Professional Documents
Culture Documents
OB 1S 1 Maternal Anatomy
Uploaded by
Kiara Loren DinglasanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
OB 1S 1 Maternal Anatomy
Uploaded by
Kiara Loren DinglasanCopyright:
Available Formats
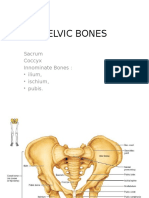
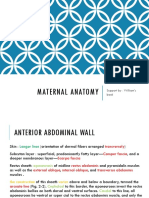
OBSTETRICS MATERNAL ANATOMY:
1S-1 | CEU-SOM A & B External and Internal
Dr. Ronaldo Santos Generative Organs
OUTLINE
Hesselbach Triangle
I. ANTERIOR ABDOMINAL WALL Boundaries:
II. EXTERNAL GENERATIVE ORGANS o Inferior: inguinal ligament
III. INTERNAL GENERATIVE ORGANS o Medial: lateral border of rectus muscles
IV . REFERENCES o Lateral: inferior epigastric vessels
Clinical significance:
I. ANTERIOR ABDOMINAL WALL o Direct hernias – involve the Hesselbach triangle
confines abdominal viscera o Indirect hernias – involve the deep inguinal ring
stretches to accommodate the expanding uterus
provides surgical access to the internal reproductive organs
Skin
Langer lines – describe the orientation of dermal fibers
o in the abdomen, transversely arranged
o vertical skin incisions – more tension, w ider scars
o low transverse incisions (Pfannenstiel) – follow
Langer lines; superior cosmetic results
Subcutaneous layer
Camper’s fascia
o superficial
o predominantly fatty layer
Scarpa’s fascia
o deeper
o more membranous layer
These are not discrete layers but instead represent a
continuum of the subcutaneous tissue layer Innervation:
Intercostal nerves (T7-T11)
Rectus Sheath – fibrous aponeuroses of the external oblique, internal Subcostal nerve (T12)
oblique, and transversus abdominis muscles join in the midline Iliohypogastric nerve – skin over suprapubic area
Ilioinguinal nerves (L1) – skin of the low er abdominal w all,
Arcuate line
upper portion of the labia majora, medial portion of the thigh
Cephalad – aponeuroses invest the rectus abdmoninis bellies T10 dermatome – approximates the level of the umbilicus
above and below
Caudal – all aponeuroses lie anterior to the rectus abdominis Clinical Significance
muscle, and only the thin transversalis fascia and peritoneum Ilioinguinal and iliohypogastric nerves
lie beneath o can be entrapped during closure of low transverse
incisions, especially if incisions extend beyond the
lateral borders of the rectus muscle
o carry sensory information only, and injury leads to
loss of sensation w ithin the areas supplied
II. EXTERNAL GENERATIVE ORGANS
PUDENDA or VULVA – includes all structures visible externally from
the pubis to the perineum: mons pubis, labia majora and minora, clitoris,
hymen, vestibule, urethral opening, and various glandular and vascular
structures
Blood Supply
Branches of fem oral artery – supply the skin and
subcutaneous layers of the anterior abdominal w all and mons
pubis
o Superficial epigastric artery
o Superficial circumflex iliac artery
o External pudendal artery
Branches of external iliac artery – supply the muscles and
fascia of the anterior abdominal w all
o Inferior deep epigastric vessels
o Deep circumflex iliac vessels kadiri ew w w
1S-1 MATERNAL ANATOMY REYES @yourroyalkateness | ROCHA @giannisrocha ①
OBSTETRICS MATERNAL ANATOMY:
1S-1 | CEU-SOM A & B External and Internal
Dr. Ronaldo Santos Generative Organs
Mons Pubis o lie inferior to the vestibular bulbs and deep to the
also called m ons veneris inferior ends of the bulbocavernosus muscle
fat-filled cushion that lies over the symphysis pubis o ducts are 1.5 to 2 cm long and open distal to the
at puberty, covered by curly hair that forms the escutcheon hymenal ring at 5 & 7 o’clock
in adult w omen, it is distributed in a triangular area o Clinical significance:
its base forms the upper margin of the symphysis pubis Follow ing trauma or infection, either duct
may sw ell and obstruct to form a cyst, or
Labia m ajora if infected, an abscess
male homologue: scrotum Paraurethral Glands
it is w here the round ligament terminate (upper border) o lies in the inferior aspect of the urethra
