Professional Documents
Culture Documents
Assessment of Fetal Well-Being 1. Fetal Movement
Uploaded by
Claire Julianne CapatiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessment of Fetal Well-Being 1. Fetal Movement
Uploaded by
Claire Julianne CapatiCopyright:
Available Formats
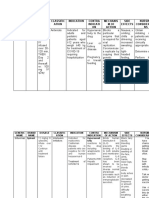
ASSESSMENT OF FETAL WELL-BEING 6.
MATERNAL SERUM ALPHA-FETOPROTEIN
1. FETAL MOVEMENT • a substance produced by the fetal liver that is present in
• can be felt by mother as quickening which begins approx. amniotic fluid and maternal serum; increase in maternal
18-20 weeks of pregnancy and peaks at 28-38 weeks. serum AF indicates open spinal or abdominal defects and
Healthy fetus moves at least 10x a day determine chromosomal defects (down syndrome/trisomy
21)
➢ SANDOVSKY METHOD- mother lying in left recumbent
position after meal and record how many fetal movements 7. TRIPLE SCREENING
she feels over the next hour; normal is twice every 10 • analysis of three indicators (serum alpha fetoprotein,
minute or average of 10-12 x/hr unconjugated estriol and HCG). Together they increase the
detection of trisomy 18 and 21. They are performed between
➢ CARDIFF METHOD- “count to ten”; the mother records the 15 and 22 weeks and considered positive if all markers are
time interval it takes for her to feel ten fetal movements, low
usually occurs within 60mins.
2. FETAL HEART RATE 8. CHORIONIC VILLI SAMPLING
• can be heard and counted as early as the 10-11th week of • biopsy and analysis of chorionic villi for chromosomal
pregnancy by the use of ultrasonic doppler; normal is 120- analysis done at 10 - 12 wks. AOG to determine the fetus’
160 beats/minute chromosomal condition
3. ULTRASOUND 9. AMNIOCENTESIS
• Diagnose pregnancy as early as 6weeks AOG • aspiration of AF from the pregnant uterus for examination at
• Confirm presence, size and location of placental and amniotic 14-16 wks. AOG; test for fetal maturity
fluid • Informed consent, empty bladder, encourage expression of
• Establish presentation and position of the fetus fears and concerns
• Predict maturity by measurement of the biparietal diameter
10. AMNIOSCOPY
4. ELECTROCARDIOGRAPHY (ECG) • inspection of the AF through the cervix and membranes
• recorded as early as 11th week of pregnancy with an amnioscope to detect meconium staining
5. Magnetic Resonance Imaging (MRI) 11. PERCUTANEOUS UMBILICAL BLOOD SAMPLING
(CORDOCENTESIS OR FUNICENTESIS)
• aspiration of blood from umbilical vein for analysis
12. FETOSCOPY • A comparison of blood pressure is made with the woman
• visualizing the fetus by inspection through a fetoscope. lying on her left side and on her back; an excessive increase
Helps in assessing fetal well-being in blood pressure when she rolls to the supine position
indicates increased risk of toxemia
13. BIOPHYSICAL PROFILE • To determine the onset of hypertension and proteinuria
• ombines 4-6 parameters into one assessment: • Mother is positive if diastolic blood pressure increases to 20
Amniotic fluid mm/hg at 5 minute interval
Placental grading and fetal heart activity
Fetal breathing movements
Fetal movement and fetal tone
DIAGNOSTIC TESTS
1. LABORATORY TESTS
• detecting the presence of human chorionic gonadotropin
(HCG), a hormone created by the chorionic villi of the
placenta, in the uterine or blood serum of the pregnant
women
• accuracy: 95-98%
• test are performed by radioimmunoassay (RIA), enzyme-
linked immunosorbent essay (ELISA), radio-receptor assay
(RRA)
2. HOME PREGNANCY TEST
• accuracy: 97%
• not accurate for those who take psychotic drugs like anti-
anxiety agents, also those with oral contraception. Oral
contraception should be discounted 5 days before the test.
