Professional Documents
Culture Documents
Psyche NX Activity
Psyche NX Activity
Uploaded by
Louraine Ville Albano Balino-Lita0 ratings0% found this document useful (0 votes)
1 views5 pagesOriginal Title
Psyche nx activity
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
1 views5 pagesPsyche NX Activity
Psyche NX Activity
Uploaded by
Louraine Ville Albano Balino-LitaCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
Republic of the Philippines
ISABELA STATE UNIVERSITY
City of Ilagan Campus
ACTIVITY #2- NUR 323 RLE
BASIC PRINCIPLES IN HISTORY TAKING
ORIENTATION / PURPOSE AND DURATION OF THE INTERVIEW…
DEMOGRAPHIC DATA
This is the first psychiatric hospital admission for Ms. X., a 21-year-old female
employed part-time as a Nurse Assistant. She currently lives with his boyfriend
and has never been married.
CHIEF COMPLAINTS
“I took an overdose of some pills but I'm fine now.”
HISTORY OF PRESENT ILLNESS
The patient is a 21-year-old female with a history of one prior suicide attempt
who was brought to the emergency room by ambulance, accompanied by his
boyfriend and roommate, after having taken an overdose of atenolol (Tenormin)
(twenty-five 25-mg tablets), zolpidem (Ambien) (twenty 10-mg tablets), and
possibly fluoxetine (Prozac) pills (number unknown) in a suicide attempt. All of
these medications had been prescribed for the patient's boyfriend. The evening
before, the patient had had a fight with his boyfriend. She believed that his
boyfriend wasn't giving him enough time and was not committed to the
relationship. They slapped and punched each other. The patient went to a bar
with another friend where he consumed four beers and a shot of vodka. When
She arrived back at home, his boyfriend told him to go to sleep, which she
interpreted as a continued lack of interest on the boyfriend's part. She locked
herself in the bathroom and took many of his boyfriend's pills. The patient filled
the empty pill bottles with water and left them in plain view on the sink. The
patient then unlocked the door and went to bed, telling his boyfriend where to
find syrup of ipecac. (Ms. X. carries the ipecac in his knapsack to induce vomiting
when he drinks too much alcohol.) Her boyfriend saw the pill bottles, realized the
patient had overdosed, and tried to induce vomiting by administering syrup of
ipecac. Unable to get the patient to vomit, she called an ambulance. Ms.. X
currently drinks alcohol once or twice each week, usually on the weekends. A
usual amount of alcohol for him consists of two vodka tonics and eight or nine
beers. Often, she drinks until she blacks out. She used marijuana this past New
Year's Eve (“a few lines”) and occasionally uses cough syrup (unknown amounts).
She denies any history of intravenous drug use. She remembers always speaking
and thinking very quickly, because she was always “so bright and talented and
good looking and smart.” In addition, she has needed little sleep since age 15. The
racing thoughts, pressured speech, and decreased need for sleep have become
more pronounced since September, when she started feeling “very up.” Since
then she has been getting at most 5 hours of sleep each night without feeling
tired. She says she can be very influential, but that he has no special powers. He
reports that he gets angry quickly and that her mood can change very easily. Since
September she also felt more depressed and physically restless. She considers
suicide frequently, “just to escape the boredom of life.” She has lost 6 pounds in
the last 2 months. There is no history of hallucinations or of delusional thought.
She locked himself in the bathroom and took many of her boyfriend's pills. The
patient filled the empty pill bottles with water and left them in plain view on the
sink. The patient then unlocked the door and went to bed, telling her boyfriend
where to find syrup of ipecac. (Ms. X. carries the ipecac in her knapsack to induce
vomiting when he drinks too much alcohol.) Her boyfriend saw the pill bottles,
realized the patient had overdosed, and tried to induce vomiting by administering
syrup of ipecac. Unable to get the patient to vomit, he called an ambulance. Ms. X
currently drinks alcohol once or twice each week, usually on the weekends. A
usual amount of alcohol for her consists of two vodka tonics and eight or nine
beers. Often, she drinks until he blacks out. She used cocaine this past New Year's
Eve (“a few lines”) and occasionally uses heroin (unknown amounts). She denies
any history of intravenous drug use. She remembers always speaking and thinking
very quickly, because she was always “so bright and talented and good looking
and smart.” In addition, she has needed little sleep since age 15. The racing
thoughts, pressured speech, and decreased need for sleep have become more
pronounced since September, when she started feeling “very up.” Since then, she
has been getting at most 5 hours of sleep each night without feeling tired. She
says he can be very influential, but that she has no special powers. She reports
that she gets angry quickly and that her mood can change very easily. Since
September she's also felt more depressed and physically restless. She considers
suicide frequently, “just to escape the boredom of life.” She has lost 6 pounds in
the last 2 months. There is no history of hallucinations or of delusional thought.
Past Psychiatric History
The patient has a history of violent outbursts. Her mother reports that as an
infant, she would bang his head against the floor. Throughout her childhood, she
got into fights with other children and would even attack family members and
teachers. In seventh grade, she threw a chair at a teacher. Once she attacked her
older brother and kicked him in the head repeatedly until he lost consciousness
and required medical attention. During her senior year in high school, the patient
was forced to see the school therapist because of a heated argument with a
teacher. The teacher claimed that the patient tried to hit him, and though the
patient denied this, she was expelled. She met with the psychologist five or six
times and stopped treatment when she graduated. There is a history of one
previous suicide attempt 2 years ago, precipitated by the infidelity of his first
boyfriend. The patient fashioned a noose and began to hang himself. When she
began to feel pain, he stopped. She never told anyone about this attempt and
never sought or received treatment. Psychotropic medication has never been
prescribed.
Family History
The patient's immediate family consists of her father (age 51), her mother (age
49), one older brother (age 26), and one younger sister (age 19). Her father
suffers from alcohol dependence. Family history is otherwise negative for
psychiatric disorders, medical disease, dementia, addiction, suicide attempts, and
violence.
Medical History
The patient suffered from Influenza five times in the past 4 years. At age 15, she
fractured her right wrist in a fight. She denies any other medical conditions. She
takes no medications and has no known drug allergies. She has never been
hospitalized or undergone any surgical procedures.
Personal History
The patient grew up in a medium-size City of Alibagu. Her relationships with
family members have always been difficult. While she often got into physical
fights with her brother and her father, there is no history of physical, verbal, or
sexual abuse. In school, she had difficulty controlling his behavior, getting into
fights and cursing a great deal. She was a good student when she worked,
receiving As and Bs and honors in middle school and in the ninth grade. She failed
all of her classes in the sophomore year and needed to repeat the year. She
attributed this to ignoring school and partying too much. During her last year of
high school, she attended a special arts school, studying drama and jazz. She
graduated from high school after 5 years. She had trouble making friends. She had
a boyfriend for 2½ years in high school, but they broke up because they argued
too much. She met her first boyfriend at age 17, but this boy cheated on her,
precipitating the previous suicide attempt. In the past 2 or 3 years, the patient has
found herself primarily attracted to men but still considers herself bisexual. After
high school, she lived with his parents for almost 2 years. During that time, she
played drums in a band and held part-time jobs as a sales clerk. These jobs never
lasted more than a few months, usually ending in verbal fights with her employer.
She applied to music school but was not accepted because of his poor high school
performance.
Six months before admission, she moved to a large city to live with his uncle,
hoping to take classes without credit. Lack of financial resources required her to
work instead. She worked for 24 hours each week, off the books, as a
veterinarian's assistant. She felt that his uncle was too controlling and
domineering and moved in with another friend in October. In November, she met
his current boyfriend, Mr. B., at a bar. A week and a half later, she moved into the
boyfriend's house in the suburbs. Mr. B. reports that his relationship with the
patient has been characterized by extreme suspiciousness and neediness. The
patient has recurrent thoughts that her boyfriend doesn't care about her and is
cheating on her, even though there is no evidence. The patient has no savings and
is supported by his boyfriend.
Her parents have severe financial difficulties and are unable to help her. Contact
with family members is presently limited to her mother and her aunt because she
doesn't get along with any other family members. The patient has had about 25
different sexual partners, about half male and half female. She does not always
practice safe sex and has engaged in high-risk behaviors such as receptive sex
without using a condom. Because of this, she has been tested for human
immunodeficiency virus (HIV) infection four times. The result was negative each
time, most recently 2 months before admission. There is a significant history of
substance abuse. During her second and third years in high school, she smoked
marijuana two to three times each week. She stopped after graduation and has
since smoked marijuana only two or three times. She used cough syrup once in
high school occasionally in the past 2 years, snorting a few lines each time. She
has used lysergic acid diethylamide (LSD) and phencyclidine (PCP) but never
regularly. She has smoked cigarettes since age 13, ranging from half a pack to 2½
packs a day. She stopped smoking for 9 months 3 years ago but resumed and
currently smokes half a pack a day.
