Professional Documents
Culture Documents
Official Lecture on Health Systems Goals
Uploaded by
LYKA ANTONETTE ABREGANAOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Official Lecture on Health Systems Goals
Uploaded by
LYKA ANTONETTE ABREGANACopyright:
Available Formats
Official Lecture#2: Health Systems
Saturday, 20 August 2022 11:31 AM
HIS Lec
1ST SEMESTER DISCUSSION NOTES
--------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------
Health System
- The combination of resources, organization, financing, & management that culminate in the delivery of health services to the population (Roemer, 1991).
In the World Health Report (WHO, 2000), a health system is defined as "all the organizations, institutions, resources, & people whose primary purpose is to improve
health."―thus, a well-performing health system provides direct health-improving activities whether in personal health care, public health services, or intersectoral
initiatives in order to achieve high health equity.
→ In the quest for "improving health", it refers to the general population (does not select
nor divide the population into those worthy of receiving health services).
- The overall goal of each health system is to: Achieve high health equity.
- Components of a health system include:
► Community
► Department or ministries of health
► Health care providers
► Health service organizations
► Pharmaceutical companies
► Health financing bodies
► Other organizations related to the health sector
- Each plays a role in the system such as governance, health service provision, and financing &
managing resources.
- Without a health system, there would exist no "thriving" of the general population; thus, mankind could run into extinction; however, the presence of a health system
provides a "resistance" to possibilities of death.
- Care for the health of the population will increase the life expectancy and decrease the chances of death of the populace.
Goals & Functions of a Health System
- The World Health Organization [WHO] identifies (3) main goals of a health system:
(1) Improving the health of populations
- The overarching goal of a health system.
- Health status should be measured over the entire population and across different socioeconomic groups.
- Populations must be protected from (2) things:
(1) Existing health risks - already present; most likely a long-term issue faced and dealt by the population.
(2) Emerging health risks - new & poses a threat to the population (e.g., COVID-19 in 2020).
- Intensive preparations for resilience to impending, but still unknown health risks must be executed to ensure the safety of populations (number#1 goal).
- Health systems should strive for equity in health by minimizing inequitable disparities.
→ Minimizing inequitable disparities is accomplished not necessarily by giving people equal treatment, but by giving them what they need.
→ Extra measures should be taken to ensure that existing inequitable disparities should not cause any differences in the delivery of healthcare to the general
population; hence, equity should be one of the foremost goals of every health system.
→ A needs assessment is therefore crucial.
→ Disparities of which may be caused by certain factors:
► Income, ethnicity, occupation, gender, geographic location, sexual orientation, etc.
- There are significant variations in health outcomes across the world, within regions, and within countries―these are inequitable disparities.
- Countries & regions with relatively similar socioeconomic status may have quite disparate health outcomes.
- The way health systems are organized contributes to this disparity―these disparities are most effectively reduced when they are recognized and their
minimization becomes an explicit national goal.
(2) Improving the responsiveness of the health system
- Responsiveness refers to providing satisfactory health services and engaging people as active partners (how fast a health system can respond to the needs of
the general population).
- It embodies the values of respectfulness, dignity, confidentiality, autonomy, quality, & timeliness in the delivery of health services.
→ Provision of services should not be delayed―if people require the administration of a certain type of health service within a certain timeframe, it should be
readily available.
- Health systems have an obligation to respond to the legitimate non-health needs & expectations of populations.
- Responsive health systems maximize people's autonomy & control, allowing them to make choices and placing them at the center of the health system.
→ Health systems should not dictate what people should do (the people should maintain autonomy & control over their preferences).
- Note that the center of a health system are the: People (general population).
→ Therefore, health systems should adjust to the needs of the people, which also cultivates the quality of reacting quickly & positively.
(3) Providing fair health financing
- An ideal health system provides social & financial risk protection in health.
- All health systems must be adequately funded to provide essential services to all citizens.
- WHO defines a fairly financed health system as one that does not deter individuals from receiving needed care due to payments required at the time of service,
and one in which each individual pays approximately the same percentage of their income for needed services regardless of social status in life.
→ A health system is "fairly financed" if even those with the most disadvantageous socioeconomic status are able to access healthcare.
→ This is evident in public hospitals, where patients are not pressured with initial down-payments before receiving the medical attention they need.
In contrast with private hospitals, which strictly require down-payments prior to performing a certain service.
- A health financing system that dissuades people form seeking needed services or impoverishes individuals & families worsens health outcomes.
→ Discouragement expressed by the people as a result of lack of funds to receive health services is a sign of that a health system is not functioning well.
Four (4) Functions of a Health System
- Note that health systems actually go beyond hospital settings, and includes both the community & agencies aimed at promoting healthcare.
(1) Health service provision
- The most visible product of the health system is: Public & private health service provision (concrete evidences of health systems).
- A health service is any service, not limited to clinical services, aimed at improving the health of populations.
HIS Lec Page 1
- A health service is any service, not limited to clinical services, aimed at improving the health of populations.
- Preventive measures as well as the promotion of a healthy way of living to avoid illnesses also form part of the best systems.
→ Services provided must not only be limited to healing nor treatment, but must be inclusive of prevention & different surveillance programs that will lead to the
improvement of the quality of life of the general population (e.g., educational materials).
→ Evident in the posters publicized by the DOH (e.g., campaigns against smoking/drinking).
- Therefore, each health system has to perform a wide range of activities to cater to these various demands.
(2) Health service inputs
- Also called: Managing resources.
- Refers to generating the essential physical resources for the delivery of health services which include:
► Medications
► Human resources (trained doctors & medical staff)
► Medical equipment
- Medicines that are not expired, state-of-the-art medical equipment, and updated, trained, & competent human resources are part of health service inputs.
- These are the different resources that need to be managed well in order to guarantee that health services will be provided efficiently to the population.
- Resources such as trained doctors, medical staff, & supply of medications often take time to be produced; hence, the health system policymakers have to respond
and use the available resources to address short-term population needs as soon as possible.
→ Note that almost all health needs are immediate, excluding chronic illnesses (which require management).
- It is the responsibility of health system policymakers.
(3) Stewardship
- Also called: Overall system oversight.
- The main responsibility of the government.
- Stewardship is defined as the supervision, or taking care of something.
- This function sets the direction, context, and policy framework for the overall health system.
- The cores of stewardship include:
(1) Identifying health priorities for the allocation of public resources
→ Performing a needs assessment is truly crucial given that for every population, there exists a different need―as such, there is the need to assess first the needs
of the population in order to prioritize the resources (i.e., buying drugs for drug cases that are not prevalent in the population).
→ Example:
► Fight against mycobacterium tuberculosis in the Philippines.
- For other countries, purchasing vaccines/drugs against mycobacterium tuberculosis would be a waste of their budgets/resources , since it is an illness
that is not prevalent in their country; however, it is one of the main health issues prioritized by the Philippines.
→ For every country & location, there will be different health risks & needs of the general population; hence, identification & prioritization of health needs of a
certain population are important before allocating a budget/resources.
(2) Identifying an institutional framework
(3) Coordinating activities with other systems related to external health care
(4) Analyzing health priorities & resource generation trends + their implications
→ Trends about the population, death tolls, usual causes of death in a certain area, and other pertinent information must be known.
(5) Generating appropriate data for effective decision-making and policymaking on health matters (research)
→ Has to have a special study in order for us to have a scientific & sound basis of why we are prioritizing a certain project.
→ Note that a budget can only do so little if not used properly.
(4) Health financing
- Health system financing includes raising & pooling resources to pay for health services.
- More on looking for the resources used to sustain a health system (e.g., buying medicine/medical equipment, paying for health professionals, etc.).
- Includes:
(1) Revenue collection
- Revenue is the money earned from payments for healthcare services.
- Each source of health financing is associated with a specific manner of organizing & pooling
of funds and purchasing services.
- The mechanisms for revenue collection include:
► General taxation
- Public health systems rely on general taxation for its financing.
► Direct household out-of-pocket expenditures
► Mandatory payroll contributions
- Social security organizations are funded through mandatory payroll
contributions from workers & employers.
► Mandatory or voluntary risk-rated contributions
► Donor financing
► Other forms of personal savings
(2) Risk pooling
- Involves gathering together or combining funds from people's taxes or income to finance
or pay for another person's expenses (health risks).
- Financial risk pooling is a form of risk management which aims to spread financial risks
from an individual to all pool members.
→ Instead of one individual shouldering the financial responsibility, all pool members
will be involved in the funding (finances are divided among the members). Shows the money allocated for medical healthcare in
- It is considered as a core function of health insurance companies. each country in dollars (with an increment of every 5
- This mechanism prevents outright payment for health services (which discourages years since 2000).
patients belonging to the poor sector from seeking healthcare).
- Participation in effective risk pooling helps families from financial losses due to health USA is ranked first not because of any political factor,
shocks; thus, ensuring financial protection. but because of high costs of medical treatment and
- Each country has its own approach to managing its financial risks to finance its healthcare malpractice insurance. Hence, allocation is higher in
system―multiple & fragmented forms of risk pooling arrangements exist in most them (the value is high primarily because the cost of
developing countries. healthcare services are also high).
- Most high-income countries follow one of the (2) main models of risk pooling:
(1) Bismarck Model - Bismarck's Law on Health Insurance of 1883. By 2015, in the Philippines, approximately Php 16,000
- Named after the Prussian Chancellor, Otto von Bismarck, which is known for per person is allocated as a budget for their health or
inventing the welfare state in the 19th century as part of the unification of Germany. medical needs.
- The Bismarck model uses an insurance system where the sickness fund finances both
the employers & the employees through payroll deduction.
- However, unlike the US insurance industry, the Bismarck-type health insurance plan covers everybody; thus ultimately collecting no profit at all.
- This is considered as a: Multi-payer model, with tight regulation giving the government the cost-control clout.
HIS Lec Page 2
- This is considered as a: Multi-payer model, with tight regulation giving the government the cost-control clout.
- Underlying principle: Health insurance covers everybody.
- Countries using the Bismarck model include:
► Germany
► France
► Belgium
► Netherlands
► Japan
► Switzerland
► Latin America (to a certain degree)
(2) Beveridge Model - Beveridge Report of the Social Insurance & Allied
Services of 1942
- Named after William Beveridge, the social reformer responsible for
designing Britain's Social Security System and the National Health Service.
- In the Beveridge model, healthcare is provided & funded by the government through tax payments (shared by the government).
- The government owns many, but not all, hospitals & clinic in the country.
→ You can seek healthcare provision from doctors of either government-owned facilities or private-owned facilities.
→ Professional fees to fund the services of these healthcare professionals will be handled by the gov't.
- Doctors may be government or private employees who collect their professional fees from the government.
- This results in low cost per capita since the government controls the healthcare services.
- Underlying principle: Healthcare is a basic human right.
- Countries using the Beveridge plan include:
► Hong Kong
► Great Britain
► Spain
► Scandinavia (most)
► New Zealand
► Cuba (the Cuban government uses total government control)
(3) Strategic purchasing
- Employs a plan of action or involves research prior to "purchasing" in order to minimize costs & maximize quality (worth the money).
- In both passive purchasing or impulsive buying, it is important to employ strategic purchasing.
- In strategic purchasing, risk-pooling organizations use collected funds and pooled financial resources wisely to finance healthcare services for the members.
- The purchaser defines the substantial part of the health provider's external incentives to develop the provider-user interaction & the health service delivery
models.
- Money saved through strategic purchasing can be used to spend for healthcare needs during "rainy days" (no need to exhaust all the funds).
→ Functions as a back-up plan.
- Important part of boosting efficiency & profitability in your company/institution.
- Able to save more by getting the best deals.
WHO Health System Framework
- In its World Health Report 2000, WHO released a single framework with (6) clearly defined building blocks & priorities which are necessary in strengthening health
systems and improving the overall health outcomes.
- This framework functions to ensure that the health system has improved efficiently in its services, have social & financial risk protections, improve the level & equity
of health, improve responsiveness, safety from non-desirable outcomes (harm), and possession of a contingency plan (back-up plan).
(1) Service delivery
- Refers to the timely delivery of quality & cost-effective personal & non-personal health services.
- Pertains to service provision that is not delayed; Usually done or occurring at a favorable time wherein it is most needed or useful.
- Quick turn-around-time [TAT] for a patient who is dying and timely delivery of service is crucial, especially in the medical field.
(2) Health workforce
- Includes individuals & groups working towards the achievement of the best health outcomes by being responsive, fair, & efficient (e.g., frontliners).
- The number of staff should be sufficient & fairly distributed to ensure competency, responsiveness, & productivity (involves collaboration).
- The most critical building block in a health system in order to ensure the provision of services―they are able to improvise in the absence of healthcare resources.
(3) Information (Health information system)
- Analyzes (requires scrutinizing data), disseminates (distribute information), and uses reliable (dependable) & relevant (timely) information on health status,
determinants, and systems performance.
- The right information can help in the proper management of patients.
- Hence, HIS is crucial in order to ascertain the best ways to augment patient care by having reliable & relevant information t o be used in the community care.
(4) Health/medical products, vaccines, & technologies
HIS Lec Page 3
(4) Health/medical products, vaccines, & technologies
- Made accessible through uninterrupted supply (supply is consistent, continuous, & timely to prevent scarcity), well-managed pharmaceutical services, and education
on the proper use of medication.
(5) Financing (Health financing system)
- Pertains to appropriate funding for healthcare services to guarantee that people can use health services when needed without fear of not having enough resources
to pay for them―helps those who do not have the financial capacity.
(6) Leadership & Governance
- Involves the task of ensuring effective stewardship of the entire health system.
- Excellent leaders & managers are needed in order to provide effective supervision.
- Also covers the monitoring of the accountability of private & public health agencies, proper system design (those behind the designing of the health system), and
appropriate regulation of health systems.
The Philippine Health System
- The health reform initiatives carried out over the years in the Philippines were primarily focused on these areas of concern:
► Health service delivery
► Health regulation
► Health financing
- These health reforms aimed at addressing issues such as poor accessibility, inequity, and inefficiency of the Philippine health system.
- How the healthcare system of the Philippines is formed can be summarized with the ff. important milestones in history:
(1) 1979: Adoption of Primary Health Care Strategy (Letter of Instruction [LOI] 949)
- Promoted participatory management of the local health care system.
- The Philippine Health Care system [PHC] is an essential health care system based on methods & technology made universally accessible to individuals.
- Healthcare provision is basic, rather than at a specialized level for people making an initial approach to a doctor or nurse for treatment.
(2) 1982: Reorganization of DOH (Executive Order [EO] 851)
- Integrated the components of health care delivery into its field of operations.
- EO 851 reorganized the DOH to synchronize health structures & operations with the shift to parliamentary form of government (formerly known as the Ministry
of Health)―later, under the presidential form, reverted back as the Department of Health.
→ The Ministry of Health has a head (minister) and departments run through a parliamentary system (state governance) by a group of people.
(3) 1988: The Generics Act (RA 6675)
- Ushered the writing of prescriptions using the generic name of the drug.
- Instead of forcing patients to by branded medicine (specific, branded drugs are not accessible & affordable to everyone) with physicians commonly prescribing
medications to patients by writing specific brand names, physicians were mandated to give out generic prescriptions.
(4) 1991: Local Government Code (RA 7160)
- Transferred the responsibility of providing health service to the local government units.
- Establishes the system and defines powers of provincial, city, municipal, & barangay governments in the Philippines―the act transferred the responsibility of
providing health services to the local government units [LGUs].
- This course of action provides for a more responsive local government structure.
→ Prevents people forced to travel to national government healthcare facilities/units to avail quality health services; as such, LGUs were delegated the specific
responsibilities & duties in order to speed up the rate of response to patient needs.
→ This response is instituted through the establishment of a decentralized system―where LGUs are delegated power, authority, responsibility, & resources to
possess the capacity to respond accordingly to patient needs.
- This is crucial development because the Philippines is an archipelago comprised of multiple, widely-dispersed islands; thus, making both communication and
transportation relatively difficult to accomplish.
- A centralized system for decision-making was deemed infeasible.
(5) 1995: National Health Insurance Act (RA 7875)
- Instituted a national health insurance mechanism for financial protection with priority given to the poor.
- Where PhilHealth plays a major role.
(6) 1999: Health Sector Reform Agenda
- Ordered the major organizational restructuring of the DOH to improve the way health care is delivered, regulated, & financed.
(7) 2005: FOURmula One [F1] for Health
- Adopted an operational framework to undertake reforms with speed, precision, & effective coordination and to improve the Philippine health system.
- Focuses on timely delivery of services.
(8) 2008: Universally Accessible Cheaper and Quality Medicines Act (RA 9502)
- Promoted and ensured access to affordable quality drugs & medicines for all.
(9) 2010: Kalusugang Pangkalahatan or Universal Health Care (Administrative Order [AO] 2010-0036)
- Provided universal health coverage & access to quality healthcare for all Filipinos.
The Philippine Health System: Leadership & Governance
(1) Department of Health [DOH]
- Mandated to provide the appropriate direction for the nation's healthcare industry.
- The incumbent DOH secretary is currently: Francisco Duque.
- Its other tasks include:
(1) Development of plans, guidelines, & standards for the health sector
(2) Technical assistance
(3) Capacity building
(4) Advisory services for disease prevention
(5) Control of medical supplies & vaccines
- DOH coordinates its national health programs through the local government
units [LGUs].
- The DOH is duty-bound to the ff. responsibilities, with the help of LGUs:
(1) Develop policies & programs for the health sector
HIS Lec Page 4
- DOH coordinates its national health programs through the local government
units [LGUs].
- The DOH is duty-bound to the ff. responsibilities, with the help of LGUs:
(1) Develop policies & programs for the health sector
(2) Provide technical assistance to its partners (e.g., local mayors, brgy. tanods, etc.)
(3) Encourage performance of the partners in the priority health programs
→ It is within their responsibility to ensure that health professionals are paid
well and are appropriately & justly compensated for their services.
(4) Develop and enforce policies & standards
(5) Design programs for large segments of the population
→ Examples are feeding programs, diabetes prevention & control programs, health & wellness programs for senior citizens, and many more.
→ Involves lab work & research as well as discussions about the different needs of a community and ensure that these needs are addressed.
Again, conducting a needs assessment is crucial to prevent offering solutions that are useless, unneeded, and not targeting any problems.
Hence, designing programs should be heavily research-based (involves analysis of data to determine which pressing issues should be allocated resources).
(6) Provide specialized & tertiary level care
(2) Local Government Units [LGUs]
- Take care of their own health services and are given autonomy under the Local Government Code [LGC] of 1991 (RA 7160).
- 78 provincial governors, 138 city mayors, 1,496 municipal mayors, & 42,025 barangay chairpersons compose the local government units of the country.
- In terms of administration, LGUs are grouped into 17 regions.
- Although they operate in a decentralized system, LGUs are under the supervision of the DOH regional health officers (work hand-in-hand with barangay tanods to
assess health concerns/burdens of disease of each community).
→ A problem should be first established, which results in the development of a need, before a solution can be conceived.
Problem identification = Needs assessment = Conception of solution/s.
→ It is through coordination with local mayors, barangay tanods, and LGUs that the DOH are able to enact accurate, timely, & necessary national health
programs.
- The provincial government is tasked to provide health services through provincial & district hospitals.
- The city & municipal governments rely on public health & primary health care centers for their primary care.
- Under the decentralized or devolved structure, the state is represented by national offices & LGUs alongside provincial, city, municipal, & barangay or village offices.
- DOH, LGUs, and the private sector participate, cooperate, & collaborate in the care of the population―Before devolution, the national health system consisted of a
three-tiered system under the direct control of the DOH:
(1) Tertiary hospitals at the national & regional levels
(2) Provincial & district hospitals and city & municipal health centers
(3) Barangay (village) health centers
- With the enactment of the LGC of 1991, the government health system now consists of basic health services―including health promotion & preventive
units―provided by cities and municipalities, provincial & province-run district hospitals of varying capacities, and mostly tertiary medical centers, specialty hospitals,
and a number of re-nationalized provincial hospital managed by DOH.
Directions of the Philippine Health Sector
(1) The Philippine Health Agenda 2016-2022 (DOH Administrative Order 2016-0038)
- Adopts the slogan "All for Health Towards Health for All" as the rallying point of its vision of a healthy Philippines by 2022.
- It expanded the scope of the Universal Health Care [UHC] directions, particularly through a whole-of-government approach (ensures that the entire government is
mobilized for this project).
- With this agenda, the health system guarantees:
► Population- & individual-level interventions for all life stages that promote health and wellness, prevent & treat the triple burden of disease, delay
complications, rehabilitation, and provide palliation for both the well & the sick.
→ The triple burden of disease includes: Communicable diseases, malnutrition, & diseases of rapid urbanization.
→ Life stages primarily focused on: Pregnant women, infants, children, adolescents, young adults, and essentially, all life stages.
► Access to health interventions through functional service delivery networks [SDNs].
► Financial freedom when accessing these interventions through Universal Health Insurance.
→ Ensures that people do not have to worry about paying given that they are insured (have covered medical costs).
→ An expansion of the Universal Health Care [UHC].
- Delayed due to the onset of the COVID-19 pandemic as an unprecedented health risk (a lot of time & attention has been directed to it).
(2) The Philippine Development Plan 2017-2022
- The first of the 4 key medium-term plans to translate the vision of a "matatag (unshaken), maginhawa (comfortable), at panatag (peace achieved from good health
coverage) na buhay" for the Filipinos and the country.
- Spearheaded by the National Economic and Development Authority [NEDA].
(3) NEDA AmBisyon Natin 2040
- A product of the Philippine Development Plan 2017-2022, this collective long-term plan envisions better life for the Filipinos and the country in the next 25 years by
formulating policies & implementing programs and projects to attain this AmBisyon.
- Requires a high level of trust in the government (assurance that this project will be continued regardless of who sits in the presidential position).
→ The project could be impeded depending on whoever new will spearhead the Philippine government.
- This plan focuses on (4) areas:
► Building a prosperous, predominantly middle-class society where no one is poor
HIS Lec Page 5
► Building a prosperous, predominantly middle-class society where no one is poor
► Promoting a long & healthy life
► Becoming smarter and more innovative
► Building a high-trust society
→ High-trust is dependent upon the success of the government in accomplishing the objectives of this project.
→ Necessitates an "exchange of trust", since trust in the government in the preliminary stages of the project is needed to encourage long-term efforts from
the government to accomplish the objectives of this project and once accomplished, more trust from the people are earned (builds more confidence in the
Filipinos towards their government in terms of implementing future projects).
(4) Sustainable Development Goals 2030
- Also known as the: 2030 Agenda.
- This compilation of 17 global development goals targets to end poverty, fight inequality & injustice, and confront issues involving climate change.
- Involves the "endgame" visions/ "holistic" goals we want to achieve as a country by 2030.
- Note that the presence of an unprecedented pandemic outbreak, COVID -19, has caused a lot of the governmental projects/plans to be delayed; nevertheless, there still
persists a need to ensure that efforts exerted to meet all of these goals are still on track once the pandemic dies.
- It is one of the responsibilities of the health systems and those who serve in the leadership & governance positions to make sure that these goals are still intact even
after the pandemic and work towards achieving them in the soonest possible time (if it cannot be achieved within the target year).
-------------------------------------------------------------------------------------------------------------------END-------------------------------------------------------------------------------------------------------------
HIS Lesson 2 Health System Video Link: HIS Lesson 2 Health System
HIS Lec Page 6
You might also like
- PBMDocument91 pagesPBMkodanda100% (1)
- (SpringerBriefs in Public Health) A. L. Hamdan (Auth.) - Strategic Thinking in A Hospital Setting-Springer International Publishing (2017) PDFDocument95 pages(SpringerBriefs in Public Health) A. L. Hamdan (Auth.) - Strategic Thinking in A Hospital Setting-Springer International Publishing (2017) PDFMohit SinghNo ratings yet
