Professional Documents
Culture Documents
Rizal MS - Edit by Dr. SIM-250422
Uploaded by
Rizal Marubob SilalahiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rizal MS - Edit by Dr. SIM-250422
Uploaded by
Rizal Marubob SilalahiCopyright:
Available Formats
LONG CASE REPORT
A CASE OF TETANUS, CHRONIC SUPPURATIVE OTITIS MEDIA, MILD
MALNUTRITION WITH INCOMPLETE IMMUNIZATION
PRESENTED BY:
RIZAL MARUBOB SILALAHI
NATIONAL BOARD EXAMINATION
MAY 20th – 22nd, 2022
INDONESIAN COLLEGE OF PEDIATRIC
TIMELINE
March, 23rd 2022 March, 23rd 2022 S
March, 31st, 2022 May, 22nd, 2022
Patient was Initial
End of follow Reported
admitted to observation
up
hospital
INDONESIAN COLLAGE OF PEDIATRIC PATIENT’S CASE REPORT
I. PATIENT IDENTITY
Name : AA Father : Mr. AH, 31 years old
Age : 10 years 3 months Education : Junior high school
Sex : Male Occupation : Fisherman
Medical Record : 00.85.94.xx Mother : Mrs BS, 29 years old
Admission date : March 23rd, 2022 Education : Senior high school
Examination date : March 23rd, 2022 Occupation : Housewife
II. HISTORY TAKING (Alloanamnesis with parents)
1. History of present illness
Chief complaint: Body stiffness since 2 days prior to hospital admission.
Three weeks prior to hospital admission, a history of discharge from
both ears was experienced. According to his mother, discharge from the ears was
found after the patient often scraped his ears with a matchstick. However, the
mother never checked the condition of the ears. His mother thought there wasn’t
any serious condition because his son was not complaining any pain.
Ten days prior to hospital admission, fluid coming out of the ear has
reduced. The patient scraped his ears with cotton buds, but the cotton was left in
his right ear. After that, the patient felt pain in his right ear. He told his mother one
day later, and then the mother brought him to the Primary Health Centre. The
cotton was taken by a general practitioner and given ear drops. Since then, the
patient has felt pain recurrently.
Five days prior to hospital admission, jaw muscle stiffness was
found. At that time, his mouth locked up but still can eat per oral with a bit
difficulty to open mouth and swallow.
Two days prior to hospital admission, the patient’s body became stiff
and tense so that the patient could not sit and had difficulty walking. The patient
had stiffness on all of his extremities. It lasted less than 5 minutes, stopped by
itself, no glared eyes, stiffness on his body, clenching fists, the back arched,
without fever, and no impaired consciousness. It happened more than 3 times per
day with the same pattern. Jaw muscle stiffness was still found, so the patient
had difficulty speaking and eating. Stiffness around his neck was found. His body
was stiff whenever his father or mother cuddled, touched, or picked him up.
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 1
Stiffness stimulated with a strong voice, touch and light was found. Due to these
complaints, his mother took him to the nearest hospital and was advised to be
hospitalized. The patient had been treated for 1 day and then referred to Adam
Malik General Hospital because no improvement was seen.
On the day of admission, at the emergency room, the patient was alert.
There was no pale, icteric, cyanosis, oedema, and dyspnea. Body stiffness, neck and
jaw muscle stiffness were found. His mouth locked up and he also had difficulties
to speak and swallow. Arched posturing still found, no risus sardonicus. Until
admission, the patient still had stiffness that occurred spontaneously and by
stimulation. Ears were a bit discharge. No prior history of fever, diarrhea, or vomit.
There is no history of caries dentis. There is no history of animal bite. Defecation
and urination are within normal limits.
2. History of previous illness
The patient had been treated for 1 day at the previous hospital. He received
ceftriaxone injection therapy 1 gr/12 hours, novalgin injection 500 mg/8 hours,
dexamethasone injection 2 mg/8 hours, and was referred with a diagnosis of
tetanus.
3. Family History
There was no family history of tetanus. Only the patient had this complaint in the
family.
Tabel 1. Family Member
No Relationship with Sex Age Details
patient
1. Father Mother Patient M 31 years old Healthy Healthy
2. Young brother F 29 years old Healthy
3. M 2 years old
4.
Conclusion: No history of similar illness in the family. All members of family are
healthy
4. Personal and social history
a. Pregnancy history. During pregnancy, the mother had no regular prenatal
check-up at health center. She did not have any significant illness and the
mother was healthy during pregnancy. He was the first planned pregnancy of a
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 2
19 years old mother. There was no history of fever, diabetes mellitus, and
hypertension during pregnancy. The quality of nutritional intake during
pregnancy was adequate.
Conclusion: Normal pregnancy history.
b. Delivery history. The patient was born live, aterm, with spontaneous delivery
at a maternity clinic and assisted by a midwife. He was aterm, vigorous, cry
immediately and without cyanosis. Birth weight was 2900 grams, body length
48 cm and head circumference were unrecalled. Conclusion: Normal
delivery history.
c. Postnatal history. There was no history of yellowish, bluish, pale, and seizure
after birth. Patient was never hospitalized before.
Conclusion: Normal postnatal history.
d. History of nutritional intake. The patient was breastfed from birth up to 1
year and 3 months. Supplementary feeding of breast milk was started from the
age of 2 month in the form of milk porridge two times daily. At six to twelve
months, he consumed soft rice 3 times a day with chicken liver or egg. Breast
milk was continued. From one to three years old, he was given rice with family
menu, 3 times a day with ½-1 adult portion and biscuits as snack. Since three
years old, the children eat family food 3 times a day that contain1-2 portions of
rice according to the children’s will with side dishes such as fish, egg or
chicken. He prefers not to eat fruit nor vegetable and he never gets formula
milk. In the last two years, the patient eats 1 portion of rice, 2 times daily with
side dishes of fish and chicken and likes to eat 1-2 pieces of fried tofu, tempe
and biscuits as his snacks. Food recall daily is 1500 kcal.
Conclusion: Nutritional intake was inadequate both in quality and
quantity.
e. Growth and developmental history.
The patient was able to sit without support by the age of 6 months, stand by
the age of 9 months, and walk at the age of 12 months. His parents did not
clearly remember other developmental status. Right now, he is in the fourth
grade of primary school and can follow the lesson well. He loves to eat snacks
with his friends.
Conclusion: Appropriate developmental with excess of growth.
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 3
f. Immunization status. BCG scar was found on the right upper arm. The
mother claimed that the patient only received Hepatitis B vaccination once at
birth, polio oral and BCG when returning home from maternity clinic and after
that, he never gets other immunizations.
Conclusion: Immunization status was incomplete.
g. Fulfilment of basic needs.
Biological. The patient received adequate primary needs (food, clothes and
shelter). He received a home meal two times a day. When he gets sick, his
parent took him to the nearest health facility in the area.
Emotional Needs. The patient received sufficient attention and affection
from the parent and other family members, especially his mother. His mother
accompanies him while staying in hospital.
Mental stimulation. The patient loves to play with other kids of the same
age at school. He can follow his educational degree well. His parents always
support him. He performs well at school.
Conclusion: The patient received adequate basic needs from his
family.
h. Family social economics status and environment.
Social Economic. The patient’s father and mother were married in 2010,
first marriage, when the father was 19 years old and the mother was 17
years old. Their monthly income is approximately Rp2.000.000 per month.
Mother is Javanese, Muslim, senior high school graduate, housewife. Father
is Malay, Muslim, junior high school graduate, fisherman. Currently, patients’
Healthcare expenses are covered by government health insurance (BPJS).
Environment. The patient lives with both of his parents and one brother in a
6 x 10 m2 permanent house with tin roof, concrete wall, and cement floor.
The house consists of two bedrooms and one bathroom located inside the
house. The source of electricity from the government electric company.
Water resource is from government water company and refilled water.
Healthy facility around the patient’s house is primary health care with a
distance of approximately 1 km.
Conclusion: Low social-economic level
III. PHYSICAL EXAMINATION when observing patient (March 23 rd, 2022)
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 4
• General examination: Alert; there were no icteric, cyanosis, oedema and dyspnea.
Body stiffness and jaw muscle stiffness were found, stiffness stimulated by touch
and light still found, arched posturing still found. Heart rate 110 bpm, regular (normal
60-120 bpm); Respiratory rate was 22 cpm, regular (normal 16-20 cpm); Axillary
temperature was 36,8°Celsius; Blood pressure was 110/70 mmHg (p50-90 th: 97-
112/58-73 mmHg); Oxygen saturation 99 % without oxygen supplementation.
• Nutritional status and anthropometry: Patient’s body weight was 22 kg (weight
for age was 66%), height was 131 cm (>p5th), ideal body weight was 27 kg (weight
for height was 81%). Head circumference was 52 cm (p>-2nd Nellhaus curve). Height
age was 8 years 6 months old. Father’s height was 168 cm and mother’s height
was 155.5 cm with genetic potential of height was 159-176 cm.
Conclusion: Underweight, normal stature and mild malnutrition.
• Head: There is no risus sardonicus. Eyes: isochoric pupils (equal 3 mm diameter),
reactive to light, no pale on conjunctiva palpebra inferior. Ears were a bit
discharge, membrane tympanic of both ears has perforated. Nose: No nasal flare.
Mouth: Trismus was found 2 cm. Neck: neck stiffness was found, no cervical
lymph node enlargement, the jugular venous pressure was R-2 cmH2O.
• Heart: Inspection: Ictus cordis was not visible; Palpation: No thrill was palpable,
ictus cordis 5-6th left intercostal space midclavicular line; Auscultation: Heart rate
110 bpm, heart sound I- II normal, no murmur.
• Lung: Inspection: Symmetrical fusiform, no retraction; Auscultation: Respiratory
rate 22 cpm, vesicular, no rales and wheezing.
• Abdominal: Inspection: no distension, no rigidity; Palpation: Soft palpable,
tenderness, mass, liver, and spleen were not palpable; Percussion: Tympani, no
shifting dullness; Auscultation: Normal bowel sound.
• Back: No deformity or gibus. Opisthotonus was found.
• Extremities: Warm, equal peripheral and central pulse, capillary refill time < 2
seconds, no oedema, palmar and plantar not pallor.
• Genital: Male, palpable testicle bilateral, volume 2 cc, penis size 5.5 cm, puberty
status A1G1P1
IV. WORK UP
1. Laboratory (March, 23rd, 2022 at 1.38 a.m): Complete Blood Count: Haemoglobin
(Hb) 12.3 mg/dl, hematocrit 36.2%, leukocytes 9,760 /uL, platelet 410,000/uL MCV
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 5
78 fl, MCH 26.6 pg, MCHC 34 g/dl, neutrophil 72.3%, lymphocyte 21.6%. Blood
glucose 107 mg/dl. Electrolytes : Sodium 140 mEq/L, Potassium 4.2 mEq/L,
Chlorida 106 mEq/L. Urinalysis : Color: Clear / pH 6 / Nitrite (-) / Protein (-) / Keton
(-) / Glucose (-) / Urobilinogen (-) / Bilirubin(-) / Nitrites : Negative / Blood (-) /
Rapid Antigen Covid 19 : Negative
V. SUMMARY
A 10- years 3-months-old male was admitted on March 23 rd,2022 at 1
a.m with the chief complaint is body stiffness. This has been experienced by the
patient for 2 days before entering the hospital. The body is stiff and tense so that
the patient cannot sit and difficulty walking. The patient had stiffness on all of his
extremities. It lasted less than 5 minutes, stopped by itself, no glared eyes,
stiffness on his body, clenching fists, the back arched, no impaired of
consciousness. It happened more than 3 times per day with the same pattern.
Jaw muscle stiffness was found so that the patient was difficult to speak and eat.
5 days prior admission, his mouth locked up but still can eat per oral with a bit
difficulty to open mouth and swallow. Stiffness around his neck was found. His
body was also stiff whenever his father or mother cuddled, touched, or picked
him up. Stiffness stimulated by a strong voice, touch and light is found. History of
fever, diarrhea and vomiting were not found. History of discharge from both ears
experienced three weeks ago, where according to his mother, discharge from the
ears was found after the patient often scrapes his ears with a matchstick, but his
mother never checked the condition of the ears. Ten days prior to hospital
admission, the patient scraped his ears with a cotton bud, but the cotton was left
in his right ear. The patient felt pain in his right ear. He told his mother one day
later, then the mother brought him to the Primary Health Centre and the cotton
was taken by a general practitioner and given ear drops. Since this time, the
patient has felt pain recurrently. Based on physical examination, the patient was
alert. Vital sign was normal. From anthropometry, it could be inferred that
nutrition status was mild malnutrition. Trismus was found 2 cm. There is no risus
sardonicus. Tympanic membrane is perforated on both ears and the fluid
coming out of the ear has reduced. Neck stiffness was still found. Abdominal
rigidity was not found. Opisthotonic posturing was found. The patient only
received Hepatitis B vaccination once at birth, polio oral and BCG when returning
home from maternity clinic and after that, he never gets other immunizations.The
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 6
laboratory result was normal. Therapy and monitoring of the patient were
continued.
VI. DIFFERENTIAL DIAGNOSIS
1. Tetanus (A.35) + Chronic Supurative Otitis Media ADS (H.67) + Mild Malnutrition
(E44.1) + Incomplete Immunization (Z28.3)
2. Abses peritonsil (J.39.0) + Chronic Suppurative Otitis Media ADS (H.67) + Mild
Malnutrition (E44.1) + Incomplete Immunization (Z28.3)
3. Meningitis (G03.9) + Chronic Suppurative Otitis Media ADS (H.67) + Mild
Malnutrition (E44.1) + Incomplete Immunization (Z28.3)
VII. WORKING DIAGNOSIS
Tetanus (A.35) + Chronic Suppurative Otitis Media ADS (H.67) + Mild
Malnutrition (E44.1) + Incomplete Immunization (Z28.3)
VIII. PROBLEM LIST
1. Tetanus
Diagnosis: anamnesis, physical examination
Management :
- Maintain a dark and quiet room for the patient, with minimal
handling
- Supportive care: IV fluid hydration and nutrition, prevention of
complication
- Antimicrobial therapy
- Control of muscle spasms with spasmolytics
- Neutralize of toxin
Prognosis: Depend on age, incubation period, period of onset, type of
tetanus and immunization status.
Prevention: Having complete immunization
2. Chronic Suppurative Otitis Media ADS
Diagnosis: anamnesis, physical examination
Management :
- Consult to Ear, Nose, and Throat Department
- Ear toilet
- Antibiotics
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 7
Prognosis: Good
Prevention: Ear hygiene
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 8
3. Mild Malnutrition
Diagnosis: anamnesis, physical examination and anthropometry as
recommended by CDC.
Management :
- Diet management
Prognosis: Good
Education: Parents had been told about the programme to increase the body
weight which targeting to high calories. The family were suggested to arrange
daily menu based in basic feeding rule.
4. Incomplete Immunization
The patient will be recommended to take other immunization which has not
been given before:
1) Hepatitis B
2) MR
3) Td vaccine
4) Oral Polio, IPV
VIII. MANAGEMENT
1. Management of emergencies
Maintain airway, breathing, circulation
Maintain adequate hydration
Give Diazepam 0.1-0.3 mg/KgBW/iv to control spam. If spasm is not
adequately controlled, neuromuscular blocking agents are used and transfer
to an intensive care unit urgently. If the patient has no IV line, give rectal
diazepam 5 mg for children under 10 kg, and rectal diazepam 10 mg for
children more than 10 kg.
2. Plans for investigation and diagnosis
Complete blood count, electrolyte, glucose ad random
Consultation plan:
Nutrition and Metabolic Disease Division
Ear, Nose and Throat Department
Pediatric Growth and Development Division
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 9
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 10
3. Medical Treatment
a) Tetanus
Metronidazole drips loading dose 15 mg/KgBW intravenously, follow by
Metronidazole drips with maintenance dose 30 mg/KgBW/day iv divided
4 doses, 170 mg/6 hours/iv for 10 days.
Diazepam injection with maintenance dose 4 mg/KgBW/day/iv given
every 3 hours, with maximal dose 25 mg/KgBW/day.
Human Tetanus Immunoglobulin (HTIG) 3000 IU/ IM
Injection of Td 0.5 ml/IM
b) Chronic Suppurative Otitis Media ADS
H202 3% 3x gtt 5 ADS
c) Mild Malnutrition
Determined nutrition status
Based on anthropometric with CDC curve it has inferred that the patient
had severe underweight and mild malnutrition.
Determined daily calories needs
Calculating calory needs targeting increasing body weight by formula
RDA x Ideal Body Weight. RDA is based on age and patient's ideal
height for 8 years and 6 months is 80 kcal/KgBW, then calory needs is
2000 kcal.
Determined feeding route Diet was given per NGT
Determined food formula
Patient was given oral nutrition supplements 250 cc/ 3 hours /NGT
Monitoring and evaluation
Determining diet acceptance, tolerance, and clinical recovery.
