrine Systemwalt65No ratings yet
- Novolin R SQ (Regular Insulin)Document3 pagesNovolin R SQ (Regular Insulin)ENo ratings yet
- 12 30 11 AADE Insulin WhitePaper PrintDocument17 pages12 30 11 AADE Insulin WhitePaper PrintMiguel Angel Fonseca RiveraNo ratings yet
- Diabetology Complete Book PDFDocument328 pagesDiabetology Complete Book PDFkguptaNo ratings yet
- Teaching Diabetes ManagementDocument5 pagesTeaching Diabetes ManagementWebster Claveria100% (5)
- Hormones and Nutrient PartitioningDocument36 pagesHormones and Nutrient Partitioningbwade2_916499061No ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults Epidemiology and PathogenesisDocument23 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults Epidemiology and PathogenesisAhraxazel Galicia Reyna100% (1)
- ChankoDocument9 pagesChankoPauloCarvalhoNo ratings yet
- Intro To Metabo (IsmDocument8 pagesIntro To Metabo (IsmManila MedNo ratings yet
- Literature Review On Diabetes Mellitus Type 2Document4 pagesLiterature Review On Diabetes Mellitus Type 2qtbghsbnd100% (1)
- Chapter 2 Intermittent Fasting and Weight LossDocument19 pagesChapter 2 Intermittent Fasting and Weight LosscharlesNo ratings yet
- City Passes Budget: A Dog For DiabetesDocument20 pagesCity Passes Budget: A Dog For DiabetesnewspubincNo ratings yet
- Patterns in The Evolution of Product Competition: Clayton ChristensenDocument11 pagesPatterns in The Evolution of Product Competition: Clayton ChristensenShawn BNo ratings yet
- Lethargic Weakness Decreased Performance: Nursing Care PlanDocument2 pagesLethargic Weakness Decreased Performance: Nursing Care PlanZhayree R.No ratings yet
- The 6 Stages of Diabetes Control & ReversalDocument7 pagesThe 6 Stages of Diabetes Control & ReversalHaleelu Abdul JaleelNo ratings yet
- Honk (Hiporosmolar Non Ketotik)Document24 pagesHonk (Hiporosmolar Non Ketotik)Raja Alfian IrawanNo ratings yet
- Diabetes Chapter 1 IntroductionDocument23 pagesDiabetes Chapter 1 IntroductionHannah CaldinoNo ratings yet
- Anti-Hyperglycemic Herbal Tea for Diabetic RatsDocument18 pagesAnti-Hyperglycemic Herbal Tea for Diabetic RatsJohn Laurence RañonNo ratings yet
- Insulin Prod ListDocument4 pagesInsulin Prod ListSteveEpsteinNo ratings yet
- Taurine Ameliorates Neuropathy in Diabetic RatsDocument6 pagesTaurine Ameliorates Neuropathy in Diabetic RatsΔημητρης ΦιλιογλουNo ratings yet
- Ampalaya Pandesal Promotes Diabetes ControlDocument11 pagesAmpalaya Pandesal Promotes Diabetes ControlCentienne BatemanNo ratings yet
- Diabetes FreedomDocument3 pagesDiabetes FreedomBiswajit BasakNo ratings yet
- Imbalanced Nutrition Less Than Body Requirements - Diabetes - NCPDocument5 pagesImbalanced Nutrition Less Than Body Requirements - Diabetes - NCPJulie Ann Jimenez Manlangit50% (4)
- Plants Used in Traditional Diabetes Treatment in NigeriaDocument68 pagesPlants Used in Traditional Diabetes Treatment in NigeriaYana PotNo ratings yet
- What Is Anatomy-WPS OfficeDocument4 pagesWhat Is Anatomy-WPS OfficePairene TalibNo ratings yet
- PBLDocument5 pagesPBLlourdes kusumadiNo ratings yet
- UGRD-GE6116 Science, Technology, and Society FINALS QUIZ 1Document21 pagesUGRD-GE6116 Science, Technology, and Society FINALS QUIZ 1Wawi Dela RosaNo ratings yet
- Insulin Therapy in Type 2 Diabetes MellitusDocument40 pagesInsulin Therapy in Type 2 Diabetes MellitusEDWIN WIJAYANo ratings yet
- Nutrition and diabetes information for studentDocument2 pagesNutrition and diabetes information for studentNova Novitarini100% (1)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 5 out of 5 stars5/5 (1)
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomFrom EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomRating: 4 out of 5 stars4/5 (1)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisFrom EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisRating: 3 out of 5 stars3/5 (2)
- Allen Carr's Easy Way for Women to Lose Weight: The original Easyway methodFrom EverandAllen Carr's Easy Way for Women to Lose Weight: The original Easyway methodRating: 4.5 out of 5 stars4.5/5 (18)
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthFrom EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthRating: 4 out of 5 stars4/5 (6)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- Keto Friendly Recipes: Easy Keto For Busy PeopleFrom EverandKeto Friendly Recipes: Easy Keto For Busy PeopleRating: 3.5 out of 5 stars3.5/5 (2)
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingFrom EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingRating: 5 out of 5 stars5/5 (59)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsFrom EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsRating: 4 out of 5 stars4/5 (49)
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingFrom EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingRating: 4 out of 5 stars4/5 (3)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- Hungry for Change: Ditch the Diets, Conquer the Cravings, and Eat Your Way to Lifelong HealthFrom EverandHungry for Change: Ditch the Diets, Conquer the Cravings, and Eat Your Way to Lifelong HealthRating: 4 out of 5 stars4/5 (7)
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainFrom EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainRating: 3.5 out of 5 stars3.5/5 (38)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- The Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthFrom EverandThe Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthRating: 5 out of 5 stars5/5 (37)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- Happy Gut: The Cleansing Program to Help You Lose Weight, Gain Energy, and Eliminate PainFrom EverandHappy Gut: The Cleansing Program to Help You Lose Weight, Gain Energy, and Eliminate PainRating: 3.5 out of 5 stars3.5/5 (6)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouFrom EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNo ratings yet
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (1)
- The Complete Beck Diet for Life: The 5-Stage Program for Permanent Weight LossFrom EverandThe Complete Beck Diet for Life: The 5-Stage Program for Permanent Weight LossRating: 3.5 out of 5 stars3.5/5 (6)
- Proteinaholic: How Our Obsession with Meat Is Killing Us and What We Can Do About ItFrom EverandProteinaholic: How Our Obsession with Meat Is Killing Us and What We Can Do About ItRating: 4.5 out of 5 stars4.5/5 (19)
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthFrom EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNo ratings yet
- How to Be Well: The 6 Keys to a Happy and Healthy LifeFrom EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeRating: 5 out of 5 stars5/5 (1)
- Foods That Cause You to Lose Weight: The Negative Calorie EffectFrom EverandFoods That Cause You to Lose Weight: The Negative Calorie EffectRating: 3 out of 5 stars3/5 (5)
- The Ultimate Volumetrics Diet: Smart, Simple, Science-Based Strategies for Losing Weight and Keeping It OffFrom EverandThe Ultimate Volumetrics Diet: Smart, Simple, Science-Based Strategies for Losing Weight and Keeping It OffNo ratings yet
- The Whole Body Reset: Your Weight-Loss Plan for a Flat Belly, Optimum Health & a Body You'll Love at Midlife and BeyondFrom EverandThe Whole Body Reset: Your Weight-Loss Plan for a Flat Belly, Optimum Health & a Body You'll Love at Midlife and BeyondRating: 4.5 out of 5 stars4.5/5 (28)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)