Professional Documents
Culture Documents
Disfagia Esofágica en Niños. Estado Del Arte y Propuesta para Un Enfoque Diagnóstico Basado en Los Síntomas (2022)
Uploaded by
7 MNTOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Disfagia Esofágica en Niños. Estado Del Arte y Propuesta para Un Enfoque Diagnóstico Basado en Los Síntomas (2022)
Uploaded by
7 MNTCopyright:
Available Formats
MINI REVIEW
published: 24 June 2022
doi: 10.3389/fped.2022.885308
Esophageal Dysphagia in Children:
State of the Art and Proposal for a
Symptom-Based Diagnostic
Approach
Gloria Lanzoni 1,2 , Camilla Sembenini 1 , Stefano Gastaldo 1 , Letizia Leonardi 1 ,
Vincenzo Pio Bentivoglio 1 , Giovanna Faggian 2 , Luca Bosa 2 , Paola Gaio 2† and
Mara Cananzi 1,2* †
1
School of Specialty in Pediatrics, University Hospital of Padova, Padua, Italy, 2 Unit of Pediatric Gastroenterology, Digestive
Endoscopy, Hepatology and Care of the Child With Liver Transplantation, Department of Women’s and Children’s Health,
University Hospital of Padova, Padua, Italy
Pediatric esophageal dysphagia (PED) is an infrequent condition that can be determined
by a large number of disorders. The etiologic diagnosis is challenging due to overlapping
clinical phenotypes and to the absence of pediatric diagnostic guidelines. This review
Edited by:
Alfonso Galderisi,
aims to summarize the most relevant causes of ED during childhood, highlight the
Hôpital Necker-Enfants Malades, clinical scenarios of PED presentation and discuss the indications of available diagnostic
France
tools. Available information supports that PED should always be investigated as it can
Reviewed by:
underlie life-threatening conditions (e.g., foreign body ingestion, mediastinal tumors),
Silvia Salvatore,
University of Insubria, Italy represent the complication of benign disorders (e.g., peptic stenosis) or constitute the
*Correspondence: manifestation of organic diseases (e.g., eosinophilic esophagitis, achalasia). Therefore,
Mara Cananzi the diagnosis of functional PED should be made only after excluding mucosal, structural,
mara.cananzi@aopd.veneto.it
† These
or motility esophageal abnormalities. Several clinical features may contribute to the
authors have contributed
equally to this work and share last diagnosis of PED. Among the latter, we identified several clinical key elements, relevant
authorship complementary-symptoms and predisposing factors, and organized them in a multi-
level, hierarchical, circle diagram able to guide the clinician through the diagnostic work-
Specialty section:
This article was submitted to up of PED. The most appropriate investigational method(s) should be chosen based on
Pediatric Gastroenterology, the diagnostic hypothesis: esophagogastroduodenoscopy has highest diagnostic yield
Hepatology and Nutrition,
a section of the journal
for mucosal disorders, barium swallow has greater sensitivity in detecting achalasia and
Frontiers in Pediatrics structural abnormalities, chest CT/MR inform on the mediastinum, manometry is most
Received: 27 February 2022 sensitive in detecting motility disorders, while pH-MII measures gastroesophageal reflux.
Accepted: 06 June 2022 Further studies are needed to define the epidemiology of PED, determine the prevalence
Published: 24 June 2022
of individual underlying etiologies, and assess the diagnostic value of investigational
Citation:
Lanzoni G, Sembenini C, methods as to develop a reliable diagnostic algorithm.
Gastaldo S, Leonardi L,
Keywords: esophageal dysphagia, esophageal disorders, achalasia, eosinophilic esophagitis, peptic esophagitis,
Bentivoglio VP, Faggian G, Bosa L,
symptom based diagnosis, children, pediatric
Gaio P and Cananzi M (2022)
Esophageal Dysphagia in Children:
State of the Art and Proposal Abbreviations: BS, Barium swallow; CI, caustic ingestion; CT, computed tomography; EA, esophageal atresia, EC, extrinsic
for a Symptom-Based Diagnostic compression; ED, Esophageal dysphagia; EGD, esophagogastroduodenoscopy; EoE, eosinophilic esophagitis; EO, esophageal
Approach. Front. Pediatr. 10:885308. obstruction; FB, foreign body; FBI, foreign body ingestion; GERD, gastroesophageal reflux disease; IE, infectious esophagitis;
doi: 10.3389/fped.2022.885308 OD, oropharyngeal dysphagia; MRI, magnetic resonance, PED, pediatric esophageal dysphagia; UGI, upper gastrointestinal.
Frontiers in Pediatrics | www.frontiersin.org 1 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
INTRODUCTION “dysphagia”), to the pediatric age (e.g., “children”), to specific
etiologies (e.g., “eosinophilic esophagitis”), or to diagnostic
Dysphagia is defined as a disruption in the swallowing process techniques (e.g., “esophageal manometry”). Papers not relevant
that can involve any structure of the upper gastrointestinal to the topic were excluded by screening of titles and abstracts.
(UGI) tract from the lips to the lower esophageal sphincter. The Paper eligibility was confirmed by direct assessment of full-
anatomical classification distinguishes oropharyngeal dysphagia text articles. When available, practice guidelines, systematic
(OD), in which the oral or pharyngeal phases of the swallowing reviews, meta-analysis, and RCTs, were considered the preferred
process are involved, from esophageal dysphagia (ED) in which references. Findings from selected studies were combined and
the underlying cause arises from the esophageal body or from the summarized to provide the best available evidence to address the
esophageal sphincters (1). Despite significant physiopathological above-mentioned research questions.
differences, the distinction between OD and ED may be Based on the revision of the literature, we developed a
challenging, due to overlapping clinical presentation, especially symptom-based diagnostic diagram aiming to guide the clinician
in infants and young children (Figure 1). Regardless of the toward the identification of the etiology underlying PED. To
site involved, dysphagia can pose significant health issues and graphically represent this process, we coded in HTML-Javascript
impair the child’s quality of life: the inability to eat properly can a dynamic sunburst chart. The diagram represents in a circular
lead to dehydration and failure to thrive; the aspiration of food graph hierarchical relational data distributed on different levels.
into the airways may cause recurrent respiratory infections and Each level represents the detalization of the previous in a
choking episodes; and, the difficulty in swallowing can elicit social centrifugal way.
isolation, anxiety, and depression (1–3).
Epidemiologic data regarding the prevalence of dysphagia in
children are lacking. A nationwide US survey estimates that 0.9% RESULTS
of children, from 3 to 17 years of age, suffer from swallowing
disorders with equal distribution between genders and mean age What Are the Most Relevant Causes of
at onset of 8.2 years (4). While OD is prevalent in children Pediatric Esophageal Dysphagia?
with neurological impairment, the causes of dysphagia are more According to the underlying pathogenetic mechanism,
heterogeneous in children without developmental issues with ED esophageal disorders can be classified into mucosal, structural,
being more relevant (5–7). and motility diseases as well as disorders caused by luminal
Pediatric ED (PED) can be the clinical manifestation of esophageal obstruction (EO) or extrinsic compression (EC). The
a wide variety of disorders. The majority of available studies main causes of PED are reported in Table 1 and are synthetically
focus on the specific etiologies of ED and, to the best of our described in Supplementary Table 1.
knowledge, no guidelines or comprehensive recommendations From an epidemiological point of view, mucosal disorders
are available for the diagnosis of PED. Due to the absence of constitute the most relevant cause of PED, with gastroesophageal
a standardized diagnostic approach, the management of PED reflux disease (GERD) and eosinophilic esophagitis (EoE)
is extremely variable, especially as regards the employment of being the more frequent. The prevalence of GERD in children
instrumental diagnostic techniques. is 6% with an incidence that progressively increases with
The aim of this review is to summarize the most relevant age (9). With a prevalence of 22.7 cases/100,000, EoE is far
causes of PED, highlight the clinical key elements able to guide the less frequent than GERD but is the leading cause of food
diagnostic process, and discuss the available diagnostic tools with impaction which constitutes the presenting symptom of disease
their specific indications. We also aim to propose a symptom- in up to the 22% of children (6, 10). Primary esophageal
based diagnostic approach able to guide clinicians through the motility disorders are a group of rare conditions subdivided,
diagnostic work-up of PED. according to the Chicago Classification 4.0, into disorders
of the esophagogastric junction outflow (i.e., Achalasia,
Esophagogastric Junction Outflow Obstruction) and disorders of
MATERIALS AND METHODS peristalsis [i.e., Distal Esophageal Spasm (DES), Hypercontractile
Esophagus (nutcracker esophagus), Ineffective Esophageal
We performed a narrative review of the literature as to satisfy the Motility (IEM), and Absent Contractility] (11). Among the latter,
Scale for the Assessment of Narrative Review Articles (SANRA) achalasia is the one most commonly reported in the pediatric
(8). The review was structured around three research questions, population but remains a rare disease with an incidence of 0.18
all relevant to the aim of the study: (i) which are the most relevant cases/100.000 children (12). No data are available regarding
causes of PED; (ii) what clinical key elements are able to guide the epidemiology of the other primary esophageal motility
the diagnostic process; (iii) what are the available diagnostic disorders in children. Esophageal atresia (EA) has a prevalence
tools. A search of the literature published after January 2000 of 0.7–3.2 cases/10,000 births and is the main representative of
was performed employing the Scopus, Embase, PubMed and structural disorders causing PED (13). Dysphagia lusoria, due to
Cochrane Library databases. The research was focused to papers an aberrant right subclavian artery, is the most frequent cause
written in English and to studies performed in human subjects of esophageal EC (14). The esophagus is the most common site
aged from 0 to 18 years old. Multiple combinations of keywords for an acute foreign body (FB) in the gastrointestinal tract. With
were employed, referring to dysphagia as a symptom (e.g., a peak incidence between the ages of 6 months and 3 years,
Frontiers in Pediatrics | www.frontiersin.org 2 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
FIGURE 1 | Common and peculiar clinical features of oropharyngeal and esophageal dysphagia (71, 72).
