Professional Documents
Culture Documents
Admission To The ICU and Monitoring Technique Early Postoperative Care
Uploaded by
Widiartha WahyudiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Admission To The ICU and Monitoring Technique Early Postoperative Care
Uploaded by
Widiartha WahyudiCopyright:
Available Formats
Admission to the ICU and Monitoring Technique
Intraoperative monitoring with
Early Postoperative Care
Intraoperative monitoring with Swan-Ganz catheter measurements and transesophageal echocardiography
(TEE) are routinely used to direct hemodynamic management and fluid administration
The pathophysiology noted after off-pump surgery is slightly
different in that patients are not subjected to the insults of CPB and cardioplegia, two factors
that contribute to a systemic inflammatory response and transient myocardial depression.
Basic Features of the Early Postoperative Period
Adequate pharmacologicsedation and pain control is essential at this time and during the weaning process
from the ventilator
Early extubation is usually defined as withdrawal of mechanical ventilation within 8 hours of surgery
Right ventricular function may be improved when positive-pressure ventilation is not required
Important to provide adequate analgesia to these patients without producing respiratory depression,
generally using nonsteroidal anti-inflammatory drugs or low doses of narcotics
CARDIOPULMONARY BYPASS
Virtually all valve surgery and most coronary bypass surgery is performed using CPB
Basically, the blood drains by gravity or with vacuum assist from the right atrium into a reservoir, is
oxygenated, cooled or warmed, and then returned to the patient through an arterial cannula usually placed
in the ascending aorta
Arterial blood gases are measured to ensure that the oxygenator is providing adequate oxygenation and that
CO2 extraction is sufficient
Venous oxygen saturation is measured to determine if the systemic flow rate is adequate (>65–70%)
Systemic hypothermia is utilized to varying degrees during on-pump surgery as a means of organ protection
during a period of nonphysiologic, nonpulsatile flow at lower mean pressures
The serum level of antibiotics falls approximately 30–50% at the time of initiation of CPB and an additional
dose of a cephalosporin should be considered at that time. Alternatively, a second dose can be given 3–4
hours after the initial dose
The optimal mean blood pressure during CPB to maintain adequate organ system perfusion is controversial.
It has been shown that cerebral blood flow is more dependent on blood pressure than on flow rate
The brain is able to maintain cerebral blood flow by autoregulation until the pressure falls below 40 mm Hg,
but this response is inadequate in diabetic and hypertensive patients, in whom a higher pressure must be
maintained
Hypotension may be related to hemodilution, use of preoperative vasodilators (ACE inhibitors, ARBs,
calcium channel blockers, and amiodarone), vasodilation during rewarming, and autonomic dysfunction. It
may also result from inadequate systemic flow rates, impairment of venous drainage, aortic regurgitation,
the administration of cardioplegia, and during return of large amounts of cardiotomy-suctioned blood into the
circulation
Hypertension may be related to vasoconstriction with hypothermia, inadequate levels of anesthesia and
analgesia, elevation in endogenous catecholamine levels, and alterations in acid-base balance and blood
gas exchange
Although a higher mean blood pressure (around 80 mm Hg) might reduce some of the neurocognitive
changes seen after bypass, the standard management is to maintain a mean blood pressure around 65 mm
Hg using vasodilators (narcotics or inhalational anesthetics) or vasopressors (phenylephrine,
norepinephrine, or vasopressin) as long as flow rates are adequate. A venous oxygen saturation exceeding
65% generally indicates that the systemic flow rate is satisfactory, although there may be differences in
regional flow (i.e., less to the kidneys and splanchnic circulation). The venous saturation tends to be higher
during systemic hypothermia due to lower oxygen extraction, and may decrease significantly during
rewarming, necessitating an increase in flow rates.
