Professional Documents
Culture Documents
Year Ii Pharmacology Drugs List
Uploaded by
saifuddinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Year Ii Pharmacology Drugs List
Uploaded by
saifuddinCopyright:
Available Formats
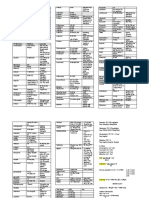
FUNDAMENTAL: ANTI-INFLAMMATORY DRUGS
Class Drug Example MOA Uses Side Effect Contraindication
Steroid - Glucocorticoid Glucocorticoid Replacement therapy Cushing syndrome - PU
- Corticosteroid 1. Inhibit leukocyte infiltrate - acute adrenal insufficiency - Round face - DM
- Prednisolone 2. Interfere with mediators of - chronic adrenal insufficiency - Buffalo hump - HTN
- Hydrocortisone inflammatory response (Addison’s disease) - Truncal obesity - TB
- Dexamethasone 3. Suppress humoral immunity - Congenital adrenal hyperplasia - Thin limbs - HSV keratitis
- Betamethasone - CHF renal failure
- Triamcinolone Corticosteroid Pharmacotherapy Others - Viral & fungal infections
- Methylprednisolone 1. Stimulate lipocortins & prevent - RA & Osteoarthritis - Fragile skin, purple striae, - Osteoporosis
synthesis of inflammatory mediators - Rheumatic fever easy bruising, hirsutism - Psychosis
2. Inhibit phospholipase A2 inhibitory - Gout - Hyperglycemia - Seizures
proteins - Hypersensitivity - Muscle weakness
3. Interfere with leukocyte infiltration - Autoimmune - Delayed wound healing
4. Inhibit release of arachidonic acid from - Asthma - Peptic ulceration, bleeding,
phospholipids - Collagen: SLE, Polyarthritis perforation
5. Reducing formation of PG nodosa, Nephrotic syndrome, - Osteoporosis
Glomerulonephritis - GC save - Cataract, glaucoma
Prednisolone life - Growth retardation
1. Limiting vascular capillary dilatation & - Eye: conjunctivitis, keratitis, - Suppression HP-adrenal
permeability retinitis axis: malaise, fever, anorexia,
2. Restrict accumulation of PMNL & - Skin: eczema, dermatitis, nausea, weakness
macrophages. Steven Johnson Syndrome GC
3. Reduce release of vasoactive kinins. save life
4. Reduce inflammatory reactions - Intestinal: UC, CD
Class Drug Example MOA Uses Side Effect Contraindication
NSAIDS - Aspirin (antiplatelet) 1. Inhibit cyclooxygenase enzyme (Cox1 - Osteoarthritis - Dyspepsia - Irritable bowel
(Nonselective) - Ibuprofen & Cox2) - Rheumatoid arthritis - Gastric ulceration/bleeding syndrome
- Ketoprofen 2. Prevent synthesis of prostaglandins - Tennis elbow - Diarrhea - Elderly with GI
- Naproxen and thromboxane. - Headache - Oedema problems
- Meloxicam 3. Reduce inflammation and pain - Migraine - Hypertension - PU (stomach bleeding)
- Acute gout - Nephrotoxicity - Kidney disease
NSAIDS - Celecoxib 1. Inhibit cyclooxygenase enzyme (Cox2) - Dysmenorrhea - Photosensitivity - IBF (CD & UC)
(COX2 - Rofecoxib 2. Prevent synthesis of prostaglandins - Postoperative pain - Risk stroke & MI (except - Transient ischaemic
Inhibitors) - Etoricoxib and thromboxane. - Muscle stiffness (PD) aspirin) attack (except aspirin)
3. Reduce inflammation and pain - Stroke (except aspirin)
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
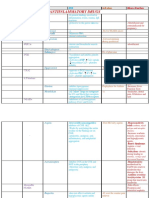
FUNDAMENTAL: ANTIHISTAMINE & PROSTAGLANDINS
Class Drug Example MOA Uses Side Effect Contraindication
H1 Receptor 1st Generation
Antagonist Antihistamine
- Meclizine
- Hydroxyzine
- Doxylamine H1 receptor antagonist
- Promethazine - Sedation
1. Inhibits histamine action at the receptor
- Clemastine - Allergic - Drowsiness
2. Competes with histamine for binding
- Dimenhydrinate - Insect bite & ivy poisoning - Dry mouth
3. Displace histamine from receptor - Glaucoma
- Diphenhydramine - Antipruritic agent - Blur vision
- Peptic ulcer
- Block runny nose - Light headedness
H1 receptor antagonist - Hypertension
2nd Generation - Preanesthetic medication - Motor incoordination
- Inhibit increased vascular permeability - Bronchial asthma
Antihistamine - Cough suppressant - Urinary hesitancy
- Inhibit allergy bronchoconstriction - COPD
- Loratadine - Labyrinth suppressant (vertigo) - Fatigue and sedation
- Cetirizine - Antihistaminic, anticholinergic, - Alteration bowel movement
H2 receptor antagonist
- Azelastine antiemetic - Diminished alertness and
- Reduce gastric acid production
- Desloratadine concentration
H2 Receptors - Cimetidine
Antagonist - Ranitidine
- Famotidine
Class Drug Example MOA Uses Side Effect Contraindication
Prostaglandins - Misoprostol 1. PG bind to PG receptors (GPCR) - Terminate pregnancy - Hypotension - NSAIDS
- Enoprostil 2. G-Protein Couple Receptors stimulate - Facilitating of labour - Bronchoconstriction - Corticosteroid inhibit
- Dinoprost inositol triphosphate (IP3) and c-AMP - Peptic ulcer: increase mucous - Vomiting and diarrhea Phospholipase A2
- Carboprost pathway production and mucosal BF - Fever and dizziness - Analogues PGE1,
- Beraprost 3. Inhibition of adenyl cyclase via G1 - Prevent platelet aggregation - Flushing PGF2α, PGI2
- Bimatoprost activation - Treat pulmonary hypertension
- Dinoprostone 4. Ca2+ mobilization from G1 leading to: - Treat glaucoma
- Unoprostone vasodilation, reduce BP, reduce acid - Enhance penile erection
secretion, bronchodilation, natriuresis, - Teat bronchial asthma
uterine contraction, increase peristalsis,
increase sensitivity to pain
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
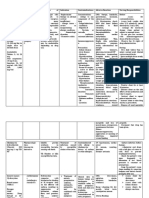
FUNDAMENTAL: ANTIMICROBIAL AGENT
Class Drug Example MOA Uses Side Effect Contraindication
Penicillins Broad Spectrum - Gram +ve aerobes - N&V - Hypersensitivity
- Ampicillin - Gram –ve aerobes - Pruritus - Steven Johnson
- Amoxicillin - Spirochetes - Headache syndrome
- Anaerobe - Leukopenia - Pregnancy and lactation
Narrow Spectrum - Branching gram -ve mother
- Penicillin G
- Penicillin V
- Procaine
- Benzathine
Beta Lactams
- Nafcilin
Class Drug Example Uses Side Effect Contraindication
Cephalosporin 1st Generation - Gram +ve cocci - Hypersensitivity - Hypersensitivity