outer surface with hair w hile inner surface without hairs o Skene glands – largest
o in children and nulliparous w omen – close o Minor vestibular glands – are shallow glands lined
apposition by simple mucin-secreting epithelium and open
o in multiparous w omen – gapes w idely along Hart line
continuous directly w ith the mons pubis o Clinical significance:
Inflammation and duct obstruction of any
merge posteriorly to form the posterior commissure
of the paraurethral glands can lead to a
urethral diverticulum formation
Labia m inora
composed of connective tissue w ith many vessels and some Vestibular Bulbs
smooth muscular fibers male homologue: corpus spongiosum of the penis
moist and reddish, similar in appearance to a mucous
almond-shaped, mainly composed of aggregations of veins
membrane
o 3 to 4 cm long, 1 to 2 cm w ide, and 0.5 to 1 cm thick
extremely sensitive because it is supplied w ith many nerve
lie beneath the bulbocavernosus muscle on either side of the
endings
vestibule
2 lamellae superiorly
Clinical significance:
o Low er pair: forms the frenulum of the clitoris
o during childbirth, the vesibular bulbs may be injured
o Upper pair: forms the prepuce and may even rupture to create a vulvar
inferiorly, it forms the fourchette
hem atoma
lining epithelium
o Outer and lateral portion of inner surface – VAGINAL OPENING AND HYMEN
stratified squamous epithelium
o Medial portion – non-keratinized squamous Vaginal opening
epithelium rimmed distally by the hymen or its remnants
o Hart line – demarcation line betw een lateral and
medial portions Hym en
o contains sebaceous follicles, few sweat glands
membrane surrounding the vaginal opening
o lacks hair follicles, eccrine glands, and apocrine
composed of elastic and collagenous connective tissue
glands
covered by stratified squamous epithelium
the aperture of the hymen varies
Clitoris
male homologue: penis Hymen is torn at several sites during first coitus. Identical
composed of a glans, a corpus, and tw o crura tears may occur by other penetration. The edges of the torn
rarely exceeds 2 cm in length hymen soon reepithelialize – hymenal caruncle
Im perforate hymen – rare lesion in w hich the vaginal orifice
covered by stratified squamous epithelium that is richly
is occluded completely, causing retention of menstrual blood
supplied w ith nerve ending
principal female erogenous organ
Vestibule
from embryonic urogenital membrane
almond-shaped
Boundaries:
o Lateral – Hart line
o Medial – external surface of hymen
o Anterior – frenulum
o Posterior – fourchette
6 openings:
o Urethra
o Vagina
o Ducts of the Bartholin glands (2)
o Ducts of the paraurethral glands/Skene glands (2)
Vestibular Glands
Bartholin’s glands
o greater vestibular glands
o 0.5 to 1 cm in diameter
saan dyan yung sa’yo char
1S-1 MATERNAL ANATOMY REYES @yourroyalkateness | ROCHA @giannisrocha ②
OBSTETRICS MATERNAL ANATOMY:
1S-1 | CEU-SOM A & B External and Internal
Dr. Ronaldo Santos Generative Organs
Vagina PERINEUM
musculo-membranous structure the diamond area betw een the thighs
extends from the vulva to the uterus boundaries are same as those of the bony pelvic outlet
interposed anteriorly and posteriorly betw een the urinary o Anterior: pubic symphysis
bladder and the rectum o Posterior: ischiopubic rami
lining epithelium: non-keratinized stratified squamous o Anterolateral: ischial tuberosities
epithelium o Posterolateral: sacrotuberous ligaments
no glands; abundant vascular supply o Posterior: coccyx
Embryology: blood supply:
o upper portion – m üllerian ducts o Internal pudendal artery (inferior rectal artery
o low er portion – urogenital sinus and posterior labial artery
Anterior Triangle – also called urogenital triangle
Boundaries: further subdivided into:
o Anteriorly, the vagina is separated from the bladder o Superficial space – closed compartment
and urethra by connective called – vesicovaginal o Deep space – continuous superiorly with the
septum pelvic cavity