- A Plan for a Single-Payer Health Care System: The Best Health Care in the WorldFrom EverandA Plan for a Single-Payer Health Care System: The Best Health Care in the WorldNo ratings yet
- Prescription: John Paul B. Garrido, RPHDocument57 pagesPrescription: John Paul B. Garrido, RPHJape Garr0% (1)
- Health Care EconomicsDocument26 pagesHealth Care Economicskneil1621100% (1)
- Rizal FinalsDocument56 pagesRizal FinalsLYKA ANTONETTE ABREGANANo ratings yet
- Healthcare Marketing India PDFDocument35 pagesHealthcare Marketing India PDFAbhishekNo ratings yet
- Understanding Clinical Trial LingoDocument36 pagesUnderstanding Clinical Trial Lingojram00No ratings yet
- Health Care Delivery System in India and AbroadDocument46 pagesHealth Care Delivery System in India and AbroadANITTA S100% (6)
- New Health Systems: Integrated Care and Health Inequalities ReductionFrom EverandNew Health Systems: Integrated Care and Health Inequalities ReductionNo ratings yet
- Handbook of Pharmaceutical Generic Development Vol 12 Part 2Document236 pagesHandbook of Pharmaceutical Generic Development Vol 12 Part 2Pablo Atapuma100% (7)
- Health Systems Strengthening - The University of MelbourneDocument14 pagesHealth Systems Strengthening - The University of MelbourneEstefanía MariñoNo ratings yet
- HEALTH CARE ENVIRONMENTDocument57 pagesHEALTH CARE ENVIRONMENTkrishnasree100% (3)
- 3.1 Concept of Health EconomicsDocument4 pages3.1 Concept of Health EconomicsmitalptNo ratings yet
- FDA FAQs On AO 2015-003Document4 pagesFDA FAQs On AO 2015-003Jacques oltrade100% (2)
- Health Care Delivery System in IndiaDocument65 pagesHealth Care Delivery System in IndiaAparna Kingini100% (1)
- Alumni Data 2008 2018Document52 pagesAlumni Data 2008 2018CIO White PapersNo ratings yet
- Healthcare Industry in IndiaDocument18 pagesHealthcare Industry in IndiaDarryl CordeiroNo ratings yet
- Health Care Delivery SystemDocument42 pagesHealth Care Delivery SystemAnusha Verghese95% (20)
- Health EconomicsDocument114 pagesHealth EconomicsGeneva Ruz BinuyaNo ratings yet
- Health System FrameworkDocument113 pagesHealth System FrameworkDesi SusantiNo ratings yet
- Bangladesh's Healthcare Delivery ExplainedDocument50 pagesBangladesh's Healthcare Delivery ExplainedDip Ayan MNo ratings yet
- Health Care Delivery System in IndiaDocument24 pagesHealth Care Delivery System in Indiarizwan89% (9)
- Health EconomicsDocument19 pagesHealth EconomicsSyamVRNo ratings yet
- Health Care Financing - 8Document13 pagesHealth Care Financing - 8copy smart50% (2)
- Health-Care Entrepreneurship: Embracing the Mindset and Skills for Competitive and Sustainable Healthcare EntrepreneurshipFrom EverandHealth-Care Entrepreneurship: Embracing the Mindset and Skills for Competitive and Sustainable Healthcare EntrepreneurshipNo ratings yet
- HEALTH PROMOTION AND PRIMARY HEALTH CAREDocument34 pagesHEALTH PROMOTION AND PRIMARY HEALTH CAREKavya S Mohan100% (2)
- Health Care Delivery System in IndiaDocument14 pagesHealth Care Delivery System in IndiaSaumiya NairNo ratings yet
- India CIS Pharma Conference Delegate ListDocument7 pagesIndia CIS Pharma Conference Delegate Listshaishav_86100% (2)
- The Philippine Health Care Delivery SystemDocument19 pagesThe Philippine Health Care Delivery SystemArianne Kamille AndesNo ratings yet
- Introduction To Health SystemsDocument61 pagesIntroduction To Health SystemsAngella100% (9)
- UNIT - 1 Health Care Delivary System in IndiaDocument48 pagesUNIT - 1 Health Care Delivary System in IndiaMrs Raina Jenifer Mascarenhas fmsonNo ratings yet
- 3 Health SystemDocument113 pages3 Health SystemTha RieNo ratings yet
- Health System: Team Teaching HSM Departemen Ilmu Kesehatan Masyarakat Fakultas Kedokteran Universitas PadjadjaranDocument113 pagesHealth System: Team Teaching HSM Departemen Ilmu Kesehatan Masyarakat Fakultas Kedokteran Universitas PadjadjaranrismarizemNo ratings yet
- 3 Health SystemDocument113 pages3 Health SystemHendryNo ratings yet
- HIS NotesDocument20 pagesHIS NotesGiane MadrigalNo ratings yet
- HEALTH CARE DELIVERY SYSTEM IN INDIADocument27 pagesHEALTH CARE DELIVERY SYSTEM IN INDIAnathsujitkr1980No ratings yet
- Health Triangle and 6 Building Blocks of Health SystemsDocument21 pagesHealth Triangle and 6 Building Blocks of Health Systemswarisara eeNo ratings yet
- HEALTH CARE DELIVERY SYSTEM Lesson PlanDocument22 pagesHEALTH CARE DELIVERY SYSTEM Lesson PlanJosephin dayanaNo ratings yet
