Professional Documents
Culture Documents
Jama Sandner 2022 Oi 220074 1659634147.83672
Uploaded by
lakshminivas PingaliOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jama Sandner 2022 Oi 220074 1659634147.83672
Uploaded by
lakshminivas PingaliCopyright:
Available Formats
Research
JAMA | Original Investigation
Association of Dual Antiplatelet Therapy With Ticagrelor
With Vein Graft Failure After Coronary Artery Bypass Graft Surgery
A Systematic Review and Meta-analysis
Sigrid Sandner, MD; Björn Redfors, MD, PhD; Dominick J. Angiolillo, MD; Katia Audisio, MD;
Stephen E. Fremes, MD; Paul W.A. Janssen, MD; Alexander Kulik, MD; Roxana Mehran, MD; Joyce Peper, MD;
Marc Ruel, MD; Jacqueline Saw, MD; Giovanni Jr Soletti, MD; Andrew Starovoytov, MD; Jurrien M. ten Berg, MD;
Laura M. Willemsen, MD; Qiang Zhao, MD, PhD; Yunpeng Zhu, MD; Mario Gaudino, MD, PhD
Editorial page 532
IMPORTANCE The role of ticagrelor with or without aspirin after coronary artery bypass graft Supplemental content
surgery remains unclear.
OBJECTIVE To compare the risks of vein graft failure and bleeding associated with ticagrelor
dual antiplatelet therapy (DAPT) or ticagrelor monotherapy vs aspirin among patients
undergoing coronary artery bypass graft surgery.
DATA SOURCES MEDLINE, Embase, and Cochrane Library databases from inception to June 1,
2022, without language restriction.
STUDY SELECTION Randomized clinical trials (RCTs) comparing the effects of ticagrelor DAPT
or ticagrelor monotherapy vs aspirin on saphenous vein graft failure.
DATA EXTRACTION AND SYNTHESIS Individual patient data provided by each trial were
synthesized into a combined data set for independent analysis. Multilevel logistic regression
models were used.
MAIN OUTCOMES AND MEASURES The primary analysis assessed the incidence of saphenous
vein graft failure per graft (primary outcome) in RCTs comparing ticagrelor DAPT with aspirin.
Secondary outcomes were saphenous vein graft failure per patient and Bleeding Academic
Research Consortium (BARC) type 2, 3, or 5 bleeding events. A supplementary analysis
included RCTs comparing ticagrelor monotherapy with aspirin.
RESULTS A total of 4 RCTs were included in the meta-analysis, involving 1316 patients and
1668 saphenous vein grafts. Of the 871 patients in the primary analysis, 435 received
ticagrelor DAPT (median age, 67 years [IQR, 60-72 years]; 65 women [14.9%]; 370 men
[85.1%]) and 436 received aspirin (median age, 66 years [IQR, 61-73 years]; 63 women
[14.5%]; 373 men [85.5%]). Ticagrelor DAPT was associated with a significantly lower
incidence of saphenous vein graft failure (11.2%) per graft than was aspirin (20%; difference,
−8.7% [95% CI, −13.5% to −3.9%]; OR, 0.51 [95% CI, 0.35 to 0.74]; P < .001) and was
associated with a significantly lower incidence of saphenous vein graft failure per patient
(13.2% vs 23.0%, difference, −9.7% [95% CI, −14.9% to −4.4%]; OR, 0.51 [95% CI, 0.35 to
0.74]; P < .001). Ticagrelor DAPT (22.1%) was associated with a significantly higher incidence
of BARC type 2, 3, or 5 bleeding events than was aspirin (8.7%; difference, 13.3% [95% CI,
8.6% to 18.0%]; OR, 2.98 [95% CI, 1.99 to 4.47]; P < .001), but not BARC type 3 or 5 bleeding
events (1.8% vs 1.8%, difference, 0% [95% CI, −1.8% to 1.8%]; OR, 1.00 [95% CI, 0.37 to
2.69]; P = .99). Compared with aspirin, ticagrelor monotherapy was not significantly
associated with saphenous vein graft failure (19.3% vs 21.7%, difference, −2.6% [95% CI,
−9.1% to 3.9%]; OR, 0.86 [95% CI, 0.58 to 1.27]; P = .44) or BARC type 2, 3, or 5 bleeding
events (8.9% vs 7.3%, difference, 1.7% [95% CI, −2.8% to 6.1%]; OR, 1.25 [95% CI, 0.69 to
2.29]; P = .46).
Author Affiliations: Author
CONCLUSIONS AND RELEVANCE Among patients undergoing coronary artery bypass graft affiliations are listed at the end of this
article.
surgery, adding ticagrelor to aspirin was associated with a significantly decreased risk of vein
Corresponding Author: Mario
graft failure. However, this was accompanied by a significantly increased risk of clinically
Gaudino, MD, PhD, Department of
important bleeding. Cardiothoracic Surgery, Weill Cornell
Medicine, New York Presbyterian
Hospital, 525 E 68th St, New York,
NY 10065 (mfg9004@med.cornell.
JAMA. 2022;328(6):554-562. doi:10.1001/jama.2022.11966 edu).
554 (Reprinted) jama.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Bypass Surgery Original Investigation Research
S
aphenous vein grafts are the most frequently used
conduits in coronary artery bypass graft (CABG) sur- Key Points
gery, yet as many as 10% to 25% occlude within the
Question Is ticagrelor dual antiplatelet therapy (DAPT) for
first year after surgery.1,2 Early saphenous vein graft failure patients undergoing coronary artery bypass graft surgery
is mainly due to thrombosis subsequent to endothelial dam- associated with differences in vein graft failure and bleeding
age or endothelial activation leading to a prothrombotic events compared with aspirin?
phenotype.2,3 Inhibition of platelet aggregation with aspirin
Findings In this individual patient data meta-analysis that
after CABG surgery has been shown to reduce early saphe- included 4 randomized clinical trials, 1316 patients and 1668
nous vein graft failure and is endorsed in current practice vein grafts, ticagrelor DAPT compared with aspirin was associated
guidelines.4-6 Dual antiplatelet therapy (DAPT), consisting of with a significantly lower incidence of vein graft failure (11.2% vs
aspirin and an oral platelet P2Y12 receptor inhibitor, is associ- 20.0%) and a significantly higher incidence of Bleeding Academic
ated with enhanced platelet inhibitory effects.7 Although Research Consortium type 2, 3, or 5 bleeding events (22.1% vs
8.7%).
DAPT is the guideline-recommended treatment after percu-
taneous coronary revascularization,7 considerable contro- Meaning In patients undergoing coronary artery bypass graft
versy exists as to the benefit of DAPT for patients after CABG surgery, adding ticagrelor to aspirin was associated with
surgery. Studies comparing ticagrelor DAPT with aspirin have a significantly decreased risk of vein graft failure, as well
as a significantly increased risk of clinically important bleeding.
yielded conflicting results,8-10 and the few studies comparing
ticagrelor monotherapy with aspirin9,11 failed to demonstrate
an effect of ticagrelor monotherapy on saphenous vein graft provided to each trial (eMethods 2 in the Supplement). Data
failure; however, they were individually underpowered. received from the individual trial teams by the analysis unit
A systematic review and individual patient data meta- at Weill Cornell Medicine were checked for completeness and
analysis of all randomized clinical trials (RCTs) comparing the consistency with previous publications. Discrepancies were re-
effects of ticagrelor DAPT or ticagrelor monotherapy with as- solved directly with the trial investigators. For harmoniza-
pirin on saphenous vein graft failure among patients under- tion of graft failure definition across trials, occlusion and/or
going CABG surgery was performed. percent stenosis per graft or anastomosis (for sequential grafts)
were provided by each trial team. Events were readjudicated
centrally. For harmonization of bleeding outcomes, bleeding
events were readjudicated by each trial team according to
Methods Bleeding Academic Research Consortium (BARC) criteria.13 All
This study design was published a priori on the International analyses were performed independently on the combined data
Prospective Register of Systematic Reviews (CRD42021291997). set of individual patient data provided for each trial. The risk
The statistical analysis protocol was prespecified to reduce of bias was assessed using the Cochrane risk-of-bias tool 214
post hoc bias. The analysis was performed in accordance (eFigure 1 in the Supplement).
with the Individual Patient Data-Preferred Reporting Items
for Systematic Reviews and Meta-Analyses (IPD-PRISMA).12 Outcomes
The PRISMA checklist was followed. Ethics approval and The primary outcome was the incidence of saphenous vein graft
patient consent were obtained locally by each trial team. failure, defined as saphenous vein graft occlusion or stenosis
The Weill Cornell Medicine Institutional Review Board greater than 50% per graft as assessed by either invasive angi-
waived the need for ethics approval for the pooled analysis ography or computed tomographic angiography at the indi-
(protocol 22-03024559). vidual trial protocol–defined follow-up. Secondary outcomes
were the incidence of saphenous vein graft failure per patient
Search Strategy and Selection Criteria (defined as patients with ≥1 failed saphenous vein graft); the in-
A medical librarian searched Ovid MEDLINE, Ovid Embase, and cidence of BARC type 2, 3, or 5 bleeding events; the composite
the Cochrane Central (Wiley) databases to identify RCTs pub- of saphenous vein graft failure or cardiovascular death; and ma-
lished between database inception and June 1, 2022, compar- jor adverse cardiac and cerebrovascular events (MACCE, de-
ing ticagrelor DAPT and/or ticagrelor monotherapy with aspi- fined as the composite of all-cause death, myocardial infarc-
rin in patients undergoing CABG surgery who had follow-up tion, stroke, or revascularization). Definitions of events in the
for graft imaging. No language restrictions were imposed. The individual trials are provided in eTable 1 in the Supplement.