o Posteriorly, there are similar tissues together that boundaries:
form the rectovaginal septum between the lower o Superior: pubic rami
portion of the vagina and the rectum o Lateral: ischial tuberosities – divides the perineum
o The upper fourth of the vaginal is separated from into anterior and posterior triangle
the rectum by the rectouterine pouch or cul de o Posterior: superficial transverse perineal muscle
sac of Douglas
Length: SUPERFICIAL SPACE OF THE ANTERIOR TRIANGLE
o Anterior: 6-8 cm • Attached at the ischial tuberosity
o Posterior: 7-10 cm attached at the ischial tuberosity and
subdivided by the cervix into fornices – anterior, posterior, Ischiocavernosus crus of clitoris helps maintain
lateral clitoral erection
the fornices are clinically important because the internal pelvic
organs can be palpated through their thin w alls • Overly the vestibular bulb and
Bartholin glands
o posterior fornix provides surgical access to the
peritoneal cavity • Attached at the perineal body and
the clitoris
Bulbocavernosus
• Constrict the vaginal lumen and aid
in the release of secretions of the
Bartholin’s gland
• Contributes to clitoral erection
• Attached to the ischial tuberosities
Superficial transverse laterally and the perineal body
perineal m uscles medially
TERM BLOOD LYMPHATIC DEEP SPACE OF THE ANTERIOR TRIANGLE
SUPPLY DRAINAGE Deep to the perineal membrane and extends up continuous superiorly
Cervicovaginal External, internal and w ith the pelvic cavity
branches of uterine common iliac nodes
UPPER THIRD artery and vaginal Contains: compressor urethrae, urethrovaginal sphincter muslces,
artery external urethral sphincter, parts of urethra and vagina, branches of
internal pudendal artery, dorsal nerve and vein of the clitoris
MIDDLE Inferior vesical Internal iliac nodes
THIRD arteries Posterior Triangle – also called the anal triangle which contains the
Middle rectal and Inguinal nodes follow ing:
LOWER THIRD internal pudendal Ischiorectal fossa
arteries o tw o fat filled w edge shaped spaces on either side of
the anal canal
1S-1 MATERNAL ANATOMY REYES @yourroyalkateness | ROCHA @giannisrocha ③
OBSTETRICS MATERNAL ANATOMY:
1S-1 | CEU-SOM A & B External and Internal
Dr. Ronaldo Santos Generative Organs
o provide support to surrounding structures, yet allow o Bulbocavernosus muscle
distension of the rectum during defecation and o Superficial transverse perineal muscles
stretching of the vagina during delivery o External anal sphincter
o this continuity of the fossae across perineal potential morbidity:
compartments allow s fluid, infection and o episiotomy may injure the perineal body
malignancy to spread o pudendal nerve injury may be associated with
Anal canal and anal sphincter complex concurrent perineal body injury
o lie in the center of the fossae
Branches of the internal pudendal vessels III. INTERNAL GENERATIVE ORGANS
Pudendal nerve
o formed by the anterior rami of S2-S4 DEVELOPMENT OF THE INTERNAL GENERATIVE ORGANS
o lies posteromedial to the ischial spines
o 3 terminal branches:
Dorsal nerve of the clitoris – supplies
the skin of the clitoris
Perineal nerve – supplies the muscles of
the anterior triangle and labial skin
Inferior rectal nerve – supplies the
external anal sphincter, anal canal’s
mucous membrane, and perineal skin
EMBRYOLOGICAL DEVELOPMENT
fusion of the tw o müllerian (paramesonephric) ducts to form a
ANUS single canal begins at the level of the inguinal crest, that is,
the gubernaculum (primordium of the round ligament) – 5th
External Anal Sphincters w eek of development
a ring of striated muscle attached to the perineal body upper ends of the müllerian ducts produce the oviducts and
anteriorly and the coccyx posteriorly the fused parts give rise to the uterus
maintains the constant state of resting contraction
the vaginal canal is not patent throughout its entire length until
receives blood supply from the inferior rectal artery the sixth month of fetal life
motor fibers come from the inferior rectal branch of the
