100% found this document useful (1 vote)
1K views19 pagesSeminar On: Benign Prostatic Hyperplasia
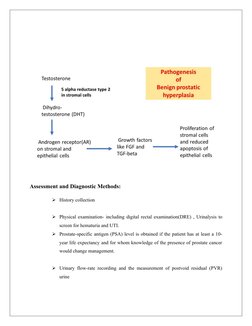
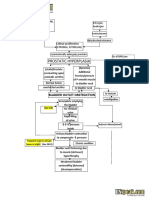
The document discusses benign prostatic hyperplasia (BPH), a common condition where the prostate gland enlarges in older men. It covers the definition, causes, risk factors, clinical manifestations, and pathophysiology of BPH. Specifically, it notes that BPH involves hyperplasia of prostate cells, often obstructing urine flow. Risk factors include aging, family history, ethnicity, and certain lifestyle factors. Common symptoms are lower urinary tract symptoms like frequent urination and weak urine stream. The pathophysiology involves hormonal changes in aging men that promote prostate cell growth.
Uploaded by
Honey PrasadCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
100% found this document useful (1 vote)
1K views19 pagesSeminar On: Benign Prostatic Hyperplasia
The document discusses benign prostatic hyperplasia (BPH), a common condition where the prostate gland enlarges in older men. It covers the definition, causes, risk factors, clinical manifestations, and pathophysiology of BPH. Specifically, it notes that BPH involves hyperplasia of prostate cells, often obstructing urine flow. Risk factors include aging, family history, ethnicity, and certain lifestyle factors. Common symptoms are lower urinary tract symptoms like frequent urination and weak urine stream. The pathophysiology involves hormonal changes in aging men that promote prostate cell growth.
Uploaded by
Honey PrasadCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd