Professional Documents
Culture Documents
ID Skin Test Injection Guide
Uploaded by
Juliezel IringanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ID Skin Test Injection Guide
Uploaded by
Juliezel IringanCopyright:
Available Formats
Intradermal Injection for Skin Test
PURPOSE
• To provide a medication that the client requires for allergy testing and TB screening
Administering an Intradermal Injection for Skin Tests
SKILL 35–5
ASSESSMENT
Assess
• Appearance of injection site
• Specific drug action and expected response
• Client’s knowledge of drug action and response
Check agency protocol about sites to use for skin tests.
PLANNING
DELEGATION
The administration of intradermal injections is an invasive technique that involves the application of
nursing knowledge, problem solving, and sterile technique. This technique is not delegated to UAP. The
nurse, however, can inform the UAP about symptoms of allergic reactions and the necessity of reporting
those observations immediately to the nurse.
Equipment
• Client’s MAR or computer printout
• Vial or ampule of the correct medication
• Sterile 1-mL syringe calibrated into hundredths of a milliliter (i.e., tuberculin syringe) and a #25-
to #27-gauge safety needle that is 1/4 to 5/8 inch long
• Alcohol swabs
• 2×2 sterile gauze square (optional)
• Clean gloves (according to agency protocol)
• Bandage (optional)
• Epinephrine on hand in case of allergic anaphylactic reaction
IMPLEMENTATION
Preparation
1. Check the MAR.
• Check the label on the medication carefully against the MAR to make sure that the correct
medication is being prepared.
• Follow the three checks for administering medications. Read the label on the medication (1) when
it is taken from the medication cart, (2) before withdrawing the medication, and (3) after
withdrawing the medication.
2. Organize the equipment.
PERFORMANCE
1. Perform hand hygiene and observe other appropriate infection
prevention procedures.
2. Prepare the medication from the vial or ampule for drug
withdrawal.
• See Skills 35–2 and 35–3.
3. Prepare the client
• Prior to performing the procedure, introduce self and verify the client’s identity using agency
protocol. Rationale: This ensures that the right client receives the medication.
4. Explain to the client that the medication will produce a small wheal, sometimes called a bleb.
• A wheal is a small raised area, like a blister. The client will feel a slight prick as the needle enters
the skin. Some medications are absorbed slowly through the capillaries into the general
circulation, and the bleb gradually disappears. Other drugs remain in the area and interact with
the body tissues to produce redness and induration (hardening), which will need to be interpreted
at a particular time (e.g., in 24 or 48 hours). This reaction will also gradually disappear.
Rationale: Information can facilitate acceptance of and compliance with the therapy.
5. Provide for client privacy.
6. Select and clean the site.
• Select a site (e.g., the forearm about a hand’s width above the wrist and three or four finger
widths below the antecubital space).
• Avoid using sites that are tender, inflamed, or swollen and those that have lesions.
• Apply gloves as indicated by agency policy.
• Cleanse the skin at the site using a firm circular motion starting at the center and widening the
circle outward. Allow the area to dry thoroughly.
7. Prepare the syringe for the injection.
• Remove the needle cap while waiting for the antiseptic to dry.
• Expel any air bubbles from the syringe. Small bubbles that adhere to the plunger are of no
consequence. Rationale: A small amount of air will not harm the tissues.
• Grasp the syringe in your dominant hand, close to the hub, holding it between thumb and
forefinger. Hold the needle almost parallel to the skin surface, with the bevel of the needle up.
Rationale: The possibility of the medication entering the subcutaneous tissue increases when
using an angle greater than 15°.
8. Inject the fluid.
• With the nondominant hand, pull the skin at the site until it is taut. For example, if using the
ventral forearm, grasp the client’s dorsal forearm and gently pull it to tighten the ventral skin.
Rationale: Taut skin allows for easier entry of the needle and less discomfort for the client.
• Insert the tip of the needle far enough to place the bevel through the epidermis into the dermis.
The outline of the bevel should be visible under the skin surface.
• Stabilize the syringe and needle. Inject the medication carefully and slowly so that it produces a
small wheal on the skin.
Rationale: This verifies that the medication entered the dermis.
• Withdraw the needle quickly at the same angle at which it was inserted. Activate the needle
safety device. Apply a bandage if indicated.
• Do not massage the area.
Rationale: Massage can disperse the medication into the tissue or out through the needle
insertion site.
• Dispose of the syringe and needle into the sharp container.
Rationale: Do not recap the needle in order to prevent needlestick injuries.
• Remove and discard gloves.
• Perform hand hygiene.
• Circle the injection site with ink to observe for redness or induration (hardening), per agency
policy.
9. Document all relevant information.
• Record the testing material given, the time, dosage, route, site, and nursing assessments
Administering an Intradermal Injection for Skin Tests—continued
SKILL 35–5
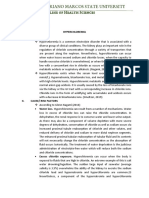
❶B
Epidermis
Dermis
Subcutaneous
tissue
❶ For an intradermal injection: A, the needle enters the skin at a 5°
to 15° angle; B, C, the medication forms a bleb or wheal under the
epidermis. ❶ C
❶A
EVALUATION
• Evaluate the client’s response to the testing substance.
Rationale: Some medications used in testing may cause allergic
reactions. Epinephrine may need to be used.
• Evaluate the condition of the site in 24 or 48 hours, depending
on the test. Measure the area of redness and induration in
millimeters
at the largest diameter and document findings.
You might also like
- Bukidnon State University College of Nursing Patient Monitoring SheetDocument6 pagesBukidnon State University College of Nursing Patient Monitoring SheetLucille Allen100% (7)
- Prevention & Management of Sports Injuries: Quimcy Dsouza Fybms-Sm (B) 75Document26 pagesPrevention & Management of Sports Injuries: Quimcy Dsouza Fybms-Sm (B) 75Quimcy100% (1)
- MCQ 1. Heart Sound Heart Sound S1 S2Document7 pagesMCQ 1. Heart Sound Heart Sound S1 S2Atirah AaNo ratings yet
- Surgical Skin PreparationDocument2 pagesSurgical Skin PreparationVanny Vien JuanilloNo ratings yet
- 4 Oet Reading Summary 2.0Document19 pages4 Oet Reading Summary 2.0Vijayalakshmi Narayanaswami0% (3)
- LESSON PLAN ON Hyper Emesis GravidarumDocument12 pagesLESSON PLAN ON Hyper Emesis GravidarumMadhavi ModaNo ratings yet
- Chapter61 Management of Patients With Neurologic DysfunctionDocument49 pagesChapter61 Management of Patients With Neurologic DysfunctionAhmed 123No ratings yet
- Taco Vs TraliDocument42 pagesTaco Vs TraliOdiet RevenderNo ratings yet
- General Instructions:: Child, (2) Treat The Child, (3) Follow-Up and (4) Counsel The Mother. Fill in The RecordingDocument2 pagesGeneral Instructions:: Child, (2) Treat The Child, (3) Follow-Up and (4) Counsel The Mother. Fill in The RecordingToni Angelie CaprechoNo ratings yet
- Purposive Communication: Lesso N 1: Communic Atio N M O D ElsDocument30 pagesPurposive Communication: Lesso N 1: Communic Atio N M O D ElsRamil Billones100% (1)
- TEPID SPONGE BATHDocument3 pagesTEPID SPONGE BATHJeonoh FloridaNo ratings yet
- NCM 200 - Preparing Administering MedicationDocument21 pagesNCM 200 - Preparing Administering MedicationjhonmarcNo ratings yet
- Drug Study AZITHROMYCINDocument2 pagesDrug Study AZITHROMYCINDannah BulliandayNo ratings yet
- Introduction to Pharmacology: Effects of Drugs & Medication AdministrationDocument2 pagesIntroduction to Pharmacology: Effects of Drugs & Medication AdministrationAdri Sinclaire100% (1)
- A Preschool-Based Intervention For Early ChildhoodDocument9 pagesA Preschool-Based Intervention For Early Childhoodmohammed MusaNo ratings yet
