Professional Documents
Culture Documents
J of Thrombosis Haemost - 2011 - VAN BIJNEN - Mechanisms and Clinical Implications of Thrombosis in Paroxysmal Nocturnal
Uploaded by
Davin TakaryantoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
J of Thrombosis Haemost - 2011 - VAN BIJNEN - Mechanisms and Clinical Implications of Thrombosis in Paroxysmal Nocturnal
Uploaded by
Davin TakaryantoCopyright:
Available Formats
Journal of Thrombosis and Haemostasis, 10: 1–10 DOI: 10.1111/j.1538-7836.2011.04562.
REVIEW ARTICLE
Mechanisms and clinical implications of thrombosis in
paroxysmal nocturnal hemoglobinuria
S . T . A . V A N B I J N E N , * W . L . V A N H E E R D E and P . M U U S *
Departments of *Hematology and Laboratory Medicine – Laboratory of Hematology, Radboud University Nijmegen Medical Centre, Nijmegen,
the Netherlands
To cite this article: van Bijnen STA, van Heerde WL, Muus P. Mechanisms and clinical implications of thrombosis in paroxysmal nocturnal
hemoglobinuria. J Thromb Haemost 2012; 10: 1–10.
in the hematopoietic stem cell (HSC). The PIGA gene
Summary. Paroxysmal nocturnal hemoglobinuria (PNH) is product is essential for correct assembly of glycosyl phos-
a rare acquired disease characterized by a clone of blood cells phatidylinositol (GPI) anchors, linking several proteins to
lacking glycosyl phosphatidylinositol (GPI)-anchored pro- the cell membrane. Therefore, this mutation results in a
teins at the cell membrane. Deficiency of the GPI-anchored clone of blood cells deficient in GPI-anchored proteins
complement inhibitors CD55 and CD59 on erythrocytes (GPI-APs). Lack of the GPI-anchored complement
leads to intravascular hemolysis upon complement activation. inhibitors CD55 and, particularly, CD59 on erythrocytes
Apart from hemolysis, another prominent feature is a highly results in increased sensitivity to complement-mediated lysis.
increased risk of thrombosis. Thrombosis in PNH results in CD55 inhibits C3 convertases, and CD59 prevents the
high morbidity and mortality. Often, thrombosis occurs at assembly of the membrane attack complex (MAC) at the
unusual locations, with the Budd–Chiari syndrome being the cell surface.
most frequent manifestation. Primary prophylaxis with The clinical spectrum of PNH is highly variable. It ranges
vitamin K antagonists reduces the risk but does not from classic PNH with large PNH clone sizes, massive
completely prevent thrombosis. Eculizumab, a mAb against hemolysis, and a high risk of thrombosis, to patients with
complement factor C5, effectively reduces intravascular relatively small clone sizes and only mild or subclinical
hemolysis and also thrombotic risk. Therefore, eculizumab hemolysis. Patients in the latter group often have an
treatment has dramatically improved the prognosis of PNH. underlying bone marrow failure disease such as aplastic
The mechanism of thrombosis in PNH is still unknown, but anemia (AA), resulting in more prominent pancytopenia [1].
the highly beneficial effect of eculizumab on thrombotic risk Particularly classic PNH patients, suffer from intravascular
suggests a major role for complement activation. Addition- hemolysis, resulting in anemia, fatigue, and hemoglobinuria.
ally, a deficiency of GPI-anchored proteins involved in Paroxysms result from complement activation above basal
hemostasis may be implicated. levels, as may occur during infection. Such a hemolytic crisis
may enhance hemoglobinuria, and elicit acute renal failure
Keywords: eculizumab, paroxysmal nocturnal hemoglobinu- and thrombotic events. Thrombosis is one of the most
ria, thrombosis. severe complications, seriously affecting quality of life, and
is a major cause of death in PNH [2]. Many patients suffer
Introduction from multiple thromboses in vital organs, such as the liver,
brain, or gut, sometimes even during anticoagulant prophy-
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare
laxis [2,3].
disease characterized by chronic intravascular hemolysis and
The mechanism of thrombosis in PNH is still not elucidated.
hemoglobinuria, an increased risk of thrombosis, and a
In this review, we report on the current state of knowledge of
variable degree of bone marrow failure. The disease is
the pathogenesis of thrombosis and its treatment in PNH.
caused by an acquired mutation of the X-linked PIGA gene
Various mechanisms that are proposed to play a role in
thrombosis in PNH are discussed (summarized in Fig. 1).
Special attention is given to eculizumab, a mAb directed to
Correspondence: Petra Muus, Department of Hematology, Radboud complement factor C5 that efficiently blocks intravascular
University Nijmegen Medical Center, HP 476, PO Box 9101, 6500 HB hemolysis and its sequelae. Importantly, strong retrospective
Nijmegen, the Netherlands.
evidence suggests that eculizumab reduces thrombotic risk in
Tel.: +31 24 3614762; fax: +31 24 3542080.
PNH [3], and it is therefore currently regarded as the best
E-mail: p.muus@hemat.umcn.nl
known prophylaxis.
Received 27 June 2011, accepted 3 November 2011
Ó 2011 International Society on Thrombosis and Haemostasis
2 S. T. A. van Bijnen et al
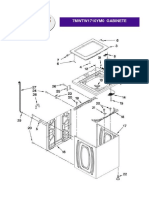
u-PAR deficiency
Fibrino
lysis
TFPI deficiency
Coagu
lation PR3 deficiency
NO scavenging
Complement-mediated damage Microvesicle release
Blood cells
Platelet activation
Free hemoglobin Vessel wall
Fig. 1. Hypothetical mechanisms for thrombosis in paroxysmal nocturnal hemoglobinuria (PNH). The hemostatic balance is maintained by coagulation
and fibrinolysis, and is influenced by factors derived from the vessel wall and blood cells. Several mechanisms have been suggested to determine the
direction of the balance towards a prothrombotic state in PNH. These include the release of free hemoglobin, which activates the endothelium and
scavenges nitric oxide (NO). In addition, complement-mediated damage of glycosyl phosphatidylinositol (GPI)-deficient blood cells may result in the
release of procoagulant microparticles into the circulation and platelet activation. Finally, deficiency of GPI-anchored fibrinolytic factors such as urokinase
plasminogen activator receptor (u-PAR), and anticoagulant factors such as tissue factor pathway inhibitor (TFPI) and, potentially, proteinase 3 (PR3),
may further disturb the hemostatic balance.
Epidemiology of thrombosis in PNH The risk of arterial thrombosis is probably also increased as
compared with age-matched healthy controls. Ziakas et al.
The cumulative 10-year incidence of thrombosis in a retro-
described 38 reports of arterial thrombosis, mainly in the
spective study of 460 PNH patients was 31% [2]. In another
central nervous system or coronary arteries, occurring in
retrospective series of 80 patients, 39% had one or more
relatively young patients, with a median age of 35 years (range:
episodes of either venous or arterial thrombosis [4]. However,
22–47 years) for acute coronary syndromes, and 37–41 years
these series included PNH patients diagnosed by less sensitive
(range: 11–76 years) for stroke [15,16]. Three arterial throm-
methods than flow cytometry, leading to overrepresentation of
botic events were reported in a cohort of 209 Japanese patients
PNH patients with larger clones, and thus a potential
(1.4%) [14], none in the series of 220 patients of Socié et al. [5],
overestimation of thrombotic risk [4,5]. On the other hand,
eight in the cohort of 80 patients of Hillmen et al. (10%) [4],
as shown by Hill et al., subclinical thrombosis is frequent,
and seven in our own cohort of 97 patients (7.2%) diagnosed
which implies an underestimation of thrombosis risk. They
between 1990 and 2011 (unpublished data). In the classic PNH
found evidence of subclinical pulmonary embolism or myo-
patient population that participated in the various eculizumab
cardial ischemia in six of 10 patients [6].
trials, 15% of pretreatment thrombotic events were arterial,
The risk of venous thrombosis correlates with PNH
located in either the cerebral vasculature (13.6%) or coronary
granulocyte clone size. The study of Hall et al. reported a
arteries (1.4%) [3]. The international PNH registry (http://
44% 10-year risk of venous thrombosis in patients with a PNH
www.pnhsource.com), a prospective follow-up study now
granulocyte clone of > 50%. In patients with smaller clone
including over 1000 patients worldwide, may provide more
sizes, this was only 5.8%, which is, however, still higher than in
definite information on the incidence and prevalence of arterial
healthy controls [7]. Moyo et al. [8] confirmed the association
and venous thrombosis in PNH [17].
between PNH granulocyte clone size and thrombosis, and
Thrombosis is the most important prognostic factor
estimated an odds ratio of 1.64 for every 10% increase in clone
affecting survival. This is even more the case for the
size. Whether PNH clone size in other lineages also correlates
subcategory of PNH patients in whom bone marrow failure
with thrombotic risk is unknown. However, for PNH platelet
is prominent (hazard ratio [HR] for classic PNH, 7.8; HR for
clone size this is expected, as it correlates strongly with PNH
AA-PNH 33) [2]. Data from several older retrospective studies
granulocyte clone size [9]. Another open question is whether
showed that in 22.2% of PNH patients the cause of death was
PNH clone size independently increases thrombotic risk or
related to thrombosis, and in Western European patients this
does so by affecting the level of hemolysis. The proportion of
proportion was even higher (37.2%) [18]. The extremely high
thrombotic events that occur during hemolytic crises has never
incidence of thrombosis in PNH and its major effects on
been systematically studied. However, case reports provide
morbidity and mortality underline its clinical importance.
evidence that thrombosis may occur in patients with large
clones even when little or no hemolysis is present [10,11].
