Professional Documents
Culture Documents
Metotrexat
Uploaded by
Muhamad Rizqy MaulanaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Metotrexat
Uploaded by
Muhamad Rizqy MaulanaCopyright:
Available Formats
RESEARCH ARTICLES
Methotrexate Pharmacok inetics
K. B. BISCHOFF*$, R. L. DEDRICK*, D. S. ZAHARKOt, and J. A. LONGSTRETH”
concept to pharmacokinetic modeling should permit the
Abstract 0 A pharmacokinetic model is presented to predict the quantitation of interspecies differences with respect to
detailed distribution and excretion of methotrexate in several drug distribution and prediction of drug concentration
mammalian species over a wide range of doses. Anatomical com-
partments include liver, kidneys, gastrointestinal tract, muscle, at specific sites as functions of dose schedule and route
and plasma; multicompartment representations simulate biliary of administration. Reliable prediction can enable more
excretion and movement of drug through the gastrointestinal tract effective drug screening and enhance the ability of the
with partial reabsorption. Tissue-to-plasma distribution coefficients clinician to devise optimum therapeutic regimens. The
include linear and strong saturable (presumed dihydrofolate re-
ductase) effects. Required parameters are measured directly or latter is of particular concern for antineoplastic drugs
estimated on the basis of physiological principles for mice, rats, for which therapeutic effect and toxicity must be bal-
dogs, and man. anced carefully.
Keyphrases 0 Methotrexate pharmacokinetics-model, mammals
Tissue/plasma distribution coefficients-methotrexate, mammals BASIS AND DEVELOPMENT OF MODEL
0 Pharmacokinetic parameters-methotrexate absorption, dis-
tribution, excretion Dihydrofolate reductase binding-metho- The model employs the lumped compartmental approach with the
trexate Model, methotrexate distribution, mammals-one, two restriction that the volumes, flows, and other properties be physi-
compartments ologically meaningful and usually independently measured. The
concept of flow-limited conditions is used for all body regions. If
quantitative membrane permeabilities were more readily available,
other cases could be considered, but this does not seem feasible at
A previous paper (1) described a preliminary mathe- present.
matical model for methotrexate pharmacokinetics in Many of the broad features described earlier (1) are valid follow-
mice. Since it was based on only one dose level, many of ing intravenous injection of methotrexate: (a) a very rapid drop
its conclusions were, necessarily, tentative. This paper in plasma concentration and an increase in gut-lumen concentration,
suggesting the importance of tissue uptake and biliary secretion :
describes much more extensive work at a variety of dose ( b ) a peak gut-lumen/plasma concentration ratio of about 100;and
levels with several species, including man. The same ( c ) linear binding of methotrexate by tissues at plasma concentra-
general rationale proposed in previous studies (1-3) is tions above 0.1 mcg./ml. At low concentration levels, the binding
utilized, namely, basing the model, as much as possible, became nonlinear (4), presumably because of the strong binding to
on established, independently verifiable, physiological dihydrofolate reductase.
The basic model, incorporating the important enterohepatic
concepts. It is important to emphasize this approach circulation, is shown in Fig. 1. The various symbols are defined in the
since, in this fashion, one can obtain pharmacokinetic
models that provide generally applicable a priori predic-
tions of drug distribution behavior. Specific details will
be given with the model description.
Cancer chemotherapeutic agents are usually screened
for activity against a limited number of tumor systems in
the mouse and rat. If their activity is sufficient to war-
rant further investigation, they are tested for toxicity in a
variety of animal species. Detailed information is
developed on quantitative and qualitative toxicology as n
well as the pharmacologic distribution and metabolic
fate. The most promising drugs are then evaluated
Gut Lumen
clinically in man.
The fundamental issues of drug toxicity include both QK
the physical aspects of drug distribution within the body -_---__
and drug effect at particular sites of action. Experience to KIDNEY
date indicates that the dynamics of drug distribution i n
the body can often be predicted on the basis of funda-
mental information on physicochemical properties,
transport, metabolism, and various excretory mecha-
nisms. The method is analogous to that used for “scale-
up” for a chemical plant where rational design can be
-----GI
I
Urine
----__
MUSCLE
- QM
based on laboratory data applied according to reason- Figure 1-Body compartments important in me,liotrexate distribri-
ably well-established techniques. Application of this fion.
1128 Journal of Pharmaceutical Sciences
ta Liver:
10
d
>
$I
E GL
2 where:
2c
4 L
a (Eq. 5 )
I- 1.0
2
W
0
Z Equation 5 defines the secretion rate (mcg./min.) of methotrexate
0 out of the liver cells into the bile ducts, and it allows for potential
0
w saturation effects (which were not observed at any dose levels
c studied).
4
::
K dr1
& 0.1 T -
dt
= r - r,
drz
r - = rl - r2
dt
0.01 I I I I I
0 60 120 180 240 Equations 6a-c are balanced directly on the secretion rate; the only
MINUTES
model parameter involved is the holding time, T . Three compart-
Figure 2-Model prediction versus experiinetituI results, mice, 3 ments are adequate to model separate experiments where the bile
mg.lkg. i.v. Solid lines are model predictions; symbols are experi- duct is cannulated and the bile concentration of methotrexate is
mentaldata. Key: GL(O), small brtestiiie; L(A), livzr; K(O), kidney; directly measured.