- Cephalexin - Enterobacteria - GI distress - Premature neonates
1. Bind to penicillin binding protein (PBP)
- Cefazolin - Gram –ve (beta lactam - Pancreatitis - Jaundice (full term
2. Inhibit final transpeptidation.
- Cefadroxil resistance, pseudomonas) - Headache & dizziness neonates)
3. Interfere synthesis of peptidoglycan in
- Methicillin Resistance - Candidal vaginitis
cell wall
2nd Generation Staphylococcus aureus (MRSA) - Rash and flushing
4. Lead to bacterial lysis and death
- Cefuroxime
- Cefprozil
- Cefaclor
3rd Generation
- Ceftriaxone
- Cefixime
- Cefoperazone
4th Generation
- Cefepime
- Cefpirome
5th Generation
- Ceftaroline
- Ceftolazone
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
FUNDAMENTAL: ANTIMICROBIAL AGENT
Class Drug Example MOA Uses Side Effect Contraindication
Carbapenems - Meropenem 1. Bind to penicillin binding protein (PBP) - Broad spectrum (beta lactam - N&V - Hypersensitivity
- Emipenem 2. Inhibit bacterial cell wall synthesis resistance) - Seizures - History of anaphylactic
- Ertapenem 3. Lead to cell wall assembly stop - Gram +ve cocci - Headache reaction
- Doripenem 4. Eventually bacterial cell lysis - Gram –ve bacilli - GI distress
- Anaerobes
Class Drug Example MOA Uses Side Effect Contraindication
Monobactams - Aztreonam 1. Bind to PBP-3 - Against gram –ve bacilli - GI distress Hypersensitivity
2. Inhibit bacterial cell wall synthesis - Intrinsic beta lactamase - Headache
3. Lead to cell wall assembly stop resistance - Vertigo
4. Eventually bacterial cell lysis
5. Highly resistant to hydrolysis by narrow
beta lactamase
Class Drug Example MOA Uses Side Effect Contraindication
Glycopeptide - Vancomycin 1. Bind to D-alanyl-D-alanine of cell wall - Multi drug resistance organism - Nephrotoxicity - Hypersensitivity
- Telavancin precursor - Broad spectrum coverage - Red man syndrome
- Dalbavancin 2. Block glycopeptide polymerisation - Against gram +ve bacteria - Anaphylactic reaction
- Oritavancin 3. Lead to inhibition of cell wall synthesis - MRSA
- Teicoplanin 4. Impairs bacterial cell membrane
permeability
5. Impairs bacterial RNA synthesis
Class Drug Example MOA Uses Side Effect Contraindication
Aminoglycoside - Gentamycin - Severe gram –ve bacilli - N&V - Hypersensitivity
(30S subunit) - Streptomycin infections - Anaemia
- Amikacin - Tuberculosis (TB) - Convulsion
1. Bind to 30S ribosomal subunit - Nephrotoxicity
2. Prevent binding of aminoacyl transfer
Class Drug Example RNA Uses Side Effect Contraindication
Tetracycline - Tetracycline 3. Inhibiting protein synthesis - Atypical bacteria: - GI distress - Hypersensitivity
(30S subunit) - Doxycycline 4. Arresting cell growth mycoplasma, rickettsia, - Photosensitivity
- Minocycline anaplasma, chlamydia, - Deposition in developing
ureaplasma, vibrio cholera bone and teeth
- Superinfection
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
FUNDAMENTAL: ANTIMICROBIAL AGENT
Class Drug Example MOA Uses Side Effect Contraindication
Macrolide - Azithromycin - Atypical pneumonia - Increase intestinal motility - Hypersensitivity
(50S subunit) - Erythromycin - URTI - Acute cholestatic hepatitis
- Clarithromycin - Chlamydia - Eosinophilia
- Gram +ve cocci - Rash
- Neisseria
1. Bind to 50S ribosomal subunit
2. Result in blockage of transpeptidation
Class Drug Example Uses Side Effect Contraindication
3. Therefore preventing peptide bond
Lincosamide - Clindamycin - Anaerobes bacteria - GI distress - Hypersensitivity
formation, ribosome assembly and
(50S subunit) - Lincomycin - Aspiration pneumonia - Clostridium difficile colitis
translation process
- Lung abscess
4. Inhibit protein synthesis
Class Drug Example Uses Side Effect Contraindication
Chloramphenicol - Chloramphenicol - Rickettsia - Dose related anaemia - Hypersensitivity
(50S subunit) - Meningitis due to - Grey baby syndrome
Haemophilus influenzae, - Anaplastic anaemia
Neisseria meningitides,
Streptococcus pneumoniae
Class Drug Example MOA Uses Side Effect Contraindication
Fluoroquinolones - Ciprofloxacin - Gram –ve bacilli in UTI and GI - Seizures - Hypersensitivity
- Levofloxacin infection - Tendinitis
- Gemifloxacin - Genital pathogen - GI distress
1. Inhibits DNA gyrase and
- Enofloxacin - Pseudomonas - Jaundice
topoisomerase
- Pneumonia
2. Interfere with bacterial DNA
- Penicillin resistance
replication, transcription, repair and
- Pneumococci
recombination
3. Thereby inhibit relaxation of
Class Drug Example Uses Side Effect Contraindication
supercoiled DNA
Quinolones - Nalidixic acid - Uncomplicated lower UTI - Nausea and vomiting - Hypersensitivity
4. Lead to breakage of bacterial DNA
- Shigellosis - allergic rash
strand
- Dizziness or vertigo
- Muscular weakness
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
FUNDAMENTAL: ANTIMICROBIAL AGENT
Class Drug Example MOA Uses Side Effect Contraindication
Sulphonamides - Sulfisoxazole 1. Interfere with synthesis of nucleic - Gram +ve bacteria - GI distress - Hypersensitivity
- Sulfamethoxazole acid - Gram –ve bacteria - Acute haemolysis in G6PD - Renal or hepatic
2. Blocking the conversion of P- - Simple UTI - Crystaluria impairment
aminobenzoic acid (PABA) to - Nocardia - Aplastic anaemia - Blood disorders
dihydrofolic acid - Toxoplasmosis - Nephrotoxicity - Porphyria
3. Give bacteriostatic action - Malaria - Pre-hepatic jaundice - SLE
4. Can be bactericidal when low
thymine concentration
Class Drug Example MOA Uses Side Effect Contraindication
Rifamycins - Rifampicin 1. Inhibit bacterial RNA synthesis - Mycobacterium tuberculosis - N&V - Hypersensitivity
(antimycobacterials) - Rifabutin 2. Bind to beta subunit of DNA- - Leprosy - Rash
dependent RNA polymerase - Haemophilus influenzae B - Pruritus
3. Prevent the elongation of RNA - Meningococcal prophylaxis - Hepatitis
4. Lead to bactericidal
Class Drug Example MOA Uses Side Effect Contraindication
DHFR (Dihydrofolate - Trimethoprim 1. Inhibit Dihydrofolate reductase - Recurring UTI - Rash - Hypersensitivity
Reductase) Inhibitors - Pyrimethamine 2. Prevent conversion of dihydrofolate - Respiratory infections - Headache and fever - Megaloblastic anaemia
to tetrahydrofolate - Ear and sinus infections - Bone marrow suppression
3. Interfere synthesis of bacterial - Shigella - Hyperkalaemia
nucleic acid and protein - Salmonella - GI disturbance
4. Lead to bacteriostatic or bactericidal
Class Drug Example MOA Uses Side Effect Contraindication
Nitroimidazoles - Metronidazole - Bacterial vaginosis - Dizziness and headache - Hypersensitivity
- Tinidazole - Trichomoniasis and giardiasis - Peripheral neuropathy - Pregnant and lactation
1. Inhibits bacterial protein synthesis
- Acute necrotising ulcerative - Sensory disturbance mother
2. Interact with bacterial DNA
gingivitis - Abdominal pain
3. Loss of DNA helical structure
- Eradicate helicobacter pylori - Anorexia
4. Breakage of DNA strand
associate PUD - Dark urine
5. Lead to bacterial cell death
- Intestinal and hepatic
amoebiasis
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
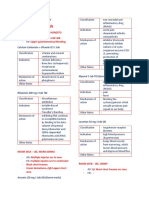
FUNDAMENTAL: ANTICANCER AND CHEMOTHERPAY
Goal of cancer treatment? Management of toxicities?
1. Curative, total eradicate of cancer cells 1. Nausea and vomiting – 5HT Antagonist (Ondansetron)
2. Palliative, reduce of symptoms (QOL) 2. Cancer cachexia – Glucocorticoid
3. Adjuvant, reduce chance of recurring 3. Hyperuricemia – Allopurinol
4. Neo-adjuvant, given before surgery to shrink the tumour 4. Hypercalcemia – Alendronate (Bisphosphonate)
5. Bone marrow suppression – Filgrastim or Sargramostim
Combination chemotherapy?
1. Suppression of drug resistance Steroid in cancer treatment?
2. Increased killing of cancer cells 1. Anti-inflammatory
3. Reduced injury to normal cells (no overlapping toxicities) 2. Increase appetite
3. Produce euphoria
General adverse effect of anti-cancer? 4. Increase body weight
1. Bone marrow – leukopenia, thrombocytopenia, anaemia 5. Prevent hypersensitivity reactions
2. GI tract – oral or intestinal ulceration, diarrhea 6. Treatment of hypercalcemia
3. Hair follicle – Alopecia (hair loss) 7. Increase antiemetic (anti-vomiting) effect
4. Gonads – menstrual irregularities, premature menarche, impaired spermatogenesis
5. Wound – impaired wound healing
6. Fetus – Teratogenesis (especially during first trimester)
Class Drug Example MOA Uses Side Effect
Alkylating agents 1. Alkylating agents (carbonium ions) - Lung cancer - Nausea and vomiting
- Cisplatin attack nucleophilic on guanine base. - Ovarian cancer - Nephrotoxicity
- Carboplatin 2. Result in cross linking, abnormal base - Breast cancer - Neurotoxicity
pairing, and cutting of DNA strands - Numbness, tingling and burning
3. Block replication and transcription of sensation
tumour cells - Bone marrow suppression
CCNS (Cell Anthracycline 1. Intercalate between base pairs - ABVD regimen - N&V
Cycle Non- - Doxorubicin 2. Inhibit topoisomerase II - Hodgkin’s lymphoma - Alopecia
Specific) Agents - Epirubicin 3. Generate free radicals - Headache
4. Block DNA and RNA synthesis - BM suppression
5. Cause cutting of strands
Antibiotics
- D-actinomycin
- Mitomycin
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
FUNDAMENTAL: ANTICANCER AND CHEMOTHERPAY
Class Drug Example MOA Uses Side Effect
1. MTX is Folic acid analog that bind with - Breast cancer - Nausea and vomiting
DHFR enzyme - Epidermoid cancer - Hepatotoxicity
2. Interfere with synthesis of tetrahydrofolate - Lung cancer - Kidney failure
3. Interfere with enzymatic processes - Advance stage Non-Hodgkin’s Lymphoma - Folic acid deficiency
4. Inhibit formation of DNA, RNA and key (NHL) - BM suppression
Antimetabolites (S phase) cellular protein during S phase
- Methotrexate 5. Stopping cancer cells
- Fluorouracil
- Fludarabine 1. Fluorouracil is thymidylate synthase inhibitor - Metastatic carcinoma of breast and GI - Nausea and vomiting
2. Block synthesis of pyrimidine thymidine - Carcinoma of ovary, cervix, urinary bladder, - Mucositis
3. Interfere with DNA replication prostate, and pancreas - Diarrhea
4. Lead to shortage of dTMP - oropharyngeal cancer - Hand and foot syndrome
5. Rapidly dividing cancerous cells undergo - Alopecia (hair loss)
thymine-less death - Hyperpigmentation
CCS (Cell Cycle Taxanes (M phase) 1. Interfere with mitotic spindle - Ovarian cancer - N&V
Specific) Agents - Paclitaxel 2.Prevent conversion of microtubule polymer - Breast cancer - Myalgia
- Docetaxel into tubulin monomers (M phase) - NSCLC - Headache
- Ixabelipone 3. Stabilising existing microtubules - Bladder cancer - BM suppression
4. Inhibit their disassembly - Prostate cancer
5. Interfere with G2 mitotic phase - Oesophageal cancer
6. Inhibit tumour cell replication and supresses
cell proliferation
Vinca alkaloids (M phase)
- Vinblastine - GI upset
- ABVD regimen
- Vincristine 1. Block the formation of mitotic spindle - Alopecia
- Hodgkin’s Lymphoma
2. Preventing the assembly of tubulin dimers - Leukopenia
- Non small cell lung cancer (NSCLC)
Podophyllotoxin (G-S phase) into microtubule - Thrombocytopenia
- Bladder cancer
- Etoposide 3. Block polymerization of tumour cell - Sweating
- Testicular cancer
- Teniposide - Muscle cramps
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
FUNDAMENTAL: DRUGS ACTING ON SYMPATHETIC SYSTEM
Sympathomimetic Sympatholytic
Increase insufficient response Reduce sympathetic activity
Stimulatory action Inhibitory action
Agonist Antagonist
SYMPATHOMIMETIC AGENT
Classification of Sympathomimetic Agonist
Direct Acting Indirect Acting
Alpha Agonist Beta Agonist Releasers (amphetamine) Reuptake Inhibitor (cocaine)
- Nonselective (norepinephrine) - Nonselective (isoproterenol)
- Alpha1 selective (phenylephrine) - Beta1 selective (dobutamine)
- Alpha2 (clonidine) - Beta2 selective (albuterol)
Pharmacological actions of catecholamine?
