Professional Documents
Culture Documents
Diabetic Autonomic Neuropathy
Diabetic Autonomic Neuropathy
Uploaded by
DrHardik DudhatraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetic Autonomic Neuropathy
Diabetic Autonomic Neuropathy
Uploaded by
DrHardik DudhatraCopyright:
Available Formats
Reviews/Commentaries/Position Statements
T E C H N I C A L R E V I E W
Diabetic Autonomic Neuropathy
AARON I. VINIK, MD, PHD1 BRAXTON D. MITCHELL, PHD3 relative risk is doubled) associated with an in-
RAELENE E. MASER, PHD2 ROY FREEMAN, MD4 creased risk of silent myocardial ischemia and
mortality. The determination of the presence
of CAN is usually based on a battery of auto-
nomic function tests rather than just on one
ABSTRACT—Diabetic autonomic neuropathy (DAN) is a serious and common complication
test. Proceedings from a consensus conference
of diabetes. Despite its relationship to an increased risk of cardiovascular mortality and its
in 1992 recommended that three tests (R-R
association with multiple symptoms and impairments, the significance of DAN has not been fully
variation, Valsalva maneuver, and postural
appreciated. The reported prevalence of DAN varies widely depending on the cohort studied and
blood pressure testing) be used for longitudi-
the methods of assessment. In randomly selected cohorts of asymptomatic individuals with
nal testing of the cardiovascular autonomic
diabetes, ⬃20% had abnormal cardiovascular autonomic function. DAN frequently coexists
system. Other forms of autonomic neuropathy
with other peripheral neuropathies and other diabetic complications, but DAN may be isolated,
can be evaluated with specialized tests, but
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
frequently preceding the detection of other complications. Major clinical manifestations of DAN
these are less standardized and less available
include resting tachycardia, exercise intolerance, orthostatic hypotension, constipation, gastro-
than commonly used tests of cardiovascular
paresis, erectile dysfunction, sudomotor dysfunction, impaired neurovascular function, “brit-
autonomic function, which quantify loss of
tle diabetes,” and hypoglycemic autonomic failure. DAN may affect many organ systems
HRV. Interpretability of serial HRV testing re-
throughout the body (e.g., gastrointestinal [GI], genitourinary, and cardiovascular). GI distur-
quires accurate, precise, and reproducible
bances (e.g., esophageal enteropathy, gastroparesis, constipation, diarrhea, and fecal inconti-
procedures that use established physiological
nence) are common, and any section of the GI tract may be affected. Gastroparesis should be
maneuvers. The battery of three recom-
suspected in individuals with erratic glucose control. Upper-GI symptoms should lead to con-
mended tests for assessing CAN is readily per-
sideration of all possible causes, including autonomic dysfunction. Whereas a radiographic
formed in the average clinic, hospital, or
gastric emptying study can definitively establish the diagnosis of gastroparesis, a reasonable
diagnostic center with the use of available
approach is to exclude autonomic dysfunction and other known causes of these upper-GI
technology. Measurement of HRV at the time
symptoms. Constipation is the most common lower-GI symptom but can alternate with episodes
of diagnosis of type 2 diabetes and within 5
of diarrhea. Diagnostic approaches should rule out autonomic dysfunction and the well-known
years after diagnosis of type 1 diabetes (unless
causes such as neoplasia. Occasionally, anorectal manometry and other specialized tests typically
an individual has symptoms suggestive of au-
performed by the gastroenterologist may be helpful. DAN is also associated with genitourinary
tonomic dysfunction earlier) serves to estab-
tract disturbances including bladder and/or sexual dysfunction. Evaluation of bladder dysfunc-
lish a baseline, with which 1-year interval tests
tion should be performed for individuals with diabetes who have recurrent urinary tract infec-
can be compared. Regular HRV testing pro-
tions, pyelonephritis, incontinence, or a palpable bladder. Specialized assessment of bladder
vides early detection and thereby promotes
dysfunction will typically be performed by a urologist. In men, DAN may cause loss of penile
timely diagnostic and therapeutic interven-
erection and/or retrograde ejaculation. A complete workup for erectile dysfunction in men
tions. HRV testing may also facilitate differen-
should include history (medical and sexual); psychological evaluation; hormone levels; mea-
tial diagnosis and the attribution of symptoms
surement of nocturnal penile tumescence; tests to assess penile, pelvic, and spinal nerve func-
(e.g., erectile dysfunction, dyspepsia, and diz-
tion; cardiovascular autonomic function tests; and measurement of penile and brachial blood
ziness) to autonomic dysfunction. Finally,
pressure. Neurovascular dysfunction resulting from DAN contributes to a wide spectrum of
knowledge of early autonomic dysfunction
clinical disorders including erectile dysfunction, loss of skin integrity, and abnormal vascular
can encourage patient and physician to im-
reflexes. Disruption of microvascular skin blood flow and sudomotor function may be among the
prove metabolic control and to use therapies
earliest manifestations of DAN and lead to dry skin, loss of sweating, and the development of
such as ACE inhibitors and -blockers,
fissures and cracks that allow microorganisms to enter. These changes ultimately contribute to
proven to be effective for patients with CAN.
the development of ulcers, gangrene, and limb loss. Various aspects of neurovascular function
can be evaluated with specialized tests, but generally these have not been well standardized and
Diabetes Care 26:1553–1579, 2003
have limited clinical utility. Cardiovascular autonomic neuropathy (CAN) is the most studied
and clinically important form of DAN. Meta-analyses of published data demonstrate that reduced
cardiovascular autonomic function as measured by heart rate variability (HRV) is strongly (i.e.,
● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ●
D
From the 1Strelitz Diabetes Research Institutes, Eastern Virginia Medical School, Norfolk, Virginia; the iabetic autonomic neuropathy
2
Department of Medical Technology, University of Delaware, Newark, Delaware; the 3Department of Med- (DAN) is among the least recog-
icine, Division of Endocrinology, Diabetes, and Nutrition, University of Maryland School of Medicine, nized and understood complica-
Baltimore, Maryland; and the 4Center for Autonomic and Peripheral Nerve Disorders, Beth Israel Deaconess
Medical Center, Harvard Medical School, Boston, Massachusetts. tions of diabetes despite its significant
Address correspondence and reprint requests to Aaron I. Vinik, MD, PhD, Director, Strelitz Diabetes negative impact on survival and quality of
Research Institutes, Eastern Virginia Medical School, 855 W. Brambleton Ave., Norfolk, VA 23510. E-mail: life in people with diabetes (1,2). A sub-
vinikai@evms.edu. type of the peripheral polyneuropathies
This paper was peer-reviewed, modified, and approved by the Professional Practice Committee, January
2003.
that accompany diabetes, DAN can
Abbreviations: AAN, American Academy of Neurology; ANS, autonomic nervous system; CAN, cardio- involve the entire autonomic nervous sys-
vascular autonomic neuropathy; DAN, diabetic autonomic neuropathy; DCCT, Diabetes Control and Com- tem (ANS). ANS vasomotor, visceromo-
plications Trial; ECG, electrocardiogram; ED, erectile dysfunction; E:I, expiration-to-inspiration; GI, tor, and sensory fibers innervate every
gastrointestinal; HRV, heart rate variability; MI, myocardial infarction; PSA, power spectral analysis; QSART, organ. DAN may be either clinically evi-
quantitative sudomotor axon reflex test; TST, thermoregulatory sweat test.
A table elsewhere in this issue shows conventional and Système International (SI) units and conversion dent or subclinical. It is manifested by
factors for many substances. dysfunction of one or more organ systems
© 2003 by the American Diabetes Association. (e.g., cardiovascular, gastrointestinal [GI],
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1553
Technical Review
genitourinary, sudomotor, or ocular) (3). subpopulation of individuals with neu- (HRV) test results was 16.7% (38). In a
Many organs are dually innervated, re- ropathy, immune mechanisms may also further study, Ziegler et al. (24) evaluated
ceiving fibers from the parasympathetic be involved (16 –18). Reduction in neu- the prevalence of CAN in 1,171 diabetic
and sympathetic divisions of the ANS. rotrophic growth factors (19), deficiency patients (647 type 1 diabetic patients, 524
DAN typically occurs as a system-wide of essential fatty acids (20), and formation type 2 diabetic patients) randomly re-
disorder affecting all parts of the ANS. In- of advanced glycosylation end products cruited from 22 diabetes centers in Ger-
deed, because the vagus nerve (the long- (localized in endoneurial blood vessels) many, Austria, and Switzerland. The
est of the ANS nerves) accounts for ⬃75% (21) also result in reduced endoneurial study found that 25.3% of patients with
of all parasympathetic activity (4), and blood flow and nerve hypoxia with al- type 1 diabetes and 34.3% of patients
DAN manifests first in longer nerves, even tered nerve function (8,11,12). The result with type 2 diabetes had abnormal find-
early effects of DAN are widespread. of this multifactorial process may be acti- ings in more than two of six autonomic
Clinical symptoms of autonomic neu- vation of polyADP ribosylation depletion function tests. If more strict criteria were
ropathy generally do not occur until long of ATP, resulting in cell necrosis and ac- used (i.e., abnormalities present in least
after the onset of diabetes. Whereas tivation of genes involved in neuronal three of six autonomic function tests), the
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
symptoms suggestive of autonomic dys- damage (22,23). prevalence of CAN was 16.8% for indi-
function may be common they may fre- viduals with type 1 diabetes and 22.1%
quently be due to other causes rather than EPIDEMIOLOGY OF DAN for individuals with type 2 diabetes. An-
to true autonomic neuropathy. Subclini- The reported prevalence of DAN varies, other study group observed nearly an
cal autonomic dysfunction can, however, depending on whether studies have been identical prevalence rate (16.6%) for in-
occur within a year of diagnosis in type 2 carried out in the community, clinic, or dividuals with insulin-dependent diabe-
diabetes patients and within two years in tertiary referral center. The variance tes (39).
type 1diabetes patients (5). Because of its among prevalence studies also reflects the Additional studies suggest that the
association with a variety of adverse out- type and number of tests performed and prevalence of DAN may be even more
comes including cardiovascular deaths, the presence or absence of signs and common than these studies report. For
cardiovascular autonomic neuropathy symptoms of autonomic neuropathy. example, using a variety of simple, vali-
(CAN) is the most clinically important Other factors that account for the marked dated, and noninvasive tests (e.g., fall in
and well-studied form of DAN. The in- variability in reported prevalence rates in- systolic blood pressure and heart rate re-
troduction over 20 years ago of simple, clude the lack of a standard accepted def- sponse after standing), Verrotti et al. (40)
noninvasive tests of cardiovascular auto- inition of DAN, different diagnostic found that 47 of 110 diabetic children
nomic function has supported extensive methods, variable study selection criteria, and adolescents showed one or more ab-
clinical and epidemiologic investigation and referral bias (24). Additional compli- normal tests for cardiovascular auto-
of CAN. These data form the strongest body cating factors include the wide variety of nomic dysfunction. These results,
of evidence for the importance of detect- clinical syndromes and confounding vari- however, recapitulate that prevalence
ing and monitoring impaired autonomic ables such as age, sex, duration of diabe- rates will vary depending on 1) different
function in patients with diabetes (6,7). tes, glycemic control, diabetes type, patient cohorts studied, 2) varied testing
height, and other factors. Table 1 reveals modalities utilized, and 3) different crite-
PATHOGENESIS OF DAN the prevalence rates of CAN for several ria used to define autonomic dysfunction.