children make up the 80% of patients presenting to emergency Our review of the literature highlighted the following as
departments with an esophageal FB (15). relevant clinical elements able to guide the diagnostic work-
When, after an appropriate evaluation, ED cannot be up of PED.
explained by another condition, functional dysphagia can be
considered in the differential diagnosis. While it is the most Age at Presentation
prevalent esophageal disorder in adults, no data are available While some disorders causing ED can develop at any age [e.g.,
regarding its prevalence in the pediatric population (16). The infectious esophagitis (IE)], other conditions tend to arise at
diagnosis relies on the Rome IV criteria which define functional a typical age (Figure 2). Congenital disorders usually occur in
dysphagia as a sense of solid and/or liquid food sticking, lodging, neonates or infants: EA always presents within the first few
or passing abnormally through the esophagus that arises in hours of life (20), while congenital esophageal stenoses usually
addition to all of the following criteria: (i) symptom onset at least become evident at weaning or after the introduction of solid
6 months before evaluation; (ii) symptom frequency of at least foods (21). FB ingestion (FBI) is typical of infants and preschool
once a week; (iii) absence of evidence that esophageal mucosal or children (22). Caustic ingestion (CI) occurs in a bimodal fashion:
structural abnormality is the cause of the symptom; (iv) absence accidental ingestion is most common under 5 years of age, while
of evidence that gastroesophageal reflux or EoE is the cause of the intentional ingestion, related to attempted suicide, mainly occurs
symptom; (v) absence of major esophageal motor disorders (17). in adolescents (23). EoE usually occurs in children between 5 and
12 years old (6, 24), and the incidence of GERD increases with
What Are the Clinical Key Diagnostic age (9, 25).
Elements for the Diagnosis of Pediatric Modality of Esophageal Dysphagia Onset
Esophageal Dysphagia? The majority of esophageal disorders presenting with dysphagia
Children with ED may present with a variety of complaints cause a chronic or intermittent dysphagia with or without a
ranging from a sensation of food getting stuck in the throat progressive pattern.
or behind the sternum to a proper inability to swallow any ED can also present acutely with a sudden inability to swallow
kind of food or beverage with associated drooling (18). In solids and/or liquids. Under these circumstances, EO should
the case of long-standing ED, compensatory behaviors, such always be suspected, especially if sialorrhea is present. While
as chewing for prolonged periods of time, using water or FBI mostly concerns infants and toddlers with no underlying
other lubricants to facilitate the passage of food, or avoiding esophageal disfunction, food impaction is the most common
problematic ingredients, can accompany and somewhat mask cause of acute EO in older children and teenagers. The latter
the presence of true dysphagia and therefore must always be is usually the presenting symptom of an esophageal disorder,
investigated (19). among which EoE is the most frequent (6, 26). Less frequent
Infants usually present with non-specific complaints such as causes consist of peptic-, caustic- or radiation-induced strictures,
feeding difficulties and bolus regurgitation, thus making it more Schatzki’s rings, esophageal diverticula, achalasia, and post-
challenging to recognize ED in this age group. surgical complications (15). IE also presents acutely but, in this
Frontiers in Pediatrics | www.frontiersin.org 3 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
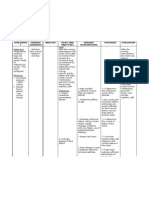
TABLE 1 | Main causes of pediatric esophageal dysphagia along with representative disease features (peak age of incidence, predisposing factors, clinical features), and
suggested diagnostic test(s).
Disease Peak age Predisposing factors Clinical features Diagnostic test(s)
Newborn- infant Children-adolescents
Mucosal GERD (25) Adolescence CI, EA, neurological Regurgitation, vomit, irritability, Heartburn, epigastric pain, EGD with biopsies,
disorders impairment, previous growth failure feeding or chest pain, pH-MII
surgery, SSc, RT. sleeping difficulties, anemia sour burps, regurgitation, vomit,
Eosinophilic 5–12 years Atopy, EA Feeding difficulties, vomit, Food impaction, heartburn, EGD with biopsies
Esophagitis (24) growth failure vomit, chocking, gagging
Infectious Any age Immunodeficiency, Odynophagia, chest pain, fever EGD with biopsies
esophagitis (27) prolonged steroid or and microbiological
antibiotic treatment sampling
Crohn’s disease Adolescence – Heartburn, chest pain, intestinal symptoms, EGD with biopsies
(74) fever, involuntary weight loss
Pill esophagitis 8–18 years Recent initiation of Odynophagia, chest pain EGD with biopsies
(42) pill/tablet treatment
Caustic <5 years, > 12 CI Chest pain, sore throat, EGD with biopsies
esophagitis (23) years odynophagia, heartburn
Radiation Any age RT Chest pain, sore throat, o EGD with biopsies
esophagitis (75) dynophagia, heartburn
Motility Achalasia (45) 7–12 years Down’s and triple A Paradoxycal ED, regurgitation of undigested food, feeding HREM, barium
disorders syndromes, difficulties, swallow, EGD
Pierre-Robin sequence chest pain, weight loss, respiratory symptoms
Systemic 8–11 years – Food impaction, heartburn, Barium swallow,
sclerosis (40) regurgitation, chest pain, SSc EGD with biopsies,
extra-intestinal features pH-MII, HREM
Structural Esophageal Neonate Concomitant Respiratory distress, impossible – Chest X-ray,
disorders atresia (20) malformations NG tube insertion, drooling barium swallow
Congenital Weaning time – Feeding difficulties, Food impaction Barium swallow,
stenosis (21) regurgitation of undigested EGD
food, respiratory symptoms-
Acquired Any age CI, GERD, EoE, Feeding difficulties, Food impaction Barium swallow,
stenosis/rings previous surgery, RT regurgitation of undigested EGD
(35, 76) food, respiratory symptoms-
Diverticula (77) Any age Motility disorders, Choking, respiratory symptoms, regurgitation of Barium swallow,
previous surgery undigested food EGD
Duplication cyst Any age – Respiratory symptoms Barium swallow,
(78) EGD,
chest CT scan or
MRI
Luminal Foreign body 6 mths-3 years – Drooling, food refusal, retching, vomit, chest pain, Chest X-ray, EGD
obstruction ingestion (15) stridor, cough
Food impaction 5–12 years Achalasia, EoE, rings, Drooling, feeding difficulties, retching, vomit, chest pain, EGD with biopsies
(15) stenoses, previous stridor, cough
surgery
Extrinsic Vascular Any age Congenital heart Respiratory symptoms Barium swallow,
compression anomalies (14) defects, Chest CT or MRI
Down’s syndrome with angio
Mediastinal Any age – Respiratory symptoms, fever, weight loss Chest X-ray,
disorders (33) barium swallow,
chest CT or MRI
case, obstructive symptoms are usually absent, while fever and the esophagus (either intrinsic or extrinsic), while the latter is
pain are predominant (27). secondary to motility disorders (28, 29).
Food Consistency Associated Symptoms
ED can be categorized based on the consistency of foods for ED may be an isolated symptom or occur in association with
which the swallowing process is impaired. Orthodox dysphagia other clinical findings.
is characterized by an impairment in managing solid foods UGI symptoms such as heartburn, epigastric pain, chest pain,
which may later involve liquids, while paradoxical dysphagia and regurgitation are usually reported in GERD (7, 25). Food
presents with a difficulty in managing liquids from symptom bolus impaction points toward the diagnosis of EoE (24). The
onset. The first is a consequence of a mechanical obstruction of combination of bolus regurgitation, chest pain, weight loss,
Frontiers in Pediatrics | www.frontiersin.org 4 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
FIGURE 2 | Graphical representation of the distribution of the different esophageal disorders by age groups.
and paradoxical dysphagia constitute the typical presentation of is a close temporal relation (<10 days) with the use of NSAIDs,
achalasia (30, 31). antibiotics (e.g., doxycycline, amoxicillin), L-arginine and iron,
Respiratory symptoms such as nocturnal cough and recurrent and the drug has been taken with little water at bedtime (42, 43).
respiratory infections are also frequently reported in patients
with esophageal achalasia due to recurrent aspiration or tracheal
compression from the dilated esophagus (32). Sore throat,
What Are the Available Diagnostic Tools?
The diagnostic work-up of PED can include a luminal, mucosal,
hoarseness, nocturnal cough, wheezing, and recurrent respiratory
anatomic, and functional assessment of the esophagus. Several
infections have been identified as atypical symptoms of GERD
diagnostic methodologies are available, the specific indications
(25). Moreover, respiratory distress, stridor and wheezing can
and diagnostic rates of which are discussed below. Moreover, pros
accompany dysphagia in the presence of any chest mass or
and cons of the main diagnostic tools are summarized in Table 2.
vascular malformation causing a compression on mediastinal
structures (14, 33).
Fever in association to odynophagia and chest pain suggest Esophagogastroduodenoscopy
the diagnosis of IE or, in case of a compatible clinical history, The methods and the indications for performing EGD in
may prompt the possibility of FBI complicated with esophageal children with ED have been reported by the ESPGHAN-ESGE
perforation and acute mediastinitis (34). Mediastinal masses can guidelines (23).
be associated to the presence of paraneoplastic fever (33). In the context of GERD-related dysphagia, EGD is useful for:
(i) defining the obstructive vs. non-obstructive nature of the
Comorbidities symptom (stenosis vs. dysmotility); (ii) detect conditions that
Several pre-existing conditions may predispose to the onset of predispose to GERD (e.g., hiatal hernia); (iii) exclude conditions
dysphagia. Former esophageal surgery, radiation therapy and CI mimicking GERD such as EoE (7, 23). Indeed, the detection
can lead to acquired stenosis and predispose to GERD (35). With of > 15 eosinophils per HPF in at least 1 biopsy specimen of the
a reported incidence as high as 70%, GERD is also common esophageal mucosa is the gold standard for the diagnosis of EoE
in children with neurological impairment (5). Achalasia has and the performance of 1–2 biopsies from the proximal, middle,
been linked to Down’s syndrome (36), Pierre-Robin sequence and distal esophagus provides for a 97–100% sensitivity in the
and other rare genetic disorders (37). Congenital heart defects detection of esophageal eosinophilia (23, 24, 44). In IE, EGD
and Down’s Syndrome are associated to vascular anomalies reveals typical mucosal changes and provide for a microbiological
causing EC (14). Allergologic disorders and EA constitute well- diagnosis (39). EGD is the method of choice for detecting the
established risk factors for the development of EoE (24, 38). characteristic features of pill-induced esophagitis which consist of
Primary or acquired immunodeficiencies as well as prolonged single or multiple ulcers, surrounded by normal mucosa, usually
antibiotic and steroid treatment favor the development of IE (34, located in the middle-third of the esophagus (42, 43).
39). Immune-mediated disorders, such as systemic sclerosis (40) EGD plays a diagnostic and therapeutic role in acute EO.
and Crohn’s disease can rarely involve the esophagus causing Any symptomatic patient with suspected FBI should emergently
ED (41). Ongoing treatment with tablets/capsules should raise undergo EGD as well as asymptomatic patients who swallowed
the possibility of pill-induced esophagitis especially when there sharp FB or button butteries. The endoscopic removal of
Frontiers in Pediatrics | www.frontiersin.org 5 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
TABLE 2 | Pros and cons of the main diagnostic tools employed in the assessment of PED (48, 73).
Pros Cons
Esophagogastroduodenoscopy • Enables direct visualization of the esophageal lumen and mucosa • Sedation needed
(EGD) • Allow histological and microbiological sampling • Unable to diagnose motility disorders
• Allows endoscopic removal of FB • Rare complications (e.g., infection, perforation,
• Allows pneumatic dilation of the esophagus bleeding)
pH-multichannel intraluminal • Allows precise evaluation of GER • Requires patient cooperation
impedance (pH-MII) • Can be coupled with EGD • No anatomical or motility information
Barium swallow • Widely available • Radiation exposure
• Provides good anatomical detail of the esophagus • Requires patient cooperation
• Can identify motility disorders (e.g., achalasia) • Cannot be performed in patients with bowel
• Can demonstrate an extrinsic compression of the esophagus obstruction or suspected perforation
• Aspiration of barium can lead to hypersensitivity
pneumonitis, and barium leakage through
perforation can lead to mediastinitis and peritonitis
High-resolution esophageal • Allows characterization of motility disorders • Requires patient cooperation
manometry (HREM) • Can be used to classify esophageal achalasia subtypes, define • No direct visualization of the esophageal anatomy
treatment and prognosis nor mucosa
• May be used to characterize congenital stenoses
Chest X-ray • Can identify radio-opaque foreign bodies • Radiation exposure
• Can identify mediastinal enlargement and pneumomediastinum
Chest CT/MRI • Allow identification of structural disorders or extrinsic esophageal • Radiation exposure (only for CT)
compression • Sedation needed in young children
• Coupled with angiography represent the gold standard for the
diagnosis of vascular anomalies causing dysphagia.
asymptomatic blunt esophageal FB is also recommended within Virtually all children with achalasia present at least one typical
24 h from the ingestion (23). BS feature; the most common consist of slow contrast transit
EGD can rise the suspicion of achalasia, and exclude through the esophagus into the stomach (96.1%), esophageal
pseudoachalasia, but is not diagnostic per se and may miss dilation (94.1%), “bird’s beak” sign (82.4%), contrast retention
early disease. Abnormalities are present in the 90% of affected in the esophagus (74%), and peristaltic anomalies (62%) (31, 45,
children with most common findings consisting of residual food 50). Besides providing excellent mucosal detail, BS is seldom
in the esophagus (75%), closed stomach cardia (73%), esophageal used for the diagnosis of esophagitis and cannot establish or
enlargement (58%), and mucosal lesions (28%) (45). In patients negate a diagnosis of GERD. However, it can detect conditions
with symptom relapse after surgery, EGD is useful to assess for predisposing to GERD (e.g., hiatal hernia) and differentiate an
reflux vs. recurrence of achalasia (30, 31). obstructing vs. a slipped/loose fundoplication (7).
EGD may also reveal a narrowing of the esophageal lumen
caused by structural lesions or EC. In these circumstances, Esophageal Function Tests
however, the definite diagnosis usually requires the employment pH-metry or dual pH-multichannel intraluminal impedance
of other diagnostic modalities including CT, MRI, and (pH-MII) are not routinely recommended for the diagnosis of
endoscopic ultrasound (46). GERD (7). However, they can be helpful in the context of GERD-
In children with a truly negative endoscopy (i.e., after an related dysphagia, as to: (i) correlate the symptom with acid/non-
adequate biopsy sampling), radiologic studies and esophageal acid reflux events; (ii) clarify the role of acid/non-acid reflux in
function tests should be warranted to investigate for subtle the etiology of esophagitis; (iii) evaluate for reflux in patients
structural lesions (e.g., rings), EC and motility disorders (47). with EoE as these two conditions are not mutually exclusive; (iv)
determine the efficacy of acid suppression in case of persisting
Radiologic Techniques dysphagia during treatment; (v) assess the onset of GERD after
Plain chest X-ray has a limited role in the assessment of PED. surgical and endoscopic treatments for achalasia (7, 24, 51).
It can identify radiopaque FBs stuck into the esophagus, exclude When available, pH-MII should be preferred to pH-monitoring
the presence of pulmonary issues when fever or respiratory and considered the gold standard diagnostic technique for the
symptoms are present, and screen for pneumomediastinum or detection of GERD in the pediatric population (52). Indeed, since
gross mediastinal enlargements (22). it allows the measurement of all reflux events irrespective of
Chest CT and MRI are needed to investigate the mediastinum pH, pH-MII allows the detection of non-acid reflux episodes
when an esophageal EC is suspected. When coupled with which have a high prevalence in the pediatric population, can be
angiography, these methodologies are the gold standard for the carried out on or off reflux therapy, and may be performed during
diagnosis of vascular anomalies causing dysphagia (14). continuous enteral feeding (49, 50, 52).
Barium swallow (BS) is useful in diagnosing esophageal High-resolution esophageal manometry (HREM) represents
webs, rings, stenoses, diverticula, tumors and EC (48, 49). the gold standard for the diagnosis of esophageal motility
Frontiers in Pediatrics | www.frontiersin.org 6 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
FIGURE 3 | Sunburst diagram representing our proposed symptom-based diagnostic approach to ED. The diagram consists of four concentric circles (or levels)
which, from the inside to the outside, represent in a hierarchical relation: (1) the clinical key elements that guide the diagnostic process; (2) relevant complementary
symptoms and disease factors predisposing to a specific etiology that, in addition to the corresponding clinical key element, may address the differential diagnosis;
(3) the most probable etiologic diagnosis/diagnoses of ED based on the clinical elements selected in the underlying levels. Each clinical key element is represented in
a different color and this color is maintained throughout the corresponding section of the graph, albeit with different tones along the different levels (i.e., rings 1, 2, 3).
Relevant complementary symptoms and predisposing factors in ring 2 make the etiologic diagnosis in ring 3 more likely; when no element is indicated it means that
the final diagnosis may not be associated to any other clinical element. A dynamic version of the diagram is available in Supplementary Material.
disorders, particularly achalasia (30, 31, 53). This technique contraction) and esophago-gastric junction relaxation (IRP4s, or
uses a standardized swallow challenge to measure peristaltic Integrated Relaxation Pressure, measured as the mean of the 4 s of
pressures throughout the esophageal body (54). The Chicago lowest pressure across the lower esophageal sphincter in the 10 s
classification algorithm classifies esophageal motility disorders window after swallow) (11). HREM has been recently combined
according to manometric measurements of esophageal peristalsis with intraluminal impedance mapping (HRIM, High Resolution
(DCI, or Distal Contractile Integral, is the amplitude x duration x Impedance Manometry). This approach allows to directly
length [mmHg∗ s∗ cm] of the distal esophageal contraction above evaluate the transit of the esophageal bolus using pressure-
20 mmHg, from the transition zone to the proximal margin of the impedance metrics (IBP, or Intra-bolus Distension Pressure,
lower esophageal sphincter; DL, or Distal Latency, is the interval indicating flow resistance; BFT, or Bolus Flow Time, indicating
between upper esophageal sphincter relaxation and the distal trans-esophagogastric junction emptying; and Impedance Ratio,
Frontiers in Pediatrics | www.frontiersin.org 7 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
indicating bolus transit failure), thus increasing the yield for of life measure has been developed and validated for children
detecting esophageal motility disorders (54). The use of the with achalasia (66). However, despite the availability of this
above-mentioned techniques has been validated in children questionnaire since 2010, it is seldom employed in pediatric
(55), although some distinctions should be considered when clinical practice (31).