P (O), plasma; and M (V),muscle.
Gut tissue:
Nomencluture section. Two rather unique features need to be
described in more detail-the “multicompartment” models used for
the biliary secretion process and for the gut lumen. In the previous
study (I), a mathematical time-delay or step function was used to
simulate the bile formation and secretion time in the liver. In other
words, a period of about 5 min. (in mice) was allowed before the
drug in the bile was introduced into the gut lumen. This abrupt 1000
introduction caused this portion of the gut-lumen-predicted curve to
overshoot the actual data, and a smoother representation of the real
“S-shaped” bile concentration efflux curve was desired. A finite
series of discrete compartments is able to d o this, as is commonly
done in chemical engineering for similar situations (5). A more ex-
tensive description and test of this scheme to represent bile function oi,
>
are given elsewhere (6),and it was found materially to improve the 3 100
present model predictions. E
The transit of drug down the gut is handled similarly, except that i
provision for transport through the intestinal wall is made. This 0
concept, rather than a single compartment with time delay, is used
again to provide a smooth response. Also, rather than a well-mixed
uniform region, the tubular nature of the gut lumen must be
accounted for to simulate the proper concentration appearing in the
feces. This is done by having the feces “exit” from the last gut-lumen
region. The rigorous details of properly accounting for binding, etc.,
were given previously (1). The complete set of mass balance equa-
tions for the various anatomical body regions can be written as
follows.
Plasmu:
(QL + + QMWP(Eq. 1)
QK
Muscle:
t
0 60 120 180 240
Kidney : MINUTES
Figure 3-Model prediction versus experimental results, mice. Empty
dCe
(
V K - = Q K CP
dt
- R,‘,) - kK -
C K
RK
(Eq. 3) symbols are 3 rng./kg.; solid symbols are 300 mg.lkg. i.u. See Fig. 2
for symbol key.
Vol. 60, No. 8, August 1971 01129
Table I-Model Parameters for Methotrexate in Several Species
Parameter Mouse Rat 5 kg., Dog/Monkey 17 kg., Dog Man
Body weight, g.” 22 200 5000 17,000 70,000
Volume, ml.“
VP 1.0 9.0 220 650 3,000
VM 10.0 100 2500 7,500 35,000
VK 0.34 1.9 30 76 280
VL 1.3 8.3 135 360 1,350
V
. -d 1.5 11.0 230 640 2,100
VGL‘ 1.5 11.0 230 640 2,100
Plasma flow rate, ml./min.b
QM 0.5 3.0 50 140 420
QK 0.8 5.0 74 190 700
QL 1.1 6.5 92 220 800
QQ 0.9 5.3 75 190 700
Tissue/plasma equilibrium
distribution ratio for
linear bindingdse
RW._ 0.15 0.15 (0. 5) (0.15)
RK 3.0 3.0 (14) 14 (3.0)
RL 10 3.0 (2.0) 2.0 (3.0)
RQ 1.0 (1.0) (1.O) (1 .O) (1.0)
Strong specific bindinge
aM 0.0 0 (0) (0) (0)
aK 0.3 0.3 (0.3) (0.3) (0.3)
aL 0.3 0.5 (0.4) (0.4) (0.4)
ao 0.1 (0.1) (0.1) (0.1) (0.1)
Kidney clearance, ml./min.d*e
kK 0.2 1.1 (20) 56 1901
Bile secretion parametersd*6
Clearance = kL,/KL,
m1.lmin.p 0.4 3.0 (2.0) 8 2w
7, mn. 2.0 2.0 (6) 8.0 (10)
Gut-lumen parameetrs’
Transit time, min. 100 100” (450) (650) (1 ,000)
Reciprocal = kp, min.-’ 0.01 0.01 (0.0022) (0.0015 ) (0.001)
ko, mcg./min. 0.20 (20) (340) (1,ooQ (1,900)
KO,rncg../ml. 6.0 (200) (200) (200) (200)
b, ml./mn. 0.001 - - - -
a “Standard” values (average). * Based on physiological information; see Appendix. c Gut and gut-lumen volumes not independently measured,
i.e., gut-lumen “concentrations” are effective values. d Measured experimentally; see text. e Values in parentheses are estimates. J Liegler et al. (15).
u Only the ratio k L / K L is needed, since no saturation was observed; so KL is very large. * Conjectural value to create best fit to data. * Compare Sikov
et al. (16).
100 ti Gut lumen:
dCcL 1 dCi
0
- -
dt - ; EI x
a=
.
d
g 10
E
i
II
I-
dc (= + Ci + bCi)
4 KG
(i = 2,3,4) (Eq. 8c)
2
W
p 1.0 In Eqs. 7 and 8, the last terms represent gut absorption from the
0 lumen to the tissue (and blood flow), with the possibility of both
0
w +
saturable [ ( ~ G C J K G CJ] and nonsaturable (bCi) effects. Both
I- effects may be important for folic acid (7, 8) and, therefore, may
a apply to methotrexate, since both substrates were reported to use the
5K 0
-r
same transport system (9). The four regions are judged sufficient to
I-
0 model the gut-lumen response. The absorption characteristics are
I assumed the same for all segments because of a lack of more detailed
$ 0.1
information; other complications, such as location-dependent
9
absorption, could be accounted for. Upon substitution of suitable
numerical values for the various parameters, these equations can be
0
solved by a computer.
PARAMETER VALUES
0.71 I I I I I Many of the parameters for mice, as given earlier (l), are retained
0 60 120 180 240
MINUTES
here, except for the case of the zero-order gut absorption. This was
reasonable for the one dose of 3 mg./kg., but the simulation was
Figure &Model prediction versus experimental results, rats, 6 mg.1 inadequate for a wider range of dose levels. The justification for the
kg. i.p. See Fig. 2for symbol key. assumption of zero-order absorption (1) was the apparent leveling of
1130 0Journal of Pharmaceutical Sciences
10
d
>
3
E
i
2
i- 1.0
2-
2
10 8F
I- z
W
4
a 0
z
I-
Z 0
W 0
0 W
z I-
8 1.0 4
1: 0.1
W
I- K
a
1a: GI
I- Lz
0.01
0 90 180 270 360
MINUTES
Figure I-Man, I mg./kg. i.0. Dark and clear symbols are results of
0.01 I I I I Q two separate experiments. See Fig. 2 for symbol key (12).
0 60 120 180 240
MINUTES kidney clearance is close to inulin, it is specifically determined for
Figure 5-Model prediction versus experimental results, rats. Empty methotrexate by comparing the time integral of the plasma concen-
symbols are 0.5 mg./kg.; solid symbols are 25 mg./kg. i.p. See Fig. 2 tration with cumulative urine formation after intraperitoneal or
f o r symbol key. intravenous injections of the drug. The tissue/plasma equilibrium
ratios are derived by some constant-infusion experiments and/or the
portion of the intravenous pulse injection curve after the initial
the plasma concentration after 2-3 hr. However, since it was found redistribution. For high concentrations, they are constants, indicat-
(10) that significant intestinal nietabolism eventually occurs, the ing linear binding; for low concentrations, they are given by the sum
reliability of the measured radioactivity at these longer times is ques- of this linear nonspecific binding (RCp) and strong binding (a),
tionable. Strong binding to dihydrofolate reductase is also a com- presumed to be associated with dihydrofolate reductase, according
plication. Thus, even though a definitive model for gut absorption is to:
still not available, it is apparently not readily saturable. Therefore,
the model accounts for both saturable and nonsaturable absorption
in Eqs. 7 and 8.
The simple physiological parameters of organ volumes and flows
for other animal species are detailed in the Appendix. Although the The magnitude of c may be estimated from the work of Werkheiser
(ll), who found that the dissociation constant of the enzyme-drug
complex is less than 1.5 X 10-lo Mfor a noncompetitive inhibitor or
1.0
d
3 d
E" >
3
2 E
2 i
2K 10 2
t I- 0.1
50 8I-
z z
W
8 0
0
z
W
t 0
6 W
I-
1a: 1.0 U
i- g 0.01
0 E
I I-
0
kIi I
b
5
...
0.1 II I I I I
0 60 120 180 240 . 0.001
MINUTES 0 60 120 180 240
MINUTES
Figure 6- Model prediction versus experimental results. Two ex-
periments, dogs, 3 mg./kg. i.u., represented by empty and solid sym- Figure I-Model prediction versus experimental results, mice, 0.12
bols. See Fig. 2 for symbol key. mg./kg. See Fig. 2 for symbol key.
Vol. 60, No. 8, August 1971 01131
less than 3 x lo-" M for a competitive inhibitor. Thus, t is of the d
order of 1 0 - 5 mcg./ml. or less. At the plasma concentrations studied,
therefore, the binding to dihydrofolate reductase may be considered
stoichiometric.
For high values of Cp, the second term in Eq. 9 is much smaller
than the first, since a is much less than RCp and t is very much less
than CP.Thus, RCp dominates, and the binding may be considered
linear. For small values of CP, however, the second term in Eq. 9
becomes important.
The bile clearance is determined by separate experiments, except
where indicated, and the complete set of parameter values used in
the simulations to be described is given in Table I.
$1
4 10
SIMULATIONS AND COMPARISONS WITH DATA
The model parameters in Table I are used in Eqs. 1-9 for simula-
q r"
0
tions of various dose levels and animal species. The values presented
in Table I were used for afl dose levels so that the model would
GG 1.0
0.01 0.1 1.0 10.0 100.0
achieve real physiological meaning. BODY WEIGHT, kg.
Figure 2 compares the model results in several body regions
with experimental data for 3 mg./kg. in the mouse. The results Figure Al-Retial plusmaflow rate. Data sources: 0, Reference 20, p.
are in good agreement, similar to those reported earlier (1) for the 127; atid A, 0 , Reference 21, p. 1483,
preliminary model, except for a better gut-lumen simulation ;
also, the curves do not level out. Figure 3 gives the results for two The same model is used for the mouse, rat, dog, and human, with
high doses, 3.0 and 300 mg./kg. Other tissues are not presented specific parameters chosen for the species to be simulated. The
in order to simplify the figure; however, they were also predictable model predicts tissue concentrations in the subhuman species and
and followed the same time course as plasma (Fig. 2). also predicts observed plasma concentrations and urinary and fecal
The same types of results are given for rats in Figs. 4 and 5, excretion in man.
showing fair agreement. Although the trend of the gut-lumen
concentration is predictable, there is more variability in the data NOMENCLATURE
obtained at the low dose. Figure 6 illustrates the comparisons for a
small amount of dog data, and the results are reasonably good. a = strong specific binding, mcg./g.
Finally, Fig. 7 compares the plasma results for man with model h = rateconstant for nonsaturable gut absorption, ml./min.
predictions and also gives predicted values for the other body re- C = drug concentration, mcg./g. or mcg./ml.
gions. The prediction of 57% of the total dose in the urine at 4 hr. Af) = injection function, rnim-1
may be compared with the observed value range of 38-75z ob- kp. = reciprocal of nominal transit time in small intestine,
served by Henderson er al. (12) at the same dose level; corresponding min.-'
values for 24 hr. are: predicted, 87%; and observed, 75-88z. Based kc = saturable rate of intestinal absorption, mcg./min.
on these illustrations, the model does a reasonable job of predicting kK = clearance by kidney, ml./min.
the methotrexate distribution for all the species at the fairly high k I, = saturable rate of drug transport into bile, mcg./min.,
dose levels ( 2 1 mg./kg.). More extensive specific clinicalexperiments Eq. 5
would be useful for more confidence in the parameter values for K = constant of Michaelis form for intestinal absorption
man. or bile formation, mcg./ml.
The case of very low doses is of interest here because it illustrates M = amount of drug, mcg.
the effect of the nonlinear strong binding in Eq. 9. The kinetics of Q = plasma flow rate, ml./min.
distribution in various body tissues are also of practical importance r = drug-transport rate in bile, mcg./min.
to dermatologists, since such low doses are used to treat psoriasis R = tissue-to-plasma equilibrium distribution ratio for
(13). Figure 8 shows the predicted and measured tissue concentra- linear binding, dimensionless
tions following an intravenous dose of 0.12 mg./kg. in the mouse. R' = variable tissue-to-plasma equilibrium distribution
Comparison with Fig. 2 (3 mg./kg.) shows clearly the effect of the ratio including effect of strong specific binding
strong binding in the liver and kidney at the low dose. The plasma f = time, min.
concentration falls rapidly in very short times, while a large fraction V = volume of compartment, ml.
of the dose is bound to these tissues. As the plasma concentration W = body weight, kg.
continues falling, the concentrations in the liver and kidney remain t = dissociation constant of enzyme-inhibitor complex,
high. As suggested by Werkheiser ( 1 l), other dihydrofolate re- mcg./ml., Eq. 9
ductase-containing tissues no doubt behave in a similar manner. 7 = nominal residence time in bile subcompartment, min.
There is evidence that dihydrofolate reductase inhibitors exhibit Subscripts
strong saturable binding in human liver, kidney, and small intzstine G = gastrointestinal tract
which persists for days but which can be dissxiated by a high dcse GL = gut lumen
of nonlabeled drug (14). K = kidney
L = liver
CONCLUSIONS M = muscle
P = plasma
A mathematical model is presented which predicts detailed dis- tissue = G, K, L, or M
tribution of methotrexate in the tissues of several mammalian I , 2, . , . = bile or gut-lumen sulxompartments
species. It is based on anatomical compartments and intercom-
partment flow transport. Tissue-to-plasma distribution coefficients APPENDIX
include provision for strong binding to dihydrofolate reductase. The
drug is cleared from the plasma by the kidney and excreted in the This section briefly summarizes the literature data used for the
bile, with subsequent partial intestinal reabsorption. At present, the physiological values of organ volumes and flows.
greatest uncertainty is in the exact kinetics to describe intestinal The volumes are essentialIy taken from the correlations of Adolph
absorption in the intact animal. The model contains multicompart- (17) an3 spot-checked with some of the authors' own organ weight
ment descriptions of the biliary system and the intestine based on data and that of Mapleson (18) and Crile and Quiring (19). Adolph
physiologic principles. Phenomena, such as local differences in (17) gives (VB1)Adolph = 0.055 (1000W)0.99,where the volume is in
intestinal absorption, could be incorporated if sufficient data were milliliters (grams for density of 1.0 g./ml.) and the body weight, W ,
available. is in kilograms. For a standard man of 70 kg., (VB1)Adolph = 3503.
1132 0Journal of Phar~:aceuticalSrirtices
With regard to flows, Fig. A1 shows data on renal plasma flow
rate as a function of body weight on log-log paper to illustrate re-
lationships in the form used by Adolph (17). The line is arbitrarily
drawn through the data; it is also bracketed by Adolph‘s relations
of para-aminohippuric acid and iodopyracet 1 clearances and
should be reliable.
Figure A2 presents hepatic plasma flow rate. The data here are
more scattered, but a reasonably good general estimate is evident.
Limited available information on muscle perfusion rate is shown in
Fig. A3. Much less data were readily available for the gut flow
rate, and they were,all for large animals. Based on these, a rough
estimate of 0.84.85, or 0.82, of the hepatic flow rate was used
(Reference20, p. 1443; Reference 22, p. 244).
In the calculation of the flow rates for Figs. Al-A3, total plasma
flow rates to the three compartments are calculated, as required, on
the basis of a hematocrit of 0.40 and organ weight-to-body weight
relationships.
G
1.or
0.01
.
LIlJ
o
0.1
I I ” ’ t 1 1 1
1.0
‘ ‘ ‘ 1 1 1 1 1 1
10.0
‘ ‘ ‘ “ I t L L
100.0 REFERENCES
BODY WEIGHT, kg.
