Professional Documents
Culture Documents
Artigo Fes
Uploaded by
Thiago Penna ChavesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Artigo Fes
Uploaded by
Thiago Penna ChavesCopyright:
Available Formats
REVIEW PHYSIOLOGY 35: 40 –56, 2020. Published December 4, 2019; doi:10.1152/physiol.00015.
2019
Electrical Stimulation of Muscle: Roger M. Enoka,1
Ioannis G. Amiridis,2 and
Electrophysiology and Rehabilitation Jacques Duchateau3
1
Department of Integrative Physiology, University of Colorado
The generation of action potentials in intramuscular motor and sensory axons Boulder, Colorado; 2Department of Physical Education and
Sport Sciences at Serres, Aristotle University of Thessaloniki,
Thessaloniki, Greece; and 3Laboratory of Applied Biology and
in response to an imposed external current source can evoke muscle contrac- Neurophysiology, ULB Neuroscience Institute, Université Libre
de Bruxelles, Brussels, Belgium
tions and elicit widespread responses throughout the nervous system that enoka@colorado.edu
impact sensorimotor function. The benefits experienced by individuals ex-
posed to several weeks of treatment with electrical stimulation of muscle
suggest that the underlying adaptations involve several physiological systems,
but little is known about the specific changes elicited by such interventions.
central nervous system; electrical stimulation; electrophysiology; evoked
contractions; therapeutic benefits
Introduction tivation of motor units can be compromised in
some conditions.
Physiologists have known about the existence of When the activation of motor units is compro-
electrical currents in nerves and muscle in humans mised, experimental and clinical studies have
since at least 1843 (41). The first recordings of demonstrated that it is possible to attenuate the
electrical activity in muscle (116) and action cur- deficit by supplementing the activation with elec-
rents in nerve (2), however, were not published trical stimulation of muscle. The typical approach
until the early 1900s. As reviewed in Duchateau is to pass an electric current between conductive
and Enoka (42), it soon became obvious to several pads attached to the skin over a targeted muscle or
eminent physiologists that the activation signal group of muscles. The outcomes from these stud-
used by the nervous system to control muscle force ies, however, have demonstrated that the forces
and the adaptations evoked by the applied current
comprised unitary electrical events known as ac-
vary with the stimulus parameters. The purpose of
tion potentials. Moreover, they found that the ac-
this brief review is to synthesize the findings on the
tion potentials generated by each motor neuron
rehabilitation potential of protocols in which elec-
are distributed to a distinct set of muscle fibers,
trical stimulation is applied percutaneously over
which together form the motor unit (83). The mo-
muscle to elicit action potentials in intramuscular
tor unit came to be recognized as the final com-
axons. Before reviewing this work, however, we
mon pathway by which the electrical activation
begin by discussing key details of the electrophys-
signal is transmitted from the nervous system to
iology underlying the evoked activity.
muscle and then transformed into contractile
activity. Electrophysiology
After ~100 years since the discovery of the motor
unit, much has been learned about the organiza- Although the application of current over a muscle
tion of motor unit activity during the performance in vivo can enable the contractile proteins to per-
of voluntary actions. As summarized in several re- form work, the activation signal is generated in
views on motor unit physiology (42, 46, 61), we intramuscular axons and not in muscle fibers di-
know that motor units are recruited in a relatively rectly, at least with pulse durations of ⱕ1 ms. The
fixed order, the force produced by a muscle over delivery of an electrical current either through
most of its operating range is controlled by con- electrodes attached to the skin or through wires
current adjustments in motor unit recruitment and inserted into the anterior thigh muscles of human
rate coding, the rate at which action potentials are volunteers during a surgical procedure was not
generated increases during faster contractions, the able to evoke a muscle contraction after intrave-
peak discharge rates achieved during most volun- nous administration of curare (68). Since curare
tary contractions are less than those necessary to blocks synaptic transmission at the neuromuscular
produce maximal motor unit force, motor unit ter- junction, this observation indicates that electrical
ritories are reorganized with advancing age and in currents evoke muscle contractions by eliciting ac-
the presence of neurological diseases, and the ac- tion potentials in intramuscular nerve fibers (100).
40 1548-9213/20 Copyright © 2020 Int. Union Physiol. Sci./Am. Physiol. Soc.
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
Moreover, Hultman and colleagues (68) found that likely depends most on the longitudinal distribu-
the current fields associated with intramuscular tion of the intramuscular currents. Although the
electrodes engaged a greater number of sensory electrical stimulation presumably activates the
axons than did percutaneous stimulation, even muscle fibers that have innervating axons located
though the current intensity delivered through the in a current field that exceeds the threshold for
surface electrodes was ~10 times greater. After ad- action-potential generation (76), it seems likely
ministration of local anesthetics into the muscle that the action potentials can propagate anti-
proximal to the stimulating electrodes to block af- dromically along motor axons from this location,
ferent feedback, they found that the application of in addition to the expected orthodromic propaga-
electrical stimulation (frequency: 20 Hz; pulse du- tion, and thereby engage most of the muscle fibers
ration: 0.5 ms) through intramuscular electrodes belonging to the motor unit. Evidence for this ex-
could evoke a force equal to the 70% of the peak pectation is provided by the observation that the
force achieved during a maximal voluntary con- generation of an action potential in a peripheral
traction (MVC). motor axon by an electrical stimulus is propagated
antidromically back to the motor neuron where it
Intramuscular Distribution of Evoked elicits an action potential that is then propagated
Responses Varies With Electrode Placement orthodromically back to the muscle, where it can
Most rehabilitation protocols that include electri- be recorded as an evoked response known as an F
cal stimulation involve the delivery of current wave (157).
through electrodes attached to the skin of the pa- Consistent with this interpretation, some evi-
tient, which means the benefits are constrained by dence suggests that the application of a current
the distribution of the current within the underly- through electrodes placed around the motor point
ing tissues. In an analytical model of a volume (20) may elicit action potentials in most of the
conductor with three layers of tissue (skin ⫽ 1 mm, muscle fibers belonging to individual motor units
fat ⫽ 1 mm, and muscle ⫽ 96 mm), Mesin and in tibialis anterior. The evidence is based on the
Merletti (97) determined that the current density similarity of the shapes of action potentials ex-
decayed to 10% of the value applied to the skin at tracted by spike-triggered averaging during the
a distance of 10 mm from the electrodes. Experi- performance of voluntary contractions and evoked
mental estimates of the intramuscular current con- contractions (FIGURE 2). The purpose of the study
firm the marked decay in current density with that compared the shapes of the action potentials
increases in distance from the source. For example, was to quantify the recruitment order for pairs of
Petrofsky et al. (113) estimated that the current motor units during voluntary and electrically
detected by a needle electrode at a depth of 0.5 cm evoked contractions (49). Spike-triggered averag-
into the muscle (~2.5 cm from the skin surface) was ing of the electromyographic (EMG) and force sig-
⬍1% of the current applied between electrodes (2 nals during voluntary contractions (FIGURE 2C)
cm ⫻ 2 cm) attached to the skin over quadriceps yielded the action potential shapes and twitch re-
femoris. Increases in the current passed between sponses of individual motor units (FIGURE 2, A
surface electrodes, therefore, result in a greater AND B). With careful grading of the applied cur-
spatial distribution of intramuscular currents to rent to evoke a muscle contraction, the similarity
elicit action potentials in the axons included within of the action potential shapes during the voluntary
a critical volume of the muscle. Petrofsky et al. and evoked contractions suggests that it was pos-
(113) found, for example, that a modest (20 mA) sible to determine the current needed to activate
sinusoidal current (30 Hz, 0.3 ms) evoked a quad- the same two motor units (FIGURE 2D). The data
riceps femoris force of 15% MVC, whereas a stron- for the pair of motor units shown in FIGURE 2
ger current (60 mA) produced a force of 75% MVC. indicate that a greater current was required to ac-
Critically, the volume of muscle activated by an tivate motor unit 1 (MU 1), which had a lower
applied current varies with the distance between recruitment threshold during the voluntary con-
the stimulating electrodes attached to the skin over traction. Such reversal of recruitment order was
a target muscle (54). observed for 28 –35% of the motor unit pairs, de-
The greater force evoked with stronger currents pending on pulse duration, suggesting that the re-
is due to an increase in the number of activated cruitment order of motor units is relatively random
motor axons (98). The applied currents are distrib- during contractions evoked by electrical stimula-
uted both into (transverse direction) and along tion applied over the muscle (49, 69, 76).
(longitudinal direction) the target muscles, with Most studies find that currents applied through
conductivity being greater in the longitudinal di- electrodes attached to the skin over a muscle tend
rection (97). Given the broad distribution of intra- to activate the more superficial muscle fibers (98,
muscular axons (FIGURE 1), the capacity of 149), but some evidence suggests that surface stim-
surface-applied currents to evoke strong forces ulation can activate deep regions within a muscle
PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org 41
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
(1). In an elegant assessment of the spatial distri- statistically significant differences in the current
bution of muscle fiber activation evoked by surface required to achieve the three M-wave sizes at the
stimulation, Okuma et al. (108) measured the am- two intramuscular locations.
plitude of the direct motor response (M wave) at These results indicate that the location of the
superficial (0.7 ⫾ 0.2 cm from the surface of the stimulating electrodes has a significant impact
muscle) and deep (2.0 ⫾ 0.3 cm) locations within on the spatial distribution of the activated mus-
the tibialis anterior muscle. The intramuscular re- cle fibers. Due to the widespread distribution of
cordings were made with fine-wire electrodes that intramuscular nerve branches in large muscles
had 0.25 cm of the insulation removed from the tip (FIGURE 1) that can give rise to several motor
of the wire. The current was applied either through points (82, 124), multiple electrodes are necessary
pads that were trimmed to fit over the middle to engage most of the motor units in a muscle (22).
one-third of each participant’s tibialis anterior In smaller muscles that have less intramuscular
muscle or an electrode (3.2-cm diameter) attached nerve branching, however, a similar force can be
over the innervating nerve (common peroneal) evoked by electrodes placed over the motor point
near the head of the fibula. The primary outcome and the innervating nerve (62).
variable was an M-wave recruitment curve that Although the terminal branches of intramus-
shows the relation between M-wave size (V·s) and cular axons are distributed widely throughout a
applied current (mA). When the current was ap- muscle (FIGURE 1), over-the-muscle stimulation
plied through the electrodes attached over the presumably results in no more than modest
muscle, they found that a greater current was amounts of jitter in the arrival time of the action
needed to achieve specific M-wave sizes (5%, 50%, potentials at the muscle fibers within and across
and 95% of maximum) at the deep location than at motor units, and this variability remains rela-
the superficial location. In contrast, when the elec- tively consistent across contraction intensities
trical stimulation was applied through the elec- (12, 33, 96). Consistent with a fundamental dif-
trodes placed over the nerve, there were no ference in the genesis of the activation signal
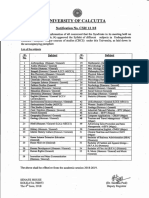
FIGURE 1. Branching of intramuscular nerves for three lower leg muscles in humans
The branching patterns were identified in cadaveric specimens (n ⫽ 8) using modified Sihler’s staining technique. The gray area in each panel indi-
cates the location of the distal attachment to the skeleton. A: tibialis anterior, innervated by branches of the deep fibular nerve. B: gastrocnemius,
the two heads (medial and lateral) are innervated by the tibial nerve. C: soleus, innervated by the tibial nerve, which branches into superficial and
deep compartments. Images are from Ref. 160 and used with permission from Surgical and Radiologic Anatomy.
42 PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
between voluntary and evoked contractions, sensory axons alone or a mixture of sensory and
Jones et al. (69) found that an increase in the cur- motor axons when the stimulating electrodes are
rent delivered to a hand muscle evoked stronger attached to the skin close to a peripheral nerve (63,
contractions but did not alter the amplitude of the 64). At low intensities, the current initially elicits
fluctuations in the low-pass-filtered force (25 Hz) action potentials in afferent axons— especially
in contrast to the signal-dependent noise observed group Ia fibers—that evoke excitatory post-synap-
during voluntary contractions. The electrical stim- tic potential in motor neurons and then engage a
ulation (25–30 Hz, 0.3 ms) was applied through spinal reflex pathway to produce an evoked re-
electrodes placed over the motor point of extensor sponse (H reflex) in a target muscle (110, 114, 125)
pollicis longus to elicit forces in the range of 20 – and to recruit low-threshold motor units (33).
70% MVC. FIGURE 3, RIGHT shows that the fluctu- Gradual increases in current intensities will pro-
ations in the filtered force signal during multiple gressively activate motor axons to produce a direct
trials of evoked contractions did not change across motor response (M wave) and eventually suppress
three target forces. In contrast, the amplitude of the H reflex completely (67). Although the stronger
the force fluctuations during the voluntary con- currents still elicit action potentials in group Ia
tractions increased with target force, which is at- afferents, the motor neurons are less responsive to
tributed to an increase in the variance of common the synaptic input provided by the sensory fibers.
synaptic input to motor neurons (48, 105, 141) that This occurs because the membrane potential be-
augments the jitter in the arrival times of the action comes refractory due the antidromic propagation
potentials at the muscle fibers. of the action potential along the motor axon back
into the spinal cord, as indicated by the recruit-
Central Distribution of Evoked Responses ment curves for M waves and H reflexes (see Fig. 1
In addition to influencing the spatial distribution in Ref. 125).
of evoked responses within the muscle, placement H reflexes and M waves can also be recorded
of the electrodes around the motor point or over when a train of electrical stimuli are used to evoke
the nerve elicits action potentials in a broad range a muscle contraction; this method of activating
of sensory axons that provide feedback received by muscle is known as neuromuscular electrical stim-
the central nervous system (103, 111, 118, 153). We ulation (NMES) (89). For example, Collins et al. (27)
know from classic studies on the Hoffmann (H) demonstrated that NMES delivered through large
reflex that it is possible with a single-stimulus pads (3–18 cm ⫻ 3.5 cm) placed over lower leg
pulse to evoke action potentials in large-diameter muscles (tibialis anterior and triceps surae) was
FIGURE 2. Recruitment order for a pair of motor units during voluntary and electrically evoked
contractions
The recruitment order of two motor units (MU1 and MU2) in tibialis anterior during a voluntary contraction (C) and
the corresponding motor unit action potentials (1) and mechanical responses (2) as determined by spike-triggered
averaging (A, B). The same two motor units, based on the similarity of the action potential shapes (D), were acti-
vated by different currents delivered through electrodes attached to the skin over the motor point of tibialis ante-
rior (cathode: 0.8-mm diameter) and on the calf muscles (anode: 2 ⫻ 3 cm). Data are from Ref. 49 and used with
permission from Experimental Brain Research.
PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org 43
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
able to elicit action potentials in sensory axons Hz and for 1-ms pulses compared with 0.05-ms
(current set below motor threshold) alone or in and 0.25-ms pulses.
both sensory and motor axons (current set above Subsequently, Bergquist et al. (15) compared the
motor threshold). When the applied current (rect- force evoked in the plantar flexors by NMES that
angular pulses) was set below motor threshold, the was delivered either through electrodes placed
electrical stimulation (100 Hz with 1-ms pulses) over the peripheral nerve (tibial nerve in the pop-
elicited a muscle force that began at 1.5–5 s after liteal fossa) or over the muscles themselves. The
stimulus onset and continued for 2–10 s until it maximal amplitude of the M wave evoked in soleus
reached a value of 2–10% of the MVC force. To was similar for the two stimulus locations, but the
demonstrate that the evoked force was attributable amplitude of the maximal H reflex normalized to
to sensory feedback, the response was abolished the maximal M-wave amplitude was greater for
after conduction along the nerve was blocked with electrodes placed over the tibial nerve (0.60 ⫾ 0.01)
an anesthetic that was applied proximal to the site than that evoked by electrodes placed over the
of electrical stimulation (19, 81). muscle (0.10 ⫾ 0.01). These findings suggest that
The magnitude of the feedback-evoked force sensory feedback, at least that transmitted by
was greater when Collins et al. (27) increased the group Ia afferents, was greater when NMES was
current intensity to elicit action potentials in delivered through electrodes placed over the nerve
motor axons and evoke an initial force that was compared with when the stimulation was delivered
~5% of the MVC value. By the end of the 7-s over the muscle. Similar findings were reported by
contraction, force had increased by 1.6-fold for the same group when the protocol was performed
the dorsiflexors and 1.9-fold for the plantar flex- on the quadriceps femoris muscles, although H-re-
ors, although there was considerable variability flex amplitude relative to M-wave amplitude was
in the magnitude of the response among partic- much less in quadriceps than in soleus (16).
ipants (16, 154). Collins et al. (27) found that the However, augmentation of the applied force by
capacity of the sensory feedback to augment the sensory feedback during over-the-muscle stimula-
applied force was greatest at a stimulus fre- tion does not rely exclusively on the activation of
quency of 100 Hz compared with 25 Hz and 200 group Ia afferents. For example, Blouin et al. (19)
FIGURE 3. Forces exerted by the thumb during voluntary and NMES-induced contractions to dif-
ferent target forces
The force was produced by the extensor pollicis longus muscle, which is solely responsible for extension of the dis-
tal phalanx of the thumb. NMES (25–30 Hz, 0.3 ms) was delivered through electrodes (cathode: 1 ⫻ 2 cm; anode:
5-cm diameter) placed around the motor point. Columns 1 and 3 show the complete force trace for the voluntary
(column 1) and NMES-evoked (column 3) forces. Columns 2 and 4 show the force fluctuations relative to average
force. The “4 s” bar indicates the absence of visual feedback. Data are from Ref. 69 and used with permission
from Journal of Neurophysiology.
44 PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
found that high-frequency stimulation (100 Hz, supraspinal pathways was reduced but that the am-
rectangular 1-ms pulses) delivered through elec- plitude for the long-latency response mediated by
trodes placed over the motor point of a muscle non-muscle afferents was unchanged. In contrast,
with weak homonymous Ia monosynaptic projec- the changes in the amplitudes of these responses
tions (flexor pollicis longus) was able to elicit extra differed when the fatiguing contraction (117 ⫾ 32 s)
torque that was abolished with a nerve block. A was evoked by NMES (supramaximal pulses at 30 Hz
similar result was obtained for biceps brachii with a duration of 0.2 ms) applied over the muscle.
(19) and for first dorsal interosseus (10), both of Despite a similar reduction in the applied force for
which have stronger Ia monosynaptic connectiv- the two fatiguing contractions (~50% of the initial
ity. Moreover, the application of anesthesia to value), the NMES condition resulted in no change in
the skin overlying first dorsal interosseus re- the amplitudes of the short- and medium-latency
duced the amplitude of the central response responses, and an increase in the amplitude of the
(long-latency reflex in response to a fast stretch long-latency response. Augmentation of the long-
of the muscle) that was augmented by electrical latency response after NMES was attributed to
stimulation (60 –100 s) applied to the skin at an feedback transmitted by cutaneous receptors in
intensity less than motor threshold (10). These response to electrical stimulation, whereas the ab-
findings were collectively interpreted as indicat- sence of a change in the short- and medium-la-
ing that electrical stimulation applied over the tency responses was likely caused by the lack of a
muscle elicits action potentials in both muscle decrease in the responsiveness of the Ia afferent
and non-muscle afferents. spinal and supraspinal reflex pathways following
When the current (2.5–10 mA; 1-ms rectangular the NMES-evoked contraction.
pulses) applied over the nerve is less than that In addition to engaging short-latency spinal
needed to elicit an H reflex in soleus, the activated pathways, the synaptic input projects to interneu-
sensory axons can transmit sufficient excitatory rons that modulate the activity of motor neurons
synaptic input to motor neurons that results in innervating synergists and contralateral homolo-
some of them discharging action potentials. Dean gous muscles (7, 53, 66, 101, 102, 138). These ef-
et al. (33) found that the activated motor units fects can be observed when electrical stimulation is
began discharging action potentials at varying la- delivered through pads attached over the muscles
tencies (0.5–29.6 s) after the onset of the electrical of one arm while the same muscles in the other
stimulation, and these motor units were all re- arm perform a submaximal voluntary contraction.
cruited at low forces during voluntary contrac- Based on EMG signals recorded with a high-den-
tions. The recruitment latency (time from the onset sity electrode (4 ⫻ 8 detection points; 10-mm in-
of electrical stimulation) decreased with an in- terelectrode distance), for example, Hamilton et al.
crease in stimulus rate from 10 to 60 Hz during the (58) found that electrical stimulation (50 and 90
constant-frequency stimulation with no further re- Hz, 0.2 and 1.0 ms) applied to the right biceps brachii
ductions at 80 and 100 Hz. Discharge rate at re- influenced both the discharge times of motor units
cruitment was low (2–5 pps), but this increased to and the spatial distribution of EMG amplitude in the
a steady-state value (~8 pps) despite there being no left biceps brachii during a submaximal (10% MVC
increase in the applied current. The discharge force) isometric contraction. Although they found
times for 24% of the action potentials occurred at that the specific adjustments varied with the fre-
an H-reflex latency, whereas the timing of most quency, pulse width, and intensity of the applied
action potentials was unrelated to that of the stim- electrical stimulation, the most common response
ulus pulse. These findings suggested that the acti- was an increase in the activity of motor units in left
vation of sensory axons with low currents enabled biceps brachii, as indicated by an increase in ab-
adjustments in motor neuron excitability that re- solute EMG amplitude (mV). However, these ef-
sulted in the generation of action potentials. fects in the left biceps brachii were most often
When the sensory response elicited by electrical observed after the 10 s of electrical stimulation
stimulation enters the spinal cord, it is dispersed to applied to the right arm had ended, which is con-
both intraspinal networks and ascending path- sistent with other reports of the effects outlasting
ways. Modulation of these pathways differs for vol- the interval during which electrical stimulation is
untary actions and those evoked by electrical applied (7, 26, 33, 93).
stimulation. In response to a ramp-and-hold The sensory feedback generated by electrical
stretch of a muscle, the reflex pathways produce stimulation of muscle also reaches supraspinal
short-, medium-, and long-latency responses. After centers. For example, NMES applied to muscle can
a sustained MVC with a hand muscle that lasted increase the responsiveness of corticospinal path-
108 ⫾ 25 s, Balestra et al. (10) found that the am- ways, as demonstrated by changes in the amplitude
plitudes of the short- and medium-latency re- of the potentials evoked in muscle by transcranial
sponses due to muscle afferents engaging spinal and magnetic stimulation (TMS) applied over the motor
PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org 45
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
cortex (24, 73, 77, 84), but the effect appears to de- tant (vastus medialis, 36 ⫾ 3%) leg muscles, but there
pend on the frequency, duration, and intensity of the was no change in the amplitude of the potentials
stimulation (25, 57, 94). Also, the change in respon- evoked in either an adjacent hand muscle (first dor-
siveness appears to differ for arm and leg muscles. sal interosseus) or a muscle in the forearm (extensor
When NMES (100 Hz, 1 ms) was applied—the cur- carpi ulnaris) (FIGURE 4). These findings were inter-
rent was set to elicit an M wave equal to 15% of the preted as indicating that NMES had a more global
maximal value—for 40 min (20-s on, 20-s off) over effect on the cortical neurons that projected to motor
the common peroneal nerve (tibialis anterior) and neurons innervating the involved leg muscles than
over the median nerve (abductor pollicis brevis), those related to the engaged arm muscles.
Mang et al. (93) found that the amplitude of the The specific cortical adjustments elicited by a
motor evoked potential increased for both target single session of NMES, at least for targeted hand
muscles (tibialis anterior, 45 ⫾ 6%; abductor pollicis muscles (first dorsal interosseus), appear to in-
brevis, 56 ⫾ 8%) with mixed effects in other muscles. volve a reduction in short-latency inhibition and
The amplitude of the motor evoked potential in- an increase in short-latency facilitation (92).
creased in both adjacent (soleus, 47 ⫾ 5%) and dis- These effects were demonstrated by comparing
the amplitudes of motor evoked potentials before
A
14 and after a conditioning stimulus was applied to
the ulnar nerve at the level of the wrist before the
12 test stimulus (transcranial magnetic stimulation
MEP amplitude (% Mmax)
over the motor cortex). NMES eliminated the
10
short-latency depression (25%) in the conditioned
8 response and augmented (33%) the later condi-
tioned response, which suggests a net increase in
6 the excitation delivered by afferent fibers to corti-
cal neurons. Moreover, NMES (100 Hz, 1 ms) ap-
4
plied to a right forearm muscle (15% MVC force)
2
for 10 min (5-s on, 5-s off) has been shown to
increase the level of interhemispheric inhibition
0 from the left to the right primary motor cortex,
Before After Before After likely due to an increase in the excitability of tran-
Tibialis anterior Abducctor scallosal neurons in the left hemisphere (57). As
pollicis brevis
with the effects observed at the spinal level, the
central adjustments elicited by NMES of ⱖ40 min
B
continue after the stimulation has ended (26, 93,
135).
0.20 0.9
These studies demonstrate that the delivery of
an electric current through electrodes attached to
MEP amplitude (mV)
MEP amplitude (mV)
0.15 the skin over either a peripheral nerve or a limb
0.6 muscle can elicit action potentials in sensory axons
that are propagated into spinal and supraspinal
0.10 networks (16, 19, 24, 26, 27, 58, 63, 64, 73, 77, 81, 92,
93, 135). These central effects are evident whether
0.3
the applied current is greater than or less than the
0.05
threshold required to evoke a muscle contraction
(10, 25, 58, 156). A number of studies have demon-
0.00 0 strated that the adjustments elicited by the sensory
Before After Before After feedback vary with the stimulus parameters, such
Leg Hand as pulse width, frequency, current amplitude, and
electrode location. These findings raise the ques-
FIGURE 4. The amplitude of motor evoked potentials in leg and arm mus-
cles before and after NMES tion of which set of parameters can elicit clinically
The motor evoked potentials (MEPs) were evoked by transcranial magnetic stimulation meaningful adaptations (134).
applied over the appropriate areas in the motor cortex. NMES (100 Hz, 1 ms) was ap-
plied for 40 min over the common peroneal nerve (tibialis anterior) and the median
nerve (abductor pollicis brevis). A: MEP amplitude (normalized to maximal M-wave am-
plitude) increased by 45 ⫾ 6% for tibialis anterior and by 56 ⫾ 8% for abductor pollicis Rehabilitation
brevis after the application of NMES. B: MEP amplitude (mV) increased by an average
of 42 ⫾ 4% for both adjacent (soleus, 47 ⫾ 5%) and distant (vastus medialis, 36 ⫾ 3%) As indicated in the title of our paper, the second
leg muscles after NMES but did not change for either adjacent (first dorsal interosseus)
or distant (extensor carpi ulnaris) arm muscles. Data are from Ref. 93 and used with half of this review focuses on the rehabilitation po-
permission from Experimental Brain Research. tential of electrical stimulation applied to muscle.
46 PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
Moreover, we limit the discussion to non-invasive standardized exercises in inpatient (6 sessions in 3
approaches that are used to elicit sensorimotor ad- days), home (6 sessions in 2 days), and outpatient
aptations (99, 114, 117, 126, 129) and not electrical (10 –12 sessions in 6 wk) settings. In addition, one
nerve stimulation that is used to assist a specific group self-administered NMES (50 Hz, 0.25 ms;
function [functional electrical stimulation (FES)]. biphasic, symmetrical stimulus pulse) applied
For example, FES is used to supplement an inad- through large-pad electrodes attached to the skin
equate muscle activation during such actions as over the relaxed quadriceps muscle of the operated
toe clearance during the gait cycle (99, 134, 135, leg while seated. The protocol involved 15 evoked
137), the leg extension phase of cycling (13, 44) and contractions (15-s on, 45-s off) at the maximal tol-
rowing (40, 140), and reaching actions (59, 75). erated intensity. Evaluation sessions were per-
Despite its primary function, FES also engages sen- formed during the rehabilitation protocol (3.5 and
sory axons that distribute input throughout the 6.5 wk after the surgical procedure) and on three
nervous system and produce adaptations that are subsequent occasions (13, 26, and 52 wk).
