Professional Documents
Culture Documents
Patient Name: Lorna Dimagiba Age: 84 Years Old Gender: Female C.S: Widow BED#: 1 Date / Shift/ Time Focus Notes (Data, Action, Response)
Uploaded by
Fau Fau DheoboOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Patient Name: Lorna Dimagiba Age: 84 Years Old Gender: Female C.S: Widow BED#: 1 Date / Shift/ Time Focus Notes (Data, Action, Response)
Uploaded by
Fau Fau DheoboCopyright:
Available Formats
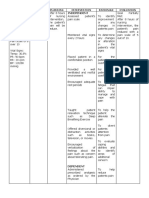
PATIENT NAME: LORNA DIMAGIBA
AGE: 84 Years old
GENDER: Female
C.S: Widow
BED#: 1
DATE / SHIFT/ TIME FOCUS NOTES (DATA, ACTION, RESPONSE)
12/01/21 Received patient, awake, sitting on a
3:00 pm chair with an ongoing IV Fluid of D5
0.45% NaCl with 20 mEq KCL per liter at
60 mL’s per hour infusing well at her right
arm.
Vital signs recorded as follows:
Temp: 36.6 c
BP: 170/90 mmHg
RR: 14 cpm
PR: 76 bpm
*Quite confused
3:15 pm Acute Pain - Assessed the client’s description of pain
- Encouraged the patient to increased oral
fluid intake
3:45 pm - Avoided urinary irritants such as coffee,
tea, colas, and alcohol.
-Applied a heating pad to the supra pubic
area or lower back.
- Encouraged relaxation techniques,
4:15 pm
massage, guided imagery, or distraction
to decrease pain and provide comfort.
- Administered appropriate medication as
5:00 pm ordered such as Celecoxib 200 mg po
once a day, Ciprofloxacin 250 mg po
every 12 hours,
Acetaminophen 325 mg po q 6 hrs prn
pain or fever.
6:00 pm Fluid Volume - Assessed patient’s general condition
- Monitored VS and charted
- Encouraged Fluid intake
- Monitored and regulated IVF at desired
rate
6:30 pm - Promoted proper ventilation and
therapeutic environment
- Emphasized the relevance of
maintaining proper nutrition and
hydration..
- Offered assistance with eating and
drinking if necessary.
7:00 pm - Placed the beverage within view and
close reach at the bedside table.
- Administered appropriate medication as
ordered.
8:00 pm Acute Confusion - Oriented patient to surroundings, staff,
and necessary activities as needed.
- Allowed sufficient time for patient to
respond, to communicate, to make
decisions.
- Provided for safety needs
8:30 pm - Kept normal fluid and electrolyte
balance; establish/maintain normal
nutrition, body temperature.
- Identified self by name at each contact;
call the patient by his or her preferred
name.
9:00 pm - Provided continuity of care when
possible (e.g., provide the same
caregivers, avoid room changes).
- Assisted the family and significant
others in developing coping strategies.
- Monitored laboratory values such as
9:30 pm CBC and oxygen saturation
- Taught family to recognize signs of early
confusion and seek medical help.
10:00 pm R- Patient is awake, restfully lying on bed
and able to maintain fluid volume at well-
designed level with a good skin turgor
and a pain scale of 2/10.
PATIENT NAME: MARTIN TOTO
AGE: 76 years old
GENDER: Male
C.S: Married
BED#: 2
DATE / SHIFT/ NOTES (DATA, ACTION,
FOCUS
TIME RESPONSE)
12/01/21 Received patient lying on bed,
3:00 pm weak and coughing.
Vital signs as follows:
Temp:38
BP: 120/80 mmHg
RR: 25
PR: 98
- skin warm to touch
- restlessness
Ineffective Breathing - Assessed and record respiratory
3:30 pm Pattern rate and depth.
- Observed breathing patterns.
- Placed patient with proper body
alignment for maximum breathing
pattern.
4:30 pm - Provided respiratory medications
and oxygen, as per doctor’s order.
- Stayed with the patient during
acute episodes of respiratory
distress.
5:30 pm - Encouraged small frequent
meals.