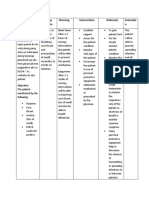
Direction:
1. Read the Psychiatric Health History of the patient.
2. Construct a hypothetical Psycho-pathology based on health history.
3. Formulate your hypothetical Nursing Care plan based on problems
identified during history taking.
4. Formulate a simulated therapy plan for the patient utilizing the proper
format.
NUR 323 RLE TEAM
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Dapagliflozin or Saxagliptin in Pediatric Type 2 DiabetesDocument13 pagesDapagliflozin or Saxagliptin in Pediatric Type 2 DiabetesEmmanuel HernandezNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Freebie Bundle-50 Pages.Document76 pagesFreebie Bundle-50 Pages.Kia MercadoNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Special Eurobarometer ReportDocument102 pagesSpecial Eurobarometer ReportKirály BélaNo ratings yet
- Covid-19 Cases: (January-September 2021)Document18 pagesCovid-19 Cases: (January-September 2021)Maria Pina Barbado PonceNo ratings yet
- On-The-Job-Training I Isu-Ilagan Auto Care Center City of Ilagan, IsabelaDocument36 pagesOn-The-Job-Training I Isu-Ilagan Auto Care Center City of Ilagan, IsabelaMaria Pina Barbado PonceNo ratings yet
- Eating Psychosexual Disorders Abuse ViolenceDocument106 pagesEating Psychosexual Disorders Abuse ViolenceMaria Pina Barbado PonceNo ratings yet
- Name: Ma Rupina B. Ponce Course: Bachelor of Science Major in Nursing Section: CDocument10 pagesName: Ma Rupina B. Ponce Course: Bachelor of Science Major in Nursing Section: CMaria Pina Barbado PonceNo ratings yet
- Polyomyelitis: Name: Ma Rupina B. Ponce Course: Bachelor of Science Major in Nursin Section: CDocument17 pagesPolyomyelitis: Name: Ma Rupina B. Ponce Course: Bachelor of Science Major in Nursin Section: CMaria Pina Barbado PonceNo ratings yet
- Name: Ma Rupina B. Ponce Course: Bachelor of Science Major in Nursing Section: C Hepatitis DefinitionDocument13 pagesName: Ma Rupina B. Ponce Course: Bachelor of Science Major in Nursing Section: C Hepatitis DefinitionMaria Pina Barbado PonceNo ratings yet
- Hook Worm InfectionsDocument10 pagesHook Worm InfectionsMaria Pina Barbado PonceNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale Evaluatio NDocument2 pagesAssessment Nursing Diagnosis Planning Intervention Rationale Evaluatio NMaria Pina Barbado PonceNo ratings yet
- Neurologic Reflexes Assessment in Magnesium Sulfate AdministrationDocument30 pagesNeurologic Reflexes Assessment in Magnesium Sulfate AdministrationMaria Pina Barbado PonceNo ratings yet
- Introduction To Antimicrobial/Anti-Infective DrugsDocument17 pagesIntroduction To Antimicrobial/Anti-Infective DrugsMaria Pina Barbado PonceNo ratings yet
- Food Poisoning DefinitionDocument10 pagesFood Poisoning DefinitionMaria Pina Barbado PonceNo ratings yet
- Nursing Care PlanDocument14 pagesNursing Care PlanMaria Pina Barbado PonceNo ratings yet
- Name: Ma Rupina B. Ponce Course: Bachelor of Science Major in Nursing Section: C Cholera DefinitionDocument17 pagesName: Ma Rupina B. Ponce Course: Bachelor of Science Major in Nursing Section: C Cholera DefinitionMaria Pina Barbado PonceNo ratings yet
- EXTERNAL FETAL MONITORING (NON - INVASIVE) (Autosaved)Document54 pagesEXTERNAL FETAL MONITORING (NON - INVASIVE) (Autosaved)Maria Pina Barbado PonceNo ratings yet
- Nur 221 Cardiac DisorderDocument22 pagesNur 221 Cardiac DisorderMaria Pina Barbado PonceNo ratings yet
- Submodule3 Theoretical Empirical-Basis Ver2 29nov2018Document17 pagesSubmodule3 Theoretical Empirical-Basis Ver2 29nov2018Maria Pina Barbado PonceNo ratings yet
- Urinary Germicides PharmaDocument11 pagesUrinary Germicides PharmaMaria Pina Barbado PonceNo ratings yet
