Professional Documents
Culture Documents
BSN 1 H Case Application Nursing Care Plan
Uploaded by
Antonio EscotoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BSN 1 H Case Application Nursing Care Plan
Uploaded by
Antonio EscotoCopyright:
Available Formats
University of San Agustin
General Luna St., 5000 Iloilo City, Philippines
www.usa.edu.ph
COLLEGE OF HEALTH AND ALLIED MEDICAL PROFESSIONS - DEPARTMENT OF NURSING
NAME: CARLOS MIGUEL S. DE LA GENTE YEAR/SECTION:BSN 1-H
Case Application - Nursing Care Plan
Construct a Nursing Care Plan for Mr. Roman & Ms. Perez:
1. Mr. Roman, 25 years of age, presents to the triage nurse at the local emergency department,
complaining of severe generalized abdominal pain. She describes it as sharp and
intermittent. He states, “Over the last 4 days, I haven’t been able to have a bowel movement.”
He states that he is able to drink liquids and urinating without difficulty. Bowel sounds are
present in all 4 quadrants, however, they are hypoactive (decreased or quiet peristalsis).
Abdomen is distended and firm to touch. He states, “Two weeks ago I feel that my back hurts.
My doctor gave me a prescription of Tylenol #3 & I have been taking it every 6 hours for
pain.” He denies pain at the present time. Abdominal x-ray reveals a large amount of stool in his
lower colon. All other diagnostic tests are unremarkable. He was prescribed with Dulcolax 1
tablet once a day.
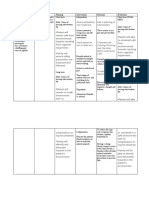
Diagnosis Goal Intervention Rationale Evaluation
Acute Abdominal Within 8 Independent: Independent: Short term:
Pain R/T pressure hours of Examine To The goal was
from distended receiving the daily promote achieved. After 4
abdomen as nursing care, routine of a patient hours of nursing
evidenced by: the patient patient. cooperatio interventions, the
will be able to n. patient reported
Subjective: express relief Obtain the Helpful in that the pain was
He states, from patient’s assessing relieved/controlle
“Two gastrointestin vital signs. the need d, that he
weeks al distress and for followed the
ago I feel maintain a Provide a interventio prescribed
that my stable stool quiet n pharmaceutical
back passage at environmen To help regimen to relieve
hurts. regular t and assess pain, that he
intervals. reduce what could verbalized non-
He also stimuli have been pharmacologic
states, (e.g., noise, the factor ways that give
"Over the lightning, affecting relief, and that he
last 4 constant the patient was able to relax
days, I interruption in his daily and sleep/rest
haven’t s) routine. correctly.
been able
to have a List all the Dependent:
bowel patient’s
movemen current Used to
t. prescription help
s. relieve
Email: cn@usa.edu.ph | Tel. No.: 0999-997-1485 | Fax No.: (033) 337-4403
University of San Agustin
General Luna St., 5000 Iloilo City, Philippines
www.usa.edu.ph
COLLEGE OF HEALTH AND ALLIED MEDICAL PROFESSIONS - DEPARTMENT OF NURSING
mild to
moderate
Objective: Dependent: pain.
Abdomen is 1. Dulcolax 1 It works
distended and tab, once a directly on
firm to touch. day the colon
2. laxative to produce
such as a bowel
Dulcolax 1- movement
tab qd .
Interdependent:
Suction to
relieve
buildup of
gas and
liquid
Surgery
2. Mrs. Perez, 48 years old, is admitted to the nursing unit 2 hours after undergoing a right
surgical removal of her breast (mastectomy). The floor nurse receives a report from the
post anesthesia care unit (PACU) nurse that includes the patient’s admitting diagnosis of
breast cancer, latest vital signs, focused assessment, medication & intravenous (IV)
orders, pain level & the time she was last medicated for pain & status of the surgical
dressing. Initially, Mrs. Perez appears to be comfortable, dozing occasionally between
short conversations with her husband, who is at her side. When she was fully awake 3
hours after, she complains of sharp, constant pain on the right side of her chest. She
rates her pain at 8 / 10 on the pain scale. She is grimacing and appears tense. The RN
took her vital signs - T = 36.5 "C; BP = 130/100 mmHg; RR = 20 bpm; PR = 80
beats/min. She inspected the surgical wound, at the right breast and reveals that the
dressing is slightly soaked with blood and intact, no pus & slightly swelling noted.
Diagnosis Goal Intervention Rationale Evaluation
Mastectomy R/T After 1 Independent: Independent: Short Term:
impaired skin hour of Establish This could Goal met. After
integrity related nurse- Rapport serve as 1hour of nurse
to surgery to patient baseline data patient
breast removal interaction Avoid sudden Sudden interactionwithi
as evidenced by: over an 8- movement movement n an 8 hour shift,
hour shift, can cause the patient was
Subjective: the patient Access mode damage to able to verbalize
She complains of will be able coping the healing and demonstrate
sharp constant to know, abilities and tissues on the theright
pain on the right pronounce, personality surgical measures
side of her chest. and show styles wound intaking of her
Email: cn@usa.edu.ph | Tel. No.: 0999-997-1485 | Fax No.: (033) 337-4403
University of San Agustin
General Luna St., 5000 Iloilo City, Philippines
www.usa.edu.ph
COLLEGE OF HEALTH AND ALLIED MEDICAL PROFESSIONS - DEPARTMENT OF NURSING
the proper To enhance post- surgical
Objective: precaution Consider the self- esteem skin.
She rates s and post- importance of and sense of
her pain surgical post-surgery self- worth.
at 8 / 10 skin care to rehabilitation The client
on the prevent . stands to
pain infection. accommodat
scale e the change
Dependent: in the center
She is Tylenol 1 tab PRN of gravity by
grimacin Advil 1 cap TID leaning to the
g and side.
appears
tense.
Email: cn@usa.edu.ph | Tel. No.: 0999-997-1485 | Fax No.: (033) 337-4403
You might also like
- U.S. Army Patent For Weaponized MycoplasmaDocument81 pagesU.S. Army Patent For Weaponized MycoplasmaAdam F.100% (1)
- Self Love Inner Child Healing With EFTDocument11 pagesSelf Love Inner Child Healing With EFTAnonymous fUL4SPRsAf100% (1)
- Assignment On Element3 Safety CultureDocument3 pagesAssignment On Element3 Safety CultureSAFETY VOFPL100% (2)
- Assessment, diagnosis, planning, intervention, and evaluation for Parkinson's patientDocument2 pagesAssessment, diagnosis, planning, intervention, and evaluation for Parkinson's patientBenjie DimayacyacNo ratings yet
- Solution Manual For Health Psychology 11th Edition Shelley Taylor Annette L StantonDocument7 pagesSolution Manual For Health Psychology 11th Edition Shelley Taylor Annette L StantonJamesThomasngec100% (45)
- NCPDocument6 pagesNCPBelle OyosNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainBasema HashhashNo ratings yet
- Valdez Reflective-Questions PDFDocument3 pagesValdez Reflective-Questions PDFDexel Lorren ValdezNo ratings yet
- Managing Premature Cervical DilatationDocument10 pagesManaging Premature Cervical DilatationRaiden VizcondeNo ratings yet
- Nursing Care Plan: Nikolai P. Funcion, FSUU-SNDocument5 pagesNursing Care Plan: Nikolai P. Funcion, FSUU-SNNikolai FuncionNo ratings yet
- Nursing Care PlanDocument1 pageNursing Care Planapi-248135371No ratings yet
- Broschyr GEM5000Document12 pagesBroschyr GEM5000Oo Kenx OoNo ratings yet
- Managing Fatigue Through Activity Pacing and RestDocument2 pagesManaging Fatigue Through Activity Pacing and ResthaniehaehaeNo ratings yet
- NCP Bed SoresDocument3 pagesNCP Bed SoresShe CalliNo ratings yet
- Subjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationDocument2 pagesSubjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationAyra PunzalanNo ratings yet
- Nursing Care Plan Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationDocument2 pagesNursing Care Plan Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationValerie FischerNo ratings yet
- Clinical Learning ContractDocument3 pagesClinical Learning ContractKaragire vedasteNo ratings yet
- NCPDocument2 pagesNCPMelissa David100% (1)
- Appendicitis - NCPDocument5 pagesAppendicitis - NCPEarl Joseph Deza100% (1)
- Sbar Template Staff To StaffDocument2 pagesSbar Template Staff To Staffrafikakurniati6100% (2)
- NCP Total Hip ReplacementDocument11 pagesNCP Total Hip ReplacementDoneva Lyn MedinaNo ratings yet
- NALAM 106 Ass. AntibioticsDocument6 pagesNALAM 106 Ass. AntibioticsBeth100% (1)