full search strategy is provided in the Supplement (eMethods Post hoc outcomes were the incidence of saphenous vein
1 in the Supplement). Identification of studies meeting the graft occlusion per graft; any graft failure (arterial or saphe-
search criteria was performed by 2 authors (S.S. and K.A.). Con- nous vein grafts); BARC type 2 through 5, 3 through 5, and 3
flicts over inclusion were resolved by consultation with a third or 5 bleeding events; the individual components of MACCE;
author (M.G.). major adverse cardiovascular events (MACE, defined as the
composite of cardiovascular death, myocardial infarction, or
Data Extraction and Quality Assessment stroke); and net adverse events (defined as graft failure [arte-
The principal investigators of the eligible trials were con- rial or saphenous vein grafts] or BARC type ≥3 bleeding event),
tacted and all agreed to share individual patient data. Speci- net adverse major clinical events (defined as all-cause death,
fications of core minimum deidentified data requirements were myocardial infarction, stroke, or BARC type ≥3 bleeding event),
jama.com (Reprinted) JAMA August 9, 2022 Volume 328, Number 6 555
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
Research Original Investigation Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Bypass Surgery
Table 1. Trial Characteristics
Experimental group Control group Time
Total No. of No. of Treatment Type to graft
Dates of No. of No. of No. of patients No. of patients No. of duration, of graft imaging,
Sourcea enrollment patients graftsb SVGs Treatment with SVGs SVGs Treatment with SVGs SVGs mo imaging mo
TAP-CABG,8 2011- 70 167 76 Ticagrelor 19 34 Placebo 23 42 3 CT angiography 3
2016 2014 90 mg 2/d + aspirin
+ aspirin 81 mg 1/d
81 mg 1/d
DACAB,9 2014- 500 1146 712 Group 1: 167 239 Aspirin 166 242 12 CT or coronary 12
2018 2015 ticagrelor 100 mg 1/d angiography
90 mg 2/d
+ aspirin
100 mg 1/d
Group 2: 166 231
ticagrelor
90 mg 2/d
TARGET,11 2014- 250 688 373 Ticagrelor 127 187 Aspirin 123 186 12 CT angiography 12
2022 2019 90 mg 2/d 81 mg 2/d
POPular 2015- 496 1078 507 Ticagrelor 249 254 Placebo 247 253 12 CT angiography 12
CABG,10 2019 90 mg 2/d + aspirin
2020 + aspirin 80 mg or
80 mg or 100 mg 1/d
100 mg 1/d
b
Abbreviations: CT, computed tomography; SVG, saphenous vein graft. Includes SVGs and arterial grafts (left and/or right internal thoracic artery, and
a
See the Methods section for the full names of the studies. radial artery).
and overall net adverse events (defined as graft failure, MACCE, procedure-related confounders that included age, sex, clini-
or BARC type ≥2 bleeding events). cal presentation, smoking, diabetes, hypertension, hyperlip-
idemia, prior myocardial infarction, chronic kidney disease,
Data Analysis use of cardiopulmonary bypass, endoscopic saphenous vein
Baseline categorical variables are reported as counts and per- graft harvesting, and sequential saphenous vein grafting.
centages. Continuous variables are reported as medians and Prespecified subgroup analyses for the primary outcome
IQRs. The primary analysis was performed according to ran- were age, sex, diabetes, smoking, acute coronary syndrome, use
domization group and compared ticagrelor DAPT with aspi- of cardiopulmonary bypass, endoscopic saphenous vein graft
rin. The primary analysis set was patients with saphenous vein harvesting, target vessel territory, use of sequential saphe-
grafts who were randomized to ticagrelor DAPT or aspirin and nous vein grafts, and treatment duration. For subgroup analy-
for whom protocol-defined imaging was available. The pri- ses, an interaction-term between the treatment and the sub-
mary outcome was evaluated using a multilevel logistic re- group of interest was included in the logistic regression model.
gression model using the GLIMMIX procedure 15 that ac- A supplementary analysis for the primary outcome com-
counted for clustering of patients within trials and clustering pared ticagrelor monotherapy with aspirin.
of grafts within patients. Treatment associations are reported Details on post hoc analyses are provided in eMethods 3
as odds ratios (ORs) and 95% CIs. in the Supplement. A post hoc random-effects network meta-
Secondary outcomes were evaluated using a multilevel analysis was performed to compare the associations of ticagre-
logistic regression model with the trial as a random effect lor DAPT, ticagrelor monotherapy, and aspirin with saphe-
(reported as OR and 95% CI) or a Cox proportional hazards nous vein graft failure.
frailty model with trial as a random effect (reported as hazard A 2-sided P value of <.05 was considered significant for all
ratio [HR] and 95% CI). Event rates were calculated using the tests. There was no adjustment for multiplicity. Because of the
Kaplan-Meier method. The proportional hazards assumption potential for type I error due to multiple comparisons, find-
was confirmed for each end point by using Schoenfeld residu- ings for analyses of secondary end points should be inter-
als and visual inspection of the Schoenfeld residuals, Kaplan- preted as exploratory. All analyses were performed using SAS
Meier plots, and log-log plots. version 9.4 (SAS Institute Inc) except for the network meta-
Sensitivity analyses for the primary outcome assessed the analysis, which was performed using R version 4.1.0.16
incidence of saphenous vein graft failure per anastomosis and
in patients who had 1-year imaging. Sensitivity models for the
primary outcome were performed in the as-treated popula-
tion (according to treatment received) and per-protocol popu-
Results
lation (according to whether treatment was received in com- Study Selection
pliance with the trial protocol), and after imputation of missing The literature search yielded 776 results, of which 557 were
data by multiple imputation (assuming a joint multivariate nor- screened for eligibility. Four trials meeting the inclusion cri-
mal distribution for all variables and imputing 20 data sets). teria were included in the analysis: Ticagrelor and Aspirin for
These sensitivity models were adjusted for baseline and the Prevention of Cardiovascular Events after Coronary Artery
556 JAMA August 9, 2022 Volume 328, Number 6 (Reprinted) jama.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Bypass Surgery Original Investigation Research
Table 2. Baseline Patient and Graft Characteristics Among Patients in the Primary Analysis
No. (%)
Ticagrelor DAPT (n = 435) Aspirin (n = 436)
Patientsa
Age, median (IQR), y 67 (60-72) 66 (61-73)
>65 y 249 (57.2) 241 (55.3)
Sex Abbreviations: ACS, acute coronary
Women 65 (14.9) 63 (14.5) syndrome; DAPT, dual antiplatelet
Men 370 (85.1) 373 (85.5) therapy; LAD, left anterior
descending artery; LVEF, left
Medical history ventricular ejection fraction;
Hypertensionb 294 (67.6) 294 (67.4) PCI, percutaneous coronary
Dyslipidemiac 275 (63.2) 266 (61.0) intervention.
a
Includes patients from the
ACS at presentationd 195 (44.8) 189 (43.3)
TAP-CABG,8 DACAB,9 and POPular
Diabetes 143 (32.9) 143 (32.8) CABG10 trials. See the Methods
Smokinge 114 (26.2) 112 (25.7) section for the full names of the
studies. Definitions and time points
Previous myocardial infarction 92 (21.2) 91 (20.9)
of measurement varied by trial.
Previous PCI 50 (11.5) 65 (14.9) b
History of hypertension or systolic
Chronic kidney diseasef 28 (6.4) 24 (5.5) blood pressure of at least 140 mm
LVEF, median (IQR), %g 58 (51-64) 60 (51-65) Hg and diastolic blood pressure of at
least 90 mm Hg.
Use of cardiopulmonary bypass 297 (68.3) 301 (69.0)
c
Baseline low-density lipoprotein
Endoscopic saphenous vein graft harvestingh 19/415 (4.6) 25/410 (6.1)
cholesterol of at least 69.5 mg/dL
Sequential saphenous vein grafts 320 (73.6) 327 (75.0) (ⱖ1.8 mmol/L).
Grafts d
ST-elevated myocardial infarction,
No. 981 996 non–ST-segment elevation ACS, or
unstable angina.
Graft type e
Current and former smoking and
Saphenous vein grafts 527 (53.7) 537(53.9) includes vaping and use of other
Arterial grafts 454 (46.3) 459 (46.1) tobacco products.
f
Graft target Glomerular filtration rate less than
LAD 407 (41.5) 403 (40.5) 60 mL/min/m2 calculated by the
Chronic Kidney Disease
Saphenous vein grafts 15 (3.7) 16 (4.0) Epidemiology Collaboration
Arterial grafts 392 (96.3) 387 (96.0) formula.
g
Non-LAD 574 (58.5) 593 (59.5) The most recent measurement
before surgery and varied by trial.