Hypotheses concerning the multiple eti- different studies, again indicating the dra-
ologies of diabetic neuropathy include a matic variability from a low of 7.7% for
metabolic insult to nerve fibers, neurovas- newly diagnosed patients with type 1 di- CLINICAL MANIFESTATIONS
cular insufficiency, autoimmune damage, abetes, when strict criteria to define CAN OF DAN
and neurohormonal growth factor defi- were used (24), to a high of 90% in poten- The metabolic disorders of diabetes lead
ciency (8). Several different factors have tial recipients of a pancreas transplant (25). to diffuse and widespread damage of pe-
been implicated in this pathogenic pro- To address issues in comparing data ripheral nerves and small vessels. Clinical
cess. Hyperglycemic activation of the from different sources, the 1988 San An- manifestations of autonomic dysfunction
polyol pathway leading to accumulation tonio Conference on Diabetic Neuropa- and other microvascular complications
of sorbitol and potential changes in the thy recommended that each laboratory frequently occur concurrently but in in-
NAD:NADH ratio may cause direct neu- should standardize the objective mea- consistent patterns (41). The ubiquitous
ronal damage and/or decreased nerve sures using their own population norms, distribution of the ANS renders virtually
blood flow (9 –11). Activation of protein reporting both absolute data and the rela- all organs susceptible to autonomic dys-
kinase C induces vasoconstriction and re- tionship of the data to the appropriate function. Therefore, a patient diagnosed
duces neuronal blood flow (11). In- normative control population. Subse- with diabetes should be suspected of hav-
creased oxidative stress, with increased quently, a number of studies have been ing at least subclinical disturbances of the
free radical production, causes vascular conducted to assess the prevalence of ANS. Overt signs and symptoms of auto-
endothelium damage and reduces nitric DAN in defined populations. nomic disease fall into one or more of the
oxide bioavailability (12,13). Alternately, For example, in a community-based following categories.
excess nitric oxide production may result population study of diabetic neuropathy
in formation of peroxynitrite and damage in Oxford, England, the prevalence of au- Cardiovascular
endothelium and neurons, a process re- tonomic neuropathy as defined by one or ● Resting tachycardia
ferred to as nitrosative stress (14,15). In a more abnormal heart rate variability ● Exercise intolerance
1554 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
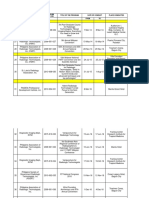
Table 1—Reported prevalence of CAN
Date of Subjects %
Author publication Diabetes type (n) Test(s) used Abnormal
Sharpey-Schafer and 1960 337 Valsalva maneuver 21
Taylor (26)
Ewing et al. (27) 1974 Mixed with autonomic symptoms 124 Handgrip test 18
Morley et al. (28) 1977 Adult diabetic patients 70 Valsalva maneuver 24
Heart rate variation 11
Hilsted and Jensen (29) 1979 Insulin-treated 126 Heart rate variation 40
Mackay et al. (30) 1980 287 Heart rate variation 30
Ewing et al. (31) 1980 Mixed with autonomic symptoms 73 Valsalva maneuver 47
Handgrip 35
Postural BP 45
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
Ewing et al. (32) 1980 Mixed with autonomic symptoms 61 Valsalva maneuver 54
Handgrip
Postural BP
Hulper and Willms (33) 1980 92 Handgrip 17
Dyrberg et al. (34) 1981 Insulin-dependent 75 Heart rate variation 27
Valsalva maneuver 17
Lying-to-standing 0
Xueli et al. (35) 1981 Newly diagnosed non-insulin-dependent Valsalva maneuver 80
O’Brien et al. (36) 1991 Insulin-dependent 506 At least two of the following: heart rate 17
variation in response to 1) rest 2)
single deep breath 3) Valsalva
maneuver or 4) standing
Ziegler et al. (24) 1992 Newly diagnosed insulin-dependent 130 At least three of the following: CV of 7.7
heart rate variation, low-and mid-
frequency bands of spectral analysis,
MCR, Valsalva maneuver, or lying-
to-standing
Ziegler et al. (24) 1992 Insulin-dependent 647 Greater than two of the following: 25.3
coefficient of variation of heart
rate variation, low- and mid-
Non-insulin-dependent 524 frequency bands of spectral analysis, 34.3
MCR, Valsalva maneuver, or lying-
to-standing
Kennedy et al. (25) 1995 Insulin-dependent 290 Heart rate variation 90
Valsalva maneuver 88
DCCT Research 1998 Insulin-dependent primary cohort 1,441 Heart rate variation 1.6–6.2
Group (37) 1–5 years’ duration; secondary Valsalva maneuver 5.5–6.3
cohort 1–15 years’ duration Postural BP 1.1
Any abnormality 2.6–23
BP, blood pressure; MCR, mean circular resultant.
● Orthostatic hypotension ● Retrograde ejaculation Pupillary
● Silent myocardial ischemia ● Female sexual dysfunction (e.g., loss of ● Pupillomotor function impairment
vaginal lubrication) (e.g., decreased diameter of dark-
GI adapted pupil)
● Esophageal dysmotility ● Argyll-Robertson pupil
● Gastroparesis diabeticorum
Metabolic
● Hypoglycemia unawareness
● Constipation
● Hypoglycemia-associated autonomic
● Diarrhea The differential diagnosis of DAN in-
● Fecal incontinence
failure
volves excluding the following condi-
tions:
Sudomotor
Genitourinary ● Anhidrosis
● Neurogenic bladder (diabetic cystopa- ● Heat intolerance ● Pure autonomic failure (formerly called
thy) ● Gustatory sweating idiopathic orthostatic hypotension)
● Erectile dysfunction ● Dry skin ● Multiple system atrophy with auto-
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1555
Technical Review
nomic failure (formerly called Shy- (45). In a study of individuals with and change there is an increase in plasma nor-
Drager syndrome) without CAN, Kahn et al. (46) showed a epinephrine. For individuals with ortho-
● Addison’s disease and hypopituitarism reduced response in heart rate and blood static hypotension, there may be a
● Pheochromocytoma pressure during exercise in individuals reduction in this response relative to the
● Hypovolemia with CAN. Roy et al. (47) demonstrated a fall in blood pressure (53). Diminished
● Medications, with anticholinergic or decreased cardiac output in response to cardiac acceleration and cardiac output,
sympatholytic effects (insulin, vasodi- exercise in individuals with CAN. The se- particularly in association with exercise,
lators, sympathetic blockers) verity of CAN has also been shown to cor- may also be important in the presentation
● Peripheral autonomic neuropathies relate inversely with an increase in heart of this disorder (53,54). Less frequently,
(e.g., amyloid neuropathy, idiopathic rate at any time during exercise and with there is a rise in norepinephrine that may
autonomic neuropathy) the maximal increase in heart rate. It be due to low blood volume or reduced
should also be noted that decreased ejec- red cell mass (55,56). Frequently, there
DAN is typically assessed by focusing tion fraction, systolic dysfunction, and di- are fluctuations in the degree of ortho-
on symptoms or dysfunction attributable astolic filling limit exercise tolerance (1). static hypotension. This may reflect post-
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
to a specific organ system. CAN is the most Given the potential for impaired exercise prandial blood pooling, the hypotensive
prominent focus because of the life- tolerance, it has been suggested that dia- role of insulin, and changing patterns of
threatening consequences of this compli- betic patients who are likely to have CAN fluid retention due to renal failure or con-
cation and the availability of direct tests of have cardiac stress testing before under- gestive heart failure (57–59).
cardiovascular autonomic function. How- taking an exercise program (45). Patients with orthostatic hypotension
ever, neuropathies involving other organ Intraoperative cardiovascular lability. typically present with lightheadedness
systems should also be considered in the Hemodynamic changes occur during sur- and presyncopal symptoms. Symptoms
optimal care of patients with diabetes. gery for individuals with and without di- such as dizziness, weakness, fatigue, vi-
abetes. Burgos et al. (48) found that sual blurring, and neck pain also may be
CAN vasopressor support was needed more of- due to orthostatic hypotension. Many pa-
Perhaps one of the most overlooked of all ten in diabetic individuals with auto- tients, however, remain asymptomatic
serious complications of diabetes is CAN nomic dysfunction than in those without. despite significant falls in blood pressure
(42). CAN results from damage to the au- The normal autonomic response of vaso- (60). If the cause of orthostatic hypoten-
tonomic nerve fibers that innervate the constriction and tachycardia did not com- sion is CAN, treatment goals should not
heart and blood vessels and results in ab- pletely compensate for the vasodilating only consist of therapies to increase the
normalities in heart rate control and vas- effects of anesthesia. Kitamura et al. (49) standing blood pressure, balanced against
cular dynamics (43). Reduced heart rate also recently demonstrated an association preventing hypertension in the supine
variation is the earliest indicator of CAN between CAN and more severe intraoper- position (61), but should also provide ed-
(44). ative hypothermia. Complications arising ucation to patients so that they avoid sit-
In a review of several epidemiological from intraoperative hypothermia include uations (e.g., vasodilation from hot
studies among individuals diagnosed decreased drug metabolism and impaired showers) that result in the creation of
with diabetes, it was shown that the wound healing. Sobotka et al. (50) symptoms (i.e., syncopal episodes). Such
5-year mortality rate from this serious showed that some diabetic patients with symptoms can result in injuries from fall-
complication is five times higher for indi- autonomic neuropathy have a reduced ing. Cardiovascular autonomic function
viduals with CAN than for individuals hypoxic-induced ventilatory drive. These testing may help differentiate CAN from
without cardiovascular autonomic in- data suggest that preoperative cardiovas- other causes of weakness, lightheaded-
volvement (4). cular autonomic screening may provide ness, dizziness, or fatigue and promote
In this report, the clinical manifesta- useful information for anesthesiologists appropriate therapeutic intervention
tions (e.g., exercise intolerance, intraop- planning the anesthetic management of (62).
erative cardiovascular lability, orthostatic diabetic patients and identify those at Silent myocardial ischemia/cardiac de-
hypotension, and increased risk of mor- greater risk for intraoperative complica- nervation syndrome. The cause of silent
tality) of the presence of CAN will be dis- tions. myocardial ischemia in diabetic patients
cussed. It will also be shown that Orthostatic hypotension. Orthostatic is controversial. It is clear, however, that a
autonomic dysfunction can affect daily hypotension is defined as a fall in blood reduced appreciation for ischemic pain
activities of individuals with diabetes and pressure (i.e., ⬎20 mmHg for systolic or can impair timely recognition of myocar-
may invoke potentially life-threatening ⬎10 mmHg for diastolic blood pressure) dial ischemia or infarction and thereby
outcomes. Advances in technology, built in response to postural change, from su- delay appropriate therapy. Table 2 and
on decades of research and clinical test- pine to standing (51). In patients with di- Fig. 1A summarize the results of 12 cross-
ing, now make it possible to objectively abetes, orthostatic hypotension is usually sectional studies, comparing the presence
identify early stages of CAN with the use due to damage to the efferent sympathetic of silent myocardial ischemia, generally
of careful measurement of autonomic vasomotor fibers, particularly in the measured by exercise stress testing be-
function. splanchnic vasculature (52). In addition, tween diabetic individuals with and with-
there is a decrease in cutaneous, splanch- out CAN.
Clinical manifestations of CAN nic, and total vascular resistance that oc- Of the 12 studies, 5 showed a statis-
Exercise intolerance. Autonomic dys- curs in the pathogenesis of this disorder. tically significant increased frequency of
function can impair exercise tolerance Normally, in response to postural silent myocardial ischemia in individuals
1556 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
Table 2—Studies of CAN and silent myocardial ischemia
% %
Tests of autonomic function Definition of CAN SMI⫹/CAN⫹ SMI⫹/CAN⫺ Notes
Reference
Niakan et al. (63) 1. Valsalva maneuver Abnormal Valsalva ratio 20% (5/25) 4% (2/48)* All subjects had symptom-
atic peripheral neuropa-
thy. Outcome was silent
myocardial infarction
Hume et al. (64) 1. HRV during deep breathing At least two of three were 36% (5/14) 20% (9/46) Asymptomatic middle-
2. Valsalva maneuver abnormal aged men, no symptoms
3. 30:15 ratio or signs of heart disease
Murray et al. (65) 1. HRV during deep breathing At least two of the first three 72% (13/18) 42% (5/12) Patients with known or
2. Valsalva maneuver tests ⫽ mild CAN suspect CAD
3. 30:15 ratio
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
4. BP response to standing
5. BP response to handgrip
Langer et al. (66) 1. HRV during deep breathing At least two of the tests were 38% (8/21) 5% (2/37)† Men only, no clinical evi-
2. Valsalva maneuver abnormal dence of CAD
3. 30:15 ratio
4. sBP response to standing
5. dBP response to handgrip
O’Sullivan et al. (67) 1. HRV during deep breathing At least two abnormal para- 65% (11/17) 4% (1/24)‡ Men ⬎40 years old. One-
2. Valsalva maneuver sympathetic function tests half of patients with
3. 30:15 ratio known or suspected
4. sBP response to standing CAD
5. dBP response to handgrip
Koistinen et al. (68) 1. HRV during deep breathing Both HRV during deep 38% (3/8) 38% (11/29) Patients with known CAD
2. 30:15 ratio breathing and 30:15 ratio
3. BP response to standing were abnormal
Hartmann et al. (69) 1. HRV at rest over 5 min Authors did not indicate 82% (9/11) 40% (4/10) CAD confirmed by coro-
2. HRV during deep breathing whether only one or both nary angiography
tests were abnormal
Jermendy et al. (70) 1. HRV during deep breathing Results of parasympathetic 30% (11/37) 0% (0/26)† Diabetic subjects with lack
2. Valsalva maneuver tests (1,2,3) were scored 0 of symptoms of angina
3. 30:15 ratio ⫽ normal, 1 ⫽ borderline, pectoris and ⱖ1 addi-
4. BP response to standing 2 ⫽ abnormal. Those with tional CVD risk factor
a score of 0–1 ⫽ without
CAN, score of 2–3 ⫽ early
CAN, and score of 4–6 ⫽
definitive CAN.