A higher risk of venous thrombosis was reported in patients
Why is the risk of thrombosis increased in PNH?
of African-American or Latin-American descent, and a lower
risk in Chinese and Japanese patients [12–14]. In Japanese Multiple mechanisms have been proposed to explain
patients, this can probably be explained by a significantly lower thrombophilia in PNH (Fig. 1); however, none of these
PNH granulocyte clone size than in Western patients [14]. mechanisms on its own sufficiently explains the extremely
Ó 2011 International Society on Thrombosis and Haemostasis
Thrombosis in PNH 3
high thrombotic risk in PNH. Below, each mechanism
Deficiency of TF pathway inhibitor (TFPI) and other GPI-APs
and its proposed relative contribution will be discussed in
involved in coagulation
detail.
TFPI limits coagulation initiation by inhibiting TF forma-
tion. TFPI forms a quaternary complex with TF, activated
Role of the endothelium
factor VII (FVIIa) and activated FX (FXa). It is mainly
Endothelial cell (EC) damage is an important factor that can produced by the endothelium of the microvasculature (85%),
contribute to thrombosis. Free hemoglobin released from but other sources include activated platelets, monocytes, and
lysed PNH erythrocytes may be directly toxic to ECs [19]. plasma. The full-length isoform TFPIa is most abundant. It
Alternatively, EC damage could result from the uptake of is bound either to glycosaminoglycans or to the cell
monocyte-derived microparticles, which may be released from membrane via an as-yet unidentified GPI-anchored cofactor
GPI-deficient monocytes upon complement damage. Such [30,31]. The alternatively spliced TFPIb also binds to the
microparticles contain tissue factor (TF), thus increasing TF membrane via a GPI anchor; however, this variant is absent
expression on ECs, as demonstrated by Aharon et al. [20]. In in platelets [32].
the studies of Simak et al. (n = 9) and Helley et al. (n = 23), Both TFPI isoforms are upregulated in monocytes upon
the numbers of EC microparticles with a prothrombotic and lipopolysaccharide stimulation. Blocking TFPI enhances
proinflammatory phenotype, indicating EC damage, were monocyte procoagulant properties [33], as may also occur in
significantly increased in PNH patients as compared with TFPI-lacking GPI-deficient monocytes. If GPI-deficient ECs
healthy controls [21]. Levels of the EC activation markers von are indeed present in PNH, lack of TFPI may render such ECs
Willebrand factor (VWF) and soluble VCAM-1 (sVCAM-1) procoagulant. However, as HSC-derived ECs are supposedly
were increased [22,23], whereas others found normal VWF infrequent, the contribution of TFPI-deficient endothelium in
levels and activity in a smaller study [24]. These results suggest PNH-related thrombosis is probably limited. On quiescent
endothelial damage or stimulation in PNH, either indirectly platelets, TFPIa is not expressed. Only upon simultaneous
by free hemoglobin, or directly by complement-mediated stimulation with collagen and thrombin do these highly
damage. activated platelets express TFPIa and several other procoag-
It is not yet known whether PNH patient ECs harbor the ulant proteins, and release TFPIa into microvesicles [32]. GPI-
PIGA mutation, and thus are more susceptible to complement deficient platelets probably lack surface expression of TFPIa
damage than normal ECs. Nevertheless, even in normal ECs, upon stimulation, which may further enhance their procoag-
the MAC upregulates TF and adhesion molecules [25]. ulant properties.
Endothelial progenitor cells can arise from the bone marrow Another protein expressed on neutrophils that is involved in
(reviewed in [26]). In myelodysplastic syndrome, it has been hemostasis is proteinase 3 (PR3). This enzyme binds to the
shown that circulating ECs (CECs) and hematopoietic cell membrane by using the GPI-anchored cofactor NB1
progenitor cells harbor identical chromosomal abnormalities, (CD177) [34]. Jankowska et al. demonstrated that PR3 is
indicating a common origin [27]. Preliminary evidence suggests absent on GPI-deficient neutrophils, and that circulating PR3
that this may also be the case in PNH. Helley et al. [23] levels were inversely correlated with PNH granulocyte clone
cultured endothelial colony-forming cells (ECFCs) from PNH size. Furthermore, PR3 reduced thrombin-induced platelet
patient mononuclear cells, and demonstrated CD55-deficient activation, suggesting that a lacking PR3 on PNH platelets
and CD59-deficient populations within these ECFCs. Further may promote platelet activation [35]. PR3 also modulates
research is required to determine whether PNH CECs or coagulation in various other ways, for example via cleavage of
ECFCs do indeed harbor PIGA mutations, and whether and the endothelial protein C receptor, degradation of TFPI,
where such cells are incorporated into the endothelium. A upregulation of EC TF expression, and cleavage of VWF [36–
recent study on the frequency of donor-derived ECs in various 39]. The net effect of deficient PR3 expression in PNH
tissues in allogeneic transplant recipients demonstrated that therefore requires further study.
only a minority of ECs originate from donor HSCs [28]. A The exact contribution of missing GPI-APs to PNH-
high frequency of GPI-deficient ECs in PNH thus seems related thrombosis is unclear. Despite a significant reduction
unlikely, suggesting that direct complement damage to GPI- in thrombosis risk during eculizumab treatment, the propor-
deficient ECs is relatively less important in endothelial tion of leukocytes and platelets lacking GPI-APs remains
activation. However, studies in liver transplant patients unchanged, or even increases in erythrocytes, arguing against
showed that recipient-derived ECs do repopulate the liver a major role for GPI-AP deficiency itself. Alternatively,
allograft [29]. Also, this study showed that, in bone marrow- patients with congenital deficiency of PIGM, another gene
transplanted mice, the liver endothelium, in contrast to other that is essential in GPI anchor synthesis, frequently suffer
organs, is partially or even completely composed of donor- from thrombosis but do not have hemolysis [40]. This would
derived ECs. These results indicate that, particularly in the suggest an important contribution of GPI-deficient cells to
liver, there might be a role for GPI-deficient bone marrow- thrombosis that is independent of hemolysis; however, in
derived ECs in PNH. these patients, all ECs are supposedly GPI-deficient, and thus
these may be the culprits.
Ó 2011 International Society on Thrombosis and Haemostasis
4 S. T. A. van Bijnen et al
Adhesion and aggregation studies performed by Grünewald
Effects of free hemoglobin and nitric oxide (NO) depletion
et al. [53] showed impaired function of PNH platelets, which
Intravascular hemolysis increases free hemoglobin levels. can be potentially explained by reactive downregulation in
Normally, free hemoglobin is rapidly cleared from the response to chronic hyperstimulation. Together with shed-
circulation by several scavenging mechanisms, such as binding ding of the MAC from the platelet membrane by vesicula-
to haptoglobin. Excessive intravascular hemolysis saturates tion, other receptors may also be lost, resulting in reduced
these scavengers, resulting in free hemoglobin in plasma, function.
which mediates direct proinflammatory, proliferative and pro-
oxidant effects on ECs [41]. Free hemoglobin irreversibly
Microparticle formation
reacts with NO to form nitrate and methemoglobin. Lysed
erythrocytes release arginase, which catalyzes the conversion Microparticles are small membrane-derived vesicles that are
of arginine, the substrate for NO synthesis, to ornithine. Both shed upon activation, inflammation, or cell damage. Under
processes decrease NO availability. NO normally maintains normal conditions, the plasma membrane is composed of
smooth muscle cell (SMC) relaxation, inhibits platelet activa- anionic phospholipids such as phosphatidylserine (PS) on the
tion and aggregation, and has anti-inflammatory effects on the inner leaflet, and choline-based phospholipids (sphingomyelin
endothelium. Through these mechanisms, decreased NO levels and phosphatidylcholine) on the outer leaflet. Membrane
may increase the thrombotic tendency in PNH (reviewed in asymmetry is lost upon cell stimulation, leading to PS
[19]). Levels of free hemoglobin in PNH patients do indeed exposure on the outer leaflet of the cell membrane, followed
strongly correlate with NO consumption and arginase levels. by cytoskeletal degradation and microparticle release. PS
Correlation of thrombotic events with low NO levels was, exposure on the surface of either microparticles or the cell
however, not tested in this study, as this would require large membrane provides a surface for the assembly of the
patient numbers [42]. In venous thrombosis though, a role for procoagulant enzyme complexes prothrombinase (FVa/
NO depletion is doubtful, as veins lack SMCs and platelets FXa) and tenase (FVIIIa/FIXa), which catalyze coagulation
contribute relatively little to venous thrombosis. Its definitive [54,55].
role, particularly in arterial thrombosis, still requires further Complement activation at the cell surface of GPI-deficient
research. cells may stimulate the release of procoagulant microparticles,
increasing the risk of thrombosis. Several studies have inves-
tigated this hypothesis. In vivo, the total level of microparticles
Platelet function
exposing PS, as measured by a prothrombinase-based assay,
Platelet activation has been proposed to play a role in PNH- was higher in PNH patients than in healthy controls. These
related thrombosis. Whereas normal platelets express both microparticles were predominantly of platelet origin. No
CD55 and CD59, these complement inhibitors are absent on correlation was found with PNH clone size in any lineage
PNH platelets [43,44]. However, while complement destroys [56]. In contrast, Simak et al. [21] used flow cytometry to
PNH erythrocytes, it probably does not directly destroy PNH enumerate PS-exposing microparticles, but did not confirm
platelets, owing to their ability to shed the MAC [45]. Although increased levels in PNH. A drawback of these studies is that
thrombocytopenia is frequent in PNH, it is generally attributed they did not quantify microparticle TF content, which strongly
to concomitant bone marrow failure and not to complement- enhances their procoagulant properties [57]. C5a was shown to
mediated damage. In two small studies of 16 patients, the induce monocyte TF expression and release of TF-containing
lifespan of the total platelet population was normal in the microparticles, a phenomenon that might be enhanced on GPI-
majority of patients [46,47]. Furthermore, the observation that, deficient leukocytes. Simak et al. [21], however, found normal
during eculizumab treatment, both PNH platelet clone size and leukocyte-derived microparticle levels, although monocyte
platelet count remain stable fits the notion that platelets survive origin was not specified. A case report of two PNH patients
complement-mediated platelet destruction [9,48,49]. with severe recurrent thrombosis did show increased levels of
Although complement does not directly destroy platelets, it circulating leukocyte-derived TF as compared with healthy
can induce platelet activation. Even on normal platelets, controls [58].
assembly of the MAC results in FV secretion from a- In vitro, PNH platelets release significantly more micropar-
granules, increased prothrombinase activity, and the release ticles than normal platelets upon MAC stimulation, as was
of platelet microvesicles in vitro [50]. As blocking CD59 on shown by Wiedmer et al. [52]. In vivo though, platelet micro-
normal platelets enhances these procoagulant responses [51], particle numbers were not significantly different from those in
a similar response to MAC assembly would be expected in healthy controls, although the variability between patients was
GPI-deficient PNH platelets. In vitro studies by Wiedmer consistently higher than between healthy donors. This implies
et al. [52] showed that PNH platelets did indeed expose more that a subgroup of patients may have higher microparticle
FVa-binding sites and increased thrombin generation more concentrations [21,56].
than normal platelets upon MAC stimulation. Ex vivo Remarkably, the levels of erythrocyte microparticles were
studies provided some evidence for in vivo platelet activation similar in PNH patients and healthy controls [21,56]. However,
[24], but these findings were not confirmed by others [43,53]. in vitro experiments did show that PNH erythrocytes release
Ó 2011 International Society on Thrombosis and Haemostasis
Thrombosis in PNH 5
higher amounts of procoagulant microparticles upon comple-
Role of the various mechanisms in the localization of
ment stimulation [59,60]. The fact that these microparticles are
thrombosis in PNH
not readily detected in vivo may suggest rapid clearance from
the circulation, implying that their clinical relevance is doubt- An intriguing but still unresolved question in the pathophys-
ful. iology of PNH-related thrombosis is its predilection for the
The predictive value of microparticle levels for thrombosis in venous system, in particular in the abdomen and brain. The
PNH is unknown. In patients with deep vein thrombosis and most frequent manifestation is Budd–Chiari syndrome (41–
pulmonary embolism, the levels of TF-containing microparti- 44% of PNH patients with thrombosis). Other frequently
cles were not elevated [61,62]. In cancer patients, however, affected sites include other intra-abdominal veins, intradermal
TF-containing, but not PS-expressing, microparticles did veins, the central nervous system, and the limbs [2,5,15,18].
predict thrombosis [63,64]. If relevant in PNH, this probably The answer to this question probably involves EC-specific
applies most to TF-containing microparticle levels; however, procoagulant and anticoagulant properties, which are highly
these levels are unknown so far. variable in different vascular beds (reviewed in [70,71]). The
specific localization of thrombosis in PNH supports the idea
that the endothelium is probably a major contributor. For
Fibrinolysis and anticoagulation
example, TFPI is preferentially expressed in the microvascu-
Impairment of fibrinolysis or anticoagulation can increase the lature. High TFPI mRNA levels are found in human lung and
tendency for thrombosis. Such impairment may result from liver tissue, and murine brain ECs [70,72]. If GPI-deficient ECs
deficiency of the GPI-anchored urokinase plasminogen acti- are present in these tissues, a lack of TFPI may have a great
vator (u-PA) receptor (u-PAR, CD87). u-PA converts plas- effect.
minogen into plasmin and, in doing so, is involved in The various mechanisms involved in PNH-related throm-
fibrinolysis and the degradation of extracellular matrix during bosis may differentially affect vascular beds. NO depletion
tissue remodeling and cell migration. Binding of u-PA to u- probably promotes arterial thrombosis via its effects on SMC
PAR enhances plasmin formation and, via this mechanism, and platelet activation and not, or to a lesser extent, venous
fibrinolysis remains localized pericellularly. u-PAR is indeed thrombosis. Bacterial and food antigens present in the mesen-
deficient on PNH leukocytes and platelets [65,66]. Plasma teric and portal veins may locally activate complement,
levels of soluble u-PAR are higher than in healthy controls, resulting in a higher hemolytic rate and consequent endothelial
and correlate with PNH granulocyte clone size [65–67], damage, platelet activation, and microparticle release, and
suggesting that u-PAR without the GPI anchor cannot bind possibly also in direct complement-mediated damage to GPI-
to the cell membrane. Thus, it may be released from GPI- deficient ECs.
deficient cells and compete with membrane-bound u-PAR for
binding of u-PA [68]. The resulting decrease in local u-PA
Frequency of congenital and acquired thrombophilia factors is
availability could increase the thrombotic risk in PNH. In a
not increased in PNH
study of 78 patients, high soluble u-PAR levels were
independently associated with thrombotic risk [66]. Arguing There is no evidence that the prevalence of known genetic
against a role for u-PAR deficiency, however, is the finding factors predisposing to thrombosis is increased in PNH
that u-PAR-deficient mice do not display spontaneous patients. The frequency of FV Leiden in 66 PNH patients
thrombosis [69]. was similar to that in healthy controls [73]. Other studies
Studies that have measured other fibrinolysis parameters reported normal levels of antithrombin, protein C, protein S
in PNH report conflicting results and do not unanimously and homocysteine in small series of PNH patients, and also
fit with global fibrinolysis impairment, as may result from similar frequencies of FV Leiden and methylenetetrahydrofo-
u-PAR deficiency [22–24]. Gralnick et al. and Helley et al. late reductase (MTHFR) and prothrombin mutations [74,75].
found normal levels of the fibrinolysis inhibitors a2-anti- In another study of 16 patients, one had FV Leiden, one had a
plasmin, plasmin–antiplasmin (PAP) complexes, and plasmin- heterozygous prothrombin mutation, and two had a homozy-
ogen activator inhibitor-1 (PAI-1), and of the fibrinolysis gous MTHFR mutation [22]. Of these patients with congenital
activator tissue-type plasminogen activator (t-PA) [23,24]. In thrombophilia factors, two experienced thrombotic events, as
contrast, Grünewald et al. demonstrated a slightly lower compared with two of 12 patients without thrombophilia.
level of plasminogen, and higher levels of D-dimer and the Although the frequency of genetic thrombophilia factors in
fibrinolysis activation markers PAP and tPA–PAI-1 com- PNH was apparently not increased in these relatively small
plex, suggesting active fibrinolysis. These changes were studies, testing for such factors may identify PNH patients at
inversely correlated with clone size, pointing to progressive additional risk. However, its value in unselected patients with
impairment in patients with higher clone sizes [22]. Levels venous thrombosis for prediction of thrombosis recurrence is
of the thrombin-activatable fibrinolysis inhibitor throm- limited [76]. Its value for treatment decisions in PNH is
bomodulin and the anticoagulant proteins antithrombin, unknown, and we therefore do not recommend routine testing.
protein C and protein S were normal in PNH patients Lupus anticoagulant was not found in two studies of, in
[22–24]. total, 26 patients, including patients with a history of venous
Ó 2011 International Society on Thrombosis and Haemostasis
6 S. T. A. van Bijnen et al
thrombosis [22,77]. Dragoni et al. found antiphospholipid patients, a transjugular intrahepatic portosystemic shunt
(APL) antibodies in five patients with and in three patients (TIPS) was placed successfully in six of seven eligible patients
without thrombosis in a series of 13 PNH patients, whereas [80]; however, TIPS placement may be associated with
in the study of Darnige et al., APL antibodies were present additional complement activation, and does not resolve
in only three of 20 patients [75,77]. Again, patient numbers thrombosis. Thrombolytic therapy with t-PA can be an
were small, and do not allow definitive conclusions to be alternative in potentially life-threatening thrombotic events,
drawn. especially when a response to conventional anticoagulation is
The JAK2-V617F mutation is frequently found in myelo- lacking. Araten et al. described nine patients in whom t-PA
proliferative diseases (MPDs). Like PNH, MPD is associated treatment resulted in resolution of the thrombus. However, in
with a high risk of thrombosis at similar locations, raising the one patient, bleeding may have contributed to a fatal outcome
question whether the JAK2-V617F mutation is involved in [81,82]. As eculizumab has been observed to abrogate a cascade
PNH as well. No JAK-V617F mutations were found by of thrombotic events, prompt initiation of eculizumab may be
Fouassier et al. [78] in 11 PNH patients with varying clone sizes attempted, as this is a much safer strategy in view of the
(range: 0.5–92%), including three patients with thrombosis, substantial bleeding risk associated with thrombolysis [83]. The
whereas Sugimori et al. [79] reported three classic PNH role of other anticoagulants, such as the newly developed
patients with JAK-V617F mutations among 21 PNH patients thrombin inhibitors, in the treatment or secondary prophylaxis
with Budd–Chiari syndrome. Interestingly, the JAK-V617F of thrombosis has not been investigated.
mutation was found in PIGA-mutated but not in normal cells.
More research on this aspect is warranted.