- Nursing Care PlanDocument5 pagesNursing Care PlankingpinNo ratings yet
- NCP PainDocument4 pagesNCP PainMark Allison BuenaventuraNo ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- Evidence-Based Nursing: I. Clinical QuestionDocument4 pagesEvidence-Based Nursing: I. Clinical QuestionRay Jorge MarmetoNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument14 pagesAssessment Diagnosis Planning Implementation Rationale EvaluationJennifer ArdeNo ratings yet
- How to treat and prevent breast engorgementDocument1 pageHow to treat and prevent breast engorgementkurniaNo ratings yet
- Healthcare - Nursing Care Plan - Excess Fluid VolumeDocument4 pagesHealthcare - Nursing Care Plan - Excess Fluid VolumeBenjamin CañalitaNo ratings yet
- Improve Patient Satisfaction ScoresDocument5 pagesImprove Patient Satisfaction ScoresAce TabioloNo ratings yet
- Learning Feedback g2Document8 pagesLearning Feedback g2Darwin DaveNo ratings yet
- Nursing Care Plan Impaired Gas ExchangeDocument1 pageNursing Care Plan Impaired Gas ExchangeKarylle PetilNo ratings yet
- Risk For Falls As Evidence by Loss of BalanceDocument4 pagesRisk For Falls As Evidence by Loss of BalanceAlexandrea MayNo ratings yet
- NCP MRMDocument2 pagesNCP MRMKhloe Cristel Llanes Torres100% (1)
- NCP Fever: Read Books, Audiobooks, and More Scribd, IncDocument10 pagesNCP Fever: Read Books, Audiobooks, and More Scribd, IncEricsonMitraNo ratings yet
- St. Paul University Nursing Care PlansDocument6 pagesSt. Paul University Nursing Care PlansRoxanne MariÑas Delvo0% (1)
- Nursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermDocument4 pagesNursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermErika Danalle ArceoNo ratings yet
- Related ReadingsDocument2 pagesRelated ReadingsIra BearNo ratings yet
- NCP Cavernous Sinus ThrombosisDocument3 pagesNCP Cavernous Sinus ThrombosisVencel Mae Famas Villahermosa50% (2)
- NCPDocument2 pagesNCPCamille VirayNo ratings yet
- NCPDocument10 pagesNCPCristina L. JaysonNo ratings yet
- NCPDocument2 pagesNCPAnne De VeraNo ratings yet
- NCPDocument10 pagesNCPNefre Dayap DarrocaNo ratings yet
- CHAPTER 4-Atty AliboghaDocument48 pagesCHAPTER 4-Atty AliboghaPaul EspinosaNo ratings yet
- NCP Knowledge Deficit PDFDocument2 pagesNCP Knowledge Deficit PDFskylertNo ratings yet
- BSN 215 Reflection Essay - LagoDocument2 pagesBSN 215 Reflection Essay - LagoAlliahkherzteen LagoNo ratings yet
- NCP Proper CholecystectomyDocument2 pagesNCP Proper CholecystectomyGail Lian SantosNo ratings yet
- NCPDocument4 pagesNCPHannah LopezNo ratings yet
- Nursing Care Plan: Imbalanced Nutrition: Less Than Body Requirements Disturbed Body Image Ineffective DenialDocument6 pagesNursing Care Plan: Imbalanced Nutrition: Less Than Body Requirements Disturbed Body Image Ineffective DenialBrix ValdrizNo ratings yet
- Nursing Diagnostic Reasoning for Otitis ExternaDocument5 pagesNursing Diagnostic Reasoning for Otitis ExternaGino Al Ballano BorinagaNo ratings yet
- College of Nursing and Allied Medical Sciences: WesleyanDocument3 pagesCollege of Nursing and Allied Medical Sciences: WesleyanPrince Juzzel Banag100% (1)
- Nursing Care PlanDocument1 pageNursing Care PlanDaisy PacoNo ratings yet
- Final Teaching PlanDocument2 pagesFinal Teaching Planapi-352581650No ratings yet
- Nursing Care Plans For Activity IntoleranceDocument4 pagesNursing Care Plans For Activity IntolerancethebigtwirpNo ratings yet
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocument2 pagesTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestNo ratings yet
- Nursing Care Plans: Desired Outcome Interventions Impaired Physical MobilityDocument6 pagesNursing Care Plans: Desired Outcome Interventions Impaired Physical MobilityNaomi MasudaNo ratings yet
- NCP CSDocument4 pagesNCP CSJM UncianoNo ratings yet
- Case StudyDocument9 pagesCase Studyapi-267715207No ratings yet
- Nursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy MalaiseDocument1 pageNursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy Malaise06eltianNo ratings yet
