Professional Documents
Culture Documents
A22M0163DR - Arpon
Uploaded by
Anton CornelCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A22M0163DR - Arpon
Uploaded by
Anton CornelCopyright:
Available Formats
OncoStrands™
Building A (G.01)
18-24 Ricketts Road
Mount Waverley
Essential Panel VIC 3149
Australia
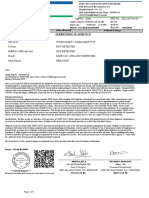
PATIENT PHYSICIAN SPECIMEN CASE
NAME SEX ORDERING PHYSICIAN EXT. SPECIMEN ID ACCESSION#
Roy Daubet Male Dr Annlelyn Beryl Ong-Cornel 22H1451 (University of Perpetual Help A22M0163DR
ARPON Medical Center)
FACILITY DATE
DATE OF BIRTH University of Perpetual Help DATE RECEIVED REPORTED
29/12/1966 MRN# Medical Center 18/09/2022 21/09/2022
- SPECIMEN TYPE
DISEASE DATE ORDERED REVIEW
Adenocarcinoma COPY TO Formalin-fixed paraffin-embedded tissue STATUS
of lung specimen Final
-
ADDRESS % TUMOR CELLULARITY REPORTED
No.55 70% BY
Concha Cruz Drive Dr. Vivek
BF Homes Rathi
Paranaque City 1720
Philippines
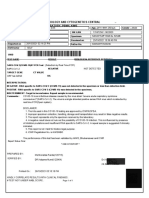
Report Summary
• • A variant of strong clinical significance detected -
TIER 1A, BRAF p.V600E - this variant has therapeutic significance in non-small cell lung carcinoma patients, with FDA approved
and NCCN/ESMO recommended therapeutic agents available, as described below.
• • Pertinent negatives - no clinically relevant mutations detected in EGFR, KRAS or MET, and no fusion transcripts detected in
ALK, ROS1, RET, NTRK1, NTRK2 or NTRK3.
• • PD-L1: TPS = 70% in this sample (on Ventana SP263)
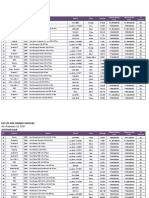
IA IB IIC IID Trials
1 0 1 0 2
Clinical Implications
VARIANT SELECT
TIER DETECTED CLINICAL IMPACT CLINICAL
(GENE/SYNTAX) TRIALS
May benefit from: Vemurafenib or Dabrafenib
In Tumor Type: Non-small cell lung cancer
IA BRAF 2
p.V600E May benefit from: Dabrafenib + Trametinib
Malignant tumor of lung, Adenocarcinoma of lung, Non-small
In Tumor Type: cell carcinoma, Non-small cell lung cancer, Squamous cell
POWERED BY Email: genomics@lifestrandsgx.com
Page 1
OncoStrands™
Essential Panel
PATIENT DOB DISEASE ACCESSION MRN REPORT DATE REPORT STATUS
Roy Daubet ARPON 29/12/1966 Adenocarcinoma of lung A22M0163DR - 21/09/2022 Final
carcinoma of lung, Glioblastoma, or Large cell carcinoma of
lung
May benefit from: Pembrolizumab or Ipilimumab + Nivolumab
Squamous cell carcinoma of lung, Adenocarcinoma of lung,
In Tumor Type: Non-small cell lung cancer, Large cell carcinoma of lung, or
Non-small cell carcinoma
Bevacizumab-bvzr, Bevacizumab-awwb, Bevacizumab, or
May benefit from: Atezolizumab
Nonsquamous nonsmall cell neoplasm of lung,
In Tumor Type: Adenocarcinoma of lung, or Large cell carcinoma of lung
May benefit from: Dabrafenib
Squamous cell carcinoma of lung, Adenocarcinoma of lung,
In Tumor Type: or Large cell carcinoma of lung
May benefit from: Vemurafenib
Squamous cell carcinoma of lung, Adenocarcinoma of lung,
In Tumor Type: or Large cell carcinoma of lung
TP53
IIC No guidelines existing in the report. 0
p.P278A
Other Test Results
• • Cytopathology: Left lower lobe lung - atypical cells highly suspicious for malignancy, favour adenocarcinoma.
• • PD-L1 IMMUNOHISTOCHEMISTRY (performed by LifeStrands Genomics) -
VENTANA PD-L1 (SP263) Rabbit Monoclonal Primary Antibody Assay:
-- Positive control results (Acceptable)
-- Negative control results (Acceptable)
-- Adequate tumour cells (>100 cells) are present
Description: Moderate and weak, occasionally strong partial and sometimes complete membranous staining in 70% of
tumour cells
Tumour Proportion Score: 70%
Clinical Interpretations
BRAF p.V600E c.1799T>A Tier IA NM_004333.4 VAF: 32.4% Depth: 12370
GENE: BRAF, serine/threonine-protein kinase B-raf, is a member of the Raf family of serine/threonine protein kinases, which signals
through the MAP kinase pathway to regulate cell proliferation and cell growth (PMID: 24737949, PMID: 29540830). BRAF mutations
and fusions have been identified in a variety of cancers, including, colorectal (PMID: 30122982), lung (PMID: 29729495), thyroid
(PMID: 12970315), and melanoma (PMID: 24737949), and a number of mutations have also been demonstrated to confer drug
resistance (PMID: 27478040).
POWERED BY Email: genomics@lifestrandsgx.com
Page 2
OncoStrands™
Essential Panel
PATIENT DOB DISEASE ACCESSION MRN REPORT DATE REPORT STATUS
Roy Daubet ARPON 29/12/1966 Adenocarcinoma of lung A22M0163DR - 21/09/2022 Final
VARIANT: BRAF V600E (previously reported as V599E) lies within the activation segment of the kinase domain of the Braf protein
(PMID: 15035987). V600E confers a gain of function to the Braf protein as demonstrated by increased Braf kinase activity,
downstream signaling, and the ability to transform cells in culture (PMID: 15035987, PMID: 29533785).
THERAPEUTICS: Currently, there are FDA approved and NCCN and ESMO guidelines recommended BRAF inhibitors approved for
treatment for advanced non-small cell lung cancer patients.
Dabrafenib in combination with trametinib is FDA and EMA approved and NCCN and ASCO guidelines recommended for use in
non-small cell lung cancer harbouring BRAF V600E mutation as preferred first-line therapy or subsequent therapy following
disease progression on a non-BRAF-targeted regimen.
Dabrafenib in combination with trametinib is ESMO (PMID: 30285222, 2018, https://www.esmo.org/guidelines/lung-and-chest-
tumours/clinical-practice-living-guidelines-metastatic-non-small-cell-lung-cancer, 2020) guideline recommended for use in
non-small cell lung cancer harboring a BRAF Val600 mutation as first-line or second-line therapy.
Ipilimumab in combination with nivolumab and chemotherapeutic agents is NCCN (Non-Small Cell Lung Cancer, 3.2022) guideline
recommended for use in non-small cell lung cancer harboring a BRAF p.(Val600Glu) mutation as first-line or subsequent therapy
without PD-1/PD-L-1 inhibitor contraindication.
Some evidence indicates that metastatic non-small cell lung cancer harboring a BRAF V600 mutation may benefit from sorafenib
in combination with erlotinib, based on a retrospective study of 72 mixed ethnicity participants (PMID: 30642457, 2018).
Some evidence indicates that metastatic non-small cell lung cancer harboring a BRAF V600 mutation may benefit from
vemurafenib in combination with cobimetinib, based on a retrospective study of 72 mixed ethnicity participants (PMID:
30642457, 2018).
Atezolizumab in combination with chemotherapeutic agents is NCCN (Non-Small Cell Lung Cancer, 3.2022) guideline
recommended for use in non-squamous non-small cell lung cancer harboring a BRAF V600E mutation as first-line therapy
without PD-1/PD-L-1 inhibitor contraindication or as preferred subsequent therapy when PD-1/PD-L1 inhibitor naive.
TP53 p.P278A c.832C>G Tier IIC NM_000546.5 VAF: 40.3% Depth: 847
GENE: TP53, tumor protein p53, is a tumor suppressor (PMID: 30562755) and oncogene (PMID: 30577483) involved in cell cycle
arrest and apoptosis, and is the most frequently mutated gene in cancer (PMID: 10065147, PMID: 22713868). TP53 germline
mutations are common in Li-Fraumeni syndrome (PMID: 30239254) and somatic missense mutations are frequent in almost all
cancer types (PMID: 30224644) and are also implicated in chemoresistance (PMID: 9927204, PMID: 24065105, PMID: 27066457).
VARIANT: TP53 P278A lies within the DNA-binding domain of the Tp53 protein (PMID: 22713868). P278A results in a loss of
transactivation activity in yeast assays (PMID: 16861262), but has not been characterized in human cells and therefore, its effect
on Tp53 protein function is unknown.
THERAPEUTICS: Currently, there are no FDA approved or NCCN-Compendium recommended treatment options for patients
harbouring this variant.
In a Phase I trial, the combination of Votrient (pazopanib) and Zolinza (vorinostat) improved progression-free survival and overall
survival in advanced solid tumor patients harboring TP53 hotspot mutations, and resulted in an increased stable disease rate of
45% (5/11), compared to a stable disease rate of 16% (4/25) in patients without detected TP53 mutations (PMID: 25669829). In a
Phase I trial, Adavosertib (MK-1775) treatment resulted in a prtial response in 3 and progressive disease in 2 of 6 patients with
advanced solid tumors harboring TP53 mutations (J Clin Oncol 38: 2020 (suppl; abstr 3624); NCT01748825).In a retrospective
analysis of a Phase I trial, Adavosertib (MK-1775) combined with a chemotherapy resulted in a 21% (4/19) response rate in
advanced solid tumor patients harboring a TP53 mutation and in those without a TP53 mutation, a 12% (4/33) response rate was
observed (PMID: 27601554). In a clinical study, VEGF/VEGFR inhibitor treatment resulted in improved rates of response (stable
disease over 6 months/partial/complete response, 31% vs 7%), time-to-treatment failure, and overall survival (both p<0.01)
compared to control in patients with TP53 mutant advanced solid tumors (n=106), but not in patients with TP53 wild-type tumors
(n=82) (PMID: 27466356). In a retrospective study, Avastin (bevacizumab) treatment was associated with increased progression-
free survival in cancer patients carrying TP53 mutations (PMID: 23670029).