- Health Care Deliver System AjayDocument41 pagesHealth Care Deliver System AjayAjay DNo ratings yet
- 2.1. Definition of Health Care SystemDocument12 pages2.1. Definition of Health Care SystemSittie Aina MunderNo ratings yet
- The Philippine Health Care SystemDocument12 pagesThe Philippine Health Care SystemMica-Ella CasasolaNo ratings yet
- Lecture 2Document25 pagesLecture 2مرتضى محمد منصورNo ratings yet
- This Study Resource WasDocument8 pagesThis Study Resource WasMae Ann BusicoNo ratings yet
- (W2) Health Care SystemDocument4 pages(W2) Health Care Systemreghin89No ratings yet
- Approaches in Community Health NursingDocument57 pagesApproaches in Community Health NursingNoelie Mae IglupasNo ratings yet
- Primary Health Care (PHC) Health For All Approach: by Amarah Tahir RIHSDocument38 pagesPrimary Health Care (PHC) Health For All Approach: by Amarah Tahir RIHSAbdur RehmanNo ratings yet
- Health Care of CommunityDocument21 pagesHealth Care of Communitypaul vinothNo ratings yet
- NCM 104 Week 3Document15 pagesNCM 104 Week 3Nathan Lloyd SangcapNo ratings yet
- CH 63 HSM IntroductionDocument8 pagesCH 63 HSM IntroductionRijane Tabonoc OmlangNo ratings yet
- Primary Health CareDocument15 pagesPrimary Health Carekinid100% (1)
- Ictm Prelim Reviewer 1Document14 pagesIctm Prelim Reviewer 1acgalamiton6249antNo ratings yet
- UNIT1 TOPIC2 - Goals and Functions of Health SystemDocument7 pagesUNIT1 TOPIC2 - Goals and Functions of Health SystemJean Marie FelipeNo ratings yet
- The Private Sector,: Universal Health Coverage and Primary Health CareDocument12 pagesThe Private Sector,: Universal Health Coverage and Primary Health CareJohn Aries CabilingNo ratings yet
- Alem Assignment Health Care SystemsDocument7 pagesAlem Assignment Health Care SystemsSileshi NegashNo ratings yet
- Chapter 103 PHCDocument47 pagesChapter 103 PHCYassir OunsaNo ratings yet
- Health SystemsDocument8 pagesHealth SystemsLloyd SalesNo ratings yet
- DR - Wali.all Health Administration LecturesDocument18 pagesDR - Wali.all Health Administration LecturesTurk JaddyNo ratings yet
- 4005-1 To 3Document49 pages4005-1 To 3Noelie Mae IglupasNo ratings yet
- How Governments Can Improve Health System StewardshipDocument24 pagesHow Governments Can Improve Health System StewardshipnilandariNo ratings yet
- Health Care Delivery System in IndiaDocument63 pagesHealth Care Delivery System in IndiaamsabavanNo ratings yet
- RP248 Health Systems, Management, and Organization in Low-And Middle Income CountriesDocument15 pagesRP248 Health Systems, Management, and Organization in Low-And Middle Income CountriesBoyIPNo ratings yet
- Week 2 NotesDocument5 pagesWeek 2 Notesu21698245No ratings yet
- Universal Health Coverage of Bangladesh - Analysis Through The Framework of Alford's Theory of Structural Interests in Health Care PPT 28 PresentedDocument30 pagesUniversal Health Coverage of Bangladesh - Analysis Through The Framework of Alford's Theory of Structural Interests in Health Care PPT 28 PresentedRashed ShukornoNo ratings yet
- Milq 054Document28 pagesMilq 054Bassam AlqadasiNo ratings yet
- 5 Star DoctorDocument25 pages5 Star DoctorNadzira KarimaNo ratings yet
- Primary Health Care PHC Health For All ApproachDocument31 pagesPrimary Health Care PHC Health For All ApproachChukwu Janefrances100% (1)
- 5 StarDocument13 pages5 StarSofie Hanafiah NuruddhuhaNo ratings yet
- The politics of health promotion: Case studies from Denmark and EnglandFrom EverandThe politics of health promotion: Case studies from Denmark and EnglandNo ratings yet
- The Corporatization of American Health Care: The Rise of Corporate Hegemony and the Loss of Professional AutonomyFrom EverandThe Corporatization of American Health Care: The Rise of Corporate Hegemony and the Loss of Professional AutonomyNo ratings yet
- Efficacy, Effectiveness And Efficiency In The Management Of Health SystemsFrom EverandEfficacy, Effectiveness And Efficiency In The Management Of Health SystemsNo ratings yet
- Rizal quiz questionsDocument7 pagesRizal quiz questionsLYKA ANTONETTE ABREGANANo ratings yet
- SY 2022-2023 Updated Chem 301 Biochem Lec Synch and AsynchDocument3 pagesSY 2022-2023 Updated Chem 301 Biochem Lec Synch and AsynchLYKA ANTONETTE ABREGANANo ratings yet
- Opportunity Identification and Selection SPC MLS2 ENTREPDocument5 pagesOpportunity Identification and Selection SPC MLS2 ENTREPLYKA ANTONETTE ABREGANANo ratings yet
- Rizal's Education and Life Abroad in EuropeDocument1 pageRizal's Education and Life Abroad in EuropeLYKA ANTONETTE ABREGANANo ratings yet