1. All α stimulation except on the GIT
2. All β inhibit except on the heart
Adrenergic Receptors
α1 α2 β1 β2
- Vasoconstriction - Inhibition of norepinephrine release - Tachycardia - Vasodilation
- Increased peripheral resistance - Inhibition of acetylcholine release - Increased lipolysis - Bronchodilation
- Increased blood pressure - Inhibition of insulin release - Increased myocardial contractility - Increased glucose release
- Mydriasis (dilatation of pupil) - Increased release of renin - Relaxed uterine smooth muscle
- Increase closured internal sphincter of - Increased muscle and liver
the bladder glycogenolysis
- Slightly increase peripheral resistance
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
CORRELATION PA, USES AND SE OF EPINEPHRINE
Drugs Site of Action Pharmacological Action Uses Side Effect
Heart - Stimulate at β1 receptor - Cardiac arrest (normal heart) - Ventricular arrhythmias
- Increase HR & FOC - e.g. electric short and drowning - Palpitation, hypertension
- Increase SBP - Cerebral haemorrhage
Blood vessel - Stimulate α1 receptor - Alleviate pulmonary congestion - Tissue necrosis
- Skin and splanchnic VC - Reduce bleeding from small vessel - Severe hypertension
- e.g. tooth extraction - Cerebral haemorrhage
- Ischemia and gangrene
Blood pressure - Increase SBP and CO (β1 receptor) - Shock to increase tissue perfusion - Transient hypertension
- Reduce DBP and PR (β2 receptor) - Except cardiogenic shock - Cerebral haemorrhage
- First choice of anaphylactic shock
Bronchial muscle - Strong β2 agonist - Bronchial asthma - Irritation and coughing
- Dilate bronchioles - Dry mouth and throat
- Headache and flushing
Epinephrine Eye - Stimulate α1 receptor - Induced mydriasis - Glaucoma
- Dilatation of radial muscle of iris - Conjunctiva decongestion
Physiological - Increase BP (α1) - Anaphylactic shock
antagonist - Stimulate HR (β1) - Relieve bronchospasm
histamine - Bronchi dilatation (β2) - Angioedema and mucosa swelling
- Inhibit histamine and SRS-A release from mast cell - Insect sting or allergen
Metabolic effect - Increase liver and skeletal muscle glycogenolysis - Hyperglycemia with DM
- Increase blood glucose (β2) patient
- Reduce insulin secretion (α1)
CNS stimulation - Fear
- Anxiety
- Sweating
- Headache
- Nausea and vomiting
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
SYMPATHOLYTIC AGENTS
Adrenergic Receptor Antagonist
Alpha Blockers Beta Blockers
Nonselective Selective Nonselective Selective Beta-1
- Phentolamine (reversible) Alpha-1 Alpha-2 1st generation 3rd generation 2nd generation 3rd generation
- Phenoxybenzamine (irreversible) - Prazosin - Yohimbine - Propranolol - Carvedilol - Acebutolol - Betaxolol
- Labetalol - Atenolol - Celiprolol
Class Drugs PA TU SE
Non selective α blocker - Phentolamine - Reduction in vascular tone - Presurgical pheochromocytoma - reflex tachycardia
- Phenoxybenzamine - Reduction in arterial and venous pressure - Raynaud phenomenon - Orthostatic HTN
- Erectile dysfunction
Selective α blocker
l - Prazosin - Reduce blood pressure with less - HTN - Postural HTN
- Yohimbine tachycardia reflex - CHF - Syncope
- Relaxing effect in smooth muscle in prostate - Prevent urinary retention (BPH) - Headache and dizziness
- Variant angina
Heart - Arrhythmias - Reduce HR
- Reduce HR - Hypertension (portal HTN) - Heart block
- Reduce FOC - Hyperthyroid - Hypotension
- Reduce SBP - Anxiety and alcohol withdrawal - Hypertension in
pheochromocytoma when use
alone
Non selective β blocker - Propranolol
Bronchial Smooth Muscle - Bronchial spasm
- Bronchoconstriction - CI in bronchial asthma
Eye - Glaucoma
- Reduce IOP
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
HAEMOPOIETIC & LYMPHOID SYSTEM: DRUGS THERAPY OF MALARIA
Class Drugs MOA TU SE
- Chloroquine (CQ) - Acute attack of CQ sensitive - GI irritation
- Piperaquine falciparum and non-falciparum - Skin rash
- Tetracycline Destroy schizonts or merozoites in the RBC. - Chemoprophylaxis - Headache
- Doxycycline 1. Accumulate in food vacuole of plasmodium - Amoebic live abscess - Skin lesions
- Clindamycin 2. Prevents polymerization of haemoglobin - Retinal damage
3. Breakdown product heme into hemozin - Myocardial depression
4. Intracellular accumulation of heme is toxic to the
- Artesunate parasite - Chloroquine resistant malaria - Nausea & vomiting
- Artemether - Multidrug resistance - Diarrhea
- Dihydroartemisinin plasmodium falciparum
- Quinine 1. Complex with DSDNA - CQ resistant to plasmodium - Haemolytic anaemia
2. Prevent strand separation falciparum - Blackwater fever
Blood Schizonticides
3. Result in block of DNA replication and transcription - Severe complicated falciparum - Intravascular coagulation
to RNA malaria - Impaired hearing
- Nausea and vomiting
- Oedema
- Renal failure
- Mefloquine - Act as blood schizonticides - Prophylaxis for CQ resistance - GI distress
- Skin rashes
- Headache and dizziness
- Seizures
- Antifolate drugs 1. Antimetabolites of PABA - CQ resistance falciparum - GI distress
2. Block folic acid synthesis - Chemoprophylaxis of CQ - Skin rashes
3. By inhibiting dihydropteroate synthase - Kidney damage
Types of therapy
1. Prophylactic
2. Therapeutic (curative)
3. Prevention of transmission
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
HAEMOPOIETIC & LYMPHOID SYSTEM: DRUGS THERAPY OF MALARIA
Class Drugs MOA TU SE
Tissue schizonts - Primaquine Destroys secondary EE stage of tissue schizonts - Prevent relapse malaria - GI distress
1. Form quinolones – quinone metabolites - Prevent transmission of infection - Pruritus
2. Electron transferring redox compound - Headache
3. Act as cellular oxidants - Haemolyses in G6PD
Gametocide - Primaquine Destroy gametocyte in blood - GI irritation
- Chloroquine - Skin rash
- Quinine - Headache
- Retinal damage
Sporonticides - Proguanil Prevent sporogony and multiplication in
- Pyrimethamine mosquito
Drugs prevention malaria in travellers?
Chloroquine & Mefloquine
Multidrug resistance malaria?
Doxycycline, Malarone, Primaquine
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
HAEMOPOIETIC & LYMPHOID SYSTEM: DRUGS TO TREAT ANAEMIA
Class Drugs MOA TU SE
Iron (Ferrous Oral 1. Biosynthesis of heme and heme-containing proteins - Iron deficiency anaemia - N&V
Sulfate) - Ferrous gluconate 2. Include haemoglobin and myoglobin - Microcytic anaemia - Dyspnoea
- Ferrous fumarate 3. Replaces Fe found in HB, myoglobin and enzymes - Dark stool
Parenteral 4. Allow transportation of oxygen via Hb - Dental discoloration
- Iron dextran
- Iron sucrose complex
Iron chelators - Deferoxamine 1. Chelates excess iron - Acute iron poisoning - Hypotension
- Hemochromatosis - Neurotoxicity
Vitamin B12 - Cyanocobalamin 1. Cofactor for enzymatic reactions that form tetrahydrofolate - Vitamin B12 deficiency - CHF
- Hydroxocobalamin 2. Converted to coenzyme B12 - Megaloblastic anaemia - Arthralgia
3. Co-B12 convert methylmalonate to succinate - Pernicious anaemia - Headache
2. Convert homocysteine to methionine - Hydroxocobalamin - Angioedema
3. Promote haematopoiesis
Folic acid - Folic acid - Require for normal DNA synthesis - Folate deficiency - Flushing
- FA converted to tetrahydrofolate by dihydrofolate reductase - Megaloblastic anaemia - Anorexia
- FA is essential for nucleoprotein synthesis - Prevent congenital neural tube - Pruritus
- To maintain erythropoiesis defects - Malaise
Erythrocyte - Epoetin alfa 1. Agonist of erythropoietin receptors expressed by red cell - Anaemia associated with chronic - Hypertension
Stimulating progenitors renal failure - Thrombotic
Agents 2 Stimulate erythroid proliferation and differentiation - HIV Infection - Pure red cells aplasia
3. Induces the release of reticulocyte from the bone marrow - Cancer
Myeloid - Granulocyte colony 1. Stimulates neutrophil progenitor proliferation and - Neutropenia - Bone pain
Growth stimulating factor differentiation - Myelodysplasia - Splenic rupture
Factors - Filgrastim 2. Activates phagocytic activity of mature neutrophils and - Aplastic anaemia
extends their survival - Cytotoxic chemotherapy
3. Mobilizes hematopoietic stem cells
Megakaryocyte - Oprelevkin (IL-11) 1. Activate IL-11 receptors - Secondary prevention - Fatigue
Growth 2. Stimulate growth of multiple lymphoid and myeloid cells, thrombocytopenia - Headache
Factors include megakaryocytes - Cytotoxic chemotherapy - Dizziness
3. Increased number of circulating platelets and neutrophils - Anaemia
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
HAEMOPOIETIC & LYMPHOID SYSTEM: DRUGS ACTING ON BLEEDING AND CLOTTING DISORDERS
Class Drugs MOA TU SE
- Heparin (LMWH) 1. Inhibit coagulation - Treatment of established venous - Haemorrhage
2. Activating antithrombin III thromboembolism - Heparin induced
3. ATIII is a naturally occurring inhibitor of thrombin and - Reduce risk VT in angina and thrombocytopenia
clotting factor IX, Xa, XI, and XII following acute MI - Alopecia
- Osteoporosis
- Hypersensitivity
Anticoagulants
Warfarin 1. Structural analog of vitamin K - Prevent progression venous - Bleeding
2. competitively inhibit Vitamin K epoxide reductase enzyme thrombosis & pulmonary embolism - Fracture tendency
3. Leading to inhibition of synthesis of coagulation factor II, VII, - Prevent arterial thromboembolic - Pruritus
IX and X - Purpura
- Ecchymosis
- Purple toe syndrome
- Aspirin 1. Irreversibly inhibit COX1 - Mild to moderate pain and fever - Thrombocytopenia
2. Resulting in direct inhibition synthesis of prostaglandin and - Rheumatic disorder - Gastric irritation
thromboxane from arachidonic acid - Angina pectoris, MI, AI stroke - Dizziness
3. Inhibit platelet aggregation - Prophylaxis of CVS event - Bronchospasm
- Ticlopidine 1. Inhibit adenosine diphosphate to platelet receptors - Intermittent claudication - Diarrhea
Antiplatelet
2. Impair ADP mediated activation of glycoprotein complex - IHD - hepatitis
3. Prevent fibrinogen binding to platelets - Prevent thrombotic stroke - cholestatic jaundice
4. Inhibit platelet aggregation and prolongs the bleeding time - Prevent subacute stent occlusion - Increase serum
cholesterol level
- TTP
- Aplastic anaemia
Fibrinolytic - Streptokinase 1. Form a complex plasminogen - Acute MI - Abdominal pain
(Thrombolytic) 2. Converts plasminogen to plasmin - Pulmonary thromboembolism - N&V
3. Plasmin break down clots, fibrinogen & other plasma protein - Arteriovenous occlusion - ARF
4. Clots dissolved - Hypotension
Coagulants - Vitamin K 1. Inhibit fibrinolysis - Short term control haemorrhage - Impaired colour vision
- Coagulation Factors 2. Prevent the binding of plasminogen and plasmin to fibrin - Menorrhagia - Anaemia
- Tranexamic Acid 3. Prevent dissolution of haemostatic plug - Hereditary angioedema - N&V
- Haemophilia patient undergo - Fatigue and cramps
dental extraction - Migraine
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
CARDIOVASCULAR SYSTEM: DRUGS USED IN HYPERCHOLESTEROLEMIA
Class Drugs MOA TU SE
HMG-CoA Prodrugs 1. Inhibit HMG-CoA reductase - Reduce LDL level - Increase creatine kinase
Reductase - Lovastatin 2. Reduce concentration of cholesterol within cell - Increase triglyceride - Increase serum aminotransferase
Inhibitors - Simvastatin 3. Low [cholesterol] stimulate synthesis of LDL receptor - Increase HDL level - Rhabdomyolysis
4. Increase number of LDL receptor - Teratogenic
Active Drugs 5. Promote uptake of LDL from blood
- Fluvastatin 6. Low intracellular cholesterol reduce VLDL secretion
- Pravastatin
Bile acid - Cholestyramine 1. Prevent recycling of bile acids - Hypercholesterolemia - Constipation
sequestrants - Colestipol 2. Bile acid-binding resin divert hepatic cholesterol - Relieves pruritus - Impair ADEK renal absorption
- Colesevelam 3. Synthesis of new bile acid (accumulation of bile acid in - Interfere intestinal drug absorption
4. Reduce amount of cholesterol in tightly regulated pool biliary obstruction)
5. Increase removal of LDL in blood
Antilipemic agent - Niacin 1. Inhibit lipolysis in adipose tissue - Lowering cholesterol - Cutaneous flush & pruritus