4. Follow Up Plan
Monitoring general condition and spasm
Monitoring vital sign
Monitoring tolerance or acceptability of liquid diet
Monitoring therapies response and side effect during treatment
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 11
5. Communication, Information and Education
Explanation about the illness (cause, therapy, complication, treatment
planning and side effect, follow-up, prevention, and prognosis).
Spasm monitoring during medication and side effect that might happen.
Explanation for nutrition status patient and programme to maintain his diet
to increase the body weight.
Motivating family to give support during the treatment.
Inform to patient’s family that hygiene is important such as ear hygiene,
dental hygiene, and wearing slippers when going outdoor.
Planning to catch up immunization in patient when patient’s condition has
stabilized.
6. Nursing care:
- Monitoring of vital sign
- General hygiene of the patient
- Hygiene monitoring for parents / caregivers, nurses, medical personnel
- Mental and emotional support
IX. FOLLOW UP (March 23rd-31st, 2022)
1. On the 1st day of treatment in Pediatric isolation ward (March 23 rd, 2022),
Body stiffness and jaw muscle stiffness were found, no fever, no
spontaneous seizure, triggering seizure was found. Patient was full alert,
heart rate was 110 bpm, respiratory rate 22 cpm, blood pressure (BP) was
110/70 mmHg. Temp: 36.7oC BW: 22 Kg; Ear: active discharges (+/+).
Mouth: Trismus 2 cm. Neck stiffness was found, no abdominal rigidity.
2. On the 2nd – 7th day of treatment in Pediatric isolation ward (March 24 rd-
31st 2022), Body stiffness and jaw muscle stiffness decreased until not
found, with no fever. Patient was full alert, heart rate was 94-104 bpm,
respiratory rate 20-22 cpm, blood pressure (BP) was 100-110/70-75 mmHg.
Temp: 36.70C BW: 22-22,5 kg; Ear: the fluid coming out has reduced until no
discharge. Mouth: Trismus 2-3,5 cm. Neck stiffness and opisthotonus were
decreased until not found, no abdominal rigidity, warm acrals, good
perfusion.
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 12
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 13
X. PROGNOSIS
• Quo ad vitam bonam
• Quo ad functionam bonam
• Quo ad sanationam bonam
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 14
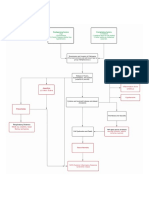
XI. SCHEME
a. Disease course timeline
March, 2022 March, 23rd 2022 March, 24th-30th 2022 March, 31st 2022
5 days prior admission Admission to Follow Up Last Follow Up
Hospital
Jaw muscle Full alert Full alert
stiffness Body stiffness Body stiffness Body
mouth locked up Jaw muscle decrease until stiffness was
but still can eat stiffness not found not found
per oral with a Neck Jaw muscle Neck muscle
bit difficulty to muscle Stiffness decrease Stiffness and
open mouth and stiffness Trismus2-3.5 cm opisthotonus
swallow. Arched posturing Neck muscle were not
Trismus 2 cm Stiffness and found.
2 days prior admission Stiffness Arched posturing Trismus 3.5 cm
triggered by Decreased until No
Body stiffness touch and light not found complication,
Jaw muscle Full alert Spasm triggered condition
stiffness History of by touch has improved
Neck muscle decreased until discharged
scraped his ears
stiffness. not found. with oral
History of DPT
His mouth locked immunization diazepam
up with difficulty to was not found Therapy : Planned for
open mouth,speak Inj. Diazepam further
and swallow. Therapy : Drip consultation in
Arched Inj. Diazepam metronidazole outpatient care
posturing Inj. HTIG Isolation in quite,
Stiffness triggered Drip metronidazole dark room
by stimulation Inj. Tdap
Full alert Treat in isolation
room
Picture 1. Timeline of illness scheme
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 15
Table 2. FOLLOW UP DURING HOSPITALIZATION
March 24th – 26th 2022 March 27th – 31st 2022
Subjective Subjective
Trismus persists, with improvement. Trismus improvement. Stiffness improve
Stiffness improve, no fever and no until not found, no fever and no dyspnea.
dyspnea. Mouth can open a bit.
Objective Objective
Vital sign: Fully alert, BP P50-90, HR Vital sign: Fully alert, BP P50-90, HR 94-
90-105 bpm, regular, RR 20-22 bpm. 104 bpm, regular, RR 20-22 bpm.
Temperature 36.8-370C General Temperature 36.6-36.80C General
examination: Body stiffness and Jaw examination: Body stiffness and Jaw muscle
muscle Stiffness decrease. Ear: the fluid Stiffness decrease until not found. Ear: the
coming out has reduced; Neck: stiffness fluid coming out has reduced until no
decrease; Mouth: trismus improvement discharge; Neck: stiffness decrease until not
(mouth open 2-2,5 cm); Cardiac: no found; Mouth: trismus improvement (mouth
abnormalities, Limbs: no swelling, warm open 2.5-3 cm); Cardiac: no abnormalities,
acrals, good perfusion, opisthotonus Limbs: no swelling, warm acrals, good
improvement. perfusion, opisthotonus not found.
Assessment Assessment
Tetanus (A.35) + Chronic Suppurative Tetanus (A.35) + Chronic Suppurative Otitis
Otitis Media ADS (H.67) + Mild Media ADS (H.67) + Mild Malnutrition
Malnutrition (E44.1) + Incomplete (E44.1) + Incomplete Immunization (Z28.3)
Immunization (Z28.3)
Plan Plan
1. Metronidazole 170 mg/6 hours/iv daily 1. Metronidazole 170 mg/6 hours/iv daily for
for 10 days.
10 days. 2. Diazepam 11 mg/3 hours/iv
2. Diazepam 11 mg/3 hours/iv 3. H202 3% 3x gtt 5 ADS
3. H202 3% 3x gtt 5 ADS 4. Liquid and semi-solid food 2000 kcal per
4. Oral nutrition supplements 250 cc/ 3 oral
hours/NGT 5. Monitor: clinical symptoms, vital signs,
5. Monitor: clinical symptoms, vital signs, spasm,oral intake tolerance.
spasm,oral intake tolerance 6. Switch diazepam oral and tapering off
diazepam.
7. Planned for further consultation in
outpatient Care.
8. Catch-up immunization
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 16
XII. Scheme of Case Analysis
RISK Low Economic History of DPT
Level Scraped ears immunization (-)
Male, 10 years 3
months
PROBLEM Tetanus
Generalized
Clinical
Neonatorum
Manifestation
Cephalic
Diagnosis Local
Treatment :
- HTIG : Textbook of Pediatric Infectious Disease, 2009. Level of evidence V, recommendation C)
- Metronidazole (Crit Care. 2014. Level of evidence IIa, recommendation B)
- Diazepam (Cochrane database of systematic reviews. 2004. Level of evidence Ib,
Recommendation A)
Prognosis
Good Prognosis
(Trop Med Int Health. 2006. Level of
evidence IIb) recommendation
B).)
Immunization
Catch Up
Biological
Improved Family Support Emotional
needs
Growth and
Development Mental
stimulation
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 17
X. CASE ANALYSIS
Tetanus, a vaccine-preventable disease, is an acute illness manifested by
neuromuscular dysfunction due to a potent exotoxin, tetanospasmin, produced by
Clostridium tetani, a motile, gram-positive, spore-forming obligate anaerobe whose
natural habitat worldwide is soil, dust and the alimentary tract of various animals.
Tetanus spores can survive boiling but not autoclaving, whereas the vegetative cells
are killed by antibiotics, heat and standard disinfectans. 1,2
Transmission is primarily through contaminated wounds. The wound may be
minor or major. In fact, in about 25% of cases in developed countries, the portal of
entry is not evident at the time of diagnosis. Tetanus may follow surgery, burns,
puncture wounds, otitis media, animal bites, oral infections, and childbirth. However,
tetanus is not contagious from person to person. 3 In this case, the portal entry for
tetanus in patients is due to his scraped ears that are not properly managed.
The toxin primarily affects inhibitory pathways, preventing the release of glycine
and γ-amino butyric acid (GABA). A failure to inhibit motor reflexes happens when
interneurons inhibiting alpha motor neurons are affected. This causes increased
muscle tone and rigidity, interposed by sudden and potentially devastating muscle
spasms. Muscles of the face are affected early because of their short axonal
pathways. The toxin does not affect the mental status and consciousness is not
directly impaired.4,5
Tetanus is most often generalized but may also localize. The incubation period
(the time from exposure to the appearance of symptoms) of tetanus is usually between
3-21 days (median of 7 days). Shorter incubation periods (<7 days) along with delays
in seeking treatment are associated with fatal outcomes. Symptoms arise 1-2 weeks
after infection.4,6 In this case, the patient's first clinical symptom is jaw muscle
stiffness, which experienced about 10 days after the patient has been scraped his
ears. Three days later, the whole body feels stiff until it forms arched posturing and
body stiffly stiffening.