evident when the device is not in use (59, 117, 131, At the primary end point (3.5 wk), the NMES
135). group exhibited less of a decline in the strength of
Similar to other investigators (126, 130, 142), we the quadriceps and hamstrings muscles and less of
distinguish between electrical-stimulation proto- a reduction in performance on three functional
cols in which the applied current exceeds motor tests (6-min walk, stair-climbing test, and timed
threshold and evokes a muscle contraction and up-and-go test). Subsequently, muscle strength re-
those for which the current is less than motor covered for both groups of participants but at 52
threshold and elicits action potentials primarily in wk remained significantly less for the control
sensory nerve fibers. When the intensity of the group relative to the NMES group (FIGURE 5). Sim-
applied current is sufficient to evoke a muscle con- ilarly, performance on the three functional tests
traction, the protocol is typically referred to as improved for both groups of participants, but the
NMES. In contrast, protocols that apply a lesser gains were greater for the NMES group. Although
current and largely engage sensory axons are the measure of muscle activation (doublet-inter-
known as transcutaneous electrical nerve stimula- polation technique) also improved for both groups
tion (TENS). of participants, NMES did not augment the capac-
ity of the nervous system to activate muscle as
Neuromuscular Electrical Stimulation indicated by the absence of a change in the level of
NMES is used most often in clinical settings to voluntary activation. Nonetheless, NMES greatly
recover skeletal muscle mass and function after a attenuated the decline in performance on the func-
period of reduced use (29, 37, 38, 87, 89, 150, 158), tional tests at the primary end point and aug-
but sometimes it is used in healthy individuals to mented the gains observed during the follow-up
augment the activation signal generated by the period (FIGURE 5C). Moreover, NMES improved
nervous system (43, 56, 143). Despite the benefits the increase in the strength of the hamstring mus-
that can be achieved with NMES treatments (121), cles, even though the treatment was applied to the
the approach is not effective for some clinical co- quadriceps muscle. These findings suggest that
horts, such as individuals who have undergone NMES elicited more global adaptations than those
cardiac valve surgery [no effect on gait speed or expected from the contractions evoked in the tar-
walking endurance (52)], those undergoing chemo- geted muscle. The protocol developed by Stevens-
therapy treatment for cancer [no effects on quad- Lapsley et al. (136) was subsequently expanded as
riceps muscle strength, thigh lean mass, or the recommended approach for using NMES to
physical activity (86)], those with mild-to-moder- restore quadriceps muscle function in individuals
ate osteoarthritis [no effect on quadriceps muscle who undergo an orthopedic procedure (133).
strength (109)], intensive care survivors [no effect Similar results have been obtained in other
on handgrip strength (112)], and critically ill pa- NMES intervention studies, even with different
tients [inability to elicit an adequate quadriceps stimulation parameters. For example, Almuklass et
muscle contraction (128)]. al. (5) performed a clinical trial in which they com-
As an example of an effective NMES protocol, pared the influence of two NMES protocols on the
Stevens-Lapsley et al. (136) performed a clinical gains in function experienced by persons living
trial to evaluate the capacity of NMES to attenuate with multiple sclerosis. Participants were ran-
the depression of muscle activation that is ob- domly assigned to receive a 6-wk treatment (18
served after total knee arthroplasty (145, 159). The sessions) of NMES applied at either 100 Hz with
60 participants were randomized into two groups 1-ms pulses or at 50 Hz with 0.26-ms pulses to the
that received standard-of-care rehabilitation either dorsiflexor and plantar flexor muscles of each leg.
alone (control group) or in combination with Each muscle group was stimulated for 10 min (4-s
NMES. All participants performed the same set of on, 12-s off) at the maximal tolerable intensity in
PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org 47
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
each session. There were no statistically significant
differences in the outcomes for the two groups of
participants, which indicates that the two NMES
protocols had similar effects on the primary out-
comes. The 6-wk intervention elicited clinically
significant improvements with moderate effect
sizes in gait speed (time to walk 25 ft.) and walking
endurance (distance walked in 6 min), and these
gains were still present at 4 wk after the interven-
tion. The NMES treatment increased muscle
strength for the dorsiflexors of the affected leg and
the plantar flexors of the less-affected leg, but not
the other muscles. Consistent with a global influ-
ence of NMES, the intervention improved self-re-
ported levels of fatigue and walking limitations and
the time to complete a pegboard test of manual
dexterity. However, there were no changes in the
daily level of physical activity and the self-reported
measure of disability status. Given that two of the
major symptoms associated with multiple sclerosis
are fatigue and walking limitations, the NMES in-
tervention was successful in reducing the burden
of the disease.
Mani et al. (95) used a similar approach to com-
pare the outcomes produced by the two NMES
protocols in healthy older adults (74 ⫾ 5 yr). The
NMES protocols were similar to those used by Al-
muklass et al. (5), and there were no statistically
significant differences in the outcomes exhibited
by the two groups of participants (100 Hz, 1 ms vs.
50 Hz, 0.26 ms). In contrast to the study on persons
with multiple sclerosis, the time course of the ad-
aptations elicited in older adults by the NMES in-
tervention varied across the outcome measures.
The primary outcomes were mobility tests, which
included gait speed (time to walk 10 m), walking
endurance (time to walk 400 m), and dynamic bal-
ance (chair-rise test and rapid step test). Gait speed
and walking endurance had improved midway
through the 6-wk intervention, with no further
changes at weeks 7 and 10. Performance on the two
tests of dynamic balance improved progressively
up to the end of the intervention (week 7), with no
FIGURE 5. Recovery of muscle function after to-
tal knee arthroplasty
The clinical trial involved two groups of participants who
performed standard rehabilitation exercises alone (con-
trol group) or in combination with NMES applied to the
quadriceps muscle of the operated leg. NMES (50 Hz,
0.25 ms) was applied to the relaxed quadriceps muscle
at the maximal tolerable intensity twice daily for 6
weeks. A: change in quadriceps strength (torque normal-
ized to body mass) across the 52-wk study, which in-
cluded the rehabilitation treatment (first two time points
after week 0) and follow-up. B: change in the strength of
the hamstring muscles. C: change in the test of walking
endurance (6-min test). *Statistically significant (P ⬍
0.05) differences between groups. Data (means ⫾ SE)
are from Ref. 136 and used with permission from Physi-
cal Therapy.
48 PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
further change during the 4-wk follow-up period. muscle NMES) or a control group for the 12-wk
The strength of the plantar flexor muscles (average intervention. NMES (80 Hz, 0.35 ms) was applied to
of both legs) was increased at the end of the inter- 8 –10 muscle groups concurrently in a single 20-
vention (week 7) and remained elevated at week 10. min (6-s on, 4-s off) session each week while par-
There were no statistically significant changes in ticipants performed six movements with minimal
the strength of the dorsiflexor, knee extensor, knee voluntary activity. The current was adjusted for
flexor, and hip flexor muscles. The changes in mo- each muscle group to achieve a rating of ⱖ “hard”
bility, therefore, seem to be unrelated to the peak on a Borg scale. The primary outcome was a self-
forces achieved during maximal isometric contrac- reported measure of pain intensity on a scale of 0
tions performed with these muscle groups. Sim- (no pain) to 10 (worst possible pain) during the last
ilarly, there were no statistically significant 4 weeks of the intervention. The pain score de-
changes in the amplitude of the force fluctua- creased significantly for the NMES group and was
tions during steady submaximal contractions accompanied by increases in the strength of the
with plantar flexor muscles, suggesting that the trunk extensor and flexor muscles. There were no
modulation of motor unit activity was not influ- statistically significant changes for the control
enced by the NMES intervention (48, 105, 141). group. Given that pain representations are local-
One of the noteworthy outcomes of these three ized to specific regions within the brain (77), the
studies (5, 95, 136) was that several weeks of NMES multiple-muscle NMES intervention must have
applied to leg muscles was able to elicit significant modulated the pathways and networks that con-
improvements in performance on clinical tests of tribute to the perception of pain.
motor function. In all three studies, the applied These NMES studies demonstrate that the appli-
current was passed between pairs of electrodes cation of electrical stimulation at an intensity suf-
attached to the skin over target muscles (knee ex- ficient to evoke a muscle contraction can elicit
tensors, plantar flexors, or dorsiflexors). An alter- improvements in tests of muscle function and
native approach is to increase the number of performance on tests of motor function. The re-
stimulation sites by placing multiple electrodes sults suggest that many of the adaptations elic-
over a single muscle group (50, 104, 121) or attach- ited by the treatment occur within the nervous
ing pairs of electrodes over many muscles (9, 11, system, but little is known about the specific
51). Two examples illustrate the types of adapta- changes underlying the gains in function and
tions that can be achieved with this approach. why the time course of the improvements varies
The first example demonstrates the capacity of across outcome variables.
multiple-muscle NMES to improve performance of
healthy individuals. The study compared the gains
Transcutaneous Electrical Nerve
achieved by sedentary adults (48 ⫾ 12 yr) after a
Stimulation
6-wk intervention that involved five 1-h training Transcutaneous electrical nerve stimulation (TENS)
sessions each week (11). NMES (rhythmic contrac- is a form of stimulation in which the applied elec-
tions at 4 Hz) was delivered through large elec- trical current is constrained to engage sensory
trodes embedded in tight-fitting shorts that evoked nerve fibers with no more than minimal evoked
contractions in the quadriceps, hamstrings, glu- muscle contractions. When the current is set at
teal, and calf muscles. Stimulus intensity was con- around motor threshold (slightly above or below),
strained by subject tolerance and an increase in it elicits action potentials in a wide range of muscle
heart rate of no more than 90% of heart-rate re- and non-muscle sensory axons (103, 110, 118, 153).
serve during prescribed exercises. The intervention With mixed success, it is used clinically at various
elicited increases in peak oxygen consumption frequencies [1–150 Hz (147)] to manage pain (106,
(10.9 ⫾ 8.5%) during a treadmill test of aerobic ca- 120), spasticity (47, 115, 132), and urinary inconti-
pacity, walking endurance (6-min walk; 7.5 ⫾ nence (142, 144). In this review, we briefly discuss
4.0%), and the strength of the quadriceps muscles an additional application of TENS when it is ap-
(27 ⫾ 22%). One critical feature of this study was plied to limb muscles: its capacity to improve sen-
that the response of each participant to the appli- sorimotor function.
cation of NMES to multiple muscles was regulated As a rehabilitation technique, TENS can be used
by trained personnel. Care is necessary with this to augment sensory feedback during the perfor-
approach, since unsupervised use of multi-muscle mance of an action (18, 31, 78, 130, 147, 153) or it
NMES systems has been reported to produce rhab- can be used as a treatment to modify neural path-
domyolysis in some individuals (72, 91). ways and networks that are engaged during pre-
The second example involves that application of scribed tasks (23, 36, 127). As an example of using
multiple-muscle NMES to individuals with chronic TENS to augment sensory feedback during an ac-
low-back pain (155). Participants were randomly tion, Almuklass and colleagues (4) assessed the
assigned to either a treatment group (multiple- influence of TENS (50 Hz, 0.2 ms) applied to the leg
PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org 49
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
muscles of persons with multiple sclerosis (MS) on significant improvements (FIGURE 6) in gait speed,
their performance of standard clinical tests. Some walking endurance, and dynamic balance for the
of the earliest signs of the damage caused by MS MS group (52 ⫾ 8 yr). There were no statistically
are changes in sensory function, which in the legs significant effects for the control group (52 ⫾ 9 yr),
is reported as numbness, tingling, pins-and-nee- except for an improvement in walking endurance
dles, and sleepy leg (8, 14, 139). The significance of (distance walked in 6 min). The specific adjust-
the sensory impairments is underscored by find- ments underlying these transient improvements in
ings of meaningful associations between loss of mobility remain to be determined.
sensation and declines in motor function, such as Work on the capacity of TENS to modify neural
decreases in vibration sensation and increases in pathways and networks has examined the influ-
the time to walk 25 ft. over a 2-year period (162). ence of its application either immediately before
Critically, much of the variance in vibration sensa- performing a prescribed task or as a treatment
tion was explained (R2 ⫽ 0.54) by MRI-detected administered over several sessions. Cohen and col-
abnormalities in the dorsal column and diagnosis leagues have performed several studies in which
subtype (161), which suggests that the accumula- they assessed the influence of a single session of
tion of sensorimotor disabilities in MS is strongly prolonged electrical nerve stimulation on hand-
associated with spinal cord abnormalities (34). arm function in stroke survivors (23, 156). The
The rehabilitation potential of targeting sensory TENS was delivered through electrodes attached to
axons was assessed by Almuklass et al. (4) when the skin over peripheral nerves (median, radial,
they compared the influence of TENS on the and ulnar) of the paretic hand and leg (peroneal,
performance of individuals with MS who had mild- sural, and tibial nerves) at an intensity just below
to-moderate levels of disability with an age- and (156) or above (23) motor threshold. The electrical
sex-matched control group on measures of gait stimulation involved bursts of 5 pulses (1 ms each)
speed (time to walk 25 ft.), walking endurance (dis- at 10 Hz (0.5 s of stimulation) once each second for
tance walked in 6 min), and dynamic balance 2 h. The primary functional outcome was the time
(chair-rise test). TENS (50 Hz, 0.2 ms) was deliv- to complete the Jebsen-Taylor Hand Function
ered through large electrodes attached to the skin Test, which comprises seven tests that quantify
over the ankle dorsiflexor muscles and the anterior manipulation and dexterity. Time to complete the
thigh muscles of the more affected leg and was test was reduced immediately after the electrical
applied continuously during the performance of nerve stimulation and at 1 and 24 h later, with the
each test. The intensity was set at just above motor greatest improvements exhibited by those partici-
threshold and was applied continuously during the pants with more pronounced impairments. More-
performance of each test. The increase in sensory over, the benefit was observed only when the
feedback elicited by TENS produced clinically stimulation was applied at two sites on the arm
concurrently and not when it was applied to the
paretic leg. Consistent with other studies on the
central effects of TENS (60, 88), Celnik et al. (23)
found that their protocol of electrical nerve stim-
ulation reduced the TMS-estimated level of short-
interval intracortical inhibition, which is mediated
by GABAergic neurotransmission. A subsequent
study found that the improvement in the accuracy
of a tracking task by healthy adults after applica-
tion of this TENS protocol for 20 min was accom-
panied by increases in EEG-derived estimates of
activity and connectivity within the sensorimotor
cortex (151).