Zarich et al. (71) 1. HRV during deep breathing Two or more abnormal test 100% (10/10) 67% (10/15) Subjects with known CAD
2. Valsalva maneuver results were classified as
3. sBP response to standing moderate to severe
4. dBP response to handgrip
MiSAD Group (72) 1. HRV during deep breathing Autonomic neuropathy score 7% (13/175) 6% (46/750) Asymptomatic men and
2. HRV from lying to standing ⱖ3 women aged 40–65
3. Orthostatic hypotension years with no prior his-
tory of CAD
Jalal et al. (73) 1. HRV during deep breathing Normal ⫽ all tests normal or 40% (12/30) 10% (3/30)† Subjects with history of
2. Valsalva maneuver one borderline; Early ⫽ CAD were excluded.
3. 30:15 ratio one of the three heart rate CAN⫺ subjects age- and
4. BP response to standing tests abnormal or two bor- sex-matched to CAN⫹
5. BP response to handgrip derline; Definite ⫽ ⱖtwo subjects
heart rate tests abnormal;
severe ⫽ ⱖtwo heart rate
tests abnormal plus one or
both BP tests abnormal
Valensi et al. (74) 1. HRV during deep breathing Not indicated 30% (10/33) 36% (15/42) Subjects asymptomatic for
2. Valsalva maneuver CAD, but had diabetes
3. 30:15 ratio and ⱖ2 additional CVD
risk factors
Total§ 110/399 108/1,069
BP, blood pressure; CAD, coronary artery disease; dBP, diastolic blood pressure; sBP, systolic blood pressure; SMI, silent myocardial ischemia. *P ⬍ 0.05; †P ⬍
0.001; §Mantel-Haenszel estimate for the pooled rate ratio for silent myocardial ischemia ⫽ 1.96 (95% CI: 1.53–2.51, P ⬍ 0.001).
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1557
Technical Review
lar function and severity of coronary ar-
tery disease as assessed by coronary
angiography and ventriculography. The
following autonomic function tests were
included: heart rate variation during deep
breathing (beats/min), 30:15 ratio, Val-
salva maneuver, blood pressure response
to standing, and blood pressure response
to sustained handgrip. All 52 individuals
manifested ischemia during exercise. A
total of 16 individuals did not experience
angina, and 10 of these had diabetes.
Comparing the silent ischemia group
(n ⫽ 16) with the group who did experi-
ence angina (n ⫽ 36) revealed impaired
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
autonomic function in the silent ischemia
group, with statistically lower 30:15 ra-
tios. In subgroup analysis, the impaired
autonomic function was found to be con-
fined to just the diabetic individuals and
not seen in the nondiabetic individuals
with silent myocardial ischemia, thus in-
dicating that subclinical autonomic neu-
ropathy is associated with silent ischemia
in individuals with diabetes (76). Hikita
et al. (77), using 24-h ambulatory electro-
cardiographic recordings, demonstrated
that HRV is reduced in diabetic patients
with silent ischemia when compared with
nondiabetic individuals with silent or
Figure 1— Association of CAN and silent myocardial infarction (SMI) in 12 studies. A: ⫹CAN, painful ischemia. Some investigators,
CAN present; ⫺CAN, no CAN found; ⫹SMI, SMI present. B: Prevalence rate ratios and 95% CIs however, have questioned whether the
for association between CAN and SMI from the 12 studies. association between CAN and silent myo-
cardial ischemia is a causal one (79), sug-
with CAN compared with individuals dence for an association. For example, gesting instead that underlying coronary
without CAN. The point estimates for the Ambepityia et al. (75) measured the angi- artery disease might be a cause of both
prevalence rate ratios in these 12 studies nal perceptual threshold (i.e., the time autonomic dysfunction and silent myo-
ranged from 0.85 to 15.53 (Fig. 1B). The from onset of 0.1 mV ST depression to the cardial ischemia (80).
prevalence rate ratio was ⬎1 in 10 of the onset of angina pectoris during exercise) The presence of CAN does not ex-
12 studies, and in 4 of these, the lower in individuals with and without diabetes. clude painful myocardial infarction (MI)
limit of the 95% CI was ⬎1. Via meta- The influence of autonomic function was among individuals with diabetes (81).
analysis, the Mantel-Haenszel estimate for assessed via heart rate variation during Chest pain in any location in a patient
the pooled prevalence rate risk for silent deep breathing (beats/min), Valsalva ma- with diabetes should be considered to be
myocardial ischemia was 1.96, with a neuver, 30:15 ratio, and blood pressure of myocardial origin until proven other-
95% CI of 1.53–2.51 (P ⬍ 0.001; n ⫽ response to standing. The perception of wise; but, of equal importance, unex-
1,468 total subjects). These data demon- angina was severely impaired in the dia- plained fatigue, confusion, tiredness,
strate a consistent association between betic patients, allowing these individuals edema, hemoptysis, nausea and vomiting,
CAN and the presence of silent myocar- to exercise longer after the onset of myo- diaphoresis, arrhythmias, cough, or dys-
dial ischemia. cardial ischemia. The delay in perception pnea should alert the clinician to the pos-
There are several additional pub- of angina was associated with the pres- sibility of silent MI (1).
lished studies that have examined the ence of cardiovascular autonomic dys-
relationship between autonomic dysfunc- function. The investigators suggested that Increased risk of mortality
tion and silent myocardial ischemia in di- the neuropathic damage to the myocar- Table 3 summarizes investigations that
abetic individuals but that are not dial sensory afferent fibers in the auto- have examined the association of auto-
included in the meta-analysis because the nomic nerve supply reduced the diabetic nomic dysfunction and mortality. These
raw numbers of case and control subjects individual’s sensitivity to regional isch- studies have consistently provided evi-
among individuals with and without car- emia by interrupting pain transmission dence for an increased mortality risk
diovascular autonomic dysfunction were (75). A study by Marchant et al. (76) ex- among diabetic individuals with CAN
not presented (75–78). However, virtu- amined 22 diabetic and 30 nondiabetic compared with individuals without CAN
ally all of these studies also provide evi- individuals who had similar left ventricu- (Table 3).
1558 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
Table 3—Studies of CAN and mortality
Follow-up Tests of autonomic Definition of % Mortality/ % Mortality/
(years) function CAN CAN⫹ CAN⫺ Notes
Reference
Ewing et al. (31) 5 1. Valsalva maneuver 53% (21/40) 15% (5/33)† Subjects who complained of
2. Handgrip symptoms suggestive of
3. Postural fall in BP autonomic neuropathy
comprised the study co-
hort. CAN⫹ subjects had
more complications at
baseline. Half of the
deaths for the CAN⫹ sub-
jects were attributed to
renal failure.
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
Sampson et al. (82) 10–15 1. HRV during deep Based on HRV and the pres- 27% (20/73) 11% (4/38) Mortality in asymptomatic
breathing ence or absence of symp- individuals with an iso-
2. Valsalva maneuver tomatic autonomic lated abnormality in au-
3. Heart rate and sBP neuropathy tonomic function tests
response to stand- was not increased. Excess
ing mortality was restricted
to those with symptom-
atic CAN (18/49 vs. 4/38).
O’Brien et al. (36) 5 HRV in response to Two or more of the four 27% (23/84) 8% (7/84)† Those with CAN had great-
1. supine rest tests were abnormal er prevalence of other
2. single deep breath complications, but in mul-
3. Valsalva maneuver tivariate analysis, CAN
4. standing for 60 s was the most important
predictor of mortality.
Ewing et al. (83) 3 1. HRV during deep Normal ⫽ all tests normal 31% (10/32) 8% (3/39)* Included men ⬍60 years
breathing or one borderline; early old. CAN⫹ subjects who
2. Valsalva maneuver ⫽ one of the three heart died (n ⫽ 10) had longer
3. 30:15 ratio rate tests abnormal or QT intervals than those
4. BP response to two borderline; definite who did not.
standing ⫽ two or more of the
5. BP response to heart rate tests abnormal;
handgrip severe ⫽ at least two of
the heart rate tests abnor-
mal and one or both of
the BP tests abnormal or
both borderline
Jermendy et al. (84) 5 1. HRV during deep Results of parasympathetic 40% (12/30) 4% (1/23)† No patients had an abnor-
breathing tests (1,2,3) were scored mal sBP response to
2. Valsalva maneuver 0 ⫽ normal, 1 ⫽ border- standing. Deceased sub-
3. 30:15 ratio line, 2 ⫽ abnormal. jects were older and had
4. sBP response to Those with a score of 0–1 more complications at
standing ⫽ without CAN; score of baseline.
2–3 ⫽ early CAN; score
of 4–6 ⫽ definitive CAN.
Rathmann et al. (85) 8 1. Coefficient of vari- Both tests abnormal 23% (8/35) 3% (1/35)* Subjects with advanced re-
ation of R-R inter- nal disease, proliferative
vals with normal retinopathy, and CVD
respiration were excluded.
2. Coefficient of vari-
ation of R-R inter-
vals with deep
respiration
Hathaway et al. (86) 2–5 (case- 1. HRV during deep Both tests abnormal 31% (4/13) 0% (0/16)* Case-control study of trans-
control 2. Valsalva maneuver plant recipients (pancreas-
study) kidney or kidney alone).
Case subjects (n ⫽ 4)
died of sudden cardiac
death within 3.5 years
posttransplant. Control
subjects survived 2–5
years posttransplant.
Continued on following page
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1559
Technical Review
Table 3—Continued
Follow-up Tests of autonomic Definition of % Mortality/ % Mortality/
(years) function CAN CAN⫹ CAN⫺ Notes
Orchard et al. (87) 2 1. HRV during deep Abnormal E:I ratio 9% (8/88) 2% (9/399)† Relative risk decreased from
breathing 4.03 to 1.37 after con-
troling for duration, renal
disease, hypertension,
and coronary heart dis-
ease.
Sawicki et al. (88) 5–13 1. R-R variation be- R-Rsupine/R-Rstanding 62% (16/26) 29% (17/59)† All subjects with overt dia-
tween supine and ⬍1.03 betic nephropathy
standing position
Navarro et al. (89) 1–11.5 1. HRV during deep Both tests abnormal 28% (101/359) 5% (6/128)‡ All subjects were candidates
breathing for pancreas transplanta-
2. Valsalva maneuver tion.
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
Toyry et al. (90) 10 1. HRV during deep Parasympathetic neu- 50% (3/6) 17% (20/116) Mortality rates for CVD
breathing ropathy ⫽ abnormal mortality only. Subjects
2. sBP decrease dur- E:I ratio were newly diagnosed
ing standing with diabetes. In multi-
variate analysis, sympa-
thetic CAN⫹ at 5-year,
follow-up predicted CVD
mortality at 10-year, fol-
low-up even after adjust-
ing for conventional CVD
risk factors.
Sawicki et al. (91) 15–16 1. R-R variation be- R-Rsupine/R-Rstanding 69% (58/84) 76% (100/132) Consecutive patients (31%
tween supine and ⬍1.03 male) enrolled over a
standing position 2-year period for im-
provement in metabolic
control.
Veglio et al. (92) 5 1. Heart rate (rest- Two or more of the tests 13% (10/75) 4% (10/241)† QTc prolongation was asso-
ing) abnormal ciated with increased
2. HRV during deep mortality risk.
breathing
3. BP response to
standing
Gerritsen et al. (93) 0.5–9.2 1. E:I difference Not NotRelative risk ⫽ 2.25 (1.13–
available available
4.45); diabetic subjects
(n ⫽ 159) identified
through a population
survey
Chen et al. (94) 7.7 HRV in response to Unique diagnostic crite- 29% (106/371) 12% (29/241)‡ CAN⫹ associated with in-
1. single deep breath ria defined by scoring creased mortality even in
2. six consecutive 3 or more the absence of postural
breaths hypotension
3. supine to standing
4. Valsalva maneuver
BP change sitting
to standing
Total§ 400/1,316 212/1,584
BP, blood pressure; CVD, cardiovascular disease; E:I difference ⫽ mean expiration to inspiration difference in R-R intervals over six consecutive breaths; R-R interval,
time interval between successive ECG R-waves; sBP, systolic blood pressure. *P ⬍ 0.05; †P ⬍ 0.01; ‡P ⬍ 0.001; §Mantel-Haenszel estimate for the pooled relative
risk for mortality ⫽ 2.14 (95% CI 1.83–2.51, P ⬍ 0.0001). Adapted from Maser et al. (94a).