On the basis of clinical findings, four different forms of tetanus have been
described. The most common type (about 80%) of reported tetanus is generalized
tetanus. The disease usually presents with a descending pattern. The first sign is
trismus or lockjaw, followed by stiffness of the neck, difficulty chewing and swallowing.
The sardonic smile of tetanus (risus sardonicus) results from intractable spasms of
facial and buccal muscles. It also may cause rigidity of abdominal muscles and
opisthotonus (the backward arching of the columna due to rigidity of the extensor
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 18
muscles of the neck and back). Other symptoms include elevated temperature,
sweating, elevated blood pressure and episodic rapid heart rate. Spasm may occur
frequently and last for several minutes. Spasms continue for 3-4 weeks.2,7,8
Localized tetanus is the unusual presentation in which patients have persistent
contraction of muscle in the same anatomic area as the injury. These contractions can
last for several weeks with subsequent resolutions.5,7 Cephalic tetanus is a rare form of
the disease. It also occurs in association with otitis media in which C. tetani is present
in the flora of the middle ear or following injuries to the head. There is involvement of
the cranial nerves, especially in the facial area. 2,7
Depending on whether it is local/ cephalic or generalized/neonatal, tetanus
typically manifests as trismus/lockjaw, risus sardonicus, dysphagia, neck stiffness,
abdominal rigidity and opisthotonus. The limbs tend to be less severely affected but
with full opisthotonus there is also flexion of the arms and extension of the legs as in a
decorticate posture. Trismus is frequently the initial symptom in both local/cephalic and
generalized tetanus.8,9 Patient in this case was a generalized form of tetanus which is
found trismus and dysphagia, neck stiffness, body stiffness and history of opisthotonus
at home.
Tetanus is diagnosed by history and clinical presentation and has minimal
differential diagnosis. A general assessment of tetanus disease severity can be
predicted prior to the onset of symptoms and can assist in determining the timing and
need for airway protection. The duration of the incubation period (from the time of
injury to the first appearance of spasms) is inversely related to the disease severity.
Specific diagnosis of tetanus by routine laboratory tests is difficult. No laboratory
findings are characteristic of tetanus. The diagnosis is entirely clinical and does not
depend upon bacteriologic confirmation. C. tetani is recovered from the wound in only
30% of cases and can be isolated from patients who do not have tetanus. Although a
positive wound culture can support the clinical diagnosis, positive culture in the
absence of symptoms does not indicate that tetanus intoxication will develop.5,7
The severity of tetanus is classified as mild, moderate, severe, and very severe.
This categorizes patients into four grades depending upon the intensity of spasms,
respiratory and autonomic involvement. Currently, Abbllet Classification is the most
widely used classification to assess the severity of tetanus. (Table 2).3,10
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 19
Tabel 3. Classification of severity of tetanus 3,10
Grade Type Sign and symptoms
I Mild Mild to moderate trismus, general spasticity, no
respiratory embarrassment, no spasm, little or no
dysphagia
II Moderate Moderate trismus, well-marked rigidity, mild to moderate
but short spasms, moderate respiratory embarrassment
with an increased respiratory rate greater than 30, mild
dysphagia
III Severe Severe trismus, generalized spasticity, reflex prolonged
spasms, increased respiratory rate
greater than 40, apnoeic spells, severe of dysphagia,
tachycardia greater than 120
IV Very severe Very severe: grade III plus violent autonomic
disturbances involving cardiovascular system. Severe
hypertension and tachycardia alternating with relative
hypotension and bradycardia, either of which may be
persistent.
In this case, there was difficulty in opening his mouth, neck stiffness, and
difficulty swallowing. There was no period of apnea, hypotension or tachycardia.
According to the classification of Ablett, patients included in degree II / moderate
tetanus.
Complication of tetanus includes those directly due to the toxin (laryngeal and
phrenic nerves palsy and cardiomyopathy). Interference with breathing can occur due
to aspiration and laryngospasm. Prolonged spasms, contractions or convulsions may
lead to fractures of long bones or of the sone. Cardiovascular complication namely
tachy/bradycardia, arrhythmias and hypertension may also occur due to stimulation of
the autonomic nervous system. Nosocomial infections are common because of
prolonged hospitalization. Secondary infections may include sepsis, indwelling
catheters, hospital-acquired pneumonia, and decubitus ulcer. Aspiration pneumonia is
a common late complication of tetanus, found in 50-70% of autopsied cases.
Complication of tetanus can be seen in the table below. 3,7 (table 3)
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 20
Tabel 4. Complications of Tetanus3
Systems Complications
Respiratory Apnoe, type I respiratory failure (atelectasis, aspiration pneumonia),
type II respiratory failure (laryngospasm, excess sedation, truncal
spasm), acute respiratory distress syndrome,
complications of ventilation and tracheostomy.
Cardiovascular Tachy/bradycardia, hypo/hypertension, myocardial ischaemia,
arrhythmias, asystole, cardiac failure
Renal Infection, renal failure
Gastrointestinal Ileus, gastric stasis, diarrhea, haemorrhage
Musculoskeletal Vertebral fracture and tendonavulsions during spasms,
temporomandibular joint dislocations, nerve palsies
General Weight loss, thromboembolic phenomenon, decubitus ulcers,
multiple organ dysfunction syndrome (MODS)
Tetanus, when suspected, must be managed promptly and aggressively. The
management of tetanus requires a multidisciplinary team approach. The goals of
treatment include interrupting the production of the toxin, neutralizing the unbound toxin,
controlling muscle spasms, managing dysautonomia and appropriate supportive
management.3,5 Provocation of muscle spasm can be reduced by placing the patient in a
dark and quiet room.11 Reflex spasm occur in most patients and can be triggered by
external stimuli such as noise, touch, or light. 12,13 In this patient, the spasm occurred
by touch stimuli. To minimize the risk of precipitating spasms, the patient should be
nursed in a dark and quiet room
An analysis of microbiological susceptibility of C. tetani isolated from wounds of
patient diagnosed with tetanus showed that initially all were susceptible to penicillin and
metronidazole. Study in Indonesia said that metronidazole has become the drug of
choice and has been used in several health services. Metronidazole is administered
intravenously with an initial dose of 15mg/KgBW, followed by a maintenance dose of 30
mg/KgBW/day at intervals every 6 hours for 7-10 days. Metronidazole is effective in
reducing the number of vegetative forms of C. tetani. As a second line, Procaine
Penicillin can be given with dose 50.000-100.000 U/KgBW 7-10 days.14 While penicillin
and metronidazole are both recommended in treating tetanus, some argue that
metronidazole may be a better option. Based on data, many experts recommended
metronidazole over penicillin.11 (Crit Care. 2014, level of evidence IIa,
recommendation B).
Ganesh Kumar et al.15 found that the patients who received metronidazole
had significantly better outcomes than procaine penicillin. The patients were less likely
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 21
to die in the hospital, showed clinical improvement, and were hospitalized for fewer
days. Free circulating toxin should be neutralized with Human Tetanus Immunoglobulin
(HTIG). HTIG does not affect toxin which already fixed to nerve terminals. As soon as
tetanus is diagnosed, the circulating toxin should be neutralized by administration of
antitoxin before the toxin can bind at distant muscle groups. 2,4
The antitoxin choice of treatment for tetanus is HTIG at a dose of 3000 to
6000 IU, single intramuscular, and a second dose is unnecessary. (Textbook of
Pediatric Infectious Disease, 2009. Level of evidence V, recommendation C). If
HTIG is unavailable, another alternative is equine or bovine derived tetanus antitoxin
(TAT). When TAT is used, it is essential to check for possible sensitivity to horse
serum, desensitization may be needed. Approximately 15% of patients given the usual
dose of TAT experience serum sickness. The usual dose of TAT is 100.000 with half
given intramuscularly and half intravenously.16
Benzodiazepines are the standard therapy for controlling muscle spasms in
tetanus. They have gained popularity over other agents due to their combined muscle
relaxant, anticonvulsant, sedative and anxiolytic effect which can be quite useful in
managing a patient with tetanus. The most popular option with regard to
benzodiazepines is diazepam, which is cheap and available in many resource limited
settings where tetanus is a significant public health problem.11,17 Using diazepam was
associated with better survival rate in children when compared to a combination of
phenobarbitone and chlorpromazine.18 (Cochrane database of systematic reviews.