- Educated patient or significant
other on proper breathing,
coughing, and splinting methods.
6:00 pm Hyperthermia - Monitored vital signs
- Tepid Sponge Bath (TSB) done
- Administered 500mg IV
Paracetamol as per doctor’s order
6:30 pm -Encouraged adequate oral fluid
intake
-Encouraged adequate rest
7:00 pm - Repositioned patient every 2
hours.
7:30 pm Fatigue - Encouraged patient to rest
- Taught patient energy
conservation methods.
- Provided comfort such as
8:00 pm massage, and cool showers.
- Offered diversional activities that
are soothing.
9:00 pm - Promoted relaxation before
sleep and providing for several
hours of uninterrupted sleep can
contribute to energy restoration.
10:00 pm R - Patient is awake, comfortably
lying on his bed, vital signs
returned to normal and maintains
an effective breathing pattern, as
evidenced by relaxed breathing at
normal rate and depth and
absence of dyspnea.
You might also like
- FDAR and 12 14Document4 pagesFDAR and 12 14Jay VillasotoNo ratings yet
- Nursing Management Concept MapDocument1 pageNursing Management Concept MapXy-Za Roy Marie100% (1)
- FDAR ProperDocument5 pagesFDAR Propermikrobyo_ng_wmsu100% (3)
- GBS Source 1Document4 pagesGBS Source 1PJHG50% (2)
- Nurses Notes Case 8Document4 pagesNurses Notes Case 8JERRYMAE RIVERANo ratings yet
- NCP LeptospirosisDocument2 pagesNCP LeptospirosisLouise Anne Asuncion OclimaNo ratings yet
- FDAR Appendicitis Bartolata Bermundo G3 3A 08 24 2021Document3 pagesFDAR Appendicitis Bartolata Bermundo G3 3A 08 24 2021Keisha Bartolata100% (2)
- Report PDFDocument2 pagesReport PDFAnonymous 6x3CyeNo ratings yet
- Patient Name: Lorna Dimagiba Age: 84 Years Old Gender: Female C.S: Widow BED#: #1Document3 pagesPatient Name: Lorna Dimagiba Age: 84 Years Old Gender: Female C.S: Widow BED#: #1Girlie MebañaNo ratings yet
- Patient'S Name: Age: Gender: C.S: BED#Document2 pagesPatient'S Name: Age: Gender: C.S: BED#Girlie MebañaNo ratings yet
- 0orpilla Jomark C. Gerd - FdarDocument2 pages0orpilla Jomark C. Gerd - FdarAphrill Pearl PacisNo ratings yet
- Litiza RenalaDocument8 pagesLitiza RenalaCaracas GeaninaNo ratings yet
- Patient Name: Maureen Wroble Age: 28 Years Old Gender: F C.S: Single BED#: #02 Date / Shift/ Time Focus Notes (Data, Action, Response)Document3 pagesPatient Name: Maureen Wroble Age: 28 Years Old Gender: F C.S: Single BED#: #02 Date / Shift/ Time Focus Notes (Data, Action, Response)mark OrpillaNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationVince Adrian FiguracionNo ratings yet
- Fdar LP 6Document4 pagesFdar LP 6Krizzia Mae ColladoNo ratings yet
- FDARDocument5 pagesFDARJulia Rae Delos SantosNo ratings yet
- Case Study (NUR)Document1 pageCase Study (NUR)Yasmien MarieNo ratings yet
- 12/07/20 3PM-11PM: Fdar ChartingDocument5 pages12/07/20 3PM-11PM: Fdar ChartingElle ctricaNo ratings yet
- Tayuan Fdar Week5 PDFDocument2 pagesTayuan Fdar Week5 PDFJozl Fahany TayuanNo ratings yet
- Nurses Notes Date Focus Data Action Response: SubjectiveDocument2 pagesNurses Notes Date Focus Data Action Response: SubjectiveGILIANNE MARIE JIMENEANo ratings yet
- Model Caz DamlaDocument9 pagesModel Caz DamlaDamla KaykusuzNo ratings yet
- Case Study On CAPDocument4 pagesCase Study On CAPjcarysuitosNo ratings yet