Eculizumab
The availability of the humanized anti-C5 mAb eculizumab has
Prevention and treatment of thrombosis in PNH
dramatically changed the treatment and prognosis of PNH. It
effectively reduces hemolysis, hemoglobinuria, transfusion
Anticoagulant prophylaxis
requirements, and anemia. In addition, symptoms attributed
Owing to the rarity of PNH, no randomized trials evaluating to hemolysis, such as smooth muscle dystonias, pulmonary
the effect of anticoagulant treatment on the risk of thrombosis hypertension, and kidney function, have been shown to
have been performed. Hall et al. retrospectively compared the improve as well, leading to an increased quality of life
frequency of thrombosis in PNH patients with large granulo- [42,48,84–88]. Preliminary data also suggest increased life-
cyte clone sizes (> 50%) between those with and without expectancy [49]. Although it was only retrospectively studied
primary prophylaxis with warfarin. They found no thrombo- with limited follow-up, the rate of thromboembolic events was
embolic events in 30 patients taking warfarin, whereas in 39 also highly significantly reduced during eculizumab treatment
patients without prophylaxis the 10-year thrombosis rate was in comparison with pretreatment rates in the same cohort of
36.5% [7]. Although these data suggest that warfarin effectively PNH patients [3]. The event rate in eculizumab-treated patients
reduces thrombotic risk in PNH, it also represents a risk of was 1.07 per 100 patient-years, vs. 7.37 per 100 patient-years in
bleeding in PNH patients, who frequently have concomitant the same patients pretreatment (P < 0.001).
thrombocytopenia. In the study of Hall et al. [7], two serious
hemorrhages were reported in 39 patients on warfarin.
Proposed effect of eculizumab on hemostasis in PNH
Nevertheless, this study was the basis for the recommendation
of the international PNH interest group to consider vitamin K Eculizumab treatment lowered the plasma levels of coagulation
antagonist (VKA) prophylaxis in patients with a PNH activation markers (prothrombin fragments 1 and 2), markers
granulocyte clone > 50% and no contraindications for of fibrinolysis (D-dimer and PAP complex), and markers of EC
prophylaxis [1]. Literature on the efficacy of antiplatelet agents activation (t-PA, sVCAM-1, VWF, and total and free TFPI)
such as acetylsalicylic acid and glycoprotein IIb–IIIa receptor [23,89]. The reduction in thrombotic risk in eculizumab-treated
antagonists in preventing arterial thrombosis in PNH is non- PNH patients suggests a major role for complement activation
existent, although PNH platelets may have a role in the in the pathogenesis of thrombosis in PNH. By blocking C5,
pathophysiology of thrombosis in PNH. PNH platelet activation, damage and microparticle release may
be reduced. Moreover, eculizumab effectively reduces intra-
vascular hemolysis, and thus free hemoglobin levels and NO
Treatment of thrombosis in PNH patients
consumption. It may therefore prevent the detrimental effects
PNH patients with a proven venous thrombosis should be of free hemoglobin on the endothelium, and restore the
treated initially with low molecular weight heparin and VKA, inhibition of platelet activation and aggregation by NO.
according to the regular practice for other patients with venous Unexpectedly, however, eculizumab treatment did not change
thrombosis. Up to now, lifelong anticoagulation has been the total numbers of either PS-exposing microparticles or EC-
recommended for such patients. In rare cases, radiologic derived microparticles, further supporting the idea that micro-
intervention has been considered in patients with acute onset of particles probably do not play a major role [23]. However, a
Budd–Chiari syndrome [1]. In a series of 15 Budd–Chiari decrease in the number of TF-containing microparticles may
Ó 2011 International Society on Thrombosis and Haemostasis
Thrombosis in PNH 7
have been missed with the use of a prothrombinase-based assay role of complement-mediated procoagulant microparticle
to enumerate microparticles. release is less well established. Finally, NO depletion is
probably particularly relevant in arterial thrombosis.
Treating thrombosis in PNH is difficult, as prospective
Eculizumab in the prevention and treatment of thrombosis in
studies are lacking and, even during anticoagulant treatment,
PNH
some patients develop multiple events. Eculizumab has
The major decrease in the thromboembolic event rate and the dramatically improved the quality of life for PNH patients,
improvement in several hemostatic parameters in eculizumab- and probably reduces the thrombotic risk, highlighting the
treated patients raises the question of whether patients major role for complement or complement-mediated hemolysis
receiving eculizumab without a history of thrombosis still in thrombosis in PNH. Although great progress has been
require additional anticoagulant prophylaxis, especially throm- made, important questions remain unanswered: how can we
bocytopenic patients at risk for bleeding. A randomized predict which patients will suffer from thrombosis, and why
controlled clinical trial comparing the incidence of thrombosis does thrombosis occur at unusual locations? Future research is
in eculizumab-treated patients without a history of thrombosis urgently needed to provide answers to these questions.
with and without VKA treatment was never performed. Kelly
et al. reported having stopped warfarin prophylaxis in 21
patients receiving eculizumab who had never had thrombosis. Disclosure of Conflict of Interests
None of these patients developed thrombosis while receiving P. Muus has served on advisory boards of Alexion Pharma-
eculizumab (mean follow-up: 10.8 months) [49]. Although few ceuticals. The other authors state that they have no conflict of
clinical data are currently available, discontinuation of VKA in interest.
patients without a history of thrombosis may be justified. The
international PNH registry may provide more data on this
topic. References
A thrombotic event in PNH is now generally considered to 1 Parker C, Omine M, Richards S, Nishimura J, Bessler M, Ware R,
be a strong indication for prompt initiation of eculizumab Hillmen P, Luzzatto L, Young N, Kinoshita T, Rosse W, Socie G.
treatment [81,90]. Whether, after a thrombotic event, addi- Diagnosis and management of paroxysmal nocturnal hemoglobinuria.
Blood 2005; 106: 3699–709.
tional anticoagulant prophylaxis should be continued lifelong
2 de Latour RP, Mary JY, Salanoubat C, Terriou L, Etienne G, Mohty
in eculizumab-treated patients to prevent recurrence is still a M, Roth S, de Guibert S, Maury S, Cahn JY, Socie G. Paroxysmal
matter of debate. Until now, only anecdotal evidence that nocturnal hemoglobinuria: natural history of disease subcategories.
discontinuation of anticoagulant treatment is safe has been Blood 2008; 112: 3099–106.
reported for three patients receiving eculizumab with a history 3 Hillmen P, Muus P, Duhrsen U, Risitano AM, Schubert J, Luzzatto
L, Schrezenmeier H, Szer J, Brodsky RA, Hill A, Socie G, Bessler M,
of venous and arterial thrombosis (follow-up: 10–42 months)
Rollins SA, Bell L, Rother RP, Young NS. Effect of the complement
[91]. On the other hand, recurrence of thrombosis during inhibitor eculizumab on thromboembolism in patients with paroxys-
treatment with both eculizumab and warfarin in a patient with mal nocturnal hemoglobinuria. Blood 2007; 110: 4123–8.
a history of thrombosis prior to eculizumab was also described 4 Hillmen P, Lewis SM, Bessler M, Luzzatto L, Dacie JV. Natural
[49]. Such cases again illustrate that neither VKA nor history of paroxysmal nocturnal hemoglobinuria. N Engl J Med 1995;
333: 1253–8.
eculizumab offer full protection from recurrent thrombosis,
5 Socie G, Mary JY, De Gramont A, Rio B, Leporrier M, Rose C,
and VKA discontinuation should be carefully considered. Heudier P, Rochant H, Cahn JY, Gluckman E. Paroxysmal nocturnal
haemoglobinuria: long-term follow-up and prognostic factors. French
Society of Haematology. Lancet 1996; 348: 573–7.
Summary and conclusion 6 Hill A, Reid A, Rother RP, Gladwin MT, Collinson PO, Gaze DC,
Lowe A, Guthrie A, Sivananthan MU, Hillmen P. High definition
Thrombosis risk is substantially increased in PNH and
contrast-enhanced MR imaging in paroxysmal nocturnal hemoglo-
correlates with PNH clone size. The development of thrombo- binuria (PNH) suggests a high frequency of subclinical thrombosis.
sis is one of the most important factors negatively influencing Haematologica 2007; 92(Suppl. 2): 24, Abstract 0066.
survival. Thrombotic events in PNH, for reasons that are not 7 Hall C, Richards S, Hillmen P. Primary prophylaxis with warfarin
yet understood, have a predilection for unusual locations in the prevents thrombosis in paroxysmal nocturnal hemoglobinuria (PNH).
Blood 2003; 102: 3587–91.
venous system, such as the abdomen and the central nervous
8 Moyo VM, Mukhina GL, Garrett ES, Brodsky RA. Natural history
system. Its pathogenesis is still not understood, but is likely of paroxysmal nocturnal haemoglobinuria using modern diagnostic
multifactorial. A major contributor is probably endothelial assays. Br J Haematol 2004; 126: 133–8.
damage caused by free hemoglobin and possibly by comple- 9 Jin JY, Tooze JA, Marsh JC, Gordon-Smith EC. Glycosylphosphat-
ment itself. Though difficult to investigate, the presence and idyl-inositol (GPI)-linked protein deficiency on the platelets of patients
with aplastic anaemia and paroxysmal nocturnal haemoglobinuria:
localization of GPI-deficient ECs is a key question to be
two distinct patterns correlating with expression on neutrophils. Br J
answered in future research. Deficiencies of other GPI-APs Haematol 1997; 96: 493–6.
involved in coagulation, such as u-PAR, and less well- 10 Abou AS, El-Haddad B, Wehbe E, Schulz T. Lysis and thrombosis:
characterized proteins, such as TFPI and PR3, possibly add manifestation of the same disease. Am J Hematol 2008; 83: 505–7.
to the thrombotic risk. Although extensively investigated, the
Ó 2011 International Society on Thrombosis and Haemostasis
8 S. T. A. van Bijnen et al
11 Kumar KS, Malet PF, Rutherford C. Paroxysmal nocturnal hemo- Biedermann BC, Seebach JD. Persistence of recipient-type endothe-
globinuria with no evidence of hemolysis presenting as Budd–Chiari lium after allogeneic hematopoietic stem cell transplantation. Hae-
syndrome. Dig Dis Sci 2000; 45: 2238–9. matologica 2011; 96: 119–27.