2004, Level of evidence I, recommendation A).
The recommended dose of diazepam is 0.1 to 0.3 mg/KgBW at intervals of 2
to 4 hours in accordance with the clinical symptoms. The recommended dose for
children under 2 years is 8 mg/KgBW/day given orally in doses of 2 to 3 mg every 3
hours. Clonic spasm can be terminated with diazepam 5 mg rectally for body weight
less than 10 kg and 10 mg rectally for children with body weight of 10 kg or more, or
diazepam intravenously 0.3 mg/KgBW/dose. When the spasm has stopped, diazepam
maintenance dose is continued. After 5-7 days, the dosage of diazepam may be
reduced every third day by approximately 10-20% of the previous dose. 14,17
In this case, the patient was given general treatment by being treated in
dark and quiet isolation room to reduce excitatory spasms, given a maintenance fluid
with D% NaCl 0.45% 20 gtt/min macro, and nutritional support in the form of liquid diet
250 cc/3 hours/NGT. To neutralize the toxin patient was given injections of
tetagam/HTIG 3000 IU/IM, metronidazole drips intravenously to kill the vegetative form
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 22
of C. tetani with maintenance dose of 30 mg/KgBW/days, given in 4 doses 170 mg/6
hours/IV. To control spasms, diazepam injection is given to the patient with a starting
dose of 4 mg/Kg/day divided 8 doses. During monitoring, spasms are no longer found,
the dose of diazepam is reduced by 15%. Body stiffness and trismus were also
reduced.
The average fatality rate associated with tetanus ranges from 25 to 70 percent,
but mortality rates can be reduced to 10 to 30 percent with modern intensive care. The
most important factor that influences outcomes is the quality of supportive care.
Mortality is highest in the very young and the very old age. Cephalic tetanus and
tetanus neonatorum are associated with the highest incidence of death. Early
administration of prophylactic antitoxin markedly increases the frequency of
survival.16/16 An unfavorable prognosis included onset of trismus < 7 days after injury
and the onset of generalized tetanic spasms < 3 days after onset of trismus. The
clinical form of tetanus also influences the outcome. A favorable prognosis is
associated with a long incubation period, absence of fever, and localized disease. The
poor prognostic factors of tetanus are also associated with age > 40 years, shorter
incubation periods (<7 days), and severity of tetanus.2,19
Tetanus outcome assessments can also use Phillips, Dakkar, and Tetanus
Severity Scores (TSS) to predict the prognosis of tetanus. The Phillips score consists
of four variables, namely incubation period, location of infection, immunization status,
and complications with a maximum score of 30, while Dakkar score consists of six
variables: incubation period, time of onset, location of infection, spasm, fever and
tachycardia with scores maximum 6. Between these three instruments, TSS has high
sensitivity and specificity in predicting the outcome of patient with tetanus. (Trop Med
Int Health. 2006. Level of evidence IIb, recommendation B). An assessment of the
severity of tetanus based on TSS to predict the prognosis of tetanus is shown in table
4.20
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 23
In this case, the incubation period is 10 days (>7 days) and the period of onset
is 3 days. Patients are also included in moderate tetanus, and from Tetanus Severity
Score (TSS), the total score obtained was 4. In general, the prognosis of this patient is
good.
Tabel 5. New prognostic score: Tetanus Severity Score (TSS) 20
Characteristics Score
Age (years)
≤ 70 0
71-80 5
> 80 10
Time from the first symptom to admission (days)
≤2 0
3-5 -5
>5 -6
Difficulty breathing on admission
No 0
Yes 4
Co-existing medical conditions
Fit and well 0
Minor illness or injury 3
Moderate-severe illness 5
Severe illness but not immediately life-threatening 5
Immediately life-threatening illness 9
Entry Site
Internal or injection 7
Others (including unknown) 0
Highest systolic blood pressure recorded during first day in hospital (mmHg)
≤ 130 0
131-140 2
> 140 4
Highest heart rate recorded during first day in hospital (bpm)
≤100 0
101-110 1
111-120 2
> 120 4
Lowest Heart rate recorded during first day in hospital (bpm)
≤110 0
> 110 -2
Highest temperature recorded during first day in hospital ( oC)
≤ 38.5 0
38.6-39 4
39.1-40 6
> 40 8
Prognosis has become progressively more favorable in developed countries.
The mortality rate of mild and moderate tetanus in Western countries is presently
about 6%, for severe tetanus it may reach as high as 60%, even in expert centers. The
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 24
course of tetanus extends over 4 to 6 weeks. In a series of Italian patients, the mean
length of stay was 40.3 days. An American series, previous vaccination status was
directly related to the severity of disease, with the case fatality ratio ranging from 6%
for patients who had received one to two doses to 15% for unvaccinated patients. 21
Prevention of tetanus can be done with wound care, administration of
prophylactic ATS and active immunization. Active immunization should begin in early
infancy with combined diphtheria toxoid-tetanus toxoid-acellular pertussis (DTaP)
vaccine at 2,3,4 and 18 months of age, with boosters at 5-7 years (DTaP) and 10-18
years of age (Td/Tdap) and 10 years intervals thereafter throughout adult life with
tetanus and reduced diphtheria toxoid (Td). 2,16 This patient has incomplete
immunization status. Based on national schedule, he only got his BCG and oral polio
vaccination when returning home from maternity clinic and has not received any other
vaccination. Patient is recommended to complete his immunization at the outpatient
care based on national immunization recommendation.
Pediatric malnutrition (undernutrition) is an imbalance between nutrient
requirement and intake, resulting in cumulative deficits of energy, protein, or
micronutrients that may negatively affect growth, development, and other relevant
outcomes. Based on its etiology, malnutrition is either (1) illness related (1 or more
diseases/injuries directly result in nutrient imbalance) or (2) caused by environmental/
behavioral factors associated with decreased nutrient intake/ delivery (or both).
Environmental factors that result in malnutrition or negatively affect its remediation
often involve socioeconomic conditions associated with inadequate food availability or
complicating behavioral disorders such as anorexia and food aversion.22
In peripheral health facilities or in the community, where height is not easily
measured, the circumference of the upper arm can be used in place of the weight for
height z score to identify malnutrition. Using arm circumference will identify a different
population as severely malnourished than using the weight for height z score. 23 The
patient was found to be clinically thin, anthropometrically weight for height was 81 %,
arm circumference was 20 cm, concluded as mild malnutrition with Low social -
economic level.
Patient reported outcomes are increasingly being used in pediatric health
services to evaluate outcomes and to inform clinical decision making from the patient
and family perspective. The Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic
Core Scales is an instrument to evaluate the population health-related quality of life
that has demonstrated good reliability, including in hospitalized pediatric patient. 24 In
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 25
this case, patient revealed no disturbances in physical functioning, social functioning,
and school functioning.
The Pediatric Symptom Checklist-17 (PSC-17) is a screening tool in detecting
psychosocial dysfunction. It is used in children aged 8-15, assisting the primary care
providers to the likelihood of finding any mental health disorder in the patient. 25 In the
case, patient had no internalizing, no externalizing, nor attention problem.
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 26
References of case analysis
1. Tadele H. Clinical profile and outcome of pediatrics tetanus: The experience of a
tertiary hospital in Ethiopia. Ethiop J Health Sci. 2017;27:559-564.
2. Arnon S. Tetanus. In: Kliegman RM, Stanton BF, St.Geme III J, Schor NF,
editors. Nelson textbook of pediatrics. Edisi 20. Philadelphia: Elsevier; 2016. p.
1432-34.
3. Mallick IH, Winslet MC. A review of the epidemiology, pathogenesis and
management of tetanus. Int J Surg. 2004;2:109-112.
4. Taylor AM. Tetanus. Crit Care Pain. 2006;6:101-104
5. Brook I. Current concepts in the management of Clostridium tetani infection.
Expert Rev Anti infect Ther. 2008;6(3):327-36
6. Current recommendations for treatment of tetanus during humanitarian
emergencies. WHO Technical Note. 2010:1-6
7. Thwaites CL, Yen LM. Tetanus. Dalam: Gordon C, Zumla A, penyunting. Tropical
disease. Edisi 22. Philadelphia:Sunders Elsevier. 2008.h.1113-18.
8. Hassel B. Tetanus: Pathophysiology, treatment, and the possibility of using
Botulinum toxin against tetanus-induced rigidity and spasms. Toxins. 2013;5:73-
83.