Blood glucose tends to be elevated due to the hormonal stress response to surgery and CPB with insulin
resistance. The infusion of insulin to maintain blood glucose <180–200 mg/dL during surgery has not been
shown to reduce inotropic requirements or the occurrence of arrhythmias, but may reduce the incidence of
neurocognitive dysfunction and other adverse outcomes, including death
CABG
Hindari peningkatan O2 demand (karena takikardia, hipertensi), terutama saat pre-bypass dan selama
induksi
Hindari ischemia dan hipertensi (karena hipotensi) karena penggunaan vasodilating agent dengan cairan
dan α-agonist
Iskemia dapat dideteksi dengan TEE, tandanya :
o regional wall motion abnormalities
o peningkatan PAP
o ECG – perubahan ST segmen
Iskemia, terapi :
o Nitroglycerine
o β-blocker (esmolol)
o Narcotic
o Jika tidak membaik, segera CPB
Fast track - low-dose fentanyl or sufentanil, inhalational anesthetics, and propofol or dexmedetomidine
Ultra Fast track - short-acting narcotic remifentanil along with a volatile inhalational anesthetic with rapid
onset and offset of effect, such as sevoflurane or desflurane
OP-CAB (off pump)
o Jantung masih berdetak
o Penggunaan Swan-Ganz dan in-line mixed vein oxygen saturation monitoring
o Bed posisi trendelenburg dan miring kanan – agar cardiac filling membaik, judicious fluid
administration, antiarrhythmic therapy (lidocaine/magnesium), a-agents (phenylephrine) and
inotropes (epinephrine/milrinone), and, on occasion, insertion of an intra-aortic balloon pump
(IABP) may be used
PANGGILAN
1. Panggilan 1 (menanyakan berapa pump, pakai bio sensor / edward, mostcare, NIRS, dll)
2. Panggilan 2 (mengantar bed ICU ke OK PPJT)
3. Panggilan 3 (pasien proses pindah dari OK ke bed, tim ICU PPJT bersiap menjemput pasien)
4. Panggilan 4 (menjemput pasien ke OK)
PVR naik (mengakibatkan Qp menurun (Qp<Qs) - (R to L dominant)) :
Vasoconstricting drugs
Hypoxemia
Acidemia
Hypercapnia (high partial pressure of arterial carbon dioxide [PaCO2])
Atelectasis
Ventilasi tekanan positif yang berlebihan
POST OPERASI OH (OPEN HEART)
1. Pasien tiba di ICU di cek lab lengkap (DL, RFT, LFT, Alb, SE, Ca, Mg, FH, GDA). Lain-lain sesuai request.
2. Cek BGA via ISTAT dilaporkan oleh tim AKV ke konsultan membius
3. Lapor BGA dan lab post op ke konsultan yang membius dan konsultan mingguan saat pasien baru datang.
Sisanya, hanya lapor ke konsultan yang membius.
4. Setiap perubahan kondisi penting dilaporkan ke konsultan ICU
5. Beberapa konsultan yang membius, minta tetap dilapori pasien-pasien post op yang masih observasian
atau bermasalah, walaupun sudah 24 jam post op atau sudah divisite oleh konsultan icu.
6. Isi ecalyptus di lakukan oleh tim pagi
7. Target balance cairan post OH
o Defisit 10 - 30 ml/kg/hari
o Jika tidak tercapai dapat diberikan lasix extra evaluasi apakah perlu maintenance atau
penurunan dosis
Notes :
Beberapa kondisi slight hiperkalemia disengaja, jgn dikoreksi bila tidak ada advis. Kalau bingung, mending
dilaporkan aja sambil usul koreksi supaya mereka aware.
Koreksi hipovolum kebanyakan dengan Plasbumin 5% atau koloid lain. Kalau bisa diresepin aja post OH
biar keluarga ga bolak balik.