Figure A2-Hepatic plasma flow rate. Data sources: 0, Reference (1) K. B. Bischoff, R. L. Dedrick, and D. S. Zaharko, J. Pharm.
20, pp. 128, 129; x, Reference 22, p. 244; 0,Reference 21, p. 641; Sci., 59, 149(1970).
and A, Reference 21, p. 1405. (2) R. L. Dedrick and K. B. Bischoff, Chem. Eng. Progr. Symp.,
Ser.’ 84,64, 32(1968).
(3) K. B. Bischoff and R. L. Dedrick, J. Pharm. Sci., 57, 1346
This seemed too small compared to the more common 5000 ml., so (1968).
the final equation used is adjusted by the ratio 5000/3500. For an (4) D. S. Zaharko, R. L. Dedrick, and V. T. Oliverio, Fed.
average hematocrit of 40%, then: Proc., 29, 41 1( 1970).
( 5 ) D. M. Himmelblau and K. B. Bischoff, “Process Analysis
Vp = (0.6) (5000/3500) (0.055) (1000W>O.Q9 and Simulation,” Wiley, New York, N.Y., 1968.
- 44wo.99 (Eq. A l ) (6) K. B. Bischoff, R. L. Dedrick, D. S. Zaharko, and S. Slater,
Proc. Ann. Conf: Eng. Med. Biol., 12, 89(1970).
At the other end of the scale, V p for a 22-g. mouse ( W = 0.022) (7) G. W. Hepner, Brit. J. Haematol., 16, 241(1969).
is then 1 ml., which is the value used in the previous work (1). (8) A. S. V. Burgen and N. J. Goldberg, Brit. J. Pharmacol., 19,
The other relations are: 31 3( 1962).
(9) I. D. Goldman, N. S. Lichtenstein, and V. T. Oliverio,
V L = 0.082(1000w)0~87
= 34W0.” (Eq. A21 J. Biol. Chem., 243, 5007(1968).
VK = 0 . 0 2 1 2 ( 1 0 0 0 ~ ) ~=
~ *75. 5 ~ 0 . 8 5 (Eq. A3) (10) D. S. Zaharko, H. Bruckner, and V. T. Oliverio, Science,
166, 887(1969).
VM =% ~/z(lOOoW)= 500w (Eq. A4) (11) W. C. Werkheiser, J. Biol. Chem., 236, 888(1961).
(12) E. S. Henderson, R. H. Adamson, and V. T. Oherio,
Adolph (17) gave the stomach and intestine weight as 0.112 Cancer Res., 25, 1018(1965).
(1000W)O.94.Since the present model considers the small intestine (13) C. J. McDonald and J. R. Bertino, Lancet, 1,8640968).
only as the participating organ, two-thirds of the weight was used: (14) D. G. Johns, R. P. Spencer, P. K. Chang, and J. R. Bertino,
Va = ~ / ~ ( 0 . 1 1 2 ) ( 1 ~ w ) o ~ g 4 J. Nucl. Med., 9, 53q1968).
(15) D. G. Liegler, E. S. Henderson, M. A. Hahn, and V. T.
= 49p.94 (Eq. A5) Oliverio, Clin. Pharmacol. Ther., 10, 849(1969).
(16) M. R. Sikov, J. M. Thomas, and D. D. Mahlum, Growth, 33,
These obviously somewhat arbitrary relations correspond reason- 57( 1969).
ably well with commonly accepted values. It was found in previous (17) E. F.Adolph, Science, 109,579(1949).
work that consistency of values for the organ volumes is more im- (18) W. W. Mapleson, J. Appl. Physiol., 18, 197(1963).
portant than absolute accuracy, which is the reason for devising the (19) G. Crile and D. P. Quiring, Ohio J. Sci., 40,219(1940).
general equations. (20) “Handbook of Circulation,” P. L. Altman, D. S. Dittmer,
and R. M. Grebe, Eds., Saunders, Philadelphia, Pa., 1959.
(21) “Handbook of Physiology,” W. F. Hamilton and P. Dow,
Eds., American Physiological Society, Washington, D. C., 1962,
sect. 2.
(22) “Medical Physics,” vol. 11, 0. Glasser, Ed., Year Book
Publishers, Chicago, Ill., 1950.
(23) T. T. Vogel, Curdiologia, 53, 19(1968).
(24) R. F. Edlich, J. Borner, and R. J. Buchin, Arch. Surg., 98,
233(1969).
ACKNOWLEDGMENTS AND ADDRESSES
Received February 16, 1971, from the *Biomedical Engineering
and Instrumentation Branch, Division of Research Services, and
?Laboratory of Chemical Pharmacology, National Cancer Institute,
National Institutes of Health, Public Health Service, U, S. Depart-
ment of Health, Education, and Welfare, Bethesda, M D 20014
5 / Accepted for publication March 15, 1971.
