Professional Documents
Culture Documents
Physiotherapy Palliative Care Assessment
Uploaded by
UshaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Physiotherapy Palliative Care Assessment
Uploaded by
UshaCopyright:
Available Formats
Physiotherapy Palliative Care Assessment
Name Date of assessment Consent Y/N
DOB GP DN
H&C Tel No
Address Other professionals Care management
Tel Number Diagnosis
Next of kin
Main problems identified by the patient (subjective assessment)
Recent medical history / treatment Recent investigations (scans / blood tests)
Relevant past medical history Medication
Social history Family support
Accommodation
Bedroom up down
Bathroom up down
Family insight Patient insight
Stairs
Access
Occupation / hobbies
Risks: Handling Y/N Behaviour Y/N Environment Y/N
Pain N/a □
Constant/intermittent
Severity 0-10
Pattern (am/pm/night)________________
Aggravated ________________________
Eased by __________________________
Patient name ___________________ Patient identifier _________________
Name of therapist (PRINT)______________________Signature _________________
Mobility N/A □
Subjective assessment
Issue Y N Details
Bed mobility
Transfers
Stairs
Balance
Falls
Mobility inside
Mobility outside
Mobility aids
Objective assessment/ Shortened Rivermead
Date Key
Turning over 5 – independent
Lying to sitting 4 – independent with aid
Sitting balance 3 – supervision
Sitting to standing 2 with 1
Standing unsupported 1 with 2
Transfers 0 cannot do
Walking indoors
Stairs Level of confidence:
Gait/Aids used
Neurological N/A □
Subjective assessment
Symptom Y N Details
P&N or numbness
Bladder, bowel, saddle parathesia
Visual disturbance or headaches
Muscle weakness
Other
Objective assessment
Muscle testing Sensation
Proprioception
Muscle tone
Range of movement testing N/A □
Name of therapist (PRINT)_______________________ Signature________________
Patient name ___________________ Patient identifier _________________
Respiratory N/A □
Underlying pathology Y N Comment
Pleural effusion
PE
COPD
Infection
SVCO
Subjective
Respiratory symptoms Y N Comment
Chest pain
Cough
Sputum
Haemoptysis
Breathlessness
Breathlessness Y N
Level of Aggravated by
breathlessness
Rest Relieved by
Minimum exertion
Walk short distance Level of anxiety / distress (emotional impact, ADL /
Hills / stairs functional impact)
BORG SCORE
24 hour pattern
Objective
Observation and Auscultation
Exercise tolerance
SaO2
Details of O2 use N/A □
Name of therapist (PRINT)_______________________ Signature ______________
Patient name ___________________ Patient identifier _________________
Fatigue N/A □
History Daily activity pattern * most important
Morning
Afternoon
Aggravated by Evening
Relieved by Sleeping pattern
Appetite / Diet Night
Day
Lymphoedema N/A □
Subjective
History of oedema – (include date of onset, progression, previous management of oedema, previous
cellulitis and management of, patients perception)
Objective Skin Condition Y/N Comments
Observation Dry
Area affected
Fragile / Taut / shiny
Fatty
Fibrotic
Fungal infection
Cobblestoning /
hyperkeratosis
Fungating lesions
Limb shape distortion
Deepened skin folds
Pitting / Oedema
Temperature changes
Lymphorrhoea
Discoloration
Venous signs (staining,
ankle flare, ulceration)
Arterial signs (cyanosis,
IC, red/blue discoloration
when limb dependent
Name of therapist (PRINT) _______________________ Signature __________
Patient name ___________________ Patient identifier _________________
Measurements
Date
Location Circumference Circumference Circumference Circumference
R L R L R L R L
Date Problem List Intervention Goals
Name of therapist (PRINT)_______________________ Signature _______________
You might also like