In a series of studies on several different cohorts,
FIGURE 6. Percent changes in clinical outcomes elicited by TENS in per- Dinse and colleagues have examined the effective-
sons with multiple sclerosis ness of somatosensory stimulation applied to the
The green bars show statistically significant differences (means ⫾ SE) in performance
for 13 individuals between a sham condition and when each test is completed with the fingertips on arm and hand function (71, 85, 127).
concurrent application of TENS (4). Positive values denote an improvement in perfor- In one of these studies, Kattenstroth et al. (71)
mance. The blue bars show the change from before to after a 3-wk intervention (9 ses- assessed the influence of 10 sessions of a TENS
sions) for 12 individuals (3). The 25-ft. data indicate maximal gait speed; the 6-min
values are the distance walked in 6 min (4) or 2 min (3); the Chair scores are for the protocol on the motor function of individuals in
chair-rise test; GPT refers to the grooved pegboard test; fatigue was measured with the subacute phase after a unilateral ischemic
the Modified Fatigue Impact Scale; and Walking refers to the self-reported assessment stroke. The study involved two groups: a TENS
of walking limitations (Multiple Sclerosis Walking Scale-12). With the exception of the
GPT, all changes (blue bars) were statistically significant. Data are from Refs. 3, 4 and group and a sham group. TENS was applied to
used with permission from the American Society of Biomechanics. the fingertips of the more-affected hand and
50 PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
comprised bursts (1.4-s on, 5-s off) of electrical for durations that range from 15 min to 2 h (36,
stimuli (20 Hz, 0.2 ms) at an intensity above sen- 151, 156) or as an intervention administered for
sory threshold (median nerve: 10.0 ⫾ 3.9 mA; ulnar several weeks (3). Also, it requires an appropriate
nerve: 6.7 ⫾ 3.5 mA) for 45 min each session. The placement of the stimulating electrodes (4, 23,
outcomes included measures of light-touch and 156). For example, synchronous activation of the
tactile discrimination, proprioception, dexterity, median and ulnar nerves elicited more beneficial
grip force, and the Jebsen-Taylor Hand Function effects on motor function than did electrical stim-
Test. The TENS group experienced significantly ulation applied to one nerve (23). Moreover, the
greater improvements in all measures of sensori- TENS electrodes need to be placed over the weak-
motor function, but the effect size (Cohen’s est muscles of the more affected leg of individuals
d ⫽ 0.72) was greatest for the measures of sensory with multiple sclerosis to elicit clinically significant
function (tactile performance). There were also sig- improvements in walking performance (4). Criti-
nificant improvements in motor function, as re- cally, the responsiveness of axons and neuromus-
ported in a parallel study by the same group (85). cular junctions tends to decline with prolonged
Consistent with the results reported for a single high-frequency stimulation (74, 107), which neces-
TENS session (23), the gains experienced by the sitates some variability in the stimulus protocol
participants were greater for those who were more (31). This diversity of protocols suggests that some
impaired (71). work is needed to identify the optimal set of pa-
In contrast to employing TENS as a stand-alone rameters needed to elicit clinically meaningful ad-
treatment, Shimodozono et al. (130) assessed the aptations in specific cohorts.
influence of the concurrent application of TENS (20 Although some studies have explored the under-
Hz, 0.25 ms) during the performance of therapeutic lying neurophysiology responsible for the benefits
exercises by individuals with severe impairments in achieved with TENS, these have largely focused on
arm function due to post-stroke hemiplegia. The changes at the cortical level (18, 30, 85, 127, 151).
4-wk treatment, which was performed 40 min/day Given the capacity of TENS to improve motor func-
on 5 days/wk (20 sessions), comprised 100 –150 tion, the gains must be mediated by adjustments in
repetitions of standardized movements about the the output from the spinal cord. Work is needed to
shoulder, elbow, and wrist joints of the affected characterize the changes in muscle activation pro-
arm. TENS was applied continuously during the duced by TENS and then to determine the path-
exercises at an intensity slightly above motor ways and networks that are modulated by TENS to
threshold, similar to the protocol used by Al- generate the observed gains.
muklass et al. (4). The primary outcome was the
change in the Fugl-Meyer Assessment Scale for the Future Directions
arm, with secondary outcomes being the range of
motion about the involved joints. The group that Whether the current applied during electrical stim-
performed the exercises with TENS experienced a ulation is greater than (NMES) or less than (TENS)
clinically significant improvement in the Fugl- motor threshold, it is capable of improving senso-
Meyer score, whereas the change for the group that rimotor function in healthy adults and some clin-
performed exercises without TENS did not differ ical cohorts. The key issues that need to be
from that for the control group. Also, the TENS resolved include identifying the stimulation details
group exhibited a significant increase in the range that maximize the benefits associated with each
of motion for elbow extension but not for shoulder protocol and characterizing the adaptations un-
flexion or wrist flexion. The gains, however, were derlying the improvements in performance.
not accompanied by changes in the scores for Although electrical stimulation—especially NMES—
spasticity. is typically applied when the person is not active
These studies on the effectiveness of TENS indi- (3, 5, 95, 136), some studies suggest that the gains
cate that the outcomes are relatively insensitive to may be more substantial when the intervention is
the duration of the stimulus pulse (range: 0.05–1.0 applied during the performance of prescribed ac-
ms), stimulus frequency (range: 10 –50 Hz), and the tions (147). In some of these studies, the stimula-
intensity of the applied current, provided it evokes tion is synchronized with a particular event in the
no more than weak contractions (23, 80, 156). action (18), whereas, in other studies, the stimula-
However, other details of the protocol appear to be tion is applied continuously (21, 29, 51, 130, 153).
more critical. For example, some studies have The relative capacity of these two approaches to
found that the outcomes are beneficial when TENS elicit clinically significant adaptations remains to
is applied continuously during an action (4, 18, be determined. Moreover, it would be of interest
130, 153), whereas others have observed significant to determine the degree of similarity between the
gains when TENS is delivered in low-frequency adjustments elicited in a single session in which
bursts of pulses during a conditioning treatment the electrical stimulation is applied concurrently
PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org 51
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
during the performance of an action and the tion. However, we know essentially nothing about
adaptations evoked by several sessions of NMES these interactions. In contrast, our knowledge on
or TENS (FIGURE 6). pain is much more advanced as methods are being
The studies cited in our review indicate that the developed that can derive predictive models from
rehabilitation potential of electrical stimulation neuroimaging data to interpret mental constructs
can range from the modulation of motor function (79). A parallel approach would generate new knowl-
in various groups of individuals to the reduction in edge on fatigue and its modulation by electrical stim-
symptom severity in clinical cohorts. In the sim- ulation of muscle.
plest case, it is not surprising that several sessions Clinical and experimental findings have demon-
of NMES can increase the strength of target mus- strated that electrical stimulation can provide a
cles (6, 11, 28, 43, 50, 136), but this result can be number of therapeutic benefits, underscoring its
quite variable (4, 21, 39, 95, 122). Although the utility as a rehabilitation tool. Although some at-
strength gains appear to be mediated by increases tempts have been made to standardize effective
in the level of muscle activation (6, 39, 70, 90), protocols (133), many of the details remain to be
several weeks of NMES can induce adaptations in established. Critically, our understanding of the re-
muscle-fiber properties (55, 152). One unexpected sponses elicited in the nervous system by the appli-
outcome of these interventions is the capacity of cation of electrical stimulation to muscle is quite
NMES to increase the strength of non-targeted rudimentary. 䡲
muscles. For example, an NMES protocol that tar-
geted the knee extensor muscles increased the No conflicts of interest, financial or otherwise, are de-
strength of both the knee extensors and knee flex- clared by the author(s).
R.M.E. and J.D. conceived and designed the review;
ors (136). Similarly, NMES training of the dorsi-
R.M.E. and J.D. prepared figures; R.M.E. and J.D. drafted
flexor muscles resulted in an increase in the EMG manuscript; R.M.E., I.G.A., and J.D. edited and revised
activity of medial gastrocnemius during the perfor- manuscript; R.M.E., I.G.A., and J.D. approved final version
mance of postural tasks (6). Even the strength of of manuscript.
muscles in the contralateral limb can be increased
by the application of NMES to one limb (17, 65).
Moreover, the application of NMES to leg muscles, References
whether in the thigh or the lower leg, can improve 1. Adams GR, Harris RT, Woodard D, Dudley GA. Mapping of
performance on a test of walking endurance (6- electrical muscle stimulation using MRI. J Appl Physiol (1985)
74: 532–537, 1993. doi:10.1152/jappl.1993.74.2.532.
min walk) (4, 11, 95, 136, 152), which suggests the
2. Adrian ED, Bronk DW. The discharge of impulses in motor
improvements in mobility involve other adapta- nerve fibres: part I. Impulses in single fibres of the phrenic
tions besides increases in muscle strength. Rela- nerve. J Physiol 66: 81–101, 1928. doi:10.1113/jphysiol.1928.
sp002509.
tively few studies, however, have probed the
3. Alenazy M, Petrigna L, Feka K, Alvarez E, Almuklass AM,
physiological adaptations responsible for these off- Enoka RM. Electrical stimulation of sensory nerves improves
target improvements in function. mobility and balance in persons with multiple sclerosis. In:
Annual Meeting of the American Society of Biomechanics,
Even more interesting is the capacity of low lev- Calgary, Canada, July 31–August 3, 2019. American Society
els of electrical nerve stimulation to reduce the of Biomechanics, 2019.
intensity of self-reported symptoms, such as pain 4. Almuklass AM, Capobianco RA, Feeney DF, Enoka RM. Sen-
sory stimulation can improve motor function in individuals
and fatigue. TENS can be effective in some clinical with multiple sclerosis. In: Annual Meeting of the American
settings for the treatment of pain (32, 119, 146), Society of Biomechanics. University of Colorado Boulder,
August 8 –11, 2017.
which it accomplishes by evoking the local release
5. Almuklass AM, Davis L, Hamilton LD, Hebert JR, Alvarez E,
of opioids to dampen inflammation-induced hy- Enoka RM. Pulse width does not influence the gains
peralgesia (123, 148) and activating central inhibi- achieved with neuromuscular electrical stimulation in peo-
ple with multiple sclerosis: double-blind, randomized trial.
tory pathways (32, 35). Although both NMES and Neurorehabil Neural Repair 32: 84 –93, 2018. doi:10.1177/
TENS can reduce self-reported levels of fatigue in 1545968317753681.
various groups of individuals (FIGURE 6) (3, 5, 29, 6. Amiridis I, Arabatzi F, Violaris P, Stavropoulos E, Hatzitaki V.
Static balance improvement in elderly after dorsiflexors elec-
32, 95), much less is known about the adaptations trostimulation training. Eur J Appl Physiol 94: 424 – 433,
responsible for a decrease in the level of fatigue. 2005. doi:10.1007/s00421-005-1326-3.
Current taxonomies of fatigue suggest that the 7. Amiridis IG, Mani D, Almuklass A, Matkowski B, Gould JR,
Enoka RM. Modulation of motor unit activity in biceps brachii
level of fatigue reported by an individual can be by neuromuscular electrical stimulation applied to the con-
modulated by factors that contribute to perceived tralateral arm. J Appl Physiol (1985) 118: 1544 –1552, 2015.
doi:10.1152/japplphysiol.00031.2015.
and performance-based measures of fatigability
8. Aydar G, Kurt S, Karaer Unaldi H, Erkorkmaz U. Restless legs
(45, 163). Of these two domains, it seems more syndrome in multiple sclerosis. Eur Neurol 65: 302–306,
likely that the factors contributing to perceived fa- 2011. doi:10.1159/000327315.
tigability—maintenance of homeostasis and psycho- 9. Babault N, Cometti G, Bernardin M, Pousson M, Chatard JC.
logical state—are the ones that respond to the Effects of electromyostimulation training on muscle strength
and power of elite rugby players. J Strength Cond Res 21:
sensory feedback associated with electrical stimula- 431– 437, 2007.
52 PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
10. Balestra C, Duchateau J, Hainaut K. Effects of 24. Charlton CS, Ridding MC, Thompson PD, Miles 38. Dirks ML, Wall BT, Snijders T, Ottenbros CL,
fatigue on the stretch reflex in a human muscle. TS. Prolonged peripheral nerve stimulation in- Verdijk LB, van Loon LJ. Neuromuscular electrical
Electroencephalogr Clin Neurophysiol 85: 46 – duces persistent changes in excitability of human stimulation prevents muscle disuse atrophy dur-
52, 1992. doi:10.1016/0168-5597(92)90101-G. motor cortex. J Neurol Sci 208: 79 – 85, 2003. ing leg immobilization in humans. Acta Physiol
doi:10.1016/S0022-510X(02)00443-4. (Oxf) 210: 628 – 641, 2014. doi:10.1111/apha.
11. Banerjee P, Caulfield B, Crowe L, Clark A. Pro- 12200.
longed electrical muscle stimulation exercise im- 25. Chipchase LS, Schabrun SM, Hodges PW. Cor-
proves strength and aerobic capacity in healthy ticospinal excitability is dependent on the pa- 39. Doucet BM, Griffin L. High versus low-frequency
sedentary adults. J Appl Physiol (1985) 99: 2307– rameters of peripheral electric stimulation: a stimulation effects on fine motor control in
2311, 2005. doi:10.1152/japplphysiol.00891.2004. preliminary study. Arch Phys Med Rehabil 92: chronic hemiplegia: a pilot study. Top Stroke Re-
1423–1430, 2011. doi:10.1016/j.apmr.2011.01. habil 20: 299 –307, 2013. doi:10.1310/tsr2004-
12. Barss TS, Ainsley EN, Claveria-Gonzalez FC, Luu 011. 299.
MJ, Miller DJ, Wiest MJ, Collins DF. Utilizing
physiological principles of motor unit recruitment 26. Christova M, Rafolt D, Golaszewski S, Nardone R, 40. Draghici AE, Picard G, Taylor JA, Shefelbine SJ.
to reduce fatigability of electrically-evoked con- Gallasch E. Electrical stimulation during skill Assessing kinematics and kinetics of functional
tractions: a narrative review. Arch Phys Med Re- training with a therapeutic glove enhances the electrical stimulation rowing. J Biomech 53: 120 –
habil 99: 779 –791, 2018. doi:10.1016/j.apmr. induction of cortical plasticity and has a positive 126, 2017. doi:10.1016/j.jbiomech.2017.01.007.
2017.08.478. effect on motor memory. Behav Brain Res 270:
171–178, 2014. doi:10.1016/j.bbr.2014.05.014. 41. Du Bois-Reymond E. Vorläufiger Abriss einer Un-
13. Bauer P, Krewer C, Golaszewski S, Koenig E, tersuchung über den sogenannten Froschstrom
Müller F. Functional electrical stimulation-as- 27. Collins DF, Burke D, Gandevia SC. Sustained con- und über die elektromotorischen Fische. Ann Phys
sisted active cycling–therapeutic effects in pa- tractions produced by plateau-like behaviour in 58: 1–30, 1843. doi:10.1002/andp.18431340102.
tients with hemiparesis from 7 days to 6 months human motoneurones. J Physiol 538: 289 –301,
after stroke: a randomized controlled pilot study. 2002. doi:10.1113/jphysiol.2001.012825. 42. Duchateau J, Enoka RM. Human motor unit re-
Arch Phys Med Rehabil 96: 188 –196, 2015. doi: cordings: origins and insight into the integrated
10.1016/j.apmr.2014.09.033. 28. Colson SS, Martin A, Van Hoecke J. Effects of motor system. Brain Res 1409: 42– 61, 2011. doi:
electromyostimulation versus voluntary isometric 10.1016/j.brainres.2011.06.011.
14. Beiske AG, Pedersen ED, Czujko B, Myhr KM. training on elbow flexor muscle strength. J Elec-
Pain and sensory complaints in multiple sclerosis. tromyogr Kinesiol 19: e311– e319, 2009. doi:10. 43. Duchateau J, Hainaut K. Training effects of sub-
Eur J Neurol 11: 479 – 482, 2004. doi:10.1111/j. 1016/j.jelekin.2008.05.009. maximal electrostimulation in a human muscle.
