Professional Documents
Culture Documents
Article Wjpps 1427890881
Uploaded by
Pramod bhalseOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Article Wjpps 1427890881
Uploaded by
Pramod bhalseCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/323869555
TREATMENT REGIMEN FOR CELPHOS POISIONING
Article in WORLD JOURNAL OF PHARMACY AND PHARMACEUTICAL SCIENCES · March 2018
CITATIONS READS
0 4,006
3 authors, including:
Rafiqa Eachkoti
Govt Medical College Srinagar (GMC)
20 PUBLICATIONS 109 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
breast cancer genetics View project
All content following this page was uploaded by Rafiqa Eachkoti on 20 March 2018.
The user has requested enhancement of the downloaded file.
WORLD JOURNAL OF PHARMACY AND PHARMACEUTICAL SCIENCES
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
SJIF Impact Factor 2.786
Volume 4, Issue 04, 953-965. Research Article ISSN 2278 – 4357
TREATMENT REGIMEN FOR CELPHOS POISIONING
Hakim Ali Qanoon1*, Rafiqa Eachkoti2, Promila Phaughat3
1
Department of Medicine and Critical Care, Maharishi Valmiki Hospital, Govt. of NCT of
Delhi, India.
2
Department of Biochemistry, Govt. Medical College and associated hospitals, Karanagar,
Srinagar, Kashmir, J&K India.
3
Department of Anesthesia and Critical Care, Maharishi Valmiki Hospital, Govt. of NCT of
Delhi, India.
Article Received on ABSTRACT
29 Jan 2015,
Celphos poisoning is a major cause of mortality largely due to non-
Revised on 22 Feb 2015,
Accepted on 18 March 2015 availability of its antidote, due to delay in appropriate management and
skepticism amongst physicians regarding the outcome. Although
different trials has been tried to counter its irreversible toxic effects but
*Correspondence for
Author hardly with any concrete success. Here we report novel intervention,
Dr. Hakim Ali Qanoon the protocol of which we have formulated and standardized for last
Department of Medicine and 1.5years, for Celphos poisioning which aims to diminish the
Critical Care, Maharishi
production and absorption of phosphine, enhance its excretion and
Valmiki Hospital, Govt. of
prevent any organ toxicity with appropriate supportive therapy. The
NCT of Delhi, India.
management plan involves gastric lavage with an aliquot of coconut oil
mixed with NaHCO3 followed by KMNO4 in Normal saline as an essential step in the initial
stage. In addition the plan involves appropriate supportive measures that were taken which
include Inj. NS-4 units (500ml each) Iv. over 6hrs, inj. Citicholine 500mg Iv. BD
(antioxidant to prevent neuronal toxicity), Tab.N-Acetyl cysteine (dispersable) 600mg 1 tab
PO BD (antioxidant, replenishing cellular glutathione), broad spectrum antibiotics eg. Inj.
Monocef 1gm Iv. BD and inj. Metronidazole 500mg Iv. TID, Magnesium (inj MgSO4
(50%)(4 ampules in 500ml of NS) as cell membrane stabilizer to prevent arrhythmias,
dopamine for inotropic support, if required and inj. Pantop -40mg Iv. BD to decrease HCl
production and for symptomatic relief. The survival rate of this novel intervention turns out
to be 91%(10/11). Early arrival, history of vomiting, early diagnosis, resuscitation, decreasing
formation and absorption of phosphine (by gastric and retrograde lavage with coconut oil
www.wjpps.com Vol 4, Issue 04, 2015. 953
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
followed by KMnO4), intensive monitoring and supportive therapy were associated with good
outcome. We, therefore, recommend the use of this regimen /protocol by all the intensivists
and physicians especially in rural and suburban areas in developing countries with limited
resources like India where instruments like gastroscope to remove undissolved pellets, or
intra-aortic balloon pump (IABP), ECMO (extracorporeal membrane oxygenation) as a
supportive measures, to provide prompt and adequate cardiovascular support till toxin is
removed, in health care divisions are hardly available.
KEYWORDS: Celphos, gastric lavage.
Abbreviations: AlP=aluminium phosphide, NS =normal saline
INTRODUCTION
Pesticide poisoning, whether due to self, accidental, occupational or for homicidal purpose, is
a global public health problem, and self-poisoning accounts for one-third of the world's
suicide rate.[1] Each year around 300,000 deaths occur worldwide due to pesticides.[2] Since
the first available report of Celphos,(trade name for aluminium phosphide (AlP), poisoning in
the early 1980s from India, it is now one of the most common causes of poisoning among
agricultural pesticides.[3,4] Most cases of Celphos poisoning are reported from northwest,
central India, some others from countries like Iran and Jordan, Sri Lanka and Morocco, with
few case reports from many developed countries. In a recent scenario AlP also poses as a
threat for chemical terrorism due to the immediate release of lethal phosphine gas.[5]
In India, AlP is marketed as an food grain fumigant formulated in the form of 3g tablet
consisting of AlP (56%) and carbamate (44%), in the names of Celphos, Alphos, Quickphos,
Phosfume, Phostoxin, Talunex, Degesch, Synfume, Chemfume, Phostek or Delicia.[6,7]
Celphos toxicity is due to the phosphine gas generated as a result of chemical reaction of
AlP with moisture or acid in the stomach [AlP+3H2O=Al(OH)3+PH3 or
AlP+3HCl=AlC13+PH3]. Once generated, phosphine(PH3) gas is rapidly absorbed throughout
the gastrointestinal tract, leading to systemic toxic effects involving the heart, lung, kidney,
liver with manifestation of serious cardiac arrhythmias, intractable shock, acidosis and
pulmonary edema. After absorption, phosphine is oxidised to oxyacids. Phosphine is excreted
in the urine as hypophosphite and also through the lung in the unchanged form. At cellular
level phosphine causes cellular hypoxia due to the inhibition of mitochondrial respiratory
www.wjpps.com Vol 4, Issue 04, 2015. 954
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
chain at cytochrome C oxidase level and due to the formation of highly reactive hydroxyl
radicals.[8,9]
After ingestion, toxic features usually develop within few minutes. In mild poisoning nausea,
repeated vomiting, diarrhea, headache, abdominal discomfort or pain and tachycardia are
common clinical features, and these patients usually show recovery.[6] On the other hand, in
moderate to severe ingestional poisoning, the signs and symptoms of the gastrointestinal,
cardiovascular, respiratory and nervous systems appear initially and, later on, features of
hepatic and renal failure and disseminated intravascular coagulation may also occur.[6,10] The
toxicity of AlP particularly affects the cardiac and vascular tissues, which manifests as
profound and refractory hypotension, congestive heart failure, electrocardiographic (ECG)
abnormalities, myocarditis, sub endocardial infarction or pericarditis. ECG abnormalities
include rhythm disturbances, ST-T changes and conduction defects. Temporal correlation in
ECG changes showed that during the initial 3–6 h, sinus tachycardia is predominant, in the 6–
12 h period ST-T changes and conduction disturbances appear, while in the later period,
arrhythmias occurred.[11]
Celphos poisoning has always been a big headache and menace for the intensivists
throughout the world probably due to nonavailability of its antidote and 100% mortality. The
literature is full of different drugs and trials to counter its irreversible toxic effects, but hardly
with any concrete success. Here we report the novel combo intervention which we have
formulated and standardized over last 1.5 years on celphos patients admitted to ICU of
Maharishivalmiki hospital, Govt of NCT of Delhi. The present study aimed at evaluating the
effectiveness of this novel intervention in decreasing the very high mortality and morbidity
that occur as a result of celphos poisoning.
MATERIALS AND METHODS
In total eleven patients got admitted to ICU of Maharishi Valmiki Hospital, Govt of NCT of
Delhi over the last 1.5 year period between June 2013-Nov. 2014 with a definite history of
intake of celphos (AlP) poison. Most of the patients were young (<42Yrs), male, married, and
literate. Most of them had taken 1-3 tablets of AlP (each 3g while 0.5g dose is lethal) and
were brought less than an hour of intake of poison. In most cases there had been legal
evidence (catridge containing AlP) of deliberate celphos intake. None of them had any
history of mental illness, or hypotension, Diabetes mellitus, Koch or bleeding. After
ingestion, nearly half of them had features of cardiogenic shock, hypotension and
www.wjpps.com Vol 4, Issue 04, 2015. 955
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
arrhythmias, mild respiratory distress, menthol like cooling upon breathing, and mild GI
symptoms like nausea, vomiting, gastric pain while only one of them who reached hospital
with delay of 2hours and had taken alcohol also, had features of combined respiratory/CVS/
CNS involvement. The approval of Ethical Committee of the institute had already been taken
for all poisoning cases. The reason for pre-approval of this treatment regimen for celphos
poisoning was that in such cases mortality is 100% with out any specific treatment and no
time should be lost in resuscitating such patients.
On admission to ICU, the patients were made comfortable on the bed, monitoring gadgets
were attached for Heart Rate (HR), Non-Invasive Blood Pressure (NIBP), ECG, Pulse
Oximetry (SpO2) and End-tidal carbon dioxide (EtCO2) and Ryle's tube was inserted through
nasal route. Novel combo intervention for celphos poisoning was initiated which included.
2.1 Gastric Lavage with 100ml of
Solution (A): 500ml of coconut oil mixed with 3 ampules of NaHCO3(7.5%,25ml vial).
Solution( B): 2 pinches of KMNO4 in one liter of normal saline (≈1:10,000 dilution).
Gastric lavage was done in three cycles via Ryles tube.Each cycle consisting of initially
giving 100ml of solution A which was suctioned back within 5 seconds up to the maximum
possible quantity without harming the patient followed by 100 ml of solution B which was
given, kept and suctioned back in similar manner.The time gap between successive lavages
was three minutes. In this procedure 50ml sterile syringes were used and all antiseptic
precautions were taken.
2.2 Retrograde lavage : Ryles tube was inserted via rectum after properly lubricating it
with lidocaine jelly (2%),taking all precautions not to perforate the gut, up to the length so
that only 15cms of ryles tube were kept outside the anal verge.Then retrograde lavage was
done in similar manner with 100ml of solution A and solution B as in gastric lavage.
Retrograde lavage was done only after completion of three cycles of gastric lavage.
2.3 Supportive therapy: included
• Inj. NS-4 units(500ml each) Iv. over 6hrs
• Inj. Citicholine 500mg Iv. BD
• Tab. N- Acetylcysteine (dispersable) 600mg 1 tab PO BD
• Inj. MgSO4 (50%)--4 ampules in 500ml of NS Iv over 24 hrs.
www.wjpps.com Vol 4, Issue 04, 2015. 956
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
• Inj. Monocef 1gm Iv. BD
• Inj. Metronidazole 500mg Iv. TID
• Inj. PANTOP -40mg Iv. BD
Symptomatic treatment was initiated on a patient to patient basis. During this period, strict
and vigil monitoring of all vital organs and important parameters like SaO2,
Electrocardiogram was done and treatment regimen were titrated according to the clinical
condition of the patients. Gastric lavage and retrograde lavage was again performed after 3
hours of admission with the same solution only once.
After admission in the ICU, all baseline routine and specific investigations were carried out
including arterial blood gas analysis (ABG), CBC, KFT/LFT/Electrolytes, chest x-rays, urine
examination, input/output monitoring, PT/INR after every 12hrs period. At the end of the
study period, all the data were arranged systematically and were subjected to statistical
analysis using non-parametric tests. Value of P<0.05 was taken as significant value.
RESULTS
In the last 1.5 years, 11 patients got admitted in ICU of Maharishi Valmiki Hospital, Govt of
NCT of Delhi, with an alleged history of Celphos intake. The demographic profile of these
patients is shown in Table 1.The age of 11 patients who got admitted in ICU ranged from 23
to 48 years, with a mean and standard deviation of 35.97±4.02. There was significant
difference on the gender basis as 81.8% (9/11) admitted with Celphos consumption were
males. The incidence of poisoning was surprisingly high with a significant proportion in the
more literate class (91%)(10/11). The incidence was significantly higher in the families of
low income 72.7% (8/11), especially among the married young members 81.8%)(9/11). The
incidence of poisoning was higher among the rural 63% (7/11) as compared to sub-urban
population. The maximum number of patients 45.5% (5/11) presented clinically with
cardiovascular instability, either in the form of hypotension or arrhythmias which was
clinically quite significant (P<0.05) [Table 2]. Mild GI symptoms in the form of nausea,
vomiting occurred in 45.5% (5/11)) which was again quite significant (P<0.05). Also, 36.3%
(4/11) of the patients presented with mild respiratory distress while only 9.1% 1(1/11) of the
patients had symptoms like altered sensorium or combined symptoms related to respiratory,
CVS or CNS [Table 2]. Significantly high 54.5% (6/11) no. of patients had two organs, liver
and kidneys, mildly affected by the poison.
www.wjpps.com Vol 4, Issue 04, 2015. 957
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
Further, 45.5%(5/11) of the patients required ionotropic support for maintaining stable
hemodynamic parameters which was again quite significant (P<0.05). The mean stay in ICU
varied from 2 to 7 days, with a mean stay of 4.2days with an SD of 1.3. The survival rate
after following this combo intervention was 91% (10/11) while only 9%(1/11) succumbed to
Celphos poisonings which again is quite significant [Table 2]. The lone mortality was due
to delay in the hospitalization (>2hrs) and the use of agents that increases the solubility of
AIP pellets like in our case the patient that died was alcoholic.
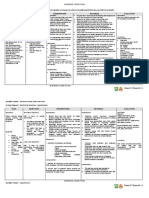
Table 1: Demographic profile of Celphos poisoning patients.
Total Number of patients 11
a) Age in years 23-48yrs (35.97±4.02)
(mean± SD)
b) Gender *9:2
Male:female
4:7*
c) Location
Sub-urban:rural
*10:1
d) Educational level
literate: illiterate
*9:2
e) Maritial status
married : unmarried
f) Family income *8:3
(<Rs5000/month:>Rs7000/month)
low : high
*P<0.05
Table :2 Clinical presentation and treatment pattern of celphos poisoning patients
CHARACTERISTICS NO. Of patients
1.Clinical presentation in emergengy ward
• GI symptoms : nausea, vomiting,abdominal pain 5/11(45.5%)*
• Respiratory distress, menthol like cooling effect upon
4/11(36.3%)*
breathing)
• CVS instability/arrhythmias 5/11(45.5%)*
• altered sensorium 1/11 (9%)
• combined respiratory/CVS/ CNS involvement 1/11(9%)
www.wjpps.com Vol 4, Issue 04, 2015. 958
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
• number of organs involved
• two (liver, kidneys) 6/11 (54.5%)*
• three(liver, kidneys, heart) 5/11(45.5%)
2. Treatment pattern and outcome
• Ionotropic support 5/11(45.5%)*
• Stay in hospital (5-7days) 4.2±1.3
• outcome (death/survival) 1/10(9/91*)%
• post discharge complications observed during followup of 0/10
one year
*P<0.05
DISCUSSION
Celphos poisoning has always been a big headache and menace for the intensivists
throughout the world probably due to non-availability of its antidote and 100% mortality
which does not encourage the physicians to try whole heartedly to salvage the patients. The
literature is full of different drugs and trials to counter its irreversible toxic effects, but hardly
with any concrete success. Here we report combo intervention for Celphos poisoning with
91% survival rate and only 9% mortality. The management plan involves gastric lavage (with
an aliquot of coconut oil mixed with NaHCO3 followed by KMNO4 in NS) as an essential
step in the initial stage. The principles aim of our management plan was to sustain life with
appropriate resuscitation measures until phosphine is excreted from the body. Although
Gastric lavage with saline or sodium bicarbonate or potassium permanganate has been
recommended by earlier studies[12] but not in the form of protocol (as discussed in material
and methods section) which we have formulated and standardized over last 1.5 year. The
rationale behind the use of a mixture of coconut oil and soda bicarbonate in our patients
aimed to decrease the formation and absorption of phosphine (PH3) produced as a result of
chemical reaction of AlP with moisture and/HCl [AlP+3H2O=Al(OH)3+PH3 or
AlP+3HCl=AlC13+PH3]. The mechanism by which coconut oil reduces the toxicity of
phosphides is unknown but most probably it forms a protective layer around the
gastrointestinal mucosa, thereby preventing the absorption of phosphine gas. Secondly, Soda
bicarbonate mainly neutralizes the HCl in stomach and thus diminishing the catalytic reaction
of phosphide with HCl, thereby inhibiting the release of phosphine from AlP pellets.[13]
Further, use of KMnO4 in NS in non-corrosive conc. (<1:10,000 dilution) is guided by the
fact that it provides alternative medium for AlP to react with, oxidising phosphine to non-
www.wjpps.com Vol 4, Issue 04, 2015. 959
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
toxic phosphate releasing Al(MnO4)3 and less toxic potassium phosphate instead (KPH2),
[AlP +3H2O+ 3KMnO4=Al(MnO4)3 +3KPH2], Phosphine/ phosphide, if it does not induce
emesis or eliminated completely by gastric and retrograde lavage, is rapidly absorbed from
the gastrointestinal mucosa and once it gains access to bloodstream it reaches various tissues
and at cellular level inhibits the mitochondrial respiratory chain and hence leads to cell
necrosis and death. It has been suggested that phosphine leads to non-competitive inhibition
of the cytochrome oxidase of mitochondria, blocking the electron transfer chain and oxidative
phosphorylation, producing an energy crisis in the cells.[4,6] Recently, Chugh et al. found
inhibition of catalase and induction of superoxide dismutase enzymes by phosphine in
humans, leading to free radical formation, lipid peroxidation and protein denaturation of cell
membrane, ultimately leading to hypoxic cell damage.[14] In our treatment regimen, novel
therapies such as N‐Acetyl cysteine (600mg tab BD) (antioxidant, replenishing cellular
glutathione), and Inj. Citicholine (500mg Iv BD) (prevents neuronal injury) have been tried to
reduce free radical damage to tissues and the results were excellent. The reason for oral
delivery of N‐Acetyl cysteine is to provide first line of protection to gastrointestinal mucosal
cells from reactive oxygen species generated as a result of loss of antioxidant enzymes and
secondarily, unlike glutathione, N‐Acetyl cysteine is more permeable antioxidant.