pudendal nerve
Internal Anal Sphincter
contributes the bulk of the anal canal resting pressure for fecal
continence
formed by the distal continuation of the inner circular muscle
layer of the rectum and colon
Anal Cushion
highly vascularized
aids in fecal continence
engorgement due to increased uterine size, excessive
straining and hard stools, can increase venous engorgement
w ithin these cushions to form hem orrhoids
Perineal Body
anchors the anorectum; also anchors the vagina
helps maintains urinary and fecal continence
maintains the orgasmic platform
prevents expansion of the urogenital hiatus
provides a physical barrier betw een the vagina and rectum
the structures that contribute to the perineal body are the ff:
o Median raphe of the levator ani
o Central tendon of the perineum
1S-1 MATERNAL ANATOMY REYES @yourroyalkateness | ROCHA @giannisrocha ④
OBSTETRICS MATERNAL ANATOMY:
1S-1 | CEU-SOM A & B External and Internal
Dr. Ronaldo Santos Generative Organs
INTERNAL GENERATIVE ORGANS
Layers of the uterus:
o Serosa (serosal layer)
• formed by the peritoneum that covers the
uterus
Cervix o Myom etrium (muscular layer)
Internal cervical os • bundles of smooth muscle united by
o upper boundary; level at w hich the peritoneum is connective tissue in w hich there are
reflected up onto the bladder many elastic fibers
Portio supravaginalis • relative more muscle in the inner w all
o covered by peritoneum on its posterior surface than the outer w all, and in the anterior
o attached to the cardinal ligaments laterally and posterior w alls than in the lateral
Portio vaginalis w alls
External cervical os before childbirth: small, oval opening • muscle fibers diminish caudally such that
External cervical os after childbirth: transverse slit, giving rise the muscle comprises only 10% of the
to the anterior and posterior cervical lip tissue mass in the cervix
Cervical stroma – compose mainly of collagen, elastin and • the interlacing myometrial fibers that
proteoglycan but very little smooth muscle surround the myometrial vessels are
Ectocervix – nonkeratinized squamous epithelium integral to control of bleeding from the
Endocervix – mucin-secreting columnar epithelium placental site during the third stage of
labor
o Endom etrium (mucosal layer)
• thin, pink, velvet-like membrane
perforated by a large number of minute
ostia of the uterine glands.
• histologically, its epithelium is single
layer of closely packed high columnar
cells than rests on a thin basement
membrane
• Uterine glands – invaginations of the
epithelieum that extend to the
myometrium
• Interglandular m esenchymal stroma –
varies remarkably throughout the ovarian
cycle, undergoes decidualization
follow ing ovulation
Uterus
Thick- w alled, hollow , muscular organ
Nulliparous: 6-8cm, fundus and cervix almost equal in length
Multiparous: 9-10cm, cervix is 1/3 of the total length
Entire posterior w all of the uterus is covered by serosa, or
peritoneum, the low er portion of w hich forms the anterior
boundary of the recto-uterine cul-de-sac or pouch of
Douglas.
Blood supply:
o Uterine artery
o Ovarian artery
Parts of uterus:
o Corpus or body
o Cervix
o Isthmus – between the internal cervical os and the
endometrial cavity; forms the lower uterine segment
during pregnancy
o Cornua – at the junction of the superior and lateral
margins
o Fundus – convex upper segment betw een the
points of insertion of the fallopian tubes
1S-1 MATERNAL ANATOMY REYES @yourroyalkateness | ROCHA @giannisrocha ⑤
OBSTETRICS MATERNAL ANATOMY:
1S-1 | CEU-SOM A & B External and Internal
Dr. Ronaldo Santos Generative Organs
• Vascular architecture of Endometrium Ovaries
Uterine and ovarian arteries arcuate arteries vary considerably in size.
radial arteries spiral/coiled arteries and o During childbearing years, they are from 2.5 to 5 cm
basal/straight arteries in length, 1.5 to 3 cm in breadth, and 0.6 to 1.5 cm
Spiral arteries – mid-portion and superficial third of in thickness.