Saphenous vein grafts 512 (89.2) 521 (87.9)
h
Changes in denominators indicate
Arterial grafts 62 (10.8) 72 (12.1)
missing data.
Bypass Graft Surgery (TAP-CABG),8 Different Antiplatelet ized to ticagrelor DAPT, and 436 patients (50.1%; 537 saphe-
Therapy Strategy after Coronary Artery Bypass Graft Surgery nous vein grafts) were randomized to aspirin (Table 2). The me-
(DACAB),9 Effect of Ticagrelor on Saphenous Vein Graft Pat- dian treatment duration was 365 days (IQR, 307-365 days) for
ency in Patients undergoing Coronary Artery Bypass Grafting patients in the ticagrelor DAPT group and 364 days (IQR, 315-
Surgery (Popular CABG),10 and Ticagrelor Antiplatelet Therapy 365 days) for patients in the aspirin group. A total of 394 pa-
to Reduce Graft Events and Thrombosis (TARGET).11 The tients (90.6%) in the ticagrelor DAPT group and 400 patients
PRISMA IPD flow diagram is provided in eFigure 2 in the (91.7%) in the aspirin group underwent protocol-defined
Supplement. imaging (eTables 2-4 in the Supplement). Protocol-defined
An overview of the included trials is provided in Table 1. imaging was performed by computed tomographic angiogra-
Two trials8,10 compared ticagrelor DAPT with aspirin, 1 trial11 phy in 789 patients and coronary angiography in 5 patients.
compared ticagrelor monotherapy with aspirin, and 1 trial9 The median time from CABG surgery to imaging was 369 days
compared ticagrelor DAPT and ticagrelor monotherapy with (IQR, 364-375 days) in the ticagrelor DAPT group and 370 days
aspirin. All trials used a 90-mg twice-daily regimen of (IQR, 364-376 days) in the aspirin group.
ticagrelor. A total of 3079 grafts (1668 saphenous vein grafts
and 1411 arterial grafts) in 1316 patients were included in the Primary Outcome
meta-analysis. The primary outcome of saphenous vein graft failure oc-
curred in 11.2% (54 of 481) of saphenous vein grafts in the ti-
Primary Analysis cagrelor DAPT group and in 20.0% (99 of 494) of saphenous
The primary analysis included 871 patients from the vein grafts in the aspirin group (difference, −8.7% [95% CI,
TAP-CABG,8 DACAB,9 and POPular CABG10 trials. A total of 435 −13.5% to −3.9%], OR, 0.51 [95% CI, 0.35 to 0.74]; P < .001;
patients (49.9%; 527 saphenous vein grafts) were random- Figure 1A).
jama.com (Reprinted) JAMA August 9, 2022 Volume 328, Number 6 557
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
Research Original Investigation Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Bypass Surgery
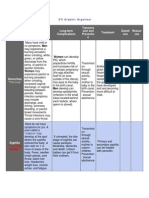
Figure 1. Individual and Pooled Estimates for Saphenous Vein Graft Failure
A Primary outcome: SVG failure per graft
No. of failed SVG/total
No. of SVG (%) Difference, Favors Favors
Source Ticagrelor DAPT Aspirin (95% CI), %a Odds ratio (95% CI)a ticagrelor DAPT aspirin P value
TAP-CABG,8 2016 4/34 (11.7) 15/42 (35.7) –24.0 (–43.7 to –4.2) 0.24 (0.07 to 0.85) .03
DACAB,9 2018 21/226 (9.3) 50/223 (22.4) –14.5 (–22.2 to –6.8) 0.35 (0.19 to 0.63) <.001
POPular CABG,10 2020 29/221 (13.1) 34/229 (14.8) –1.8 (–9.4 to 5.8) 0.87 (0.46 to 1.64) .62
Overall 54/481 (11.2) 99/494 (20.0) –8.7 (–13.5 to –3.9) 0.51 (0.35 to 0.74) <.001
0.1 1 5
Odds ratio (95% CI)
B Secondary outcome: SVG failure per patient
No. of patients with ≥1 failed SVG/
total No. of patients with SVG (%) Difference, Favors Favors
Source Ticagrelor DAPT Aspirin (95% CI), %a Odds ratio (95% CI)a ticagrelor DAPT aspirin P value
TAP-CABG,8 2016 4/19 (21.1) 14/23 (60.9) –40.0 (–66.9 to –12.7) 0.17 (0.04 to 0.72) .02
DACAB,9 2018 20/157 (12.7) 45/153 (29.4) –16.7 (–25.6 to –7.8) 0.35 (0.20 to 0.63) <.001
POPular CABG,10 2020 28/218 (12.8) 33/224 (14.7) –1.9 (–8.3 to 4.5) 0.85 (0.50 to 1.47) .57
Overall 52/394 (13.2) 92/400 (23.0) –9.7 (–14.9 to –4.4) 0.51 (0.35 to 0.74) <.001
0.1 1 5
Odds ratio (95% CI)
a
Adjusted by trial.
DAPT indicates dual antiplatelet therapy; SVG, saphenous vein graft.
Secondary Outcomes The association of ticagrelor DAPT with the risk of saphe-
When assessed per patient, saphenous vein graft failure oc- nous vein graft failure was consistent across all prespecified
curred in 13.2% (52 of 394) of patients in the ticagrelor DAPT subgroups (Figure 3).
group and 23.0% (92 of 400) of patients in the aspirin group
(difference, −9.7% [95% CI, −14.9% to −4.4%]; OR, 0.51 [95% Post Hoc Outcomes
CI, 0.35 to 0.74]; P < .001; Figure 1B). Ticagrelor DAPT was associated with a significantly lower
Ticagrelor DAPT was associated with a significantly higher risk of saphenous vein graft occlusion than was aspirin (9.6%
risk of BARC type 2, 3, or 5 bleeding events compared with as- vs 16.2%; difference, −6.6% [95% CI, −11.0% to −2.2%]; OR,
pirin (22.1% vs 8.7%, difference; 13.3% [95% CI, 8.6% to 18.0%]; 0.55 [95% CI, 0.37 to 0.82]; P = .003) (eFigure 6 in the
OR, 2.98 [95% CI, 1.99 to 4.47]; P < .001) (Figure 2A; eFig- Supplement).
ure 3 in the Supplement). Ticagrelor DAPT was associated with The results of the post hoc analyses for any graft failure
a significantly lower risk of the composite of saphenous vein were consistent with the main analysis (eTable 6 in the Supple-
graft failure or cardiovascular death compared with aspirin ment). The association of ticagrelor DAPT with any graft fail-
(13.9% vs 23.4%: difference, −9.4% [95% CI, −14.7% to −4.1%]; ure remained consistent when stratified by graft type and tar-
OR, 0.52 [95% CI, 0.36 to 0.76]; P < .001) but was not signifi- get vessel territory (eFigure 7 in the Supplement).
cantly associated with lower risk of MACCE (6.7% vs 5.5%; dif- The association of ticagrelor DAPT with bleeding events
ference, 1.2% [95% CI, −2.0% to 4.3%]; HR, 1.21 [95% CI, 0.70 is shown in Figure 2 and eFigure 3 in the Supplement. There
to 2.08]; P = .50; Figure 2B). were no instances of BARC type 5 bleeding events. The asso-
ciation of ticagrelor DAPT with the risk of BARC type 2, 3, or 5
Prespecified Sensitivity and Subgroup Analyses bleeding events was consistent across important clinical sub-
The results for the primary outcome were confirmed in the sen- groups (eFigure 8 in the Supplement). Ticagrelor DAPT was not
sitivity analysis for saphenous vein graft failure per anasto- associated with significant differences in the individual com-
mosis (ticagrelor DAPT vs aspirin, 8.6% vs 14.6%; difference, ponents of MACCE or MACE (Figure 2).