Chadwick’s sign- bluish discoloration
3. Roll-Over Test (ROT)
Goodell’s sign- softening of cervix
• Performed to pregnant mother suspected to develop
Hegar’s sign- lower segment of uterus softens
Pregnancy Induced Hypertension (PIH) between
Braxton Hicks- contraction
28th and 32ndweeks of gestation
Ballotement- upward pushing
PHYSIOLOGIC CHANGES IN PREGNANCY: • Lightheaded- due to compression of inferior vena cava
1. Reproductive System: (rolled towel under the woman’s right hip)
A. Uterus:
• Enlarges and thickens 5. Skin color changes- inc. MELANIN production
• Increases in fibro elastic tissue • Striae gravidarum
• Change in shape fr. pear-like to ovoid • Linea negra
• Blood vessels increase in size • Melasma
HEGAR’S SIGN – lower segment softens • Vascular spiders on the thigh (varicose
B. Cervix: • veins)
• Vascular and edematous • Increased perspiration
• GOODELL’S SIGN – softening of the cervix
C. Vagina: 6. Respiration:
• CHADWICK’S SIGN – bluish discoloration • Displaced diaphragm
• LEUKORRHEA - ↑secretion/discharges • Lung expands laterally to compensate for shortness of
breath
2. Abdominal Wall:
• Striae Gravidarum 7. Digestive System:
• Melasma / Chloasma / Mask of Pregnancy • Stomach & intestines are displaced
• Slow stomach peristalsis
3. Breasts: • Delayed stomach emptying
• Feeling of fullness • HEARTBURN/ PYROSIS: regurgitation of acidic stomach
• Hyperplasia contents through the cardiac sphincter into the esophagus
• Darkening of areola Management:
• Secretion of colostrum by 4th month • Avoid fried & fatty foods
• Nipples are erected • Sips of milk at frequent intervals
• Small frequent meals taken slowly
4. Circulation: • Bend at the knees not at waist
• Circulating volume increases 30-50% • Constipation/flatulence
• Physiologic anemia & easily fatigability • Nausea & Vomiting - Eat dry toast, dry cereal before getting
• Increase cardiac output up out of bed
• Decrease circulation to lower extremities, edema, • HYPEREMESIS GRAVIDARUM
varicosities • Hemorrhoids
• Palpitation may occur • Appetite increases after first 3 months
MANAGING DISCOMFORTS OF PREGNANCY
8. Urinary System: FIRST TRIMESTER
• Increases output a. Nausea and vomiting (morning sickness)
• Increases in frequency occurs first 3 months b. Palmar erythema - Calamine lotion
c. Urinary frequency – Kegel’s exercise
9. Musculoskeletal: d. Breast tenderness
• Lordotic position – due to e. Fatigue
backache/fatigue • Waddling gait/ f. Leukorrhea (increased vaginal discharge that is white in
Duck walk – low heeled/flat shoes color)
• Leg cramps due to: g. Headache
Pressure of the gravid uterus
Low calcium, Fatigue/Muscle Tense SECOND TRIMESTER and THIRD TRIMESTER
Management: a. Heartburn/ Heart Palpitations
• Increase calcium intake b. Ankle edema
• Dorsiflex the foot & press the knees c. Varicose veins
• Frequent period of rest d. Hemorrhoids
• Do not massage e. Constipation
f. Backache
10. Weight: g. Leg cramps
• First trimester – allowed: 1.5 – 3 lbs. h. Abdominal Pain
• 2nd and 3rd allowed: 10-11 lbs./trimester i. Shortness of breath
• Total allowable weight gain:20-25lbs/10-12 kg
• Distribution of weight gain: DANGER SIGNS IN PREGNANCY
1. Vaginal bleeding, no matter how slight
Fetus 7 lbs. 2. Swelling of the face & fingers
Placenta 1 lb. 3. Severe, continuous headache
Amniotic fluid 1.5 lbs. 4. Flashes of light before the eyes
Uterine weight 2 lbs. 5. Pain in the abdomen
Blood volume 1 lb. 6. Persistent vomiting
Weight of breast 1.5 – 3 lbs. 7. Chills & fever
Additional fluid 2 lbs. 8. Sudden escape of fluid from the vagina
Fat & fluid accumulation 4 – 6 lbs.
20-25 lbs.
PRENATAL SELF CARE NEEDS
• BATHING- daily tub or showers due to sweating that tends
to increase in pregnancy
• BREAST CARE - wearing firm supportive bra with wide straps
to spread weight across the shoulders. Wash breast with
clear tap water (no soap) to remove or minimize infections.