- High Risk Labor and DeliveryDocument8 pagesHigh Risk Labor and DeliveryMaria Pina Barbado PonceNo ratings yet
- Human Machine Interfac1Document10 pagesHuman Machine Interfac1Maria Pina Barbado PonceNo ratings yet
- Module Nutrition and Diet Therapy Chapter 3Document5 pagesModule Nutrition and Diet Therapy Chapter 3Maria Pina Barbado PonceNo ratings yet
- Pinya ReflectionDocument2 pagesPinya ReflectionMaria Pina Barbado PonceNo ratings yet
- Community Health Survey: College of NursingDocument3 pagesCommunity Health Survey: College of NursingMaria Pina Barbado PonceNo ratings yet
- Comparative Chart FrontDocument1 pageComparative Chart Frontbella friscaamaliaNo ratings yet
- RANITIDINEDocument2 pagesRANITIDINEChoox PriiNo ratings yet
- Armodafinil and ModafinilDocument1 pageArmodafinil and ModafinilJayson TribacoNo ratings yet
- Acute Pancreatitis in Children Risk Factors, Management, and OutcomesDocument6 pagesAcute Pancreatitis in Children Risk Factors, Management, and OutcomesjcambiottiNo ratings yet
- Glomerular Disorders - Part I & Part II (ARI NOTES)Document144 pagesGlomerular Disorders - Part I & Part II (ARI NOTES)Laiba FatimaNo ratings yet
- Cara Melihat Data Trend Penggunaan Barang Fast MoveingDocument164 pagesCara Melihat Data Trend Penggunaan Barang Fast MoveingRahul UmarelaNo ratings yet
- Grants Released in Fy 2022-23Document20 pagesGrants Released in Fy 2022-23infoNo ratings yet
- Beamotil Tablet Information LeafletDocument3 pagesBeamotil Tablet Information Leafletadam malikNo ratings yet
- BerodualDocument1 pageBerodualAelysa PabloNo ratings yet
- RULAHASAN U15100002 Case Manual (W4) Rotation3Document8 pagesRULAHASAN U15100002 Case Manual (W4) Rotation3HIND MOHAMEDNo ratings yet
- Von WillebrandDocument11 pagesVon WillebrandRAHUL SUTHARNo ratings yet
- Jurnal Analis KesehatanDocument7 pagesJurnal Analis KesehatanMugiaman Edi hamdaniNo ratings yet
- ArrhythmiaDocument8 pagesArrhythmiaPrecious Grace CabahugNo ratings yet
- Review of Literature On Diabetes Mellitus in IndiaDocument6 pagesReview of Literature On Diabetes Mellitus in Indiaafmztsqbdnusia100% (1)
- Anaemia in PregnancyDocument29 pagesAnaemia in PregnancySampritha P GNo ratings yet
- Hallucinations PresentationDocument14 pagesHallucinations PresentationAbeer salehNo ratings yet
- New Price ListDocument25 pagesNew Price ListayurtrixofficialNo ratings yet
- DP New Patient Form - 2023Document5 pagesDP New Patient Form - 2023cdbn2326No ratings yet
- COVID-19 - Vaccine - AstraZeneca - UK - Vaccine Analysis Print 24 Nov 2022Document132 pagesCOVID-19 - Vaccine - AstraZeneca - UK - Vaccine Analysis Print 24 Nov 2022Mary-Jane StevensNo ratings yet
- Colorectal AdenocarcinomaDocument48 pagesColorectal Adenocarcinomamingchuan chuNo ratings yet
- J Neuro Oncol 2022Document10 pagesJ Neuro Oncol 2022EvelynNo ratings yet
- 2.4 SURG1 OncoDocument8 pages2.4 SURG1 OncoGeriz Daniella VigoNo ratings yet
- Immunopatologi Sepsis - DR Nur Farhanah SPPD K-PTIDocument29 pagesImmunopatologi Sepsis - DR Nur Farhanah SPPD K-PTIanita tri hastutiNo ratings yet
- MICP CaseDocument5 pagesMICP CaseRALPH EDELWEISS GAPASINNo ratings yet
- Applied Radiation Oncology: Case Report: Strip Alopecia in High-Dose VMAT-based Stereotactic RadiosurgeryDocument4 pagesApplied Radiation Oncology: Case Report: Strip Alopecia in High-Dose VMAT-based Stereotactic RadiosurgeryBiplab SarkarNo ratings yet
- Atrial Fibrillation Occurring During Acute Hospitalization AHA 2023Document23 pagesAtrial Fibrillation Occurring During Acute Hospitalization AHA 2023Lena Hinojosa SarabiaNo ratings yet
- Anti-Inflammatory AssignmentDocument2 pagesAnti-Inflammatory AssignmentNicole Ava ChangNo ratings yet