POWERED BY Email: genomics@lifestrandsgx.com
Page 3
OncoStrands™
Essential Panel
PATIENT DOB DISEASE ACCESSION MRN REPORT DATE REPORT STATUS
Roy Daubet ARPON 29/12/1966 Adenocarcinoma of lung A22M0163DR - 21/09/2022 Final
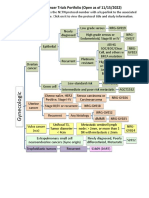
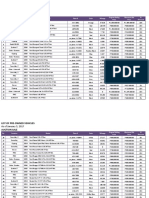
Clinical Trials
Clinical Trials associated with this patient's genomic profile and tumor type as displayed below.
TITLE TRIAL IDENTIFIER PHASE VARIANT
Targeted Therapy Directed by NCT02465060 II BRAF
Genetic Testing in Treating Patients https://clinicaltrials.gov/show/NCT02465060 p.V600E
With Advanced Refractory Solid c.1799T>A
Tumors, Lymphomas, or Multiple
Myeloma (The MATCH Screening
Trial)
Study of Safety, Pharmacokinetics, NCT04249843 I BRAF
and Antitumor Activity of https://clinicaltrials.gov/show/NCT04249843 p.V600E
BGB-3245 in Participants With c.1799T>A
Advanced or Refractory Tumors
Significant Negative Findings
No clinically relevant variants detected in EGFR, MET or KRAS, and no fusion transcripts detected in ALK, ROS1, RET, NTRK1,
NTRK, NTRK3.
Tier III - Variants of Uncertain Significance
No variants were reported for this classification tier.
Other Comments
Current FDA approved treatments for specific genetic alterations in metastatic non-small
cell lung carcinoma-
ALK fusions - Crizotinib, ceritinib, alectinib, brigatinib, lorlatinib
BRAF V600E - Dabrafenib + trametinib
EGFR ex 19 del, L858Rm - Afatinib, dacomitinib, erlotinib, gefitinib, osimertinib
EGFR ex 20 insertions - Amivantamab
EGFR nonresistant mutations other than exon 19deletions and L858R - Afatinib
EGFR T790M - Osimertinib
KRAS G12C - Sotorasib
MET exon 14 skipping - Capmatinib, tepotinib
RET fusions - Pralsetinib, selpercatinib
ROS1 fusions - Crizotinib, entrectinib
FDA approved tumour agnostic indications -
POWERED BY Email: genomics@lifestrandsgx.com
Page 4
OncoStrands™
Essential Panel
PATIENT DOB DISEASE ACCESSION MRN REPORT DATE REPORT STATUS
Roy Daubet ARPON 29/12/1966 Adenocarcinoma of lung A22M0163DR - 21/09/2022 Final
NTRK1 or NTRK2 or NTRK3 fusions - Entrectinib, larotrectinib
MSI-H, TMB-H - Pembrolizumab
FDA-listed genetic alterations contraindicated for specific treatments with TRK inhibitors -
NTRK1 and NTRK3 known acquired resistance mutations (eg, NTRK1 G595R and G667C; NTRK3 F617L, G623R, and G696A)
FDA-approved combination treatments with nontargeted therapies for specific genetic
alterations-
EGFR exon 19 deletions, L858R - Erlotinib + ramucirumab
Current NCCN recommended biomarkers for sequencing in NSCLC-
Mutations - BRAF, EGFR, HER2, KRAS, MET
Amplifications - MET
Fusions - ALK, NTRK1, NTRK2, NTRK3, RET, ROS1
Tier Definitions
Tier I-A: Approved therapy. Included in professional guidelines.
Tier I-B: Well-powered studies with consensus from experts in the field.
Tier II-C: Approved therapies for different tumour types or investigational therapies. Multiple small published studies with some
consensus. Inclusion criteria for clinical trials.
Tier II-D: Limited clinical or preclinical studies.
Tier III (VUS): Variants of Unknown Clinical Significance.
Tier IV: Benign or likely benign variants (not included in the report)
Test Information
REPORTED GENES: AKT1, AKT2, AKT3, ALK, AR, ARAF, BRAF, CD274, CDK4, CDKN2A, CHEK2, CTNNB1, EGFR, ERBB2, ERBB3, ERBB4, ESR1, FGFR1,
FGFR2, FGFR3, FGFR4, FLT3, GNA11, GNAQ, GNAS, HRAS, IDH1, IDH2, KIT, KRAS, MAP2K1, MAP2K2, MET, MTOR, NRAS, NRG1, NTRK1, NTRK2, NTRK3,
NUTM1, PDGFRA, PIK3CA, PTEN, RAF1, RET, ROS1, RSPO2, RSPO3, SMO, TP53 CGW VERSION: CGW_v6.20 DATABASE DETAILS: The versions,
releases, builds, dates of the following databases were used to generate this report: Genomic Build: GRCh37.p13 | Genomic Annotation
Sources: NCBI RefSeq v105 | COSMIC: v96 | dbNSFP: 4.2c | ExAC: v1.0 | dbscSNV: v1.1 | ClinVar: 20220702 | NHLBI ESP: v.0.0.30 | gnomAD: r2.1 |
dbSNP: 149 ASSAY METHODOLOGY:
ASSAY METHODS: This is a laboratory developed test and has been extensively validated in-house utilising the Oncomine™ Precision targeted
next-generation sequencing assay, which is run on the ThermoFisher GenexusTM Integrated Sequencer to detect DNA and RNA based variants
in formalin-fixed paraffin embedded (FFPE) samples. The assay uses ThermoFisher’s proprietary AmpliSeq™ enrichment chemistry to enable
nucleic acid input sequencing. The Oncomine™ Precision assay is designed to detect multiple classes of variants including single nucleotide
variants (SNVs), multi-nucleotide variants (MNVs), small Insertions /Deletions (Indels), copy number variations (CNVs), and gene fusions. The
50 gene panel includes detection of hotspot mutations in 45 genes, CNV detection in 14 genes, and the detection of gene-fusions from RNA
in 18 genes.
DNA and RNA are extracted and quantified using the GenexusTM Purification System. The Sequencer performs library preparation, sequencing,
and secondary analysis. Multiplex primer design and sample barcoding leverage Ion AmpliSeqTM HD technology to generate results from
multiple samples in a single run.
SECONDARY ANALYSIS METHODS: DNA/RNA analysis was performed locally using GenexusTM analysis platform. Variant files i.e., VCF/BAM files
from this pipeline were then uploaded to the Clinical Genomics Workspace (CGW) from Pierian. Variant files were then parsed and combined
into compatible formats and analyzed using the CGW software platform using an in-house bioinformatics pipeline.
VARIANT CALLING: Variants are reported according to HGVS nomenclature (www.hgvs.org/mutnomen) and classified per the AMP
classification system into tiers IA, IB, IIC, IID, III, and IV. These tiers are stratified by clinical utility ('actionability' for clinical decision-making as
to diagnosis, prognosis, treatment options, and carrier status) and previously reported data in the medical literature. Variants found in
gnomAD (https:// gnomad.broadinstitute.org/) that have ≥1% minor allele frequency (except those that are also in Clinvar denoted as clinically
POWERED BY Email: genomics@lifestrandsgx.com
Page 5
OncoStrands™
Essential Panel
PATIENT DOB DISEASE ACCESSION MRN REPORT DATE REPORT STATUS
Roy Daubet ARPON 29/12/1966 Adenocarcinoma of lung A22M0163DR - 21/09/2022 Final
relevant, used in a clinical diagnostic assay, or reported as a mutation in a publication) are classified as known polymorphisms.
DNA/RNA VARIANTS (SNVS, INSERTIONS, DELETIONS, CNVS, AND GENE FUSIONS)
Based on the in-house validation using clinical samples and various types of reference standards, the assay can detect SNVs/Short Deletions
with 100% accuracy, sensitivity and specificity at ≥5% limit of detection. For the detection of Copy Number Variations (CNVs), the assays
demonstrated 100% accuracy, 98.6% sensitivity and 100% specificity (CNVs on NGS platforms is an estimate based on prediction algorithm
which consider multiple factors. The gene amplification of ≥5 is considered a true prediction on this platform). For Fusions, the assay
demonstrated 100% accuracy, 98.6% sensitivity and 100% specificity (based on high confidence fusion calls (≥10 copies).
Additional Notes:
• • Variants located outside of targeted regions will not be detected.
• • This assay is clinically validated for the detection of somatic variants in somatic tumor specimens.
• • It is possible that pathogenic variants may not be reported by one or more of the tools because of the parameters used. However, tool
parameters were optimized to maximize specificity and sensitivity.