$ Present address: School of Chemical Engineering, Cornell
University, Ithaca, NY 14850
1 Diodrast.
Vol. 60, No. 8, August 1971 01133
You might also like
- A Winning SBIR From 2002 StudentDocument18 pagesA Winning SBIR From 2002 StudentJennifer Holman100% (3)
- Robotic-Assisted Minimally Invasive Surgery - A Comprehensive Textbook (Tsuda S.)Document331 pagesRobotic-Assisted Minimally Invasive Surgery - A Comprehensive Textbook (Tsuda S.)alvcardx100% (3)
- Csa Book MRCGP Csa Cases MRCGP CourseDocument22 pagesCsa Book MRCGP Csa Cases MRCGP CourseEshtiag43% (7)
- Occupational Therapy's Role in Managing ArthritisDocument2 pagesOccupational Therapy's Role in Managing ArthritisThe American Occupational Therapy AssociationNo ratings yet
- Non Compartmental PharmacokineticsDocument72 pagesNon Compartmental PharmacokineticsJaspreet Guraya90% (10)
- Dermatology Finals (Sept. 2014)Document14 pagesDermatology Finals (Sept. 2014)Paz VidaNo ratings yet
- Drug Metabolism and PharmacokineticsDocument48 pagesDrug Metabolism and PharmacokineticsYunistya Dwi CahyaniNo ratings yet
- Modifikasi Formula Enteral Rumah Sakit Siap SeduhDocument8 pagesModifikasi Formula Enteral Rumah Sakit Siap SeduhAsfi Ni'amNo ratings yet
- Mathematical Models for Drug Diffusion Through CompartmentsDocument5 pagesMathematical Models for Drug Diffusion Through CompartmentsbloosomeNo ratings yet
- Matrix Method for Determining Most Rate-Limiting StepsDocument7 pagesMatrix Method for Determining Most Rate-Limiting StepsclapatriciasaNo ratings yet
- Mathematical Models for Drug Diffusion Through Blood and TissueDocument5 pagesMathematical Models for Drug Diffusion Through Blood and TissueJuan Andres Bueno HortuaNo ratings yet
- Valentine2005 Developing Liquid Chromatography Ion Mobility Mass Spectometry TechniquesDocument13 pagesValentine2005 Developing Liquid Chromatography Ion Mobility Mass Spectometry TechniquesSoraya OchsNo ratings yet
- Pharmacokinetics of Drugs Following IV Bolus, IV Infusion, and Oral AdministrationDocument46 pagesPharmacokinetics of Drugs Following IV Bolus, IV Infusion, and Oral AdministrationMalalaFernándezNo ratings yet
- Pascua Maestro2018Document8 pagesPascua Maestro2018dayse marquesNo ratings yet
- García Aparicio Carlos Diffusion of Small Molecules 2012Document7 pagesGarcía Aparicio Carlos Diffusion of Small Molecules 2012FranciscoNo ratings yet
- Polymer Controlled Drug DeliveryDocument6 pagesPolymer Controlled Drug DeliveryrajadcetNo ratings yet
- Application Percolation Theory To Characterize The Release Behavior Carteolol Matrix SystemsDocument8 pagesApplication Percolation Theory To Characterize The Release Behavior Carteolol Matrix SystemsSuneel PandeyNo ratings yet
- Pharmacokinetic ModelsDocument36 pagesPharmacokinetic ModelsInnocent MwilaNo ratings yet
- CR SRDocument8 pagesCR SRADVOCATE ASHUTOSH SHARMANo ratings yet
- Mathematical Models of Drug Dissolution PDFDocument9 pagesMathematical Models of Drug Dissolution PDFClaudia GarcíaNo ratings yet
- Qsar and Drug DesignDocument65 pagesQsar and Drug Design16_dev5038No ratings yet
- Metabolomics: Topics in Chemical Biology: Advanced ArticleDocument10 pagesMetabolomics: Topics in Chemical Biology: Advanced ArticleazzaassNo ratings yet
- Pharmacokinetics Model SignificanceDocument12 pagesPharmacokinetics Model Significancevai amiNo ratings yet
- Iontophoretic Transdermal Drug Delivery: A Multi-Layered ApproachDocument19 pagesIontophoretic Transdermal Drug Delivery: A Multi-Layered ApproachMohamad Aprianto PaneoNo ratings yet
- 2023 Binding PropertiesDocument47 pages2023 Binding PropertiesМихаил ГородковNo ratings yet
- Stoic Hi o Metric Modelling of Cell MetabolismDocument11 pagesStoic Hi o Metric Modelling of Cell MetabolismFernanda PerezNo ratings yet
- Article 321548Document8 pagesArticle 321548Altair FonsecaNo ratings yet
- J. Biol. Chem.-2011-Witney-24572-80Document9 pagesJ. Biol. Chem.-2011-Witney-24572-80Joy BorowitzNo ratings yet
- Adobe Scan Feb 13, 2023Document10 pagesAdobe Scan Feb 13, 2023Indra KumarNo ratings yet
- Drug Release Kinetics ModelsDocument7 pagesDrug Release Kinetics ModelsSajid Khan SadozaiNo ratings yet
- Differences between compartment and non-compartment PK modelsDocument5 pagesDifferences between compartment and non-compartment PK modelsIlyax KahnNo ratings yet
- Compartmental ModelDocument5 pagesCompartmental ModelIlyax KahnNo ratings yet