Ewing et al. (31) reported a 2.5-year failure, and 29% were from sudden death. athy compared with an 8% mortality rate
mortality rate of 27.5% that increased to This study also revealed that symptoms of in diabetic subjects with normal auto-
53% after 5 years in diabetic patients with autonomic neuropathy, especially post- nomic function tests. Among individuals
abnormal autonomic function tests com- ural hypotension, and gastric symptoms who died, there was no difference in du-
pared with a mortality rate of only 15% in the presence of abnormal autonomic ration of diabetes between those with and
over the 5-year period among diabetic pa- function tests carried a particularly poor without autonomic neuropathy. As was
tients with normal autonomic function prognosis. true for the study performed by Ewing et
test results. It should be noted that half of A study by O’Brien (36) reported al. (31); a significant number of the deaths
the deaths in individuals with abnormal 5-year mortality rates of 27% in patients (10/23) of the neuropathic patients were
autonomic function tests were from renal having asymptomatic autonomic neurop- attributable to renal failure. O’Brien et al.,
1560 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
Table 4—Discriminant analysis of 5-year survival in type 1 diabetic patients follow-up intervals in these studies
ranged from 1 to 16 years. In all 15 stud-
Variable Change in Rao’s V Significance ies, the baseline assessment for cardiovas-
cular autonomic function was made on
Autonomic neuropathy 44.8 0.0001
the basis of one or more of the tests de-
Systolic blood pressure 18.1 0.0001
scribed by Ewing et al. (95). Total mortal-
Foot disease 13.4 0.0002
ity rates were higher in subjects with CAN
BMI 3.1 0.08
at baseline than in subjects whose base-
Peripheral sensorimotor neuropathy 3.5 0.06
line assessment was normal, with statisti-
Proteinuria 2.6 0.1
cally significant differences in 11 of the
Macrovascular disease 1.9 0.2
studies. The study-specific relative risks
Duration of diabetes — —
ranged from 0.91 for the study by Sawicki
Retinopathy — —
et al. (91) to 9.20 for the study by Jer-
Smoking — —
mendy et al. (84). Figure 2B shows the
Duration of diabetes, retinopathy, and smoking were not found to be significant predictors of death. Adapted
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
from O’Brien et al. (36).
relative risks and 95% CIs for each study,
as well as the pooled risk estimate esti-
mated by the Mantel-Haenszel procedure.
however, compared the relative impor- jects revealed a fourfold higher mortality The pooled estimate of the relative risk,
tance of various factors associated with rate in individuals with CAN at baseline based on 2,900 total subjects, was 2.14,
mortality by discriminate analysis of sur- compared with individuals without. with a 95% CI of 1.83–2.51 (P ⬍ 0.0001).
vivors and nonsurvivors using Rao’s step- However, after adjusting for baseline dif-
wise selection method and revealed that ferences between individuals with and Association of CAN with major
autonomic neuropathy was more of an in- without CAN for markers related to renal cardiovascular events
dependent predictive factor than systolic and cardiovascular disease, the relative The relationship between CAN and major
blood pressure, foot disease, BMI, sensory risk decreased from 4.03 to 1.37 and was cardiovascular events has been assessed
neuropathy, proteinuria, and macrovas- no longer statistically significant. in two prospective studies. Specifically,
cular disease (36) (Table 4). Another population-based study (the the relationship between baseline CAN
Rathmann et al. (85) reported the re- Hoorn study) examined 159 individuals and the subsequent incidence of a fatal or
sults of a study designed to assess the risk with type 2 diabetes (85 had newly diag- nonfatal cardiovascular event, defined as
of mortality due to CAN among patients nosed diabetes) who were followed for an an MI, heart failure, resuscitation from
with CAN but without a clinical manifes- average of nearly 8 years. All-cause as well ventricular tachycardia or fibrillation, an-
tation of severe complications (protein- as cardiovascular mortality were found to gina, or the need for coronary revascular-
uria, proliferative retinopathy, coronary be associated with impaired autonomic ization, was examined (64,74). The
artery disease, or stroke) 8 years after their function in this study. In addition, the in- relative risks associated with CAN in
first clinical examination. The mortality of vestigators suggested that cardiovascular these studies were 2.2 and 3.4, respec-
diabetic patients with CAN increased autonomic dysfunction in individuals al- tively, with the latter result just achieving
steadily over the 8-year period (6% after 2 ready at high risk (e.g., those with diabe- statistical significance (P ⬍ 0.05). It
years, 14% after 4 years, 17% after 6 tes, high blood pressure, or a history of would appear, therefore, that there is an
years, and 23% after 8 years) compared cardiovascular disease) may be particu- association between CAN and major car-
with an age-, sex-, and duration of diabe- larly hazardous (93). diovascular events, but given the small
tes–matched control group where there number of events that occurred in each of
was one death. Autonomic dysfunction Meta-analysis of the relationship these studies, more follow-up studies are
was found to be an independent risk fac- between CAN and mortality required.
tor with poor prognosis. Some autonomic As noted above, the relationship of CAN
neuropathic symptoms (orthostatic hy- and mortality in diabetic individuals has Potential reasons for the increased
potension, gastroparesis, gustatory sweat- been evaluated in a number of studies on mortality rate associated with CAN
ing, and erectile impotence) were found an individual basis. Analysis of each of Despite the increased association with
more frequently among subjects who these studies as a single entity, however, mortality, the causative relationship be-
died (85). only includes a limited number of sub- tween CAN and the increased risk of
Two separate population-based stud- jects. Thus, in this section, results were mortality has not been conclusively estab-
ies have also examined the association of pooled from a number of studies into a lished. Several mechanisms have been
CAN and mortality. Orchard et al. (87) meta-analysis for the purpose of obtain- suggested including a relationship with
studied a population-based sample of in- ing more precise estimates. Studies were autonomic control of respiratory func-
dividuals with type 1 diabetes. Individu- included in this meta-analysis if they were tion. Page and Watkins (96) reported 12
als for this study were identified through a based on diabetic individuals, included a cardiorespiratory arrests in eight diabetic
hospital-based registry system and were baseline assessment of HRV, and included individuals with severe autonomic neu-
considered to be representative of all type a mortality follow-up (94a). ropathy and suggested that diabetic indi-
1 diabetic patients residing in Allegheny Table 3 and Fig. 2A summarize the viduals with CAN have impaired
County, Pennsylvania. Initial analyses results from 15 different studies that have respiratory responses to conditions of
based on a 2-year follow-up of 487 sub- included a follow-up of mortality. The hypoxia and may be particularly suscep-
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1561
Technical Review
ute to the marked increase in cardiovas-
cular mortality. Diabetic patients with
CAN are predisposed to a lack of the nor-
mal nighttime decrease in blood pressure
because of an increased prevalence of
sympathetic activity (100). A disturbed
circadian pattern of sympathovagal activ-
ity with prevalent nocturnal sympathetic
activity combined with higher blood
pressure values during the night and in-
creased left ventricular hypertrophy
could represent another important link
between CAN and an increased risk of
mortality.
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
CAN and sudden death
A number of researchers have reported
sudden unexpected deaths among sub-
jects identified with autonomic neuropa-
thy (31,82,85). One potential cause of
sudden death may be explained by severe
but asymptomatic ischemia, eventually
inducing lethal arrhythmias (85). An
autonomic imbalance resulting in QT
prolongation may also predispose indi-
viduals to life-threatening cardiac ar-
rhythmias and sudden death (101).
Results from the EURODIAB IDDM Com-
plications Study showed that male pa-
tients with impaired HRV had a higher
corrected QT prolongation than males
Figure 2—Relative risks and 95% CIs for association between CAN and mortality in 15 studies. without this complication (102). Imaging
A: Association of CAN and mortality in 15 studies. ⫹CAN, CAN present; ⫺CAN, no CAN found. of myocardial sympathetic innervation
B: Log relative risks from the 15 studies. with various radiotracers (e.g., meta-
iodobenzylguanidine) has shown that
tible to medications that depress the res- diabetic glomerulopathy by mechanisms predisposition to arrhythmias and an as-
piration system. An impaired ability to not completely understood (36). A conse- sociation with mortality may also be re-
recognize hypoglycemia and impaired re- quential increase in cardiovascular risk lated to intracardiac sympathetic
covery from hypoglycemic episodes due experienced by individuals with ne- imbalance (103,104).
to defective endocrine counterregulatory phropathy has also been noted. In one The significance of CAN as an in-
mechanisms are also potential reasons for study of type 1 diabetic individuals, hy- dependent cause of sudden death has,
death (36). Other investigators have pertension along with LDL and HDL cho- however, been recently questioned (105).
noted explanations for the high mortality lesterol concentrations were found to be In the Rochester Diabetic Neuropathy
rate as an interaction with other concom- independent correlates of CAN (97). Study, the investigators found that all case
itant disorders that also carry high risks of These results suggested that a disturbed subjects (individuals with and without di-
mortality. Clarke et al. (7) speculated that cardiovascular risk profile seen in indi- abetes) with sudden death had severe cor-
the increased mortality found for patients viduals with nephropathy might lead to onary artery disease or left ventricular
with clinical symptoms of autonomic both cardiovascular disease and CAN. dysfunction. Therefore, they suggested
neuropathy were due to both a direct ef- Other investigators have also shown inde- that although CAN could be a contribut-
fect of the autonomic neuropathy itself pendent associations of autonomic dys- ing factor, it was not a significant inde-
and an indirect, but parallel, association function with markers of cardiovascular pendent cause of sudden death. Heart
with accelerating microvascular compli- risk (e.g., elevated blood pressure [98], failure is, however, common in individu-
cations. O’Brien et al. (36) suggested that body weight, glycosylated hemoglobin, als with diabetes, identified by the pres-
the high rate of mortality due to end-stage and overt albuminuria [99]). Long-term ence of neuropathy, even in individuals
renal disease among diabetic patients follow-up studies are needed to distin- without evidence of coronary artery dis-
with autonomic neuropathy may have guish the exact roles of cardiovascular risk ease or left ventricular dysfunction (106).
been due to the parallel development of factors, nephropathy, and CAN in the eti- The association of cardiovascular auto-
late-stage neuropathy and nephropathy. ology of cardiovascular disease. Nonethe- nomic dysfunction in the absence of cor-
The presence of autonomic neuropathy less, CAN cosegregates with indexes of onary disease and cardiomyopathy
may accelerate the rate of progression of macrovascular risk, which may contrib- requires further study.
1562 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
Increased mortality after an MI the parasympathetic nervous system (e.g., progress. This underscores the need for
Mortality rates after an MI are also higher heart rate response to deep breathing) are performance of quantitative autonomic
for diabetic patients than for nondiabetic typically abnormal before those responses function tests to identify individuals at
patients (107). This may be due to auto- that are mediated by the sympathetic risk for premature death (121).
nomic insufficiency, increasing the ten- nerves. Although one might speculate ● Type 1 and type 2 diabetes may have
dency for development of ventricular then that parasympathetic damage occurs different progression paths.
arrhythmia and cardiovascular events af- before sympathetic damage, this may not ● The relationship between autonomic
ter infarction. Fava et al. (108) showed always be true. The increased frequency damage and duration of diabetes is not
that the presence of autonomic neuropa- of abnormalities detected via tests of the clear although numerous studies sup-
thy contributed to a poor outcome in a parasympathetic system may merely be a port an association (116).
study of 196 post-MI diabetic patients. In reflection of the test (e.g., sensitivity) and ● Prevalence and mortality rates may be
another study, Katz et al. (109) showed not of the natural history of nerve fiber higher among individuals with type 2
that a simple bedside test that measured damage (111). Thus, it may be better to diabetes, potentially due in part to
1-min HRV during deep breathing was a describe the natural history of autonomic longer duration of glycemic abnormal-
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
good predictor of all-cause mortality for dysfunction as developing from early to ities before diagnosis.
185 patients (17.8% with diabetes) after a more severe involvement rather than to
first MI. These investigators also sug- anticipate a sequence of parasympathetic OTHER AUTONOMIC
gested that cardiovascular autonomic to sympathetic damage (111). NEUROPATHIES
function testing provided a predictive Although much remains to be learned
value that could be used to identify a sub- about the natural history of CAN, previ- GI autonomic neuropathy
group of patients after an MI who are a ous reports can be coalesced into a few GI symptoms are relatively common
high risk for cardiovascular death (109). observations that provide some insight among patients with diabetes and often
Dysfunction of the ANS is associated with regard to progression of autonomic reflect diabetic GI autonomic neuropathy
with increased risk of mortality in indi- dysfunction: (7,122). It should be noted, however, that
viduals with diabetes. It is true, however, although GI symptoms are common,
that at least some of the association be- ● It can be detected at the time of diagno- symptoms may be more likely due to
tween CAN and mortality appears to be sis (24,44,112). other factors than to autonomic dysfunc-
due to an increased prevalence of other ● Neither age nor type of diabetes are lim- tion. GI manifestations of DAN are di-
complications in individuals with CAN. iting factors in its emergence, being verse, and symptoms and pathogenic
Though the exact pathogenic mechanism found in young individuals with newly mechanisms have been categorized ac-
is unclear, it is realized that some deaths diagnosed type 1 diabetes and older in- cording to which section of the GI tract is
may be avoidable through early identifi- dividuals newly diagnosed with type 2 affected:
cation of these higher-risk patients and by diabetes (5,24,40,44,113,114).