OncoStrands™Essential Panel Gene List
DNA Hotspot Genes
AKT1 AKT2 AKT3 ALK AR ARAF BRAF CDK4 CDKN2A CHEK2 CTNNB1 EGFR ERBB2 ERBB3 ERBB4 ESR1 FGFR1 FGFR2 FGFR3 FGFR4 FLT3 GNA11
GNAQ GNAS HRAS IDH1 IDH2 KIT KRAS MAP2K1 MAP2K2 MET MTOR NRAS NTRK1 NTRK2 NTRK3 PDGFRA PIK3CA PTEN RAF1 RET ROS1 SMO TP53
Copy Number Variation (CNV) Genes
ALK AR CD274 CDKN2A EGFR ERBB2 ERBB3 FGFR1 FGFR2 FGFR3 KRAS MET PIK3CA PTEN
Fusion (RNA) Genes
ALK AR BRAF EGFR ESR1 FGFR1 FGFR2 FGFR3 MET NRG1 NTRK1 NTRK2 NTRK3 NUTM1 RET ROS1 RSPO2 RSPO3
DISCLAIMER:
This is a laboratory developed test, and its performance characteristics have been determined by LifeStrands Genomics. This Report was
generated using the materials and methods described above, which required the use of various reagents, protocols, instruments, software,
databases, and other items, some of which were provided or made accessible by third parties. A defect or malfunction in any such reagents,
protocols, instruments, software, databases, and or other items may compromise the quality or accuracy of the Report. The Report has been
created based on, or incorporates references to, various scientific manuscripts, references, and other sources of information, including
without limitation manuscripts, references, and other sources of information that were prepared by third parties that describe correlations
between certain genetic mutations and particular diseases (and/or certain therapeutics that may be useful in ameliorating the effects of such
diseases). Such information and correlations are subject to change over time in response to future scientific and medical findings. LifeStrands
Genomics makes no representation or warranty of any kind, expressed or implied, regarding the accuracy of the information provided by or
contained in such manuscripts, references, and other sources of information. If any of the information provided by or contained in such
manuscripts, references, and other sources is later determined to be inaccurate, the accuracy and quality of the Report may be adversely
impacted. LifeStrands Genomics is not obligated to notify you of any impact that future scientific or medical research findings may have on
the Report. The Report must always be interpreted and considered within the clinical context, and a physician should always consider the
Report along with all other pertinent information and data that a physician would prudently consider prior to providing a diagnosis to a
patient or developing and implementing a plan of care for a patient. The Report should never be considered or relied upon alone in making
any diagnosis or prognosis. The manifestation of many diseases is caused by more than one gene variant, a single gene variant may be
relevant to more than one disease, and certain relevant gene variants may not have been considered in the Report. In addition, many diseases
are caused or influenced by modifier genes, epigenetic factors, environmental factors, and other variables that are not addressed by the
Report (or that are otherwise unknown). This Report is based on a next generation sequencing assay which does not distinguish between
somatic and germline variants. If a germline variant is in question, further testing may be recommended. As such, the relevance of the Report
should be interpreted in the context of a patient's clinical manifestations. The Report provided by LifeStrands Genomics is provided on an AS
IS basis. LifeStrands Genomics makes no representation or warranty of any kind, expressed or implied, regarding the Report. In no event shall
LifeStrands Genomics be liable for any actual damages, indirect damages, and/or special or consequential damages arising out of or in any
way connected with the Report, your use of the Report, your reliance on the Report, or any defect or inaccurate information included within
the Report. Medical knowledge annotation is constantly updated and reflects the current knowledge at the time.
POWERED BY Email: genomics@lifestrandsgx.com
Page 6
OncoStrands™
Essential Panel
PATIENT DOB DISEASE ACCESSION MRN REPORT DATE REPORT STATUS
Roy Daubet ARPON 29/12/1966 Adenocarcinoma of lung A22M0163DR - 21/09/2022 Final
Report electronically reviewed and signed out by: Dr Vivek Rathi
Date Reported: 21/09/2022