- Nursing Care Plan Assessment Diagnosis Planning Implementation Rationale Evaluation IndependentDocument4 pagesNursing Care Plan Assessment Diagnosis Planning Implementation Rationale Evaluation IndependentLau100% (1)
- Diabetic KetoacidosisDocument5 pagesDiabetic KetoacidosisJamie IllmaticNo ratings yet
- JaboneteDocument7 pagesJabonetejohn loyolaNo ratings yet
- Assessment Diagnosis Scientific Background Planning Implementation Rationale EvaluationDocument2 pagesAssessment Diagnosis Scientific Background Planning Implementation Rationale EvaluationREOLALAS, Mariane JoyNo ratings yet
- Hypovolemic Shock Sample NCPDocument14 pagesHypovolemic Shock Sample NCPRENEROSE TORRES100% (1)
- Cholelithiasis (Case Presentation)Document19 pagesCholelithiasis (Case Presentation)Ian CiarNo ratings yet
- FDARDocument3 pagesFDARGirlie MebañaNo ratings yet
- Post-Natal Mother: Postnatal Care Plan FORDocument14 pagesPost-Natal Mother: Postnatal Care Plan FORpriyanka100% (10)
- Villanueva Bsn-1a - NcplecDocument6 pagesVillanueva Bsn-1a - NcplecKhyra Ysabelle VillanuevaNo ratings yet
- Benjamin Button - 56Document97 pagesBenjamin Button - 56Aubrey Unique EvangelistaNo ratings yet
- Nurses Notes Soapie Day 2Document3 pagesNurses Notes Soapie Day 2Sunny Al asadiNo ratings yet
- Date/Shift Focus DataDocument2 pagesDate/Shift Focus Datakuro hanabusaNo ratings yet
- Nurses Notes Case 8Document4 pagesNurses Notes Case 8JERRYMAE RIVERANo ratings yet
- Draft HTN 1 PDFDocument8 pagesDraft HTN 1 PDFAko ay Wala poNo ratings yet
- Enrichment Class On DocumentationDocument20 pagesEnrichment Class On Documentationronnelgalang.rgNo ratings yet
- NCP2 - Active PhaseDocument14 pagesNCP2 - Active PhasepriyankaNo ratings yet
- FDARDocument2 pagesFDARMikaela Mae GonzagaNo ratings yet
- Group Fdar Hemophilia ADocument2 pagesGroup Fdar Hemophilia AMika SaldañaNo ratings yet
- Ischemic StrokeDocument25 pagesIschemic Strokebcdpqyck8xNo ratings yet
- NCP For HemorrhoidsDocument3 pagesNCP For HemorrhoidsTADURAN RENE MAE ANGELLI F.No ratings yet
- Fdar Lp6 MontemayorDocument5 pagesFdar Lp6 MontemayorEden Marie MangaserNo ratings yet
- Dungog, Daniel Mark A.Document1 pageDungog, Daniel Mark A.tophergonzales45No ratings yet
- Sickle Cell - RahafDocument39 pagesSickle Cell - RahafgalalNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale Evaluation Subjective: Short Term: IndependentDocument3 pagesAssessment Diagnosis Planning Implementation Rationale Evaluation Subjective: Short Term: IndependentGuillao LensNo ratings yet
- Outline of Nursing Care Plan: 1. Hyperthermia Hyperthermia Associated With High FeverDocument2 pagesOutline of Nursing Care Plan: 1. Hyperthermia Hyperthermia Associated With High FeverFarah FildzahNo ratings yet
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation Short Term Goal: IndependentDocument4 pagesNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation Short Term Goal: IndependentasdasdasdNo ratings yet
- FHP - NCP - Kidney FailureDocument9 pagesFHP - NCP - Kidney FailureFrancis AdrianNo ratings yet
- Chapter IDocument8 pagesChapter IRahmakumalasariNo ratings yet
- TTP Care Plan 1 JevansDocument8 pagesTTP Care Plan 1 Jevansapi-439893609No ratings yet
- Capacio Case#5&6Document7 pagesCapacio Case#5&6Lorenz CapacioNo ratings yet