1468-1331.2004.00815.x. Med Sci Sports Exerc 20: 99 –104, 1988. doi:10.
29. Coote S, Hughes L, Rainsford G, Minogue C, 1249/00005768-198802000-00015.
15. Bergquist AJ, Clair JM, Collins DF. Motor unit re- Donnelly A. Pilot randomized trial of progressive
cruitment when neuromuscular electrical stimula- resistance exercise augmented by neuromuscu- 44. Edwards T, Motl RW, Sebastião E, Pilutti LA. Pilot
tion is applied over a nerve trunk compared with a lar electrical stimulation for people with multiple randomized controlled trial of functional electri-
muscle belly: triceps surae. J Appl Physiol (1985) sclerosis who use walking aids. Arch Phys Med cal stimulation cycling exercise in people with
110: 627– 637, 2011. doi:10.1152/japplphysiol. Rehabil 96: 197–204, 2015. doi:10.1016/j.apmr. multiple sclerosis with mobility disability. Mult
01103.2010. 2014.09.021. Scler Relat Disord 26: 103–111, 2018. doi:10.
1016/j.msard.2018.08.020.
16. Bergquist AJ, Wiest MJ, Collins DF. Motor unit 30. Cuypers K, Leenus DJF, van den Berg FE, Levin
recruitment when neuromuscular electrical stim- O, Thijs H, Swinnen SP, Meesen RLJ. Long-term 45. Enoka RM, Duchateau J. Translating fatigue to hu-
ulation is applied over a nerve trunk compared TENS treatment decreases cortical motor repre- man performance. Med Sci Sports Exerc 48: 2228 –
with a muscle belly: quadriceps femoris. J Appl sentation in multiple sclerosis. Neuroscience 250: 2238, 2016. doi:10.1249/MSS.0000000000000929.
Physiol (1985) 113: 78 – 89, 2012. doi:10.1152/ 1–7, 2013. doi:10.1016/j.neuroscience.2013.06.
japplphysiol.00074.2011. 046. 46. Enoka RM, Duchateau J. Rate coding and the
control of muscle force. Cold Spring Harb Per-
17. Bezerra P, Zhou S, Crowley Z, Brooks L, Hooper 31. Cuypers K, Levin O, Thijs H, Swinnen SP, spect Med 7: a029702, 2017. doi:10.1101/
A. Effects of unilateral electromyostimulation su- Meesen RLJ. Long-term TENS treatment im- cshperspect.a029702.
perimposed on voluntary training on strength proves tactile sensitivity in MS patients. Neu-
and cross-sectional area. Muscle Nerve 40: 430 – rorehabil Neural Repair 24: 420 – 427, 2010. 47. Estes SP, Iddings JA, Field-Fote EC. Priming neu-
437, 2009. doi:10.1002/mus.21329. doi:10.1177/1545968309356301. ral circuits to modulate spinal reflex excitability.
Front Neurol 8: 17, 2017. doi:10.3389/fneur.
18. Bisio A, Avanzino L, Gueugneau N, Pozzo T, Rug- 32. Dailey DL, Rakel BA, Vance CGT, Liebano RE, 2017.00017.
geri P, Bove M. Observing and perceiving: a Amrit AS, Bush HM, Lee KS, Lee JE, Sluka KA.
combined approach to induce plasticity in human Transcutaneous electrical nerve stimulation re- 48. Feeney DF, Mani D, Enoka RM. Variability in com-
motor cortex. Clin Neurophysiol 126: 1212–1220, duces pain, fatigue and hyperalgesia while re- mon synaptic input to motor neurons modulates
2015. doi:10.1016/j.clinph.2014.08.024. storing central inhibition in primary fibromyalgia. both force steadiness and pegboard time in
Pain 154: 2554 –2562, 2013. doi:10.1016/j.pain. young and older adults. J Physiol 596: 3793–
19. Blouin JS, Walsh LD, Nickolls P, Gandevia SC. 2013.07.043. 3806, 2018. doi:10.1113/JP275658.
High-frequency submaximal stimulation over
muscle evokes centrally generated forces in 33. Dean JC, Clair-Auger JM, Lagerquist O, Collins 49. Feiereisen P, Duchateau J, Hainaut K. Motor unit
human upper limb skeletal muscles. J Appl DF. Asynchronous recruitment of low-threshold recruitment order during voluntary and electri-
Physiol (1985) 106: 370 –377, 2009. doi:10. motor units during repetitive, low-current stimu- cally induced contractions in the tibialis anterior.
1152/japplphysiol.90939.2008. lation of the human tibial nerve. Front Hum Neu- Exp Brain Res 114: 117–123, 1997. doi:10.1007/
rosci 8: 1002, 2014. doi:10.3389/fnhum.2014. PL00005610.
20. Botter A, Oprandi G, Lanfranco F, Allasia S, 01002.
Maffiuletti NA, Minetto MA. Atlas of the muscle 50. Feil S, Newell J, Minogue C, Paessler HH. The
motor points for the lower limb: implications for 34. DeLuca GC, Alterman R, Martin JL, Mittal A, effectiveness of supplementing a standard re-
electrical stimulation procedures and electrode Blundell S, Bird S, Beale H, Hong LS, Esiri MM. habilitation program with superimposed neuro-
positioning. Eur J Appl Physiol 111: 2461–2471, Casting light on multiple sclerosis heterogeneity: muscular electrical stimulation after anterior
2011. doi:10.1007/s00421-011-2093-y. the role of HLA-DRB1 on spinal cord pathology. cruciate ligament reconstruction: a prospec-
Brain 136: 1025–1034, 2013. doi:10.1093/brain/ tive, randomized, single-blind study. Am J
21. Broekmans T, Roelants M, Feys P, Alders G, awt031. Sports Med 39: 1238 –1247, 2011. doi:10.1177/
Gijbels D, Hanssen I, Stinissen P, Eijnde BO. 0363546510396180.
Effects of long-term resistance training and si- 35. DeSantana JM, Da Silva LFS, De Resende MA,
multaneous electro-stimulation on muscle Sluka KA. Transcutaneous electrical nerve stimu- 51. Filipovic A, Grau M, Kleinöder H, Zimmer P, Hol-
strength and functional mobility in multiple lation at both high and low frequencies activates lmann W, Bloch W. Effects of whole-body elec-
sclerosis. Mult Scler 17: 468 – 477, 2011. doi:10. ventrolateral periaqueductal grey to decrease trostimulation program on strength, sprinting,
1177/1352458510391339. mechanical hyperalgesia in arthritic rats. Neuro- jumping, and kicking capacity of elite soccer
science 163: 1233–1241, 2009. doi:10.1016/j. players. J Sports Sci Med 15: 639 – 648, 2016.
22. Buckmire AJ, Arakeri TJ, Reinhard JP, Fuglevand neuroscience.2009.06.056.
AJ. Mitigation of excessive fatigue associated 52. Fontes Cerqueira TC, Cerqueira Neto ML, Cacau
with functional electrical stimulation. J Neural 36. Dickstein R, Kafri M. Effects of antecedent TENS LAP, Oliveira GU, Silva Júnior WMD, Carvalho
Eng 15: 066004, 2018. doi:10.1088/1741-2552/ on EMG activity of the finger flexor muscles and VO, Mendonça JT, Santana Filho VJ. Ambulation
aade1c. on grip force. Somatosens Mot Res 25: 139 –146, capacity and functional outcome in patients un-
2008. doi:10.1080/08990220802131416. dergoing neuromuscular electrical stimulation af-
23. Celnik P, Hummel F, Harris-Love M, Wolk R, Co- ter cardiac valve surgery: a randomised clinical
hen LG. Somatosensory stimulation enhances the 37. Di Filippo ES, Mancinelli R, Marrone M, Doria C, trial. Medicine (Baltimore) 97: e13012, 2018. doi:
effects of training functional hand tasks in pa- Verratti V, Toniolo L, Dantas JL, Fulle S, Pi- 10.1097/MD.0000000000013012.
tients with chronic stroke. Arch Phys Med Rehabil etrangelo T. Neuromuscular electrical stimulation
88: 1369 –1376, 2007. doi:10.1016/j.apmr.2007. improves skeletal muscle regeneration through
08.001. satellite cell fusion with myofibers in healthy el-
derly subjects. J Appl Physiol (1985) 123: 501–
512, 2017. doi:10.1152/japplphysiol.00855.2016.
PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org 53
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
53. Gajewska-Woźniak O, Grycz K, Czarkowska- 68. Hultman E, Sjöholm H, Jäderholm-Ek I, Krynicki J. 83. Liddell EGT, Sherrington CS. Recruitment and
Bauch J, Skup M. Electrical stimulation of low- Evaluation of methods for electrical stimulation some other factors of reflex inhibition. Proc R Soc
threshold proprioceptive fibers in the adult rat of human skeletal muscle in situ. Pflugers Arch Lond B 97: 488 –518, 1925. doi:10.1098/rspb.
increases density of glutamatergic and cholin- 398: 139 –141, 1983. doi:10.1007/BF00581062. 1925.0016.
ergic terminals on ankle extensor ␣-motoneu-
rons. PLoS One 11: e0161614, 2016. doi:10. 69. Jones KE, Hamilton AF, Wolpert DM. Sources of 84. Liu H, Au-Yeung SSY. Corticomotor excitability
1371/journal.pone.0161614. signal-dependent noise during isometric force effects of peripheral nerve electrical stimulation
production. J Neurophysiol 88: 1533–1544, 2002. to the paretic arm in stroke. Am J Phys Med
54. Gobbo M, Gaffurini P, Bissolotti L, Esposito F, doi:10.1152/jn.2002.88.3.1533. Rehabil 96: 687– 693, 2017. doi:10.1097/PHM.
Orizio C. Transcutaneous neuromuscular electri- 0000000000000748.
cal stimulation: influence of electrode positioning 70. Jubeau M, Zory R, Gondin J, Martin A, Maffiuletti
and stimulus amplitude settings on muscle re- NA. Late neural adaptations to electrostimula- 85. Lotze M, Ladda AM, Roschka S, Platz T, Dinse
sponse. Eur J Appl Physiol 111: 2451–2459, tion resistance training of the plantar flexor mus- HR. Priming hand motor training with repetitive
2011. doi:10.1007/s00421-011-2047-4. cles. Eur J Appl Physiol 98: 202–211, 2006. doi: stimulation of the fingertips: performance gain
10.1007/s00421-006-0264-z. and functional imaging of training effects. Brain
55. Gondin J, Brocca L, Bellinzona E, D’Antona G, Stimul 10: 139 –146, 2017. doi:10.1016/j.brs.
Maffiuletti NA, Miotti D, Pellegrino MA, Bottinelli 71. Kattenstroth JC, Kalisch T, Sczesny-Kaiser M, 2016.10.004.
R. Neuromuscular electrical stimulation training Greulich W, Tegenthoff M, Dinse HR. Daily repet-
induces atypical adaptations of the human skel- itive sensory stimulation of the paretic hand for 86. Maddocks M, Halliday V, Chauhan A, Taylor V,
etal muscle phenotype: a functional and pro- the treatment of sensorimotor deficits in patients Nelson A, Sampson C, Byrne A, Griffiths G, Wil-
teomic analysis. J Appl Physiol (1985) 110: 433– with subacute stroke: RESET, a randomized, cock A. Neuromuscular electrical stimulation of
450, 2011. doi:10.1152/japplphysiol.00914.2010. sham-controlled trial. BMC Neurol 18: 2, 2018. the quadriceps in patients with non-small cell
doi:10.1186/s12883-017-1006-z. lung cancer receiving palliative chemotherapy: a
56. Gondin J, Cozzone PJ, Bendahan D. Is high-fre- randomized phase II study. PLoS One 8: e86059,
quency neuromuscular electrical stimulation a 72. Kemmler W, Froelich M, von Stengel S, Kleinöder 2013. doi:10.1371/journal.pone.0086059.
suitable tool for muscle performance improve- H. Whole-body electromyostimulation – the need
ment in both healthy humans and athletes? Eur J for common sense! Rationale and guideline for a 87. Maddocks M, Nolan CM, Man WD, Polkey MI,
Appl Physiol 111: 2473–2487, 2011. doi:10.1007/ safe and effective training. Dtsch Z Sportmed 67: Hart N, Gao W, Rafferty GF, Moxham J, Higgin-
s00421-011-2101-2. 218 –221, 2016. doi:10.5960/dzsm.2016.246. son IJ. Neuromuscular electrical stimulation to
improve exercise capacity in patients with severe
57. Gueugneau N, Grosprêtre S, Stapley P, Lepers R. 73. Khaslavskaia S, Ladouceur M, Sinkjaer T. Increase COPD: a randomised double-blind, placebo-con-
High-frequency neuromuscular electrical stimula- in tibialis anterior motor cortex excitability fol- trolled trial. Lancet Respir Med 4: 27–36, 2016.
tion modulates interhemispheric inhibition in lowing repetitive electrical stimulation of the doi:10.1016/S2213-2600(15)00503-2.
healthy humans. J Neurophysiol 117: 467– 475, common peroneal nerve. Exp Brain Res 145:
2017. doi:10.1152/jn.00355.2016. 309 –315, 2002. doi:10.1007/s00221-002-1094-9. 88. Maeda Y, Lisi TL, Vance CG, Sluka KA. Release of
GABA and activation of GABA(A) in the spinal
58. Hamilton LD, Mani D, Almuklass AM, Davis LA, 74. Kiernan MC, Lin CS, Burke D. Differences in ac- cord mediates the effects of TENS in rats. Brain
Vieira T, Botter A, Enoka RM. Electrical nerve tivity-dependent hyperpolarization in human sen- Res 1136: 43–50, 2007. doi:10.1016/j.brainres.
stimulation modulates motor unit activity in con- sory and motor axons. J Physiol 558: 341–349, 2006.11.061.
tralateral biceps brachii during steady isometric 2004. doi:10.1113/jphysiol.2004.063966.
contractions. J Neurophysiol 120: 2603–2613, 89. Maffiuletti NA. Physiological and methodological
2018. doi:10.1152/jn.00235.2018. 75. Kim SH, Park JH, Jung MY, Yoo EY. Effects of considerations for the use of neuromuscular elec-
task-oriented training as an added treatment to trical stimulation. Eur J Appl Physiol 110: 223–
59. Hara Y, Obayashi S, Tsujiuchi K, Muraoka Y. The electromyogram-triggered neuromuscular stimu- 234, 2010. doi:10.1007/s00421-010-1502-y.
effects of electromyography-controlled func- lation on upper extremity function in chronic
tional electrical stimulation on upper extremity stroke patients. Occup Ther Int 23: 165–174, 90. Maffiuletti NA, Pensini M, Martin A. Activation of
function and cortical perfusion in stroke patients. 2016. doi:10.1002/oti.1421. human plantar flexor muscles increases after elec-
Clin Neurophysiol 124: 2008 –2015, 2013. doi:10. tromyostimulation training. J Appl Physiol (1985)
1016/j.clinph.2013.03.030. 76. Knaflitz M, Merletti R, De Luca CJ. Inference of 92: 1383–1392, 2002. doi:10.1152/japplphysiol.
motor unit recruitment order in voluntary and 00884.2001.