POWERED BY Email: genomics@lifestrandsgx.com
Page 7
You might also like
- Adrenal IncidentalomaDocument46 pagesAdrenal IncidentalomaFelipe GomezNo ratings yet
- INITIATING ANTIFUNGAL THERAPY FOR INVASIVE FUNGAL INFECTIONDocument17 pagesINITIATING ANTIFUNGAL THERAPY FOR INVASIVE FUNGAL INFECTIONdocjeevan89No ratings yet
- BAETS Guidelines 2003Document28 pagesBAETS Guidelines 2003Claudia IrimieNo ratings yet
- Cancer Sarcoma Chemotherapy Regimen V2.1 May 2012Document75 pagesCancer Sarcoma Chemotherapy Regimen V2.1 May 2012Niken AmritaNo ratings yet
- Incidentaloma Adrenal Endocrine Society 2020Document128 pagesIncidentaloma Adrenal Endocrine Society 2020Adriana MirandaNo ratings yet
- Adult Desmoid Tumors: Biology, Management and Ongoing TrialsDocument7 pagesAdult Desmoid Tumors: Biology, Management and Ongoing TrialsGustavo GasperiNo ratings yet
- Guideline for Suspected Adrenal IncidentalomaDocument3 pagesGuideline for Suspected Adrenal IncidentalomaMica SaeronNo ratings yet
- Patient with Right Lower Lobe PneumoniaDocument20 pagesPatient with Right Lower Lobe PneumoniaranjithNo ratings yet
- Adrenal IncidentalomaDocument128 pagesAdrenal IncidentalomaJorge Adrian Romero SanchezNo ratings yet
- Episcleral Brachytherapy For RetinoblastomaDocument6 pagesEpiscleral Brachytherapy For Retinoblastomamadimadi11No ratings yet
- s41587-024-02168-5Document5 pagess41587-024-02168-5nfbdywhjntNo ratings yet
- ReportDocument1 pageReportabbasalizaidi07No ratings yet
- WHO Classifications of Lung TumorDocument26 pagesWHO Classifications of Lung Tumorayeshanabilla8808100% (1)
- Davis Symposium AdvancesInSarcomaDocument55 pagesDavis Symposium AdvancesInSarcomaFernando SilalahiNo ratings yet
- TDM Monitoring Sampling Guideline Form 2022 Iso CodeDocument2 pagesTDM Monitoring Sampling Guideline Form 2022 Iso Codenur nadirahNo ratings yet
- Neeman Presentation On OncologyDocument20 pagesNeeman Presentation On Oncologyjlduorah7118100% (1)
- Manzil DuaDocument1 pageManzil DuaAshfaque HossainNo ratings yet
- NCTN GYNE TrialsDocument3 pagesNCTN GYNE TrialsYagami SinNo ratings yet
- Report 2419324Document9 pagesReport 2419324Milan TiwariNo ratings yet
- Ttf1 MarkerDocument6 pagesTtf1 MarkerRuben NatarîșNo ratings yet
- Friday, 29 May 2020: Roche Analyst EventDocument44 pagesFriday, 29 May 2020: Roche Analyst EventpatrickNo ratings yet
- Der Aio - Ogic Surgery: Cryosurgery of Cutaneous CarcinomasDocument10 pagesDer Aio - Ogic Surgery: Cryosurgery of Cutaneous CarcinomasZahraNo ratings yet
- Tri Star Corporate PresentationDocument35 pagesTri Star Corporate PresentationshaanbhagatNo ratings yet
- Dept of Molecular Biology and Cytogenetics Central - Laboratory, PBMH, KimsDocument1 pageDept of Molecular Biology and Cytogenetics Central - Laboratory, PBMH, KimsashishNo ratings yet
- Dept of Molecular Biology and Cytogenetics Central - Laboratory, PBMH, KimsDocument1 pageDept of Molecular Biology and Cytogenetics Central - Laboratory, PBMH, KimsashishNo ratings yet
- Chapter 42 Tumour MarkersDocument23 pagesChapter 42 Tumour MarkersLAMA LAMANo ratings yet
- Basic OncologyDocument42 pagesBasic Oncologybudiagungnugraha100% (1)
- DEBIRI - How To StartDocument66 pagesDEBIRI - How To Startpaquidermo85No ratings yet
- Fendo 13 921812Document8 pagesFendo 13 921812ivan dario hernandez erazoNo ratings yet
- CASE 7: Cerebrovascular Accident, Bleed vs. Infarct: JMJ Marist BrothersDocument9 pagesCASE 7: Cerebrovascular Accident, Bleed vs. Infarct: JMJ Marist Brothersspain michaelisNo ratings yet
- URO 3 - Neoplasm in The Genitourinary TractDocument8 pagesURO 3 - Neoplasm in The Genitourinary TractHa Jae kyeongNo ratings yet
- 1 - Intro - E.Castro Guidelines Webinar ProstateDocument12 pages1 - Intro - E.Castro Guidelines Webinar Prostateveaceslav coscodanNo ratings yet
- Lesson 5Document3 pagesLesson 5NER CARLO SANTOSNo ratings yet
- Minimal Residual Disease in Multiple Myeloma - An Important Tool in Clinical TrialsDocument2 pagesMinimal Residual Disease in Multiple Myeloma - An Important Tool in Clinical TrialsSeungman ParkNo ratings yet