slowing, with therapy, the progression of ● Poor glycemic control plays a central ● Esophageal enteropathy (disordered
autonomic dysfunction and its associated role in development and progression peristalsis, abnormal lower esophageal
conditions. In addition, it would appear (44,115–117). sphincter function)
that autonomic function testing is a valu- ● Intensive therapy can slow the progres- ● Gastroparesis diabeticorum (nonob-
able tool in identifying a subgroup of sion and delay the appearance of abnor- structive impairment of gastric propul-
post-MI patients who are at high risk for mal autonomic function tests (37). sive activity; brady/tachygastria,
death. ● Subclinical autonomic neuropathy can pylorospasm)
be detected early using autonomic ● Diarrhea (impaired motility of the small
Association of cerebrovascular function tests (26,41,44). bowel [bacterial overgrowth syn-
disease and CAN ● Autonomic features that are associated drome], increased motility and secre-
The frequency of ischemic cerebrovascu- with sympathetic nervous system dys- tory activity [pseudocholeretic diarrhea])
lar events is increased in individuals with function (e.g., orthostatic hypotension) ● Constipation (dysfunction of intrinsic
type 2 diabetes. The impact of autonomic are relatively late complications of dia- and extrinsic intestinal neurons, de-
dysfunction on the risk of the develop- betes (31,41,116,118 –120). creased or absent gastrocolic reflex)
ment of strokes was examined by Toyry et ● There is an association between CAN ● Fecal incontinence (abnormal internal
al. (110), who followed a group of 133 and diabetic nephropathy that contrib- anal sphincter tone, impaired rectal
type 2 diabetic patients for 10 years. Dur- utes to high mortality rates (31,44,82). sensation, abnormal external sphincter)
ing the study period, 19 individuals had ● Gallbladder atony and enlargement
one or more strokes. Abnormalities of Even with consensus regarding these
parasympathetic and sympathetic auto- general observations, much remains un- Esophageal dysfunction results at
nomic function were found to be inde- clear: least in part from vagal neuropathy (123);
pendent predictors of stroke in this symptoms include heartburn and dys-
cohort (110). ● Some individuals with symptoms asso- phagia for solids. Via the use of radioiso-
ciated with autonomic neuropathy die topic techniques that quantify gastric
Progression of CAN suddenly and unexpectedly (31,44,82). emptying, it appears that ⬃50% of pa-
Results of the cardiovascular autonomic ● Clinical signs and symptoms of auto- tients with longstanding diabetes have de-
function tests that are mediated mainly by nomic dysfunction do not always layed gastric emptying (gastroparesis)
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1563
Technical Review
(124). Gastric emptying largely depends are sensory abnormalities that result in marker for the development of general-
on vagus nerve function, which can be impaired bladder sensation, an elevated ized vascular disease and for premature
severely disrupted in diabetes. Gastropa- threshold for initiating the micturition re- demise from a myocardial infarct, and pe-
resis in diabetes is usually clinically silent, flex and an asymptomatic increase in nile failure may be a portent of upcoming,
although severe diabetic gastroparesis is bladder capacity and retention. and possible preventable, cardiovascular
one of the most debilitating of all diabetic The parasympathetic nerves that orig- events (138). ED etiology in diabetes is
GI complications. Major clinical features inate in the intermediolateral column of multifactorial, including neuropathy, vas-
of this disorder are early satiety, anorexia, sacral segments S2–S4 provide the major cular disease, metabolic control, nutri-
nausea, vomiting, epigastric discomfort, excitatory input to the urinary bladder. tion, endocrine disorders, psychogenic
and bloating. Episodes of nausea or vom- Activation of the muscarinic, cholinergic, factors, and anti-diabetes drugs. Retro-
iting may last days to months or occur in and postganglionic pelvic nerve fibers re- grade ejaculation into the bladder also oc-
cycles (125). sult in contraction of the urinary bladder. curs in diabetic males. ED should alert
Diarrhea is evident in 20% of diabetic When there is damage to the efferent physicians to perform cardiovascular
patients, particularly those with known parasympathetic fibers to the urinary evaluations for these patients.
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
DAN (1). Diarrhea is typically intermit- bladder, symptoms such as hesitancy in
tent, but bowel movements may occur 20 micturition, weak stream, and dribbling Sexual dysfunction in women
or more times per day with urgency, and ensue, with a reduction in detrusor activ- Females with diabetes may have de-
the stools are often watery. Bacterial over- ity (i.e., detrusor areflexia). This leads to creased sexual desire and increased pain
growth due to stasis of the bowel may incomplete bladder emptying, an in- during intercourse and are at risk of de-
contribute to diarrhea, in which case creased postvoid residual, decreased peak creased sexual arousal and inadequate lu-
broad-spectrum antibiotics (e.g., tetracy- urinary flow rate, bladder overdistention, brication (139).
cline and metronidazole) are useful. Indi- and urine retention. Finally, overflow in-
viduals with constipation may have less continence occurs because of denervation Anemia of autonomic dysfunction
than three bowel movements per week, of the external and internal sphincter It has been shown that type 1 diabetic
and these may alternate with diarrhea. (129,130). The somatic pudendal nerve individuals with early nephropathy and
Treatment of diarrhea with or without innervates the external sphincter, where- symptomatic autonomic neuropathy have
constipation should always involve the as the sympathetic hypogastric nerves inappropriately low levels of erythropoi-
use of a prokinetic agent rather than con- innervate the internal sphincter. Individ- etin for the severity of their anemia (140).
stipating agents that create vicious cycles uals with bladder dysfunction are predis- These individuals can, however, mount
of constipation and diarrhea (1). Fecal in- posed to the development of urinary tract an appropriate erythropoietin response to
continence due to poor sphincter tone infections, including pyelonephritis, moderate hypoxia. The mechanism that
(126) is common for individuals with di- which may accelerate or exacerbate renal underlies the erythropoietin-deficient
abetes (127) and may be associated with failure (131,132). anemia is unclear. Reduced sympathetic
severe paroxysmal diarrhea or constitute Urinary frequency is another com- stimulation of erythropoietin production
an independent disorder of anorectal dys- monly associated symptom of autonomic has been previously hypothesized as the
function. dysfunction of the genitourinary system. cause of ineffective erythropoiesis result-
Unfortunately, 37–50% of individuals ing in anemia (141).
Genitourinary autonomic with diabetes have symptoms of bladder
neuropathy dysfunction, and 43– 87% of individuals RELATIONSHIP OF
The neurogenic bladder, also called cys- with type 1 diabetes have physiological AUTONOMIC NEUROPATHY
topathy, may be due to DAN (62). An ex- evidence of bladder dysfunction (129, TO HYPOGLYCEMIA
amination of the neuroanatomy of the 133,134). RESPONSIVENESS
genitourinary system provides an insight
into the extent to which autonomic fibers Erectile dysfunction Hypoglycemic unawareness and
are involved with its proper control. Serv- Erectile dysfunction (ED) is the most DAN
ing as a receptacle for the storage and ap- common form of organic sexual dysfunc- DAN plausibly could cause or contribute
propriate evacuation of urine, the urinary tion in males with diabetes, with an inci- to hypoglycemia unawareness, but this
bladder comprises three layers of inter- dence estimated to be between 35 and relationship is complex. Two groups con-
digitating smooth muscle (i.e., detrusor 75% (135). ED is defined as the consistent cluded that unawareness of hypoglycemia
muscle). This muscle forms an internal inability to attain and maintain an erec- and inadequate counterregulation occur
sphincter at the junction of the bladder tion adequate for sexual intercourse, usu- independently of autonomic neuropathy.
neck and urethra, and although it is not ally qualified by being present for several Ryder et al. (142) noted “little evidence”
anatomically discrete, there is localized months and occurring at least half the of autonomic neuropathy in 12 diabetic
autonomic innervation so that it functions time. An estimated 20 –30 million men in patients with a history of unawareness of
as a physiological sphincter. Afferent the U.S. have ED (136). In a large cohort hypoglycemia and 7 patients with inade-
nerve impulses of bladder sensation and study of men 53–90 years old, a signifi- quate hypoglycemic counterregulation.
reflex bladder contraction are carried by cant association between diabetes (and They also observed no history of un-
sympathetic, parasympathetic, and so- duration of diabetes) and ED was found awareness of hypoglycemia in seven pa-
matic nerves to the spinal cord (128). The when comparing diabetic men with non- tients with clear evidence of autonomic
earliest bladder autonomic dysfunctions diabetic men of similar age (137). ED is a neuropathy, and in six of the seven, there
1564 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
was adequate hypoglycemic counterregu- 150). The presence of autonomic neurop- of motor nerve function and sensory
lation. Based on these findings, they sug- athy, however, further attenuates the nerve function deficits. The lack of inter-
gested that there was no causal relation epinephrine response to hypoglycemia in est in the development of such measures
between DAN and unawareness of hypo- diabetic subjects after recent hypoglyce- was partly due to the erroneous but com-
glycemia or inadequate hypoglycemic mic exposure (144 –146) in most, but not monly held view that autonomic neurop-
counterregulation (142). Hepburn et al. all, studies (148). Furthermore, individu- athy was only a small and relatively
(143) reported that 7 of 17 patients with als with abnormal autonomic function obscure contributor to the peripheral
absent awareness of hypoglycemia had no have a greater risk for severe hypoglyce- neuropathies affecting individuals with
evidence of autonomic dysfunction. mia (151). diabetes (116,118,120).
Based on these data, they suggested that In the early 1970s, Ewing et al. (95)
loss of hypoglycemia awareness is not in- RELATIONSHIP OF proposed five simple noninvasive cardio-
variably associated with abnormal cardio- AUTONOMIC NEUROPATHY vascular reflex tests (i.e., Valsalva maneu-
vascular autonomic function tests. TO TISSUE PERFUSION ver, heart rate response to deep breathing,
Careful examination of these studies Microvascular skin flow is under the con- heart rate response to standing up, blood
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
suggests, however, that the relationship trol of the ANS and is regulated by both pressure response to standing up, and
between autonomic neuropathy and hy- the central and peripheral components. blood pressure response to sustained
poglycemic unawareness may be more In diabetes, the rhythmic contraction of handgrip) that have been applied success-
complex than these reports suggest. Ry- arterioles and small arteries is disordered. fully by many. The clinical literature has
der et al. observed that patients with au- Microvascular insufficiency may be a consistently identified these five tests as
tonomic neuropathy had a negligible cause of diabetic neuropathy (152). Mi- they have been widely used in a variety of
plasma pancreatic polypeptide response crovascular blood flow can be accurately studies. The tests are valid as specific
(3.7 pmol/l), and this response was also measured noninvasively using laser markers of autonomic neuropathy if end-
blunted in the patients with inadequate Doppler flowmetry. Defective blood flow organ failure has been carefully ruled
hypoglycemic counterregulation (72.4 in the small capillary circulation is found out and other potential factors such as
pmol/l) compared with that of the control with decreased responsiveness to mental concomitant illness, drug use (including
subjects (414 pmol/l; P ⬍ 0.05) (142). arithmetic, cold pressor, handgrip, and antidepressants, over-the-counter anti-
Furthermore, 10 of 17 individuals with heating. The defect is associated with a histamines and cough/cold preparations,
hypoglycemia unawareness reported by reduction in the amplitude of vasomotion diuretics, and aspirin), lifestyle issues
Hepburn et al. had evidence of autonomic and resembles premature aging (153). (such as exercise, smoking, and caffeine
dysfunction (145). Taken together, even There are differences in the glabrous and intake), and age are taken into account. A
these data suggest that there is some over- hairy skin circulations. In hairy skin, a large body of evidence indicates that these
lap between the features of autonomic functional defect is found before the de- factors can, to various degrees, affect the
neuropathy and hypoglycemic unaware- velopment of neuropathy (154). The clin- cardiovascular ANS and potentially other
ness. More recent data suggest that the ical counterpart is dry skin, loss of autonomic organ systems (157).
presence of autonomic neuropathy fur- sweating, and the development of fissures Heart rate response to deep breathing
ther attenuates the epinephrine response and cracks that are portals of entry for is for the most part a function of parasym-
to hypoglycemia in diabetic individuals microorganisms leading to infectious pathetic activity, although the sympa-
after recent hypoglycemic exposure ulcers and ultimately gangrene. A pro- thetic nervous system may affect this
(144 –146). spective study by Boyko et al. (155) dem- measure (158). Similarly, it is parasympa-
onstrated the effect of autonomic thetic activity that plays the greatest role
Hypoglycemic autonomic failure neuropathy on the risk of developing a in the heart rate regulation for short-term
The spectrum of reduced counterregula- foot ulcer independent of other measures standing, where the act of standing in-
tory hormone responses (in particular of sensory neuropathy. Autonomic neu- volves low-level exercise and parasympa-
epinephrine) and decreased symptom ropathy may also lead to increased oste- thetic tone is withdrawn to produce a
perception of hypoglycemia due to de- oclastic activity resulting in reduced bone sudden tachycardic response (159). In re-
creased ANS activation after recent ante- density. Thus, Young et al. (156) sug- sponse to subsequent underlying blood
cedent hypoglycemia has been termed gested that the significant relationship be- pressure changes while standing, a
“hypoglycemia-induced autonomic fail- tween reduced bone mineral density and baroreceptor-mediated reflex involves the
ure” (147–149). Hypoglycemia-induced severity of diabetic neuropathy in the sympathetic nerves for further heart rate
autonomic failure leads to a vicious cy- lower extremities of individuals with control (160). Heart rate response to the
cle of hypoglycemia unawareness that Charcot neuroarthropathy may reflect the Valsalva maneuver is influenced by both
induces a further decrease in counter- severity of autonomic neuropathy. parasympathetic and sympathetic activ-
regulatory hormone responses to hypo- ity. Measurements of blood pressure re-
glycemia. This vicious cycle occurs CLINICAL TESTING OF sponse to standing and blood pressure
commonly in individuals with diabetes AUTONOMIC FUNCTION response to sustained handgrip are used
who are in strict glycemic control. The to assess sympathetic activity.
reduced epinephrine response to ante- Assessing cardiovascular autonomic Heart rate response to deep breathing
cedent hypoglycemia occurs in the ab- function (i.e., beat-to-beat heart rate variation,
sence of DAN as measured by standard Quantitative tests of autonomic function R-R variation). Beat-to-beat variation in
tests of autonomic function (143,148, have historically lagged behind measures heart rate with respiration depends on
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1565
Technical Review
parasympathetic innervation. Pharmaco- ver includes tachycardia and peripheral ● Phase III: Blood pressure falls and
logical blockade of the vagus nerve with vasoconstriction during strain, followed heart rate increases with cessation of
atropine all but abolishes respiratory si- by an overshoot in blood pressure and expiration.
