Professional Documents
Culture Documents
The Joys, Challenges and Struggles of Community-Based Health Care Services?
Uploaded by
Bugs Benny0 ratings0% found this document useful (0 votes)
11 views2 pagesCommunity health focuses on the collective well-being of populations within a neighborhood or region that often share characteristics. Community health programs aim to improve access to preventive healthcare services, engage citizens in care decisions, and lower costs. However, providing community-based healthcare faces challenges due to social factors like uneven economic development and the divide between private and public services. Community health centers serve as primary care providers for underserved communities and address disparities by ensuring equitable access to resources. They form strong community bonds to identify local health needs and risks in order to empower residents and improve average lifespans.
Original Description:
Original Title
JOY
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCommunity health focuses on the collective well-being of populations within a neighborhood or region that often share characteristics. Community health programs aim to improve access to preventive healthcare services, engage citizens in care decisions, and lower costs. However, providing community-based healthcare faces challenges due to social factors like uneven economic development and the divide between private and public services. Community health centers serve as primary care providers for underserved communities and address disparities by ensuring equitable access to resources. They form strong community bonds to identify local health needs and risks in order to empower residents and improve average lifespans.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views2 pagesThe Joys, Challenges and Struggles of Community-Based Health Care Services?
Uploaded by
Bugs BennyCommunity health focuses on the collective well-being of populations within a neighborhood or region that often share characteristics. Community health programs aim to improve access to preventive healthcare services, engage citizens in care decisions, and lower costs. However, providing community-based healthcare faces challenges due to social factors like uneven economic development and the divide between private and public services. Community health centers serve as primary care providers for underserved communities and address disparities by ensuring equitable access to resources. They form strong community bonds to identify local health needs and risks in order to empower residents and improve average lifespans.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
The joys, challenges and struggles of community-based health care services?
Community health is the collective well-being of community members. In addition to living in
the same neighborhood or region, these populations often share health characteristics, ethnicities,
and socioeconomic conditions.
For instance, some low-income communities might experience high obesity rates due to limited
availability of nutritious foods in local grocery stores. This places them in an area commonly
known as a food desert.
In addition, a population might be exposed to contaminants from a nearby plant or waste facility.
Community health programs improve access to preventive health care services, engage citizens
in care decisions, and seek out lower medical costs.
Social contradictions, including uneven economic development and the private-public duality,
make community-based provision of health care difficult. The unrestricted expansion of private
medical centers has been criticized from several perspectives including inadequate coordination
of services, high costs, and negative effects on urban housing and living conditions. Corporate
and professional control over health policy, monopolization, and public subsidization foster
expansion of private institutions. While private facilities enlarge, public health-care institutions
deteriorate, close, or shift to private management. Many clients eligible for care at public
hospitals do not receive adequate attention in the private sector. Despite their achievements,
community clinics have problems that threaten their survival. The financial insecurity of
community clinics is an inherent feature of the private-public duality that affects the entire
health-care system. Community clinics and public hospitals offer a potential for broader
organizing and empowerment.
The public health worker’s goal in community-focused care is to enhance healthcare services and
patient outcomes in targeted populations. By applying public health theory on a local,
personalized level, community health providers can cater services to a specific demographic and
bring a sense of wellness to communities that would otherwise lack proper access to care.
Community health programs address disparities by ensuring equitable access to health resources.
Such disparities include living in an isolated rural area with limited healthcare providers or being
unable to afford health insurance. Community health centers often serve as the primary care
provider in communities where health equity is limited by socioeconomic factors.
Those seeking to apply public health principles to address a local population’s needs must
understand the area’s unique characteristics. This allows them to interact dynamically with
community members and create a lasting positive impact on the population.
The goal of a community health provider is to offer comprehensive services that grant
communities direct and immediate access to essential resources, including medical, dental,
pharmacy, and mental health care. By educating area residents on what resources are available
and giving them the tools to access care, public health workers empower people to take control
of their own health.
Community public health initiatives focus on identifying specific geographic areas with high
levels of need and helping those communities overcome barriers to living healthier lives.
Community members’ average lifespans can differ by 20 to 30 years based on inequities that
restrict access to healthy food, affordable health care, and mental health support.
Community health professionals form strong bonds with citizens, as well as area health care and
social services providers. This enables them to complete essential tasks, such as uncovering
regional health risks, educating local residents on healthy behaviors, or establishing community
health resources to close gaps in care.
You might also like
- Community HealthDocument19 pagesCommunity Healthjoydanay07No ratings yet
- Hvchap10 PDFDocument15 pagesHvchap10 PDFswarnaNo ratings yet
- Public HealthDocument13 pagesPublic HealthNimra JamilNo ratings yet
- The Role of Public Health NursesDocument16 pagesThe Role of Public Health NursesCarl Chariven A. PaguyoNo ratings yet
- Expository Essay - CHNDocument2 pagesExpository Essay - CHNRogerQuxNo ratings yet
- Functions of The Community in Healthcare ProvisionDocument1 pageFunctions of The Community in Healthcare ProvisioniscahaumaNo ratings yet
- Challenges and Difficulties With Community HealthDocument3 pagesChallenges and Difficulties With Community HealthGame GamerNo ratings yet
- Health Disparities in United StatesDocument7 pagesHealth Disparities in United Stateslagatduncan520No ratings yet
- Introduction To Healthcare InequalityDocument9 pagesIntroduction To Healthcare Inequalitysheniabishun76No ratings yet
- 1541147225agere HealthDocument9 pages1541147225agere HealthREJOICE STEPHANIE DZVUKUMANJANo ratings yet
- Describe Your Own Community Using Picture/sDocument4 pagesDescribe Your Own Community Using Picture/sKyla TuazonNo ratings yet
- Community Health CareersDocument3 pagesCommunity Health CareersReina NishiyamaNo ratings yet
- Karn Article OrganizedDocument7 pagesKarn Article OrganizedRakshitha HMNo ratings yet
- Community Refers To The People of A District or Country Considered Collectively, Especially in TheDocument17 pagesCommunity Refers To The People of A District or Country Considered Collectively, Especially in TheFranz Simeon ChengNo ratings yet
- The Community Health Centre Model of Care: A Statement of PrinciplesDocument2 pagesThe Community Health Centre Model of Care: A Statement of Principlesummaid singhNo ratings yet
- Sharrone Azzel Jussil Week 1 Assignment SEJ2121001: What Is Community Nursing?Document3 pagesSharrone Azzel Jussil Week 1 Assignment SEJ2121001: What Is Community Nursing?arasoNo ratings yet
- Topic 5. Poverty and Health - XEA 406Document5 pagesTopic 5. Poverty and Health - XEA 406Anita BoboNo ratings yet
- Questions and Answers From The Webinar Community Health Workers: Their Role in Preventing and Controlling Chronic ConditionsDocument13 pagesQuestions and Answers From The Webinar Community Health Workers: Their Role in Preventing and Controlling Chronic ConditionsGift EseNo ratings yet
- Providin G Health Care: Group 1Document14 pagesProvidin G Health Care: Group 1Kopi MopiNo ratings yet
- LasellmDocument9 pagesLasellmapi-296534570No ratings yet
- SAMPLE SDGsDocument2 pagesSAMPLE SDGsHammas Ahmed SiddiquiNo ratings yet
- The Community Health Policy OverviewDocument8 pagesThe Community Health Policy OverviewGalakpai KolubahNo ratings yet
- Difference Between Community Health Nurse and A Public Health NurseDocument1 pageDifference Between Community Health Nurse and A Public Health NurseKim Angelo ReyesNo ratings yet
- No 4Document1 pageNo 4georgechris12eNo ratings yet
- Community Oriented Primary Care: Meaning and Scope: General ConsiderationsDocument33 pagesCommunity Oriented Primary Care: Meaning and Scope: General ConsiderationsShams JailaniNo ratings yet
- CHN 104Document1 pageCHN 104May MayNo ratings yet
- Community Strategy New ContentDocument23 pagesCommunity Strategy New ContentPhilip MutuaNo ratings yet
- The Role of Government As An Institution of Health Care DeliveryDocument7 pagesThe Role of Government As An Institution of Health Care DeliveryZechariah NicholasNo ratings yet
- Research (Community Health Center)Document19 pagesResearch (Community Health Center)Luego, Brent Jarryd P.No ratings yet
- 001 - EN Unit 4 Demographic Inequalities in Health SSDocument3 pages001 - EN Unit 4 Demographic Inequalities in Health SSRicardo DomingosNo ratings yet
- EssayDocument6 pagesEssayAnkit BhattraiNo ratings yet
- Enhancing Accessibility of Sustainable Healthcare in Rural AreasDocument7 pagesEnhancing Accessibility of Sustainable Healthcare in Rural AreasSusmita SenNo ratings yet
- What Is The Role of Medical Services On The Implementation of Different Interventions For People With Disabilities?Document2 pagesWhat Is The Role of Medical Services On The Implementation of Different Interventions For People With Disabilities?Õbsëqúiœus Menam MikreNo ratings yet
- Primary Health CareDocument15 pagesPrimary Health Carekinid100% (1)
- Community DiagnosisDocument3 pagesCommunity DiagnosisWayne GretzkyNo ratings yet
- Community As Client: Applying The Nursing Process: Prepared By: DR - Soad AlnassryDocument42 pagesCommunity As Client: Applying The Nursing Process: Prepared By: DR - Soad AlnassryAmnah AbudayahNo ratings yet
- The Impact of Protected Characteristics On Patient Care in Healthcare SettingsDocument2 pagesThe Impact of Protected Characteristics On Patient Care in Healthcare Settingsfareehakanwar93No ratings yet
- Task Analysis: Roles and Tasks of BHW/CHWDocument30 pagesTask Analysis: Roles and Tasks of BHW/CHWdanielNo ratings yet
- RRL-Community Health Nursing, Community, MalnutritionDocument5 pagesRRL-Community Health Nursing, Community, MalnutritionAndee SalegonNo ratings yet
- Lab Community Health Nursing Nur 193Document6 pagesLab Community Health Nursing Nur 193Bryan Lloyd Ballestar RayatNo ratings yet
- Healthcare EssayDocument1 pageHealthcare EssayHITNo ratings yet
- CHN ActivityDocument1 pageCHN ActivityMaxine RicafortNo ratings yet
- Health Care System SendDocument113 pagesHealth Care System SendAsma AsriNo ratings yet
- 2 Community Healtyh Nursing - Field in NursingDocument12 pages2 Community Healtyh Nursing - Field in NursingsannsannNo ratings yet
- Assign 1Document2 pagesAssign 1lydiacherotich7496No ratings yet
- Nikhil R - E190Document13 pagesNikhil R - E190jacacomarketingNo ratings yet
- Community ConnectDocument10 pagesCommunity ConnectAkash MauryaNo ratings yet
- ArticleDocument5 pagesArticleAnnie AsgharNo ratings yet
- Primary Health CareDocument14 pagesPrimary Health CareAprille SgrrNo ratings yet
- Social Factor and Illness-1Document36 pagesSocial Factor and Illness-1Asad AnZari0% (1)
- Community Nursing and Care Continuity LEARNING OUTCOMES After CompletingDocument23 pagesCommunity Nursing and Care Continuity LEARNING OUTCOMES After Completingtwy113100% (1)
- What Is The Role of Medical Sociology in Our Day To Day LifeDocument5 pagesWhat Is The Role of Medical Sociology in Our Day To Day Lifedanyalkhattak739No ratings yet
- Community PharmacyDocument9 pagesCommunity PharmacyShowmic Ahmed50% (2)
- Community Health WorkersDocument11 pagesCommunity Health WorkersAneesh Ramachandran PillaiNo ratings yet
- Health Disparities and Health Education-1finalDocument13 pagesHealth Disparities and Health Education-1finalbrendahronoh254No ratings yet
- Universal Health Coverage With EquityDocument2 pagesUniversal Health Coverage With EquityBryan GarmaNo ratings yet
- Article CHNDocument2 pagesArticle CHNIanMayNo ratings yet
- Relevance of Sociology To HealthcareDocument9 pagesRelevance of Sociology To HealthcareMaría RecioNo ratings yet
- Risk Assessment MethodologiesDocument2 pagesRisk Assessment MethodologiesBugs BennyNo ratings yet
- Epidemiology - The Natural History of DiseaseDocument37 pagesEpidemiology - The Natural History of DiseaseBugs BennyNo ratings yet
- Dynamics of Disease TransmissionDocument29 pagesDynamics of Disease TransmissionBugs BennyNo ratings yet
- Community-Based Health Care ServiceDocument14 pagesCommunity-Based Health Care ServiceBugs BennyNo ratings yet