the endometrium, responsive to hormones o After menopause, ovarian size diminishes
Basal arteries – basal layer, not responsive to remarkably.
hormones rest in a slight depression on the lateral w all of the pelvis,
called ovarian fossa of Waldeyer between the divergent
Round Ligam ents external and internal iliac vessels
extend from the lateral portion of the uterus attached to the broad ligament by the m esovarium
arise below and anterior to the origin of the oviducts. the parts include the follow ing:
terminate in the upper portion of the labium majus. o Cortex – outer layer, contains oocytes and
Sampson artery runs w ithin this ligament. developing follicles
corresponds embryologically to the gubernaculum testis of o Medulla – central portion, composed of loose
men connective tissue
clinically significant w hen doing puerperal tubal sterilization the ovaries are supplied w ith both sympathetic nerves from
the ovarian plexus and parasympathetic nerves
Broad Ligam ents
w ing-like structures from lateral margins to pelvic sidew all
each consist of an anterior leaf and a posterior leaf
drapes over structures extending from the cornu
mesosalpinx, mesoteres, mesovarium, mesometrium
suspensory ligament or infundibulopelvic ligament – from the
fimbriated end of the f allopian tube to the pelvic w all, where
ovarian vessels traverse
Cardinal Ligaments
transverse cervical or Mackendrodt ligament
thick base of the broad ligament that is continuous w ith the
connective tissue of the pelvic floor
Uterosacral Ligaments
from its attachment posterolaterally to the supravaginal
portion of the cervix and inserts into the fascia over the sacrum Lym phatics
form the lateral boundaries of the pouch of Douglas Cervix – terminate mainly in the hypogastric nodes, which are
situated near the bifurcation of the common iliac vessels.
Fallopian Tubes Body of the uterus – internal iliac nodes and periaortic lymph
also called oviducts nodes
vary in length from 8 to 14 cm.
lumen is lined by mucous membrane
IV. REFERENCES
its parts consist:
o interstitial portion
o isthmus Lecture PPT of Dr. Santos
o ampulla Clinical Anatomy by Regions, 9th Edition (Snell, 2011)
o infundibulum or fimbriated extremity – funnel- YL1 Anatomy Trans (Tinio et al, 2018)
shaped opening at the distal
tubal smooth muscle: inner circular and outer longitudinal,
undergo rhythmic contraction or peristalsis tow ard the uterine
cavity
epithelium in close contact w ith muscle layer because there is
no submucosa
epithelium – columnar cells (some ciliated, others secretory)
ไม่ง่ายเลยคุณก็แข็งแรงขึ้น
“It never gets easier, you just get stronger.”
1S-1 MATERNAL ANATOMY REYES @yourroyalkateness | ROCHA @giannisrocha ⑥
You might also like
- Abortion and Sterilization: Medical and Social AspectsFrom EverandAbortion and Sterilization: Medical and Social AspectsJane E. HodgsonNo ratings yet
- 2023 OB/GYN Coding Manual: Components of Correct CodingFrom Everand2023 OB/GYN Coding Manual: Components of Correct CodingNo ratings yet
- (Gyne) 2.1 PCOS, Hyperandrogenism & Hyperprolactenemia (OnaCruz) - WiniDocument10 pages(Gyne) 2.1 PCOS, Hyperandrogenism & Hyperprolactenemia (OnaCruz) - WiniDexter IanNo ratings yet
- Total Abdominal HysterectomyDocument19 pagesTotal Abdominal HysterectomyMeidina Rachma Amanda100% (1)
- Pelvic Inflammatory Disease by SlidesgoDocument51 pagesPelvic Inflammatory Disease by SlidesgoGina MorenoNo ratings yet