−6.1% [95% CI, −9.9% to −2.4%]; OR, 0.54 [95% CI, 0.37 to Ticagrelor DAPT was associated with a significantly lower
0.80]; P < .001; eFigure 4 in the Supplement) and in the sen- risk of net adverse events than was aspirin (17.0% vs 27.8%;
sitivity analysis that included only patients with protocol- difference, −10.6% [95% CI, −16.3% to −4.9%]; OR, 0.53 [95%
defined imaging at 1 year (eFigure 5 in the Supplement). Sen- CI, 0.38 to 0.75]; P < .001) but was not associated with signifi-
sitivity analyses for the primary outcome in the as-treated and cant differences in net adverse major clinical events or over-
per-protocol populations and after imputation of missing data all net adverse events (eTable 7 in the Supplement).
were also consistent with the main analysis (eTable 5 in the In the network meta-analysis with aspirin as the refer-
Supplement). ence group, ticagrelor DAPT was associated with a significantly
558 JAMA August 9, 2022 Volume 328, Number 6 (Reprinted) jama.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Bypass Surgery Original Investigation Research
Figure 2. Pooled Estimates for Bleeding Events and Cardiovascular Events
A Bleeding events
Bleeding Academic No. of patients with event/ Favors
Research Consortium total No. of patients (%) Difference, ticagrelor Favors
typea Ticagrelor DAPT Aspirin (95% CI), %b Odds ratio (95% CI)b DAPT aspirin P value
2-5c 97/435 (22.3) 38/436 (8.7) 13.5 (8.8 to 18.2) OR 3.02 (2.02 to 4.54) <.001
2, 3, or 5d 96/452 (22.1) 38/436 (8.7) 13.3 (8.6 to 18.0) OR 2.98 (1.99 to 4.47) <.001
3-5c 10/435 (2.3) 8/436 (1.8) 0.5 (–1.4 to 2.3) OR 1.25 (0.49 to 3.22) .64
3 or 5c 8/435 (1.8) 8/436 (1.8) 0.0 (–1.8 to 1.8) OR 1.00 (0.37 to 2.69) .99
0.1 1 10 60
Odds ratio (95% CI)
B Cardiovascular events
No. of patients with event/ Favors
total No. of patients (%) Difference, Odds or hazard ticagrelor Favors
Outcome Ticagrelor DAPT Aspirin (95% CI), %b ratio (95% CI)b DAPT aspirin P value
SVG failure or CV deathd 55/397 (13.9) 94/402 (23.4) –9.4 (–14.7 to –4.1) OR 0.52 (0.36 to 0.76) <.001
MACCEd,e 29/435 (6.7) 24/436 (5.5) 1.2 (–2.0 to 4.3) HR 1.21 (0.70 to 2.08) .50
All-cause deathc 9/435 (2.1) 4/436 (0.9) 1.2 (–0.5 to 2.8) HR 2.26 (0.70 to 7.35) .17
CVf 3/435 (0.7) 3/436 (0.7) 0.0 (–1.1 to –1.1) HR 1.01 (0.20 to 4.99) .99
Non-CVf 6/435 (1.4) 1/436 (0.2) 1.2 (0.0 to 2.3) HR 6.03 (0.73 to 50.05) .10
Myocardial infarctionc 8/435 (1.8) 6/436 (1.4) 0.5 (–1.2 to 2.1) HR 1.35 (0.47 to 3.88) .60
Strokec 6/435 (1.4) 11/436 (2.5) –1.2 (-3.0 to 0.7) HR 0.55 (0.20 to 1.47) .22
Revascularizationc 12/435 (2.8) 7/436 (1.6) 1.0 (–7.9 to 3.1) HR 1.74 (0.69 to 4.43) .26
MACEc,g 16/435 (3.7) 20/436 (4.6) –0.9 (–3.6 to 1.7) HR 0.80 (0.42 to 1.55) .48
0.1 1 10 60
Odds or hazard ratio (95% CI)
a b
Type 0 indicates no bleeding; type 1, bleeding that is not actionable and does Adjusted by trial.
not cause the patient to seek unscheduled performance of studies, c
Post hoc outcomes.
hospitalization, or treatment; type 2, any overt, actionable sign of hemorrhage d
Secondary outcome.
(eg, bleeding that does not fit type 3, 4, or 5 criteria but meets at least 1 of the
e
following: [1] requires nonsurgical medical intervention, [2] leads to Defined as the composite of all-cause death, myocardial infarction, stroke, or
hospitalization or increased level of care, or [3] prompts evaluation); type 3a, revascularization.
overt bleeding plus hemoglobin drop of 3 to 5 g/dL (provided hemoglobin f
Additional outcomes.
drop is related to the bleeding event) or any transfusion with overt bleeding; g
Defined as the composite of cardiovascular death, myocardial infarction, or
3b, overt bleeding plus hemoglobin drop of 5 g/dL (provided hemoglobin drop
stroke.
is related to the bleeding event), cardiac tamponade, bleeding requiring
surgical intervention for control (excluding dental, nasal, skin, or hemorrhoid), Includes patients from the TAP-CABG,8 DACAB,9 and POPular CABG10 trials.
and bleeding requiring intravenous vasoactive agents; 3c, intracranial See the Methods section for the full names of the studies.
hemorrhage (does not include microbleeds or hemorrhagic transformation, CV indicates cardiovascular; DAPT, dual antiplatelet therapy; HR, hazard ratio;
does include intraspinal), subcategories confirmed by autopsy or imaging or MACCE, major adverse cardiac and cerebrovascular event; MACE, major
lumbar puncture, intraocular bleed compromising vision; type 4, coronary adverse cardiovascular event; OR, odds ratio; SVG, saphenous vein graft.
artery bypass graft surgery–related bleeding; and type 5, fatal bleeding.
lower risk of saphenous vein graft failure per graft (OR, 0.49
[95% CI, 0.27 to 0.87]) whereas ticagrelor monotherapy was Discussion
not (OR, 0.94 [95% CI, 0.51 to 1.74]; I2 = 55.4%; eFigure 9 in
the Supplement). In this individual patient data meta-analysis of 4 RCTs includ-
ing 1316 patients and 1668 saphenous vein grafts, ticagrelor
Supplementary Analysis DAPT was associated with a significantly lower risk of saphe-
Ticagrelor monotherapy was not associated with a signifi- nous vein graft failure and a significantly higher risk of clini-
cant difference in saphenous vein graft failure compared with cally important bleeding events than was aspirin.
aspirin per graft (19.3% vs 21.7%; difference, −2.6% [95% CI, CABG surgery is the treatment of choice for patients
−9.1% to 3.9%]; OR, 0.86 [95% CI, 0.58 to 1.27]; P = .44) or per with high-complexity coronary artery disease and those with
patient (25.2% vs 29.3%; difference, −4.1% [95% CI, −11.9% to reduced left ventricular ejection fraction.6 In the US alone
3.7%]; OR, 0.81 [95% CI, 0.55 to 1.20]; P = .30; eTable 8 in the approximately 300 000 patients undergo CABG surgery
Supplement). There was no significant difference between ti- annually.17 The saphenous vein is used in more than 90% of
cagrelor monotherapy and aspirin in the association with BARC CABG procedures.18
type 2, 3, or 5 bleeding events (8.9% vs 7.3%; difference, 1.7%; RCTs investigating the effect of ticagrelor DAPT vs aspi-
[95% CI, −2.8% to 6.1%]; OR, 1.25 [95% CI, 0.69 to 2.29]; P = .46; rin on saphenous vein graft failure have reported conflicting
eTable 9 in the Supplement). results. In the DACAB trial,9 ticagrelor DAPT significantly
jama.com (Reprinted) JAMA August 9, 2022 Volume 328, Number 6 559
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
Research Original Investigation Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Bypass Surgery
Figure 3. Saphenous Vein Graft Failure in Subgroups
No. of failed SVG/
total No. of SVG (%) Difference, Odds ratio Favors Favors
Ticagrelor DAPT Aspirin (95% CI), %a (95% CI)a ticagrelor DAPT aspirin P value
Age, y
>65 28/253 (11.1) 61/270 (22.6) –11.0 (–17.7 to –4.2) 0.43 (0.26 to 0.72)
.37
≤65 26/228 (11.4) 38/224 (17.0) –6.1 (–12.9 to 0.07) 0.62 (0.35 to 1.09)
Sex
Women 10/71 (14.1) 10/70 (14.3) 1.4 (–12.0 to 14.8) 1.03 (0.35 to 3.08)
.15
Men 44/410 (10.7) 89/424 (21.0) –10.2 (–15.4 to –5.1) 0.46 (0.30 to 0.68)
Diabetesb
Yes 19/168 (11.3) 43/164 (26.2) –14.7 (–23.5 to –5.8) 0.36 (0.19 to 0.68)
.16
No 35/313 (11.1) 56/330 (17.0) –5.8 (–11.5 to –0.1) 0.62 (0.39 to 0.99)
Smoking
Yes 13/137 (9.5) 26/132 (19.7) –10.4 (–19.1 to –1.6) 0.43 (0.20 to 0.89)
.58
No 41/344 (11.9) 73/362 (20.2) –8.0 (–13.7 to –2.3) 0.54 (0.35 to 0.84)
ACSc
Yes 25/238 (10.5) 44/227 (19.4) –9.2 (–16.1 to –2.2) 0.48 (0.27 to 0.84)
.83
No 29/243 (11.9) 55/267 (20.6) –8.5 (–15.2 to –1.8) 0.53 (0.32 to 0.88)
Use of CPB
Yes 33/331 (10.0) 55/357 (15.4) –4.8 (–10.1 to 0.5) 0.62 (0.38 to 1.02)
.15
No 21/150 (14.0) 44/137 (32.1) –18.1 (–28.0 to –8.3) 0.34 (0.19 to 0.63)
Sequential SVGd
Yes 41/287 (14.3) 70/304 (23.0) –8.6 (–16.1 to –1.0) 0.56 (0.33 to 0.93)
.41
No 13/194 (6.7) 29/190 (15.3) –8.7 (–15.5 to –1.9) 0.40 (0.19 to 0.84)
0.1 1 5
Odds ratio (95% CI)
c
Subgroup analyses for harvesting technique and target vessel territory could Includes ST-segment elevation myocardial infarction, non–ST-segment
not be performed due to the limited number of events in the endoscopic- elevation ACS, or unstable angina. Definitions varied by trial.
harvesting group and left anterior descending coronary artery territory group. d
Defined as saphenous vein grafts with more than 1 anastomosis.