- (Technology Brief) : DESI-Mass Spectrometry Imaging Investigation of Discrete and Cassette Drug Dosed TissuesDocument3 pages(Technology Brief) : DESI-Mass Spectrometry Imaging Investigation of Discrete and Cassette Drug Dosed TissuesLuis Alberto AnguianoNo ratings yet
- Chapter Summary: (Hours) (G/ML)Document2 pagesChapter Summary: (Hours) (G/ML)Marco Aurelio Santander MartinezNo ratings yet
- Tipos de CineticasDocument10 pagesTipos de CineticasPedro Rivas TorresNo ratings yet
- E 1280 - 97 R03 RteyodaDocument9 pagesE 1280 - 97 R03 RteyodaFreddy MoncayoNo ratings yet
- Physiologic Pharmacokinetic ModelDocument20 pagesPhysiologic Pharmacokinetic ModelKamrun Nesa100% (1)
- Methods and Advances in Metabolic Flux Analysis: A Mini ReviewDocument9 pagesMethods and Advances in Metabolic Flux Analysis: A Mini ReviewAmal ..No ratings yet
- A Computational Procedure For Determining Energetically Favorable Binding Sites On Biologically Important MacromoleculesDocument9 pagesA Computational Procedure For Determining Energetically Favorable Binding Sites On Biologically Important Macromoleculeskundaningale007No ratings yet
- Biomaterials in Drug Delivery (Lowman - 2004)Document31 pagesBiomaterials in Drug Delivery (Lowman - 2004)lejartkNo ratings yet
- Compartmental Modeling in The Analysis of Biological SystemsDocument49 pagesCompartmental Modeling in The Analysis of Biological Systemsdilka dariyaNo ratings yet
- Computational Biology and Chemistry: Tikam Chand Dakal, Rajender Kumar, Dindial RamotarDocument11 pagesComputational Biology and Chemistry: Tikam Chand Dakal, Rajender Kumar, Dindial RamotarMATIAS MARAMBIO SOTONo ratings yet
- Metabolic Control Theory: Its Role in Microbiology and BiotechnologyDocument16 pagesMetabolic Control Theory: Its Role in Microbiology and BiotechnologyEstalin CaizapantaNo ratings yet
- Mechanism of Action of Methotrexate in Rheumatoid Arthritis, and The Search For BiomarkersDocument12 pagesMechanism of Action of Methotrexate in Rheumatoid Arthritis, and The Search For BiomarkersFaMe TanapornNo ratings yet
- A Theoretical Physiologically-Based Pharmacokinetic Approach To Ascertain Covariates Explaining The Large Interpatient Variability in Tacrolimus DispositionDocument12 pagesA Theoretical Physiologically-Based Pharmacokinetic Approach To Ascertain Covariates Explaining The Large Interpatient Variability in Tacrolimus Disposition陈梓强No ratings yet
- Cellpenetrating Peptides As A Novel Transdermal Drug Delivery SystemDocument8 pagesCellpenetrating Peptides As A Novel Transdermal Drug Delivery SystemHinal AmbasanaNo ratings yet
- ASTM MedicalDocument9 pagesASTM MedicalSubidorDeLibrosNo ratings yet
- 2006 Consensus Agreement On The Design and Conduct of Clinical Studies With Low-Level Laser Therapy and Light Therapy For Musculoskeletal Pain and DisordersDocument2 pages2006 Consensus Agreement On The Design and Conduct of Clinical Studies With Low-Level Laser Therapy and Light Therapy For Musculoskeletal Pain and DisordersDetian WangNo ratings yet
- JCC Dop 43 1298 2022Document15 pagesJCC Dop 43 1298 2022Natalia ZaryczNo ratings yet
- Erosion Release ControlDocument8 pagesErosion Release ControlADVOCATE ASHUTOSH SHARMANo ratings yet
- Compartmental & Non-Compartmental PharmacokineticsDocument21 pagesCompartmental & Non-Compartmental PharmacokineticsVikas JhawatNo ratings yet
- Tolerancia y Dependencia de DrogasDocument10 pagesTolerancia y Dependencia de DrogasLopez LionelNo ratings yet
- Multicompartmentivbolus GoodDocument41 pagesMulticompartmentivbolus Gooduday sainiNo ratings yet
- Lee2017 Article GeneralizedPlasmaSkimmingModelDocument11 pagesLee2017 Article GeneralizedPlasmaSkimmingModelovyNo ratings yet
- Noncompartmental PK AnalysisDocument30 pagesNoncompartmental PK AnalysisNair RahulNo ratings yet
- Sem Dial 2021 CRRT PrinciplesDocument8 pagesSem Dial 2021 CRRT PrinciplesArun KumarNo ratings yet
- A Targeted MetabolomicsDocument24 pagesA Targeted MetabolomicsnandareginaldoNo ratings yet
- Nanotechnological Approaches For The Delivery of MacromoleculesDocument8 pagesNanotechnological Approaches For The Delivery of MacromoleculesAnida Maria Moraes GomesNo ratings yet
- CHAPTER 2 Pharmacologic PrinciplesDocument59 pagesCHAPTER 2 Pharmacologic PrinciplesASLY LUCIANA MARQUEZ GALLARDONo ratings yet
- Computational Methods For Prediction of Drug LikenessDocument10 pagesComputational Methods For Prediction of Drug LikenesssciencystuffNo ratings yet
- The Tape-Stripping Technique As A Method For Drug Quantification in SkinDocument27 pagesThe Tape-Stripping Technique As A Method For Drug Quantification in SkinfelinsiamelvanNo ratings yet