2. Reduce level of plasma FA and TG - Raising plasma HDL - Nausea and abdominal pain
3. Reduce VLDL concentration in liver - Hyperuricemia and gout
4. Reduce plasma LDL concentration - Hepatotoxicity
Fibrates - Fenofibrate 1. Reduce total plasma triglyceride - Hypertriacyl-glycerolemias - Nausea
- Gemfibrozil 2. Activation of PPAR-alpha and lipoprotein lipase - Type III hyperlipidemia - Lithiasis
3. Reduce production of apoprotein CIII - Myositis
4. Increase synthesis of apoprotein AI, AII and FA - Elevate level of sulfonylureas
transport protein
5. Result in increasing VLDL catabolism and FA oxidation
6 Increase HDL level
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
CARDIOVASCULAR SYSTEM: ANTIHYPERTENSIVE (DRUG THERAPY OF HYPERTENSION)
Class Drugs MOA TU SE
Thiazide 1. Inhibit NA reabsorption in distal tubule - Hypertension - Photosensitivity
- Hydrochlorothiazide 2. Increased excretion of Na, K, Mg, H ions and water - Oedema - Hyperglycemia
3. Promote diuresis - Renal dysfunction
4. Reduce (ECF volume, CO, BP) - Orthostatic hypotension
5. Direct vasodilation, reduce (PR and BP)
Loop Diuretic 1. Inhibit reabsorption of NA and Cl in ascending LoH - Oedema - N&V
- Furosemide 2. Interfere with chloride binding cotransport system - Hypertension - Dehydration
3. Causing Na excretion in urine - Oliguria in renal failure - Muscle spams
Diuretics 4, Promote diuresis - Acute pulmonary oedema - Orthostatic hypotension
K Sparring Diuretic 1. Steroid that resemble aldosterone - Oedema - N&V
- Spironolactone 2. Inhibit aldosterone receptor in DCT - Malignant ascites - Hepatotoxicity
3. Increase excretion of NaCl and water - Diagnose primary hyperaldosteronism - Muscle spasm
4. Maintain K and H ions - Nephrotic syndrome - Hypotension
5. Promote diuresis - CHF with oedema
- Hypertension
- Heart failure
Class Drugs MOA TU SE
Central SL 1. Stimulate central alpha adrenergic receptors - Hypertension - N&V
- Methyldopa 2. Use false receptor (alpha-methylnorepinephrine) - Drowsiness
- Clonidine 3. Reduce sympathetic outflow - Bradycardia
4. Lead to fall in BP - Orthostatic hypotension
Neuronal Blocker 1. Cause depletion of NE, serotonin & catecholamine - Hypertension - Nasal congestion
- Reserpine 2. Result in reduce BP, bradycardia & CNS depression - Chronic psychosis - Abdominal cramps
- Guanethidine 3. Decrease CO and PR lead to hypotensive effect - Bradycardia
Sympatholytic
α1 Receptor Blocker 1. Competitively inhibit postsynaptic α1 adrenoreceptor - Hypertension - Angina
- Prazosin in vascular SM. - Heart failure - Dyspnoea
- Doxazosin 2. Result in vasodilation, decrease TPR and BP - BPH (Raynaud’s syndrome) - Oedema
β Receptor Blocker 1. Competitively block β1 and β2 receptors - Angina pectoris - N&V
- Propranolol 2. Reduce HR, BP, CO & myocardial contractility - Pheochromocytoma - Hallucination
- Atenolol 3. Reduce angiotensin level (reduce renin) - Hypertrophic cardiomyopathy - Hypotension
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
CARDIOVASCULAR SYSTEM: ANTIHYPERTENSIVE (DRUG THERAPY OF HYPERTENSION)
Class Drugs MOA TU SE
Direct 1. Direct vasodilators at arterioles - Hypertension - SLE like syndrome
- Nitroprusside 2. Inhibit Ca release from sarcoplasmic reticulum - CHF - Postural hypotension
- Hydralazine 3. Inhibit myosin phosphorylation in arterial SM - Hypertensive crisis - Tachycardia
- Minoxidil - Anorexia
- Diazoxide
Vasodilators Calcium Chanel Blocker 1. Inhibit transmembrane influx of extracellular Ca2+ - Hypertension - Peripheral oedema
- Nifedipine (vessel) 2. Inhibit across myocardial and vascular SM layers - Angina pectoris - Heartburn
- Verapamil (cardiac) 3. Without changing serum calcium concentrations - Raynaud’s syndrome - Hypotension
4. Result in inhibit of cardiac and vascular SM - Constipation
contraction - Dyspnoea
5. Dilatation of coronary and systemic arteries - Headache
ACE Inhibitors 1. Sulfhydryl contain ACE inhibitor - Hypertension - N&V
- Captopril 2. Inhibit ACE - CHF - Hypotension
3. Prevent conversion of Angiotensin I to II - Post MI - Dyspnoea
4. Increase plasma renin activity - Diabetic nephropathy - Pruritus
5. Reduce aldosterone secretion
6. Promotes sodium and water excretion
Angiotensin
Antagonist ARBs (Angiotensin II) 1. Bind to angiotensin I receptor - Hypertension - N&V
- Irbesartan 2. Block vasoconstriction and aldosterone secreting - Diabetic nephropathy - Fatigue
effect of angiotensin II - Heartburn
3. Inhibit release of aldosterone - Orthostatic hypotension
4. Unable to reabsorb NaCl and water
5. Reduce plasma volume
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
CARDIOVASCULAR SYSTEM: DRUG FOR HEART FAILURE
Class Drugs MOA TU SE
- Digoxin 1. Inhibit Na, K, ATPase - CHF - N&V
2. Increase intracellular Na - Atrial fibrillation - Headache
3. Increase intracellular Ca via Na-Ca exchange carrier mechanism - Slow ventricular rate - Bradycardia
4. Increase myocardial uptake of Ca - Increase sensitivity of AV nodes - Arrhythmias
5. Augments Ca release to myofilaments during excitation - Increase peripheral VR
6. Invoke positive inotropic responses
Therefore stimulate:
Positive - Myocardial contractility
inotropic agent - Increase CO
- Promotes diuresis
- Reduce diastolic pressure
- Increase systemic venous pressure
- Milrinone 1. Increase calcium influx in the heart during action potential - HF - N&V
2. Inhibit phosphodiesterase - Thrombocytopenia
- Liver enzyme change
Beta agonist - Dobutamine 1. Bind at Beta adrenergic receptor - Management of acute HF - Tachycardia
- Dopamine 2. Activates adenyl cyclase to produce cAMP - Tolerance
3. cAMP activate protein kinase - Arrhythmias
4. Phosphorylation of calcium channel - Peripheral vasoconstriction
5. Increase calcium flow into cell
6. Increase FoC of heart muscle
Beta blockers - Propranolol 1. Competitively inhibit beta-1 and beta-2 receptors - CHF - Dizziness
- Atenolol 2. Decrease in heart rate - Bradycardia
- Bisoprolol 3. Myocardial contractility - Bronchospasm
- Metoprolol 4. BP and myocardial oxygen demand - Orthostatic hypotension
- Carvedilol 5. Negative inotropic effect and membrane stabilising activity
Other drugs use?