- Obstetric Anal Sphincter Injury (OASIS) - UpToDateDocument39 pagesObstetric Anal Sphincter Injury (OASIS) - UpToDateErickNo ratings yet
- Presented by DR - Shahbaz Ahmad Professor of Community MedicineDocument76 pagesPresented by DR - Shahbaz Ahmad Professor of Community MedicinePriya bhattiNo ratings yet
- Pelvic BoneDocument15 pagesPelvic BoneYoanneveline TanakNo ratings yet
- Cardiac Disease in PregnancyDocument28 pagesCardiac Disease in PregnancyviharadewiNo ratings yet
- Claire Maevelle A. Laxamana BSP - 3ADocument10 pagesClaire Maevelle A. Laxamana BSP - 3ACLaire Maevelle Angeles LaxamanaNo ratings yet
- Surgery - Data Show (All-In-One Collections)Document399 pagesSurgery - Data Show (All-In-One Collections)anmar alkhudhriNo ratings yet
- Benign and Malignant Ovarian Tumors: Case 1Document14 pagesBenign and Malignant Ovarian Tumors: Case 1Charrie RagadiNo ratings yet
- Rapid Review of Hematology (Aug 31, 2013) - (9350909618) - (Jaypee Brothers Medical Pub)Document149 pagesRapid Review of Hematology (Aug 31, 2013) - (9350909618) - (Jaypee Brothers Medical Pub)Dana AhmedNo ratings yet
- PulseDocument43 pagesPulseAngelo LacisteNo ratings yet
- GEN GallBladderInstrumentsADocument10 pagesGEN GallBladderInstrumentsANeo Rodriguez AlvaradoNo ratings yet
- Evaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusDocument7 pagesEvaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusGabyliz Gonzalez CastilloNo ratings yet
- Disorder of Sex DevelopmentDocument40 pagesDisorder of Sex DevelopmentAndi AdityaNo ratings yet
- ANATOMY OF FEMALE InternalDocument49 pagesANATOMY OF FEMALE InternalJohaifha CompaniaNo ratings yet
- Ob-Gyn Review Part 3Document101 pagesOb-Gyn Review Part 3filchibuffNo ratings yet
- Foreign Body in Pharynx, Larynx, Trachea & Tracheobronchial TreeDocument26 pagesForeign Body in Pharynx, Larynx, Trachea & Tracheobronchial TreehashyNo ratings yet
- Normal Conduct of LaborDocument62 pagesNormal Conduct of LaborFaye Cabotaje LinganNo ratings yet
- Conduct of LaborDocument8 pagesConduct of LaborChristine Evan HoNo ratings yet
- Pregnancy and Labor at Fetal Malpresentations and Abnormal PelvisDocument40 pagesPregnancy and Labor at Fetal Malpresentations and Abnormal PelvisCoral Srinivasa Ramalu100% (1)
- Hepatitis B in PregnancyDocument17 pagesHepatitis B in PregnancysnazzyNo ratings yet
- Breast Cancer - McMaster Pathophysiology Review PDFDocument8 pagesBreast Cancer - McMaster Pathophysiology Review PDFAprilla Ayu W.No ratings yet
- Breast MassDocument38 pagesBreast MassLester Paul SivilaNo ratings yet
- Mass in Epigastrium-2Document37 pagesMass in Epigastrium-2brown_chocolate87643100% (1)
- Ultrasound-Guided Invasive Procedures in ObstetricsDocument18 pagesUltrasound-Guided Invasive Procedures in ObstetricsariNo ratings yet
- Obs History Taking FormatDocument24 pagesObs History Taking FormatBibek PandeyNo ratings yet
- Procedural ReportDocument14 pagesProcedural ReportiamcharraeNo ratings yet
- د.عبد الزهره THE GYNAECOLOGICAL EXAMINATION-1 (Muhadharaty)Document29 pagesد.عبد الزهره THE GYNAECOLOGICAL EXAMINATION-1 (Muhadharaty)MohammedNo ratings yet
- Gyne ReflectionDocument18 pagesGyne ReflectionKC Dela RosaNo ratings yet
- Second Trimester Complications 2015Document64 pagesSecond Trimester Complications 2015gibreilNo ratings yet
- Cervical CancerDocument6 pagesCervical CancerCnette S. LumboNo ratings yet