- Blood and Bone MarrowDocument35 pagesBlood and Bone MarrowLYKA ANTONETTE ABREGANANo ratings yet
- Pre-Hispanic Philippines and Western ExpansionismDocument23 pagesPre-Hispanic Philippines and Western ExpansionismLYKA ANTONETTE ABREGANANo ratings yet
- (MIDTERMS) Gforms & Quipper AnswersDocument26 pages(MIDTERMS) Gforms & Quipper AnswersLYKA ANTONETTE ABREGANANo ratings yet
- TEM 100 LECTURE ON MARKETING AND CUSTOMER VALUEDocument9 pagesTEM 100 LECTURE ON MARKETING AND CUSTOMER VALUELYKA ANTONETTE ABREGANANo ratings yet
- Labor Standards - SPC Mls2 - EntrepDocument5 pagesLabor Standards - SPC Mls2 - EntrepLYKA ANTONETTE ABREGANANo ratings yet
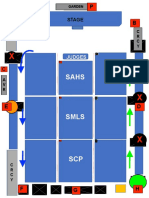
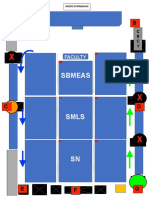
- Sugata 2022 Final Floor PlanDocument2 pagesSugata 2022 Final Floor PlanLYKA ANTONETTE ABREGANANo ratings yet
- Operations Management - SPC Mls2 - EntrepDocument6 pagesOperations Management - SPC Mls2 - EntrepLYKA ANTONETTE ABREGANANo ratings yet
- Security Committee Designated AreasDocument2 pagesSecurity Committee Designated AreasLYKA ANTONETTE ABREGANANo ratings yet
- Sugata Floor PlanDocument2 pagesSugata Floor PlanLYKA ANTONETTE ABREGANANo ratings yet
- HIS 1st Semester LIMS ReviewDocument4 pagesHIS 1st Semester LIMS ReviewLYKA ANTONETTE ABREGANANo ratings yet
- Official Lecture#5 - Health Information SystemsDocument3 pagesOfficial Lecture#5 - Health Information SystemsLYKA ANTONETTE ABREGANANo ratings yet
- Official Lecture#4 - Overview of Health InformaticsDocument3 pagesOfficial Lecture#4 - Overview of Health InformaticsLYKA ANTONETTE ABREGANANo ratings yet
- Official Lecture#1 - Vision, Mission, Core Values, & Objectives of The InstitutionDocument4 pagesOfficial Lecture#1 - Vision, Mission, Core Values, & Objectives of The InstitutionLYKA ANTONETTE ABREGANANo ratings yet
- Official Lecture#3 - Primary Health Care & Healthcare Delivery SystemDocument6 pagesOfficial Lecture#3 - Primary Health Care & Healthcare Delivery SystemLYKA ANTONETTE ABREGANANo ratings yet
- Report Suspected Drug ReactionsDocument2 pagesReport Suspected Drug ReactionsanandryajiNo ratings yet
- Drug Development Process Explained in 40 StepsDocument16 pagesDrug Development Process Explained in 40 StepsNachiket PatelNo ratings yet
- South Sudan National Health Policy 2016 To 2025 2Document40 pagesSouth Sudan National Health Policy 2016 To 2025 2Winny DianaNo ratings yet
- Economic Analysis Indian Pharma IndustryDocument19 pagesEconomic Analysis Indian Pharma IndustryPooja SajanNo ratings yet
- Wenstrup Biosimilars Letter To FDADocument3 pagesWenstrup Biosimilars Letter To FDAGreg BrooksNo ratings yet
- Patient Safety Quality Care MovementDocument11 pagesPatient Safety Quality Care Movementapi-325099570No ratings yet
- Facts About Pharmaceutical MarketingDocument13 pagesFacts About Pharmaceutical MarketingClaudia DavidNo ratings yet
- Pharma LitigationDocument24 pagesPharma LitigationDarshan DarjiNo ratings yet
- Welcome Coffee & Registrations Welcome Note - Exito Media Concepts Private LimitedDocument1 pageWelcome Coffee & Registrations Welcome Note - Exito Media Concepts Private LimitedAmey NalawadeNo ratings yet
- Acetaminophen COADocument1 pageAcetaminophen COAHamza HaqueNo ratings yet
- Regional National Accounts Sales in Boston MA Resume Stephen SanfaconDocument2 pagesRegional National Accounts Sales in Boston MA Resume Stephen SanfaconstephensanfaconNo ratings yet
- Ijser: The Impact of Applying Social Media in The Healthcare IndustryDocument3 pagesIjser: The Impact of Applying Social Media in The Healthcare IndustryIin Fadhilah Utami NewNo ratings yet
- Organizaational ChangeDocument94 pagesOrganizaational ChangeAravind Kumar KotamsettyNo ratings yet
- An Emperical Study On Consumer's Perception Towards Health Insurance in Gwalior District of Madhya PradeshDocument6 pagesAn Emperical Study On Consumer's Perception Towards Health Insurance in Gwalior District of Madhya PradeshPARTH PATELNo ratings yet
- GULRUKHDocument5 pagesGULRUKHGulrukh SadullaevaNo ratings yet
- Medfield Pharma AssignmentDocument2 pagesMedfield Pharma AssignmentDebanu MahapatraNo ratings yet
- October 19, 2018 Approval Letter - VarivaxDocument2 pagesOctober 19, 2018 Approval Letter - VarivaxUltimo NezNo ratings yet
- WB p167000 FzkphkeDocument13 pagesWB p167000 FzkphkeVic MelendezNo ratings yet
- Northern Region Customers FY 18-19Document4 pagesNorthern Region Customers FY 18-19Nitin PulyaniNo ratings yet
- Name of Pharmacy: ................................. CityDocument1 pageName of Pharmacy: ................................. Cityravi sheladiyaNo ratings yet