interpreting the results. Patient characteristics and esophageal
length and caliber have a significant impact on esophageal
pressure topography metrics, thus, in pediatric patients reference DISCUSSION
ranges should be adjusted for size (55). Moreover, children under
7 years of age are often unable to tolerate the procedure and Our review of the literature shows that PED is caused
patient movement and crying can produce measurement artifacts by a heterogeneous group of disorders, among which EoE
that can impair study interpretation (54). and GERD are the most frequent, summarizes the diverse
clinical scenarios of PED presentation, and highlights the most
Questionnaires and Clinical Scales appropriate investigational method(s) based on the diagnostic
As said above (section “What Are the Clinical Key Diagnostic hypothesis. Despite available knowledge regarding individual
Elements for the Diagnosis of Pediatric Esophageal Dysphagia”, etiologies, this revision also confirms the lack of pediatric
the clinical identification as well as the measurement of PED epidemiological data and the absence of diagnostic guidelines
pose several challenges. To address this issue, questionnaires regarding PED as a symptom.
and clinical outcome metrics (COMs) have been developed to In adults, ED is considered an alarm sign that may underlie
identify, quantify, and monitor the presence of a swallowing the presence of esophageal carcinoma (67, 68). In children,
problem either independently from the underlying etiology or in ED is not clearly recognized as a red flag given the rarity
specific pathological contexts (19). of esophageal cancer in this age group. However, available
The Eating Assessment Tool (EAT-10) (56) and its pediatric information regarding the etiology of PED supports that this
modified version (57) (PEDI-EAT-10) are symptom-based symptom should always be investigated as it can underlie
questionnaires that support the clinician in identifying the life-threatening conditions (e.g., FBI, CI, mediastinal tumors),
presence of a swallowing problem and in assessing the risk of represent the complication of benign esophageal disorders (e.g.,
penetration/aspiration (Supplementary Tables 2, 3). GERD-related stenosis) or constitute the clinical manifestation of
The Reflux Symptom Index (RSI) (58) is a self-administered an organic disease (e.g., EoE, achalasia). Therefore, in children as
nine-item instrument to detect laryngopharyngeal reflux in adults, the diagnosis of functional dysphagia should only be
(Supplementary Table 4). It has been recently proven to be made after demonstrating the absence of mucosal, structural, or
inaccurate in assessing the presence of gastroesophageal reflux esophageal motility abnormalities (17).
in children and infants when compared to pH-MII. Indeed, Several diagnostic protocols are available for the diagnosis of
although the number of acid refluxes directly correlates with ED but none has been specifically made for children. No sufficient
the RSI, a normal RSI value does not exclude the presence of a data are available to develop a diagnostic algorithm for PED or
pathological MII-pH (59). advocate for the superiority of a diagnostic test over another as
Several scoring systems have been developed for the clinical first-line investigation.
evaluation of EoE. In adults, the Eosinophilic Esophagitis Activity We propose a diagnostic approach tailored on the main
Index was found to have the best validity and responsiveness diagnostic suspect(s) deriving from the clinical evaluation of the
in a systematic review: this tool focuses on dysphagia induced child. To this end, we have identified six clinical key elements
by food of different consistencies and on behavioral adaptation capable of recognizing patients who require an immediate
in daily life (60, 61). In children, the Pediatric Eosinophilic medical evaluation (i.e., signs of acute EO and fever) or directing
Esophagitis Symptom Score (PEESS) (62) has been validated toward a diagnosis (i.e., history of food impaction, isolated
to assess dysphagia in subjects from 2 to 18 years of age dysphagia, paradoxical dysphagia, respiratory symptoms, UGI
based on child and/or parent proxy scores (Supplementary symptoms). As none of abovementioned clinical key elements
Tables 5, 6). The aforementioned indexes are useful in assessing can be univocally associated to a single etiology, we have also
and monitoring EoE symptoms; nevertheless, they cannot be identified relevant complementary symptoms and predisposing
used to make assumptions on the biological activity of EoE, as factors that, combined to clinical key elements, can support
they have a predictive unsatisfactory value (63). the clinician throughout the diagnostic process. This symptom-
The Eckardt score has been specifically developed for based approach is graphically represented in a circular graph
esophageal achalasia to establish clinical disease severity at with hierarchical relational data distributed on different levels
diagnosis and to evaluate treatment efficacy during follow-up (Figure 3). Once one or more diagnostic hypotheses have been
(30, 64, 65). The score is based on the three main symptoms made, the most appropriate investigational method(s) should
associated with achalasia (dysphagia, regurgitation, and chest be chosen based on the specificities of individual tests. EGD
pain) in adjunct to weight loss included as a marker of the has highest diagnostic yield for the evaluation of luminal and
patient’s capacity to maintain nutrition (Supplementary Table 7). mucosal disorders. BS has a greater sensitivity in detecting
Unfortunately, the application of the Eckardt score in children achalasia and structural abnormalities, is non-invasive and can
is limited since the questionnaire is only validated for subjects be used to confirm indication and define setting (diagnostic vs.
older than 14 years of age (31, 65). A disease-specific quality operative) prior to perform EGD (28, 69, 70). Chest CT and MR
Frontiers in Pediatrics | www.frontiersin.org 8 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
provide detailed anatomical information on the mediastinum. the results. GF and LB performed a critical review of the
Manometry is the most sensitive technique to detect motility findings and participated in the preparation of the manuscript.
disorders, while pH-MII evaluates the presence of acid/non-acid All authors contributed to the article and approved the
reflux (48, 49, 70). submitted version.
To the best of our knowledge, this is the first comprehensive
review regarding PED. Large scale studies are needed to
define the epidemiology of PED, determine the prevalence of ACKNOWLEDGMENTS
underlying etiologies, and assess the diagnostic value of available
investigational methods as to establish the relative risk of We would like to thank the Pediatric Residency Program and the
disease and develop a reliable diagnostic algorithm. Prospective Department of Women’s and Children’s Health of the University
studies should be conducted, or a machine-learning approach Hospital of Padova for the support in producing and publishing
implemented, to validate our symptom-based approach for the this manuscript. We are grateful to Marco Tognin for his support
etiological definition of PED. in programming the Sunburst dynamic diagram.
AUTHOR CONTRIBUTIONS SUPPLEMENTARY MATERIAL
GL, PG, and MC wrote the manuscript, prepared tables and The Supplementary Material for this article can be found
figures which all authors reviewed. GL, CS, SG, LL, VPB, online at: https://www.frontiersin.org/articles/10.3389/fped.
and PG performed the literature search and summarized 2022.885308/full#supplementary-material
REFERENCES 12. Marlais M, Fishman JR, Fell JM, Haddad MJ, Rawat DJ. UK incidence of
achalasia: an 11-year national epidemiological study. Arch Dis Child. (2011)
1. Dodrill P, Gosa MM. Pediatric dysphagia: physiology, assessment, and 96:192–4. doi: 10.1136/adc.2009.171975
management. Ann Nutr Metab. (2015) 66(Suppl. 5):24–31. doi: 10.1159/ 13. Nassar N, Leoncini E, Amar E, Arteaga-Vazquez J, Bakker MK, Bower C,
000381372 et al. Prevalence of esophageal atresia among 18 international birth defects
2. van den Engel-Hoek L, de Groot IJ, de Swart BJ, Erasmus CE. Feeding and surveillance programs. Birth Defects Res A Clin Mol Teratol. (2012) 94:893–9.
swallowing disorders in pediatric neuromuscular diseases: an overview. J doi: 10.1002/bdra.23067
Neuromuscul Dis. (2015) 2:357–69. doi: 10.3233/JND-150122 14. Levitt B, Richter JE. Dysphagia lusoria: a comprehensive review. Dis
3. Tutor JD, Gosa MM. Dysphagia and aspiration in children. Pediatr Pulmonol. Esophagus. (2007) 20:455–60. doi: 10.1111/j.1442-2050.2007.00787.x
(2012) 47:321–37. 15. Fung BM, Sweetser S, Wong Kee Song LM, Tabibian JH. Foreign object
4. Bhattacharyya N. The prevalence of pediatric voice and swallowing problems ingestion and esophageal food impaction: an update and review on endoscopic
in the United States. Laryngoscope. (2015) 125:746–50. doi: 10.1002/lary.24931 management. World J Gastrointest Endosc. (2019) 11:174–92. doi: 10.4253/
5. Romano C, van Wynckel M, Hulst J, Broekaert I, Bronsky J, Dall’Oglio wjge.v11.i3.174
L, et al. European society for paediatric gastroenterology, hepatology and 16. Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren
nutrition guidelines for the evaluation and treatment of gastrointestinal and M, Tack J, et al. Worldwide Prevalence and Burden of Functional
nutritional complications in children with neurological impairment. J Pediatr Gastrointestinal Disorders, Results of Rome Foundation Global Study.
Gastroenterol Nutr. (2017) 65:242–64. doi: 10.1097/MPG.0000000000001646 Gastroenterology. (2021) 160:99.e–114.e. doi: 10.1053/j.gastro.2020.
6. Shaheen NJ, Mukkada V, Eichinger CS, Schofield H, Todorova L, Falk 04.014
GW. Natural history of eosinophilic esophagitis: a systematic review of 17. Aziz Q, Fass R, Gyawali CP, Miwa H, Pandolfino JE, Zerbib F. Functional
epidemiology and disease course. Dis Esophagus. (2018) 31:doy015. doi: 10. esophageal disorders. Gastroenterology. (2016). 150:1368–79.
1093/dote/doy015 18. Sherman PM, Hassall E, Fagundes-Neto U, Gold BD, Kato S, Koletzko S,
7. Rosen R, Vandenplas Y, Singendonk M, Cabana M, DiLorenzo C, Gottrand et al. A global, evidence-based consensus on the definition of gastroesophageal
F, et al. Pediatric gastroesophageal reflux clinical practice guidelines: reflux disease in the pediatric population. Am J Gastroenterol. (2009)
joint recommendations of the North American society for pediatric 104:1278–95; quiz96.
gastroenterology, hepatology, and nutrition and the European society for 19. Nguyen N, Furuta GT, Menard-Katcher C. Recognition and assessment of
pediatric gastroenterology, hepatology, and nutrition. J Pediatr Gastroenterol eosinophilic esophagitis: the development of new clinical outcome Metrics.