- Comprehensive Health Assessment of The Older Person in Health and Aged CareDocument24 pagesComprehensive Health Assessment of The Older Person in Health and Aged Carenavdeep1133No ratings yet
- 01 Nursing Note SampleDocument1 page01 Nursing Note Sampletesttest testNo ratings yet
- MED-F-003 OPD Patient Assesment NurseDocument2 pagesMED-F-003 OPD Patient Assesment Nursedrakmalik71No ratings yet
- Initial Evaluation (Date) General DataDocument24 pagesInitial Evaluation (Date) General DataPM LESTER DE LA CRUZNo ratings yet
- Pharmacist Patient Communication and History TakingDocument7 pagesPharmacist Patient Communication and History TakingMuhammad AbubakarNo ratings yet
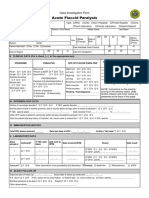
- Case Investigation Form - Acute Flaccid ParalysisDocument2 pagesCase Investigation Form - Acute Flaccid Paralysisclaverialc10No ratings yet
- Case Investigation Forms - Pidsrmop3ed 1Document16 pagesCase Investigation Forms - Pidsrmop3ed 1RHU Dupax del Sur100% (3)
- Template IeDocument24 pagesTemplate IeShan EstanislaoNo ratings yet
- MANZIL-Pre Employment - CV Data Collection TemplateDocument5 pagesMANZIL-Pre Employment - CV Data Collection TemplatePrince Jariz SalonoyNo ratings yet
- Assessment and Management of PainDocument75 pagesAssessment and Management of PainprashantNo ratings yet
- Cagayan de Oro City College of Nursing Assessment Form General InformationDocument11 pagesCagayan de Oro City College of Nursing Assessment Form General Informationdjanggo18No ratings yet
- RevisedDocument16 pagesRevisedZymer Lee AbasoloNo ratings yet
- 2014 06 21 KAB PT Assessment Form - GENERAL PDFDocument12 pages2014 06 21 KAB PT Assessment Form - GENERAL PDFDaniel raja SotardodoNo ratings yet
- Case Report Form For HFMDDocument2 pagesCase Report Form For HFMDMendez RhuNo ratings yet
- CRF HFMD AsmghDocument2 pagesCRF HFMD AsmghRyeowook RyeNo ratings yet
- Case Study 3 CVD Bleed HCVD Type 2 DM CICD Stage 5 WorksheetDocument27 pagesCase Study 3 CVD Bleed HCVD Type 2 DM CICD Stage 5 WorksheetJade HemmingsNo ratings yet
- Physical Therapy Lymphedema Assessment FormDocument4 pagesPhysical Therapy Lymphedema Assessment FormTopaz CompanyNo ratings yet
- Measles Case FormDocument3 pagesMeasles Case FormVlad BăhneanuNo ratings yet
- Acute Flaccid Paralysis: Case Investigation FormDocument2 pagesAcute Flaccid Paralysis: Case Investigation FormBarbie CincoNo ratings yet
- Assessment ToolDocument2 pagesAssessment ToolSarah CruzNo ratings yet
- Pain AssessmentDocument10 pagesPain Assessmentaashika15No ratings yet
- Weekly Case ReportDocument6 pagesWeekly Case ReportAyat AlshawayNo ratings yet
- 6 Pre-Operative Information FormDocument1 page6 Pre-Operative Information FormAina Haravata50% (2)
- Cervical AssesmentDocument3 pagesCervical Assesmentahmadkiblawi884No ratings yet
- Aefi CifDocument4 pagesAefi CifVic KwanNo ratings yet
- Log Book Final YearDocument24 pagesLog Book Final YearAnnie KhanNo ratings yet
- Related Learning Experience Requirements For Medical and Surgical Ward AreasDocument14 pagesRelated Learning Experience Requirements For Medical and Surgical Ward AreasDummy AccountNo ratings yet
- Kause and Effect MOT Intake Form Carrie KauseDocument4 pagesKause and Effect MOT Intake Form Carrie KauseCarrie KauseNo ratings yet
- CheatsheetsDocument2 pagesCheatsheetsprosie392No ratings yet
- Acute Flaccid Paralysis: Case Investigation FormDocument2 pagesAcute Flaccid Paralysis: Case Investigation FormPaul Angelo E. Caliva0% (1)
- Ekstravasation AssesmentDocument2 pagesEkstravasation AssesmentHelena Christy100% (1)
- Clinical Face Sheet: - A.M. - P.M. - A.M. - P.MDocument7 pagesClinical Face Sheet: - A.M. - P.M. - A.M. - P.MRenea Joy ArruejoNo ratings yet