60. Heba S, Puts NA, Kalisch T, Glaubitz B, Haag electrically elicited contractions. J Appl Physiol
LM, Lenz M, Dinse HR, Edden RA, Tegenthoff (1985) 68: 1657–1667, 1990. doi:10.1152/jappl. 91. Malnick SDH, Band Y, Alin P, Maffiuletti NA. It’s
M, Schmidt-Wilcke T. Local GABA concentra- 1990.68.4.1657. time to regulate the use of whole body electrical
tion predicts perceptual improvements after stimulation. BMJ 352: i1693, 2016. doi:10.1136/
repetitive sensory stimulation in humans. 77. Knash ME, Kido A, Gorassini M, Chan KM, Stein bmj.i1693.
Cereb Cortex 26: 1295–1301, 2016. doi:10. RB. Electrical stimulation of the human common
1093/cercor/bhv296. peroneal nerve elicits lasting facilitation of corti- 92. Mang CS, Bergquist AJ, Roshko SM, Collins DF.
cal motor-evoked potentials. Exp Brain Res 153: Loss of short-latency afferent inhibition and
61. Heckman CJ, Enoka RM. Motor unit. Compr 366 –377, 2003. doi:10.1007/s00221-003-1628-9. emergence of afferent facilitation following neu-
Physiol 2: 2629 –2682, 2012. doi:10.1002/cphy. romuscular electrical stimulation. Neurosci Lett
c100087. 78. Kouzaki M, Kimura T, Yoshitake Y, Hayashi T, 529: 80 – 85, 2012. doi:10.1016/j.neulet.2012.08.
Moritani T. Subthreshold electrical stimulation 072.
62. Heyters M, Carpentier A, Duchateau J, Hainaut reduces motor unit discharge variability and de-
K. Twitch analysis as an approach to motor unit creases the force fluctuations of plantar flexion. 93. Mang CS, Clair JM, Collins DF. Neuromuscular
activation during electrical stimulation. Can J Neurosci Lett 513: 146 –150, 2012. doi:10.1016/ electrical stimulation has a global effect on cor-
Appl Physiol 19: 451– 461, 1994. doi:10.1139/ j.neulet.2012.02.020. ticospinal excitability for leg muscles and a fo-
h94-037. cused effect for hand muscles. Exp Brain Res
79. Kragel PA, Kano M, Van Oudenhove L, Ly HG, 209: 355–363, 2011. doi:10.1007/s00221-011-
63. Hoffmann P. Über die Beziehunger der Sehnre- Dupont P, Rubio A, Delon-Martin C, Bonaz BL, 2556-8.
flexe zur willkürlichen Bewegung und zum Tonus. Manuck SB, Gianaros PJ, Ceko M, Reynolds Losin
Z Biol 68: 351–370, 1918. EA, Woo CW, Nichols TE, Wager TD. Generaliz- 94. Mang CS, Lagerquist O, Collins DF. Changes in
able representations of pain, cognitive control, corticospinal excitability evoked by common per-
64. Hoffmann P. Utersuchung über die Eigenreflexe and negative emotion in medial frontal cortex. oneal nerve stimulation depend on stimulation
(Sehnenreflexe) menschlicher Muskeln. Berlin: Nat Neurosci 21: 283–289, 2018. doi:10.1038/ frequency. Exp Brain Res 203: 11–20, 2010. doi:
Springer, 1922. s41593-017-0051-7. 10.1007/s00221-010-2202-x.
65. Hortobágyi T, Scott K, Lambert J, Hamilton G, 80. Kwon DR, Kim J, Kim Y, An S, Kwak J, Lee S, Park 95. Mani D, Almuklass AM, Amiridis IG, Enoka RM.
Tracy J. Cross-education of muscle strength is S, Choi YH, Lee YK, Park JW. Short-term micro- Neuromuscular electrical stimulation can im-
greater with stimulated than voluntary contrac- current electrical neuromuscular stimulation to prove mobility in older adults but the time course
tions. Mot Contr 3: 205–219, 1999. doi:10.1123/ improve muscle function in the elderly. Medicine varies across tasks: Double-blind, randomized
mcj.3.2.205. (Baltimore) 96: e7407, 2017. doi:10.1097/MD. trial. Exp Gerontol 108: 269 –275, 2018. doi:10.
0000000000007407. 1016/j.exger.2018.04.018.
66. Howard JD, Enoka RM. Maximum bilateral con-
tractions are modified by neurally mediated in- 81. Lagerquist O, Walsh LD, Blouin JS, Collins DF, 96. Mani D, Feeney DF, Enoka RM. The modulation
terlimb effects. J Appl Physiol (1985) 70: 306 – Gandevia SC. Effect of a peripheral nerve block of force steadiness by electrical nerve stimulation
316, 1991. doi:10.1152/jappl.1991.70.1.306. on torque produced by repetitive electrical stim- applied to the wrist extensors differs for young
ulation. J Appl Physiol (1985) 107: 161–167, and older adults. Eur J Appl Physiol 119: 301–
67. Hugon M. Methodology of the Hoffmann reflex 2009. doi:10.1152/japplphysiol.91635.2008. 310, 2019. doi:10.1007/s00421-018-4025-6.
in man. In: New Developments in Electromyog-
raphy and Clinical Neurophysiology, edited by 82. Lateva ZC, McGill KC, Johanson ME. The inner- 97. Mesin L, Merletti R. Distribution of electrical
Desmedt JE. Basel: Karger, 1973, vol 3., p. 277– vation and organization of motor units in a series- stimulation current in a planar multilayer aniso-
293. fibered human muscle: the brachioradialis. J Appl tropic tissue. IEEE Trans Biomed Eng 55: 660 –
Physiol (1985) 108: 1530 –1541, 2010. doi:10. 670, 2008. doi:10.1109/TBME.2007.902248.
1152/japplphysiol.01163.2009.
54 PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
98. Mesin L, Merlo E, Merletti R, Orizio C. Investiga- 112. Patsaki I, Gerovasili V, Sidiras G, Karatzanos E, 127. Schmidt-Wilcke T, Wulms N, Heba S, Pleger B,
tion of motor unit recruitment during stimulated Mitsiou G, Papadopoulos E, Christakou A, Routsi Puts NA, Glaubitz B, Kalisch T, Tegenthoff M,
contractions of tibialis anterior muscle. J Electro- C, Kotanidou A, Nanas S. Effect of neuromuscu- Dinse HR. Structural changes in brain morphol-
myogr Kinesiol 20: 580 –589, 2010. doi:10.1016/ lar stimulation and individualized rehabilitation ogy induced by brief periods of repetitive sen-
j.jelekin.2009.11.008. on muscle strength in intensive care unit survi- sory stimulation. Neuroimage 165: 148 –157,
vors: a randomized trial. J Crit Care 40: 76 – 82, 2018. doi:10.1016/j.neuroimage.2017.10.016.
99. Miller L, McFadyen A, Lord AC, Hunter R, Paul L, 2017. doi:10.1016/j.jcrc.2017.03.014.
Rafferty D, Bowers R, Mattison P. Functional 128. Segers J, Hermans G, Bruyninckx F, Meyfroidt G,
electrical stimulation for foot drop in multiple 113. Petrofsky J, Laymon M, Prowse M, Gunda S, Langer D, Gosselink R. Feasibility of neuromus-
sclerosis: a systematic review and meta-analysis Batt J. The transfer of current through skin and cular electrical stimulation in critically ill patients.
of the effect on gait speed. Arch Phys Med Re- muscle during electrical stimulation with sine, J Crit Care 29: 1082–1088, 2014. doi:10.1016/j.
habil 98: 1435–1452, 2017. doi:10.1016/j.apmr. square, Russian and interferential waveforms. J jcrc.2014.06.024.
2016.12.007. Med Eng Technol 33: 170 –181, 2009. doi:10.
1080/03091900802054580. 129. Sheffler LR, Chae J. Neuromuscular electrical
100. Mines GR. On the summation of contractions. J stimulation in neurorehabilitation. Muscle Nerve
Physiol 46: 1–27, 1913. doi:10.1113/jphysiol. 114. Pierrot-Deseilligny E, Mazevet D. The monosyn- 35: 562–590, 2007. doi:10.1002/mus.20758.
1913.sp001577. aptic reflex: a tool to investigate motor control in
humans. Interest and limits. Neurophysiol Clin 130. Shimodozono M, Noma T, Matsumoto S, Miyata R,
101. Minetto MA, Botter A, Gamerro G, Varvello I, 30: 67– 80, 2000. doi:10.1016/S0987-7053(00) Etoh S, Kawahira K. Repetitive facilitative exercise
Massazza G, Bellomo RG, Maffiuletti NA, Saggini 00062-9. under continuous electrical stimulation for severe
R. Contralateral effect of short-duration unilat- arm impairment after sub-acute stroke: a random-
eral neuromuscular electrical stimulation and fo- 115. Ping Ho Chung B, Kam Kwan Cheng B. Immedi- ized controlled pilot study. Brain Inj 28: 203–210,
cal vibration in healthy subjects. Eur J Phys ate effect of transcutaneous electrical nerve stim- 2014. doi:10.3109/02699052.2013.860472.
Rehabil Med 54: 911–920, 2018. doi:10.23736/ ulation on spasticity in patients with spinal cord
S1973-9087.18.05004-9. injury. Clin Rehabil 24: 202–210, 2010. doi:10. 131. Shin HK, Cho SH, Jeon HS, Lee YH, Song JC,
1177/0269215509343235. Jang SH, Lee CH, Kwon YH. Cortical effect and
102. Monaghan CC, Hermens HJ, Nene AV, Tenniglo functional recovery by the electromyography-
MJB, Veltink PH. The effect of FES of the tibial 116. Piper H. Electrophysiologie Menschliger Mus- triggered neuromuscular stimulation in chronic
nerve on physiological activation of leg muscles keln. Berlin: Springer-Verlag, 1912. stroke patients. Neurosci Lett 442: 174 –179,
during gait. Med Eng Phys 32: 332–338, 2010. 2008. doi:10.1016/j.neulet.2008.07.026.
doi:10.1016/j.medengphy.2010.01.003. 117. Prochazka A. Motor neuroprostheses. Compr
Physiol 9: 127–148, 2018. doi:10.1002/cphy. 132. Slovak M, Chindo J, Nair KPS, Reeves ML, Heller
103. Moran F, Leonard T, Hawthorne S, Hughes CM, c180006. B, Barker AT. Sensory barrage stimulation in the
McCrum-Gardner E, Johnson MI, Rakel BA, Sluka treatment of elbow spasticity: a crossover dou-
KA, Walsh DM. Hypoalgesia in response to trans- 118. Radhakrishnan R, Sluka KA. Deep tissue affer- ble blind randomized pilot trial. Neuromodula-
cutaneous electrical nerve stimulation (TENS) de- ents, but not cutaneous afferents, mediate trans- tion 19: 220 –226, 2016. doi:10.1111/ner.12383.
pends on stimulation intensity. J Pain 12: 929 – cutaneous electrical nerve stimulation-Induced
935, 2011. doi:10.1016/j.jpain.2011.02.352. antihyperalgesia. J Pain 6: 673– 680, 2005. doi: 133. Spector P, Laufer Y, Elboim Gabyzon M, Kittel-
10.1016/j.jpain.2005.06.001. son A, Stevens Lapsley J, Maffiuletti NA. Neuro-
104. Morf C, Wellauer V, Casartelli NC, Maffiuletti NA. muscular electrical stimulation therapy to restore
Acute effects of multipath electrical stimulation 119. Rakel BA, Zimmerman MB, Geasland K, Embree quadriceps muscle function in patients after or-
in patients with total knee arthroplasty. Arch J, Clark CR, Noiseux NO, Callaghan JJ, Herr K, thopaedic surgery: a novel structured approach.
Phys Med Rehabil 96: 498 –504, 2015. doi:10. Walsh D, Sluka KA. Transcutaneous electrical J Bone Joint Surg Am 98: 2017–2024, 2016. doi:
1016/j.apmr.2014.10.011. nerve stimulation for the control of pain during 10.2106/JBJS.16.00192.
rehabilitation after total knee arthroplasty: A ran-
105. Negro F, Holobar A, Farina D. Fluctuations in domized, blinded, placebo-controlled trial. Pain 134. Stein RB, Everaert DG, Roy FD, Chong S, So-
isometric muscle force can be described by one 155: 2599 –2611, 2014. doi:10.1016/j.pain.2014. leimani M. Facilitation of corticospinal connec-
linear projection of low-frequency components 09.025. tions in able-bodied people and people with
of motor unit discharge rates. J Physiol 587: central nervous system disorders using eight in-
5925–5938, 2009. doi:10.1113/jphysiol.2009. 120. Resende L, Merriwether E, Rampazo EP, Dailey terventions. J Clin Neurophysiol 30: 66 –78, 2013.
178509. D, Embree J, Deberg J, Liebano RE, Sluka KA. doi:10.1097/WNP.0b013e31827ed6bd.
Meta-analysis of transcutaneous electrical nerve
106. Neto MLP, Maciel LYS, Cruz KML, Filho VJS, stimulation for relief of spinal pain. Eur J Pain 22: 135. Stein RB, Everaert DG, Thompson AK, Chong SL,
Bonjardim LR, DeSantana JM. Does electrode 663– 678, 2018. doi:10.1002/ejp.1168. Whittaker M, Robertson J, Kuether G. Long-term
placement influence tens-induced antihyperalge- therapeutic and orthotic effects of a foot drop
sia in experimental inflammatory pain model? 121. Routsi C, Gerovasili V, Vasileiadis I, Karatzanos E, stimulator on walking performance in progres-
Braz J Phys Ther 21: 92–99, 2017. doi:10.1016/j. Pitsolis T, Tripodaki E, Markaki V, Zervakis D, sive and nonprogressive neurological disorders.
bjpt.2017.03.003. Nanas S. Electrical muscle stimulation prevents Neurorehabil Neural Repair 24: 152–167, 2010.
critical illness polyneuromyopathy: a randomized doi:10.1177/1545968309347681.