- Phase II INTERACT-ION Study: Ezabenlimab (BI 754091) and MDCF (Docetaxel, Cisplatin, and 5-Fluorouracil) Followed by Chemoradiotherapy in Patients With Stage III Squamous Cell Anal CarcinomaDocument11 pagesPhase II INTERACT-ION Study: Ezabenlimab (BI 754091) and MDCF (Docetaxel, Cisplatin, and 5-Fluorouracil) Followed by Chemoradiotherapy in Patients With Stage III Squamous Cell Anal CarcinomaStefano KimNo ratings yet
- Monthly Census JANUARY 2017: Far Eastern University Dr. Nicanor Reyes Medical Foundation Department of SurgeryDocument79 pagesMonthly Census JANUARY 2017: Far Eastern University Dr. Nicanor Reyes Medical Foundation Department of SurgeryLhaineVennetNo ratings yet
- Affimed Presentation-Mar2020 Final-1 PDFDocument22 pagesAffimed Presentation-Mar2020 Final-1 PDFElio GonzalezNo ratings yet
- Chemotherapy and Targeting Therapy in Colon CancerDocument62 pagesChemotherapy and Targeting Therapy in Colon CancerIndonesian Journal of CancerNo ratings yet
- Linfoma y Leumicias UntDocument77 pagesLinfoma y Leumicias UntJAIME YOSHIMAR MENDEZ PEREZNo ratings yet
- Tema 1 WistubaDocument58 pagesTema 1 WistubaMarcus ShawNo ratings yet
- Covid19 Sidebyside VaccinecompareDocument55 pagesCovid19 Sidebyside VaccinecompareTIFFANIE CHRISTEL UYNo ratings yet
- Recreate 1 SourceDocument3 pagesRecreate 1 SourcesayyedrindianNo ratings yet
- 4 - Uncertainty Estimation For Margin Detection in Cancer SurgeryDocument10 pages4 - Uncertainty Estimation For Margin Detection in Cancer SurgeryImtenan makkiNo ratings yet
- Solid Tumor NGS Profiling Sample ReportDocument5 pagesSolid Tumor NGS Profiling Sample Reportaditi jhaveriNo ratings yet
- Reassessment of Differentiated Thyroid Cancer Patients Using The 8th TNM Classification System: A Comparative StudyDocument10 pagesReassessment of Differentiated Thyroid Cancer Patients Using The 8th TNM Classification System: A Comparative StudyShintya DewiNo ratings yet
- Department of Laboratory SciencesDocument1 pageDepartment of Laboratory SciencesYolopoloNo ratings yet
- Clinical GuidlinesDocument200 pagesClinical GuidlinesMujtaba NadeemNo ratings yet
- Update On The Role of Egfr Inhibitors in Cancer TherapeuticsDocument19 pagesUpdate On The Role of Egfr Inhibitors in Cancer TherapeuticskonasperhatiNo ratings yet
- PSMADocument10 pagesPSMADiego GavilanesNo ratings yet
- DR Sandeep AgarwlDocument43 pagesDR Sandeep AgarwlPushpanjali Crosslay HospitalNo ratings yet
- Journal of Feline Medicine and Surgery 2013 Scherk 785 808Document26 pagesJournal of Feline Medicine and Surgery 2013 Scherk 785 808Roberto RibeiroNo ratings yet
- Covidl 9 Test - Google Drive: St. Luke'sDocument2 pagesCovidl 9 Test - Google Drive: St. Luke'sAya BeeNo ratings yet
- Wie Demeyer 2019Document7 pagesWie Demeyer 2019Gustavo VerardinoNo ratings yet
- CS21388130 Report 1Document1 pageCS21388130 Report 1Aswin BabuNo ratings yet
- Anestesia FelinaDocument33 pagesAnestesia FelinaAna Francisca Flores MestreNo ratings yet
- Articulo 1recto SuperiorDocument7 pagesArticulo 1recto SuperiorCarolinaNo ratings yet
- Protocolo de Vacunacion Gato IsfmDocument24 pagesProtocolo de Vacunacion Gato IsfmValentina FranciscaNo ratings yet
- Bionikk Lancet 2022 VanoDocument13 pagesBionikk Lancet 2022 VanomarieNo ratings yet
- ActaDV 100 11 5753Document9 pagesActaDV 100 11 5753NandaNo ratings yet
- Hypofractionated and Stereotactic Radiation Therapy: A Practical GuideFrom EverandHypofractionated and Stereotactic Radiation Therapy: A Practical GuideOrit Kaidar-PersonNo ratings yet
- NSCLC Guideline Updates Focus on Targeted TherapiesDocument22 pagesNSCLC Guideline Updates Focus on Targeted TherapiesAnton CornelNo ratings yet
- Ib 21PD0092-93Document3 pagesIb 21PD0092-93Anton CornelNo ratings yet
- Ltopf Individual Application Form PDFDocument1 pageLtopf Individual Application Form PDFAnonymous ouLAfTt81% (32)
- Cost-Plus-Percentage-Fee Agreement BreakdownDocument12 pagesCost-Plus-Percentage-Fee Agreement BreakdownAnton Cornel100% (4)
- DEED OF SALE OF MOTOR VEHICLE-templateDocument2 pagesDEED OF SALE OF MOTOR VEHICLE-templateIvy Mallari QuintoNo ratings yet
- The Mad Drive September-October Masterlist 2015Document887 pagesThe Mad Drive September-October Masterlist 2015Anton CornelNo ratings yet
- GPS102-B User ManualDocument19 pagesGPS102-B User ManualMarco ChacanaNo ratings yet
- Wheels QuotationDocument4 pagesWheels QuotationAnton CornelNo ratings yet
- Quote 2016 TantanDocument12 pagesQuote 2016 TantanAnton CornelNo ratings yet