- Health AssessmentDocument12 pagesHealth Assessmentjmzxmdy597No ratings yet
- Elem Sec Health CardsDocument17 pagesElem Sec Health CardsMary Grace CalipesNo ratings yet
- ACI Cognition Screening For Older AdultsDocument2 pagesACI Cognition Screening For Older AdultsBadrun IbrahimNo ratings yet
- Postnatal AssessmentDocument8 pagesPostnatal Assessmentsaritha OrugantiNo ratings yet
- Measles CIF 2014Document2 pagesMeasles CIF 2014RionaMarieMagbutayNo ratings yet
- Peds WW Form1 - 1Document17 pagesPeds WW Form1 - 1Karess AvilloNo ratings yet
- Swallowing ChecklistsDocument5 pagesSwallowing ChecklistsTaylor MayNo ratings yet
- Providence WC Clinic Referral FormDocument3 pagesProvidence WC Clinic Referral FormlisamaurerNo ratings yet
- DM Foot 81Document20 pagesDM Foot 81Zar Ni OoNo ratings yet
- Lumbar Assessment Form FILLABLE Jun 2020Document2 pagesLumbar Assessment Form FILLABLE Jun 2020FejesNo ratings yet
- Soap TemplateDocument3 pagesSoap TemplaterohitNo ratings yet
- Operating Room NotesDocument35 pagesOperating Room NotesMagdaraog Gabrielle A.No ratings yet
- Initial Patient AssessmentDocument8 pagesInitial Patient AssessmentDaniel GalitzineNo ratings yet
- Case Study IcuDocument31 pagesCase Study Icujanna mae patriarcaNo ratings yet
- Surgical Safety Checklist: Feu-Dr. Nicanor Reyes Medical Foundation Medical ReyesDocument1 pageSurgical Safety Checklist: Feu-Dr. Nicanor Reyes Medical Foundation Medical Reyesnictan 14No ratings yet
- NUR 263 Daily Assessment Worksheet Rubric 2024Document12 pagesNUR 263 Daily Assessment Worksheet Rubric 2024vercia8877No ratings yet
- Shoulder PT AssessmentDocument5 pagesShoulder PT AssessmentNEELESH CHOUDHARYNo ratings yet
- Cardiac Tamponade: Tarlac State University College of Science Department of NursingDocument17 pagesCardiac Tamponade: Tarlac State University College of Science Department of NursingKrisianne Mae Lorenzo FranciscoNo ratings yet
- Final NcarDocument47 pagesFinal NcarLeixter Win BalingaoNo ratings yet
- Geriatric Assessment FormDocument3 pagesGeriatric Assessment FormEsmeralda Barnaha100% (1)
- 2 Gordons GeriaDocument7 pages2 Gordons GeriaAiraa ShaneNo ratings yet
- History TakingDocument45 pagesHistory TakingAmmar Hussain MemonNo ratings yet
- Comprehensive Geriatric Assessment Proforma Apr-15Document11 pagesComprehensive Geriatric Assessment Proforma Apr-15Udin Nicotinic100% (2)
- RAD RLE Guide - Written RequirementsDocument5 pagesRAD RLE Guide - Written RequirementsAngelo MadjosNo ratings yet
- Checklist Anxiety DisorderDocument1 pageChecklist Anxiety DisorderUlicer CruzNo ratings yet
- Fitness Form & Hospital ListDocument24 pagesFitness Form & Hospital ListAbhijeetMhatreNo ratings yet
- Pre-Employment Medical Examination (For Leader/ Manager Job Level)Document4 pagesPre-Employment Medical Examination (For Leader/ Manager Job Level)drirajaNo ratings yet
- Picker Nodule, (Prurigo Nodularis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPicker Nodule, (Prurigo Nodularis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Psychology - Psychological AssDocument7 pagesPsychology - Psychological AssUshaNo ratings yet
- Jospt 1984 5 6 348Document25 pagesJospt 1984 5 6 348Hbk RajneeshNo ratings yet
- Highland Physio Inc. Privacy Policy Information For Patient: What Is Personal Information?Document11 pagesHighland Physio Inc. Privacy Policy Information For Patient: What Is Personal Information?UshaNo ratings yet
- Neck Pain and Disability Scale (NPAD) Objectives: Target Population: Method of Use: Validated Languages: ReferencesDocument1 pageNeck Pain and Disability Scale (NPAD) Objectives: Target Population: Method of Use: Validated Languages: ReferencesUshaNo ratings yet
- KOOS Scoring InstructionsDocument3 pagesKOOS Scoring InstructionsUshaNo ratings yet