Diuretics, ACEi, and Vasodilators
**refer to: cardiovascular system: antihypertensive (drug therapy of hypertension)
**inotropic effect: change the force of contraction in heart (+ve ino: strengthen, -ve ino: weaken)
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
CARDIOVASCULAR SYSTEM: ANTI-ARRHYTHMICS
Class Drugs MOA TU SE
Class I – Sodium - Procainamide (IA) 1. Block Na channel - Acute MI - Bradycardia
Channel Blockers 2. Reduce conduction velocity through myocardium - Supraventricular tachyarrhythmia - Myalgia
- Lidocaine (IB) 1. Lidocaine alters signal conduction - Ventricular arrhythmias - Sleepiness
2. Prolong inactivation of fast voltage gated Na channel - Digoxin poisoning - Vomiting
3. Inhibit action potential (AP) propagation - Cardiac catheterization - Pupillary changes
4. Stop generation of AP - Hallucinations
- Flecainide (IC) 1. Block Na channel in the heart - Supraventricular tachycardia - Tachycardia
2. Slowing upstroke cardiac AP - Wolff Parkinson White Syndrome - Dizziness
3. Slowing conduction - Blurred vision
4. Reduce muscle contractility - Chest pain
5. Decrease in ejection fraction
Class II – Beta - Propranolol 1. Competitively inhibit beta-1 and beta-2 receptors - CHF - Dizziness
Blockers 2. Decrease in heart rate - Cardiac arrhythmias - Bradycardia
3. Myocardial contractility - Bronchospasm
4. BP and myocardial oxygen demand
5. Negative inotropic effect
6. Membrane stabilising activity
Class III – Potassium - Amiodarone 1. Inhibit adrenergic stimulation - Ventricular arrhythmias - Hypotension
Channel Blockers 2. Block K channel - Ventricular tachycardia - Fatigue
3. Prolong AP duration - Anorexia
4. Reduce AV conduction - Photosensitivity
Class IV – Calcium - Verapamil 1. Inhibit calcium entry into slow channels during - Supraventricular arrhythmias - Bradycardia
Channel Blockers depolarisation - Angina pectoris - Flushing
2. Relaxes coronary vascular SM - Prophylaxis MI - Fatigue
3. Coronary vasodilation - Hepatotoxicity
4. Increase myocardial oxygen delivery
5. Slow AV node conduction
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
CARDIOVASCULAR SYSTEM: ANTI-ARRHYTHMICS
Class Drugs MOA TU SE
Class V - Adenosine 1. Endogenous purine nucleoside - Supraventricular tachycardia - Nausea
2. Stimulate A1 receptors - Myocardial imaging - Headache
3. Slow conduction time through AV nodes - Bradycardia
4. Stimulate A2 receptors - Bronchospasm
5. Produce peripheral and coronary vasodilation
6. Increasing blood flow in normal arteries
Positive Inotropic - Digoxin 1. Inhibit Na, K, ATPase - CHF - N&V
Agent 2. Increase intracellular Na - Atrial fibrillation - Headache
3. Increase intracellular Ca via Na-Ca exchange carrier - Slow ventricular rate - Bradycardia
mechanism - Increase sensitivity of AV nodes - Arrhythmias
4. Increase myocardial uptake of Ca - Increase peripheral VR
5. Augments Ca release to myofilaments during excitation
6. Invoke positive inotropic responses
Therefore stimulate:
- Myocardial contractility
- Increase CO
- Promotes diuresis
- Reduce diastolic pressure
- Increase systemic venous pressure
Prepared by Shafuan Abu Bakar (MSU-MBBS Batch April 2019)
***Please make photocopy and share this to your friends
You might also like
- Cramsheet (Exam Cram Nclex PN)Document2 pagesCramsheet (Exam Cram Nclex PN)Katrina Reyes94% (32)
- NSAIDS and SteroidsDocument2 pagesNSAIDS and Steroidsmed testNo ratings yet
- Commonly Prescribed Psych MedsDocument2 pagesCommonly Prescribed Psych MedsburlacuraduuNo ratings yet
- Pediatric DosesDocument17 pagesPediatric DosesIris MambuayNo ratings yet
- Gastrointestinal: Nclex-Rn ReviewerDocument34 pagesGastrointestinal: Nclex-Rn ReviewerJohnasse Sebastian NavalNo ratings yet
- IV Antibiotics and PO Medications Dosing ChartDocument3 pagesIV Antibiotics and PO Medications Dosing ChartNikki DiocampoNo ratings yet
- Med-Surg Lecture 4th Year 1st Sem (Incomplete)Document70 pagesMed-Surg Lecture 4th Year 1st Sem (Incomplete)Raezhell Dianne RachoNo ratings yet
- General Principles of Clinical ToxicologyDocument34 pagesGeneral Principles of Clinical ToxicologySigita KazūneNo ratings yet
- Drug Study AtorvastatinDocument1 pageDrug Study AtorvastatinEzron Kendrick DuranNo ratings yet
- HydrocortisoneDocument2 pagesHydrocortisoneIvanne Hisoler100% (15)
- MethotrexateDocument2 pagesMethotrexateIvanne Hisoler83% (6)
- Drug Study PrednisoloneDocument2 pagesDrug Study Prednisoloneunnamed personNo ratings yet
- DexamethasoneDocument3 pagesDexamethasoneGwyn RosalesNo ratings yet
- Naproxen Sodium Drug StudyDocument1 pageNaproxen Sodium Drug StudyKarl Lourenz Deysolong100% (1)
- IV Infusion One Compartment ModelDocument18 pagesIV Infusion One Compartment ModelMubammad MursaleenNo ratings yet
- Vincristine Drug StudyDocument4 pagesVincristine Drug StudyNiziu BearsNo ratings yet
- GOUTDocument36 pagesGOUTGanesha Gamma 2017100% (1)
- Uji Toxi LabDocument19 pagesUji Toxi LabSivajothi RamuNo ratings yet
- Pharmacy and Therapeutics Committee Policies and ProceduresDocument5 pagesPharmacy and Therapeutics Committee Policies and ProceduresPHARMACY OLMCMCNo ratings yet
- Prednisone Drug StudyDocument3 pagesPrednisone Drug StudyNiziu BearsNo ratings yet
- Drug Study: Patient Name: SSG. Tungson, Christian 34 Y/oDocument11 pagesDrug Study: Patient Name: SSG. Tungson, Christian 34 Y/oNelle ReyNo ratings yet
- 7endocrine DrugsDocument2 pages7endocrine DrugsSOFIA ALYSSA MARIE ABUDENo ratings yet
- Addison's Disease (Primary Adrenal Insufficiency)Document5 pagesAddison's Disease (Primary Adrenal Insufficiency)sunnnydayNo ratings yet
- Dr. Kobal Low CarbDocument42 pagesDr. Kobal Low CarbGhea Putri HendrianiNo ratings yet
- Myasthenia Gravis TransDocument2 pagesMyasthenia Gravis Trans2013SecBNo ratings yet
- Pharmacological effects and clinical applications of corticosteroids in dentistryDocument27 pagesPharmacological effects and clinical applications of corticosteroids in dentistryFinnyalfNo ratings yet
- Drug Study GuideDocument40 pagesDrug Study GuideFERL KAILA SANTOSNo ratings yet
- Drugstudy - Gorospe, Diana R.Document2 pagesDrugstudy - Gorospe, Diana R.Diana GorospeNo ratings yet