9. Wilfert C, Hotez P. Tetanus (lockjaw) and neonatal tetanus.In: Gershon A, Hotez
P, Katz S, editor. Krugman’s infectious disease of children. 11 th Edition.
Philadelphia: Mosby. 2004. p. 655-62.
10. Cook TM, Protheroe RT, Handel JM. Tetanus: a review of the literature. Br J
Anaesth. 2001;87(3):477-87.
11. Rodrigo C, Fernando D, Rajapakse S. Pharmacological management of tetanus:
an evidence-based review. Critical care. 2014;18:1-10
12. Bae C, Bourget D. Tetanus. Stat Pearls. 2021 December 1 [accessed February 3 2022].
Available from: https://www.ncbi.nlm.nih.gov/books/NBK459217/
13. Schleiss MR. Tetanus (clostridium tetani). In: Kliegman R, Stanton B, St Geme J, Schor
N, editors. Nelson textbook of pediatrics. Philadelphia: Elsevier; 2016. p. 6253.
14. Tetanus. Dalam: Soedarmo SSP, Garna H, Hadinegoro SSS, Satari HI, editors.
Buku ajar Infeksi dan Pediatri Tropis. Edisi Kedua. 2012.p.322-9
15. Kumar AVG, Kothari VM, Krishnan A, Karnad DR. Benzathine penisillin,
metronidazol, and benzyl penisillin in the treatment of tetanus: a randomized
controlled trial. Ann Trop Med Parasitol. 2004;98(1):59-63
16. Cherry JD, Harisson RE. Tetanus. In: Feigin RD, Demmler-Harrison GJ, Cherry
JD, Kaplan SL, editors. Feigin and Cherry’s Textbook of Pediatric Infectious
Disease. 6th Edition. Philadelphia: Saunders Elsevier:2009. p.1870-80.
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 27
17. Ismoedijanto, Nassirudin M, Prajitno BW. Diazepam in severe tetanus treatment:
case report. Southeast Asian J Trop Med Public Health. 2004;35(1):175-80
18. Okoromah CAN, Lesi AFE. Diazepam for treating tetanus. Cochrane database of
systematic reviews. 2004. Issue 1. Art.No: CD003954.
19. Chalya P, Mabula JB, Dass RM, Mbelenge N, Mshana SE, Gilyoma JM. Ten-
year experiences with Tetanus at a Tertiary hospital in Northwestern Tanzania: A
retrospective review of 102 cases. World J Emerge Surg. 2011;6:20.
20. Thwaites CL, Yen LM, Glover C, Tuan PQ, Nga NT, Parry J, dkk. Predicting the
clinical outcome of tetanus : the tetanus severity score. Trop Med Int Health.
2006;11(3):279-87.
21. Ogunrin O. Tetanus- A review of current concepts in management. Journal of
post graduate medicine. 2009;11:46-59.
22. Mehta NM, Corkins MR, Lyma B, Malone A, Goday PS & American Society for
Parenteral and Enteral Nutrition (ASPEN) Board of Directors. Defining pediatric
malnutrition: a paradigm shift toward etiology‐related definitions. Journal of
Parenteral and Enteral Nutrition.2013:37(4):460-481.
23. Manary, MJ, & Sandige, HL. Management of acute moderate and severe
childhood malnutrition.BMJ. 2008;337:a2180
24. Limbers CA, Ripperger SJ, Heffer RW, & Varni JW. Patient-reported Pediatric
Quality of Life Inventory™ 4.0 Generic Core Scales in pediatric patients with
attention-deficit/hyperactivity disorder and comorbid psychiatric disorders:
feasibility, reliability, and validity. Value in Health. 2011;14(4):521-530.
25. Murphy JM, Bergmann P, Chiang C, Sturner R, Howard B, & Jellinek M. The
PSC-17: subscale scores, reliability, and factor structure in a new national
sample. Pediatrics.2016;138:3.
Evidence based practice journal list :
1. Rodrigo C, Fernando D, Rajapakse S. Pharmacological management of tetanus:
an evidence-based review. Critical care. 2014;18:1-10
2. Cherry JD, Harisson RE. Tetanus. In: Feigin RD, Demmler-Harrison GJ, Cherry
JD, Kaplan SL, editor. Feigin and Cherry’s Textbook of Pediatric Infectious
Disease. 6th Edition. Philadelphia: Saunders Elsevier:2009. p.1870-80.
3. Okoromah CAN, Lesi AFE. Diazepam for treating tetanus. Cochrane database of
systematic reviews. 2004. Issue 1. Art.No: CD003954.
4. Thwaites CL, Yen LM, Glover C, Tuan PQ, Nga NT, Parry J, dkk. Predicting the
clinical outcome of tetanus : the tetanus severity score. Trop Med Int Health.
2006;11(3):279-87.
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 28
ABBREVIATION LIST
ADS Auricula dextra sinistra
BCG Bacille Calmette Guerin
bpm beat per minutes
BMI Body Mass Index
BP Blood pressure
C Celcius
CDC Centers for Disease Control and Prevention
CT scan Computerized tomography scan
cm Centimeter
CRT Capillary refill time
dL deciliter
DPT Difteri Pertusis Tetanus
g gram
GCS Glasgow Coma Scale
GABA Gamma amino butyric acid
Hb Hemoglobin
HDL high-density lipoprotein
Ht Hematocrit
HTIG Human Tetanus Immunoglobulin
IBW Ideal Body Weight
IM Intramuscular
IPV Inactivated Polio Virus
IU International Unit
kcal kilo calorie
Kg kilo gram
kgBW kilogram body weight
L liter
LDL low-density lipoprotein
m meter
mEq milliequivalent
mg milligram
ml milliliter
mmHg milimeter of mercury
MD Maintenance dose
MR Measles Rubella
NGT Nasogastric Tube
RDA Recommended Dietary Allowance
TAT Tetanus antitoxin
TT Tetanus Toxoid
Td Tetanus diphteria
Tdap Tetanus diphtheria acellular pertusis
TSS Tetanusseverity score
tpm times per minute
WHO World Health Organization
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 29
APPENDIX I
Growth Chart
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 30
APPENDIX II
Nellhaus Head Circumference Chart
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 31
APPENDIX III
Mid-Arm Circumference
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 32
APPENDIX IV
Blood Pressure
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 33
APPENDIX V
Tanner Stage
AA, Male, 10 years 3 months
G1P1, testicle volume 2cm/2cm
National Evaluation, May 20th - 22nd 2022, Rizal Marubob Silalahi 34
You might also like
- GAPS Stories: Personal Accounts of Improvement and Recovery Through the GAPS Nutritional ProtocolFrom EverandGAPS Stories: Personal Accounts of Improvement and Recovery Through the GAPS Nutritional ProtocolRating: 5 out of 5 stars5/5 (1)
- Long Case Report Dr. Rizal Marubob Silalahi - PPDS IKA FK USUDocument34 pagesLong Case Report Dr. Rizal Marubob Silalahi - PPDS IKA FK USURizal Marubob SilalahiNo ratings yet
- In the Shadow of Illness: Parents and Siblings of the Chronically Ill ChildFrom EverandIn the Shadow of Illness: Parents and Siblings of the Chronically Ill ChildNo ratings yet
- Case of Tetanus, Otitis Media and MalnutritionDocument32 pagesCase of Tetanus, Otitis Media and MalnutritionRizal Marubob SilalahiNo ratings yet
- Complete Guide for Infant Feeding: Grow Healthily and HappilyFrom EverandComplete Guide for Infant Feeding: Grow Healthily and HappilyNo ratings yet
- Long Case RMS-16Document34 pagesLong Case RMS-16Rizal Marubob SilalahiNo ratings yet
- Case Report on Child with Wilms TumorDocument84 pagesCase Report on Child with Wilms TumorCindy PrayogoNo ratings yet
- CR HSPDocument55 pagesCR HSPCindy PrayogoNo ratings yet
- SKBB II Novita AssaDocument56 pagesSKBB II Novita AssaDessyadoeNo ratings yet
- LC Nur Liya EDITDocument51 pagesLC Nur Liya EDITAbdurrahman HasanuddinNo ratings yet
- Nurul Sylvana Long Case Baru-1 (1) - 1Document42 pagesNurul Sylvana Long Case Baru-1 (1) - 1Abdurrahman HasanuddinNo ratings yet
- LONG CASE DR OcaDocument20 pagesLONG CASE DR OcanurfadillahNo ratings yet
- Local Board Examination AdeDocument41 pagesLocal Board Examination AdeAbdurrahman HasanuddinNo ratings yet
- TIMELINE DIAGRAM: PATIENT'S NEPHROTIC SYNDROME HISTORYDocument44 pagesTIMELINE DIAGRAM: PATIENT'S NEPHROTIC SYNDROME HISTORYMuhammad Rifani KnNo ratings yet