nus arrhythmia, whereas sympathetic bradycardia after release of strain. The re- ● Phase IV: Blood pressure increases
blockade with the use or pretreatment of sponse is mediated through alternating above the baseline value (overshoot)
propranolol has only a slight effect on it activation of parasympathetic and sympa- because of residual vasoconstriction
(158). Several different techniques have thetic nerve fibers. Pharmacological and restored normal venous return and
been described in clinical literature, but blockade studies using atropine, phentol- cardiac output.
measurement during paced deep breath- amine (an ␣-adrenergic antagonist), and
ing is considered the most reliable. The propranolol (a nonspecific -adrenergic The Valsalva ratio is determined from
patient lies quietly and breathes deeply at blocker) confirm dual involvement of au- the ECG tracings by calculating the ratio
a rate of six breaths per minute (a rate that tonomic nerve branches for the response of the longest R-R interval after the ma-
produces maximum variation in heart to this maneuver by demonstrating the neuver (reflecting the bradycardic re-
rate) while a heart monitor records the drugs’ varied effects of attenuation or aug- sponse to blood pressure overshoot) to
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
difference between the maximum and mentation of the hemodynamic response the shortest R-R interval during or shortly
minimum heart rates. Over a number of to the maneuver at specific times during after the maneuver (reflecting tachycardia
years, there have been several different the response (162). In patients with auto- as a result of strain).
measures of R-R variation. The following nomic damage from diabetes, the reflex With regard to the progression of au-
six measures have most consistently been pathways are damaged. This is seen as a tonomic dysfunction in diabetes, the Val-
reported (standard deviation, coefficient blunted heart rate response and some- salva maneuver may be the best method
of variation, mean circular resultant, max- times as a lower-than-normal decline in to monitor this longitudinally (121).
imum minus minimum, expiration-to- blood pressure during strain, followed by Quantitative analysis of nerve function
inspiration [E:I] ratio, and spectral a slow recovery after release. (e.g., autonomic function testing) paral-
analysis) (43). There are advantages, dis- In the standard Valsalva maneuver, lels that of clinical neuropathy in that the
advantages, and considerations that need the supine patient, connected to an ECG rate of progression is slow, gradual, and
to be recognized for all of the measures of monitor, forcibly exhales for 15 s against a an insidious process (164). In a study by
R-R variation. fixed resistance (40 mmHg) with an open Levitt et al. (121), the rate of deterioration
Heart rate response to standing. This glottis. A sudden transient increase in in- of the Valsalva ratio was 0.015 per year for
test evaluates the cardiovascular response trathoracic and intra-abdominal pres- individuals with type 1 diabetes, which
elicited by a change from a horizontal to a sures, with a consequent hemodynamic was more than twice that expected from
vertical position. The typical heart rate re- response, results. With performance of cross-sectional studies of the aging effect
sponse to standing is largely attenuated by the Valsalva maneuver, there is a transient in normal individuals of a similar age
a parasympathetic blockade achieved increase in intraocular and intracranial range.
with atropine (159). In healthy subjects, pressure, creating a small theoretical risk All of the tests described above for the
there is a characteristic and rapid increase of intraocular hemorrhage and lens dislo- assessment of cardiovascular autonomic
in heart rate in response to standing that is cation (163). In practical terms, however, function can be performed by a general
maximal at approximately the 15th beat the risk is minimal because comparable practitioner. Those patients with cardio-
after standing. This is followed by a rela- pressures occur in the performance of vascular autonomic dysfunction who
tive bradycardia that is maximal at ap- daily activities. have system-specific symptoms will need
proximately the 30th beat after standing. The response to performance of the to be referred to a specialist for refined
In patients with diabetes and autonomic Valsalva maneuver has four phases and in testing.
neuropathy, there is only a gradual in- healthy individuals can be observed as Power spectral analysis. Analysis of
crease in heart rate. The patient is con- follows: HRV can also be assessed by spectral anal-
nected to an electrocardiogram (ECG) ysis of a series of successive R-R intervals
monitor while lying down and then ● Phase I: Transient rise in blood pres- (frequency domain analyses). This can be
stands to a full upright position. ECG sure and a fall in heart rate due to com- performed on short R-R sequences (e.g., 7
tracings are used to determine the 30:15 pression of the aorta and propulsion of min) or on 24-h ECG recordings. The
ratio, calculated as the ratio of the longest blood into the peripheral circulation. main advantage of power spectral analysis
R-R interval (found at about beat 30) to Hemodynamic changes are mostly sec- (PSA) is that HRV can be measured across
the shortest R-R interval (found at about ondary to mechanical factors. a range of frequencies and that less patient
beat 15). Because the maximum and min- ● Phase II: Early fall in blood pressure participation is necessary (165). The
imum R-R intervals may not always occur with a subsequent recovery of blood heart rate power spectrum is typically di-
at exactly the 15th or 30th beats after pressure later in the phase. The blood vided into two frequency bands: low
standing, Ziegler et al. (161) redefined the pressure changes are accompanied by (0.04 – 0.15 Hz) and high (0.15– 0.4 Hz).
maximum/minimum 30:15 ratio as the an increase in heart rate. There is a fall The high-frequency region is generally
longest R-R interval during beats 20 – 40 in cardiac output due to impaired ve- considered a marker of vagal activity,
divided by the shortest R-R interval dur- nous return causing compensatory car- whereas the low-frequency component is
ing beats 5–25. diac acceleration, increased muscle influenced by both sympathetic and vagal
Valsalva maneuver. In healthy subjects, sympathetic activity, and peripheral re- activity (165).
the reflex response to the Valsalva maneu- sistance. A study providing a direct compar-
1566 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
ison of PSA and some time-domain Assessing cardiovascular adrenergic quence of compensatory cardiovascular
techniques for quantifying HRV was (sympathetic) function responses to maintain homeostasis. As for
completed by Freeman et al. (166). In this Systolic blood pressure response to the stand response, the normal tilted re-
study, conventional methods to calculate standing. Blood pressure normally flex consists of an elevation in heart rate
“max-min,” standard deviation, E:I ratio, changes only slightly on standing from a and vasoconstriction. If reflex pathways
Valsalva ratio, and 30:15 ratio were used, sitting or supine position. The response to are defective, blood pressure falls mark-
as were those for the low-frequency standing is mediated by sympathetic edly with hemodynamic pooling. An ab-
(0.02– 0.15 Hz) and high-frequency nerve fibers. In healthy subjects, there is normal response is defined similarly to
(0.15–1.0 Hz) power for the heart rate an immediate pooling of blood in the de- that associated with standing.
power spectra of 15 type 1 diabetic pa- pendent circulation resulting in a fall in
tients. Intrasubject comparisons were blood pressure that is rapidly corrected by Assessing GI autonomic function.
achieved through multiple linear regres- baroreflex-mediated peripheral vasocon- Even with mild symptoms, gastroparesis
sion analysis for which the “predicted” striction and tachycardia. In normal indi- interferes with nutrient delivery to the
viduals, the systolic blood pressure falls small bowel and therefore disrupts the re-
spectral power was plotted against the ac-
by ⬍10 mmHg in 30 s. In diabetic pa-
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
lationship between glucose absorption
tual time-domain values. The time-
tients with autonomic neuropathy, and exogenous insulin administration.
domain values were found to correlate
baroreflex compensation is impaired. A This can result in wide swings of glucose
very strongly with high-frequency spec- response is considered abnormal when levels and unexpected episodes of post-
tral indexes, especially the Valsalva and the diastolic blood pressure decreases prandial hypoglycemia and apparent
30:15 ratios (linear regression gave R2 val- more than 10 mmHg or the systolic blood “brittle diabetes.” Therefore, gastroparesis
ues of 0.85 and 0.90, respectively). An- pressure falls by 30 mmHg within 2 min should be suspected in patients with er-
other study by Howorka et al. (167) after standing (32,168,169). A task force ratic glucose control.
compared the spectral and time-domain of the American Academy of Neurology The finding of retained food in the
test results for a population of 119 dia- (AAN) and the American Autonomic So- stomach after an 8- to 12-h fast in the
betic patients. A band from 0.15 to 5.0 Hz ciety defined orthostatic hypotension as a absence of obstruction is diagnostic of
was assigned as the high-frequency band, fall in systolic blood pressure of ⱖ20 gastroparesis. Basic diagnostic tests in-
whereas low frequency was 0.005 to 0.15 mmHg or diastolic blood pressure of ⱖ10 clude upper-GI endoscopy or barium se-
Hz. Spectral indexes were power and den- mmHg accompanied by symptoms (51). ries to rule out structural or mucosal
sity and were compared with standard Diastolic blood pressure response to abnormalities of the GI tract. Evaluation
Ewing tests of HRV (I:E difference, Val- sustained handgrip. In this test, sus- of the patient with suspected diabetic gas-
salva ratio, and 30:15 ratio). The multiple tained muscle contraction as measured by troparesis might include the following:
correlation between variables of PSA and a handgrip dynamometer causes a rise in
the Ewing battery “was high, and over systolic and diastolic blood pressure and ● Assessment of glycemic control
83% of cases were classified in an identi- heart rate. This rise is caused by a reflex ● Medication history, including the use of
cal way by both diagnostic tests.” These arc from the exercising muscle to central anticholinergic agents, ganglion block-
researchers went on to conclude that their command and back along efferent fibers. ers, and psychotropic drugs
The efferent fibers innervate the heart and ● Gastroduodenoscopy to exclude pylo-
investigation “showed that short-term
PSA of HRV is of similar diagnostic value muscle, resulting in increased cardiac ric or other mechanical obstruction
output, blood pressure, and heart rate. ● Manometry to detect antral hypomotil-
as the Ewing battery concerning the pres-
ence of cardiovascular autonomic neu- The dynamometer is first squeezed to iso- ity and/or pylorospasm
metric maximum, then held at 30% max- ● Double-isotope scintigraphy to mea-
ropathy” (167). Ziegler et al. (161) made
their own test comparison using 120 imum for 5 min. The normal response is a sure solid-phase gastric emptying; this
healthy subjects and 21 diabetic patients. rise of diastolic blood pressure ⬎16 requires ingestion of a solid labeled
mmHg, whereas a response of ⬍10 with radionuclides. Liquid emptying
PSA testing with subjects at rest was per-
mmHg is considered abnormal (168). Pa- gives false-negative results. The blood
formed with low frequency being defined
tients with DAN are more likely to exhibit glucose should be normal at the time of
as 0.01– 0.05 Hz, mid-frequency as 0.05– only a small diastolic blood pressure rise. testing because hyperglycemia de-
0.15 Hz, and high frequency as 0.15– 0.5 Response to tilting. The hemodynamic creases gastric motility.
Hz. This study also used a standard Ewing response to standing is a commonly per- ● Electrogastrography detects abnormal-
battery of tests, which included coeffi- formed measure of autonomic function. ities in GI pacemaking, but its role has
cient of variation, E:I ratio, Valsalva ratio, Passive head-up tilting provides a more not been established in diagnosis or
max-min, 30:15 ratio, and other time- precise level of standardization to the or- treatment decision making.
domain measures. Findings for HRV tests thostatic stimulus and reduces the mus-
were that, with the exception of the Val- cular contraction of the legs, which can Most of the specialized evaluations for as-
salva ratio, “results of most tests were sig- reduce lower-leg pooling of blood. A tilt sessment of gastroparesis will typically be
nificantly associated with each other. . .” angle of 60° is commonly used for this performed by a gastroenterologist.
and that correlations between time- test. The tilt may be maintained for Constipation. Constipation is the most
domain measures were highest for the 10 – 60 min or until the patient’s ortho- common GI complication, affecting
high-frequency band (r ⫽ 0.36 – 0.81; static symptoms can be reproduced. The nearly 60% of diabetic patients (1). It is
P ⬍ 0.001) (161). orthostatic stress of tilting evokes a se- believed to be due to DAN rather than
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1567
Technical Review
myopathic changes. The gastrocolic reflex ● A trial on a gluten-free diet is war- ● Autonomic neuropathy testing (e.g.,
is impaired, but stimulation of colonic ranted, and confirmation of the diagno- HRV)
smooth muscle with neostigmine is nor- sis with upper-GI endoscopy and/or ● Intracavernosal injection of vasoactive
mal (170). small bowel biopsy may be required. compound (e.g., papaverine and pros-
Tests for the diagnosis and assess- ● If Crohn’s disease is suspected, up- taglandin E1 [PGE1]) with a response of
ment of constipation might include the per-GI barium examination with dedi- ⬃65–70% of the time reflecting a pre-
following: cated small bowel follow-through dominantly neurogenic cause of ED
● Measurement of vitamin B-12 and fo- and compatible with a significant arte-
● Anorectal manometry for evaluating late rial component. Failure of the response
sphincter tone and the rectal anal inhib- ● If history and examination suggest suggests venous incompetence.
itory reflex to distinguish colonic hypo- small bowel disease, hydrogen breath ● Hormonal evaluation (luteinizing hor-
motility from rectosigmoid dysfunction test and Schilling’s test are required. mone, testosterone, free testosterone,
causing outlet obstructive symptoms Positive breath means lactose intoler- prolactin)
● Assessment of colonic segmental transit ance and/or bacterial overgrowth. Pos- ● Psychological evaluation (Minnesota
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
time. This may be accomplished by itive Schilling’s test may be diagnostic Multiphasic Personality Inventory
means of segmental transit of radio- of bacterial overgrowth. [MMPI])
paque markers that are ingested orally. ● Stools tested for occult blood (which, if
● Pelvic examination, with careful bi- present, requires follow-up upper- and A proposed scheme for evaluation of
manual examination for women lower-GI endoscopy) ED is shown in Fig. 3 (1).