- Urodynamics: Committee 7Document56 pagesUrodynamics: Committee 7Coral Garcia RiveraNo ratings yet
- FIGO Cancer Report 2018 PDFDocument128 pagesFIGO Cancer Report 2018 PDFAndi Tiara S. AdamNo ratings yet
- Obstetrics and Gynecological InstrumentsDocument31 pagesObstetrics and Gynecological InstrumentsGAYATHRI RAKESHNo ratings yet
- Endometriosis With Salpingitis Simulating Acute AppendicitisDocument20 pagesEndometriosis With Salpingitis Simulating Acute AppendicitisWyendae CliquersNo ratings yet
- Care of A Client With: Neonatal Pneumonia: University of Southern Philippines Foundation Salinas Drive, Lahug, Cebu CityDocument22 pagesCare of A Client With: Neonatal Pneumonia: University of Southern Philippines Foundation Salinas Drive, Lahug, Cebu CityAsterlyn ConiendoNo ratings yet
- Tog Journal 2016Document61 pagesTog Journal 2016thevijay007100% (1)
- AUVARD Vaginal SpeculaDocument24 pagesAUVARD Vaginal SpeculaRoy SandiNo ratings yet
- Congenital Anomelies of Reproductive OrgansDocument47 pagesCongenital Anomelies of Reproductive Organsdr_shamimrNo ratings yet
- CPG Uterine InversionDocument3 pagesCPG Uterine InversionRahmayanti YuliaNo ratings yet
- CTT InsertionDocument18 pagesCTT InsertionRen-Ren NazarenoNo ratings yet
- The Management of Asherman Syndrome: A Review of LiteratureDocument11 pagesThe Management of Asherman Syndrome: A Review of LiteratureEuphra Adellheid100% (1)
- Malaria in Pregnancy 4Document35 pagesMalaria in Pregnancy 4api-3705046No ratings yet
- Endoscopy - Hysteroscopy and Laparoscopy Indications, Contraindications and ComplicationsDocument16 pagesEndoscopy - Hysteroscopy and Laparoscopy Indications, Contraindications and Complicationsselatur100% (1)
- Table 4.1 AFS Classifi Cation System (: The Embryological-Clinical Classifi CationDocument111 pagesTable 4.1 AFS Classifi Cation System (: The Embryological-Clinical Classifi CationArya Syafaromania RachmaNo ratings yet
- RISE REVIEW - Female Reproductive SystemDocument9 pagesRISE REVIEW - Female Reproductive SystemGerben Villanueva100% (1)
- Acog Practice Bulletin Summary: Pregestational Diabetes MellitusDocument3 pagesAcog Practice Bulletin Summary: Pregestational Diabetes MellitusMaría Fernanda Palma AcostaNo ratings yet
- Harare Obs N GynDocument96 pagesHarare Obs N GynRobert L G MabongaNo ratings yet
- 002 Intrapartum Fetal Heart Rate Monitoring 3a - ACOG Bulletin 106 PDFDocument11 pages002 Intrapartum Fetal Heart Rate Monitoring 3a - ACOG Bulletin 106 PDFale_fearNo ratings yet
- Medical History Taking Study GuideDocument6 pagesMedical History Taking Study GuideSarra Mood ImanNo ratings yet
- Obstetrics, Gynaecology-Textbook of Obstetrics and Gynaecology For Medical Students, 2nd Edition-Akin Agboola-2006Document559 pagesObstetrics, Gynaecology-Textbook of Obstetrics and Gynaecology For Medical Students, 2nd Edition-Akin Agboola-2006fagiy51113No ratings yet
- Module E Shock, MODS Roy Model-Oxygenation-Perfusion Required Readings (See Syllabus For Detailed Reading)Document7 pagesModule E Shock, MODS Roy Model-Oxygenation-Perfusion Required Readings (See Syllabus For Detailed Reading)Jeff ZhouNo ratings yet
- Uterine FibroidsDocument21 pagesUterine FibroidsPrasun BiswasNo ratings yet
- Pulmonary Disorders in PregnancyDocument49 pagesPulmonary Disorders in PregnancyMara Medina - BorleoNo ratings yet
- Management of CA Vulva 2Document33 pagesManagement of CA Vulva 2api-3705046No ratings yet