Kadang juga beberapa minta loading Kristaloid (paling sering Asering sih kalo aku)
Biar ga konsul bolak balik, mungkin bisa diliat tren nya aja untuk hemodinamik dan suhu rectal. Kalau
terkesan bermasalah, lapor sambil minta advis
Misal : " mohon ijin dok, untuk suhu trennya cenderung naik dibandingkan saat turun dari OK. jika di atas
37,5 apa boleh kami extra pct 1 gr" (misalnya.. )
Jika TD namun euvolume dapat diberikan NE atau Adrenalin pada pediatri
ST elevasi di semua lead curiga Perikarditis post-op
Weaning inotropik dan vasoaktif
o Adre / NE dlu setelah itu Dobu / Dopa terakhir Milrinon
o Sebelum aff Milrinon masuk Captopril dlu sebagai Vasodilator.
BP TURUN
Hypovolemia
Sudden termination of a drug infusion
Acute blood loss (drain)
Myocardial ischemia
Severe myocardial dysfunction
Arrhythmias
Ventilatory problems
Kinking or transient occlusion of the line, producing a dampened tracing
MENILAI KECUKUPAN CAIRAN
MAP
CVP target > 6-8
PLR kenaikan > 20%
IVC
KOREKSI NaBic
1 mEq/KgBB dalam 3 jam
100 mEq dalam 4 jam (dewasa)
(Tergantung kondisi)
PVR turun :
Vasodilating drugs
Alkalemia
Hypocapnia (low PaCO2)
Strenuous exercise
SVR naik :
Hypothermia
Hypovolemia
Cardiogenic shock
Stress response
Syndromes of low cardiac output
SVR turun :
Anaphylactic and neurogenic shock
Anemia
Cirrhosis
Vasodilation
DRAIN POST OPERASI
5cc/kg/jam REOPEN
3cc/kg/jam dalam 3 jam berturut - turut REOPEN
(tiap jam evaluasi : dapat diberikan extra Transamin 1 gram dan Vit K 2 ampul)
You might also like
- Common Post Operative Complication and ManagementDocument7 pagesCommon Post Operative Complication and ManagementprofarmahNo ratings yet
- Clinical evaluation and diagnosis of shockDocument3 pagesClinical evaluation and diagnosis of shockStephen CrossNo ratings yet
- Anaesthetic Management of PheochromocytomaDocument22 pagesAnaesthetic Management of PheochromocytomaZoelNo ratings yet
- Shock ManagementDocument26 pagesShock ManagementMuhammad Irfanuddin Bin IbrahimNo ratings yet
- Post Op CardiacDocument7 pagesPost Op CardiacsimplyputmonicNo ratings yet
- Ghid Resuscitare 2015Document53 pagesGhid Resuscitare 2015BejinaruOanaSiCristiNo ratings yet
- Open Heart 1Document18 pagesOpen Heart 1mohamedNo ratings yet
- MNI SAH ProtocolDocument10 pagesMNI SAH ProtocolAbo ZakariaNo ratings yet
- Dr. Sunatrio - Management Hypovolemic ShockDocument59 pagesDr. Sunatrio - Management Hypovolemic ShockArga Putra SaboeNo ratings yet
- Understanding Shock Types and TreatmentsDocument75 pagesUnderstanding Shock Types and TreatmentsaulianmediansyahNo ratings yet
- Approach To ShockDocument40 pagesApproach To ShockDivesh NaiduNo ratings yet
- Ghid Resuscitare 2015Document53 pagesGhid Resuscitare 2015Diana TiganucNo ratings yet
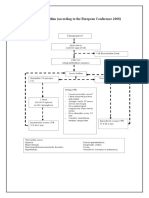
- Universal Algorithm (According To The European Conference 2000)Document11 pagesUniversal Algorithm (According To The European Conference 2000)Pawan MishraNo ratings yet
- Note On Cardiopulmonary Physiotherapy PDFDocument16 pagesNote On Cardiopulmonary Physiotherapy PDFTsz Kwan CheungNo ratings yet