Treatment duration varied in 1 trial only. Includes patients from the TAP-CABG,8 DACAB,9 and POPular CABG10 trials.
a
Adjusted by trial. See the Methods section for the full names of the studies.
b ACS indicates acute coronary syndrome; CPB, cardiopulmonary bypass;
Self-reported diagnosis, elevated hemoglobin A1c levels, or active therapy.
Definitions varied by trial. DAPT, dual antiplatelet therapy; SVG, saphenous vein graft.
increased saphenous vein graft patency 1 year after CABG. greatly limits the clinical relevance of the results from trial-
In contrast, in the POPular CABG trial,10 ticagrelor DAPT did level meta-analyses.
not significantly reduce saphenous vein graft occlusion 1 year In the present work, graft failure and bleeding events were
after CABG surgery. The TAP-CABG trial8 also did not find a readjudicated using a common definition before pooling, al-
significant difference in the absolute risk of saphenous vein lowing generation of homogeneous pooled estimates of the as-
graft occlusion between ticagrelor DAPT and aspirin 3 months sociation of ticagrelor DAPT with saphenous vein graft fail-
after CABG. ure and bleeding events.
In addition, the published RCTs were all individually un- This comprehensive synthesis of all RCTs with angio-
derpowered to detect even moderate differences in bleeding graphic follow-up provides solid evidence that ticagrelor DAPT
outcomes. Although they did not individually report an in- is associated with a significantly lower risk of saphenous vein
crease in major bleeding events with ticagrelor DAPT,8-10 a solid graft failure 1 year after CABG surgery. The association of ti-
estimate of the risk to benefit ratio of ticagrelor DAPT after cagrelor DAPT with the risk of saphenous vein graft failure was
CABG surgery was not possible. consistent across subgroups. However, compared with aspi-
An aggregate network meta-analysis of 20 RCTs that as- rin, ticagrelor DAPT was also associated with a significantly
sessed the effects of oral antithrombotic drugs and included higher risk of BARC type 2 or higher bleeding events. There was
2 RCTs (203 patients) comparing ticagrelor DAPT with aspirin also an absolute increase in the risk of all-cause death in the
did not show a significant difference in major bleeding events ticagrelor DAPT group, although not statistically significant.
between the groups (OR, 1.93 [95% CI, 0.30-12.4]).19 In an- Taken together, the present analysis suggests that a patient’s
other meta-analysis of 5 RCTs and 3996 patients, there was no individual risk of graft failure, ischemic events, and bleeding
significant difference in the risk of bleeding between ticagrelor– needs to be weighed carefully when deciding whether to add
based antiplatelet therapy vs aspirin and/or clopidogrel (rela- ticagrelor to aspirin after CABG surgery. Longer-term follow-up
tive risk, 1.04 [95% CI, 0.95-1.14]; P = .41).20 However, indi- is required to fully evaluate a potential benefit of ticagrelor
vidual studies used different bleeding definitions and this DAPT on clinical events.21
560 JAMA August 9, 2022 Volume 328, Number 6 (Reprinted) jama.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Bypass Surgery Original Investigation Research
Individual RCTs investigating the effect of ticagrelor mono- agement across the included RCTs. Third, the duration of ti-
therapy vs aspirin after CABG surgery have not shown an effect cagrelor DAPT and timing of follow-up ranged from 3 to 12
on saphenous vein graft failure but have all been limited by the months across the included RCTs. Fourth, the analysis was not
small sample size.9,11 In this meta-analysis, ticagrelor mono- designed to evaluate differences in clinical outcomes be-
therapy was not associated with a significant difference in the tween groups. Lastly, protocol-directed imaging was missing
risk of saphenous vein graft failure compared with aspirin, but in 9.1% of patients. However, patient characteristics were bal-
the pooled estimate was compatible with a potential benefit of anced across randomization groups for patients who under-
ticagrelor monotherapy. Because ticagrelor monotherapy was went imaging, and the results for the primary outcome were
not associated with a significant difference in the risk of bleed- consistent after multiple imputation of missing data.
ing events compared with aspirin, its role as a treatment option
after CABG surgery requires further investigation.
Conclusions
Limitations
This study has several limitations. First, the pooled analysis In patients undergoing coronary artery bypass graft surgery,
is subject to the limitations of the original RCTs, including the adding ticagrelor to aspirin was associated with a signifi-
open-label treatment allocation in 1 of them, although out- cantly decreased risk of vein graft failure. However, this was
come adjudication was blinded in all RCTs. Second, there was accompanied by a significantly increased risk of clinically im-
heterogeneity in surgical technique and postoperative man- portant bleeding.
ARTICLE INFORMATION Obtained funding: Janssen, Ruel. Research Foundation; receiving personal fees from
Accepted for Publication: June 23,2022. Administrative, technical, or material support: Cine-Med, Janssen, and WebMD; receiving less
Janssen, Ruel, Saw, Soletti, Starovoytov. than 1% of equity in Applied Therapeutics Equity,
Author Affiliations: Department of Cardiac Supervision: Angiolillo, Janssen, Soletti, Elixir Medical, Stel, and ControlRad Equity (spouse)
Surgery, Medical University of Vienna, Vienna, Starovoytov, ten Berg, Willemsen, Gaudino. outside the submitted work; and having other
Austria (Sandner); Weill Cornell Medicine, New Other - protocol review: Willemsen. financial or nonfinancial interests in Boston
York, New York (Sandner); Department of Scientific Corp and divested final stock options of
Cardiology, Sahlgrenska University Hospital, Conflict of Interest Disclosures: Dr Sandner
reported receiving institutional research grants less than 1% in Claret Medical. Dr Saw reported
Gothenburg, Sweden (Redfors); Division of receiving grants from AstraZeneca outside the
Cardiology, University of Florida College of from Vascular Grafts Solutions outside the
submitted work. Dr Angiolillo reported receiving submitted work and serving as the principal
Medicine, Jacksonville (Angiolillo); Department of investigator for the TAP-CABG study. Dr ten Berg
Cardiothoracic Surgery, Weill Cornell Medicine, consulting fees or honoraria from Abbott, Amgen,
AstraZeneca, Bayer, Biosensors, Boehringer reported receiving speaker fees from AstraZeneca,
New York, New York (Audisio, Soletti, Gaudino); Bayer, Boehringer Ingelheim, and Celecor and
Schulich Heart Centre, Sunnybrook Health Sciences Ingelheim, Bristol Myers Squibb, Chiesi,
Daiichi-Sankyo, Eli Lilly, Haemonetics, Janssen, institutional research grants from AstraZeneca and
Centre, University of Toronto, Toronto, Ontario, ZonMw. Dr Willemsen reported receiving grants
Canada (Fremes); Institute of Health Policy Merck, PhaseBio, PLx Pharma, Pfizer, and Sanofi;
and research grants to his institution from Amgen, from AstraZeneca funding of the POPular CABG
Management and Evaluation, University of Toronto, trial during the conduct of the study. Dr Zhao
Toronto, Ontario, Canada (Fremes); Department of AstraZeneca, Bayer, Biosensors, CeloNova, CSL
Behring, Daiichi-Sankyo, Eisai, Eli Lilly, Gilead, reported receiving grants from AstraZeneca during
Cardiology, St Antonius Hospital, Nieuwegein, the the conduct of the study and from Chugai Pharma
Netherlands (Janssen, Peper, ten Berg, Willemsen); Janssen, Matsutani Chemical Industry Co, Merck,
Novartis, Osprey Medical, Renal Guard Solutions, China outside the submitted work. Dr Zhu reported
Division of Cardiac Surgery, Boca Raton Regional receiving personal fees from Chugai Pharma China
Hospital and Florida Atlantic Hospital, Boca Raton and the Scott R. MacKenzie Foundation. Dr Janssen
reported receiving grants from AstraZeneca outside the submitted work. No other disclosures
(Kulik); Zena and Michael A. Wiener Cardiovascular were reported.
Institute, Icahn School of Medicine at Mount Sinai, funding for the POPular CABG trial during the
New York, New York (Mehran); Division of Cardiac conduct of the study. Dr Kulik reported receiving Funding/Support: This study was supported using
Surgery, University of Ottawa Heart Institute, grants from AstraZeneca during the conduct of the internal funds from the Department of
Ottawa, Ontario, Canada (Ruel); Division of study. Dr Mehran reported receiving research Cardiothoracic Surgery at Weill Cornell Medicine,
Cardiology, Vancouver General Hospital, British grants from Abbott, Abiomed, Alleviant Medical, New York.
