Professional Documents
Culture Documents
Lateral - Ankle Reconstruction Protocol
Uploaded by
Novaria PuspitaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lateral - Ankle Reconstruction Protocol
Uploaded by
Novaria PuspitaCopyright:
Available Formats
U W H E A LT H S P O R T S R E H A B I L I T A T I O N
Rehabilitation Guidelines for
Lateral Ankle Reconstruction
The ankle is a very complex joint. The muscles of the lower leg, ankle ankle sprains or even progress to the
There are actually three joints that and foot also help to stabilize the ankle ankle giving way with routine daily
make up the ankle complex: the joint dynamically. When the ankle activities. Aggressive rehabilitation,
tibiotalar joint, the subtalar joint and complex starts to move excessively in bracing, taping and orthotics are all
the distal tibiofibular joint. Stability one direction, reactive corrective firing non-surgical options that may be
of a joint is maintained by connective of the opposite muscle groups can help appropriate to prevent instability.
tissue structures and the dynamic stabilize the joint. The muscles that are
If these measures fail to control the
support of the surrounding muscles. primarily responsible for preventing
instability it may be necessary to
The primary stabilizing connective lateral ankle sprains are the peroneus
restore the anatomy of the lateral
tissues are ligaments. A ligament longus and brevis (Figure 2). The
ankle with surgical reconstruction.
connects bone to bone to limit excessive ability for these muscles to react quickly
The preferred surgical method is to
movement. The outside (lateral) ankle is not only related to their strength but
perform an anatomic repair of the
complex is stabilized at each of the more importantly by proprioception,
anterior talofibular and calcaneofibular
three joints by three major ligaments. which is the body’s ability to sense the
ligaments via a technique called
The tibiotalar joint is stabilized by the position of the joint and subsequently
the Brostrom repair, which involves
anterior talofibular (ATFL) ligament. correct it as necessary by sending nerve
shortening the attenuated ligaments
The subtalar joint is stabilized by the impulses to the appropriate muscles.
and a direct repair with suture
calcaneofibular (CF) ligament and the Proprioception can be enhanced or
fixation. When the anatomical repair
tibiofibular joint is stabilized by the trained with the use of balance exercises
is reinforced with the advancement of
anterior and posterior tibiofibular so these are commonly used in ankle
the inferior extensor retinaculum, it
(ATFL and PTFL) ligaments (Figure 1). sprain prevention and rehabilitation
is called the modified Brostrom repair.
programs.
When the repair is further augmented
Lateral ankle sprains are very with a slip of the peroneus brevis tendon
Intraosseus
Membrane Tibia common, especially in sports such as through a drill hole in the fibula it is
ATFL (tibiofibular)
basketball and volleyball. Generally referred to as a modified Brostrom-
Fibula ATFL (talofibular) athletes recover well from this type Evans technique. The peroneus brevis
of injury with physical therapy and tendon then acts as a check to inversion
PTFL
Talus rehabilitation. However, up to 20% stresses and provides reinforcement to
of lateral ankle sprains can lead to the anatomical repair without limiting
CFL
chronic pain and instability. This long-term inversion/eversion motion or
Calcaneus
instability may occur via repetitive strength. For revision surgeries or in the
(continued)
Figure 1
The health care team for
the UW Badgers and proud
sponsor of UW Athletics
621 SCIENCE DRIVE • MADISON, WI 53711 • UWSPORTSMEDICINE.ORG
Rehabilitation Guidelines for Lateral Ankle Reconstruction
case of excessive instability, an allograft strength, proprioception, movement reference to the average individual,
(cadaver tissue, usually a tendon) control and guide the athlete’s return but individual patients will progress
may be needed to reconstruct both the to sport. The rehabilitation guidelines at different rates depending on their
anterior talofibular and calcaneofibular are presented in a criterion based age, associated injuries, pre-injury
ligaments. progression. Specific time frames, health status, rehabilitation compliance
After surgery, rehabilitation with a restrictions and precautions are and injury severity. The technique
physical therapist or athletic trainer given to protect healing tissues and used for reconstruction may alter the
is needed to restore range of motion, the surgical repair/reconstruction. rehabilitation as well.