- Care of Patients With Acute Biologic CrisisDocument72 pagesCare of Patients With Acute Biologic CrisisJames QuilingNo ratings yet
- Anaesthesia For Renal TransplantationDocument46 pagesAnaesthesia For Renal TransplantationShehan WijayasiriwardanaNo ratings yet
- MKSAP Questions: Intern ReportDocument37 pagesMKSAP Questions: Intern Reportfidelurtecho4881No ratings yet
- Cardiac Arrest With Pulmonary Embolism For PrintDocument32 pagesCardiac Arrest With Pulmonary Embolism For PrintSitthikorn StrikerrNo ratings yet
- Tips On How To Answer An Essay Question by Doaa Kamal 2001Document9 pagesTips On How To Answer An Essay Question by Doaa Kamal 2001Amr El TaherNo ratings yet
- ECMO Management Lecture 5Document39 pagesECMO Management Lecture 5dnafredyNo ratings yet
- Uia 11 ANAESTHESIA AND CHRONIC RENAL FAILUREDocument4 pagesUia 11 ANAESTHESIA AND CHRONIC RENAL FAILUREfadhiliNo ratings yet
- Neurology Case 6Document3 pagesNeurology Case 6muhammadridhwanNo ratings yet
- Post Resuscitation Care: 15 SEPTEMBER 2014Document27 pagesPost Resuscitation Care: 15 SEPTEMBER 2014Arnold DanielNo ratings yet
- Shock Five Point ZeroDocument78 pagesShock Five Point ZeroprashsubbuNo ratings yet
- TIVA in CKDDocument7 pagesTIVA in CKDfixheartNo ratings yet
- Intensive Care Unit (ICU) Manual 2020-21Document146 pagesIntensive Care Unit (ICU) Manual 2020-21anithaNo ratings yet
- Grand Round Case Presentation: by DR Sanjay Khare MD MedicineDocument19 pagesGrand Round Case Presentation: by DR Sanjay Khare MD MedicineHrishikeshNo ratings yet
- Recovery Room Care: BY Rajeev KumarDocument50 pagesRecovery Room Care: BY Rajeev Kumarramanrajesh83No ratings yet
- Acute Renal Failure Nursing Care PlanDocument15 pagesAcute Renal Failure Nursing Care PlanRanusha AnushaNo ratings yet
- Total Anomalous Venous ReturnDocument4 pagesTotal Anomalous Venous ReturnJohn Bernard Ting TizonNo ratings yet
- 8 - DR. Khaled - Cardiac SurgeryDocument26 pages8 - DR. Khaled - Cardiac SurgeryMuhand.No ratings yet
- Early Post-Operative Pulmonary Hypertension Management in The ICUDocument34 pagesEarly Post-Operative Pulmonary Hypertension Management in The ICUari wijayantiNo ratings yet
- HarrisDocument25 pagesHarrisHafiz AlfarizieNo ratings yet
- Master File 2003 - Body As A WholeDocument32 pagesMaster File 2003 - Body As A Wholeobinna12No ratings yet
- Post Operative HypotensionDocument7 pagesPost Operative HypotensionbbyesNo ratings yet
- Cardiac SurgeryDocument19 pagesCardiac SurgerySimon JosanNo ratings yet
- Medical Scenario 1Document42 pagesMedical Scenario 1murphy 1087No ratings yet
- Resuscitation and Shock: LSU Medical Student Clerkship, New Orleans, LADocument40 pagesResuscitation and Shock: LSU Medical Student Clerkship, New Orleans, LAFarazNo ratings yet
- Cardiogenic Shock 11Document2 pagesCardiogenic Shock 11Kemal TaufikNo ratings yet
- Ct7 Fluid, Electrolyte ImbalanceDocument9 pagesCt7 Fluid, Electrolyte ImbalanceAlondra VelascoNo ratings yet
- ShockDocument20 pagesShockعبدالواسع الاهنوميNo ratings yet