• DENTAL CARE - good tooth brushing habits
• PERINEAL CARE - douching is contraindicated due to force
of the irrigation that can cause it to enter the cervix and lead
to infection; also alters pH of vagina leading to increased risk
of bacterial growth
• EMOTIONAL – “Couvade Syndrome”
• DRESSING - avoid garters, and knee high stocking that can
impede lower extremity circulation
• SEXUAL ACTIVITY - no sexual restrictions
• EXERCISE - important to prevent circulatory stasis in lower
extremities 6. Past medical history
• SLEEP 7. Gynecological history
• EMPLOYMENT 8. Ob history
• TRAVEL 9. Birthing Plan
TETANUS TOXOID IMMUNIZATION SCHEDULE FOR WOMEN FREQUENCY OF PRENATAL VISIT
• Foods to Avoid 1st and 2nd Trimester • Once a month up to 32
o Food with caffeine weeks
o Artificial sweeteners 32-36 Weeks • Twice a month (every 2
Weight loss diet weeks)
36-40 Weeks • Four times a month
COMPONENTS OF PRENATAL VISIT (every week)
1. Health history ➢ 80% of pregnant women in the Philippines should have at
2. Chief concern least 5 prenatal visits. (DOH Goal)
3. Any exposure to disease
4. Ingestion of drugs
5. Family & social profile
EMOTIONAL AND PSYCHOLOGICAL ADAPTATIONS TO PREGNANCY 3. Random Blood Sugar (RBS)
STRESSORS: 4. Blood Typing
1. Circumstances to pregnancy- couvade syndrome 5. Venereal Disease Research Laboratory (VDRL)
2. Meaning of Pregnancy to the couple 6. Hepatitis B Screening
3. Responsibilities associated with parenthood 7. Ultrasonography
4. Resources available to family
PREPARATION FOR LABOR AND DELIVERY
PSYCHOLOGICAL TASK OF PREGNANCY 1. Childbirth Education
• FIRST TRIMESTER 2. Preconception Classes
o TASK – ACCEPTING THE PREGNANCY 3. Expectant Parenting Classes
Woman and partner both spent time recovering from shock of 4. Childbirth Plan – hospital, type of delivery, etc.
learning they are pregnant and concentrate on what it feels like to 5. Childbirth Classes
be pregnant. A common reaction is ambivalence, or feeling both 6. Responsible Parenthood- contraceptives like LAM (4-6months),
pleased and not pleased at the pregnancy use of condom, knowledge on fertility (cycle, spinnbarkeit/
• SECOND TRIMESTER: mucus), etc.
o TASK – ACCEPTING THE BABY
Woman and partner move through emotions such as
narcissism and introversions as they concentrate on what it will
feel like to be a parent. Role playing and increased dreaming
are common
• THIRD TRIMESTER:
o TASK – PREPARING FOR THE BABY AND END OF
PREGNANCY
Woman and partner grow impatient with pregnancy as they ready
themselves for birth EMOTIONAL RESPONSES:
1. Self-concept related to body image
2. Mood swings related to biophysical & social changes
3. Ambivalence related to fear & anxiety
4. Sexual concerns related to biophysical changes
LABORATORY AND DIAGNOSTIC EXAMINATIONS (ACCORDING TO DOH
STANDARDS))
1. CBC
2. Urinalysis – hPL (insulin)
You might also like
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Maternal Quiz NotesDocument79 pagesMaternal Quiz NotesPasay Trisha Faye Y.No ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Pharma - Drugs Affecting Git MotilityDocument6 pagesPharma - Drugs Affecting Git MotilityBobet ReñaNo ratings yet
- Obstetric Case Study CesarianDocument16 pagesObstetric Case Study CesarianRazan NasereddineNo ratings yet
- Comprehensive Table of Drugs: Cholinergic Agonists (Parasympathomimetics)Document31 pagesComprehensive Table of Drugs: Cholinergic Agonists (Parasympathomimetics)filchibuffNo ratings yet
- A Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutFrom EverandA Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutRating: 5 out of 5 stars5/5 (1)