Columbia, Canada (Saw, Starovoytov); Division of AM-Pharma, Applied Therapeutics, Arena, Role of the Funder/Sponsor: The funder had no
Cardiology St Paul’s Hospital, University of British AstraZeneca, Bayer, Beth Israel Deaconess, role in the design and conduct of the study;
Columbia, Vancouver, Canada (Saw); Ruijin Hospital Biosensors, Biotronik, Bristol Myers Squibb, Boston collection, management, analysis, and
Shanghai Jiao Tong University School of Medicine, Scientific Research, CardiaWave Research, interpretation of the data; preparation, review, or
Shanghai, China (Zhao, Zhu). CellAegis, CeloNova, CERC, Chiesi, Concept approval of the manuscript; and decision to submit
Medical, CSL Behring, Daiichi Sankyo Inc, Duke the manuscript for publication.
Author Contributions: Drs Sandner and Redfors University, Humacyte, Idorsa Pharmaceuticals, Insel
had full access to all of the data in the study and Gruppe AG, Janssen, Medtronic, Novartis,
take responsibility for the integrity of the data and REFERENCES
OrbusNeich, Philips, Vivasure, and Zoll, all to her
the accuracy of the data analysis. Drs Sandner and institution; serving as a consultant to the California 1. Antonopoulos AS, Odutayo A, Oikonomou EK,
Redfors contributed equally. Institute for Regenerative Medicine; serving on the et al; SAFINOUS-CABG (Saphenous Vein Graft
Concept and design: Sandner, Fremes, Mehran, scientific advisory board of the American Medical Failure—An Outcomes Study in Coronary Artery
Peper, Ruel, Zhao, Zhu, Gaudino. Association; serving on the advisory boards of Bypass Grafting) group. Development of a risk
Acquisition, analysis, or interpretation of data: CERC (Biosnsors), Abbott, Arena, Biotronik, score for early saphenous vein graft failure: an
Sandner, Redfors, Angiolillo, Audisio, Fremes, CardiaWave, Chiesi, Concept Medical, Humacyte, individual patient data meta-analysis. J Thorac
Janssen, Kulik, Peper, Ruel, Saw, Soletti, Magenta, Novartis, and Philips, all to her institution; Cardiovasc Surg. 2020;160(1):116-127.e4. doi:10.
Starovoytov, ten Berg, Willemsen, Gaudino. serving on the board of the American College of 1016/j.jtcvs.2019.07.086
Drafting of the manuscript: Sandner, Redfors, Kulik, Cardiology, and as a committee member of the 2. Xenogiannis I, Zenati M, Bhatt DL, et al.
Gaudino. Women in Innovations of the Society for Saphenous vein graft failure: from pathophysiology
Critical revision of the manuscript for important Cardiovascular Angiography, all to her institution; to prevention and treatment strategies. Circulation.
intellectual content: All authors. serving as an unpaid faculty of the Cardiovascular
Statistical analysis: Redfors, Kulik, Gaudino.
jama.com (Reprinted) JAMA August 9, 2022 Volume 328, Number 6 561
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
Research Original Investigation Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Bypass Surgery
2021;144(9):728-745. doi:10.1161/CIRCULATIONAHA. 9. Zhao Q, Zhu Y, Xu Z, et al. Effect of ticagrelor June 14, 2022. https://documentation.sas.com/api/
120.052163 plus aspirin, ticagrelor alone, or aspirin alone on collections/pgmsascdc/9.4_3.3/docsets/statug/
3. Gaudino M, Antoniades C, Benedetto U, et al; saphenous vein graft patency 1 year after coronary content/glimmix.pdf?locale=en#nameddest=
ATLANTIC (Arterial Grafting International artery bypass grafting: a randomized clinical trial. statug_glimmix_syntax01
Consortium) Alliance. Mechanisms, consequences, JAMA. 2018;319(16):1677-1686. doi:10.1001/jama. 16. Network Meta-Analysis Using Frequentist
and prevention of coronary graft failure. Circulation. 2018.3197 Methods. R version 2.5-0; July 11, 2022. Accessed
2017;136(18):1749-1764. doi:10.1161/ 10. Willemsen LM, Janssen PWA, Peper J, et al. June 14, 2022. https://cran.r-project.org/web/
CIRCULATIONAHA.117.027597 Effect of adding ticagrelor to standard aspirin on packages/netmeta/netmeta.pdf
4. Chakos A, Jbara D, Singh K, Yan TD, Tian DH. saphenous vein graft patency in Patients 17. Bowdish ME, D’Agostino RS, Thourani VH, et al.
Network meta-analysis of antiplatelet therapy Undergoing Coronary Artery Bypass Grafting STS adult cardiac surgery database: 2021 update on
following coronary artery bypass grafting (CABG): (POPular CABG): a randomized, double-blind, outcomes, quality, and research. Ann Thorac Surg.
none versus one versus two antiplatelet agents. placebo-controlled trial. Circulation. 2020;142(19): 2021;111(6):1770-1780. doi:10.1016/j.athoracsur.2021.
Ann Cardiothorac Surg. 2018;7(5):577-585. doi:10. 1799-1807. doi:10.1161/CIRCULATIONAHA.120. 03.043
21037/acs.2018.09.02 050749
18. Schwann TA, Habib RH, Wallace A, et al.
5. Sousa-Uva M, Neumann FJ, Ahlsson A, et al; 11. Kulik A, Abreu AM, Boronat V, Kouchoukos NT, Operative outcomes of multiple-arterial versus
ESC Scientific Document Group. 2018 ESC/EACTS Ruel M. Ticagrelor versus aspirin and vein graft single-arterial coronary bypass grafting. Ann Thorac
guidelines on myocardial revascularization. Eur J patency after coronary bypass: a randomized trial. Surg. 2018;105(4):1109-1119. doi:10.1016/j.
Cardiothorac Surg. 2019;55(1):4-90. doi:10.1093/ J Card Surg. 2022;37(3):563-570. doi:10.1111/jocs. athoracsur.2017.10.058
ejcts/ezy289 16189
19. Solo K, Lavi S, Kabali C, et al. Antithrombotic
6. Lawton JS, Tamis-Holland JE, Bangalore S, et al; 12. Stewart LA, Clarke M, Rovers M, et al; treatment after coronary artery bypass graft
Writing Committee Members. 2021 ACC/AHA/SCAI PRISMA-IPD Development Group. Preferred surgery: systematic review and network
guideline for coronary artery revascularization: Reporting Items for Systematic Review and meta-analysis. BMJ. 2019;367:l5476. doi:10.1136/
a report of the American College of Meta-Analyses of individual participant data: the bmj.l5476
Cardiology/American Heart Association Joint PRISMA-IPD Statement. JAMA. 2015;313(16):1657-
1665. doi:10.1001/jama.2015.3656 20. von Scheidt M, Bongiovanni D, Tebbe U, et al.
Committee on Clinical Practice Guidelines. J Am Coll Ticagrelor-based antiplatelet regimens in patients
Cardiol. 2022;79(2):e21-e129. doi:10.1016/j.jacc. 13. Mehran R, Rao SV, Bhatt DL, et al. Standardized treated with coronary artery bypass grafting:
2021.09.006 bleeding definitions for cardiovascular clinical trials: a meta-analysis of randomized controlled trials. Eur
7. Angiolillo DJ, Galli M, Collet JP, Kastrati A, a consensus report from the Bleeding Academic J Cardiothorac Surg. 2020;57(3):520-528. doi:10.
O’Donoghue ML. Antiplatelet therapy after Research Consortium. Circulation. 2011;123(23): 1093/ejcts/ezz260
percutaneous coronary intervention. 2736-2747. doi:10.1161/CIRCULATIONAHA.110.
009449 21. Steg PG, Bhatt DL, Simon T, et al; THEMIS
EuroIntervention. 2022;17(17):e1371-e1396. doi:10. Steering Committee and Investigators. Ticagrelor in
4244/EIJ-D-21-00904 14. Sterne JAC, Savović J, Page MJ, et al. RoB 2: patients with stable coronary disease and diabetes.