General time frames are also given for
Lateral View
Soleus muscle
Extensor digitorum longus muscle
Fibularis (peroneus)
longus muscle Superior extensor retinaculum
Tendinous sheath of tibialis anterior
Fibularis (peroneus)
brevis muscle Lateral malleoulus and subcutaneous bursa
Calcaneal (Achilles) tendon Inferior extensor retinaculum
Tendinous sheath of extensor digitorum
Common tendinous sheath
longus and peroneus tertius
of fibularis (peroneus)
longus and brevis
Tendinous sheath of
extensor hallucis longus
Subcutaneous calcaneal bursa
(Subtendinous) bursa
of calcaneal tendon
Superior
and Inferior
fibular (peroneal) retinacula
Calcaneus
Extensor digitorum brevis muscle
Fibularis (peroneus) tertius tendon
Fibularis Fibularis
Abductor digiti minimi muscle (peroneus) (peroneus)
Tuberosity of 5th metatarsal bone
longus brevis
tendon tendon
Figure 2
2 621 SCIENCE DRIVE • MADISON, WI 53711 • UWSPORTSMEDICINE.ORG
Rehabilitation Guidelines for Lateral Ankle Reconstruction
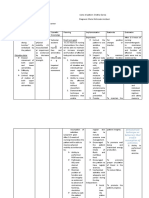
PHASE I (Surgery to 6 weeks after surgery)
Appointments • 2 weeks after surgery, the patient is seen by the surgeon; within 2-5 days of this
first visit with the surgeon following surgery, the patient should have the first
rehabilitation appointment
Rehabilitation Goals • Protection of the post-surgical ankle
Precautions • Non-weight bearing until the first visit following surgery with the surgeon, then
touchdown weight bearing (TDWB) in a boot or cast
Range of Motion (ROM) • No range of motion at this time, unless specified by surgeon, depending on
Exercises technique
(Please do not exceed the ROM
specified for each exercise and
time period)
Suggested Therapeutic • 4-way straight leg raises
Exercise • Full arc quad sets
• Abdominal isometrics
• Planks from knees
Cardiovascular Fitness • Upper Body Ergometer per patient
PHASE II (begin 6 weeks after surgery)
Appointments • Rehabilitation appointments are one time a week for ~4 weeks
Rehabilitation Goals • Continued protection of the repair
• 75% of full active range of motion
• Total leg strength to permit transition to weight bearing
• Wean out of boot to an ankle stabilizing orthoses (ASO)
Precautions • No inversion or eversion range of motion to protect the repair
• Progressive and graduated return to weight bearing
Range of Motion (ROM) • Active and Active Assistive range of motion for ankle plantarflexion and dorsifexion
Exercises • Active and Active Assistive range of motion for forefoot and toe mobility
(Please do not exceed the ROM
specified for each exercise and
time period)
3 621 SCIENCE DRIVE • MADISON, WI 53711 • UWSPORTSMEDICINE.ORG
Rehabilitation Guidelines for Lateral Ankle Reconstruction
Suggested Therapeutic • Ankle isometric strengthening in neutral
Exercise • Double leg balance exercises - starting in neutral with very short range of motion
excursions
• Standing 4-way straight leg raises
• Planks from feet—forward and lateral
Cardiovascular Fitness • Upper Body Ergometer, gentle stationary biking
PHASE III (begin after meeting Phase II criteria, usually 10 to 12 weeks after surgery)
Appointments • Rehabilitation appointments are one to two times per week
Rehabilitation Goals • Full active range of motion in weight bearing and non-weightbearing positions
• 5/5 (full strength) peroneal strength in neutral and plantarflexed positions
• 5/5 hip strength
• Normal gait mechanics
Precautions • No jumping, hopping or sports
• ASO to protect repair outside of therapy appointments
Suggested Therapeutic • Ankle strengthening exercise progression: progressing from short arc isotonics to
Exercise full arc isotonics to eccentric strengthening
• Balance progression: Double leg unstable surface to single leg stable surface
• Gait Drills: forward march, backward march, side stepping, backward stepping, hip
circle walk
• Gentle stretching as needed to regain full range of motion