All AlP poisoning require hemodynamic monitoring and early resuscitation with fluids and
vasoactive agents. In our cases 4 liters of NS were administered within first 6hrs guided by
Central Venous Pressure (CVP) (with an aim to keep CVP at around 8-10cm of water) in
order to maintain adequate hydration and renal perfusion required for renal excretion of
phosphine.. Further, cardiac dose of dopamine 2-5μg/kg/min was given to those patients who
required ionotropic support. The proton pump inhibitors added in our protocol were given in
order to decrease the production of HCl and for symptomatic relief.
Mild GI symptoms like nausea, vomiting, abdominal pain and diarrhea are usually the first to
occur after exposure. 45.5% (5/11) patients in our study group came with these symptoms.
However none of them reported to have GI bleeding as reported by various studies. Most of
patients in our study group developed altered LFT and KFT profile (in the form of raised
aspartate transaminase (AST) or creatinine), respiratory and metabolic acidosis (as depicted
in ABG reports) which subsided within few days after appropriate measures were taken.
www.wjpps.com Vol 4, Issue 04, 2015. 960
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
Furthermore magnesium (Inj. MgSO4 (50%) -4 ampules in 500ml of NS Iv over 24 hrs) has
been added as a therapeutic option in our treatment plan. Magnesium acts as a cell membrane
stabilising agent and prevents cardiac arrythmais induced by phoshine toxicity. Myocardial
depression from Celphos toxicity is not uncommon and carries a very high mortality.[15,16]
These cardiotoxic effects were quite marked in our patients as 45.5% (5/11) of the patients
required ionotropic support. Vascular changes may lead to marked low blood pressure that
does not respond well to vasopressor agents. Cardiotoxicity/toxic chemical myocarditis is
manifested as depressed left ventricular ejection fraction, ECG changes varying from ST
segment elevation/depression, PR prolongation, broad QRS complexes, and right or left
bundle branch block, supraventricular ectopics or fibrillation.[11,17]
In acute poisoning cases, death due to acute hepatocellular toxicity and fulminant hepatic
failure can occur. Blood and protein in the urine, and acute kidney failure due to pHOSHINE
toxicity and circulatory shock can occur. Also, there have been reports of significant
hypomagnesemia and massive focal myocardial damage [18,19] Chronic exposures to very low
concentrations may result in anemia, bronchitis, GI disturbances, and visual, speech, and
motor disturbances.[20] Severe exposure can cause accumulation of fluid in the lungs,
pulmonary edema, which may have a delayed onset of 72 hours or more after exposure.
Furthermore, this phosphine gas is eliminated through the lungs; hence, due to high
concentration in the respiratory alveoli, it is responsible for direct alveolar damage.[21] Acute
respiratory distress syndrome (ARDS) and exudative pleural effusions can develop. Studies
in the past have shown increased levels of inflammatory markers (cytokines and interleukins)
in ARDS, which increase the capillary permeability. This combined effect of increase in
capillary permeability due to global hypoxia and ARDS could be responsible for the
exudative effusion seen predominantly in the pleural cavity and not in other serous
cavities.[22]
The findings of our study do correlate with various studies worldwide, as most of our patients
presented with arrhythmias of varying nature, hypotension, altered LFT and KFT profile,
respiratory and metabolic acidosis, mild respiratory and GI disturbances. However, only one
of our patients developed multi-organ system failure and died. Rest of Patients (10/11) did
not devoloped life threatening complications like acute hepatocellulae toxicity, massive focal
myocadial damage, GI bleeding ,cardiac failure, non cardiogenic pulmonary edema(ARDS).
This could be possibility due to early hospitalization, and immediate resuscitation of the
www.wjpps.com Vol 4, Issue 04, 2015. 961
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
patients by our novel intervention which aimed to diminish the production and absorption of
phosphine and enhance its excretion plus intensive monitoring and appropriate supportive
therapy added in our protocol to prevent any organ toxicity.
The main principles of our novel intervention are the following.
• Diminishing the production and absorption of phosphine and accelerating its removal
through GI tract as explained earlier
• Reduce organ toxicity with appropriate supportive measures like use of antioxidants to
reduce free radical damage, magnesium supplementation as cell membrane stabilizer to
prevent arrhythmias.
• Use of broad spectrum antibiotics as coconut oil used in lavage is non-sterile and proton
pump inhibitors to counter acidic medium required for phosphine production.
• Phosphine is excreted through urine also. Therefore, adequate hydration and renal
perfusion by low-dose dopamine 2–5 μg/kg/minute must be maintained. Diuretics are not
useful in the presence of profound shock.
• Enhance phosphine excretion, especially through lungs, if required, by increasing the
respiratory rate, which becomes easier when the patient is paralyzed, sedated and put on
mechanical ventilation.
Improved intensive care, availability of gastroscope in far flung areas, social awareness
regarding its toxicity, strict laws and legislations regarding the free sales of the chemical
could further reduce the mortality due to AlP toxicity as there is no antidote available
presently. In acute poisioning cases, advanced measures like use of intra-aortic balloon pump
(IABP) to mechanically support the heart can be evaluated, in future, to reduce toxic
myocarditis with refractory shock due to AlP poisoning.[23,24] The possibility of a beneficial
effect of extracorporeal life support (ECLS) as a supportive measure[25] may prove a useful
treatment modality, in future, as this device can maintain adequate tissue perfusion to prevent
multiorgan failure and give time to recovery of myocardial tissue from phosphine-induced
injury.