12 Araten DJ, Thaler HT, Luzzatto L. High incidence of thrombosis in 29 Gao Z, McAlister VC, Williams GM. Repopulation of liver endo-
African-American and Latin-American patients with paroxysmal thelium by bone-marrow-derived cells. Lancet 2001; 357: 932–3.
nocturnal haemoglobinuria. Thromb Haemost 2005; 93: 88–91. 30 Zhang J, Piro O, Lu L, Broze GJ Jr. Glycosyl phosphatidylinositol
13 Le XF, Yang TY, Yang XY, Wang XM. Characteristics of paroxys- anchorage of tissue factor pathway inhibitor. Circulation 2003; 108:
mal nocturnal hemoglobinuria in China. Clinical analysis of 476 cases. 623–7.
Chin Med J (Engl) 1990; 103: 885–9. 31 Maroney SA, Cunningham AC, Ferrel J, Hu R, Haberichter S,
14 Nishimura J, Kanakura Y, Ware RE, Shichishima T, Nakakuma H, Mansbach CM, Brodsky RA, Dietzen DJ, Mast AE. A GPI-anchored
Ninomiya H, Decastro CM, Hall S, Kanamaru A, Sullivan KM, co-receptor for tissue factor pathway inhibitor controls its intracellular
Mizoguchi H, Omine M, Kinoshita T, Rosse WF. Clinical course trafficking and cell surface expression. J Thromb Haemost 2006; 4:
and flow cytometric analysis of paroxysmal nocturnal hemoglobinuria 1114–24.
in the United States and Japan. Medicine (Baltimore) 2004; 83: 32 Maroney SA, Haberichter SL, Friese P, Collins ML, Ferrel JP, Dale
193–207. GL, Mast AE. Active tissue factor pathway inhibitor is expressed on
15 Ziakas PD, Poulou LS, Rokas GI, Bartzoudis D, Voulgarelis M. the surface of coated platelets. Blood 2007; 109: 1931–7.
Thrombosis in paroxysmal nocturnal hemoglobinuria: sites, risks, 33 Basavaraj MG, Gruber FX, Sovershaev M, Appelbom HI, Osterud B,
outcome. An overview. J Thromb Haemost 2007; 5: 642–5. Petersen LC, Hansen JB. The role of TFPI in regulation of TF-induced
16 Poulou LS, Vakrinos G, Pomoni A, Michalakis K, Karianakis G, thrombogenicity on the surface of human monocytes. Thromb Res
Voulgarelis M, Ziakas PD. Stroke in paroxysmal nocturnal haemo- 2010; 126: 418–25.
globinuria: patterns of disease and outcome. Thromb Haemost 2007; 34 von Vietinghoff S, Tunnemann G, Eulenberg C, Wellner M, Cristina
98: 699–701. CM, Luft FC, Kettritz R. NB1 mediates surface expression of the
17 Muus P, Szer J, Schrezenmeier H, Brodsky RA, Bessler M, Socie G, ANCA antigen proteinase 3 on human neutrophils. Blood 2007; 109:
Urbano-Ispizua A, Maciejewski J, Rosse W, Kanakura Y, Khursigara 4487–93.
G, Karnell A, Bedrosian CL, Hillmen P. Evaluation of paroxysmal 35 Jankowska AM, Szpurka H, Calabro M, Mohan S, Schade AE,
nocturnal hemoglobinuria disease burden: the patientÕs perspective. A Clemente M, Silverstein RL, Maciejewski JP. Loss of expression of
Report from the International PNH Registry. Blood (Annual Meeting neutrophil proteinase-3: a factor contributing to thrombotic risk in
Abstracts) 2010; 116: Abstract 1525. paroxysmal nocturnal hemoglobinuria. Haematologica 2011; 96:954–
18 Ray JG, Burows RF, Ginsberg JS, Burrows EA. Paroxysmal noc- 962.
turnal hemoglobinuria and the risk of venous thrombosis: review and 36 Renesto P, Si-Tahar M, Moniatte M, Balloy V, van Dorsselaer A,
recommendations for management of the pregnant and nonpregnant Pidard D, Chignard M. Specific inhibition of thrombin-induced cell
patient. Haemostasis 2000; 30: 103–17. activation by the neutrophil proteinases elastase, cathepsin G, and
19 Rother RP, Bell L, Hillmen P, Gladwin MT. The clinical sequelae of proteinase 3: evidence for distinct cleavage sites within the aminoter-
intravascular hemolysis and extracellular plasma hemoglobin: a novel minal domain of the thrombin receptor. Blood 1997; 89: 1944–53.
mechanism of human disease. JAMA 2005; 293: 1653–62. 37 Raife TJ, Cao W, Atkinson BS, Bedell B, Montgomery RR, Lentz
20 Aharon A, Tamari T, Brenner B. Monocyte-derived microparticles SR, Johnson GF, Zheng XL. Leukocyte proteases cleave von Wille-
and exosomes induce procoagulant and apoptotic effects on endothe- brand factor at or near the ADAMTS13 cleavage site. Blood 2009; 114:
lial cells. Thromb Haemost 2008; 100: 878–85. 1666–74.
21 Simak J, Holada K, Risitano AM, Zivny JH, Young NS, Vostal JG. 38 Villegas-Mendez A, Montes R, Ambrose LR, Warrens AN, Laffan M,
Elevated circulating endothelial membrane microparticles in Lane DA. Proteolysis of the endothelial cell protein C receptor by
paroxysmal nocturnal haemoglobinuria. Br J Haematol 2004; 125: neutrophil proteinase 3. J Thromb Haemost 2007; 5: 980–8.
804–13. 39 Steppich BA, Seitz I, Busch G, Stein A, Ott I. Modulation of tissue
22 Grunewald M, Siegemund A, Grunewald A, Schmid A, Koksch M, factor and tissue factor pathway inhibitor-1 by neutrophil proteases.
Schopflin C, Schauer S, Griesshammer M. Plasmatic coagulation and Thromb Haemost 2008; 100: 1068–75.
fibrinolytic system alterations in PNH: relation to clone size. Blood 40 Almeida AM, Murakami Y, Layton DM, Hillmen P, Sellick GS,
Coagul Fibrinolysis 2003; 14: 685–95. Maeda Y, Richards S, Patterson S, Kotsianidis I, Mollica L, Crawford
23 Helley D, de Latour RP, Porcher R, Rodrigues CA, Galy-Fauroux I, DH, Baker A, Ferguson M, Roberts I, Houlston R, Kinoshita T,
Matheron J, Duval A, Schved JF, Fischer AM, Socie G. Evaluation of Karadimitris A. Hypomorphic promoter mutation in PIGM causes
hemostasis and endothelial function in patients with paroxysmal inherited glycosylphosphatidylinositol deficiency. Nat Med 2006; 12:
nocturnal hemoglobinuria receiving eculizumab. Haematologica 2010; 846–51.
95: 574–81. 41 Wagener FA, Eggert A, Boerman OC, Oyen WJ, Verhofstad A,
24 Gralnick HR, Vail M, McKeown LP, Merryman P, Wilson O, Chu I, Abraham NG, Adema G, van Kooyk Y, de Witte T, Figdor CG.
Kimball J. Activated platelets in paroxysmal nocturnal haemoglo- Heme is a potent inducer of inflammation in mice and is counteracted
binuria. Br J Haematol 1995; 91: 697–702. by heme oxygenase. Blood 2001; 98: 1802–11.
25 Tedesco F, Pausa M, Nardon E, Introna M, Mantovani A, Dobrina 42 Hill A, Rother RP, Wang X, Morris SM Jr, Quinn-Senger K, Kelly R,
A. The cytolytically inactive terminal complement complex activates Richards SJ, Bessler M, Bell L, Hillmen P, Gladwin MT. Effect of
endothelial cells to express adhesion molecules and tissue factor eculizumab on haemolysis-associated nitric oxide depletion, dyspnoea,
procoagulant activity. J Exp Med 1997; 185: 1619–27. and measures of pulmonary hypertension in patients with paroxysmal
26 Murasawa S, Asahara T. Endothelial progenitor cells for vasculo- nocturnal haemoglobinuria. Br J Haematol 2010; 149: 414–25.
genesis. Physiology (Bethesda) 2005; 20: 36–42. 43 Maciejewski JP, Young NS, Yu M, Anderson SM, Sloand EM.
27 la Porta MG, Malcovati L, Rigolin GM, Rosti V, Bonetti E, Trav- Analysis of the expression of glycosylphosphatidylinositol anchored
aglino E, Boveri E, Galli A, Boggi S, Ciccone M, Pramparo T, Mazzini proteins on platelets from patients with paroxysmal nocturnal hemo-
G, Invernizzi R, Lazzarino M, Cazzola M. Immunophenotypic, globinuria. Thromb Res 1996; 83: 433–47.
cytogenetic and functional characterization of circulating endothelial 44 Vu T, Griscelli-Bennaceur A, Gluckman E, Sigaux F, Carosella ED,
cells in myelodysplastic syndromes. Leukemia 2008; 22: 530–7. Menier C, Scrobohaci ML, Socie G. Aplastic anaemia and paroxysmal
28 Mueller RJ, Stussi G, Puga YG, Nikolic M, Soldini D, Halter J, nocturnal haemoglobinuria: a study of the GPI-anchored proteins on
Meyer-Monard S, Gratwohl A, Passweg JR, Odermatt B, Schanz U, human platelets. Br J Haematol 1996; 93: 586–9.