- Pregnancy Hypertension GuideDocument5 pagesPregnancy Hypertension GuideIrene FranzNo ratings yet
- HPN Drug StudyDocument4 pagesHPN Drug StudyJohn Haider Colorado GamolNo ratings yet
- Physical Evaluation Checklist For NurseDocument3 pagesPhysical Evaluation Checklist For NurseGiridhar RagavasimhanNo ratings yet
- Case Study, Chapter 42, Management of Patients With Musculoskeletal TraumaDocument2 pagesCase Study, Chapter 42, Management of Patients With Musculoskeletal TraumaAhmad BaolayyanNo ratings yet
- Anatomy and Physiology of NeonatesDocument17 pagesAnatomy and Physiology of NeonatesYu ShiNo ratings yet
- Nursing Management of Common IV DrugsDocument6 pagesNursing Management of Common IV DrugsStephanie Dellera AgdanNo ratings yet
- Transcultural Nursing Quiz 2Document2 pagesTranscultural Nursing Quiz 2Jenny AjocNo ratings yet
- EAMC DFCM OPD Charting Guidelines As of March 2022Document19 pagesEAMC DFCM OPD Charting Guidelines As of March 2022Adrian MaterumNo ratings yet
- UrethritisDocument11 pagesUrethritismarej143No ratings yet
- Concept Map Worksheet Fatime Sanogo Jasgou1752Document1 pageConcept Map Worksheet Fatime Sanogo Jasgou1752Jasmyn RoseNo ratings yet
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocument4 pagesTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestNo ratings yet
- Pulmonary Hypertension: Causes, Symptoms, Diagnosis and TreatmentDocument10 pagesPulmonary Hypertension: Causes, Symptoms, Diagnosis and TreatmentCkaye GansubinNo ratings yet
- Renal Concept MapDocument8 pagesRenal Concept MapXtine CajiNo ratings yet
- Drug StudyDocument4 pagesDrug StudyDean Angelo BarrientosNo ratings yet
- CVD Bleed Case StudyDocument25 pagesCVD Bleed Case StudyMargaret Jenaw JenawNo ratings yet
- Optimizing Perioperative CareDocument8 pagesOptimizing Perioperative CareJan Crizza Dale R. FrancoNo ratings yet
- Pharmacologic management of bleomycinDocument1 pagePharmacologic management of bleomycinKim ApuradoNo ratings yet
- GERD Pathophysiology Cleveland ClinicDocument17 pagesGERD Pathophysiology Cleveland ClinicMavisNo ratings yet
- Postpartum HemorrhageDocument5 pagesPostpartum Hemorrhageapi-354418387No ratings yet
- Case Presentations and Patient Check-insDocument3 pagesCase Presentations and Patient Check-insJam Knows RightNo ratings yet
- Drug Study CovidDocument5 pagesDrug Study CovidR Hornilla Arcega0% (1)
- Pamantasan NG Cabuyao College of Health Allied Sciences College of NursingDocument43 pagesPamantasan NG Cabuyao College of Health Allied Sciences College of NursingSofea MustaffaNo ratings yet
- Newborn Screening Policy Catarman Doctors Hospital, Inc.: University of Eastern PhilippinesDocument7 pagesNewborn Screening Policy Catarman Doctors Hospital, Inc.: University of Eastern PhilippinesGenn Medrano GirayNo ratings yet
- Improving a Family's Sleeping Habits Through EducationDocument10 pagesImproving a Family's Sleeping Habits Through EducationtaniaNo ratings yet
- Pathophysiology MaiaDocument2 pagesPathophysiology Maiajia88No ratings yet
- Drug StudyDocument8 pagesDrug StudyJay-ar Batara SorianoNo ratings yet
- A Review On Otitis Media (Karnapaka) : Ayurvedic Aspects and TreatmentDocument4 pagesA Review On Otitis Media (Karnapaka) : Ayurvedic Aspects and TreatmentEditor_IAIMNo ratings yet
- Drug StudyDocument7 pagesDrug StudyCharmz_asherahNo ratings yet
- Hydrocephalus in Adult PresentDocument25 pagesHydrocephalus in Adult PresentmarthintoriNo ratings yet
- Case Presentation of Acute PyelonephritisDocument1 pageCase Presentation of Acute PyelonephritisANALYN ANUBNo ratings yet
- Bronchiolitis Clinical Practice GuidelineDocument21 pagesBronchiolitis Clinical Practice GuidelineJuwita PratiwiNo ratings yet