Cardiovascular Fitness • Walking, biking, Stairmaster and elliptical (if Phase II criteria is met)
• No swimming
Progression Criteria • Full ankle strength on manual muscle testing and single leg balance equal to the
other side
4 621 SCIENCE DRIVE • MADISON, WI 53711 • UWSPORTSMEDICINE.ORG
Rehabilitation Guidelines for Lateral Ankle Reconstruction
PHASE IV (begin after meeting Phase III criteria, usually 14-16 weeks after surgery)
Appointments • Rehabilitation appointments are once every 2 to 3 weeks
Rehabilitation Goals • Patient to demonstrate stability with higher velocity movements and change of
direction movements that replicate sport specific patterns
• No apprehension or instability with high velocity change of direction movements
• Improve core and hip strength as well as mobility to eliminate any compensatory
stresses to the ankle
• Cardiovascular endurance for specific sport or work demands
Precautions • Progress gradually into provocative exercises by increasing velocity and
progressing from known to unanticipated movement patterns
Suggested Therapeutic • Impact control exercises beginning 2 feet to 2 feet, progressing from 1 foot to
Exercise • the other and then 1 foot to the same foot
• Movement control exercises beginning with low velocity, single plane activities and
progressing to higher velocity, multi-plane activities
• Return to running drills focusing of proper gait mechanics without compensations
or significant post exercise soreness
• Balance progression: Single leg stable surface to single leg unstable surface
• Strength and control drills related to sport specific movements, including dynamic
balance and strength in plantarflexed positions
• Sport/work specific balance and proprioceptive drills
• Hip and core strengthening
• Stretching for patient specific muscle imbalances
Cardiovascular Fitness • Design to use sport specific energy systems
Progression Criteria • Patient may return to sport after receiving clearance from the orthopedic surgeon
and the physical therapist/athletic trainer
These rehabilitation guidelines were developed collaboratively by Marc Sherry, PT, DPT, LAT, CSCS, PES (msherry@uwhealth.org)
and the UW Health Sports Medicine physician group.
Updated 6/2014
At UW Health, patients may have advanced diagnostic and /or treatment options, or may receive educational materials that vary from this information. Please be aware that this information is not intended to replace
the care or advice given by your physician or health care provider. It is neither intended nor implied to be a substitute for professional advice. Call your health provider immediately if you think you may have a medical
emergency. Always seek the advice of your physician or other qualified health provider prior to starting any new treatment or with any question you may have regarding a medical condition.
SM-39916-14
Copyright 2014 UW Health Sports Medicine Center
5 621 SCIENCE DRIVE • MADISON, WI 53711 • UWSPORTSMEDICINE.ORG
You might also like
- Trigger Point Therapy Made Simple Serious Pain Relief in 4 Easy StepsDocument275 pagesTrigger Point Therapy Made Simple Serious Pain Relief in 4 Easy StepsMohaideen Subaire100% (10)
- Above Knee Amputation Good One PDFDocument9 pagesAbove Knee Amputation Good One PDFSenthilkumar Thiyagarajan100% (1)
- Assessing Lateral Hip StabilityDocument7 pagesAssessing Lateral Hip StabilityCristian Alejandro Flores PinuerNo ratings yet
- Soft Tissue Balance KneeDocument10 pagesSoft Tissue Balance KneeNitin BansalNo ratings yet
- Ankle Instab Presentation and ManagementDocument7 pagesAnkle Instab Presentation and Managementfahmiatul lailiNo ratings yet
- Functional Rehabilitation of Lumbar Spine Injuries in The AthleteDocument8 pagesFunctional Rehabilitation of Lumbar Spine Injuries in The AthleteTiago DiasNo ratings yet