- NCM 104 RLE Module 3 FinalsDocument22 pagesNCM 104 RLE Module 3 FinalsAlexander DontonNo ratings yet
- Principles of Bag TechniqueDocument3 pagesPrinciples of Bag TechniqueClare AlcoberNo ratings yet
- Pneumonia Definations & ClassificationsDocument29 pagesPneumonia Definations & ClassificationsJimitNo ratings yet
- K44 - Nutrition During LactationDocument26 pagesK44 - Nutrition During Lactationbilli lisanuddinNo ratings yet
- Management of Patients With Gastric and Duodenal DisordersDocument7 pagesManagement of Patients With Gastric and Duodenal DisordersintotheunknownNo ratings yet
- Chickenpox What Is Chickenpox?Document19 pagesChickenpox What Is Chickenpox?s.khan9211rediffmail.comNo ratings yet
- PUCAN, Julienne BSN III-D - SGD - HYPO&HYPERCHLOREMIADocument10 pagesPUCAN, Julienne BSN III-D - SGD - HYPO&HYPERCHLOREMIAJulienne PucanNo ratings yet
- Barangay Health Services Environmental SanitationDocument5 pagesBarangay Health Services Environmental SanitationNessa Layos MorilloNo ratings yet
- CHN Lec Activity 2Document3 pagesCHN Lec Activity 2RickNo ratings yet
- Advanced Wound Care and Dressing Resource UnitDocument6 pagesAdvanced Wound Care and Dressing Resource UnitGreg Martin OrbegosoNo ratings yet
- Tranexamic AcidDocument18 pagesTranexamic AcidFatima Love Ariate-ArcasetasNo ratings yet
- AnthraxDocument29 pagesAnthraxstevensb055No ratings yet
- Chloride Imbalance Causes and TreatmentsDocument2 pagesChloride Imbalance Causes and Treatmentsed123edNo ratings yet
- Skeletal Muscle Physiology PDFDocument6 pagesSkeletal Muscle Physiology PDFAstri Ggamjong Xiao LuNo ratings yet
- CHN Immunization NotesDocument9 pagesCHN Immunization NotesJustin AncogNo ratings yet
- Important Estimates in Pregnancy & Danger Signs in Pregnancy PDFDocument3 pagesImportant Estimates in Pregnancy & Danger Signs in Pregnancy PDFTandingco, Olivia Mari H.No ratings yet
- Bacillary DysenteryDocument32 pagesBacillary Dysenteryapi-199163990% (1)
- Maternal and Child Health CareDocument7 pagesMaternal and Child Health CareNessa Layos MorilloNo ratings yet
- Legaspi - Preparing Medication From A Vial ChecklistDocument4 pagesLegaspi - Preparing Medication From A Vial ChecklistJason LumayaNo ratings yet
- Alteration in Fluid and Electrolyte Status Lecture NotesDocument11 pagesAlteration in Fluid and Electrolyte Status Lecture Notes0912247251No ratings yet
- Burns Rule of Nines 2013Document1 pageBurns Rule of Nines 2013ellenningrumNo ratings yet
- Nutrition Essentials for Growing PreschoolersDocument6 pagesNutrition Essentials for Growing PreschoolersKeerthana VNo ratings yet
- Final Examination Reviewer (Nha 100) Post Test C11Document13 pagesFinal Examination Reviewer (Nha 100) Post Test C11Prince Mark BadilloNo ratings yet
- Leopolds Maneuver - Return DemoDocument1 pageLeopolds Maneuver - Return DemornrmmanphdNo ratings yet
- MODULE-9-Biotechnology, Genetically Modified Organisms, and Gene TherapyDocument5 pagesMODULE-9-Biotechnology, Genetically Modified Organisms, and Gene TherapyKerry NuñezNo ratings yet
- Midwifery Evolution, Concepts and TheoriesDocument92 pagesMidwifery Evolution, Concepts and TheoriesRoxanne Jane S. Graycochea100% (1)
- Community Health Nursing ReviewerDocument10 pagesCommunity Health Nursing ReviewerNicole CastillaNo ratings yet
- Administering Opthalmic MedicationsDocument5 pagesAdministering Opthalmic MedicationsAnika PleñosNo ratings yet