- Abnormal OBDocument34 pagesAbnormal OBLawrence NemirNo ratings yet
- Common Medical AbbreviationsDocument3 pagesCommon Medical AbbreviationsBráian Tzéims άλμπαNo ratings yet
- Drug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityDocument2 pagesDrug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityJoshua DavantesNo ratings yet
- Imci Rec Form FinalDocument1 pageImci Rec Form FinalHecia Gaga-aNo ratings yet
- Pediatric Respiratory Disorders General InterventionsDocument2 pagesPediatric Respiratory Disorders General Interventionscayla mae carlosNo ratings yet
- Drugs Affecting Reproductive System: Presented By: BSN 2A Group 1Document34 pagesDrugs Affecting Reproductive System: Presented By: BSN 2A Group 1David BernalNo ratings yet
- RP-Case History of A Child With Sickle Cell Anemia in IndiaDocument5 pagesRP-Case History of A Child With Sickle Cell Anemia in IndiaMarie Kelsey Acena MacaraigNo ratings yet
- Rifaximin Nihms443516Document10 pagesRifaximin Nihms443516MIHAELANo ratings yet
- Drugs Study Ward 9 (Corvera)Document5 pagesDrugs Study Ward 9 (Corvera)Herbert Almendras HuyoNo ratings yet
- Nursing Assessment, Planning, Implementation and EvaluationDocument2 pagesNursing Assessment, Planning, Implementation and EvaluationDiana MuañaNo ratings yet
- Medications and Nursing Responsibilities for Bone HealthDocument6 pagesMedications and Nursing Responsibilities for Bone HealthDarla JoyceNo ratings yet
- 2nd Activity - Patient With Cough and FeverDocument40 pages2nd Activity - Patient With Cough and FeverJethro Floyd QuintoNo ratings yet
- Nursing Student Masters Blood Transfusion SkillsDocument2 pagesNursing Student Masters Blood Transfusion Skillscaitie miracleNo ratings yet
- RRS at RRLDocument19 pagesRRS at RRLNicole MangosanNo ratings yet
- Medical Abbreviation TermsDocument7 pagesMedical Abbreviation TermsJmarie Brillantes PopiocoNo ratings yet
- Discharge Planning:: Return To The Emergency Department IfDocument2 pagesDischarge Planning:: Return To The Emergency Department IfJordz PlaciNo ratings yet
- Drug Study: Phinma University of PangasinanDocument4 pagesDrug Study: Phinma University of PangasinanBrythym De GuzmanNo ratings yet
- Concept Map 1Document2 pagesConcept Map 1yfortilus100% (1)
- HANDOUT Chapter 11 Promoting Fetal and Maternal HealthDocument7 pagesHANDOUT Chapter 11 Promoting Fetal and Maternal HealthClouiseNo ratings yet
- Febrile SeizureDocument6 pagesFebrile SeizurepipimseptianaNo ratings yet
- Reflection/ Analysis PaperDocument2 pagesReflection/ Analysis PaperClaire Julianne CapatiNo ratings yet
- Capati HospitalformsDocument3 pagesCapati HospitalformsClaire Julianne CapatiNo ratings yet
- Asynchronous Activity: What Does Good Posture Look Like?Document10 pagesAsynchronous Activity: What Does Good Posture Look Like?Claire Julianne CapatiNo ratings yet
- Assignment No. 2Document2 pagesAssignment No. 2Claire Julianne CapatiNo ratings yet
- Type of Gene TherapyDocument3 pagesType of Gene TherapyClaire Julianne CapatiNo ratings yet
- Health Care EthicsDocument5 pagesHealth Care EthicsClaire Julianne CapatiNo ratings yet
- FCL Concept-PaperDocument5 pagesFCL Concept-PaperClaire Julianne CapatiNo ratings yet
- Final Seatwork RPHDocument2 pagesFinal Seatwork RPHClaire Julianne CapatiNo ratings yet
- CV and Educational Background of Tomas M. MadayagDocument12 pagesCV and Educational Background of Tomas M. MadayagJovel TomNo ratings yet
- HTM 01 01 PartADocument59 pagesHTM 01 01 PartAwaseem kausarNo ratings yet
- Case HirschsprungDocument29 pagesCase HirschsprungPriscila StevanniNo ratings yet