8. Saw J, Wong GC, Mayo J, et al. Ticagrelor and a revised tool for assessing risk of bias in N Engl J Med. 2019;381(14):1309-1320. doi:10.1056/
aspirin for the prevention of cardiovascular events randomised trials. BMJ. 2019;366:l4898. doi:10. NEJMoa1908077
after coronary artery bypass graft surgery. Heart. 1136/bmj.l4898
2016;102(10):763-769. doi:10.1136/heartjnl-2015- 15. SAS/STAT 14.3 User’s Guide: the GLIMMIX
308691 Procedure. SAS Institute Inc; 2017. Accessed
562 JAMA August 9, 2022 Volume 328, Number 6 (Reprinted) jama.com
© 2022 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by Narayan Rao V Tummala on 08/11/2022
You might also like
- 1638.fullDocument8 pages1638.fulldps_1976No ratings yet
- CirculationahaDocument11 pagesCirculationahamony saNo ratings yet
- Jama Gaudino 2020 Oi 200052Document9 pagesJama Gaudino 2020 Oi 200052Peter Vidal jrNo ratings yet
- Article Final Examination SN-27-Sep-2021Document43 pagesArticle Final Examination SN-27-Sep-2021Natwara KaloyNo ratings yet
- Version of Record:: ManuscriptDocument23 pagesVersion of Record:: Manuscriptmiko balisiNo ratings yet
- 0178959e6a78&ie SdarticleDocument7 pages0178959e6a78&ie SdarticleRiza Adi SaputraNo ratings yet
- Antithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextDocument12 pagesAntithrombotic Therapy After Revascularization in Patients With Peripheral Arterial Disease: What Is Here, What Is NextenviNo ratings yet
- Bleeding and Ischemic Risks of Ticagrelor Monotherapy After Coronary InterventionsDocument14 pagesBleeding and Ischemic Risks of Ticagrelor Monotherapy After Coronary InterventionsKardiologi ManadoNo ratings yet
- Editorial 2Document4 pagesEditorial 2david1086No ratings yet
- De Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IDocument43 pagesDe Escalation From Ticagrelor To Clopidogrel in Patients With Acute Myocardial IAkhmad HidayatNo ratings yet
- Schwartz 2010Document4 pagesSchwartz 2010Edson CarneiroNo ratings yet
- Antithrombotic Therapy After Transcatheter Aortic Valve ReplacementDocument15 pagesAntithrombotic Therapy After Transcatheter Aortic Valve ReplacementChris SoilworkNo ratings yet
- 1 s2.0 S0002870321004427 MainDocument10 pages1 s2.0 S0002870321004427 MainJair BasantesNo ratings yet
- Ticagrelor in Patients With Stable Coronary Disease and DiabetesDocument11 pagesTicagrelor in Patients With Stable Coronary Disease and DiabetesPaulo VictorNo ratings yet
- 2719-Article Text Orig-23698-1-10-20210712Document2 pages2719-Article Text Orig-23698-1-10-20210712Oeij Henri WijayaNo ratings yet
- JCCR 06 00205Document3 pagesJCCR 06 00205Oeij Henri WijayaNo ratings yet
- Stroke CADISSDocument8 pagesStroke CADISSInge Dackrisna DaudNo ratings yet
- Articles: BackgroundDocument12 pagesArticles: BackgroundStefania CristinaNo ratings yet
- Nejmoa 2206606Document10 pagesNejmoa 2206606dipan diratuNo ratings yet
- Endovascular Treatment of Femoropopliteal Arterial Occlusive Disease - Current Techniques and LimitationsDocument10 pagesEndovascular Treatment of Femoropopliteal Arterial Occlusive Disease - Current Techniques and Limitationsafso afsoNo ratings yet
- CABANADocument14 pagesCABANAIsmael Rivera DiazNo ratings yet
- Cabg Surgery Perspectives3Document36 pagesCabg Surgery Perspectives3meenakshi sundaramNo ratings yet
- The Hybrid Coronary Approach For Optimal Revascularization: JACC Review Topic of The WeekDocument13 pagesThe Hybrid Coronary Approach For Optimal Revascularization: JACC Review Topic of The WeekAhmad FauzanNo ratings yet
- 1 s2.0 S0735109719300956 MainDocument9 pages1 s2.0 S0735109719300956 MainAlberto PolimeniNo ratings yet
- ACO Peripro 2016Document10 pagesACO Peripro 2016Philippe Bocanegra FernándezNo ratings yet
- Jama You 2020 Oi 200094 1603319690.60891Document11 pagesJama You 2020 Oi 200094 1603319690.60891edo adimastaNo ratings yet
- Fana Alemseged Endovascular Thrombectomy For Basil - 231118 - 114208Document8 pagesFana Alemseged Endovascular Thrombectomy For Basil - 231118 - 114208Luis Guilherme ScalianteNo ratings yet
- Fsurg 10 1285553Document11 pagesFsurg 10 1285553William ChokNo ratings yet
- Ticagrelor With or Without Aspirin in High-Risk Patients After PCIDocument11 pagesTicagrelor With or Without Aspirin in High-Risk Patients After PCIAdane PetrosNo ratings yet
- Pi Is 0007091217540015Document10 pagesPi Is 0007091217540015Yoga WibowoNo ratings yet
- Doac Vs AvkDocument32 pagesDoac Vs AvkOlga BabiiNo ratings yet
- Effect of Ticagrelor Plus Aspirin, Ticagrelor Alone, or Aspirin Alone On Saphenous Vein Graft Patency 1 Year After Coronary Artery Bypass Grafting A Randomized Clinical TrialDocument10 pagesEffect of Ticagrelor Plus Aspirin, Ticagrelor Alone, or Aspirin Alone On Saphenous Vein Graft Patency 1 Year After Coronary Artery Bypass Grafting A Randomized Clinical TrialMr. LNo ratings yet
- Thrombosis Research: Regular ArticleDocument4 pagesThrombosis Research: Regular ArticleDavy JonesNo ratings yet
- Jama Kamel 2024 Oi 230163 1706898479.89128Document9 pagesJama Kamel 2024 Oi 230163 1706898479.89128Srinivas PingaliNo ratings yet
- Lancet CABG in Patients With Diabetes and Multivessel Diseas (Commento 10 Marzo)Document2 pagesLancet CABG in Patients With Diabetes and Multivessel Diseas (Commento 10 Marzo)Mr. LNo ratings yet
- Short - and Long-Term Outcomes at A Single InstitutionDocument7 pagesShort - and Long-Term Outcomes at A Single InstitutionJonathan Frimpong AnsahNo ratings yet
- Packer 2019Document14 pagesPacker 2019Renata D GNo ratings yet
- Complications After Peripheral Vascular Interventions in OctogenariansDocument7 pagesComplications After Peripheral Vascular Interventions in OctogenariansIrina NeamtuNo ratings yet
- Non Vitamin K Antagonist Oral Anticoagulation The Future of Anticoagulation Following Mitral Reparative SurgeryDocument3 pagesNon Vitamin K Antagonist Oral Anticoagulation The Future of Anticoagulation Following Mitral Reparative SurgeryPaul HartingNo ratings yet
- PIIS0003497509012442Document5 pagesPIIS0003497509012442Tri RachmadijantoNo ratings yet
- Endovascular Solution in Peripheral Artery DiseaseDocument36 pagesEndovascular Solution in Peripheral Artery DiseaseArintia AubreyNo ratings yet
- Chowdhury-Secemsky2022 Article AtherectomyVsOtherModalitiesFoDocument9 pagesChowdhury-Secemsky2022 Article AtherectomyVsOtherModalitiesFoEnrique San NorbertoNo ratings yet
- Preliminary Experience With Cangrelor For Endovascular Treatment ofDocument9 pagesPreliminary Experience With Cangrelor For Endovascular Treatment ofPedro VillamorNo ratings yet
- Pci Versus Cabg in Cad, Serruys (2009)Document12 pagesPci Versus Cabg in Cad, Serruys (2009)Henrique MachadoNo ratings yet
- jamaneurology_liang_2023_oi_230009_1678913710.52029Document8 pagesjamaneurology_liang_2023_oi_230009_1678913710.52029nazar shekhoNo ratings yet
- Carotid Angioplasty and Stent-Induced Bradycardia and Hypotension: Impact of Prophylactic Atropine Administration and Prior Carotid EndarterectomyDocument6 pagesCarotid Angioplasty and Stent-Induced Bradycardia and Hypotension: Impact of Prophylactic Atropine Administration and Prior Carotid EndarterectomyIndia SunshineNo ratings yet
- Carotid Artrey DiseaseDocument6 pagesCarotid Artrey DiseaseOnon EssayedNo ratings yet
- Multivessel CADDocument4 pagesMultivessel CADJohn HetharieNo ratings yet
- Recent Advances and Future Trends in Cardiology: Upendra Kaul, Parneesh AroraDocument4 pagesRecent Advances and Future Trends in Cardiology: Upendra Kaul, Parneesh Arorashamir naazNo ratings yet
- The Cleveland Clinic Experience From 89 To 98Document10 pagesThe Cleveland Clinic Experience From 89 To 98Vlad NeagoeNo ratings yet
- Syntax ScoreDocument10 pagesSyntax ScoreInggitaDarmawanNo ratings yet
- Blah 5 AsdsadsaDocument5 pagesBlah 5 Asdsadsaprern27No ratings yet
- Aca 19 225Document6 pagesAca 19 225M Ali AdrianNo ratings yet
- Isar React 5Document11 pagesIsar React 5Pedro JalladNo ratings yet