- Drugs and NCPDocument4 pagesDrugs and NCPApril Anne CostalesNo ratings yet
- Piperacillin Tazobactam (Zosynpiperacillin)Document1 pagePiperacillin Tazobactam (Zosynpiperacillin)ENo ratings yet
- Individual Aging Vs Population AgingDocument74 pagesIndividual Aging Vs Population AgingAnthony RiggsNo ratings yet
- 8 Drug StudyDocument9 pages8 Drug StudyJohn Michael M. RosalesNo ratings yet
- Availability: Classifications: Antihistamine Antipruritic Pregnancy Category: CDocument4 pagesAvailability: Classifications: Antihistamine Antipruritic Pregnancy Category: CCay SevillaNo ratings yet
- Assessing The SkinDocument22 pagesAssessing The Skinjasnate84No ratings yet
- Conjunctivitis Nursing ManagementDocument3 pagesConjunctivitis Nursing Managementflex gyNo ratings yet
- Involving Family, Domestic Relations, Women and Children. (2015) - Philippine JudicialDocument10 pagesInvolving Family, Domestic Relations, Women and Children. (2015) - Philippine JudicialAngel MayNo ratings yet
- Tetanus toxoid immunization schedule for womeneditDocument4 pagesTetanus toxoid immunization schedule for womeneditEdwin Delos Reyes AbuNo ratings yet
- Types of PneumoniaDocument6 pagesTypes of PneumoniasakuraleeshaoranNo ratings yet
- Bag Technique Lecture Notes PDFDocument4 pagesBag Technique Lecture Notes PDFtanmai nooluNo ratings yet
- College of Nursing: Rifadin RifampinDocument4 pagesCollege of Nursing: Rifadin RifampinAnika PleñosNo ratings yet
- Delivery Room Technique GuideDocument10 pagesDelivery Room Technique GuideAl-waleed JulkanainNo ratings yet
- MineDocument3 pagesMineJM NelsonNo ratings yet
- Gregorio, Forgive Us All: Community Health Nursing 1 Activity #1Document2 pagesGregorio, Forgive Us All: Community Health Nursing 1 Activity #1Cacamo Rexell-anNo ratings yet
- Checklist Preparing Medications From Vials and AmpulesDocument4 pagesChecklist Preparing Medications From Vials and AmpulesDenvic0% (1)
- Assessment of A Pregnant FamilyDocument4 pagesAssessment of A Pregnant FamilyLuna Sang-anNo ratings yet
- Optimizing Perioperative CareDocument8 pagesOptimizing Perioperative CareJan Crizza Dale R. FrancoNo ratings yet
- Clinical Guidelines (Nursing) - Indwelling Urinary Catheter - Insertion and Ongoing CareDocument8 pagesClinical Guidelines (Nursing) - Indwelling Urinary Catheter - Insertion and Ongoing CareLeeNo ratings yet
- Enteral and Parenteral Feeding: Mylin G. Abalus NUTN 204 LecturerDocument24 pagesEnteral and Parenteral Feeding: Mylin G. Abalus NUTN 204 Lecturerminhmap90_635122804No ratings yet
- Administering An Intradermal InjectionDocument2 pagesAdministering An Intradermal InjectionNikka AurelleNo ratings yet
- Adminstration of Intradermal InjectionDocument2 pagesAdminstration of Intradermal InjectionMicroporeNo ratings yet
- Parenteral Catheterization Enema ChecklistDocument8 pagesParenteral Catheterization Enema ChecklistJessoliver GalvezNo ratings yet
- Olfu Vision MissionDocument1 pageOlfu Vision MissionJuliezel IringanNo ratings yet
- NCMA217RLE - Performance Task 1Document2 pagesNCMA217RLE - Performance Task 1Juliezel IringanNo ratings yet
- LIFE CYCLE AND GOAL SETTING Activity OutputDocument4 pagesLIFE CYCLE AND GOAL SETTING Activity OutputJuliezel IringanNo ratings yet
- Case Scenario 1Document3 pagesCase Scenario 1Juliezel IringanNo ratings yet
- Iringan (1st Activity PHED 112)Document2 pagesIringan (1st Activity PHED 112)Juliezel IringanNo ratings yet