CONCLUSION
Due to no known specific antidote, management for celphos poisoning remains primarily
supportive care. With the novel intervention we have formulated and standardized over last
1.5 years we were able to save 91% of our patients. Early arrival, diagnosis, history of
vomiting after consumption of AlP, EARLY resuscitation and decreased formation and
www.wjpps.com Vol 4, Issue 04, 2015. 962
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
absorption of phospine (by lavage with coconut oil and KMnO4) intensive monitoring and
supportive therapy were the core of our intervention that resulted in good outcome. We,
therefore, recommend the use of this protocol by all the intensivists and physicians especially
in rural and suburban areas in developing countries with limited resources like India where
instruments like gastroscope, to remove undissolved pellets or intra-aortic balloon pump
(IABP), extracorporeal life support (ECLS), as a supportive measures to provide prompt and
adequate cardiovascular support till toxin is removed, in health care divisions are hardly
available.
ACKNOWLEDGMENT
The authors gratefully acknowledge the technical staff of Maharishi Valmiki Hospital, Govt
of NCT of Delhi for providing technical help.
REFERENCES
1. Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal
pesticide self-poisoning: Systemic review. BMC Public Health., 2007; 7: 357–71.
2. Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: A continuing
tragedy in developing countries. Int J Epidemiol., 2003; 32: 902–9.
3. Murali R, Bhalla A, Singh D, Singh S. Acute pesticide poisoning: 15 years experience of
a large North-West Indian hospital. ClinToxicol (Phila), 2009; 47: 35–8
4. Gargi J, Rai H, Chanana A, Rai G, Sharma G, Bagga IJ. Current trend of poisoning-a
hospital profile. J Indian Med Assoc., 2006; 104: 72-3–94.
5. Bogle RG, Theron P, Brooks P, Dargan PI, Redhead J. Aluminium phosphide
poisoning. Emerg Med J., 2006; 23: e3
6. Goel A, Aggarwal P. Pesticide poisoning. Natl Med J India., 2007; 20: 182–91.
7. Aluminium phosphide poisoning. [Last accessed on 2009 Aug 16]. Available
from:www.who.int/entity/ipcs/poisons/pim_aluminium_phosphide.pdf.
8. Chefurka W, Kashi KP, Bond EJ. The effect of phosphine on electron transport of
mitochondria.PesticideBiochem Physiol., 1976; 6: 65–84.
9. Bolter CJ, Chefurka W. Extramitochondrial release of hydrogen peroxide from insect and
mouse liver mitochondria using the respiratory inhibitors phosphine, myxothiazol, and
antimycin and spectral analysis of inhibited cytochromes. Arch BiochemBiophys., 1990;
278: 65–72.
www.wjpps.com Vol 4, Issue 04, 2015. 963
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
10. Proudfoot AT. Aluminium and zinc phosphide poisoning. ClinToxicol (Phila) 2009; 47:
89–100.
11. Katira R, Elhance GP, Mehrotra ML, Srivastava SS, Mitra A, Agarwala R, et al. A study
of aluminium phosphide (ALP) poisoning with special reference to electrocardiographic
changes. J Assoc Physicians India, 1990; 38: 471–3.
12. Kondo S, Tokuhashi K, Nagai H, Iwasaka M, Kaise M. Spontaneous Ignition Limits of
Silane and Phosphine.Combust. Flame., 1995; 101: 170–4.
13. Valmas N, Ebert PR. Comparative Toxicity of Fumigants and a Phosphine Synergist
Using a Novel Containment Chamber for the Safe Generation of Concentrated Phosphine
Gas. PLoS One., 2006; 1: e130.
14. Chugh SN, Arora V, Kaur S, Sood AK. Toxicity of exposed aluminium phosphide. J
Assoc Physicians India, 1993; 41: 569-70.
15. Bogle RG, Theron P, Brooks P, Dargan PI, Redhead J. Aluminium phosphide poisoning.
Emerg Med J., 2006; 23: e3
16. Siwach SB, Singh P, Ahlawat S, Dua A, Sharma D. A study of serum and tissue
magnesium content in patients of aluminium phosphide poisoning and critical evaluation
of high dose MgSO4 therapy in reducing mortality. J Assoc Physicians India., 1994; 42:
107–10.
17. Mathur A, Swaroop A, Aggarwal A. ECG changes in aluminium phosphide and organo
phosphorus poisoning. Indian Pract, 1999; 52: 249-52.
18. Suman RL, Savani M. Pleural Effusion - A Rare Complication of Aluminium Phosphide
Poisoning. Indian Paediatr, 1999; 36: 1161-3.
19. Chugh SN. Aluminium Phosphide in Lall SB, Essentials of Clinical Toxicology. New
Delhi: Narosa Publishing House, 1998; 41-6.
20. Lall SB, Sinha K, Mittra S, Seth SD. An experimental study on cardio toxicity of
aluminium phosphide. Indian J Exp Biol, 1997; 35: 1060-4.
21. Sudakin DL. Occupational exposure to aluminium phosphide and phosphine gas: A
suspected case report and review of the literature. Hum ExpToxicol, 2005; 24: 27-33.
22. Suman RL, Savani M. Pleural Effusion - A Rare Complication of Aluminium Phosphide
Poisoning. Indian Paediatr, 1999; 36: 1161-3
23. L, Adhyapak S, Jaydev S, Shetty G, Varghese K, Patil C, et al. Intra-aortic balloon pump
in toxic myocarditis due to aluminium phosphide poisoning. J Med Toxicol, 2009; 5:
80–3.
www.wjpps.com Vol 4, Issue 04, 2015. 964
Hakim et al. World Journal of Pharmacy and Pharmaceutical Sciences
24. Shivaprasad C. Fatal aluminium phosphide poisoning due to myocardial depression
refractory to high dose inotropic support and intra-aortic balloon counterpulsation. Indian
J Crit Care Med., 2008; 12: 37–8.