- Effect of Core Stabilization Training On Endurance of Trunk Extensor and Functional Capacity in Subjects With Mechanical Low Back PainDocument8 pagesEffect of Core Stabilization Training On Endurance of Trunk Extensor and Functional Capacity in Subjects With Mechanical Low Back PainDr. Krishna N. SharmaNo ratings yet
- Journals Ijatt 14 3 Article-P10-PreviewDocument2 pagesJournals Ijatt 14 3 Article-P10-PreviewAayush KatyalNo ratings yet
- Snatch Balance TechniqueDocument8 pagesSnatch Balance TechniqueBatta ZahranNo ratings yet
- Treating Scapular Dyskinesis Through RehabilitationDocument8 pagesTreating Scapular Dyskinesis Through RehabilitationYa ChenNo ratings yet
- Theme 3. Lumbopelvic Motor Control, Instability and PainDocument9 pagesTheme 3. Lumbopelvic Motor Control, Instability and PainThéo BattalianNo ratings yet
- PDF CrackDocument12 pagesPDF Crackdj_reaverNo ratings yet
- Basic Biomechanics of The HipDocument8 pagesBasic Biomechanics of The HipManuel Azael Rodríguez CigalaNo ratings yet
- 2016 Biomechanics of the hipDocument8 pages2016 Biomechanics of the hipilanNo ratings yet
- Biomechanic of FootDocument8 pagesBiomechanic of FootMichealowen BabygoalNo ratings yet
- Biomechanic of Foot PDFDocument8 pagesBiomechanic of Foot PDFMichealowen BabygoalNo ratings yet
- Shoulder Dislocation TechniquesDocument9 pagesShoulder Dislocation TechniqueskenthepaNo ratings yet
- Treatment and Rehabilitation of Fractures (Stanley Hoppenfeld)Document1 pageTreatment and Rehabilitation of Fractures (Stanley Hoppenfeld)小蓮花No ratings yet
- (I) Biomechanics of The Knee Joint: Mini-Symposium: Soft Tissue Surgery in The KneeDocument8 pages(I) Biomechanics of The Knee Joint: Mini-Symposium: Soft Tissue Surgery in The KneeMat MarinhoNo ratings yet
- Principles of Core Stability in The Training and in The Rehabilitation: Review of LiteratureDocument6 pagesPrinciples of Core Stability in The Training and in The Rehabilitation: Review of LiteratureMagno FilhoNo ratings yet
- Core Stability ReviewDocument6 pagesCore Stability ReviewJoílton OliveiraNo ratings yet
- Corestabilityexerciseprinciples VakuthotaDocument7 pagesCorestabilityexerciseprinciples Vakuthotarafael ferreira .silvaNo ratings yet
- Anatomy, Function, and Rehabilitation of The Popliteus Musculotendinous ComplexDocument16 pagesAnatomy, Function, and Rehabilitation of The Popliteus Musculotendinous ComplexJacinta SeguraNo ratings yet
- Kinesiology of Shoulder ComplexDocument13 pagesKinesiology of Shoulder ComplexJaymin BhattNo ratings yet
- Faries NSCA Core StabilizationDocument16 pagesFaries NSCA Core StabilizationSean SibbettNo ratings yet
- 10.popliteus Musculotendinous ComplexDocument15 pages10.popliteus Musculotendinous Complex黃郁庭No ratings yet
- Mobility Screening For The CoreDocument6 pagesMobility Screening For The CoreАнастасия ХомяковаNo ratings yet
- 5 Biomechanics of The Vertebral Column 2Document40 pages5 Biomechanics of The Vertebral Column 2Daniel PereiraNo ratings yet
- Osteopathic Manipulative Treatment in Tarsal Somatic Dysfunction: A Case StudyDocument5 pagesOsteopathic Manipulative Treatment in Tarsal Somatic Dysfunction: A Case StudyВиктория ГоробинскаяNo ratings yet
- Jumper's Knee: Joseph M. David, MS, Pt1Document5 pagesJumper's Knee: Joseph M. David, MS, Pt1Hanako HanabiNo ratings yet
- Maintaining Joint Range of MotionDocument27 pagesMaintaining Joint Range of MotionKiko KikoNo ratings yet
- Anatomy and Bio Mechanics of The KneeDocument15 pagesAnatomy and Bio Mechanics of The KneeaimanshalpyNo ratings yet
- IASTM and Stretching Plantar FasciitisDocument11 pagesIASTM and Stretching Plantar FasciitisNicolás Ayelef ParraguezNo ratings yet
- Open Repair of Anterior Shoulder Instability: Michael J. PagnaniDocument11 pagesOpen Repair of Anterior Shoulder Instability: Michael J. PagnaniJaime Vázquez ZárateNo ratings yet
- Thebiomechanics of Fixed AnklefootorthosesDocument9 pagesThebiomechanics of Fixed AnklefootorthosesUshsbsNo ratings yet