- Understanding Ethics and MoralityDocument2 pagesUnderstanding Ethics and MoralityJuliezel IringanNo ratings yet
- Preparing MedicationsDocument18 pagesPreparing MedicationsJuliezel IringanNo ratings yet
- Therapeutic communication in nursingDocument1 pageTherapeutic communication in nursingJuliezel IringanNo ratings yet
- Critical ThinkingDocument3 pagesCritical ThinkingJuliezel IringanNo ratings yet
- Cmca Lec Prelim ReviewerDocument26 pagesCmca Lec Prelim ReviewerCrystal MiranaNo ratings yet
- X-Ray Findings and Key Signs in RadiologyDocument3 pagesX-Ray Findings and Key Signs in RadiologylilyNo ratings yet
- 8.A Case Report of Rabies With Long Incubation ImporDocument3 pages8.A Case Report of Rabies With Long Incubation ImporAndra CristianaNo ratings yet
- Graviola1 Triamazon, AntiCancer, InglesDocument2 pagesGraviola1 Triamazon, AntiCancer, InglesManuel SierraNo ratings yet
- Homeopathy Aggravation Guide: Understanding Reactions to RemediesDocument2 pagesHomeopathy Aggravation Guide: Understanding Reactions to RemediesMd Mohebbullah ChowdhuryNo ratings yet
- Tristianti Nur Khasanah 180205136 18a3Document3 pagesTristianti Nur Khasanah 180205136 18a3Tristianti NurkhaNo ratings yet
- Dexmet Vs LignocaineDocument22 pagesDexmet Vs LignocaineDr.S.Easwaramoorthy IAGES Secretary 2020No ratings yet
- CamScanner 09-04-2023 13.33Document4 pagesCamScanner 09-04-2023 13.33BILAL AYALANo ratings yet
- Vertigo: Causes, Symptoms and TreatmentDocument3 pagesVertigo: Causes, Symptoms and TreatmentJemsner IrothNo ratings yet
- Traumatic Brain Injury (TBI)Document17 pagesTraumatic Brain Injury (TBI)Ashish DootNo ratings yet
- 14 03-21 Cord CareDocument16 pages14 03-21 Cord Careapi-250478881No ratings yet
- CNH Construction Health DeclarationDocument1 pageCNH Construction Health DeclarationEna Ahmad PieNo ratings yet
- Tugas Ipg UlfaDocument8 pagesTugas Ipg UlfaUlfa Mukhlisa Putri UlfaNo ratings yet
- CP Assessment Format (DDRC)Document5 pagesCP Assessment Format (DDRC)maitriNo ratings yet
- Atrophic Glossitis Causes, Symptoms, Signs, TreatmentDocument16 pagesAtrophic Glossitis Causes, Symptoms, Signs, TreatmentPutrisya Rafanael SafageNo ratings yet
- Proped PDF Dox PDFDocument76 pagesProped PDF Dox PDFMuzamil RiasatNo ratings yet
- GSIS vs. de Castro 185035Document2 pagesGSIS vs. de Castro 185035Juan DoeNo ratings yet
- Ayurvedic Insights of Avascular Necrosis of Femoral HeadDocument4 pagesAyurvedic Insights of Avascular Necrosis of Femoral HeadIJAR JOURNALNo ratings yet
- Assessment Nursing Diagnosis Goals/ Expected Outcome S Nursing Intervention S Scientific Rationale Nursing Theory Core Values EvaluationDocument2 pagesAssessment Nursing Diagnosis Goals/ Expected Outcome S Nursing Intervention S Scientific Rationale Nursing Theory Core Values Evaluation8lueCzarcasmNo ratings yet
- Patient - Carpal Tunnel ReleaseDocument2 pagesPatient - Carpal Tunnel Releaseapi-277825138No ratings yet
- AntacidsDocument2 pagesAntacidsMegan SamsonNo ratings yet
- STIsDocument31 pagesSTIsAbdulmumin UsmanNo ratings yet
- Med. Potvrda - PZO ANIMA - Dr. Duduchki - Stevanovski Vlatko 2021Document1 pageMed. Potvrda - PZO ANIMA - Dr. Duduchki - Stevanovski Vlatko 2021omitevskiNo ratings yet
- Surveillance of Healthcare-Associated Infections in Indonesian HospitalsDocument12 pagesSurveillance of Healthcare-Associated Infections in Indonesian HospitalsRidha MardiyaniNo ratings yet