Nutr. (2018) 66:516–54. Gastroenterol Hepatol (N Y). (2015) 11:670–4.
8. Baethge C, Goldbeck-Wood S, Mertens S. SANRA-a scale for the quality 20. Pinheiro PF, Simoes e Silva AC, Pereira RM. Current knowledge on esophageal
assessment of narrative review articles. Res Integr Peer Rev. (2019) 4:5. doi: atresia. World J Gastroenterol. (2012) 18:3662–72.
10.1186/s41073-019-0064-8 21. Trappey AF III, Hirose S. Esophageal duplication and congenital esophageal
9. Martigne L, Delaage PH, Thomas-Delecourt F, Bonnelye G, Barthelemy P, stenosis. Semin Pediatr Surg. (2017) 26:78–86. doi: 10.1053/j.sempedsurg.2017.
Gottrand F. Prevalence and management of gastroesophageal reflux disease 02.003
in children and adolescents: a nationwide cross-sectional observational study. 22. Kramer RE, Lerner DG, Lin T, Manfredi M, Shah M, Stephen
Eur J Pediatr. (2012) 171:1767–73. doi: 10.1007/s00431-012-1807-4 TC, et al. Management of ingested foreign bodies in children: a
10. Arias A, Perez-Martinez I, Tenias JM, Lucendo AJ. Systematic review with clinical report of the NASPGHAN Endoscopy Committee. J Pediatr
meta-analysis: the incidence and prevalence of eosinophilic oesophagitis in Gastroenterol Nutr. (2015) 60:562–74. doi: 10.1097/MPG.0000000000
children and adults in population-based studies. Aliment Pharmacol Ther. 000729
(2016) 43:3–15. 23. Thomson M, Tringali A, Dumonceau JM, Tavares M, Tabbers MM,
11. Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman Furlano R, et al. Paediatric gastrointestinal endoscopy: European society for
S, et al. Esophageal motility disorders on high-resolution manometry: Chicago paediatric gastroenterology hepatology and nutrition and European Society
classification version 4.0((c)). Neurogastroenterol Motil. (2021) 33:e14058. doi: of gastrointestinal endoscopy guidelines. J Pediatr Gastroenterol Nutr. (2017)
10.1111/nmo.14058 64:133–53. doi: 10.1097/MPG.0000000000001408
Frontiers in Pediatrics | www.frontiersin.org 9 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
24. Papadopoulou A, Koletzko S, Heuschkel R, Dias JA, Allen KJ, Murch SH, et al. 46. Terui K, Saito T, Mitsunaga T, Nakata M, Yoshida H. Endoscopic management
Management guidelines of eosinophilic esophagitis in childhood. J Pediatr for congenital esophageal stenosis: a systematic review. World J Gastrointest
Gastroenterol Nutr. (2014) 58:107–18. doi: 10.1097/MPG.0b013e3182a80be1 Endosc. (2015) 7:183–91. doi: 10.4253/wjge.v7.i3.183
25. Poddar U. Gastroesophageal reflux disease (GERD) in children. Paediatr Int 47. Triggs J, Pandolfino J. Recent advances in dysphagia management. F1000Res.
Child Health. (2019) 39:7–12. (2019) 8:F1000FacultyRev–1527. doi: 10.12688/f1000research.18900.1
26. De Matteis A, Pagliaro G, Corleto VD, Pacchiarotti C, Di Giulio E, 48. Ghazanfar H, Shehi E, Makker J, Patel H. The role of imaging modalities
Villa MP, et al. Eosinophilic esophagitis in children: clinical findings and in diagnosing dysphagia: a clinical review. Cureus. (2021) 13:e16786. doi:
diagnostic approach. Curr Pediatr Rev. (2020) 16:206–14. doi: 10.2174/ 10.7759/cureus.16786
1573396315666191004110549 49. Debi U, Sharma M, Singh L, Sinha A. Barium esophagogram in various
27. Bordea MA, Pirvan A, Gheban D, Silaghi C, Lupan I, Samasca G, et al. esophageal diseases: a pictorial essay. Indian J Radiol Imaging. (2019) 29:141–
Infectious esophagitis in romanian children: from etiology and risk factors 54. doi: 10.4103/ijri.IJRI_465_18
to clinical characteristics and endoscopic features. J Clin Med. (2020) 9:939. 50. Rosenwald KD, Hayes K, Menard-Katcher C, Belkind-Gerson J.
doi: 10.3390/jcm9040939 Implementation of a timed barium esophagram protocol for assessment
28. Liu LWC, Andrews CN, Armstrong D, Diamant N, Jaffer N, Lazarescu A, et al. of esophageal function in children. J Pediatr Gastroenterol Nutr. (2020)
Clinical practice guidelines for the assessment of uninvestigated esophageal 71:470–5. doi: 10.1097/MPG.0000000000002829
dysphagia. J Can Assoc Gastroenterol. (2018) 1:5–19. doi: 10.1093/jcag/gwx008 51. Mousa HM, Rosen R, Woodley FW, Orsi M, Armas D, Faure C, et al.
29. Kotilea K, Mahler T, Bontems P, Deviere J, Louis H. Management of esophageal Esophageal impedance monitoring for gastroesophageal reflux. J Pediatr
motility disorders in children: a review. Acta Gastroenterol Belg. (2018) Gastroenterol Nutr. (2011) 52:129–39. doi: 10.1097/MPG.0b013e3181ffde67
81:295–304. 52. Quitadamo P, Tambucci R, Mancini V, Cristofori F, Baldassarre M, Pensabene
30. Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RTACG. Clinical L, et al. Esophageal pH-impedance monitoring in children: position paper on
guidelines: diagnosis and management of achalasia. Am J Gastroenterol. (2020) indications, methodology and interpretation by the SIGENP working group.
115:1393–411. doi: 10.14309/ajg.0000000000000731 Dig Liver Dis. (2019) 51:1522–36. doi: 10.1016/j.dld.2019.07.016
31. van Lennep M, van Wijk MP, Omari TIM, Salvatore S, Benninga MA, 53. Yamasaki T, Tomita T, Mori S, Takimoto M, Tamura A, Hara K, et al.
Singendonk MMJ, et al. Clinical management of pediatric achalasia: a survey Esophagography in patients with esophageal achalasia diagnosed with high-
of current practice. J Pediatr Gastroenterol Nutr. (2019) 68:521–6. doi: 10.1097/ resolution esophageal manometry. J Neurogastroenterol Motil. (2018) 24:403–
MPG.0000000000002221 9. doi: 10.5056/jnm17147
32. Tashiro J, Petrosyan M, Kane TD. Current management of pediatric achalasia. 54. Omari TI, Krishnan U. What is the role of high-resolution oesophageal
Transl Gastroenterol Hepatol. (2021) 6:33. manometry in paediatrics? J Paediatr Child Health. (2020) 56:1754–9. doi:
33. Ranganath SH, Lee EY, Restrepo R, Eisenberg RL. Mediastinal masses in 10.1111/jpc.15057
children. AJR Am J Roentgenol. (2012) 198:W197–216. 55. Singendonk MMJ, Omari TI, Rommel N, van Wijk MP, Benninga MA, Rosen
34. Hoversten P, Kamboj AK, Katzka DA. Infections of the esophagus: an update R, et al. Novel pressure-impedance parameters for evaluating esophageal
on risk factors, diagnosis, and management. Dis Esophagus. (2018) 31:1–9. function in pediatric achalasia. J Pediatr Gastroenterol Nutr. (2018) 66:37–42.
doi: 10.1093/dote/doy094 doi: 10.1097/MPG.0000000000001647
35. Ghiselli A, Bizzarri B, Ferrari D, Manzali E, Gaiani F, Fornaroli F, et al. 56. Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al.
Endoscopic dilation in pediatric esophageal strictures: a literature review. Acta Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol
Biomed. (2018) 89:27–32. doi: 10.23750/abm.v89i8-S.7862 Laryngol. (2008) 117:919–24.
36. Zarate N, Mearin F, Hidalgo A, Malagelada JR. Prospective evaluation of 57. Soyer T, Yalcin S, Arslan SS, Demir N, Tanyel FC. Pediatric eating assessment
esophageal motor dysfunction in Down’s syndrome. Am J Gastroenterol. tool-10 as an indicator to predict aspiration in children with esophageal atresia.
(2001) 96:1718–24. doi: 10.1111/j.1572-0241.2001.03864.x J Pediatr Surg. (2017) 52:1576–9. doi: 10.1016/j.jpedsurg.2017.02.018
37. Farrokhi F, Vaezi MF. Idiopathic (primary) achalasia. Orphanet J Rare Dis. 58. Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux
(2007) 2:38. symptom index (RSI). J Voice. (2002) 16:274–7. doi: 10.1016/s0892-1997(02)
38. Krishnan U. Eosinophilic esophagitis in children with esophageal atresia. Eur 00097-8
J Pediatr Surg. (2015) 25:336–44. 59. Mantegazza C, Mallardo S, Rossano M, Meneghin F, Ricci M, Rossi P, et al.