- Focus Charting: Date Time Focus Nurse'S Remarks D She Is Is Gravid 2, paraDocument6 pagesFocus Charting: Date Time Focus Nurse'S Remarks D She Is Is Gravid 2, paraVincent SalvadorNo ratings yet
- Case Study Assessing Thorax and LungsDocument4 pagesCase Study Assessing Thorax and LungsMaurice CudalNo ratings yet
- Assess The Plan To Provide Advice The Advice TheDocument3 pagesAssess The Plan To Provide Advice The Advice TheDarwin QuirimitNo ratings yet
- Placenta Previa: G4 T2 P0 A1 L2Document42 pagesPlacenta Previa: G4 T2 P0 A1 L2SteffiNo ratings yet
- ABELLAR - TPR, Graphing, ChartingDocument4 pagesABELLAR - TPR, Graphing, ChartingJeah Bearl AbellarNo ratings yet
- NCP FormatDocument3 pagesNCP FormatSuzete PagaduanNo ratings yet
- Activity 1 - Case Agent RookieDocument2 pagesActivity 1 - Case Agent RookieChristian ConcepcionNo ratings yet
- Apis Mellifica; or, The Poison of the Honey-Bee, Considered as a Therapeutic AgentFrom EverandApis Mellifica; or, The Poison of the Honey-Bee, Considered as a Therapeutic AgentNo ratings yet
- Soak It In: Hydrotherapy Treatments In 20 Minutes or Less for Health and BeautyFrom EverandSoak It In: Hydrotherapy Treatments In 20 Minutes or Less for Health and BeautyNo ratings yet
- Reyes, Crisel P.Document24 pagesReyes, Crisel P.Fau Fau DheoboNo ratings yet
- Finals 3Document5 pagesFinals 3Fau Fau DheoboNo ratings yet
- NX Intervention MIDocument3 pagesNX Intervention MIFau Fau DheoboNo ratings yet
- Classification of Explosives A. According To VelocityDocument3 pagesClassification of Explosives A. According To VelocityFau Fau DheoboNo ratings yet
- The Three Core Functions and Ten Essential Public Health ServicesDocument5 pagesThe Three Core Functions and Ten Essential Public Health ServicesFau Fau DheoboNo ratings yet
- Nursing Procedure Checklist: Skill Is Not Performed Correctly and Not Done If The Student Failed To Perform The SkillDocument2 pagesNursing Procedure Checklist: Skill Is Not Performed Correctly and Not Done If The Student Failed To Perform The SkillFau Fau DheoboNo ratings yet
- Skills Laboratory Cyclical RotationDocument17 pagesSkills Laboratory Cyclical RotationFau Fau DheoboNo ratings yet
- Family Profile: HusbandDocument6 pagesFamily Profile: HusbandFau Fau DheoboNo ratings yet
- MCN Nursing 1Document107 pagesMCN Nursing 1Fau Fau DheoboNo ratings yet
- MAMDocument2 pagesMAMFau Fau DheoboNo ratings yet
- Case Study PatientDocument23 pagesCase Study PatientFau Fau DheoboNo ratings yet
- Name of Patient: Age: 35 Gender: Male Room Number: Chief Complain: Physician: Admitting Diagnosis: Current Assessment: VSDocument1 pageName of Patient: Age: 35 Gender: Male Room Number: Chief Complain: Physician: Admitting Diagnosis: Current Assessment: VSFau Fau DheoboNo ratings yet
- Assessment Diagnosis Planning Interventions Rationale Evaluation IndependentDocument2 pagesAssessment Diagnosis Planning Interventions Rationale Evaluation IndependentFau Fau DheoboNo ratings yet
- Discharge Care Plan: MedicineDocument2 pagesDischarge Care Plan: MedicineFau Fau DheoboNo ratings yet
- Family Case LoadDocument17 pagesFamily Case LoadFau Fau Dheobo100% (1)
- Subjective: Independent: Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesSubjective: Independent: Assessment Diagnosis Planning Intervention Rationale EvaluationFau Fau DheoboNo ratings yet