- Myanmar Health Assistant Association Vacancy Announcement (VA - 052/2023 MHAA-HR)Document3 pagesMyanmar Health Assistant Association Vacancy Announcement (VA - 052/2023 MHAA-HR)Zawhtet HtetNo ratings yet
- Bender Gestalt TestDocument3 pagesBender Gestalt TestAleena ThakurtaNo ratings yet
- A Beautiful Mind QuizDocument3 pagesA Beautiful Mind QuizTruanoPro0% (1)
- By: Dr. Ayman Bukhari House Officer Obstetrics & GynaecologyDocument54 pagesBy: Dr. Ayman Bukhari House Officer Obstetrics & GynaecologyBharat ThapaNo ratings yet
- Sofía Amador. Comprension de Textos en Ingles PDFDocument7 pagesSofía Amador. Comprension de Textos en Ingles PDFDéimar AmadorNo ratings yet
- Fitness Goals and Target Heart RateDocument8 pagesFitness Goals and Target Heart RateRuben Rosendal De AsisNo ratings yet
- Stroke Prediction System Using ANN (Artificial Neural Network)Document3 pagesStroke Prediction System Using ANN (Artificial Neural Network)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Martindale drug reference 38th edition downloadDocument3 pagesMartindale drug reference 38th edition downloadChristian SosaNo ratings yet
- Tellus 68 MsdsDocument7 pagesTellus 68 MsdsMalou Castillo UmaliNo ratings yet
- Newest - Hled325 Stress Management Lesson Plan StartDocument6 pagesNewest - Hled325 Stress Management Lesson Plan Startapi-199880580No ratings yet
- DepEd Puerto Princesa City School Bridging Gaps ReportDocument2 pagesDepEd Puerto Princesa City School Bridging Gaps ReportJazzele LongnoNo ratings yet
- Precision Medicine in Cancers and Non-Communicable DiseasesDocument343 pagesPrecision Medicine in Cancers and Non-Communicable DiseasesBenaia João NHAMITAMBONo ratings yet
- Scalp Acupuncture BasicsDocument27 pagesScalp Acupuncture BasicsGanga SinghNo ratings yet
- Eat To 80 Percent Full Infographic TFDocument1 pageEat To 80 Percent Full Infographic TFNikola KaraklajicNo ratings yet
- K - Birth Plan ChecklistDocument2 pagesK - Birth Plan ChecklistPatrick LinNo ratings yet
- THE ETHICS OF PUBLIC HEALTH SURVEILLANCE MCQsDocument2 pagesTHE ETHICS OF PUBLIC HEALTH SURVEILLANCE MCQsChaman Lal Karotia100% (1)
- Golden RiceDocument6 pagesGolden RiceJoshua AgravioNo ratings yet
- CPE5601 Diagnosis and Treatment of Feeding and Eating DisordersDocument16 pagesCPE5601 Diagnosis and Treatment of Feeding and Eating DisordersSiti MuslihaNo ratings yet
- Pelaporan IKP Puskesmas - 200921 (1), Edit Taufiq 20 Sept 2021Document54 pagesPelaporan IKP Puskesmas - 200921 (1), Edit Taufiq 20 Sept 2021diniayu100% (1)
- Baking Soda Cures Cancer, Fungus and InflammationDocument6 pagesBaking Soda Cures Cancer, Fungus and Inflammationsheriff77080% (5)
- Hosneara Begum - Aastha ConcentDocument2 pagesHosneara Begum - Aastha ConcentAbul HasnatNo ratings yet
- Prognostic Value of Admission Blood Glucose in Diabetic and Non-Diabetic Patients With Intracerebral HemorrhageDocument7 pagesPrognostic Value of Admission Blood Glucose in Diabetic and Non-Diabetic Patients With Intracerebral HemorrhageNur Irma SafitriNo ratings yet
- Dahlar Release Bag 500 - MSDSDocument7 pagesDahlar Release Bag 500 - MSDSApol Aguisanda JrNo ratings yet
- McWilliams (2009)Document4 pagesMcWilliams (2009)Stacy Lanier100% (1)
- ADHD AdultDocument3 pagesADHD AdultCristinaNo ratings yet
- Hormonal TherapiesDocument39 pagesHormonal TherapiesJalal EltabibNo ratings yet
- Increases in COVID 19 Are Unrelated To Levels of Vaccination Across 68 Countries and 2947 Counties in The United StatesDocument4 pagesIncreases in COVID 19 Are Unrelated To Levels of Vaccination Across 68 Countries and 2947 Counties in The United StatesKyle Becker95% (19)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)