- Diagnosis and Treatment of Shock: Dr. Refli Hasan SPPD, SPJP (K) FihaDocument37 pagesDiagnosis and Treatment of Shock: Dr. Refli Hasan SPPD, SPJP (K) FihaWinson ChitraNo ratings yet
- Past Years SNQ Answer by RCSIDocument47 pagesPast Years SNQ Answer by RCSIhelamahjoubmounirdmo100% (1)
- Jurnal Kedokteran Dan Kesehatan IndonesiaDocument5 pagesJurnal Kedokteran Dan Kesehatan IndonesiaZulkarnain MuinNo ratings yet
- Abdominal Aortic Aneurysms-EditDocument32 pagesAbdominal Aortic Aneurysms-EditrandikaNo ratings yet
- SHOCK GUIDEDDocument70 pagesSHOCK GUIDEDrajevikramNo ratings yet
- CardioDocument9 pagesCardioVirgilio Reyes ManuelNo ratings yet
- AAAkateDocument5 pagesAAAkateprem kotiNo ratings yet
- Intensive Care For The Critically Ill Adult: T.SunilkumarDocument47 pagesIntensive Care For The Critically Ill Adult: T.SunilkumarYamini ChowdaryNo ratings yet
- CLASS 2 Low Cardiac Output Syndrome in Cardiac SurgeryDocument53 pagesCLASS 2 Low Cardiac Output Syndrome in Cardiac SurgeryjuanolivelloNo ratings yet
- Intra-Abdominal Hypertension GuideDocument40 pagesIntra-Abdominal Hypertension GuideBayu Surya Dana100% (1)
- Laproscopic SurgeryDocument80 pagesLaproscopic SurgeryAqeel AhmadNo ratings yet
- Massive Transfusion ProtocolsDocument12 pagesMassive Transfusion ProtocolsEhrli CuaresmaNo ratings yet
- Acute HFDocument36 pagesAcute HFeman roshdyNo ratings yet
- Management of Paediatric Shock - Fluids and InotropesDocument78 pagesManagement of Paediatric Shock - Fluids and InotropesRahmanu ReztaputraNo ratings yet
- ShockDocument2 pagesShockKemal TaufikNo ratings yet
- Unit II (B) Intra-Aortic Balloon Pump Counter PulsationDocument24 pagesUnit II (B) Intra-Aortic Balloon Pump Counter PulsationUmme HabibaNo ratings yet
- Renal Emergency RevisiDocument103 pagesRenal Emergency Revisidesy f sarahNo ratings yet
- Mrs. Bagent 1-9 BWAKANANG SHETDocument5 pagesMrs. Bagent 1-9 BWAKANANG SHETaaron tabernaNo ratings yet
- Local Weather ForecastingDocument37 pagesLocal Weather ForecastingSayarith GarcíaNo ratings yet
- Cabanatuan City's Contingency Plan for DisastersDocument89 pagesCabanatuan City's Contingency Plan for DisastersRamona FlowersNo ratings yet
- Common Mistakes in Drainage Submissions To PUB (BPU) : Muhammad Zahid Centralised Services Department (Building Plan Unit)Document51 pagesCommon Mistakes in Drainage Submissions To PUB (BPU) : Muhammad Zahid Centralised Services Department (Building Plan Unit)Freddie KooNo ratings yet
- Regional Boundaries MapDocument1 pageRegional Boundaries MapNgaire TaylorNo ratings yet
- NATIONAL INSTITUTE FOR RESEARCH, DEVELOPMENT AND TESTING IN ELECTRICAL ENGINEERINGDocument5 pagesNATIONAL INSTITUTE FOR RESEARCH, DEVELOPMENT AND TESTING IN ELECTRICAL ENGINEERINGAnne KelleyNo ratings yet
- A320 Memory ItemsDocument9 pagesA320 Memory ItemsTomas HezNo ratings yet
- Brief Note On Borak and Its TributriesDocument3 pagesBrief Note On Borak and Its TributriesNILRATAN SARKARNo ratings yet