- The Biomechanics of Posterior Lumbar Interbody.14Document5 pagesThe Biomechanics of Posterior Lumbar Interbody.14danielalexandersinaga.xiiipa2No ratings yet
- Foot and Ankle ArthrokinematicsDocument6 pagesFoot and Ankle ArthrokinematicsCraig StewartNo ratings yet
- FascialFitness in DaltonDocument12 pagesFascialFitness in DaltonQuiroprácticaParaTodosNo ratings yet
- Jospt 1995 21 5 277Document10 pagesJospt 1995 21 5 277GerardoNo ratings yet
- Herteil 1998Document5 pagesHerteil 1998Felipe AcuñaNo ratings yet
- donatelli-1985-normal-biomechanics-of-the-foot-and-ankleDocument9 pagesdonatelli-1985-normal-biomechanics-of-the-foot-and-ankleosteopedcursoNo ratings yet
- Shoulder Rehab ProgressionsDocument30 pagesShoulder Rehab ProgressionsSiti FahwizaNo ratings yet
- SM UCL Reconstruction PDFDocument6 pagesSM UCL Reconstruction PDFinesdeliaNo ratings yet
- Ijspt-Biomechanics and Pathomechanics of The Patellofemoral JointDocument11 pagesIjspt-Biomechanics and Pathomechanics of The Patellofemoral JointDevi MigiekaNo ratings yet
- Jospt 1995 21 5 277Document6 pagesJospt 1995 21 5 277GERARDO TORRES RUIZNo ratings yet
- B15 M4 - Sports Injury (Dr. W. Mana-Ay 2014)Document8 pagesB15 M4 - Sports Injury (Dr. W. Mana-Ay 2014)Dakila Vine VillanNo ratings yet
- Shoulder Conditions in Agility Dogs: T T T TDocument5 pagesShoulder Conditions in Agility Dogs: T T T TJuan-PabloChaperoArenasNo ratings yet
- Radio Logical Evaluation of Lumbar Interfertebral InstabilityDocument6 pagesRadio Logical Evaluation of Lumbar Interfertebral Instabilityiss kimNo ratings yet
- Core Muscle Injuries (Athletic Pubalgia, Sports Hernia) : PathophysiologyDocument5 pagesCore Muscle Injuries (Athletic Pubalgia, Sports Hernia) : PathophysiologyandiNo ratings yet
- Core Stability An IntroductionDocument70 pagesCore Stability An Introductionruth sosaNo ratings yet
- CH 41 LBP - Braddom's Physical Medicine & RehabilitationDocument46 pagesCH 41 LBP - Braddom's Physical Medicine & RehabilitationPyrectic WilliamsNo ratings yet
- Core Stability Exercise PrinciplesDocument6 pagesCore Stability Exercise Principlesphysioali0% (2)
- 1 s2.0 S1877056811000818 MainDocument4 pages1 s2.0 S1877056811000818 MainEvans JohnNo ratings yet
- Core Muscle Strengthening in The AthleteDocument48 pagesCore Muscle Strengthening in The AthleteNicu Tanase-RaduNo ratings yet
- TX 5 - Short - BDocument29 pagesTX 5 - Short - BDr. Sidra Qureshi100% (1)
- Dasar Rias 2Document9 pagesDasar Rias 2AnDi Anggara PeramanaNo ratings yet
- Iliotibial Band Syndrome: Soft Tissue and Biomechanical Factors in Evaluation and TreatmentDocument12 pagesIliotibial Band Syndrome: Soft Tissue and Biomechanical Factors in Evaluation and TreatmentThazarNo ratings yet
- Muscle Re-Education by Venkata RamaiahDocument8 pagesMuscle Re-Education by Venkata Ramaiahvenkata ramakrishnaiahNo ratings yet
- Functional Capacity ImprovementDocument16 pagesFunctional Capacity ImprovementNovaria PuspitaNo ratings yet
- Grafik Cardiac Rehabilitation After AMIDocument9 pagesGrafik Cardiac Rehabilitation After AMINovaria PuspitaNo ratings yet
- Consensus Statement On ESWT Indications and ContraindicationsDocument4 pagesConsensus Statement On ESWT Indications and ContraindicationsNovaria PuspitaNo ratings yet
- Cardiac Rehab: Improving Function & Reducing RiskDocument33 pagesCardiac Rehab: Improving Function & Reducing RiskNovaria PuspitaNo ratings yet
- Cardiac Rehab: Improve Heart Failure Symptoms Through ExerciseDocument29 pagesCardiac Rehab: Improve Heart Failure Symptoms Through ExerciseNovaria PuspitaNo ratings yet
- Preventing and Treating OH As Easy As ABCDocument13 pagesPreventing and Treating OH As Easy As ABCiri_balNo ratings yet
- Supraveghere Sold in Paralizie InfantilaDocument19 pagesSupraveghere Sold in Paralizie InfantilaAlina MerticariuNo ratings yet
- Use of MusicDocument6 pagesUse of MusicNovaria PuspitaNo ratings yet