25. Megarbane B, Deye N, Leprince P. Clinical review: Aggressive management and
extracorporeal support for drug-induced cardiotoxicity. Critical Care., 2007; 11: 207.
www.wjpps.com Vol 4, Issue 04, 2015. 965
View publication stats
You might also like
- Jop 12583 Rev EVcurrentprotocolsDocument7 pagesJop 12583 Rev EVcurrentprotocolsali baridiNo ratings yet
- Advances in Indole-Containing Alkaloids As Potential Anticancer Agents by Regulating AutophagyDocument12 pagesAdvances in Indole-Containing Alkaloids As Potential Anticancer Agents by Regulating AutophagyBRAYAN MORENONo ratings yet
- Fol Firin OxDocument11 pagesFol Firin OxGuilherme SalgadoNo ratings yet
- Kusum D.V., Bhosale U.V. - Formulation and Optimization of Polymeric Nano Drug Delivery System of Acyclovir Using 3 (2) Full Factorial DesignDocument10 pagesKusum D.V., Bhosale U.V. - Formulation and Optimization of Polymeric Nano Drug Delivery System of Acyclovir Using 3 (2) Full Factorial DesignJordy CanalesNo ratings yet
- Amylase and Dipeptidyl Peptidase 4 DPP 4 Inhibitory Effects of Melicope Latifolia Bark Extracts and Identification of Bioactive Constituents Using inDocument11 pagesAmylase and Dipeptidyl Peptidase 4 DPP 4 Inhibitory Effects of Melicope Latifolia Bark Extracts and Identification of Bioactive Constituents Using inRohaniNo ratings yet
- Formulation, Optimizationand Evaluation of Sublingual Film of Enalapril Maleate Using 3 Full Factorial DesignDocument9 pagesFormulation, Optimizationand Evaluation of Sublingual Film of Enalapril Maleate Using 3 Full Factorial DesignPRASANTA KUMAR MOHAPATRANo ratings yet
- Design and Charaterzation of Ethosome Drug Delivery System Containing Isradipine For Topical ApplicationDocument12 pagesDesign and Charaterzation of Ethosome Drug Delivery System Containing Isradipine For Topical ApplicationBaru Chandrasekhar Rao100% (1)
- AIJPMS - Volume 3 - Issue 1 - Pages 15-31Document17 pagesAIJPMS - Volume 3 - Issue 1 - Pages 15-31Eman MahmoudNo ratings yet
- Vasodilator Effect of 1-Trifluoromethoxyphenyl-3-1Document7 pagesVasodilator Effect of 1-Trifluoromethoxyphenyl-3-1Syed Danish AliNo ratings yet
- Tajdar-Khan-et-al - ccl4Document18 pagesTajdar-Khan-et-al - ccl4drvenkataNo ratings yet
- Immuno Supre SiveDocument16 pagesImmuno Supre SiveMartalina LimbongNo ratings yet
- Op ManagmentDocument3 pagesOp ManagmentThevaprathapan ChellathuraiNo ratings yet
- Intensive Care 1Document6 pagesIntensive Care 1raitchuNo ratings yet
- Peptide and Protein DeliveryFrom EverandPeptide and Protein DeliveryChris Van Der WalleRating: 2 out of 5 stars2/5 (1)
- 6 Non-Infectious Indications For AntibioticsDocument3 pages6 Non-Infectious Indications For Antibioticscustomize36No ratings yet
- A Renaissance in Peptide TherapeuticsDocument4 pagesA Renaissance in Peptide TherapeuticsReza-ul JalilNo ratings yet
- MURAYYADocument5 pagesMURAYYADebby NandaaNo ratings yet
- Invitro Studies On The Effect of Adhatoda Vasica Nees. in Adipocyte 3T3 - L1 Cell LinesDocument15 pagesInvitro Studies On The Effect of Adhatoda Vasica Nees. in Adipocyte 3T3 - L1 Cell LinesDR. BALASUBRAMANIAN SATHYAMURTHYNo ratings yet
- Diana College of Nursing, No.68, Chokkanahalli, Jakkur Post, Bangalore-64Document28 pagesDiana College of Nursing, No.68, Chokkanahalli, Jakkur Post, Bangalore-64AnggraAnzhaniNo ratings yet
- J Addr 2020 11 008Document69 pagesJ Addr 2020 11 008thanaNo ratings yet
- Recent Advances in Anti-Aging Medicine: Review ArticleDocument8 pagesRecent Advances in Anti-Aging Medicine: Review Articlemariana sanguinettiNo ratings yet
- Translational Glycobiology in Human Health and DiseaseFrom EverandTranslational Glycobiology in Human Health and DiseaseMichelle KilcoyneNo ratings yet
- Drugs Developed in IndiaDocument8 pagesDrugs Developed in IndiaSneha Karan JagtapNo ratings yet
- International Consensus Guidelines For The Optimal Use of The PolymyxinsDocument30 pagesInternational Consensus Guidelines For The Optimal Use of The PolymyxinsMaria Josefa Henriquez SanhuezaNo ratings yet
- OB TXA Case Study - 090752Document10 pagesOB TXA Case Study - 090752Marlin LopezNo ratings yet
- New Aspects of Therapy of Hepatocellular Carcinoma PDFDocument16 pagesNew Aspects of Therapy of Hepatocellular Carcinoma PDFKrrliveNo ratings yet
- Assessment of Antidiabetic Effect of 4-HIL in Type 2 Diabetic and Healthy Sprague Dawley RatsDocument11 pagesAssessment of Antidiabetic Effect of 4-HIL in Type 2 Diabetic and Healthy Sprague Dawley RatsMaxin BangsalNo ratings yet
- Pulsatile Dds PDFDocument19 pagesPulsatile Dds PDFSiva PrasadNo ratings yet
- Clinical Toxicology: Clinical Biochemistry of HepatotoxicityDocument19 pagesClinical Toxicology: Clinical Biochemistry of HepatotoxicitySailu karriNo ratings yet