Ó 2011 International Society on Thrombosis and Haemostasis
Thrombosis in PNH 9
45 Sims PJ, Wiedmer T. The response of human platelets to activated 64 Thaler J, Ay C, Weinstabl H, Dunkler D, Simanek R, Vor-
components of the complement system. Immunol Today 1991; 12: mittag R, Freyssinet JM, Zielinski C, Pabinger I. Circulating
338–42. procoagulant microparticles in cancer patients. Ann Hematol 2011; 90:
46 Devine DV, Siegel RS, Rosse WF. Interactions of the platelets in 447–53.
paroxysmal nocturnal hemoglobinuria with complement. Relationship 65 Ploug M, Plesner T, Ronne E, Ellis V, Hoyer-Hansen G, Hansen NE,
to defects in the regulation of complement and to platelet survival Dano K. The receptor for urokinase-type plasminogen activator is
in vivo. J Clin Invest 1987; 79: 131–7. deficient on peripheral blood leukocytes in patients with paroxysmal
47 Louwes H, Vellenga E, de Wolf JT. Abnormal platelet adhesion on nocturnal hemoglobinuria. Blood 1992; 79: 1447–55.
abdominal vessels in asymptomatic patients with paroxysmal noctur- 66 Sloand EM, Pfannes L, Scheinberg P, More K, Wu CO, Horne M,
nal hemoglobinuria. Ann Hematol 2001; 80: 573–6. Young NS. Increased soluble urokinase plasminogen activator recep-
48 Hill A, Hillmen P, Richards SJ, Elebute D, Marsh JC, Chan J, Mojcik tor (suPAR) is associated with thrombosis and inhibition of plasmin
CF, Rother RP. Sustained response and long-term safety of ecu- generation in paroxysmal nocturnal hemoglobinuria (PNH) patients.
lizumab in paroxysmal nocturnal hemoglobinuria. Blood 2005; 106: Exp Hematol 2008; 36: 1616–24.
2559–65. 67 Ronne E, Pappot H, Grondahl-Hansen J, Hoyer-Hansen G, Plesner
49 Kelly RJ, Hill A, Arnold LM, Brooksbank GL, Richards SJ, Cullen T, Hansen NE, Dano K. The receptor for urokinase plasminogen
M, Mitchell LD, Cohen DR, Gregory WM, Hillmen P. Long term activator is present in plasma from healthy donors and elevated in
treatment with eculizumab in paroxysmal nocturnal hemoglobinuria: patients with paroxysmal nocturnal haemoglobinuria. Br J Haematol
sustained efficacy and improved survival. Blood 2011; 117: 6786–92. 1995; 89: 576–81.
50 Sims PJ, Wiedmer T. Induction of cellular procoagulant activity by the 68 Ninomiya H, Hasegawa Y, Nagasawa T, Abe T. Excess soluble uro-
membrane attack complex of complement. Semin Cell Biol 1995; 6: kinase-type plasminogen activator receptor in the plasma of patients
275–82. with paroxysmal nocturnal hemoglobinuria inhibits cell-associated
51 Sims PJ, Rollins SA, Wiedmer T. Regulatory control of complement fibrinolytic activity. Int J Hematol 1997; 65: 285–91.
on blood platelets. Modulation of platelet procoagulant responses by a 69 Bugge TH, Flick MJ, Danton MJ, Daugherty CC, Romer J, Dano K,
membrane inhibitor of the C5b–9 complex. J Biol Chem 1989; 264: Carmeliet P, Collen D, Degen JL. Urokinase-type plasminogen acti-
19228–35. vator is effective in fibrin clearance in the absence of its receptor or
52 Wiedmer T, Hall SE, Ortel TL, Kane WH, Rosse WF, Sims PJ. tissue-type plasminogen activator. Proc Natl Acad Sci USA 1996; 93:
Complement-induced vesiculation and exposure of membrane pro- 5899–904.
thrombinase sites in platelets of paroxysmal nocturnal hemoglobinu- 70 Aird WC. Vascular bed-specific thrombosis. J Thromb Haemost 2007;
ria. Blood 1993; 82: 1192–6. 5(Suppl 1): 283–91.
53 Grunewald M, Grunewald A, Schmid A, Schopflin C, Schauer S, 71 Rosenberg RD, Aird WC. Vascular-bed – specific hemostasis and
Griesshammer M, Koksch M. The platelet function defect of parox- hypercoagulable states. N Engl J Med 1999; 340: 1555–64.
ysmal nocturnal haemoglobinuria. Platelets 2004; 15: 145–54. 72 Maroney SA, Ferrel FP, Mast AE. Expression of tissue factor path-
54 Hugel B, Martinez MC, Kunzelmann C, Freyssinet JM. Membrane way inhibitor (TFPI) by brain endothelium. Blood (ASH Annual
microparticles: two sides of the coin. Physiology (Bethesda) 2005; 20: Meeting Abstracts) 2008; 112: Abstract 23.
22–7. 73 Nafa K, Bessler M, Mason P, Vulliamy T, Hillmen P, Castro-
55 Zwaal RF, Schroit AJ. Pathophysiologic implications of membrane Malaspina H, Luzzatto L. Factor V Leiden mutation investigated by
phospholipid asymmetry in blood cells. Blood 1997; 89: 1121–32. amplification created restriction enzyme site (ACRES) in PNH
56 Hugel B, Socie G, Vu T, Toti F, Gluckman E, Freyssinet JM, patients with and without thrombosis. Haematologica 1996; 81: 540–2.
Scrobohaci ML. Elevated levels of circulating procoagulant micro- 74 Griscelli-Bennaceur A, Gluckman E, Scrobohaci ML, Jonveaux P, Vu
particles in patients with paroxysmal nocturnal hemoglobinuria and T, Bazarbachi A, Carosella ED, Sigaux F, Socie G. Aplastic anemia
aplastic anemia. Blood 1999; 93: 3451–6. and paroxysmal nocturnal hemoglobinuria: search for a pathogenetic
57 Owens AP III, Mackman N. Microparticles in hemostasis and link. Blood 1995; 85: 1354–63.
thrombosis. Circ Res 2011; 108: 1284–97. 75 Dragoni F, Iori AP, Pignoloni P, Minotti C, Chiarotti F, Mazzucconi
58 Liebman HA, Feinstein DI. Thrombosis in patients with paroxysmal MG, Mengarelli A, Arcese W, Foa R, Avvisati G. Thrombophilic
noctural hemoglobinuria is associated with markedly elevated plasma screening in patients with paroxysmal nocturnal haemoglobinuria: a
levels of leukocyte-derived tissue factor. Thromb Res 2003; 111: 235–8. pilot study. Br J Haematol 2010; 150: 492–4.
59 Ninomiya H, Kawashima Y, Hasegawa Y, Nagasawa T. Comple- 76 Baglin T, Gray E, Greaves M, Hunt BJ, Keeling D, Machin S, Mackie
ment-induced procoagulant alteration of red blood cell membranes I, Makris M, Nokes T, Perry D, Tait RC, Walker I, Watson H.
with microvesicle formation in paroxysmal nocturnal haemoglobinuria Clinical guidelines for testing for heritable thrombophilia. Br J Hae-
(PNH): implication for thrombogenesis in PNH. Br J Haematol 1999; matol 2010; 149: 209–20.
106: 224–31. 77 Darnige L, de Latour RP, Zemori L, Socie G, Fischer AM, Helley D.
60 Kozuma Y, Sawahata Y, Takei Y, Chiba S, Ninomiya H. Procoag- Antiphospholipid antibodies in patients with paroxysmal nocturnal
ulant properties of microparticles released from red blood cells in haemoglobinuria receiving eculizumab. Br J Haematol 2011; 153:
paroxysmal nocturnal haemoglobinuria. Br J Haematol 2011; 152: 789–91.
631–9. 78 Fouassier M, Girodon F, Cleyrat C, Robillard N, Garand R,
61 Steppich BA, Hassenpflug M, Braun SL, Schomig K, von Beckerath Hermouet S. Absence of JAK2-V617F in paroxysmal nocturnal hae-
O, von Beckerath N, Eckstein HH, Ott I. Circulating tissue factor and moglobinuria-associated thrombosis. Thromb Haemost 2009; 102:
microparticles are not increased in patients with deep vein thrombosis. 180–2.
Vasa 2011; 40: 117–22. 79 Sugimori C, Shain KH, Caceres G, Sokol L, Araten DJ, Maciejewski
62 Garcia RP, Eikenboom HC, Tesselaar ME, Huisman MV, Nijkeuter JP, Zou J, Epling-Burnette PK, List AF. Co-existence of JAKV617F
M, Osanto S, Bertina RM. Plasma levels of microparticle-associated and PIG-A mutations in primary Budd–Chiari syndrome. Blood (ASH
tissue factor activity in patients with clinically suspected pulmonary Annual Meeting Abstracts) 2009; 114: 3193.
embolism. Thromb Res 2010; 126: 345–9. 80 Hoekstra J, Leebeek FW, Plessier A, Raffa S, Darwish MS, Heller J,
63 Zwicker JI, Liebman HA, Neuberg D, Lacroix R, Bauer KA, Furie Hadengue A, Chagneau C, Elias E, Primignani M, Garcia-Pagan JC,
BC, Furie B. Tumor-derived tissue factor-bearing microparticles are Valla DC, Janssen HL. Paroxysmal nocturnal hemoglobinuria in
associated with venous thromboembolic events in malignancy. Clin Budd–Chiari syndrome: findings from a cohort study. J Hepatol 2009;
Cancer Res 2009; 15: 6830–40. 51: 696–706.