● Three stools tested for occult blood Once diagnosed, treatment may in-
(which, if present, requires that a com- Specialized tests for the assessment of di- clude withdrawal from offending medica-
plete blood count, iron count, TIBG, abetic diarrhea will typically be per- tions coupled with psychological
proctosigmoidoscopy and barium en- formed by a gastroenterologist. counseling, medical treatment, or sur-
ema, or full colonoscopy be performed) The severe and intermittent nature of gery. Medical treatment may include sil-
diabetic diarrhea makes treatment and as- denafil taken at a dose of 50 mg. A lower
Most of these procedures will typically be sessment difficult. Because afferent de- dosage is needed for individuals with re-
performed by a specialist. nervation may contribute to the problem, nal failure or liver dysfunction. Sildenafil
Diarrhea. Assessment of diarrhea in pa- a bowel program that includes restriction should not be taken by individuals with
tients with diabetes might include the fol- of soluble fiber and regular effort to move unstable ischemic heart disease or those
lowing: the bowels is indicated. In addition, trials using nitroglycerin or other nitrate-con-
of gluten-free diet, restriction of lactose, taining medications. Specialized assess-
● History to rule out diarrhea secondary cholestyramine, clonidine, somatostatin ment of ED will typically be performed by
to ingestion of lactose, nonabsorbable analog, pancreatic enzyme supplements, a urologist.
hexitols, or medication (especially bi- and antibiotics such as metronidazole Female sexual dysfunction. Female
guanides, ␣-glucosidase inhibitors, and may be indicated. sexual dysfunction assessment using vag-
tetrahydrolipostatin) inal plethysmography to measure lubrica-
● History to rule out other causes, espe- Assessing genitourinary autonomic tion and vaginal flushing has not been
cially iatrogenic ones function well established or standardized.
● Travel and sexual histories and ques- ED. ED is assessed by both taking a med- Bladder dysfunction. Evaluation of di-
tioning regarding similar illnesses ical history and specific tests, which abetic bladder dysfunction should be
among both household members and might include the following: done for any diabetic patient with recur-
coworkers ● Sexual function history (libido, erectile rent urinary tract infection, pyelonephri-
● History of prior ethanol consumption function, ejaculatory function, fertility) tis, incontinence, or a palpable bladder. The
● History of pancreatitis and biliary stone ● Medication history evaluation might include the following:
diseases ● Assessment of glycemic control
● Examination for enteric pathogens and ● Measurement of nocturnal penile tu- ● Assessment of renal function
ova and parasites mescence ● Urinary culture
● Patients with large-volume diarrhea or ● Measurement of penile and brachial ● Postvoid ultrasound to assess residual
fecal fat should be further studied with blood pressure with Doppler probes volume and upper– urinary tract dilation
a 72-h fecal fat collection: the d-xylose and calculation of the penile-brachial ● Cystometry and voiding cystometro-
test is an appropriate screen for small pressure index (⬍0.7 suggests penile gram to measure bladder sensation and
bowel malabsorptive disorders. vascular disease) volume pressure changes associated
● If significant steatorrhea is detected, as- ● Sacral outflow (S2, S3, and S4) assess- with bladder filling with known vol-
sess pancreatic calcification with plain ment, which represents the sacral para- umes of water and voiding
film of abdomen and perform formal sympathetic divisions: anal sphincter
pancreatic function tests. tone, perianal sensation, anal wink, and Specialized assessment of bladder dys-
● If celiac disease is suspected, measure bulbocavernous reflex are clinical fea- function will typically be performed by a
serum levels of celiac disease antibody tures of denervation of the important urologist.
profile, including gliadin, endomysial, nerve supply that enable erections to Diabetic cystopathy manifests as an
gluten, and reticulin antibodies. occur. increase in threshold of occurrence of a
1568 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
Figure 3—Evaluation of diabetic
patients with ED (138). NPT, noc-
turnal peniletumescence.
detrusor reflex contraction. A grossly nervous system, from the hypothalamus The QSART involves iontophoresis of
overdistended bladder should be drained to the sweat glands, but is not able to dif- a cholinergic agonist to measure axon re-
by catheter to improve contractility, and ferentiate between pre- and postgangli- flex–medicated sudomotor responses
the patient should be instructed to void onic causes of anhidrosis. Postganglionic quantitatively to evaluate postganglionic
by the clock rather than waiting for the sudomotor function can be determined sudomotor function. Four sites are used
sensation of bladder distention. Cholin- by measuring sweat output after ionto- and studied simultaneously with the pa-
ergic agents or clean intermittent self- phoresis or intradermal injection of cho- tient supine. The test, typically done by
catheterization may also be used to facility linergic agonists. recording from the forearm and three
emptying. Tests of sudomotor function evaluate lower-extremity skin sites, has high sen-
the extent, distribution, and location of sitivity, specificity, and reproducibility,
Assessing sudomotor function deficits in sympathetic cholinergic func- with a coefficient of variation of 20% if
Testing of the eccrine sweat glands pro- tion. These tests include the quantitative performed by trained personnel. The test
vides a measure of sympathetic cholin- sudomotor axon reflex test (QSART), the is not generally available and requires the
ergic function. Thermoregulatory sweat sweat imprint, the thermoregulatory purchase of expensive specialized equip-
testing assesses both central and periph- sweat test (TST), and the sympathetic ment.
eral aspects of the efferent sympathetic skin response. A sweat imprint may be formed by the
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1569
Technical Review
secretion of active sweat glands into a ence of either a proximal or distal ANS nomic neuropathy) in clinical studies.
plastic or silicone mold in response to lesion. The selection of standardized measure-
iontophoresis of a cholinergic agonist. ● Hand grip. Peripheral contralateral (in- ment techniques based on reliability and
This test can be used to determine sweat dex finger, pulp surface) response to precision studies was encouraged. The
gland density, sweat droplet size, and sustained 40% maximum grip on a dy- expressed purpose was to recommend
sweat volume per area. namometer is biphasic over 60 s. The common inter-study methodologies that
The TST assesses both central and pe- initial normal response is 40 –50% re- would facilitate the comparison of results
ripheral aspects of the efferent sympa- duction of flow from basal during the from one clinical investigation to another.
thetic nervous system, from the initial 20 –30 s, followed by a dilation Specifically concerning the assessment of
hypothalamus to the sweat glands. It is a resulting in a return to typically super- CAN, the panel recognized strong evi-
well-standardized test and evaluates the basal levels; there is no response if the dence for three tests of heart rate control
distribution of sweat by a change in color peripheral ANS is damaged. (mainly tests of parasympathetic control).
of an indicator powder on the skin after ● Cold pressor. Immersion of the con- The three tests recommended were heart
exposure to infrared light. The TST is tralateral hand in cold (ice) water typi- rate response to 1) deep breathing, 2)
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
semiquantitative (percentage of anterior cally results in a 50 – 60% reduction in standing, and 3) the Valsalva maneuver.
body anhidrosis) and has a high sensitiv- peripheral skin blood flow at the con- Two tests of blood pressure control were
ity. The specificity is low, however, be- tralateral pulp index surface. In some also recommended: blood pressure re-
cause it is not able to differentiate between individuals, this response becomes bi- sponse to 1) standing or passive tilting
pre- and postganglionic causes of an- phasic after prolonged exposure (30 s) and 2) sustained handgrip. These tests
hidrosis. In combination with QSART, to such intense cold because it is ex- were judged suitable for both routine
the specificity of the TST for delineating tremely uncomfortable. There is a pre- screening and monitoring the progress of
the lesion site is significantly increased. dominately peripheral component, but autonomic neuropathy (3). No tests of
The sympathetic skin response (or pain generates a centrally mediated re- sweating, sympathetic skin responses,
peripheral autonomic surface potential) is sponse. pupillary reflexes, or genitourinary or GI
generated by the sweat glands and over- ● Heating and gravity. Heating the limb function were considered to be suffi-
lying epidermis. This response may occur to 44°C and dropping it below the level ciently well standardized for routine clin-
spontaneously or can be evoked by stim- of the heart results in a marked increase ical use.
uli such as respiration and startle. The in blood flow in normal subjects. The Results from earlier research suggest-
sympathetic skin response can be mea- response is a measure of autonomic mi- ed that using a battery of cardiovascular
sured with surface electrodes connected crovascular integrity and is markedly tests (some indicating parasympathetic
to a standard electromyogram instru- depressed in patients with AN. involvement and others indicating possi-
ment. The response habituates with re- ble sympathetic involvement) would
peated stimuli and is subject to variability. Assessing pupillary function make it possible to follow the progression
Delivering stimuli at irregular intervals Patients with DAN show delayed or of autonomic function over time (30).
may minimize habituation. Concordance absent reflex response to light and di- The San Antonio consensus panel further
between the sympathetic skin response minished hippus due to decreased sym- extended the utility of tests of cardiovas-
and sudomotor function has been shown pathetic activity and reduced resting cular autonomic function by suggesting
in some but not all studies. pupillary diameter (7). Pupillary mea- that a battery of tests could be used to
Peripheral neurovascular responses. surements are usually only performed in a stage patients with autonomic neuropa-
Smooth muscle microvasculature in the research setting. thy. A three-stage model was proposed as
periphery reacts sympathetically to a follows:
number of stressor tasks. These may be CURRENT GUIDELINES FOR
divided into those dependent on the in- THE DIAGNOSIS OF ● Early stage: abnormality of heart rate
tegrity of the central nervous system (ori- AUTONOMIC NEUROPATHY response during deep breathing alone
enting response and mental arithmetic) Several worldwide consensus meetings ● Intermediate stage: an abnormality of
and those dependent on the distal sympa- have been convened since the 1980s to Valsalva response
thetic axon (handgrip and cold pressor evaluate the growing evidence concern- ● Severe stage: the presence of postural
tests): ing tests for the assessment of diabetic hypotension
neuropathy. Two of the meetings (the San
● Orienting response. Orienting re- Antonio Conference on Diabetic Neurop- The San Antonio Consensus Panel
sponse is the vasoconstriction and re- athy held in 1988 and a second confer- also made several general recommenda-
sulting drop in peripheral (index finger, ence in 1992) were jointly sponsored by tions regarding the need to fully classify
pulp surface) skin blood flow when a the American Diabetes Association and DAN:
subject engages in speech after several AAN. The consensus statement published
minutes of relaxation with music. by the expert panel at the 1988 San Anto- ● Symptoms possibly reflecting auto-
● Mental arithmetic. Mental arithmetic nio Conference was a synthesis of re- nomic neuropathy should not, by
as a serial subtraction task typically re- viewed research efforts to date in the themselves, be considered markers for
sults in a 30% reduction in peripheral clinical assessment of neuropathies and its presence.
(index finger, pulp surface) skin blood offered recommendations for the testing ● Noninvasive validated measures of au-
flow. There is no response in the pres- of diabetic neuropathy (including auto- tonomic neural reflexes should be used
1570 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
as specific markers of autonomic neu- not be effective in detecting the cardio- volvement in asymptomatic patients.
ropathy if end-organ failure is carefully vascular involvement that autonomic Because late stages of CAN are indicators
ruled out and other important factors function tests detect at early stages of of poor prognosis in diabetic patients,
such as concomitant illness, drug use, emergence. Thus, tests for other forms of early prognostic capabilities offer a signif-
and age are taken into account. diabetic peripheral neuropathy should icant contribution to diagnosis and sub-
● An abnormality on more than one test not be substituted for tests of cardiovas- sequent therapy.
on more than one occasion is desirable cular autonomic dysfunction. Evidence from clinical literature can
to establish the presence of autonomic be found that support recommendations
dysfunction. SAFETY OF TESTING for various subpopulations. They include
● Independent tests of both parasympa- PROCEDURES the following.
thetic and sympathetic function should An expert panel from the AAN reviewed a
be performed. number of standardized measures and Diabetic patients with a history of
● A battery of quantitative measures of found that noninvasive autonomic tests poor glycemic control
autonomic reflexes should be used to were found to have a high value-to-risk Long-term poor glycemic control can
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
monitor improvement or deterioration ratio (163). Some tests do, however, carry only increase the risk of developing ad-
of autonomic nerve function. a small risk for an adverse event. The Val- vanced diabetic neuropathy, although
salva maneuver transiently increases in- long-term follow-up studies are lacking
trathoracic, intraocular, and intracranial (117). Mustonen et al. (173) showed in a
In 1992, a second jointly sponsored pressure, creating, for example, a small 4-year follow-up study of 32 individuals
conference was convened to review the theoretical risk of intraocular hemorrhage with type 2 diabetes that poor glycemic
state-of-the-art of diabetic neuropathy and lens dislocation (163). In practical control was an important determinant of
measures used in epidemiological and terms, the risk is minimal because com- the progression of autonomic nerve dys-
clinical studies including cross-sectional, parable intrathoracic pressures occur in function.