39. Rosolowski M, Kierzkiewicz M. Etiology, diagnosis and treatment of infectious Laryngeal signs and pH-multichannel intraluminal impedance in infants and
esophagitis. Prz Gastroenterol. (2013) 8:333–7. doi: 10.5114/pg.2013.39914 children: the missing ring: LPR and MII-pH in children. Dig Liver Dis. (2020)
40. Kadakuntla A, Juneja A, Sattler S, Agarwal A, Panse D, Zakhary N, 52:1011–6. doi: 10.1016/j.dld.2020.05.001
et al. Dysphagia, reflux and related sequelae due to altered physiology in 60. Schoepfer AM, Straumann A, Panczak R, Coslovsky M, Kuehni CE, Maurer E,
scleroderma. World J Gastroenterol. (2021) 27:5201–18. doi: 10.3748/wjg.v27. et al. Development and validation of a symptom-based activity index for adults
i31.5201 with eosinophilic esophagitis. Gastroenterology. (2014) 147:1255–66.e21. doi:
41. Ammoury RF, Pfefferkorn MD. Significance of esophageal Crohn disease in 10.1053/j.gastro.2014.08.028
children. J Pediatr Gastroenterol Nutr. (2011) 52:291–4. doi: 10.1097/MPG. 61. Warners MJ, Hindryckx P, Levesque BG, Parker CE, Shackelton LM, Khanna
0b013e3181ec21b5 R, et al. Systematic review: disease activity indices in eosinophilic esophagitis.
42. Bordea MA, Pirvan A, Sarban C, Margescu C, Leucuta D, Samasca G, et al. Am J Gastroenterol. (2017) 112:1658–69.
Pill -induced erosive esophagitis in children. Clujul Med. (2014) 87:15–8. 62. Franciosi JP, Hommel KA, DeBrosse CW, Greenberg AB, Greenler AJ, Abonia
doi: 10.15386/cjm.2014.8872.871.mab1 JP, et al. Development of a validated patient-reported symptom metric for
43. Hu SW, Chen AC, Wu SF. Drug-induced esophageal ulcer in adolescent pediatric eosinophilic esophagitis: qualitative methods. BMC Gastroenterol.
population: experience at a single medical center in central Taiwan. Medicina (2011) 11:126. doi: 10.1186/1471-230X-11-126
(Kaunas). (2021) 57:1286. doi: 10.3390/medicina57121286 63. Lucendo AJ, Molina-Infante J, Arias A, von Arnim U, Bredenoord AJ,
44. Dellon ES, Liacouras CA, Molina-Infante J, Furuta GT, Spergel JM, Zevit Bussmann C, et al. Guidelines on eosinophilic esophagitis: evidence-based
N, et al. Updated international consensus diagnostic criteria for eosinophilic statements and recommendations for diagnosis and management in children
esophagitis: proceedings of the AGREE conference. Gastroenterology. (2018) and adults. United European Gastroenterol J. (2017) 5:335–58. doi: 10.1177/
155:1022–33.e10. doi: 10.1053/j.gastro.2018.07.009 2050640616689525
45. Jarzebicka D, Czubkowski P, Sieczkowska-Golub J, Kierkus J, Kowalski A, 64. Taft TH, Carlson DA, Triggs J, Craft J, Starkey K, Yadlapati R, et al. Evaluating
Stefanowicz M, et al. Achalasia in children-clinical presentation, diagnosis, the reliability and construct validity of the Eckardt symptom score as a
long-term treatment outcomes, and quality of life. J Clin Med. (2021) 10:3917. measure of achalasia severity. Neurogastroenterol Motil. (2018) 30:e13287.
doi: 10.3390/jcm10173917 doi: 10.1111/nmo.13287
Frontiers in Pediatrics | www.frontiersin.org 10 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
65. Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with 76. Towbin AJ, Diniz LO. Schatzki ring in pediatric and young adult patients.
achalasia treated by pneumatic dilation. Gastroenterology. (1992) 103:1732–8. Pediatr Radiol. (2012) 42:1437–40. doi: 10.1007/s00247-012-2482-3
doi: 10.1016/0016-5085(92)91428-7 77. Lindholm EB, Hansbourgh F, Upp JR Jr., Cilloniz R, Lopoo J. Congenital
66. Marlais M, Fishman JR, Rawat DJ, Haddad M. Development and validation esophageal diverticulum - a case report and review of literature. J Pediatr Surg.
of a disease-specific quality-of-life measure for children with achalasia. Eur J (2013) 48:665–8.
Pediatr Surg. (2010) 20:92–4. doi: 10.1055/s-0029-1243622 78. Sun CF, Chen CH, Ke PZ, Ho TL, Lin CH. Esophageal duplication
67. Stapley S, Peters TJ, Neal RD, Rose PW, Walter FM, Hamilton W. The risk cyst presenting with stridor in a child with congenital pulmonary airway
of oesophago-gastric cancer in symptomatic patients in primary care: a large malformation: a case report and literature review. Medicine (Baltimore). (2019)
case-control study using electronic records. Br J Cancer. (2013) 108:25–31. 98:e16364. doi: 10.1097/MD.0000000000016364
68. Jones R, Latinovic R, Charlton J, Gulliford MC. Alarm symptoms in early
diagnosis of cancer in primary care: cohort study using General Practice Conflict of Interest: The authors declare that the research was conducted in the
Research Database. BMJ. (2007) 334:1040. doi: 10.1136/bmj.39171.637106.AE absence of any commercial or financial relationships that could be construed as a
69. Kakodkar K, Schroeder JW Jr. Pediatric dysphagia. Pediatr Clin North Am. potential conflict of interest.
(2013) 60:969–77.
70. Navaneethan U, Eubanks S. Approach to patients with esophageal Dysphagia. Publisher’s Note: All claims expressed in this article are solely those of the authors
Surg Clin North Am. (2015) 95:483–9. doi: 10.1016/j.suc.2015.02.004 and do not necessarily represent those of their affiliated organizations, or those of
71. Moroco AE, Aaronson NL. Pediatric dysphagia. Pediatr Clin North Am. (2022) the publisher, the editors and the reviewers. Any product that may be evaluated in
69:349–61. this article, or claim that may be made by its manufacturer, is not guaranteed or
72. Rommel N, Hamdy S. Oropharyngeal dysphagia: manifestations and endorsed by the publisher.
diagnosis. Nat Rev Gastroenterol Hepatol. (2016) 13:49–59.
73. Zerbib F, Omari T. Oesophageal dysphagia: manifestations and diagnosis. Nat Copyright © 2022 Lanzoni, Sembenini, Gastaldo, Leonardi, Bentivoglio, Faggian,
Rev Gastroenterol Hepatol. (2015) 12:322–31. doi: 10.1038/nrgastro.2014.195 Bosa, Gaio and Cananzi. This is an open-access article distributed under the terms
74. Ramaswamy K, Jacobson K, Jevon G, Israel D. Esophageal Crohn disease in of the Creative Commons Attribution License (CC BY). The use, distribution or
children: a clinical spectrum. J Pediatr Gastroenterol Nutr. (2003) 36:454–8. reproduction in other forums is permitted, provided the original author(s) and the
doi: 10.1097/00005176-200304000-00006 copyright owner(s) are credited and that the original publication in this journal
75. Nesheiwat Z, Akbar H, Kahloon A, Mahajan K. Radiation Esophagitis. is cited, in accordance with accepted academic practice. No use, distribution or
Treasure Island, FL: StatPearls (2022). reproduction is permitted which does not comply with these terms.
Frontiers in Pediatrics | www.frontiersin.org 11 June 2022 | Volume 10 | Article 885308
Lanzoni et al. Esophageal Dysphagia in Children
GLOSSARY
Antibiotic therapy, recent or ongoing prolonged antibiotic therapy; Atopy, former diagnosis of one or more atopic disorders; CI,
history of caustic ingestion; Esophageal atresia, previous surgery for esophageal atresia; GERD, gastroesophageal reflux disease;
Immunodeficiency, former diagnosis of congenital or acquired immunodeficiency; Lower GI symptoms, lower gastrointestinal
symptoms (e.g., abdominal pain, chronic diarrhea, blood in stool); Neurologic impairment, child with neurological disability; Pill-
capsule therapy, recent or ongoing treatment with pill or capsules; Radiotherapy, previous radiation therapy; Respiratory symptoms,
associated respiratory symptoms (e.g., cough, recurrent infections); Steroid therapy, recent or ongoing prolonged steroid treatment;
Esophageal surgery, previous surgery on the esophagus; Systemic sclerosis, former diagnosis of systemic sclerosis; Upper GI symptoms,
upper gastrointestinal symptoms (e.g., heartburn, epigastric pain, sour burps, regurgitation, vomit).