Ó 2011 International Society on Thrombosis and Haemostasis
10 S. T. A. van Bijnen et al
81 Luzzatto L, Gianfaldoni G, Notaro R. Management of paroxysmal effect of the complement inhibitor eculizumab on kidney function in
nocturnal haemoglobinuria: a personal view. Br J Haematol 2011; 153: patients with paroxysmal nocturnal hemoglobinuria. Am J Hematol
709–20. 2010; 85: 553–9.
82 Araten DJ, Notaro R, Kernan NA, Boulad F, Castro-Malaspina H, 87 Schubert J, Hillmen P, Roth A, Young NS, Elebute MO, Szer J,
Small TN, Scaradavou A, Magnan H, Prockop SE, Chaffee S, Gon- Gianfaldoni G, Socie G, Browne P, Geller R, Rother RP, Muus P.
sky J, Thertulien R, Tarquini R, Luzzatto L. Thrombolytic therapy for Eculizumab, a terminal complement inhibitor, improves anaemia in
reversal of thrombosis in paroxysmal nocturnal hemoglobinuria (PNH). patients with paroxysmal nocturnal haemoglobinuria. Br J Haematol
Blood (ASH Annual Meeting Abstracts) 2010; 116: Abstract 4239. 2008; 142: 263–72.
83 Schutgens RE, Pruissen-Peeters KA, Muus P. A cascade of throm- 88 Brodsky RA, Young NS, Antonioli E, Risitano AM, Schrezenmeier
boembolic processes in a patient with paroxysmal nocturnal haemo- H, Schubert J, Gaya A, Coyle L, de Castro C, Fu CL, Maciejewski JP,
globinuria terminated by treatment with eculizumab. Thromb Haemost Bessler M, Kroon HA, Rother RP, Hillmen P. Multicenter phase 3
2011; 106: 383–5. study of the complement inhibitor eculizumab for the treatment of
84 Hillmen P, Hall C, Marsh JC, Elebute M, Bombara MP, Petro BE, patients with paroxysmal nocturnal hemoglobinuria. Blood 2008; 111:
Cullen MJ, Richards SJ, Rollins SA, Mojcik CF, Rother RP. Effect of 1840–7.
eculizumab on hemolysis and transfusion requirements in patients with 89 Weitz IC. Thrombosis in paroxysmal nocturnal hemoglobinuria – in-
paroxysmal nocturnal hemoglobinuria. N Engl J Med 2004; 350: 552–9. sights into the role of complement in thrombosis. Thromb Res 2010;
85 Hill A, Rother RP, Hillmen P. Improvement in the symptoms of 125(Suppl. 2): S106–7.
smooth muscle dystonia during eculizumab therapy in paroxysmal 90 Brodsky RA. How I treat paroxysmal nocturnal hemoglobinuria.
nocturnal hemoglobinuria. Haematologica 2005; 90(Suppl. 12): Blood 2009; 113: 6522–7.
ECR40. 91 Emadi A, Brodsky RA. Successful discontinuation of anticoagulation
86 Hillmen P, Elebute M, Kelly R, Urbano-Ispizua A, Hill A, Rother RP, following eculizumab administration in paroxysmal nocturnal hemo-
Khursigara G, Fu CL, Omine M, Browne P, Rosse W. Long-term globinuria. Am J Hematol 2009; 84: 699–701.
Ó 2011 International Society on Thrombosis and Haemostasis
You might also like
- Thrombotic Thrombocytopenic Purpura and Hemolytic Uremic SyndromeDocument9 pagesThrombotic Thrombocytopenic Purpura and Hemolytic Uremic SyndromeRex RuthorNo ratings yet
- Virchow TriadDocument6 pagesVirchow Triadarif 2006No ratings yet
- (2005) AAP Thrombocytopenia in ChildhoddDocument11 pages(2005) AAP Thrombocytopenia in ChildhoddFabiola Vania FeliciaNo ratings yet
- 11-Paroxysmal Nocturnal HaemoglobinuriaDocument6 pages11-Paroxysmal Nocturnal HaemoglobinuriaHamid IqbalNo ratings yet
- Aplastic Anemia - An Overview: DR Aniruddh Shrivastava Guided By: DR S.H. Talib SIRDocument42 pagesAplastic Anemia - An Overview: DR Aniruddh Shrivastava Guided By: DR S.H. Talib SIRdoctoranswerit_84161No ratings yet
- 3032 Full PDFDocument12 pages3032 Full PDFcinosure1No ratings yet
- Diagnosis and Management of Paroxysmal Nocturnal HemoglobinuriaDocument11 pagesDiagnosis and Management of Paroxysmal Nocturnal Hemoglobinuriaida ayu agung WijayantiNo ratings yet
- Contemporary Management of Major Haemorrhage in Critical CareDocument13 pagesContemporary Management of Major Haemorrhage in Critical CareYo MeNo ratings yet
- Review ArticleDocument10 pagesReview ArticleXena Poetri Xaverya RenggaNo ratings yet
- Coagulation DisordersDocument26 pagesCoagulation DisordersLia pramitaNo ratings yet
- Polisitemia VeraDocument4 pagesPolisitemia VeraJicko Street HooligansNo ratings yet
- Thrombocytopenia: An Update: K. J. Smock, S. L. PerkinsDocument10 pagesThrombocytopenia: An Update: K. J. Smock, S. L. PerkinsRevathy GunaseelanNo ratings yet
- Coagulation DisordersDocument26 pagesCoagulation DisordersLia pramita0% (1)
- Immune Thrombocytopenic Purpura: 3. DiagnosisDocument3 pagesImmune Thrombocytopenic Purpura: 3. DiagnosisAy'oe Ithyu RezthuNo ratings yet
- Nephrotic Syndrome in Adults: Acute Medicine 2018 17 (1) : 36-43 36Document8 pagesNephrotic Syndrome in Adults: Acute Medicine 2018 17 (1) : 36-43 36Deddy TriwijayaNo ratings yet
- Diagnosis and Management of PNHDocument12 pagesDiagnosis and Management of PNHapi-26302710No ratings yet
- Paroxysmal Nocturnal Hemoglobinuria: March 8, 2005Document46 pagesParoxysmal Nocturnal Hemoglobinuria: March 8, 2005Farina ReenaNo ratings yet
- Liver International - 2016 - Peck Radosavljevic - Thrombocytopenia in Chronic Liver DiseaseDocument16 pagesLiver International - 2016 - Peck Radosavljevic - Thrombocytopenia in Chronic Liver DiseaseLaila Kurnia PramonoNo ratings yet
- Primary and Secondary Thrombocytosis in ChildhoodDocument13 pagesPrimary and Secondary Thrombocytosis in ChildhoodSofia RuanoNo ratings yet
- 2007 Nov 07 CompleteDocument62 pages2007 Nov 07 CompleteKay BristolNo ratings yet
- Pathology Bleeding DisordersDocument67 pagesPathology Bleeding DisordersMarcelliaNo ratings yet
- How I Treat Essential ThrombocythemiaDocument12 pagesHow I Treat Essential ThrombocythemiaJicko Street HooligansNo ratings yet
- Pancytopenia and BicytopeniaDocument12 pagesPancytopenia and BicytopeniaRonny DoankNo ratings yet
- Vasoplegic Syndrome Following Cardiothoracic Surgery-Review of Pathophysiology and Update of Treatment Options - PMCDocument21 pagesVasoplegic Syndrome Following Cardiothoracic Surgery-Review of Pathophysiology and Update of Treatment Options - PMCluis orlando bustamante rojasNo ratings yet
- 10 Pulmonary HypertensionDocument14 pages10 Pulmonary HypertensionVictor PazNo ratings yet
- Wa0004.Document17 pagesWa0004.nhunhuochachNo ratings yet
- Bleeding and Coagulation Disorders: DR Nidhi Chaurasia JR-1 MDS PedodonticsDocument66 pagesBleeding and Coagulation Disorders: DR Nidhi Chaurasia JR-1 MDS PedodonticsDrNidhi KrishnaNo ratings yet
- Cardiovascular ProtectionDocument8 pagesCardiovascular ProtectionJags BuddyNo ratings yet
- Spontaneous Bleeding in Thrombocytopenia - Is It Really Spontaneou 2018Document7 pagesSpontaneous Bleeding in Thrombocytopenia - Is It Really Spontaneou 2018Janner S-RNo ratings yet
- Ijccm 23 S185 PDFDocument4 pagesIjccm 23 S185 PDFSambit DashNo ratings yet
- ZabalaDocument9 pagesZabalaZulqi SusiloNo ratings yet
- Literature AbdoDocument20 pagesLiterature AbdothestaffforpediatricptNo ratings yet
- Portal Vein Thrombosis: ReviewDocument9 pagesPortal Vein Thrombosis: ReviewMahmoud AbouelsoudNo ratings yet
- Defining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsDocument7 pagesDefining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsZikry AuliaNo ratings yet
- Miyata 2006Document7 pagesMiyata 2006Mestre O ToloNo ratings yet
- Ppendix Olor IguresDocument16 pagesPpendix Olor IguresChamara Mudalinayaka100% (1)
- 234 FullDocument8 pages234 FullLaura Daniela MurilloNo ratings yet
- Thrombocytopenia in CirrhosisDocument4 pagesThrombocytopenia in Cirrhosismy accountNo ratings yet