- College of Agriculture, Forestry, and Environmental SciencesDocument6 pagesCollege of Agriculture, Forestry, and Environmental SciencesZeus CuiNo ratings yet
- B02 Placa Fría Frost TopDocument2 pagesB02 Placa Fría Frost TopOrlando VilladiegoNo ratings yet
- PresentationDocument15 pagesPresentationMicaella AragonNo ratings yet
- Fokker 50 Normal Checklist for Cockpit Safety InspectionDocument2 pagesFokker 50 Normal Checklist for Cockpit Safety InspectionMo All100% (4)
- Meteorology and Oceanography 1Document3 pagesMeteorology and Oceanography 1Antonino FioreNo ratings yet
- 10481-Osl-Xxge-En-Dat-0001 - 0 - Ifi - Meteorological Data For Akk ProjectDocument25 pages10481-Osl-Xxge-En-Dat-0001 - 0 - Ifi - Meteorological Data For Akk ProjectArunNo ratings yet
- Design of Buildings Windloads ProfHaefnerDocument9 pagesDesign of Buildings Windloads ProfHaefnerVianda KauriviNo ratings yet
- The World Factbook: O C e A N S:: Atlantic OceanDocument5 pagesThe World Factbook: O C e A N S:: Atlantic OceanWajahat GhafoorNo ratings yet
- Top Inactive Volcanoes in the PhilippinesDocument6 pagesTop Inactive Volcanoes in the PhilippinesChristian ParadoNo ratings yet
- Biotic and Abiotic FactorsDocument15 pagesBiotic and Abiotic Factorsapi-536437763No ratings yet
- Nav Composites 02-Flexture Concrete CompositesDocument29 pagesNav Composites 02-Flexture Concrete Compositesendah anggraeniNo ratings yet
- Daily log template and Clean Energy LLC substation daily log (January 1-2, 2021Document15 pagesDaily log template and Clean Energy LLC substation daily log (January 1-2, 2021OceanbnNo ratings yet
- Geography P1 Nov 2022 Eng PDFDocument20 pagesGeography P1 Nov 2022 Eng PDFSipho MthiNo ratings yet
- Toro WheelHorse 48" Plow Blade 79253Document20 pagesToro WheelHorse 48" Plow Blade 79253Kevins Small Engine and Tractor ServiceNo ratings yet
- Internet of Things (IoT) Solution For The Health Consequences Caused by Cremation in Modern IndiaDocument7 pagesInternet of Things (IoT) Solution For The Health Consequences Caused by Cremation in Modern IndiaIJRASETPublicationsNo ratings yet
- Micro Climate: Average High and Low TemperatureDocument9 pagesMicro Climate: Average High and Low Temperatureedward kenwayNo ratings yet
- How Jet Streams Affect Indian MonsoonDocument10 pagesHow Jet Streams Affect Indian MonsoonVikram DasNo ratings yet
- A2 Wordlist Unit 11Document4 pagesA2 Wordlist Unit 11pta26.hdNo ratings yet
- Entry Test Grade 8 2021Document3 pagesEntry Test Grade 8 2021Ардак АлламуратоваNo ratings yet
- The Trough-and-Ridge Diagram: Shorter ContributionDocument5 pagesThe Trough-and-Ridge Diagram: Shorter ContributionGonzalo RosadoNo ratings yet
- Transform Fault BoundaryDocument2 pagesTransform Fault BoundaryStef LibaoNo ratings yet
- Geog 213Document365 pagesGeog 213Fatima TwumasiNo ratings yet
- 1b) - 14 Environment (Protection) Fourth Amendment Rules, 2018Document6 pages1b) - 14 Environment (Protection) Fourth Amendment Rules, 2018Tarun KathpaliaNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (41)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)