- Structural Characterization of p53 Protein Using Raman SpectroscopyDocument10 pagesStructural Characterization of p53 Protein Using Raman SpectroscopyWilson Agudelo CatañoNo ratings yet
- Chemistry Methods - 2020 - Cau T - Conceptual and Computational DFT Based in Silico Fragmentation Method For TheDocument15 pagesChemistry Methods - 2020 - Cau T - Conceptual and Computational DFT Based in Silico Fragmentation Method For TheJessicaNo ratings yet
- Granular Materials at Meso-scale: Towards a Change of Scale ApproachFrom EverandGranular Materials at Meso-scale: Towards a Change of Scale ApproachNo ratings yet
- Metabolite Safety in Drug DevelopmentFrom EverandMetabolite Safety in Drug DevelopmentSuzanne L. IversonNo ratings yet
- Understanding The Mechanisms of Action of MethotrexateDocument6 pagesUnderstanding The Mechanisms of Action of MethotrexateMuhamad Rizqy MaulanaNo ratings yet
- I Cant Help Falling in Love With You 28406 1535202387 K15 Us LetterDocument1 pageI Cant Help Falling in Love With You 28406 1535202387 K15 Us LetterMuhamad Rizqy MaulanaNo ratings yet
- IPv4 and IPv6 localhost addresses and free countersDocument811 pagesIPv4 and IPv6 localhost addresses and free countersDam JamNo ratings yet
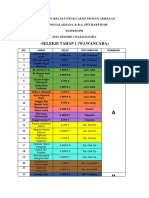
- Seleksi Tahap 1 (Wawancara)Document2 pagesSeleksi Tahap 1 (Wawancara)Muhamad Rizqy MaulanaNo ratings yet
- FAQs on Rabies: Causes, Symptoms, PreventionDocument4 pagesFAQs on Rabies: Causes, Symptoms, PreventionRonn BautistaNo ratings yet
- Dichotomous Key SampleDocument1 pageDichotomous Key SampleGerald ShouNo ratings yet
- Lymphatic System and Immunity: Student Learning OutcomesDocument8 pagesLymphatic System and Immunity: Student Learning Outcomeslily1liang-1No ratings yet
- PosterDocument1 pagePosterChetanNo ratings yet
- MCQ HTNDocument18 pagesMCQ HTNmohamed mowafeyNo ratings yet
- Spot The Difference: 1 This Diagram Shows The Male Reproductive SystemDocument3 pagesSpot The Difference: 1 This Diagram Shows The Male Reproductive SystemPedroDavid JoaquinFernandoNo ratings yet
- GERD SchwartzDocument10 pagesGERD SchwartzMina Tharwat AzerNo ratings yet
- AMBU Mark IV e Mark IV Baby Partes e AcessoriosDocument1 pageAMBU Mark IV e Mark IV Baby Partes e AcessoriosNícolasNo ratings yet
- Preparing For A Glucose Tolerance TestDocument3 pagesPreparing For A Glucose Tolerance Testconnect.rohit85No ratings yet
- Kursus Pementoran Dalam KejururawatanDocument40 pagesKursus Pementoran Dalam KejururawatanNajlaa RaihanaNo ratings yet
- Acute Gastroenteritis Individual TaskDocument5 pagesAcute Gastroenteritis Individual TaskMaria Lourdes ManganarNo ratings yet
- PSUR RedactionDocument28 pagesPSUR RedactionЗухра ИбрагимоваNo ratings yet
- Family Planning Semester VDocument82 pagesFamily Planning Semester Vduaabdullah33No ratings yet
- Increased Intracranial Pressure STUDENT Lewis 10th Ed Chapter - 056 - 2Document75 pagesIncreased Intracranial Pressure STUDENT Lewis 10th Ed Chapter - 056 - 2Marie Joy MadambaNo ratings yet
- Terapi Cairan Dalam Praktek Sehari-Hari Oleh DR - Sumara Niman, SP - AnDocument49 pagesTerapi Cairan Dalam Praktek Sehari-Hari Oleh DR - Sumara Niman, SP - AnRiony GusbaniansyahNo ratings yet
- A Case Study On Urinalysis and Body FluidsDocument17 pagesA Case Study On Urinalysis and Body Fluidsrakish16No ratings yet
- Central Post-Stroke Pain - Clinical Characteristics, Pathophysiology, and ManagementDocument12 pagesCentral Post-Stroke Pain - Clinical Characteristics, Pathophysiology, and ManagementKarimah Ihda Husna YainNo ratings yet
- Paper 3 Argumentative Essay Alexis-2Document9 pagesPaper 3 Argumentative Essay Alexis-2api-314832012No ratings yet
- Biosimilar Insulin GlargineDocument59 pagesBiosimilar Insulin GlarginenellizulfiaNo ratings yet
- Learning TaskDocument4 pagesLearning TaskAngelica GuillermoNo ratings yet
- Gloves, gown, mask, eye protection as needed based on anticipated exposureDocument46 pagesGloves, gown, mask, eye protection as needed based on anticipated exposureJayrelle D. SafranNo ratings yet
- Proposal of MulumebetDocument40 pagesProposal of MulumebetMulumebet EshetuNo ratings yet
- Subject Final FSDocument42 pagesSubject Final FSbangladeshusembassyNo ratings yet
- Em Form NktiDocument7 pagesEm Form NktiJerico Wendell Gee RubioNo ratings yet
- Hipo HiperthyroidDocument49 pagesHipo HiperthyroidMuhammad Bilal Bin AmirNo ratings yet