- Reflections On Self Compassion Exercise PDFDocument3 pagesReflections On Self Compassion Exercise PDFNash PanimbangNo ratings yet
- Daftar Obat Mengandung PrekursorxlsDocument22 pagesDaftar Obat Mengandung PrekursorxlswawanNo ratings yet
- Finding Love After Heartbreak EbookDocument201 pagesFinding Love After Heartbreak EbookNancy Sarakikya100% (3)
- Resolution 2017Document2 pagesResolution 2017Thess Tecla Zerauc Azodnem90% (21)
- List of Prohibited and Hazardous ChemicalDocument40 pagesList of Prohibited and Hazardous ChemicalKee SarakarnkosolNo ratings yet
- What Do Unions Do - Freeman & MedoffDocument18 pagesWhat Do Unions Do - Freeman & MedoffrshnjsphNo ratings yet
- Gastrointestinal and HepatobiliaryDocument54 pagesGastrointestinal and Hepatobiliaryjeshema100% (2)
- Healthcare Technology & Distribution JPMDocument41 pagesHealthcare Technology & Distribution JPMRonit MirchandaniNo ratings yet
- Human Body - A Visual Encyclopedia - Brown, Morgan, Walker, Woodward (DK Publishing 2012 9780756693077 Eng) PDFDocument258 pagesHuman Body - A Visual Encyclopedia - Brown, Morgan, Walker, Woodward (DK Publishing 2012 9780756693077 Eng) PDFchbenengeli94% (17)
- Doctors AreDocument2 pagesDoctors Areanon_703664359No ratings yet
- HR in ConstructionDocument34 pagesHR in ConstructionJeet Pawar0% (1)
- Dyslexia and Dentistry: FeatureDocument3 pagesDyslexia and Dentistry: FeatureDr.Nay AungNo ratings yet
- Food TerrorismDocument2 pagesFood TerrorismEditor IJTSRDNo ratings yet
- Minkler - Personal Responsibility For HealthDocument22 pagesMinkler - Personal Responsibility For HealthColesniuc Adina100% (1)
- Gastric LavageDocument19 pagesGastric LavageAnita Santiago Soguilon100% (1)
- Green Horn - Volume 31, Edition 4Document24 pagesGreen Horn - Volume 31, Edition 4Springfield VT NewsNo ratings yet
- Capstone Research Final Manuscript Group4 Baetiong 2Document31 pagesCapstone Research Final Manuscript Group4 Baetiong 2sabrinacabridoNo ratings yet
- Heartstopper Volume 4Document3 pagesHeartstopper Volume 4Hope SooNo ratings yet
- Manual de Terapia Interpersonal AdolescentesDocument76 pagesManual de Terapia Interpersonal Adolescentesjanine claudia olivera bejarNo ratings yet
- Gingipain Periodontitis DogDocument5 pagesGingipain Periodontitis Dogvioleta.enachescu-1No ratings yet
- UT Dallas Syllabus For nsc3361.001.08f Taught by Van Miller (vxm077000)Document5 pagesUT Dallas Syllabus For nsc3361.001.08f Taught by Van Miller (vxm077000)UT Dallas Provost's Technology GroupNo ratings yet
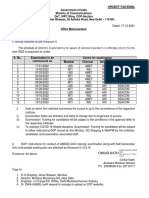
- GMDSS Exam Schedule For Year 2022Document7 pagesGMDSS Exam Schedule For Year 2022Mani ThapaNo ratings yet
- Cisco Healthcare SolutionsDocument4 pagesCisco Healthcare SolutionsHassan AlsafiNo ratings yet
- Peptic UlcerDocument5 pagesPeptic UlcerKomal KhanNo ratings yet
- Basic Life SupportDocument28 pagesBasic Life SupportMaesaNo ratings yet
- Formical-B, Force D, Folamil, PamorelinDocument18 pagesFormical-B, Force D, Folamil, PamorelinKevin SNo ratings yet
- Ancel Keys - Atherosclerosis: A Problem in Newer Public HealthDocument22 pagesAncel Keys - Atherosclerosis: A Problem in Newer Public Healthacolpo100% (1)
- Correcting Mold MisinformationDocument8 pagesCorrecting Mold MisinformationhazmatlinkNo ratings yet
- Salvia For Dementia Therapy: Review of Pharmacological Activity and Pilot Tolerability Clinical TrialDocument9 pagesSalvia For Dementia Therapy: Review of Pharmacological Activity and Pilot Tolerability Clinical TrialAleksa LukicNo ratings yet
- Generic HACCP Model For Poultry Slaughter: United States Department of AgricultureDocument45 pagesGeneric HACCP Model For Poultry Slaughter: United States Department of AgricultureLayxi KieuNo ratings yet