- Immunopharmacology PDFDocument2 pagesImmunopharmacology PDFErica Hyeyeon LeeNo ratings yet
- Opioids & MSK TreatmentDocument6 pagesOpioids & MSK TreatmentNashrah HusnaNo ratings yet
- Most Common DrugsDocument10 pagesMost Common DrugsNashat SaadiNo ratings yet
- Wuolah-Free-Topic 27Document2 pagesWuolah-Free-Topic 27Moldovan Maria TatianaNo ratings yet
- Drug Sheet 2Document88 pagesDrug Sheet 2Umbe ChinakaNo ratings yet
- Badassery For Patho Exam 3Document19 pagesBadassery For Patho Exam 3HannaNo ratings yet
- Drug Study 1.1Document2 pagesDrug Study 1.1Arianne Nicole PinuelaNo ratings yet
- Autocids, Gout & R. ARTHRITIS-NursingDocument36 pagesAutocids, Gout & R. ARTHRITIS-NursingManikanta GupthaNo ratings yet
- Indikasi Efek Samping Dan Kontra Indikasi ObatDocument2 pagesIndikasi Efek Samping Dan Kontra Indikasi ObatKrisnaNo ratings yet
- CelecoxibDocument2 pagesCelecoxibAxseal ANo ratings yet
- IT 7 - Gout - RADDocument40 pagesIT 7 - Gout - RADIsal MutaqqienNo ratings yet
- JINANG's Drug Data SummaryDocument4 pagesJINANG's Drug Data SummaryiammaiaNo ratings yet
- Name of DrugDocument6 pagesName of DrugGail Leslie HernandezNo ratings yet
- NSAIDs: Mechanisms, Uses and Adverse EffectsDocument43 pagesNSAIDs: Mechanisms, Uses and Adverse EffectsTes B FourieNo ratings yet
- Leaflet Cushing SyndromeDocument2 pagesLeaflet Cushing SyndromesepthyaniNo ratings yet
- StreptomycinDocument1 pageStreptomycinDemilyn Fat100% (2)
- Pharmacology Reviewer Module 1Document10 pagesPharmacology Reviewer Module 1Krizia mae LaureanoNo ratings yet
- Drug study classification and indicationsDocument4 pagesDrug study classification and indicationsROLAND LAURENCE BARGO JARDIOLINNo ratings yet
- Drug Study FormDocument4 pagesDrug Study FormRhea LaplanaNo ratings yet
- ThyroxineDocument37 pagesThyroxinedfdxgfcvhbNo ratings yet
- Disorder and MedsDocument6 pagesDisorder and MedsKaty PerchieNo ratings yet
- Addison's Disease FileDocument25 pagesAddison's Disease FileZyla KrisshaNo ratings yet
- DRUG STUDY: NIFEDIPINE FOR HYPERTENSION AND ANGINADocument28 pagesDRUG STUDY: NIFEDIPINE FOR HYPERTENSION AND ANGINAginosan100% (1)
- Case Study - ESRD (DS, NCP)Document8 pagesCase Study - ESRD (DS, NCP)Zhy CaluzaNo ratings yet
- ADDISONS DSE - Etio Trends&Issues + DSDocument9 pagesADDISONS DSE - Etio Trends&Issues + DSgraceNo ratings yet
- A. Drug StudyDocument8 pagesA. Drug Studyyfc22No ratings yet
- MBR 2019 - Pathology HandoutsDocument98 pagesMBR 2019 - Pathology HandoutsRgm UyNo ratings yet
- NSAIDs Lecture 2 Mechanism of Action and ClassificationDocument12 pagesNSAIDs Lecture 2 Mechanism of Action and Classificationأحہمہد بہنہ قہمہوNo ratings yet
- Screening For Micro and Macrovascular ComplicationDocument38 pagesScreening For Micro and Macrovascular ComplicationRoby KieranNo ratings yet
- Ph119.1 Final NotesDocument13 pagesPh119.1 Final NotesANDREA GAIL ANONUEVONo ratings yet
- Pharmacology LectureDocument18 pagesPharmacology LectureChloe MorningstarNo ratings yet
- PcolDocument17 pagesPcolThea JulianaNo ratings yet
- FA PharmacologyDocument94 pagesFA PharmacologyMarcos CrespoNo ratings yet
- Immunology '' Immunology-Immunosuppressants Immunology '' Immunology-Immunosuppressants Section IiDocument8 pagesImmunology '' Immunology-Immunosuppressants Immunology '' Immunology-Immunosuppressants Section IiMarcos CrespoNo ratings yet
- DS Isph GS DRDocument7 pagesDS Isph GS DRTanya Victoria Lean ClaudioNo ratings yet
- NSAIDSDocument19 pagesNSAIDSDonna Kelly DuranNo ratings yet
- SBRC General PrinciplesDocument51 pagesSBRC General Principlesdalia khamoNo ratings yet
- Drug StudyDocument10 pagesDrug StudyNine SaguiboNo ratings yet
- Aldosterone: International Series of Monographs in Pure and Applied BiologyFrom EverandAldosterone: International Series of Monographs in Pure and Applied BiologyNo ratings yet
- 10 - 01 - Investigator BrochureDocument6 pages10 - 01 - Investigator BrochureLaura SaglietiNo ratings yet
- Pharmacology & Therapeutics Supplements: Ali Raza Chaudary (N67)Document110 pagesPharmacology & Therapeutics Supplements: Ali Raza Chaudary (N67)bajan100% (1)
- Helicobacter Test and Medication ListDocument124 pagesHelicobacter Test and Medication ListralucaIONo ratings yet
- Health Canada Info FactsheetDocument2 pagesHealth Canada Info Factsheetapi-26034055No ratings yet
- Type A vs Type B adverse drug reactions comparisonDocument2 pagesType A vs Type B adverse drug reactions comparisonchristinaj98No ratings yet
- Journal ClubDocument28 pagesJournal Clubapi-355090691No ratings yet
- MIDAZOLAM DRUG STUDYDocument5 pagesMIDAZOLAM DRUG STUDYShara Lailanie A. AzisNo ratings yet
- Polio Sabin GDS03.IPI01 PDFDocument5 pagesPolio Sabin GDS03.IPI01 PDFDevalina JunaharNo ratings yet
- Globela Pharma PVT LTD Party Content 1536648997Document10 pagesGlobela Pharma PVT LTD Party Content 1536648997Chetan dhadhlaNo ratings yet
- Anti Psychotic DrugsDocument6 pagesAnti Psychotic DrugsJoseph NyirongoNo ratings yet
- NepafenacDocument4 pagesNepafenacrasfaqur100% (1)
- Research PaperDocument6 pagesResearch PaperNitin BansalNo ratings yet
- Persediaan Obat 2023jan-JuniDocument136 pagesPersediaan Obat 2023jan-JuniSandra Puspa KartikaNo ratings yet
- BCS 1 1 PDFDocument38 pagesBCS 1 1 PDFHely PatelNo ratings yet
- Anti Epileptic DrugsDocument89 pagesAnti Epileptic DrugsInderjeet SohalNo ratings yet
- Pharmacokinetics of AnestheticsDocument5 pagesPharmacokinetics of AnestheticsFairysparklesNo ratings yet
- Brochure Managing High CholesterolDocument16 pagesBrochure Managing High CholesterolSonukumar AgrawalNo ratings yet
- Amorolfine ClorhidratoDocument17 pagesAmorolfine ClorhidratocarbouNo ratings yet
- CNS Stimulants 2010Document38 pagesCNS Stimulants 2010Neal KirkNo ratings yet
- Novel Uses of Drug Transporters For Drug Delivery: A Case Study With GabapentinDocument46 pagesNovel Uses of Drug Transporters For Drug Delivery: A Case Study With GabapentinyosysilalahiNo ratings yet
- Digital vaccine certificate detailsDocument1 pageDigital vaccine certificate detailsHindunZawawi 008No ratings yet