- Nursing Care PlansDocument2 pagesNursing Care PlansatchiekNo ratings yet
- Nursing Assessment - Pediatric Clients in The Community New 1 1Document7 pagesNursing Assessment - Pediatric Clients in The Community New 1 1Ugalde AlyssakyleNo ratings yet
- Case Study, Chapter 70, Management of Patients WithOncologic or Degenerative Neurologic DisordersDocument1 pageCase Study, Chapter 70, Management of Patients WithOncologic or Degenerative Neurologic Disordersclyde i am100% (1)
- Cues Objectives Interventions Rationale Evaluation: Nursing Care PlanDocument1 pageCues Objectives Interventions Rationale Evaluation: Nursing Care Planaprilrosehibaya100% (1)
- Case StudyDocument8 pagesCase Studyjds6z4sgfwNo ratings yet
- Nursing Care Plan for Isabella C. DomingoDocument2 pagesNursing Care Plan for Isabella C. DomingojussNo ratings yet
- BSN 1 J Case Application Interactive TheoriesDocument8 pagesBSN 1 J Case Application Interactive TheoriesAntonio EscotoNo ratings yet
- Case 3 Tuberculosis Group 3Document72 pagesCase 3 Tuberculosis Group 3Antonio EscotoNo ratings yet
- Almart C. Interview PandemicDocument1 pageAlmart C. Interview PandemicAntonio EscotoNo ratings yet
- Betty Neuman Case ApplicationDocument2 pagesBetty Neuman Case ApplicationAntonio EscotoNo ratings yet
- 016 - Attachment For Full Scale Shear Pads - 01 Mar 11Document54 pages016 - Attachment For Full Scale Shear Pads - 01 Mar 11nadraNo ratings yet
- Boys WH Swim Results 9.14Document4 pagesBoys WH Swim Results 9.14The LedgerNo ratings yet
- PED011 Final Req 15Document3 pagesPED011 Final Req 15macabalang.yd501No ratings yet
- Myotonic Dystrophy PresentationDocument8 pagesMyotonic Dystrophy Presentationapi-318918663No ratings yet
- Amrik PED SURGDocument24 pagesAmrik PED SURGAditya DharmajiNo ratings yet
- Ayushman BharatDocument18 pagesAyushman BharatNeethu VincentNo ratings yet
- Assignment: TopicDocument12 pagesAssignment: TopicAthul RNo ratings yet
- Parental Involvement Scale - Guide To QuestionnaireDocument2 pagesParental Involvement Scale - Guide To QuestionnaireAldrin ZolinaNo ratings yet
- Chapter 06 Try inDocument18 pagesChapter 06 Try inمحمد حسنNo ratings yet
- Abortion Research PaperDocument6 pagesAbortion Research Paperapi-511989965No ratings yet
- Lgu CaDocument70 pagesLgu CaMENRO GENERAL NATIVIDADNo ratings yet
- Final CHN g1Document52 pagesFinal CHN g1Cariology YuNo ratings yet
- Kebutuhan Cairan NeonatusDocument3 pagesKebutuhan Cairan NeonatusGendis SudjaNo ratings yet
- TriumphDebate SeptOct2021 OfficialBriefDocument134 pagesTriumphDebate SeptOct2021 OfficialBriefRebecca WardNo ratings yet
- Po 2021 FebruariDocument28 pagesPo 2021 FebruariNila Permata SariNo ratings yet
- Ideals, The Self & FlexibilityDocument1 pageIdeals, The Self & FlexibilityCamille ArandilNo ratings yet
- Republic of The Philippines Province of Rizal Municipality of Rodriguez Barangay Geronimo Office of Sangguniang KabataanDocument3 pagesRepublic of The Philippines Province of Rizal Municipality of Rodriguez Barangay Geronimo Office of Sangguniang KabataanMark MagsilaNo ratings yet
- Development Stages in Middle and Late AdolescenceDocument19 pagesDevelopment Stages in Middle and Late AdolescenceJohn Anniel BundalianNo ratings yet
- DR Preeti UdaipurDocument19 pagesDR Preeti Udaipurpreeti senthiyaNo ratings yet
- Life Saving Rules Poster in EnglishDocument11 pagesLife Saving Rules Poster in Englishkumalk3815No ratings yet
- Weight World: 1) Organic TurmericDocument6 pagesWeight World: 1) Organic TurmericGANESWAR BARIKNo ratings yet
- Stay With Peace of Mind: Arrival and Departure Team MembersDocument2 pagesStay With Peace of Mind: Arrival and Departure Team MembersSNo ratings yet
- Multimodal PDFDocument11 pagesMultimodal PDFCarlos CahuayaNo ratings yet
- 2018 - Johor (Kota Tinggi) - P2Document20 pages2018 - Johor (Kota Tinggi) - P2AIMANNo ratings yet
- Department of Social Welfare and DevelopmentDocument4 pagesDepartment of Social Welfare and DevelopmentJhana May PayatNo ratings yet