- Acute Otitis Media: Dr. Ajay Manickam Junior Resident RG Kar Medical College HospitalDocument20 pagesAcute Otitis Media: Dr. Ajay Manickam Junior Resident RG Kar Medical College HospitalchawkatNo ratings yet
- 10 - Neonaticide, Infanticide and Child HomicideDocument45 pages10 - Neonaticide, Infanticide and Child HomicideWala AbdeljawadNo ratings yet
- The Importance of Proteinuria in Preeclampsia and Its Predictive Role in Maternal and Neonatal OutcomesDocument9 pagesThe Importance of Proteinuria in Preeclampsia and Its Predictive Role in Maternal and Neonatal OutcomesimuhammadfahmiNo ratings yet
- Giotto Image3D BrochureDocument16 pagesGiotto Image3D BrochureGriselda Maria Pinto SanchezNo ratings yet
- Key To Eye Diagnosis by Tashfeen NasiraDocument8 pagesKey To Eye Diagnosis by Tashfeen Nasiralakshay sharmaNo ratings yet
- Rent AgreementDocument4 pagesRent Agreementkhushbu chitreNo ratings yet
- Additional RRLDocument3 pagesAdditional RRLManuel Jaro ValdezNo ratings yet
- Medical Questionnaire: To Be Filled by Attending PhysicianDocument3 pagesMedical Questionnaire: To Be Filled by Attending PhysiciansusomNo ratings yet
- Charting SystemsDocument4 pagesCharting SystemsLydia D. GalinganNo ratings yet
- Grading Scale 2017 PDFDocument2 pagesGrading Scale 2017 PDFAlibek ZhumanazarovNo ratings yet
- Commonly Billed Codes: Spinal Cord StimulationDocument21 pagesCommonly Billed Codes: Spinal Cord StimulationKrishna KumarNo ratings yet
- 35 - Eposter - Subhenjit Ray.Document1 page35 - Eposter - Subhenjit Ray.Subhenjit RoyNo ratings yet
- JM Shah Benefits of BiowellDocument2 pagesJM Shah Benefits of BiowellManagerNo ratings yet
- 2018 Urinary Tract Infections in ChildrenDocument12 pages2018 Urinary Tract Infections in ChildrenYudit Arenita100% (1)
- Surgical Management of Abomasal DiseaseDocument16 pagesSurgical Management of Abomasal DiseaseAbdul MajeedNo ratings yet
- Urdaneta City University Graduate School UrdanetaDocument13 pagesUrdaneta City University Graduate School UrdanetaMa Theresa PunoNo ratings yet
- Fetal Colonic GradeDocument7 pagesFetal Colonic Gradedgina8800No ratings yet
- Rishum 1 262421216 2Document1 pageRishum 1 262421216 2HellcroZNo ratings yet
- Assessment Diagnosis Rationale Plan Interventions Rationale EvaluationDocument14 pagesAssessment Diagnosis Rationale Plan Interventions Rationale EvaluationDuran JustineNo ratings yet
- Bowel IncontinenceDocument4 pagesBowel IncontinenceprashanthNo ratings yet
- Hypertency Emergency Acute PDFDocument12 pagesHypertency Emergency Acute PDFmasdika09No ratings yet
- Speech Language Pathology (SLP)Document6 pagesSpeech Language Pathology (SLP)Shariq MNo ratings yet
- RBC Disorder BcqsDocument68 pagesRBC Disorder BcqsMukhtiar AhmedNo ratings yet
- Medrobotics Receives FDA Clearance For ColorectalDocument2 pagesMedrobotics Receives FDA Clearance For ColorectalmedtechyNo ratings yet
- M SDocument162 pagesM SAnn Claudette SyNo ratings yet
- Conducting A Nurse Consultation: ClinicalDocument6 pagesConducting A Nurse Consultation: ClinicalAlif Akbar HasyimiNo ratings yet
- Maternal and Early-Life Nutrition and HealthDocument4 pagesMaternal and Early-Life Nutrition and HealthTiffani_Vanessa01No ratings yet
- Departm Ent of Education: R e P U B Lic of Tlje JH JilippineffDocument7 pagesDepartm Ent of Education: R e P U B Lic of Tlje JH JilippineffJoyce CarilloNo ratings yet