107. Noto Y, Misawa S, Kanai K, Sato Y, Shibuya K, parallel intervention trial. Crit Care 14: R74, 2010.
Isose S, Nasu S, Sekiguchi Y, Fujimaki Y, Ohmori doi:10.1186/cc8987. 136. Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff
S, Nakagawa M, Kuwabara S. Activity-dependent DG, Kohrt WM. Early neuromuscular electrical
changes in impulse conduction of single human 122. Russ DW, Clark BC, Krause J, Hagerman FC. stimulation to improve quadriceps muscle strength
motor axons: a stimulated single fiber electro- Development of a neuromuscular electrical stim- after total knee arthroplasty: a randomized con-
myography study. Clin Neurophysiol 122: 2512– ulation protocol for sprint training. Med Sci trolled trial. Phys Ther 92: 210 –226, 2012. doi:10.
2517, 2011. doi:10.1016/j.clinph.2011.05.005. Sports Exerc 44: 1810 –1819, 2012. doi:10.1249/ 2522/ptj.20110124.
MSS.0b013e31825423f1.
108. Okuma Y, Bergquist AJ, Hong M, Chan KM, Col- 137. Street T, Taylor P, Swain I. Effectiveness of func-
lins DF. Electrical stimulation site influences the 123. Sabino GS, Santos CMF, Francischi JN, de Re- tional electrical stimulation on walking speed,
spatial distribution of motor units recruited in sende MA. Release of endogenous opioids fol- functional walking category, and clinically mean-
tibialis anterior. Clin Neurophysiol 124: 2257– lowing transcutaneous electric nerve stimulation ingful changes for people with multiple sclerosis.
2263, 2013. doi:10.1016/j.clinph.2013.04.015. in an experimental model of acute inflammatory Arch Phys Med Rehabil 96: 667– 672, 2015. doi:
pain. J Pain 9: 157–163, 2008. doi:10.1016/j. 10.1016/j.apmr.2014.11.017.
109. Palmieri-Smith RM, Thomas AC, Karvonen-Gutier- jpain.2007.09.003.
rez C, Sowers M. A clinical trial of neuromuscular 138. Stutzig N, Siebert T, Granacher U, Blickhan R.
electrical stimulation in improving quadriceps mus- 124. Saitou K, Masuda T, Michikami D, Kojima R, Alteration of synergistic muscle activity following
cle strength and activation among women with Okada M. Innervation zones of the upper and neuromuscular electrical stimulation of one mus-
mild and moderate osteoarthritis. Phys Ther 90: lower limb muscles estimated by using multi- cle. Brain Behav 2: 640 – 646, 2012. doi:10.1002/
1441–1452, 2010. doi:10.2522/ptj.20090330. channel surface EMG. J Hum Ergol (Tokyo) 29: brb3.87.
35–52, 2000.
110. Pantaleão MA, Laurino MF, Gallego NLG, Cabral 139. Svendsen KB, Jensen TS, Hansen HJ, Bach FW.
CMN, Rakel B, Vance C, Sluka KA, Walsh DM, 125. Schieppati M. The Hoffmann reflex: a means of Sensory function and quality of life in patients
Liebano RE. Adjusting pulse amplitude during assessing spinal reflex excitability and its descend- with multiple sclerosis and pain. Pain 114: 473–
transcutaneous electrical nerve stimulation (TENS) ing control in man. Prog Neurobiol 28: 345–376, 481, 2005. doi:10.1016/j.pain.2005.01.015.
application produces greater hypoalgesia. J Pain 1987. doi:10.1016/0301-0082(87)90007-4.
12: 581–590, 2011. doi:10.1016/j.jpain.2010.11. 140. Taylor JA, Picard G, Widrick JJ. Aerobic capacity
001. 126. Schuhfried O, Crevenna R, Fialka-Moser V, Pater- with hybrid FES rowing in spinal cord injury: com-
nostro-Sluga T. Non-invasive neuromuscular parison with arms-only exercise and preliminary
111. Panizza M, Nilsson J, Roth BJ, Basser PJ, Hallett electrical stimulation in patients with central ner- findings with regular training. PM R 3: 817– 824,
M. Relevance of stimulus duration for activation vous system lesions: an educational review. J 2011. doi:10.1016/j.pmrj.2011.03.020.
of motor and sensory fibers: implications for the Rehabil Med 44: 99 –105, 2012. doi:10.2340/
study of H-reflexes and magnetic stimulation. 16501977-0941.
Electroencephalogr Clin Neurophysiol 85: 22–29,
1992. doi:10.1016/0168-5597(92)90097-U.
PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org 55
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
REVIEW
141. Thompson CK, Negro F, Johnson MD, Holmes MR, 149. Vanderthommen M, Depresseux JC, Dauchat L, 156. Wu CW, Seo HJ, Cohen LG. Influence of electric
McPherson LM, Powers RK, Farina D, Heckman CJ. Degueldre C, Croisier JL, Crielaard JM. Spatial somatosensory stimulation on paretic-hand func-
Robust and accurate decoding of motoneuron be- distribution of blood flow in electrically stimu- tion in chronic stroke. Arch Phys Med Rehabil 87:
haviour and prediction of the resulting force out- lated human muscle: a positron emission tomog- 351–357, 2006. doi:10.1016/j.apmr.2005.11.019.
put. J Physiol 596: 2643–2659, 2018. doi:10.1113/ raphy study. Muscle Nerve 23: 482– 489,
JP276153. 2000. doi:10.1002/(SICI)1097-4598(200004)23:4 157. Yamada M, Nakazawa T, Kyoso M, Ishijima M.
⬍482:AID-MUS5⬎3.0.CO;2-I. Single motor unit F-waves in the thenar muscles
142. Tracey JM, Stoffel JT. Secondary and tertiary studied by the multichannel surface EMG. Elec-
treatments for multiple sclerosis patients with 150. Vaz MA, Baroni BM, Geremia JM, Lanferdini FJ, tromyogr Clin Neurophysiol 47: 43– 47, 2007.
urinary symptoms. Investig Clin Urol 57: 377– Mayer A, Arampatzis A, Herzog W. Neuromus-
383, 2016. doi:10.4111/icu.2016.57.6.377. cular electrical stimulation (NMES) reduces struc- 158. Yoshida Y, Ikuno K, Shomoto K. Comparison of
tural and functional losses of quadriceps muscle the effect of sensory-level and conventional mo-
143. Truong AD, Kho ME, Brower RG, Feldman DR, and improves health status in patients with knee tor-level neuromuscular electrical stimulations on
Colantuoni E, Needham DM. Effects of neuro- osteoarthritis. J Orthop Res 31: 511–516, 2013. quadriceps strength after total knee arthroplas-
muscular electrical stimulation on cytokines in doi:10.1002/jor.22264. ty: a prospective randomized single-blind trial.
peripheral blood for healthy participants: a pro- Arch Phys Med Rehabil 98: 2364 –2370, 2017.
spective, single-blinded Study. Clin Physiol Funct 151. Veldman MP, Maurits NM, Zijdewind I, Maffiu- doi:10.1016/j.apmr.2017.05.005.
Imaging 37: 255–262, 2017. doi:10.1111/cpf. letti NA, van Middelkoop S, Mizelle JC, Horto-
12290. bágyi T. Somatosensory electrical stimulation 159. Yoshida Y, Mizner RL, Snyder-Mackler L. Associ-
improves skill acquisition, consolidation, and ation between long-term quadriceps weakness
144. Tubaro A, Puccini F, De Nunzio C. The manage- transfer by increasing sensorimotor activity and and early walking muscle co-contraction after to-
ment of overactive bladder: percutaneous tibial connectivity. J Neurophysiol 120: 281–290, 2018. tal knee arthroplasty. Knee 20: 426 – 431, 2013.
nerve stimulation, sacral nerve stimulation, or doi:10.1152/jn.00860.2017. doi:10.1016/j.knee.2012.12.008.
botulinum toxin? Curr Opin Urol 25: 305–310,
2015. doi:10.1097/MOU.0000000000000180. 152. Vivodtzev I, Debigaré R, Gagnon P, Mainguy V, 160. Yu D, Yin H, Han T, Jiang H, Cao X. Intramuscular
Saey D, Dubé A, Paré ME, Bélanger M, Maltais F. innervations of lower leg skeletal muscles: appli-
145. Valtonen A, Pöyhönen T, Heinonen A, Sipilä S. Functional and muscular effects of neuromuscu- cations in their clinical use in functional muscular
Muscle deficits persist after unilateral knee re- lar electrical stimulation in patients with severe transfer. Surg Radiol Anat 38: 675– 685, 2016.
placement and have implications for rehabilita- COPD: a randomized clinical trial. Chest 141: doi:10.1007/s00276-015-1601-x.
tion. Phys Ther 89: 1072–1079, 2009. doi:10. 716 –725, 2012. doi:10.1378/chest.11-0839.
2522/ptj.20070295. 161. Zackowski KM, Smith SA, Reich DS, Gordon-Lip-
153. Walker ER, Hyngstrom AS, Schmit BD. Sensory kin E, Chodkowski BA, Sambandan DR, Shtey-
146. Vance CG, Chimenti RL, Dailey DL, Hadlandsmyth electrical stimulation improves foot placement man M, Bastian AJ, van Zijl PC, Calabresi PA.
K, Zimmerman MB, Geasland KM, Williams JM, during targeted stepping post-stroke. Exp Brain Sensorimotor dysfunction in multiple sclerosis
Merriwether EN, Alemo Munters L, Rakel BA, Crof- Res 232: 1137–1143, 2014. doi:10.1007/s00221- and column-specific magnetization transfer-im-
ford LJ, Sluka KA. Development of a method to 014-3823-2. aging abnormalities in the spinal cord. Brain 132:
maximize the transcutaneous electrical nerve 1200 –1209, 2009. doi:10.1093/brain/awp032.
stimulation intensity in women with fibromyalgia. 154. Wegrzyk J, Fouré A, Vilmen C, Ghattas B, Maffiu-
J Pain Res 11: 2269 –2278, 2018. doi:10.2147/ letti NA, Mattei JP, Place N, Bendahan D, Gondin 162. Zackowski KM, Wang JI, McGready J, Calabresi
JPR.S168297. J. Extra Forces induced by wide-pulse, high-fre- PA, Newsome SD. Quantitative sensory and mo-
quency electrical stimulation: Occurrence, mag- tor measures detect change overtime and corre-
147. Vance CGT, Dailey DL, Rakel BA, Sluka KA. Using nitude, variability and underlying mechanisms. late with walking speed in individuals with
TENS for pain control: the state of the evidence. Clin Neurophysiol 126: 1400 –1412, 2015. doi:10. multiple sclerosis. Mult Scler Relat Disord 4: 67–
Pain Manag 4: 197–209, 2014. doi:10.2217/pmt. 1016/j.clinph.2014.10.001. 74, 2015. doi:10.1016/j.msard.2014.11.001.
14.13.
155. Weissenfels A, Teschler M, Willert S, Hettchen M, 163. Zijdewind I, Prak RF, Wolkorte R. Fatigue and
148. Vance CGT, Radhakrishnan R, Skyba DA, Sluka Fröhlich M, Kleinöder H, Kohl M, von Stengel S, fatigability in persons with multiple sclerosis. Ex-
KA. Transcutaneous electrical nerve stimulation Kemmler W. Effects of whole-body electromyo- erc Sport Sci Rev 44: 123–128, 2016. doi:10.
at both high and low frequencies reduces pri- stimulation on chronic nonspecific low back pain 1249/JES.0000000000000088.
mary hyperalgesia in rats with joint inflammation in adults: a randomized controlled study. J Pain
in a time-dependent manner. Phys Ther 87: 44 – Res 11: 1949 –1957, 2018. doi:10.2147/JPR.
51, 2007. doi:10.2522/ptj.20060032. S164904.
56 PHYSIOLOGY • Volume 35 • January 2020 • www.physiologyonline.org
Downloaded from journals.physiology.org/journal/physiologyonline (131.000.192.090) on May 4, 2022.