Frontiers in Pediatrics | www.frontiersin.org 12 June 2022 | Volume 10 | Article 885308
You might also like
- Confidentiality and Privacy in HealthcareDocument22 pagesConfidentiality and Privacy in Healthcarensen69No ratings yet
- Belsha2016 - INdication of EndosDocument9 pagesBelsha2016 - INdication of EndosThinh NguyenNo ratings yet
- (2022 - Frontiers in Pediatrics) Pediatric Inetstinal Pseudo-Obstruction Progress and ChallengesDocument11 pages(2022 - Frontiers in Pediatrics) Pediatric Inetstinal Pseudo-Obstruction Progress and ChallengesMel DíazNo ratings yet
- Nutrients: Malnutrition in Eosinophilic Gastrointestinal DisordersDocument12 pagesNutrients: Malnutrition in Eosinophilic Gastrointestinal DisordersSST KNo ratings yet
- Practices in Paediatric Gastrointestinal Endoscopy at Kenyatta National Hospital and Gertrudes Children's Hospital in Nairobi KenyaDocument11 pagesPractices in Paediatric Gastrointestinal Endoscopy at Kenyatta National Hospital and Gertrudes Children's Hospital in Nairobi Kenyafrankline nyabutoNo ratings yet
- Disfagia JPGN 2023Document8 pagesDisfagia JPGN 2023monicarodriguezsalas82No ratings yet
- 19d. CPG Article - ESPGHAN 2008Document42 pages19d. CPG Article - ESPGHAN 2008Aditya Angela AdamNo ratings yet
- Sintusek 2023Document20 pagesSintusek 2023rsthsn6z8xNo ratings yet
- Diagnosis and Management of Pediatric DysphagiaDocument9 pagesDiagnosis and Management of Pediatric DysphagiaHERNAN DANIEL RODRIGUEZ HERRERANo ratings yet
- Fped 09 705624Document7 pagesFped 09 705624iuliaNo ratings yet
- 1543-2165-134 6 815 PDFDocument11 pages1543-2165-134 6 815 PDFmmigod666No ratings yet
- Effect of Swallowing Rehabilitation Protocol On Swallowing Function in Patients With Esophageal Atresia Andor Tracheoesophageal Fistula.Document6 pagesEffect of Swallowing Rehabilitation Protocol On Swallowing Function in Patients With Esophageal Atresia Andor Tracheoesophageal Fistula.Anonymous xvlg4m5xLXNo ratings yet
- Endoscopy Findings in Dyspepsia PatientsDocument6 pagesEndoscopy Findings in Dyspepsia PatientsmalaNo ratings yet
- B Celiaca Al Toma PDFDocument31 pagesB Celiaca Al Toma PDFSimona JuncuNo ratings yet
- Environmental Enteric Dysfunction and Growth Failure/Stunting in Global Child HealthDocument12 pagesEnvironmental Enteric Dysfunction and Growth Failure/Stunting in Global Child HealthNurul RamadhiniNo ratings yet
- Am JPerinatol 2014Document7 pagesAm JPerinatol 2014VanessaGGSNo ratings yet
- Jurnal DisfagiaDocument19 pagesJurnal DisfagiaYenny FramelaNo ratings yet
- Management of Gastroesophageal Reflux Disease in Pediatric Patients A Literature ReviewDocument8 pagesManagement of Gastroesophageal Reflux Disease in Pediatric Patients A Literature ReviewAndhika DNo ratings yet
- Irritable Bowel Syndrome: A Disease Still Searching For Pathogenesis, Diagnosis and TherapyDocument15 pagesIrritable Bowel Syndrome: A Disease Still Searching For Pathogenesis, Diagnosis and TherapyGaudeamus IgiturNo ratings yet
- Instrumental Assessment of Pediatric DysphagiaDocument12 pagesInstrumental Assessment of Pediatric DysphagiaCarolina Lissette Poblete BeltránNo ratings yet
- PBD in Pediatric AchalasiaDocument6 pagesPBD in Pediatric AchalasiamuhammadfahmanNo ratings yet
- Advances in Evaluation of Chronic Diarrhea in InfantDocument21 pagesAdvances in Evaluation of Chronic Diarrhea in InfantDr. Faten AlKatebNo ratings yet
- Physiology & Behavior: Gastrointestinal Microbiota in Children With Autism in SlovakiaDocument9 pagesPhysiology & Behavior: Gastrointestinal Microbiota in Children With Autism in SlovakiaRezky FajrianiNo ratings yet
- WJG 18 4335Document7 pagesWJG 18 4335aalmadasalazarNo ratings yet
- Nihms 723708Document14 pagesNihms 723708Natalia G. SevillanoNo ratings yet
- Endoscopy in Pediatric Inflammatory Bowel DiseaseFrom EverandEndoscopy in Pediatric Inflammatory Bowel DiseaseLuigi Dall'OglioNo ratings yet
- Kasar Pkmrs BBBDocument5 pagesKasar Pkmrs BBBIriamana Liasyarah MarudinNo ratings yet
- Acute Appendicitis in Children PDFDocument6 pagesAcute Appendicitis in Children PDFMusyawarah MelalaNo ratings yet
- Otro MasDocument41 pagesOtro Masalba farran martiNo ratings yet
- Clinical Guidelines Secondary Prevention of Gastric CancerDocument1 pageClinical Guidelines Secondary Prevention of Gastric Cancerhenrique.uouNo ratings yet
- Feeding Problems Including Avoidant Restrictive Food Intake Disorder in Young Children With Autism Spectrum Disorder in A Multiethnic PopulationDocument12 pagesFeeding Problems Including Avoidant Restrictive Food Intake Disorder in Young Children With Autism Spectrum Disorder in A Multiethnic PopulationKaren MurilloNo ratings yet
- WilsonDocument11 pagesWilsonCarmen OpreaNo ratings yet
- Pediatric Gastroesophageal Reflux DiseaseDocument5 pagesPediatric Gastroesophageal Reflux Diseasegemala wahabNo ratings yet
- Prader WilliDocument15 pagesPrader WilliGVHHNo ratings yet
- Gastroschisis: Prenatal Diagnosis and OutcomeDocument16 pagesGastroschisis: Prenatal Diagnosis and OutcomeEnvhy WinaNo ratings yet
- Hidronefrosisi 1Document12 pagesHidronefrosisi 1Zwinglie SandagNo ratings yet
- Clinical Manifestations of Giambliasis in ChildrenDocument3 pagesClinical Manifestations of Giambliasis in ChildrenCentral Asian StudiesNo ratings yet
- Effectivity of Treatment For Children With Functional DyspepsiaDocument8 pagesEffectivity of Treatment For Children With Functional DyspepsiaBungaNo ratings yet
- Epidemiology Asia PIBD 2022Document16 pagesEpidemiology Asia PIBD 2022bowie135No ratings yet
- Estreñimiento y TeaDocument9 pagesEstreñimiento y TeaElena Martin LopezNo ratings yet
- Laryngomalacia and Swallowing Function in ChildrenDocument7 pagesLaryngomalacia and Swallowing Function in ChildrenmelaniaNo ratings yet
- Bowel Intussusception in Adult - Prevalence, Diagnostic Tools and Therapy 2021Document8 pagesBowel Intussusception in Adult - Prevalence, Diagnostic Tools and Therapy 2021吳醫師No ratings yet
- Lower Urinary Tract Function in Children and Adolescents Update ReportDocument11 pagesLower Urinary Tract Function in Children and Adolescents Update ReportAshwin KumarNo ratings yet
- Best Practice & Research Clinical GastroenterologyDocument16 pagesBest Practice & Research Clinical GastroenterologyAhmad IhsanNo ratings yet
- Diagnosis and Management of Bladder Bowel Dysfunction in Children With Urinary Tract Infections A Position Statement From The International Children's Continence Society.Document14 pagesDiagnosis and Management of Bladder Bowel Dysfunction in Children With Urinary Tract Infections A Position Statement From The International Children's Continence Society.Daniela Rodríguez MartínezNo ratings yet
- Jean Retrospective Analysis of Candida-Related Conditions in Childhood Cari SyO9CZhDocument5 pagesJean Retrospective Analysis of Candida-Related Conditions in Childhood Cari SyO9CZhIrsalina SalmaNo ratings yet
- Foreign Body and Caustic Ingestions in Children - A Clinical Practice GuidelineDocument16 pagesForeign Body and Caustic Ingestions in Children - A Clinical Practice GuidelineMaría José Medina MercadoNo ratings yet
- Guideline For The Evaluation of Cholestatic.23Document15 pagesGuideline For The Evaluation of Cholestatic.23Yuliawati HarunaNo ratings yet
- PAPER (ENG) - Swallowing Disturbance Questionnaire For Detecting DysphagiaDocument5 pagesPAPER (ENG) - Swallowing Disturbance Questionnaire For Detecting DysphagiaAldo Hip NaranjoNo ratings yet
- Standardization of pediatric LUT terminologyDocument11 pagesStandardization of pediatric LUT terminologyAhmad HaqulNo ratings yet
- Guarino 2014Document21 pagesGuarino 2014ChangNo ratings yet
- 1 s2.0 S1521691822000038 MainDocument1 page1 s2.0 S1521691822000038 Mainafg_19No ratings yet
- When The Limp Has A Dietary Cause - A Retrospective Study On Scurvy in A Tertiary Italian Pediatric HospDocument9 pagesWhen The Limp Has A Dietary Cause - A Retrospective Study On Scurvy in A Tertiary Italian Pediatric HospgistaluvikaNo ratings yet
- Feeding and Swallowing Issues in Genetic DisordersDocument11 pagesFeeding and Swallowing Issues in Genetic DisorderspaulaNo ratings yet
- Dysphonia in Children: Journal of Voice: Official Journal of The Voice Foundation July 2012Document5 pagesDysphonia in Children: Journal of Voice: Official Journal of The Voice Foundation July 2012Nexi anessaNo ratings yet
- Resumen: Funtional Abdominal Pain - PathogenesisDocument17 pagesResumen: Funtional Abdominal Pain - Pathogenesisjoal510No ratings yet
- Fimmu 12 620124Document18 pagesFimmu 12 620124mulooNo ratings yet
- Nutrients 14 03831Document11 pagesNutrients 14 03831Laura PiastrelliniNo ratings yet
- Organic Versus Functional: DyspepsiaDocument16 pagesOrganic Versus Functional: DyspepsiahelenaNo ratings yet
- DisfoniaDocument5 pagesDisfoniaRosario Crisóstomo PinochetNo ratings yet