- Penyakit Paru RestriktifDocument36 pagesPenyakit Paru RestriktifNovaria Puspita100% (2)
- Spasticity After SCI PDFDocument10 pagesSpasticity After SCI PDFNovaria PuspitaNo ratings yet
- In Store Poster 2Document4 pagesIn Store Poster 2Monica LauraNo ratings yet
- How Art Can HealDocument16 pagesHow Art Can HealNguyễn Phạm Minh NgọcNo ratings yet
- Ospe-Ll 16Document35 pagesOspe-Ll 16Muthu GuhaanNo ratings yet
- Manejo de Las Deformidades de Pie en Niños Con Trastornos NeuromotoresDocument12 pagesManejo de Las Deformidades de Pie en Niños Con Trastornos NeuromotoresEmiliano Emmanuel RussoNo ratings yet
- NCP of Impaired MobilityDocument3 pagesNCP of Impaired MobilityHazel Cabrera0% (1)
- Patofisiologi CTS 1Document4 pagesPatofisiologi CTS 1Michael DeniNo ratings yet
- Congenital Hip DysplasiaDocument24 pagesCongenital Hip DysplasiaElizabeth Quiñones100% (1)
- M.A. in Yoga and Naturopathy, Regulation, Course Structure and Syllabus DetailsDocument15 pagesM.A. in Yoga and Naturopathy, Regulation, Course Structure and Syllabus DetailsS SarojNo ratings yet
- Evidence Based Guidelines For Complex Regional Pain Syndrome Type 1Document49 pagesEvidence Based Guidelines For Complex Regional Pain Syndrome Type 1roooNo ratings yet
- Acupuncture: Ancient Treatment For Modern IllnessesDocument31 pagesAcupuncture: Ancient Treatment For Modern IllnessesJessica PaulNo ratings yet
- Functional Re EducationDocument38 pagesFunctional Re EducationDhruvNo ratings yet
- Occupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesDocument2 pagesOccupational English Test: Writing Sub-Test: Nursing Time Allowed: Reading Time: 5 Minutes Writing Time: 40 MinutesAnit XingNo ratings yet
- 0 - Biomechanics of Lumbar SpineDocument25 pages0 - Biomechanics of Lumbar SpineCHAITANYA SAHITHINo ratings yet
- Chapter 10 - The Lower Limb: Snell 9 EdDocument138 pagesChapter 10 - The Lower Limb: Snell 9 EdFerjie Angelica DalandaoNo ratings yet
- Lab Manuals, Paraffin, HydrocollatorDocument12 pagesLab Manuals, Paraffin, HydrocollatorChristian MontesNo ratings yet
- Joshis External Stabilisation System Jess For Recurrent Ctev Due To Irregular Follow Up PDFDocument5 pagesJoshis External Stabilisation System Jess For Recurrent Ctev Due To Irregular Follow Up PDFshankarNo ratings yet
- Milan Resume Template ProfessionalDocument3 pagesMilan Resume Template ProfessionalRaviNo ratings yet
- Tennis Elbow and Golfer's Elbow GuideDocument40 pagesTennis Elbow and Golfer's Elbow GuideVijay PradeepNo ratings yet
- Physiotherapeutic Management of Patients With Pregnancy-Related Pelvic Girdle PainDocument24 pagesPhysiotherapeutic Management of Patients With Pregnancy-Related Pelvic Girdle PainAndrei MurariuNo ratings yet
- Musculoskeletal Medicine in The Usa Education and Training of Family PhysiciansDocument4 pagesMusculoskeletal Medicine in The Usa Education and Training of Family PhysiciansDavidBeatonComuladaNo ratings yet
- Brachial NeuritisDocument7 pagesBrachial Neuritisfirza yoga baskoroNo ratings yet
- Jersey FingerDocument2 pagesJersey FingerBogdan TudorNo ratings yet
- Amputation Rehab GoalsDocument58 pagesAmputation Rehab GoalsHikaru99 otakuNo ratings yet
- Writers Cramp - A Major Conundrum: Review Article44Document7 pagesWriters Cramp - A Major Conundrum: Review Article44IJAR JOURNALNo ratings yet
- Design CPMDocument5 pagesDesign CPMNura Eky VNo ratings yet
- Lower Limbs MCQs Section 1 TitleDocument148 pagesLower Limbs MCQs Section 1 TitleCaim ZNo ratings yet
- Respiratory Therapist Project - Amber SchoenickeDocument21 pagesRespiratory Therapist Project - Amber Schoenickeapi-619891965No ratings yet
- Massage Therapist Resume ExamplesDocument7 pagesMassage Therapist Resume Examplesafjwdbaekycbaa100% (2)
- Prehabilitation in Paediatric Orthopaedic Surgery Reduces Hospital Length of StayDocument8 pagesPrehabilitation in Paediatric Orthopaedic Surgery Reduces Hospital Length of StayZvonkitza CertanecNo ratings yet