- Kelenjar LakrimalDocument44 pagesKelenjar LakrimalNurfanida Natasya MNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Pussy Pedia 2008Document47 pagesPussy Pedia 2008LCLibrary40% (153)
- Health-Asessment-Finals 2Document92 pagesHealth-Asessment-Finals 2Ebun Rosa100% (1)
- Hotpantz: Herbal GynecologyDocument28 pagesHotpantz: Herbal GynecologyMandy M.100% (20)
- Aesthetic Labia Minora and Clitoral Hood Reduction Using Extended Central Wedge ResectionDocument10 pagesAesthetic Labia Minora and Clitoral Hood Reduction Using Extended Central Wedge ResectionHazel Vivian Soliz AlconzNo ratings yet
- Shendi Obs OsceDocument35 pagesShendi Obs OsceYassin Jamal67% (3)
- The Vulva - Structure - Innervation - TeachMeAnatomyDocument3 pagesThe Vulva - Structure - Innervation - TeachMeAnatomywzt2001No ratings yet
- Procedure 28-18 Assessing The Female Genitals and Inguinal AreaDocument2 pagesProcedure 28-18 Assessing The Female Genitals and Inguinal Areakirsten galletaNo ratings yet
- Resolution-Rape (Final)Document7 pagesResolution-Rape (Final)HadjieLimNo ratings yet
- LaparosDocument3 pagesLaparosMurtaz BokhuaNo ratings yet
- Background and Precancerous Diseases of Female Genital Organs.Document43 pagesBackground and Precancerous Diseases of Female Genital Organs.Dae Shim100% (1)
- Chapter 2 Maternal Anatomy WilliamsDocument60 pagesChapter 2 Maternal Anatomy WilliamsDiskaAstariniNo ratings yet
- Bartholin's Gland Cyst MarsupializationDocument3 pagesBartholin's Gland Cyst MarsupializationAde Churie Tanjaya50% (2)
- 1a. Reproductive OrgansDocument60 pages1a. Reproductive OrgansJerrald Meyer L. BayaniNo ratings yet
- MARTINEZ PEREZ Labia Minora Elongation As Understood byDocument15 pagesMARTINEZ PEREZ Labia Minora Elongation As Understood byGuillermoMartinezPerezNo ratings yet
- A Brief Materia Medica of Some Lesser-Known NosodesDocument103 pagesA Brief Materia Medica of Some Lesser-Known NosodesnitkolNo ratings yet
- Instructional Module in Understanding The Self: School of Teacher EducationDocument5 pagesInstructional Module in Understanding The Self: School of Teacher EducationAlyanna MagkalasNo ratings yet
- Prolapse in CattleDocument2 pagesProlapse in Cattleirma safitriNo ratings yet
- Case Study 3D FinaaaalDocument34 pagesCase Study 3D FinaaaalPaul AnteNo ratings yet
- Perineum - The Anatomy of The PerineumDocument6 pagesPerineum - The Anatomy of The PerineumimvavNo ratings yet
- Suturing Perineal LacerationsDocument49 pagesSuturing Perineal LacerationsOfel Santillan100% (2)
- Anaphy Finals ReviewerDocument193 pagesAnaphy Finals Reviewerxuxi dulNo ratings yet
- Phantom ObgynDocument4 pagesPhantom ObgynHengki HaryandaNo ratings yet
- Pochette Imp. Vagino AngDocument26 pagesPochette Imp. Vagino AngMontrealthrowaway19No ratings yet
- Obstetrics LacerationsDocument15 pagesObstetrics LacerationsMauricio CorreaNo ratings yet
- Meat Curtains - Google SearchDocument1 pageMeat Curtains - Google SearchMr. BeddingfieldNo ratings yet
- Jurnal Kuda 1Document21 pagesJurnal Kuda 1Yulistia FadhilahNo ratings yet
- A Review On Yoni DhupanaDocument3 pagesA Review On Yoni DhupanaResearch Park0% (1)
- MCHN OutlineDocument15 pagesMCHN OutlineAngel Strauss KmpsnNo ratings yet
- Toygasms! - Sadie AllisonDocument161 pagesToygasms! - Sadie Allisonmtine40% (5)
- KKPMT IV Genito Uri N60 - N99Document170 pagesKKPMT IV Genito Uri N60 - N99Clarains FriskaNo ratings yet