- Noncirrhotic Portal Hypertension: ReviewDocument6 pagesNoncirrhotic Portal Hypertension: ReviewIsrael BlancoNo ratings yet
- Should Aspirin Be Used For Thrombotic Events in Patients With Membranous NepropathyDocument3 pagesShould Aspirin Be Used For Thrombotic Events in Patients With Membranous NepropathyEda SopNo ratings yet
- Venous ThromboembolismDocument14 pagesVenous ThromboembolismCélia BetkaouiNo ratings yet
- PDFSNDocument9 pagesPDFSNShanaz NovriandinaNo ratings yet
- Hematology 2012 Falanga 571 81Document11 pagesHematology 2012 Falanga 571 81Zikry AuliaNo ratings yet
- Thrombosis Research: Simon Mantha, Martin S. Tallman, Sean M. Devlin, Gerald A. So FFDocument5 pagesThrombosis Research: Simon Mantha, Martin S. Tallman, Sean M. Devlin, Gerald A. So FFStephan Arvid Skog MarambioNo ratings yet
- Thrombotic Thrombocytopenic PurpuraDocument5 pagesThrombotic Thrombocytopenic PurpuraAhsan Tanio DaulayNo ratings yet
- Idiopathic Thrombocytopenic Purpura: Pathophysiology and ManagementDocument9 pagesIdiopathic Thrombocytopenic Purpura: Pathophysiology and ManagementAnonymous 0SYzMqje2No ratings yet
- Coagulopatia y Sepsis EngDocument10 pagesCoagulopatia y Sepsis Engadrian mendoza croesNo ratings yet
- Disorder of PlateletsDocument27 pagesDisorder of PlateletsRoby KieranNo ratings yet
- Bone Marrow Failure 2008-09Document15 pagesBone Marrow Failure 2008-09Karan BhattNo ratings yet
- Chap 4 Blood HemoDocument23 pagesChap 4 Blood HemoDianne GalangNo ratings yet
- Crux 70 PDFDocument12 pagesCrux 70 PDFNona NonicaaNo ratings yet
- Rheumatology 2010 Hepburn 2243 54Document12 pagesRheumatology 2010 Hepburn 2243 54Desti Siliawati IINo ratings yet
- ALL Pulmonary Leukostasis2Document6 pagesALL Pulmonary Leukostasis2Pratita Jati PermatasariNo ratings yet
- Cytometry Part B Clinical - 2017 - Dezern - ICCS ESCCA Consensus Guidelines To Detect GPI Deficient Cells in ParoxysmalDocument8 pagesCytometry Part B Clinical - 2017 - Dezern - ICCS ESCCA Consensus Guidelines To Detect GPI Deficient Cells in ParoxysmalzafeersmaNo ratings yet
- Hermansky Pudlak Syndrome Report of A Case and Review of The LiteratureDocument5 pagesHermansky Pudlak Syndrome Report of A Case and Review of The LiteraturepushkaradmaneNo ratings yet
- Sepsis-Induced Coagulopathy and Disseminated Intravascular CoagulationDocument8 pagesSepsis-Induced Coagulopathy and Disseminated Intravascular CoagulationVasFel GicoNo ratings yet
- Myeloproliferative Neoplasms: Diagnostic Workup of The Cythemic PatientDocument9 pagesMyeloproliferative Neoplasms: Diagnostic Workup of The Cythemic PatientHashim AhmadNo ratings yet
- Balam I 2012 Compli HipDocument18 pagesBalam I 2012 Compli HipRosario RosarioNo ratings yet
- Pathophysiology of Cerebral Venous Thrombosis - An Overview.Document4 pagesPathophysiology of Cerebral Venous Thrombosis - An Overview.claudio RivasNo ratings yet
- Arun Case CircDocument3 pagesArun Case CircDavin TakaryantoNo ratings yet
- Hu 2013Document5 pagesHu 2013Javier Dario Cifuentes SandovalNo ratings yet
- Arun Case CircDocument3 pagesArun Case CircDavin TakaryantoNo ratings yet
- BCR 2021 241644Document3 pagesBCR 2021 241644Davin TakaryantoNo ratings yet
- FffsfsDocument5 pagesFffsfsDavin TakaryantoNo ratings yet
- Tumor Pituitari: Pembimbing: Ervita Yuda, DR., SPPD, M.Kes Davin Takaryanto, DRDocument34 pagesTumor Pituitari: Pembimbing: Ervita Yuda, DR., SPPD, M.Kes Davin Takaryanto, DRDavin TakaryantoNo ratings yet
- 7MWTW1710YM0Document8 pages7MWTW1710YM0Izack-Dy JimZitNo ratings yet
- Traffic Speed StudyDocument55 pagesTraffic Speed StudyAnika Tabassum SarkarNo ratings yet
- All About Ignition Coils: Technical InformationDocument15 pagesAll About Ignition Coils: Technical InformationTrương Ngọc ThắngNo ratings yet
- New York State - NclexDocument5 pagesNew York State - NclexBia KriaNo ratings yet
- Problems of Spun Concrete Piles Constructed in Soft Soil in HCMC and Mekong Delta - VietnamDocument6 pagesProblems of Spun Concrete Piles Constructed in Soft Soil in HCMC and Mekong Delta - VietnamThaoNo ratings yet
- 14 DETEMINANTS & MATRICES PART 3 of 6 PDFDocument10 pages14 DETEMINANTS & MATRICES PART 3 of 6 PDFsabhari_ramNo ratings yet
- 2023-2024 Draft Benzie County Budget BookDocument91 pages2023-2024 Draft Benzie County Budget BookColin MerryNo ratings yet
- A Comprehensive Review On Renewable and Sustainable Heating Systems For Poultry FarmingDocument22 pagesA Comprehensive Review On Renewable and Sustainable Heating Systems For Poultry FarmingPl TorrNo ratings yet
- COMMUNICATIONS Formulas and ConceptsDocument24 pagesCOMMUNICATIONS Formulas and ConceptsAllan Paul Lorenzo Abando76% (17)
- SHPXXX 20 IS XX 13Document240 pagesSHPXXX 20 IS XX 13Geyciane PinheiroNo ratings yet
- Organization of Brigada Eskwela Steering and Working CommitteesDocument2 pagesOrganization of Brigada Eskwela Steering and Working CommitteesCherry Lou RiofrirNo ratings yet
- Vacuum Dehydrator & Oil Purification System: A Filter Focus Technical Publication D1-14Document1 pageVacuum Dehydrator & Oil Purification System: A Filter Focus Technical Publication D1-14Drew LeibbrandtNo ratings yet
- Easy Pictionary Words: Angel Eyeball PizzaDocument3 pagesEasy Pictionary Words: Angel Eyeball Pizzakathy158No ratings yet
- Phet Body Group 1 ScienceDocument42 pagesPhet Body Group 1 ScienceMebel Alicante GenodepanonNo ratings yet
- Firmware Upgrade To SP3 From SP2: 1. Download Necessary Drivers For The OMNIKEY 5427 CKDocument6 pagesFirmware Upgrade To SP3 From SP2: 1. Download Necessary Drivers For The OMNIKEY 5427 CKFilip Andru MorNo ratings yet
- How To Make Affidavit at Pune Collector OfficeDocument1 pageHow To Make Affidavit at Pune Collector Officejayram1961No ratings yet
- 2 Players The One With Steam BaronsDocument1 page2 Players The One With Steam BaronsBrad RoseNo ratings yet
- As 3789.2-1991 Textiles For Health Care Facilities and Institutions Theatre Linen and Pre-PacksDocument9 pagesAs 3789.2-1991 Textiles For Health Care Facilities and Institutions Theatre Linen and Pre-PacksSAI Global - APACNo ratings yet
- Techgig Open Round CompetitionDocument6 pagesTechgig Open Round CompetitionAnil Kumar GodishalaNo ratings yet
- WS-250 4BB 60 Cells 40mm DatasheetDocument2 pagesWS-250 4BB 60 Cells 40mm DatasheetTejash NaikNo ratings yet
- Sage 200 Evolution Training JourneyDocument5 pagesSage 200 Evolution Training JourneysibaNo ratings yet
- BP Azspu Driver Fatigue & Tiredness Management ProcedureDocument11 pagesBP Azspu Driver Fatigue & Tiredness Management ProcedureEl Khan100% (1)
- CH 3 Revision Worksheet 2 Class 6 CSDocument1 pageCH 3 Revision Worksheet 2 Class 6 CSShreyank SinghNo ratings yet
- 3D Archicad Training - Module 1Document3 pages3D Archicad Training - Module 1Brahmantia Iskandar MudaNo ratings yet
- Eudemon8000E XDocument2 pagesEudemon8000E XGladys Medina100% (1)
- Biotechnology WebquestDocument2 pagesBiotechnology Webquestapi-353567032No ratings yet
- (1895) Indianapolis Police ManualDocument122 pages(1895) Indianapolis Police ManualHerbert Hillary Booker 2ndNo ratings yet
- Final Answers Chap 002Document174 pagesFinal Answers Chap 002valderramadavid67% (6)
- Scientific American - Febuary 2016Document84 pagesScientific American - Febuary 2016Vu NguyenNo ratings yet
- Instructions: This Affidavit Should Be Executed by The PersonDocument1 pageInstructions: This Affidavit Should Be Executed by The PersonspcbankingNo ratings yet