- Child's Dengue Case ReportDocument77 pagesChild's Dengue Case ReportHans NatanaelNo ratings yet
- Case Report on Persistent Allergic Rhinitis, Hypertension and Obesity in a ChildDocument67 pagesCase Report on Persistent Allergic Rhinitis, Hypertension and Obesity in a ChildCindy PrayogoNo ratings yet
- ENT Dr. Angel Case 29 Jan 17.00Document85 pagesENT Dr. Angel Case 29 Jan 17.00Cindy PrayogoNo ratings yet
- Makalah Ce Carissa - 18.08.2020 PK 18.26Document75 pagesMakalah Ce Carissa - 18.08.2020 PK 18.26sumbiaindrianiNo ratings yet
- CR4 - Dea BKDocument45 pagesCR4 - Dea BKThadea Odilia TandiNo ratings yet
- Martini Ulok Edit1Document62 pagesMartini Ulok Edit1RonnyRahardjaNo ratings yet
- Longcase Fix TB MilierDocument42 pagesLongcase Fix TB MilierAbdurrahman HasanuddinNo ratings yet
- 1UN EnglishDocument33 pages1UN EnglishireneaureliaNo ratings yet
- Makalah Long Case MF 21.11Document18 pagesMakalah Long Case MF 21.11Mejestha SimanjuntakNo ratings yet
- CR 1 HansDocument48 pagesCR 1 HansHans NatanaelNo ratings yet
- Longcase MiriawatiDocument17 pagesLongcase MiriawatiMuhammad Ali Syahrun MubarokNo ratings yet
- Growth and Development Case StudyDocument31 pagesGrowth and Development Case StudyLyca Mae AurelioNo ratings yet
- Makalahkoheri 10:7:19Document18 pagesMakalahkoheri 10:7:19PutuIantaParamaSiwiNo ratings yet
- UL Darmawan Murdono EngDocument48 pagesUL Darmawan Murdono EngpermatamoNo ratings yet
- En Longcase Dr. Diah SaputriDocument47 pagesEn Longcase Dr. Diah SaputriPutuIantaParamaSiwiNo ratings yet
- Comprehensive Nursing Health History (Adult)Document5 pagesComprehensive Nursing Health History (Adult)Ciedelle Honey Lou DimaligNo ratings yet
- Adolescent Lupus Case ReportDocument16 pagesAdolescent Lupus Case ReportMuhammad Ali Syahrun MubarokNo ratings yet
- Case Study GastroenteritisDocument28 pagesCase Study GastroenteritisAngelinaNo ratings yet
- Nursing Care Plan Pneumonia With Congenital Heart DiseaseDocument18 pagesNursing Care Plan Pneumonia With Congenital Heart DiseaseKarri Ann Tonel100% (2)
- Pedia Case PreDocument3 pagesPedia Case PreMikkelo SususcoNo ratings yet
- A. Biographical DataDocument6 pagesA. Biographical DataDRANo ratings yet
- Patient TimelineDocument51 pagesPatient TimelineRonnyRahardjaNo ratings yet
- A Care Study ON Normal Spontaneous Vaginal DeliveryDocument35 pagesA Care Study ON Normal Spontaneous Vaginal DeliveryCharlskin LetzNo ratings yet
- Acute Gastroenteritis (AGE) : A Case Study ONDocument28 pagesAcute Gastroenteritis (AGE) : A Case Study ONCedy L. CieloNo ratings yet
- Patient Timeline for Acute Myeloblastic LeukemiaDocument37 pagesPatient Timeline for Acute Myeloblastic LeukemiaRenata YolandaNo ratings yet
- DH - Shafira Herowati F - 1102017213Document38 pagesDH - Shafira Herowati F - 1102017213Shafira HfNo ratings yet
- A Case Study Of Malignant Bilateral Pleural Effusion Secondary To Breast CancerDocument77 pagesA Case Study Of Malignant Bilateral Pleural Effusion Secondary To Breast CancerJacky ChanNo ratings yet
- Lapkaslit CPDocument22 pagesLapkaslit CPRonni Untung HNo ratings yet
- Laporan Kasus Gangguan KecemasanDocument27 pagesLaporan Kasus Gangguan KecemasanNovtiara Dwita PutriNo ratings yet
- Calculus CholecystitisDocument48 pagesCalculus CholecystitisEdderlyn LamarcaNo ratings yet
- Case Study of Placenta PreviaDocument24 pagesCase Study of Placenta Previajeelani saima86% (36)
- Timeline: October 7 2017 October 8 2017 October 12 2017 October 13 2017Document43 pagesTimeline: October 7 2017 October 8 2017 October 12 2017 October 13 2017ireneaureliaNo ratings yet
- Case Study On AGEDocument28 pagesCase Study On AGEzyxert100% (19)
- Premature Infant Case ReportDocument35 pagesPremature Infant Case ReportHandoyo KooNo ratings yet
- Case Report Neurology DivisionDocument82 pagesCase Report Neurology DivisionOlgHaENo ratings yet
- Case Study On PneumoniaDocument31 pagesCase Study On PneumoniaLarah Mae Andog85% (20)
- Correction LuqmanDocument15 pagesCorrection LuqmanLuqman MalekNo ratings yet
- Juvenile Idiopathic Oligoarthritis Case ReportDocument32 pagesJuvenile Idiopathic Oligoarthritis Case ReportMuhammad Rifani KnNo ratings yet
- Care Study 1-5 CorrectionsDocument69 pagesCare Study 1-5 CorrectionsAfricaTeddyNo ratings yet
- BSN 2 Case Study On Family Nursing ProcessDocument13 pagesBSN 2 Case Study On Family Nursing ProcessRainier IbarretaNo ratings yet
- A Case Study On Acute Tonsillopharyngitis: Bulacan State University City of Malolos, Bulacan College of NursingDocument61 pagesA Case Study On Acute Tonsillopharyngitis: Bulacan State University City of Malolos, Bulacan College of NursingHomework PingNo ratings yet
- DR - ERLIN FixDocument31 pagesDR - ERLIN FixFelicia Angela KanzilNo ratings yet
- Nursing Care Plan for Mrs. Yolanda Yambut BenavidezDocument8 pagesNursing Care Plan for Mrs. Yolanda Yambut BenavidezRafi LabNo ratings yet
- Case Write Up on 1-Year-Old Boy with Cough and Rapid BreathingDocument7 pagesCase Write Up on 1-Year-Old Boy with Cough and Rapid Breathinganon_67984147No ratings yet
- Pedia Polyarteritis Nodosa HistoryDocument15 pagesPedia Polyarteritis Nodosa HistoryMar Kristian Vero LumenNo ratings yet
- Case Study Rle - Pedia Charity WardDocument40 pagesCase Study Rle - Pedia Charity WardKrizelle MesinaNo ratings yet
- Morning Report Saturday Night, April 10 2021: Rms / Viy / SriDocument17 pagesMorning Report Saturday Night, April 10 2021: Rms / Viy / SriRizal Marubob SilalahiNo ratings yet
- e-SOAL TRIAL MCQ KANDIDAT ENT AGUSTUS 20062022Document2 pagese-SOAL TRIAL MCQ KANDIDAT ENT AGUSTUS 20062022Rizal Marubob SilalahiNo ratings yet
- PPDS Results RecapitulationDocument54 pagesPPDS Results RecapitulationRizal Marubob SilalahiNo ratings yet
- 2972-Author Form-Prodi RMSDocument1 page2972-Author Form-Prodi RMSRizal Marubob SilalahiNo ratings yet
- 2972-Article Text-10687-1-2-20220208 (2) ManuscriptDocument12 pages2972-Article Text-10687-1-2-20220208 (2) ManuscriptRizal Marubob SilalahiNo ratings yet
- ABSENSI KEGIATAN Divisi TK-PedsosDocument7 pagesABSENSI KEGIATAN Divisi TK-PedsosRizal Marubob SilalahiNo ratings yet
- ABSENSI KEGIATAN DivisiDocument8 pagesABSENSI KEGIATAN DivisiRizal Marubob SilalahiNo ratings yet
- PE.4 - BPEd2NUÑEZ, MYRADocument25 pagesPE.4 - BPEd2NUÑEZ, MYRANuñez MyraNo ratings yet
- Emergency First Aid and CPRDocument15 pagesEmergency First Aid and CPRvhlactaotaoNo ratings yet
- ResumedieteticinternshipDocument1 pageResumedieteticinternshipapi-208833628No ratings yet
- Incidence of Aphasia in Ischemic StrokeDocument9 pagesIncidence of Aphasia in Ischemic StrokeIndia SunshineNo ratings yet
- Antisense Oligonucleotide Biotechnology, Applications and FutureDocument29 pagesAntisense Oligonucleotide Biotechnology, Applications and FuturesurojitarpitaNo ratings yet
- MSDS Sodium CarbonateDocument6 pagesMSDS Sodium CarbonateEndang SupriyatnaNo ratings yet
- Alzheimer's Disease: A Guide to Symptoms, Causes, Stages and TreatmentsDocument16 pagesAlzheimer's Disease: A Guide to Symptoms, Causes, Stages and TreatmentsKathleen DiangoNo ratings yet
- Mal de Ojo (English)Document2 pagesMal de Ojo (English)Tim OrtizNo ratings yet