- Pharmaceuticals 16 00191Document18 pagesPharmaceuticals 16 00191unknownNo ratings yet
- Formulation and Evaluation of Time Dependendt Release of Montelukast Tablets by Using Mini Tablet TechnologyDocument13 pagesFormulation and Evaluation of Time Dependendt Release of Montelukast Tablets by Using Mini Tablet TechnologyBaru Chandrasekhar RaoNo ratings yet
- 1705128278galley Proof-Knowledge, Attitude and Practice and Associated Factors On Oxygen Therapy Among Nurses and Midwives in Y12 HMC-2022 GCDocument11 pages1705128278galley Proof-Knowledge, Attitude and Practice and Associated Factors On Oxygen Therapy Among Nurses and Midwives in Y12 HMC-2022 GCKirubel TesfayeNo ratings yet
- Role of PRF in ProsthodonticsDocument11 pagesRole of PRF in ProsthodonticsAkshayaa BalajiNo ratings yet
- Baru 2Document8 pagesBaru 2Nazihan Safitri AlkatiriNo ratings yet
- 11 Iajps11072017Document7 pages11 Iajps11072017Baru Chandrasekhar RaoNo ratings yet
- Guidelines For The Diagnosis and Treatment of Helicobacter Pylori Infection in Korea, 2013 Revised EditionDocument24 pagesGuidelines For The Diagnosis and Treatment of Helicobacter Pylori Infection in Korea, 2013 Revised EditionRobert UntaruNo ratings yet
- Bio Evailabilitas Dan Bioekivalensi Aciclovir BABEDocument13 pagesBio Evailabilitas Dan Bioekivalensi Aciclovir BABERian Nurdiana100% (1)
- SexyDocument14 pagesSexyDr.Ramkaran SainiNo ratings yet
- Formulation and Evaluation of Once A Day Dual CompDocument9 pagesFormulation and Evaluation of Once A Day Dual CompKuldeep VinchurkarNo ratings yet
- Clove (Syzygium Aromaticum L.), A Potential Chemopreventive Agent For Lung CancerDocument10 pagesClove (Syzygium Aromaticum L.), A Potential Chemopreventive Agent For Lung CancerpriyaNo ratings yet
- 13 Iajps13102017 PDFDocument6 pages13 Iajps13102017 PDFBaru Chandrasekhar RaoNo ratings yet
- Formulation and Evaluation of Sublingual Tablet of Enalapril Maleate by 32 Full Factorial DesignDocument17 pagesFormulation and Evaluation of Sublingual Tablet of Enalapril Maleate by 32 Full Factorial DesignPRASANTA KUMAR MOHAPATRANo ratings yet
- Anti-Cancer Products From Marine Sponges: Progress and PromiseDocument3 pagesAnti-Cancer Products From Marine Sponges: Progress and PromiseRizkiNo ratings yet
- (216 235) V10N5CTDocument20 pages(216 235) V10N5CTgritty gallantNo ratings yet
- Controlled Delivery SystemsDocument12 pagesControlled Delivery SystemsSusan NyaguthiìNo ratings yet
- A Prolonged Release Parenteral Drug Delivery SystemDocument11 pagesA Prolonged Release Parenteral Drug Delivery SystemronnymcmNo ratings yet
- Controlled Release Drug Formulation in Pharmaceuticals: A Study On Their Application and PropertiesDocument17 pagesControlled Release Drug Formulation in Pharmaceuticals: A Study On Their Application and PropertiesintanNo ratings yet
- PharmacovigilanceinClinicalDentistry SCDocument6 pagesPharmacovigilanceinClinicalDentistry SCIoana AntonesiNo ratings yet
- Safety, Analgesic, and Anti-Inflammatory Effects of Aqueous and Methanolic Leaf Extracts of Hypericum Revolutum Subsp. KenienseDocument11 pagesSafety, Analgesic, and Anti-Inflammatory Effects of Aqueous and Methanolic Leaf Extracts of Hypericum Revolutum Subsp. KenienseInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cancer Treatment and the Ovary: Clinical and Laboratory Analysis of Ovarian ToxicityFrom EverandCancer Treatment and the Ovary: Clinical and Laboratory Analysis of Ovarian ToxicityNo ratings yet
- Enhancement of The Solubility and Bioavailability of Pitavastatin Through A Self-Nanoemulsifying Drug Delivery System (SNEDDS)Document18 pagesEnhancement of The Solubility and Bioavailability of Pitavastatin Through A Self-Nanoemulsifying Drug Delivery System (SNEDDS)Lina WinartiNo ratings yet
- Efect AntihiperglicemicDocument5 pagesEfect AntihiperglicemicVasincuAlexandruNo ratings yet
- Interaccion Alimento - FarmacoDocument8 pagesInteraccion Alimento - FarmacoNATALIA TOVAR ORTIZNo ratings yet
- Preparation and Characterization of Isoniazid-Loaded Crude Soybean Lecithin LiposomesDocument8 pagesPreparation and Characterization of Isoniazid-Loaded Crude Soybean Lecithin LiposomesPavesan NaidooNo ratings yet
- 2020 Article 1654Document13 pages2020 Article 1654alyaNo ratings yet
- Pomegranate Juice HealingDocument23 pagesPomegranate Juice HealingKingNo ratings yet
- Design and Development of Controlled Porosity Osmotic Pump Tablets of Zidovudine Using Sodium Chloride As Osmogen For The Treatment of Aids JPR 19Document8 pagesDesign and Development of Controlled Porosity Osmotic Pump Tablets of Zidovudine Using Sodium Chloride As Osmogen For The Treatment of Aids JPR 19gritty gallantNo ratings yet