- Summary of Andrew J. Wakefield's Waging War On The Autistic ChildFrom EverandSummary of Andrew J. Wakefield's Waging War On The Autistic ChildNo ratings yet
- NMZ 031Document11 pagesNMZ 0317 MNTNo ratings yet
- Kaac 002Document20 pagesKaac 0027 MNTNo ratings yet
- Ezz 330Document9 pagesEzz 3307 MNTNo ratings yet
- Czab 133Document9 pagesCzab 1337 MNTNo ratings yet
- Dmaa 046Document19 pagesDmaa 0467 MNTNo ratings yet
- Ocaa 179Document12 pagesOcaa 1797 MNTNo ratings yet
- SUC Involvement in Social Work EducationDocument23 pagesSUC Involvement in Social Work Education7 MNTNo ratings yet
- Scoping Studies. Towards A Methodological (2005)Document15 pagesScoping Studies. Towards A Methodological (2005)7 MNTNo ratings yet
- Gnac 060Document11 pagesGnac 0607 MNTNo ratings yet
- Reproductive Health Policy Saga: Restrictive Abortion Laws in Low-And Middle-Income Countries (Lmics), Unnecessary Cause of Maternal MortalityDocument20 pagesReproductive Health Policy Saga: Restrictive Abortion Laws in Low-And Middle-Income Countries (Lmics), Unnecessary Cause of Maternal Mortality7 MNTNo ratings yet
- Pnab 038Document9 pagesPnab 0387 MNTNo ratings yet
- Ooz 071Document9 pagesOoz 0717 MNTNo ratings yet
- Torsión de Órganos Abdominales y Pélvicos. Una Revisión (2020)Document6 pagesTorsión de Órganos Abdominales y Pélvicos. Una Revisión (2020)7 MNTNo ratings yet
- Datos 3Document17 pagesDatos 37 MNTNo ratings yet
- Opioides en Pacientes Ancianos Con Deterioro Cognitivo. Una Revisión Narrativa (2022)Document14 pagesOpioides en Pacientes Ancianos Con Deterioro Cognitivo. Una Revisión Narrativa (2022)7 MNTNo ratings yet
- Síndrome de Dolor Miofascial Temporomandibular. Etiología y Modulación Biopsicosocial. La Revisión Narrativa (2021)Document16 pagesSíndrome de Dolor Miofascial Temporomandibular. Etiología y Modulación Biopsicosocial. La Revisión Narrativa (2021)7 MNTNo ratings yet
- Datos UnoDocument9 pagesDatos Uno7 MNTNo ratings yet
- Andreas Kousios, Panayiotis Kouis, Alexandros Hadjivasilis, and Andrie PanayiotouDocument15 pagesAndreas Kousios, Panayiotis Kouis, Alexandros Hadjivasilis, and Andrie Panayiotou7 MNTNo ratings yet
- El Papel de La Tecnología de Realidad Extendida en La Educación Sanitaria. Hacia Un Enfoque Centrado en El Alumno (2021)Document6 pagesEl Papel de La Tecnología de Realidad Extendida en La Educación Sanitaria. Hacia Un Enfoque Centrado en El Alumno (2021)7 MNTNo ratings yet
- Multimorbilidad y Polifarmacia en Personas Mayores. Desafíos y Oportunidades para La Práctica Clínica (2020)Document11 pagesMultimorbilidad y Polifarmacia en Personas Mayores. Desafíos y Oportunidades para La Práctica Clínica (2020)7 MNTNo ratings yet
- Negar La Verdad No Cambia Los Hechos. Un Análisis Sistemático de La Negación Pseudocientífica Del Síndrome de Dolor Regional Complejo (2021)Document18 pagesNegar La Verdad No Cambia Los Hechos. Un Análisis Sistemático de La Negación Pseudocientífica Del Síndrome de Dolor Regional Complejo (2021)7 MNTNo ratings yet
- Comprender Los Factores Psicológicos, Fisiológicos y Genéticos Que Afectan La Medicina Del Dolor de Precisión. La Revisión Narrativa (2021)Document17 pagesComprender Los Factores Psicológicos, Fisiológicos y Genéticos Que Afectan La Medicina Del Dolor de Precisión. La Revisión Narrativa (2021)7 MNTNo ratings yet
- Mantenimiento de La Actividad Física. Una Revisión Narrativa Crítica y Direcciones para Futuras Investigaciones (2021)Document13 pagesMantenimiento de La Actividad Física. Una Revisión Narrativa Crítica y Direcciones para Futuras Investigaciones (2021)7 MNTNo ratings yet
- Rheumatic Heart Disease Anno 2020. Impacts of Gender and Migration On Epidemiology and Management (2020)Document9 pagesRheumatic Heart Disease Anno 2020. Impacts of Gender and Migration On Epidemiology and Management (2020)7 MNTNo ratings yet
- Componentes Anatómicos e Histológicos de La Zona Bilaminar de La Articulación Temporomandibular. Una Revisión Narrativa (Chile-2021)Document7 pagesComponentes Anatómicos e Histológicos de La Zona Bilaminar de La Articulación Temporomandibular. Una Revisión Narrativa (Chile-2021)7 MNTNo ratings yet
- Azadirachta Indica (Neem) Como Potencial Activo Natural para Productos Dermocosméticos y Tópicos. Una Revisión Narrativa (Brasil-2022)Document17 pagesAzadirachta Indica (Neem) Como Potencial Activo Natural para Productos Dermocosméticos y Tópicos. Una Revisión Narrativa (Brasil-2022)7 MNTNo ratings yet
- Modelos Animales de Lesión Espinal para Estudiar El Dolor de Espalda y SCI (2020)Document6 pagesModelos Animales de Lesión Espinal para Estudiar El Dolor de Espalda y SCI (2020)7 MNTNo ratings yet
- Ciencias Del Comportamiento en La Optimización de La Terapia Farmacológica y No Farmacológica para La Diabetes Tipo 2 (2021)Document19 pagesCiencias Del Comportamiento en La Optimización de La Terapia Farmacológica y No Farmacológica para La Diabetes Tipo 2 (2021)7 MNTNo ratings yet
- Vitamin D and Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD) - An Update (2020)Document14 pagesVitamin D and Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD) - An Update (2020)7 MNTNo ratings yet
- District Environment Plan - BalrampurDocument51 pagesDistrict Environment Plan - BalrampurVikas SrivastavaNo ratings yet
- ARBR 2806 Edit ReportDocument5 pagesARBR 2806 Edit ReportJosé Manuel Valencia GallardoNo ratings yet
- NCP-Deficient Fluid VolumeDocument1 pageNCP-Deficient Fluid Volumejanmichael8No ratings yet
- Mabini National High School Midterm Exam ReviewDocument3 pagesMabini National High School Midterm Exam ReviewRoseann EnriquezNo ratings yet
- 68-Article Text-809-1-10-20230904Document12 pages68-Article Text-809-1-10-20230904w6pz4fnn6wNo ratings yet
- Higado Graso No Alcoholico y Niveles de PCRDocument6 pagesHigado Graso No Alcoholico y Niveles de PCRperuliz19No ratings yet
- Actual Nursing DiagnosisDocument4 pagesActual Nursing DiagnosisJp CasperNo ratings yet
- A Single-Arm Study To Evaluate The Transfer of Drospirenone To Breast Milk After Reaching Steady State, Following Oral Administration of 4 MG Drospirenone in Healthy Lactating Female VolunteersDocument7 pagesA Single-Arm Study To Evaluate The Transfer of Drospirenone To Breast Milk After Reaching Steady State, Following Oral Administration of 4 MG Drospirenone in Healthy Lactating Female VolunteersfadhilNo ratings yet
- RPT F2 Science DLP 2018Document19 pagesRPT F2 Science DLP 2018Mei Shan SiowNo ratings yet
- Daconil 720 SC: Safety Data SheetDocument9 pagesDaconil 720 SC: Safety Data SheetAngelicaNo ratings yet
- Food Security - Definition and Measurement PDFDocument3 pagesFood Security - Definition and Measurement PDFFristhaPratiwi100% (1)
- Population Trends in INDIADocument8 pagesPopulation Trends in INDIAcheedikrishnaNo ratings yet
- Fitness Testing Guide PDFDocument10 pagesFitness Testing Guide PDFdodovadaNo ratings yet
- Fecalysis: Verian John Hoo - Sudario College of Medical TechnologyDocument58 pagesFecalysis: Verian John Hoo - Sudario College of Medical Technologyepson printerNo ratings yet
- NCLEX-RN Test Plan 2010Document10 pagesNCLEX-RN Test Plan 2010PhilippineNursingDirectory.com100% (1)
- Nutrition Care Process Note-IcuDocument2 pagesNutrition Care Process Note-Icuapi-1032325430% (1)
- Gym PlanDocument56 pagesGym PlanAlize Ch0% (1)
- West Kazakhstan UniversityDocument3 pagesWest Kazakhstan UniversityshahulNo ratings yet
- AmJClinNutr 2014 Weaver 1525 42 3Document19 pagesAmJClinNutr 2014 Weaver 1525 42 3Dijana NaloskaNo ratings yet
- Core Values Safe Quality NursingDocument8 pagesCore Values Safe Quality NursingAzhily Jones HisolerNo ratings yet
- With Answers No RationaleDocument41 pagesWith Answers No RationaleronnaxNo ratings yet
- No Article Title Time of Publication Authors Journal Name Received Date Revised Date Accepted DateDocument4 pagesNo Article Title Time of Publication Authors Journal Name Received Date Revised Date Accepted DateAnin Kalma MartadinataNo ratings yet
- GRADE 8 Teaching Guide Catchup Bullying and Its Impact On Mental Health Health 8Document6 pagesGRADE 8 Teaching Guide Catchup Bullying and Its Impact On Mental Health Health 8iamtherealjuandelacruzNo ratings yet
- W9 Teori Akuntansi RS ASPDocument4 pagesW9 Teori Akuntansi RS ASPJessicaNo ratings yet
- The FGM Initiative Final Report 2013Document61 pagesThe FGM Initiative Final Report 2013TinaStiffNo ratings yet
- Comparison of Supervised Exercise and Home Exercise After Ankle FractureDocument6 pagesComparison of Supervised Exercise and Home Exercise After Ankle FractureKaren MuñozNo ratings yet
- Research Proposal On Fast FoodDocument8 pagesResearch Proposal On Fast FoodManish Ravat100% (5)
- MAPEH 6- WEEK 1 ActivitiesDocument4 pagesMAPEH 6- WEEK 1 ActivitiesCatherine Renante100% (2)
- (Edited) N31-G6-SOP-and-Conceptual-FrameworkDocument5 pages(Edited) N31-G6-SOP-and-Conceptual-Frameworkst michael machine shopNo ratings yet