- Tissues Worksheet Class 9 Chapter 2Document3 pagesTissues Worksheet Class 9 Chapter 2My Fact worldNo ratings yet
- Management of Hypertensive Elderly in Clinical Dentistry: Patcharaphol Samnieng, Kantapong PloydanaiDocument9 pagesManagement of Hypertensive Elderly in Clinical Dentistry: Patcharaphol Samnieng, Kantapong PloydanaiSatya AsatyaNo ratings yet
- NLE 2015 Questions SampleDocument8 pagesNLE 2015 Questions SampleJona Suarez100% (4)
- (Libribook - Com) Integrative Preventive Medicine 1st EditionDocument582 pages(Libribook - Com) Integrative Preventive Medicine 1st EditionDaoud Issa100% (1)
- Novi Lestari 1911304150 B3Document3 pagesNovi Lestari 1911304150 B3FarahNo ratings yet
- Sexual Health Education ToolkitDocument69 pagesSexual Health Education ToolkitEndiNo ratings yet
- Ceklist Obstetric HemorrhageDocument2 pagesCeklist Obstetric HemorrhageSarah SabrinaNo ratings yet
- Kleinman & KleinmanDocument24 pagesKleinman & Kleinmanjigues100% (1)
- 55 Cases in NeurologyDocument419 pages55 Cases in NeurologykhawlahbintialazwarNo ratings yet
- Malrotation and Volvulus Great Ormond Street HospitalDocument1 pageMalrotation and Volvulus Great Ormond Street Hospitalghy7jbj96sNo ratings yet
- 800-Organic Fertilizer For Greenhouse TomatoesDocument10 pages800-Organic Fertilizer For Greenhouse Tomatoesgonzalo_hbNo ratings yet
- Angel Summer Field Report (Max Hospital)Document50 pagesAngel Summer Field Report (Max Hospital)varshasharma05100% (1)
- Discharge PlanDocument4 pagesDischarge Plandeo_gratias14No ratings yet
- Leah Alesna Reyes Et Al vs. Sisters of Mercy Hospital Et Al - gr130547Document4 pagesLeah Alesna Reyes Et Al vs. Sisters of Mercy Hospital Et Al - gr130547Dani EsequeNo ratings yet
- YouTube Promotes BrandsDocument6 pagesYouTube Promotes BrandsSilpi YuliantiNo ratings yet
- COVID-19 Vaccination Certificate from India's Ministry of HealthDocument1 pageCOVID-19 Vaccination Certificate from India's Ministry of HealthDIGITAL 143No ratings yet
- FaciitisDocument17 pagesFaciitisdalaginding clophNo ratings yet
- DuPont History PDFDocument17 pagesDuPont History PDFDefenceDogNo ratings yet
- Incision and DrainageDocument8 pagesIncision and DrainageAbraham ChiuNo ratings yet
- Urinary Tract Infections in ChildrenDocument8 pagesUrinary Tract Infections in ChildrenLorelie AsisNo ratings yet
- Patient Ratio1:4Nurse:Patient Ratio1:6Intensive Care UnitNurse:Patient Ratio1:2Operating Room Nurse:Patient Ratio1:1Emergency RoomNurse:Patient Ratio1:3General Medical-SurgicalDocument53 pagesPatient Ratio1:4Nurse:Patient Ratio1:6Intensive Care UnitNurse:Patient Ratio1:2Operating Room Nurse:Patient Ratio1:1Emergency RoomNurse:Patient Ratio1:3General Medical-SurgicalDarren FloresNo ratings yet
- Samuel VinhoDocument5 pagesSamuel Vinhosamuel rangelNo ratings yet
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Aging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayFrom EverandAging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayNo ratings yet
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouFrom EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouRating: 3.5 out of 5 stars3.5/5 (5)
- Whole Body Barefoot: Transitioning Well to Minimal FootwearFrom EverandWhole Body Barefoot: Transitioning Well to Minimal FootwearRating: 4 out of 5 stars4/5 (16)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)
- Body by Science: A Research Based Program for Strength Training, Body building, and Complete Fitness in 12 Minutes a WeekFrom EverandBody by Science: A Research Based Program for Strength Training, Body building, and Complete Fitness in 12 Minutes a WeekRating: 4.5 out of 5 stars4.5/5 (84)
- Music For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicFrom EverandMusic For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicRating: 5 out of 5 stars5/5 (1)
- Power of 10: The Once-A-Week Slow Motion Fitness RevolutionFrom EverandPower of 10: The Once-A-Week Slow Motion Fitness RevolutionRating: 3.5 out of 5 stars3.5/5 (11)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsFrom EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsRating: 5 out of 5 stars5/5 (95)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (66)
- Endure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceFrom EverandEndure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceRating: 4.5 out of 5 stars4.5/5 (237)
- The Seven Spiritual Laws of Yoga: A Practical Guide to Healing Body, Mind, and SpiritFrom EverandThe Seven Spiritual Laws of Yoga: A Practical Guide to Healing Body, Mind, and SpiritRating: 4.5 out of 5 stars4.5/5 (73)
- Weight Lifting Is a Waste of Time: So Is Cardio, and There’s a Better Way to Have the Body You WantFrom EverandWeight Lifting Is a Waste of Time: So Is Cardio, and There’s a Better Way to Have the Body You WantRating: 4.5 out of 5 stars4.5/5 (38)
- Relentless: From Good to Great to UnstoppableFrom EverandRelentless: From Good to Great to UnstoppableRating: 5 out of 5 stars5/5 (783)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!From EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Rating: 4.5 out of 5 stars4.5/5 (22)
- Not a Diet Book: Take Control. Gain Confidence. Change Your Life.From EverandNot a Diet Book: Take Control. Gain Confidence. Change Your Life.Rating: 4.5 out of 5 stars4.5/5 (124)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (110)
- Roxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingFrom EverandRoxane Gay & Everand Originals: Built for This: The Quiet Strength of PowerliftingRating: 4.5 out of 5 stars4.5/5 (132)
- You: Breathing Easy: Meditation and Breathing Techniques to Relax, Refresh and RevitalizeFrom EverandYou: Breathing Easy: Meditation and Breathing Techniques to Relax, Refresh and RevitalizeRating: 3 out of 5 stars3/5 (5)
- SAS Training Manual: How to get fit enough to pass a special forces selection courseFrom EverandSAS Training Manual: How to get fit enough to pass a special forces selection courseRating: 4 out of 5 stars4/5 (3)
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- Body by Science: A Research Based Program to Get the Results You Want in 12 Minutes a WeekFrom EverandBody by Science: A Research Based Program to Get the Results You Want in 12 Minutes a WeekRating: 4 out of 5 stars4/5 (38)
- Buteyko Breathing Course Manual: For use with the Advanced Buteyko CourseFrom EverandButeyko Breathing Course Manual: For use with the Advanced Buteyko CourseRating: 5 out of 5 stars5/5 (1)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesFrom EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesNo ratings yet
- The Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandThe Yamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (19)
- The Calisthenics Codex: Fifty Exercises for Functional FitnessFrom EverandThe Calisthenics Codex: Fifty Exercises for Functional FitnessRating: 4 out of 5 stars4/5 (9)
- 7 Weeks to 10 Pounds of Muscle: The Complete Day-by-Day Program to Pack on Lean, Healthy Muscle MassFrom Everand7 Weeks to 10 Pounds of Muscle: The Complete Day-by-Day Program to Pack on Lean, Healthy Muscle MassRating: 4 out of 5 stars4/5 (2)