- BAI Annual Report 2013Document62 pagesBAI Annual Report 2013Anton Cornel0% (1)
- Peter Xu Contact and Bicycle Parts PricelistDocument6 pagesPeter Xu Contact and Bicycle Parts PricelistAnton CornelNo ratings yet
- The Mad Drive November Masterlist 2016Document701 pagesThe Mad Drive November Masterlist 2016Anton CornelNo ratings yet
- 2015 Transformation Story Butuan CityDocument6 pages2015 Transformation Story Butuan CityAnton CornelNo ratings yet
- BRO PAT Deli Cheesecake Recipe Sheet - V2 - tcm293-97740Document2 pagesBRO PAT Deli Cheesecake Recipe Sheet - V2 - tcm293-97740Anton CornelNo ratings yet
- Auction PricelistDocument14 pagesAuction PricelistAnton CornelNo ratings yet
- Auction Pricelist 1.12.17 PDFDocument15 pagesAuction Pricelist 1.12.17 PDFAnton CornelNo ratings yet
- Kalita Wave InstructionsDocument2 pagesKalita Wave InstructionsAnton CornelNo ratings yet
- Respiratory Medicine 2022 Curriculum FINALDocument58 pagesRespiratory Medicine 2022 Curriculum FINALDr Sneha's Skin and Allergy Clinic IndiaNo ratings yet
- Spinal Tumor StrongDocument45 pagesSpinal Tumor StrongbettyNo ratings yet
- Vessel Design AssignmentDocument15 pagesVessel Design AssignmentBlue BlazeNo ratings yet
- Week 5 Quiz GenesDocument7 pagesWeek 5 Quiz Genesapi-288374214No ratings yet
- Learning Lab - A Proposal Writing Short CourseDocument9 pagesLearning Lab - A Proposal Writing Short CourseMichael JonesNo ratings yet
- 50315-72475-1-PB (1) Parotid TumorDocument3 pages50315-72475-1-PB (1) Parotid TumorShashank MisraNo ratings yet
- Spatial Components of Molecular Tissue BiologyDocument11 pagesSpatial Components of Molecular Tissue Biologymd913No ratings yet
- Vitamin KDocument2 pagesVitamin KDee Trooth100% (1)
- Homeopathic PracticeDocument313 pagesHomeopathic PracticeMarian Claudiu50% (2)
- Ca LidahDocument27 pagesCa LidahArnaz AdisaputraNo ratings yet
- Darul Ulum Pesantren Seeks New TeachersDocument8 pagesDarul Ulum Pesantren Seeks New TeachersDidik SadiantoNo ratings yet
- Clinical Benefit in Patients With Advanced Solid Tumors Treated With Modified Citrus Pectin: A Prospective Pilot StudyDocument8 pagesClinical Benefit in Patients With Advanced Solid Tumors Treated With Modified Citrus Pectin: A Prospective Pilot Studyyafit_armon5854No ratings yet
- Digitalali CX Pathway - Transcript - Digital TechnologiesDocument12 pagesDigitalali CX Pathway - Transcript - Digital TechnologiesN.a. M. TandayagNo ratings yet
- English For Academic and Professional PurposesDocument10 pagesEnglish For Academic and Professional Purposesazileinra OhNo ratings yet
- Radiation Risk AssessmentDocument48 pagesRadiation Risk AssessmentKonstantinos G. ZeimpekisNo ratings yet
- 681 FullDocument6 pages681 FullKurnia AnharNo ratings yet
- TEENS Marijuana BrochureDocument20 pagesTEENS Marijuana BrochureGabriella FeraruNo ratings yet
- Triple Negative Breast Cancer Therapy Current and Future Perspectives (Review)Document17 pagesTriple Negative Breast Cancer Therapy Current and Future Perspectives (Review)asdffdsaNo ratings yet
- Dr. Mohammed E. Zakaria - Medics Index MemberDocument4 pagesDr. Mohammed E. Zakaria - Medics Index MemberMedicsindex Telepin SlidecaseNo ratings yet
- Breast Cancer Case StudyDocument66 pagesBreast Cancer Case StudyChandan Srivastava100% (2)
- Lifeline Provides Critical Illness CoverageDocument60 pagesLifeline Provides Critical Illness CoverageAsish Kumar JenaNo ratings yet
- How To Cope With Lifes Problems Vol. 1 Study GuideDocument141 pagesHow To Cope With Lifes Problems Vol. 1 Study GuideJedediah Phiri100% (1)
- Radiotherapy for Non-Melanoma Skin CancerDocument9 pagesRadiotherapy for Non-Melanoma Skin CancerJesús Alexis Alvarado AbreuNo ratings yet
- Primer: Hepatocellular CarcinomaDocument28 pagesPrimer: Hepatocellular CarcinomaAinun Aii NoorNo ratings yet
- Saturn in Scorpio 2Document13 pagesSaturn in Scorpio 2Simon LoongNo ratings yet
- Storybook - Lucy Has A TumourDocument19 pagesStorybook - Lucy Has A TumourZeynepNo ratings yet
- FriquitinibDocument11 pagesFriquitinibMr. LNo ratings yet
- 05.15.17 Bone Pathology (Atkinson) - NotesDocument8 pages05.15.17 Bone Pathology (Atkinson) - NotesDan WuiytNo ratings yet
- Quiz Bee Questions Grade 4Document3 pagesQuiz Bee Questions Grade 4Suset Binongo Losanoy88% (56)