- Thoracic Outlet Syndrome Patient InformationDocument3 pagesThoracic Outlet Syndrome Patient InformationUshaNo ratings yet
- Anat 6.5 Basal Ganglia - QuijanoDocument6 pagesAnat 6.5 Basal Ganglia - Quijanolovelots1234No ratings yet
- Up 'Til Dawn Position Paper AlsDocument6 pagesUp 'Til Dawn Position Paper AlsBrittany Morgan BooneNo ratings yet
- Fluids and ElectrolytesDocument62 pagesFluids and ElectrolytesLacy Ds FruitNo ratings yet
- Chapter 32 - Anesthesia For Genitourinary SurgeryDocument20 pagesChapter 32 - Anesthesia For Genitourinary SurgeryfewNo ratings yet
- Pediatric Shelf NotesDocument20 pagesPediatric Shelf NotesRajanNo ratings yet
- Dermatology USMLE Step 1, 2 NotesDocument10 pagesDermatology USMLE Step 1, 2 NotesitzjuliiaNo ratings yet
- Test Bank For Interpreting Ecgs A Practical Approach 3rd Edition Bruce ShadeDocument26 pagesTest Bank For Interpreting Ecgs A Practical Approach 3rd Edition Bruce Shadesuspendgruesome1iNo ratings yet
- Introduction PD T2DMDocument6 pagesIntroduction PD T2DMBadr BenzekriNo ratings yet
- Cough, Cold, and Allergy: AntitussivesDocument8 pagesCough, Cold, and Allergy: AntitussivesSalsabila RaniahNo ratings yet
- Towards Better Patient Care Drugs To Avoid in 2024Document11 pagesTowards Better Patient Care Drugs To Avoid in 2024Juan Diego Sánchez BaenaNo ratings yet
- Kubba 2001 (Intervention For Recurren Idiopathix Epistaksis in ChildrenDocument26 pagesKubba 2001 (Intervention For Recurren Idiopathix Epistaksis in ChildrenRaudhah SimahateNo ratings yet
- Oregon Medical Marijuana Act HandbookDocument24 pagesOregon Medical Marijuana Act HandbookornormlNo ratings yet
- Cardiac RehabilitationDocument28 pagesCardiac Rehabilitationshivalingam20No ratings yet
- Anthropometric Measurements: Hameed LatifDocument14 pagesAnthropometric Measurements: Hameed LatifSyeda Zainab AbbasNo ratings yet
- Pediatric JRA: Tan May Vern at Rachel 1000614239Document63 pagesPediatric JRA: Tan May Vern at Rachel 1000614239mayvernNo ratings yet
- Implantable Cardioverter DefibrillatorDocument5 pagesImplantable Cardioverter DefibrillatorvishwanathNo ratings yet
- Ophthalmic Drugs PDFDocument21 pagesOphthalmic Drugs PDFHussain Syed100% (2)
- Grand Case Presentation (MI, COPD and BPH)Document80 pagesGrand Case Presentation (MI, COPD and BPH)Sarah Lim100% (2)
- Carpas PDFDocument678 pagesCarpas PDFAbdulsalam HashiNo ratings yet
- Appendicitis Case StudyDocument35 pagesAppendicitis Case StudyWilliam Soneja CalapiniNo ratings yet
- Hypertension Nursing Care Plan..nkDocument16 pagesHypertension Nursing Care Plan..nkchishimba louisNo ratings yet
- Chapter 10 - The General SurveyDocument5 pagesChapter 10 - The General SurveyNathan WilliamsNo ratings yet
- BALANITISDocument2 pagesBALANITISMel Izhra N. MargateNo ratings yet
- NCM 112 Endterm Care of Clients With Problems in Cellular Aberrations Acute and ChronicDocument8 pagesNCM 112 Endterm Care of Clients With Problems in Cellular Aberrations Acute and ChronicApril FlorendoNo ratings yet
- Diseases of Nerve, Muscle and Neuromuscular JunctionDocument50 pagesDiseases of Nerve, Muscle and Neuromuscular JunctionMalueth AnguiNo ratings yet
- Drug StudyDocument2 pagesDrug Studykev mondaNo ratings yet
- Dermatologic PharmacologyDocument31 pagesDermatologic PharmacologyFor ChristNo ratings yet
- Endoscopic Retrograde Cholangiopancreatogr AHY: Alitre, Noel Christian Postgraduate InternDocument12 pagesEndoscopic Retrograde Cholangiopancreatogr AHY: Alitre, Noel Christian Postgraduate InternJoher MendezNo ratings yet
- Reactive - Arthritis - TextDocument2 pagesReactive - Arthritis - TextSathvika BNo ratings yet
- Endocrine PathologyDocument1 pageEndocrine Pathologyagama_lNo ratings yet