- Moh Rafiqi Oktamis - P27820121072 - Jurnal Sistem PencernaanDocument91 pagesMoh Rafiqi Oktamis - P27820121072 - Jurnal Sistem PencernaanReg B24 Moh Rafiqi Oktamis TDIII Kep SoetomoNo ratings yet
- Nanostructured Lipid Carrier System For Topical deDocument13 pagesNanostructured Lipid Carrier System For Topical deJonathas MoreiraNo ratings yet
- DR Dicky - Antiinflamatory Effect of ABM in High Fat Diet Induced MiceDocument7 pagesDR Dicky - Antiinflamatory Effect of ABM in High Fat Diet Induced MiceFuma AjiNo ratings yet
- Non-Severe Pneumonia: 25 MG/KG 2 Times Per Day For 3 DaysDocument4 pagesNon-Severe Pneumonia: 25 MG/KG 2 Times Per Day For 3 DaysPramod bhalseNo ratings yet
- The Significance of Clinical Practice Guidelines ODocument7 pagesThe Significance of Clinical Practice Guidelines OPramod bhalseNo ratings yet
- The Yellow Wall-PaperDocument10 pagesThe Yellow Wall-PaperJuan Luis H GNo ratings yet
- Using ADX To Trade BreakoutsDocument44 pagesUsing ADX To Trade BreakoutsKrisMo Da100% (14)
- Veselin Iliev IQP PDFDocument94 pagesVeselin Iliev IQP PDFspock45No ratings yet
- Acute Kidney Injury W/ Hyperkalemia NCPDocument5 pagesAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNo ratings yet
- PathophysiologyDocument34 pagesPathophysiologyeunams_1195% (20)
- Pulmonary Hypertension Associated With Bronchopulmonary Dysplasia A ReviewDocument9 pagesPulmonary Hypertension Associated With Bronchopulmonary Dysplasia A ReviewEduardo Rios DuboisNo ratings yet
- Cardio OoooDocument11 pagesCardio OoooBrian BaggayanNo ratings yet
- 200 Special Topics For 42 BCSDocument187 pages200 Special Topics For 42 BCSRezaul RazibNo ratings yet
- CA - Adult Health Nursing PDFDocument55 pagesCA - Adult Health Nursing PDFMarvin Heramis RyanNo ratings yet
- Rheumatic Heart DiseaseDocument68 pagesRheumatic Heart DiseaseFuji Khairunnisa0% (1)
- Presentation Chapter 27 Pulmonary Embolism and ARDS CaseDocument91 pagesPresentation Chapter 27 Pulmonary Embolism and ARDS Caseavoyiad100% (1)
- Sample MCQs by Lawrence KindoDocument6 pagesSample MCQs by Lawrence KindoSecret AgentNo ratings yet
- 1,000 Questions To Help You Pass The Emergency Medicine BoardsDocument338 pages1,000 Questions To Help You Pass The Emergency Medicine Boardseric91% (11)
- Acute Decompensated Heart Failure: ReviewDocument11 pagesAcute Decompensated Heart Failure: ReviewFercee PrimulaNo ratings yet
- Lecture 01 - CVSDocument45 pagesLecture 01 - CVSHeeb WardaNo ratings yet
- 11 Lung PathologyDocument7 pages11 Lung PathologycarlgangcaNo ratings yet
- Teaching Plan - Pulmonary Edema-Maxine AndersonDocument3 pagesTeaching Plan - Pulmonary Edema-Maxine Andersonmander3No ratings yet
- Respiratory Plab 1 Notes 2014: SamsonDocument19 pagesRespiratory Plab 1 Notes 2014: Samsonزكريا عمرNo ratings yet
- Idiopathic Systemic Capillary Leak Syndrome - UpToDateDocument17 pagesIdiopathic Systemic Capillary Leak Syndrome - UpToDatenikos papamakariosNo ratings yet
- Proper Fluid Therapy, Vasopressors, and Inotropic - Dr. VidyaDocument40 pagesProper Fluid Therapy, Vasopressors, and Inotropic - Dr. VidyaTinton PristiantoNo ratings yet
- CHF PathophysiologyDocument4 pagesCHF PathophysiologyVirtudazo JessaNo ratings yet
- Fluids and ElectrolytesDocument179 pagesFluids and ElectrolytesduypalaNo ratings yet
- Familial Dilated Cardiomyopathy of Young Portuguese Water DogsDocument9 pagesFamilial Dilated Cardiomyopathy of Young Portuguese Water DogsJessareth Atilano CapacioNo ratings yet
- Levin (1993) - Drowning and Near Drowning (Klasifikasi Tenggelam)Document16 pagesLevin (1993) - Drowning and Near Drowning (Klasifikasi Tenggelam)Filbert TandeanNo ratings yet
- Module 2 - Symptoms and Syndromes in Diseases of Internal OrgansDocument133 pagesModule 2 - Symptoms and Syndromes in Diseases of Internal OrgansХассан ЯасирNo ratings yet
- Cor Pulmonale ReDocument35 pagesCor Pulmonale ReFabb NelsonNo ratings yet
- NSG 210 Study GuideDocument25 pagesNSG 210 Study GuideyasserNo ratings yet
- Cardiogeneicpulmonaryedema December2019Document9 pagesCardiogeneicpulmonaryedema December2019Amaranto Santoso ongkoNo ratings yet
- Myocarditis Pediatrics-1Document5 pagesMyocarditis Pediatrics-1AMOS MELINo ratings yet
- Cardiology. Scheme ..Dof3tna - Net... EgyDrDocument4 pagesCardiology. Scheme ..Dof3tna - Net... EgyDrJilan El SherBiny100% (1)
- Pneumonia Docs 1Document8 pagesPneumonia Docs 1carlosNo ratings yet
- PacuDocument45 pagesPacuHeron TitarsoleNo ratings yet
- Course Description: 3. Communities (Community Service)Document35 pagesCourse Description: 3. Communities (Community Service)April Mae Magos LabradorNo ratings yet