You might also like
- Electroson & Electro StimulationDocument4 pagesElectroson & Electro StimulationKumar Aditya100% (2)
- The Role of Electrical Stimulators in Contemporary Physical TherapyDocument33 pagesThe Role of Electrical Stimulators in Contemporary Physical Therapyeager_learner100% (2)
- Nervous System: Third EditionDocument36 pagesNervous System: Third EditionAlexis Tobar100% (1)
- Introduction To NeuropsychologyDocument15 pagesIntroduction To NeuropsychologyPsychology Department Ilahia Arts CollegeNo ratings yet
- Nervous SYSTESTDocument19 pagesNervous SYSTESTedwalk1250% (2)
- Child Development A Cultural Approach 2nd Edition Arnett Test Bank 1Document117 pagesChild Development A Cultural Approach 2nd Edition Arnett Test Bank 1joshua100% (36)
- Emg, NCVDocument38 pagesEmg, NCVMaria Isabel Nabor100% (1)
- EBB 2020 Phase 1 TestDocument9 pagesEBB 2020 Phase 1 TestMohamed Hamed IssaNo ratings yet
- Electrofisiología Cardiaca Kimee NeyssaDocument17 pagesElectrofisiología Cardiaca Kimee NeyssaNEYSSA KIMEE SAINT VILNo ratings yet
- The Australian Journal of Physiotherapy: Electrodiagnostic TechniquesDocument4 pagesThe Australian Journal of Physiotherapy: Electrodiagnostic TechniquesumangNo ratings yet
- JSH 20 LLDocument8 pagesJSH 20 LLomelbat-1No ratings yet
- Conexión Directa ANTIGUA (2009) Entre El Cerebro y Protesisdirect - Neural - Sensory - Feedback - and - Control - of - A - Prosthetic - ArmDocument5 pagesConexión Directa ANTIGUA (2009) Entre El Cerebro y Protesisdirect - Neural - Sensory - Feedback - and - Control - of - A - Prosthetic - ArmAERMNo ratings yet
- Motor Stimulation With Interferential Cu 1985 Australian Journal of PhysiothDocument6 pagesMotor Stimulation With Interferential Cu 1985 Australian Journal of PhysiothEmad Tawfik AhmadNo ratings yet
- 1 s2.0 S1877065715000779 MainDocument7 pages1 s2.0 S1877065715000779 Mainxian karachiNo ratings yet
- 1 s2.0 S1053811919304240 MainDocument10 pages1 s2.0 S1053811919304240 MainlabsoneducationNo ratings yet
- Chronic Electrical Nerve Stimulation As A Therapeutic Intervention For Peripheral Nerve RepairDocument6 pagesChronic Electrical Nerve Stimulation As A Therapeutic Intervention For Peripheral Nerve RepaircontremonicaNo ratings yet
- Bio 122 FR 09 - Muscle ContractionDocument10 pagesBio 122 FR 09 - Muscle ContractionLance CarandangNo ratings yet
- Adaptações Neurais Ao Treinamento de Força Indo Além Da Estimulação Magnética Transcraniana e Estudos ReflexosDocument23 pagesAdaptações Neurais Ao Treinamento de Força Indo Além Da Estimulação Magnética Transcraniana e Estudos ReflexosSheilani MartinsNo ratings yet
- NMESDocument5 pagesNMESVALDEZ, Kessia Faye Carmela R.No ratings yet
- eStimAndRegeneration PDFDocument7 pageseStimAndRegeneration PDFkalanathNo ratings yet
- Biofeedback Electrostimulation For Bionic and Long-Lasting Neural ModulationDocument12 pagesBiofeedback Electrostimulation For Bionic and Long-Lasting Neural ModulationdfdffNo ratings yet
- 1 s2.0 S1935861X21000590 MainDocument18 pages1 s2.0 S1935861X21000590 MainGerové InvestmentsNo ratings yet
- Research PaperDocument14 pagesResearch PaperAnurag MathurNo ratings yet
- A Estimulação Elétrica Terapêutica Melhora A Função em Crianças Com Deficiência Uma Revisão Abrangente Da LiteraturaDocument17 pagesA Estimulação Elétrica Terapêutica Melhora A Função em Crianças Com Deficiência Uma Revisão Abrangente Da LiteraturaMatheus AlmeidaNo ratings yet
- Why Exercise Builds Muscles: Titin Mechanosensing Controls Skeletal Muscle Growth Under LoadDocument15 pagesWhy Exercise Builds Muscles: Titin Mechanosensing Controls Skeletal Muscle Growth Under LoadRaul Docto100% (1)
- Germer Et Al JNE 2019Document15 pagesGermer Et Al JNE 2019richardNo ratings yet
- Advanced Exoskeleton Armv1.5Document5 pagesAdvanced Exoskeleton Armv1.5MasterAnimusNo ratings yet
- Application of EMG Signals For ControlliDocument6 pagesApplication of EMG Signals For Controlliashwin321501No ratings yet
- Onlinefirst Talaber Laha2021Document13 pagesOnlinefirst Talaber Laha2021Irena HNo ratings yet
- 10 1152@ajpcell 00016 2016Document14 pages10 1152@ajpcell 00016 2016Muttley ZNo ratings yet
- Yong-Hyun 2011Document7 pagesYong-Hyun 2011GorkaBuesaNo ratings yet
- Škarabot2020 Article TheKnownsAndUnknownsOfNeuralAdDocument11 pagesŠkarabot2020 Article TheKnownsAndUnknownsOfNeuralAdR.No ratings yet
- A Critical Review of Interfaces With The Peripheral Nervous System For The Control of Neuroprostheses and Hybrid Bionic SystemsDocument30 pagesA Critical Review of Interfaces With The Peripheral Nervous System For The Control of Neuroprostheses and Hybrid Bionic SystemsJoao PauloNo ratings yet
- Neuromuscular 2 PDFDocument23 pagesNeuromuscular 2 PDFSandra Milena Infante TrujilloNo ratings yet
- Mechanotherapy How Physical TherapistsDocument5 pagesMechanotherapy How Physical TherapistsMiguel Angel Lancheros PimentelNo ratings yet
- Electromyography and Its Applications in OrthodonticsDocument5 pagesElectromyography and Its Applications in Orthodonticsmehdi chahrourNo ratings yet
- Ibata & Terentjev 2021 - Titin Mechanosensing Controls Skeletal Muscle Growth Under LoadDocument15 pagesIbata & Terentjev 2021 - Titin Mechanosensing Controls Skeletal Muscle Growth Under LoadIvan TaranovNo ratings yet
- 297 FullDocument10 pages297 FullGaluhFahmiNo ratings yet
- Mechanisms of Su'Praspinal Actions Upon Spinal Cord Activities. Reticular Inhibitory Mechanisms On Alpha-Extensor MotoneuronsDocument13 pagesMechanisms of Su'Praspinal Actions Upon Spinal Cord Activities. Reticular Inhibitory Mechanisms On Alpha-Extensor MotoneuronsJulien FerreresNo ratings yet
- Magnetoelectric Brain Stimulation in TheDocument9 pagesMagnetoelectric Brain Stimulation in ThesukohomaNo ratings yet
- Introduction EmgDocument3 pagesIntroduction EmgVaneet KumarNo ratings yet
- Ntroduction: Electromyography (Emg) IDocument2 pagesNtroduction: Electromyography (Emg) IbogdanneamtuNo ratings yet
- Research P MedicalDocument11 pagesResearch P MedicalPKNo ratings yet
- Neural Signals For Command Control and Feedback in Functional Neuromuscular Stimulation: A ReviewDocument13 pagesNeural Signals For Command Control and Feedback in Functional Neuromuscular Stimulation: A ReviewAlioune Badara DioufNo ratings yet
- (2001) Burke D. Excitability of Human AxonsDocument11 pages(2001) Burke D. Excitability of Human AxonsLucía del ValleNo ratings yet
- Functional Electrical Stimulation of Denervated MusclesDocument7 pagesFunctional Electrical Stimulation of Denervated MusclesMirko GrausoNo ratings yet
- Physiological Based Motor Control of Postural Balance: July 2019Document7 pagesPhysiological Based Motor Control of Postural Balance: July 2019Nadia ImranNo ratings yet
- Neuromuscular Junction 3Document18 pagesNeuromuscular Junction 3Annisa RahmaNo ratings yet
- Liu Shig An 2010Document10 pagesLiu Shig An 2010AMARNATH PRASADNo ratings yet
- Posture Control AND Trajectory Formation During ARM Movement'Document7 pagesPosture Control AND Trajectory Formation During ARM Movement'Krishna VeniNo ratings yet
- Deficit SensoriomotorDocument7 pagesDeficit SensoriomotorAnonymous FWF4P38wHNo ratings yet
- Electrodiagnosis of The Muscular Dystrophies M HaywardDocument6 pagesElectrodiagnosis of The Muscular Dystrophies M HaywardJuan Jose Lopez ReyesNo ratings yet
- Lesson 2: Electromyography IiDocument17 pagesLesson 2: Electromyography Iiعباس حماديNo ratings yet
- Needle Electromyography: Basic ConceptsDocument14 pagesNeedle Electromyography: Basic ConceptsUlises VillanuevaNo ratings yet
- Physiol 00002 2018Document14 pagesPhysiol 00002 2018Pablo IgnacioNo ratings yet
- Spinal Cord Stimulation in Chronic Pain ManagementDocument10 pagesSpinal Cord Stimulation in Chronic Pain ManagementnaimNo ratings yet
- 1 s2.0 S0987705319301790 MainDocument7 pages1 s2.0 S0987705319301790 MainRaquel PintoNo ratings yet
- Muscle Contractile Characteristic Relationship To High-IntensityDocument6 pagesMuscle Contractile Characteristic Relationship To High-IntensityCharisNo ratings yet
- Muscle Motor Point Identification Is Essential For Optimizing Neuromuscular Electrical Stimulation UseDocument6 pagesMuscle Motor Point Identification Is Essential For Optimizing Neuromuscular Electrical Stimulation UsestefanoNo ratings yet
- Excitability Modulation of The Motor Sys PDFDocument12 pagesExcitability Modulation of The Motor Sys PDFСтанислав ЗубковNo ratings yet
- 1963 Mountcastle-Muscle Spindles? PDFDocument28 pages1963 Mountcastle-Muscle Spindles? PDFSilvio SánchezNo ratings yet
- Stretch-Induced Enhancement of Mechanical PowerDocument8 pagesStretch-Induced Enhancement of Mechanical PowerCharisNo ratings yet
- Ijbb 121 PDFDocument8 pagesIjbb 121 PDFRahma WatiNo ratings yet
- Shahani 1973Document14 pagesShahani 1973Abril CruzNo ratings yet
- Bioactivity study of modified curcumin loaded polymeric nanoparticlesFrom EverandBioactivity study of modified curcumin loaded polymeric nanoparticlesNo ratings yet
- Efeitos Da Atividade Fisica Na OsteoartroseDocument26 pagesEfeitos Da Atividade Fisica Na OsteoartroseThiago Penna ChavesNo ratings yet
- Treino de Propriocepção Na Prevenção Do Entorse de TornozeloDocument3 pagesTreino de Propriocepção Na Prevenção Do Entorse de TornozeloThiago Penna ChavesNo ratings yet
- Tratamento Das Lesões Ligamentares Agudas Do TornozeloDocument13 pagesTratamento Das Lesões Ligamentares Agudas Do TornozeloThiago Penna ChavesNo ratings yet
- Exercise-Based Rehabilitation Reduces Reinjury Following Acute Lateral Ankle Sprain: A Systematic Review Update With Meta-AnalysisDocument20 pagesExercise-Based Rehabilitation Reduces Reinjury Following Acute Lateral Ankle Sprain: A Systematic Review Update With Meta-AnalysisThiago Penna ChavesNo ratings yet
- Crio Na Artite ReumatoideDocument13 pagesCrio Na Artite ReumatoideThiago Penna ChavesNo ratings yet
- Os Suportes Externos Melhoram o Equilíbrio Dinâmico em Pacientes Com Instabilidade Crônica Do Tornozelo - Uma Meta-AnáliseDocument19 pagesOs Suportes Externos Melhoram o Equilíbrio Dinâmico em Pacientes Com Instabilidade Crônica Do Tornozelo - Uma Meta-AnáliseThiago Penna ChavesNo ratings yet
- Reabilitação Após Tratamento Cirúrgico de Rupturas e Rupturas Do Tendão Fibular.Document10 pagesReabilitação Após Tratamento Cirúrgico de Rupturas e Rupturas Do Tendão Fibular.Thiago Penna ChavesNo ratings yet
- Intervenções Terapêuticas para Aumentar A Dorsiflexão Do Tornozelo Após Entorse Do TornozeloDocument14 pagesIntervenções Terapêuticas para Aumentar A Dorsiflexão Do Tornozelo Após Entorse Do TornozeloThiago Penna ChavesNo ratings yet
- Brazilian Journal of Physical TherapyDocument13 pagesBrazilian Journal of Physical TherapyThiago Penna ChavesNo ratings yet
- Artigo FesDocument20 pagesArtigo FesThiago Penna ChavesNo ratings yet
- Artigo FesDocument12 pagesArtigo FesThiago Penna ChavesNo ratings yet
- 2016 Exercises With Partial Vascular Occlusion in Patients With Knee Osteoarthritis A Randomized Clinical TrialDocument7 pages2016 Exercises With Partial Vascular Occlusion in Patients With Knee Osteoarthritis A Randomized Clinical TrialRoque Esteban Beltran GallardoNo ratings yet
- Artigo FesDocument19 pagesArtigo FesThiago Penna ChavesNo ratings yet
- Artigo FesDocument10 pagesArtigo FesThiago Penna ChavesNo ratings yet
- Science G 6 DappDocument6 pagesScience G 6 DappChester Austin Reese Maslog Jr.No ratings yet
- Test Bank For Anatomy and Physiology From Science To Life 2nd Edition by JenkinsDocument9 pagesTest Bank For Anatomy and Physiology From Science To Life 2nd Edition by JenkinsAlanMartinezkgqn100% (38)
- Basic Human AnatomyDocument6 pagesBasic Human AnatomySuman KumarNo ratings yet
- Psychedelic Drugs in Biomedicine. Review 2017Document14 pagesPsychedelic Drugs in Biomedicine. Review 2017Luis Henrique SalesNo ratings yet
- UG Physiology PDFDocument38 pagesUG Physiology PDFAmaradeepika JagannathanNo ratings yet
- TMP 26 FDDocument64 pagesTMP 26 FDFrontiersNo ratings yet
- (Oklahoma Notes) Roger Thies Ph.D. (Auth.), Roger Thies Ph.D. (Eds.) - Physiology-Springer-Verlag New York (1995)Document287 pages(Oklahoma Notes) Roger Thies Ph.D. (Auth.), Roger Thies Ph.D. (Eds.) - Physiology-Springer-Verlag New York (1995)MaadaNo ratings yet
- ITP ReviewerDocument8 pagesITP ReviewerBailey EtormaNo ratings yet
- Synaptic TransmissionDocument35 pagesSynaptic TransmissiondehaNo ratings yet
- Anaphy Midterm Week 2 Notes (Nervous System)Document20 pagesAnaphy Midterm Week 2 Notes (Nervous System)Zosia SageNo ratings yet
- My Psychology 1st Edition Pomerantz Test BankDocument35 pagesMy Psychology 1st Edition Pomerantz Test Bankescout.stoopvr5nbf100% (24)
- Science 10 - Learning Module 3QDocument86 pagesScience 10 - Learning Module 3QJovanni SimbulanNo ratings yet
- Aakash ZoologyDocument18 pagesAakash ZoologyYUGESH SINGARAM0% (1)
- Bio Level-Neurotransmission 2010Document15 pagesBio Level-Neurotransmission 2010api-233795225No ratings yet
- Structure of Synapse AND Mechanism of Synaptic Transmission: Prepared By: F3H (Science) Julai 08 Ipgm KsahDocument14 pagesStructure of Synapse AND Mechanism of Synaptic Transmission: Prepared By: F3H (Science) Julai 08 Ipgm KsahtembikailaiciNo ratings yet
- Inventions Weird and Awesome InventionsDocument48 pagesInventions Weird and Awesome InventionsKat MirandaNo ratings yet
- NSLNDocument7 pagesNSLNhandel21No ratings yet
- Muscle Physiology and NeurophysiologyDocument68 pagesMuscle Physiology and NeurophysiologyAlan MagpantayNo ratings yet
- Animal Tissues - DPP (00-00-2022)Document14 pagesAnimal Tissues - DPP (00-00-2022)mahir malikNo ratings yet
- A LZHEIMER'SDocument9 pagesA LZHEIMER'SPaul Mark PilarNo ratings yet
- Structure and Function of Nervous SystemDocument58 pagesStructure and Function of Nervous SystemFUN FLARE SHADOWNo ratings yet
- Brain Development During The Preschool YearsDocument21 pagesBrain Development During The Preschool Yearseup_1983No ratings yet
- 523 MIS QuestionsDocument8 pages523 MIS QuestionsGoda KondapallyNo ratings yet
- PERDEV - Q1 - Mod5 - The Brain Parts Functions and Societal RelationshipDocument26 pagesPERDEV - Q1 - Mod5 - The Brain Parts Functions and Societal Relationshipcherryochoco13No ratings yet
- Research Statement GabrielleGutierrezDocument6 pagesResearch Statement GabrielleGutierrezGabrielle GutierrezNo ratings yet