- Ticagrelor or Prasugrel in Patients With ST-Segment-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention 2020Document9 pagesTicagrelor or Prasugrel in Patients With ST-Segment-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention 2020Juan David Blanco VasquezNo ratings yet
- 1 s2.0 S0272638622009222 MainDocument12 pages1 s2.0 S0272638622009222 MainResidenPatKlin Juli2022No ratings yet
- Left Atrial Appendage Occlusion 1Document37 pagesLeft Atrial Appendage Occlusion 1Antonia AdinaNo ratings yet
- Cortez-Neuroradiology 2020Document10 pagesCortez-Neuroradiology 2020Pedro VillamorNo ratings yet
- Contrast-Induced Acute Kidney Injury: Review Topic of The WeekDocument9 pagesContrast-Induced Acute Kidney Injury: Review Topic of The WeekreioctabianoNo ratings yet
- Transcatheter Aortic Valve Replacement: A How-to Guide for Cardiologists and Cardiac SurgeonsFrom EverandTranscatheter Aortic Valve Replacement: A How-to Guide for Cardiologists and Cardiac SurgeonsNo ratings yet
- s00125-024-06145-0_240426_192850Document12 pagess00125-024-06145-0_240426_192850lakshminivas PingaliNo ratings yet
- Sunday Academic Meet-13 240428 083750Document9 pagesSunday Academic Meet-13 240428 083750lakshminivas PingaliNo ratings yet
- FALLA CARDIACA CON FEVI PRESERVADA 2024(1)Document19 pagesFALLA CARDIACA CON FEVI PRESERVADA 2024(1)MarcoNo ratings yet
- Consequences of Medical Negligence and Litigations.1Document9 pagesConsequences of Medical Negligence and Litigations.1lakshminivas PingaliNo ratings yet
- STATS Annexure-82. B.Sc. (Programme) Mathematical SciencesDocument58 pagesSTATS Annexure-82. B.Sc. (Programme) Mathematical Sciencesatultiwari8No ratings yet
- TRIGONOMETRYDocument23 pagesTRIGONOMETRYAnnisa Musvita SariNo ratings yet
- s00125-024-06145-0_240426_192850Document12 pagess00125-024-06145-0_240426_192850lakshminivas PingaliNo ratings yet
- Annexure-74. (B.sc. (Hons) Maths (REVISED)Document86 pagesAnnexure-74. (B.sc. (Hons) Maths (REVISED)hmingthansangiNo ratings yet
- Oer TrigonometryDocument471 pagesOer TrigonometryIman AhmedNo ratings yet
- GLP1RA PregnancyDocument10 pagesGLP1RA Pregnancylakshminivas PingaliNo ratings yet
- ccpc15 Neurocritical Care WorkbookDocument46 pagesccpc15 Neurocritical Care WorkbookJeremy HamptonNo ratings yet
- Atomic Structure Mind MapDocument2 pagesAtomic Structure Mind Maplakshminivas PingaliNo ratings yet
- MCQs in Cardiovascular MedicineDocument144 pagesMCQs in Cardiovascular MedicineRiham Mohye Eldeen MohammedNo ratings yet
- Mi Over DiagnosisDocument2 pagesMi Over Diagnosislakshminivas PingaliNo ratings yet
- Nej Mp 2314068Document3 pagesNej Mp 2314068lakshminivas PingaliNo ratings yet
- Diabetes Obesity Metabolism - 2024 - Kim - Cardiorenal Outcomes and Mortality After Sodium‐Glucose Cotransporter‐2Document11 pagesDiabetes Obesity Metabolism - 2024 - Kim - Cardiorenal Outcomes and Mortality After Sodium‐Glucose Cotransporter‐2lakshminivas PingaliNo ratings yet
- 004Document40 pages004lakshminivas PingaliNo ratings yet
- Malaria in IcuDocument13 pagesMalaria in Iculakshminivas PingaliNo ratings yet
- Nej Mp 2314068Document3 pagesNej Mp 2314068lakshminivas PingaliNo ratings yet
- Nej Mp 2400463Document3 pagesNej Mp 2400463lakshminivas PingaliNo ratings yet
- Mathematics: Full Marks Zero Marks: 0 in All Other CasesDocument31 pagesMathematics: Full Marks Zero Marks: 0 in All Other CasesAbhishek KumarNo ratings yet
- Ivabradine in Septic ShockDocument11 pagesIvabradine in Septic Shocklakshminivas PingaliNo ratings yet
- MCQs in Cardiovascular MedicineDocument144 pagesMCQs in Cardiovascular MedicineRiham Mohye Eldeen MohammedNo ratings yet
- List Suggested Books Indian Authors Publishers PDFDocument52 pagesList Suggested Books Indian Authors Publishers PDFAbhinav GargNo ratings yet
- Cerebral Venous and Dural Sinus Thrombosis (1)Document11 pagesCerebral Venous and Dural Sinus Thrombosis (1)lakshminivas PingaliNo ratings yet
- Dyslipidemia in WomenDocument7 pagesDyslipidemia in Womenlakshminivas PingaliNo ratings yet
- Report Neural InterfacesDocument106 pagesReport Neural Interfaceslakshminivas PingaliNo ratings yet
- PHP Q5 ZGfoDocument13 pagesPHP Q5 ZGfoak978420No ratings yet
- KDBH-LipidManagementDocument1 pageKDBH-LipidManagementlakshminivas PingaliNo ratings yet
- Calculus PDFDocument374 pagesCalculus PDFJonnyy12No ratings yet
- Gouty Arthritis: Presented By: Petit Ivy Mae B. NacarioDocument21 pagesGouty Arthritis: Presented By: Petit Ivy Mae B. NacarioMarivic DianoNo ratings yet
- Disclosures: Kori Dewing, DNP, ARNP Virginia Mason Medical Center October 29, 2013Document3 pagesDisclosures: Kori Dewing, DNP, ARNP Virginia Mason Medical Center October 29, 2013Alexander Diaz ZuletaNo ratings yet
- SpirulinaDocument57 pagesSpirulinaMarcus Gibson100% (4)
- Kami Export - Kenny Frias - Subfields in Psychology Classified Ads 2Document1 pageKami Export - Kenny Frias - Subfields in Psychology Classified Ads 2Kenny FriasNo ratings yet
- Ronald Glick, MD Medical Director-Center For Integrative Medicine at UPMC ShadysideDocument42 pagesRonald Glick, MD Medical Director-Center For Integrative Medicine at UPMC ShadysideAnonymous LXV7Pwp100% (1)
- Medico Central DesignDocument21 pagesMedico Central DesignBiing BeengNo ratings yet
- Clinical Massage Therapy - S. Jurch Hill, 2009) WWDocument562 pagesClinical Massage Therapy - S. Jurch Hill, 2009) WWMohsen Bt92% (12)
- MK Sastry Nada Protocol The Grassroots TreatmentDocument12 pagesMK Sastry Nada Protocol The Grassroots Treatmentwilyanto yangNo ratings yet
- Non CariousDocument4 pagesNon CariousUpasana BhandariNo ratings yet
- History of Reconstructive and Aesthetic SurgeryDocument22 pagesHistory of Reconstructive and Aesthetic SurgeryIde Bagoes Insani100% (2)
- Root ResorptionDocument112 pagesRoot Resorptionnancy george100% (1)
- Complete Report of Introduction Biotechnology: "Tempe Making (Soybean Cake) "Document21 pagesComplete Report of Introduction Biotechnology: "Tempe Making (Soybean Cake) "1123khaliqNo ratings yet
- Cns 765 Assignment 7Document9 pagesCns 765 Assignment 7api-664836263No ratings yet
- Remember: Goals and Plan of Care Should Be Base According To Client's Problems/needs NOT According To Your OwnDocument11 pagesRemember: Goals and Plan of Care Should Be Base According To Client's Problems/needs NOT According To Your Ownavinash dhameriyaNo ratings yet
- Stress Activities Part 1Document22 pagesStress Activities Part 1JGO0% (5)
- Fluoride RemovalDocument16 pagesFluoride RemovalSandeep_AjmireNo ratings yet
- Attending Physicians Statement Crisis Cover Renal Failure - 041222Document2 pagesAttending Physicians Statement Crisis Cover Renal Failure - 041222max leeNo ratings yet
- Polarity ReversalDocument2 pagesPolarity Reversalapi-269724919100% (1)
- Asthma Nursing Care Plan - NCP - Ineffective Airway ClearanceDocument2 pagesAsthma Nursing Care Plan - NCP - Ineffective Airway ClearanceCyrus De Asis92% (24)
- Drug Recipe Comp 1581005894Document1,198 pagesDrug Recipe Comp 1581005894sirajul_islam_anikNo ratings yet
- Community Wellness Sti Graphic OrganizerDocument3 pagesCommunity Wellness Sti Graphic Organizerapi-291220650No ratings yet
- "Iligtas Sa Tigdas Ang Pinas ": Guide For Vaccination TeamDocument24 pages"Iligtas Sa Tigdas Ang Pinas ": Guide For Vaccination Teamkbl27No ratings yet
- Psyche A AkDocument21 pagesPsyche A AkSamuel John SaludezNo ratings yet
- HeartattackDocument2 pagesHeartattackapi-249970646No ratings yet
- Benjamin Lynch, 2017 - Intolerance, MTHFR and Methylation, Dealing With HistamineDocument4 pagesBenjamin Lynch, 2017 - Intolerance, MTHFR and Methylation, Dealing With HistamineSara AzuliNo ratings yet
- TCHP Shock Series Part 2Document2 pagesTCHP Shock Series Part 2ikeernawatiNo ratings yet
- Part ADocument41 pagesPart AAmar G PatilNo ratings yet
- Template - Case Report ArticleDocument4 pagesTemplate - Case Report Articlegerald randyNo ratings yet
- Annotated Bibliography Final DraftDocument4 pagesAnnotated Bibliography Final Draftapi-271972577No ratings yet