longitudinal, and therapeutic trials. the performance of daily activities. In the The DCCT provided extensive clini-
While recognizing the importance of clin- published literature of over 100 studies, cal evidence that good metabolic control
ical measures such as medical and neuro- there have been no reports of deaths dur- reduces diabetic complications. Specifi-
logical history and physical examination, ing testing and no reports of adverse cally with regard to cardiovascular auto-
conference participants also recognized events after completion of the tests at- nomic function, the DCCT showed that
the subjective nature of such measures tributable to the procedures. The Dia- intensive glycemic control prevented the
and emphasized the importance of objec- betes Control and Complications Trial development of abnormal heart rate vari-
tive measures, including autonomic func- (DCCT), one of the largest trials to use ation and slowed the deterioration of au-
tion tests in the case of autonomic cardiovascular autonomic function tests, tonomic dysfunction over time for
neuropathy. The panel in 1992 also re- evaluated 1,441 patients with type 1 dia- individuals with type 1 diabetes (37). Un-
vised its recommendation to include betes in 29 centers over a mean duration fortunately, however, one cannot predict
three tests for the longitudinal testing of of 6.5 years without procedural compli- what the metabolic control will be (or has
the cardiovascular ANS: 1) heart rate re- cations (37). When used by properly been) over a long period of time by look-
sponse during deep breathing, 2) Valsalva trained individuals, autonomic function ing at current HbA1c results.
maneuver, and 3) postural blood pressure tests are a safe and effective diagnostic Poor glycemic control may also be a
testing (157). tool. consequence of DAN (e.g., gastroparesis
It is important to note that tests that Patient cooperation is required for that goes unidentified). Treatment of GI
specifically evaluate cardiovascular auto- performing autonomic function tests. dysfunction often improves glycemic
nomic function are part of the consensus Thus, children may pose some challenges control.
guidelines. Although there is an associa- related to performance (such as the attain-
tion between the presence of peripheral ment of the expiration pressure target re- Diagnosed diabetic patients
somatic neuropathy and DAN, research- quired for the Valsalva maneuver and the Primary prevention of diabetes is the ab-
ers have reported that the appearance of performance of metronomic breathing) solute goal. Unfortunately, that goal has
parasympathetic dysfunction may be in- and the cooperation and attention re- not yet been obtained. However, it has
dependent of peripheral neuropathy quirements of the test situation. These been shown that lifestyle intervention can
(171). Weinberg and Pfeifer (172) have same challenges may also apply to elderly reduce the incidence of type 2 diabetes
also shown that reduced HRV may be pre- patients, where deterioration of physio- (174). Individuals that do develop diabe-
dictive of the development of symptom- logical response is of concern, and to de- tes, however, are likely to suffer from its
atic somatic neuropathy, although these velopmentally and cognitively disabled complications. In fact, researchers have
results require follow-up in a larger study individuals. confirmed the presence of autonomic
cohort. Therefore, assessment modalities neuropathy at presentation (24). Some
that are used to measure other forms of WHO IS A CANDIDATE FOR manifestations of autonomic neuropathy
diabetic peripheral neuropathy, such as TESTING? may even precede the diagnosis of diabe-
tests of sensory or motor nerve fiber func- Autonomic function tests based on tes by several years (175).
tion (e.g., monofilament probe, quantita- changes in heart rate variation and blood In its entirety, the evidence supports
tive sensory tests, or nerve conduction pressure regulation can detect cardiovas- the contention that all patients with dia-
studies) and tests of muscle strength, may cular complications at early stages of in- betes, regardless of metabolic control, are
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1571
Technical Review
at risk for autonomic complications. does not take into account the clinical re- and reeducation of the patient with regard
Given that CAN may be life-threatening search advances that have been made in to hypoglycemia.
and the assessment for its presence can be the treatment of diabetes. Tests that pro-
easily performed, testing for cardiovascu- vide evidence of further health conse- To facilitate the decision to initiate
lar autonomic dysfunction is suggested quences may bring patients to medical treatment for cardiovascular
for individuals with diabetes. This in- attention before other signs of diabetic autonomic dysfunction
cludes testing to identify children and ad- end-organ injury emerge, making proac- Several different factors have been impli-
olescents with autonomic neuropathy. As tive treatment, particularly the establish- cated in the potential metabolic-vascular
some researchers have reported, the inci- ment of intensive diabetes care, possible. pathogenic process of diabetic neuropa-
dence of reduced HRV (measured using The results of autonomic function testing thy (e.g., activation of the polyol pathway,
PSA) has been shown to be 15% in chil- can contribute to good patient manage- increased oxidative stress, reduction in
dren (176). Massin et al. (177) demon- ment in the following ways. neurotrophic growth factors, deficiency
strated that early puberty is a critical of essential fatty acids, and formation of
period for the development of CAN and advanced glycosylation end products)
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
suggested that all type 1 diabetic patients To assist in the establishment (or (10,21,183,184). Thus, timely identifica-
should be screened for CAN beginning at reestablishment) of tight glycemic tion of autonomic dysfunction in diabetic
the first stage of puberty. With regard to control patients may expedite end-organ prophy-
whether either sex is more likely to de- Early observations by researchers that laxis such as the use of ACE inhibitors and
velop autonomic dysfunction, the litera- near-normal glycemic control seems to be aspirin and the use of pharmacological
ture has revealed conflicting reports. For the most effective way to delay the onset and nonpharmacological interventions to
example, in the DCCT, the presence of of CAN in type 1 diabetes has been con- improve blood pressure and lipid control.
autonomic neuropathy correlated with firmed by evidence from the DCCT (37). Improved nutrition and reduced alcohol
male sex along with age and duration Intensive insulin therapy has been shown and tobacco consumption are additional
(178). Jaffe et al. (179) show male sex to to be effective at preventing multiple options available to patients with diabetes
be predictive of depressed HRV in addi- complications in patients with type 1 di- who are identified with autonomic nerve
tion to age, duration, and retinopathy. abetes and is postulated to be effective for dysfunction. Interventions to modulate
However, in another study of type 1 dia- patients with type 2 diabetes, although reduced heart rate variation currently be-
betic individuals, females along with clinical studies are underway in the latter. ing studied in clinical trials are based on
other parameters (e.g., lipids and hyper- In its earliest stages, there has been theories of the pathogenesis of CAN.
tension) were found to be independent some clinical demonstration that auto- Evidence from clinical trials evaluat-
determinants of autonomic dysfunction nomic dysfunction may be influenced ing the use of antioxidants is promising.
(97). May et al. (180) showed a signifi- within a few days to a few weeks with Early identification of CAN permits
cantly reduced E:I ratio for females in a effective treatment (44,112). Delay in in- timely initiation of therapy with the anti-
random sample of 120 type 1 diabetic in- stituting appropriate interventions can oxidant ␣-lipoic acid (thioctic acid),
dividuals, along with older age, longer only increase the likelihood of developing which appears to slow or reverse progres-
duration, and elevated glucose, triglycer- advanced neuropathies. Stabilization of sion of neuropathies in some studies
ides, blood pressure, and urinary albumin the neuropathies (generally considered to (185), but further testing is necessary.
excretion. be any delays in further progression) Other antioxidants such as vitamin E have
through tight glycemic control seems pos- been shown to improve the ratio of car-
MANAGEMENT sible, whereas reversal of the condition diac sympathetic to parasympathetic tone
IMPLICATIONS OF may be less likely (44,182). Again, the in type 2 diabetic individuals with CAN
CARDIOVASCULAR results from the DCCT show that inten- (186) but may mitigate the effects of st-
AUTONOMIC NEUROPATHY sive glycemic treatment can prevent the atins and niacin in treating or preventing
Identifying individuals at risk is only the development of abnormal heart rate vari- macrovascular disease.
first step in managing patients and ulti- ation and slow the deterioration of auto- Studies using ACE inhibitors as a
mately affecting outcomes. After identifi- nomic dysfunction over time for means to improve heart rate variation
cation, effective management must be individuals with type 1 diabetes (37). have resulted in conflicting results.
provided. Proactive measures are re- Although the relationship between Whereas quinapril significantly increased
quired, because if those patients at high features of autonomic neuropathy and parasympathetic activity after 3 months of
risk or those shown to be in early stages hypoglycemic unawareness is complex treatment (187), cardiovascular auto-
are not treated until advanced symptom- and there is overlap, it is recognized that nomic function did not change signifi-
atology is present, little has been autonomic neuropathy may cause or con- cantly after 12 months of treatment with
achieved. tribute to the development of hypoglyce- trandolapril (188).
Unfortunately, information pre- mic unawareness. In most individuals The use of cardioselective (e.g.,
sented at the fifth Regenstrief conference with hypoglycemic unawareness, raising atenolol) or lipophilic (e.g., propranolol)
on the intensive management of type 2 the target may be necessary to prevent re- -blockers may also modulate the effects
diabetes indicated that physicians may peat episodes. Thus, emphasizing tight of autonomic dysfunction (1). By oppos-
feel that screening is not of value because control for individuals with autonomic ing the sympathetic stimulus, they may
treatment options for identified compli- dysfunction should also include in- restore the parasympathetic-sympathetic
cations are limited (181). Such a view creased vigilance in glycemic monitoring balance. Recently, the administration of
1572 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
metoprolol to ramipril-treated type 1 di- troduced to a now potentially motivated of clinical evaluation and patient observa-
abetic patients with abnormal albumin- patient. tion; rather, it enhances the clinical as-
uria has been shown to improve As mentioned previously, clinicians sessment of the diabetic patient by
autonomic dysfunction (189). must be careful when giving recommen- providing an objective, quantifiable, and
Although the benefit of currently dations with regard to exercise for indi- reproducible measure of autonomic func-
available agents in treating neuropathies viduals with CAN. This does not mean, tion.
is unproven, the investment in research however, that exercise is inappropriate
(time, labor, and money) attests to the po- for individuals with CAN. In fact, Ho- GLOSSARY
tential for treatment of detected neuropa- worka et al. (192) showed that physical
thies. Because the pathogenesis of CAN is training improved heart rate variation in Autonomic nervous system (ANS) –
most likely a multifactorial process, a insulin-requiring diabetic individuals The portion of the nervous system that
combination of therapies directed simul- with early CAN. Thus, careful testing to regulates individual organ function and
taneously at different parts of the patho- evaluate cardiovascular autonomic func- homeostasis not under voluntary control.
genic pathway may be needed. In tion and its degree of development is ex- An efferent and afferent system, the ANS
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
addition, the goal of these interventions tremely important. Clinicians working transmits impulses from the central ner-
should be directed at the prevention of together with the patient can develop an vous system to peripheral organ systems.
further deterioration of cardiovascular appropriate exercise program that will This results in control of heart rate and
autonomic dysfunction rather than ex- yield a plan for reaping maximum bene- force of contraction, constriction and di-
pecting to realize improved function. fits. latation of blood vessels, contraction and
relaxation of smooth muscle in various
To emphasize the importance of SUMMARY — Autonomic dysfunc- organs, visual accommodation, pupillary
adherence to diet and exercise tion is a prevalent and serious complica- size, and secretions from exocrine and
interventions tion for individuals with diabetes. The endocrine glands. The ANS is also re-
It is again emphasized that lifestyle inter- clinical manifestations of autonomic dys- sponsible for conveying visceral sensa-
ventions (e.g., adherence to diet and ex- function can affect daily activities (e.g., tion. The ANS is typically divided into
ercise) can reduce the incidence of type 2 exercise), produce troubling symptoms two divisions: the parasympathetic and
diabetes (174). Recently, a report indi- (e.g., syncope), and cause lethal out- the sympathetic systems on the basis of
cated that impaired glucose tolerance may comes. The patient’s history and physical anatomical and functional differences.
be associated with the development of di- examination are ineffective for early indi- Cardiovascular autonomic function
abetic neuropathy (i.e., sensory polyneu- cations of autonomic nerve dysfunction, testing – A number of simple objective
ropathy) (190). Should this be confirmed and thus recommendations for the use of tests of cardiovascular autonomic func-
in large prospective studies coupled with noninvasive tests that have demonstrated tion and reflexes to aid in the diagnosis of
evidence that primary intervention would efficacy are warranted. cardiovascular autonomic neuropathy.
prevent the development of neuropathy, The economic impact of the recom- Cardiovascular autonomic neuropathy
this would put even greater emphasis on mendation to use autonomic function (CAN) – This disorder results from dam-
the importance of lifestyle interventions testing is minimal compared with the eco- age to the fibers of the ANS with associ-
and screening at or soon after diagnosis. nomic impact of the catastrophic events ated abnormalities of heart rate control
Motivation to adhere and remain related to advanced cardiovascular, cere- and vascular dynamics.
compliant with nonpharmacological in- brovascular, and renal complications. Diabetic autonomic neuropathy (DAN)
terventions is difficult. Current research The relative cost of testing will always be – A neuropathic disorder associated with
suggests that preventive measures (glyce- less than the incremental costs of treating diabetes that includes manifestations in
mic control, diet, and exercise) intro- either a detected complication or the the peripheral components of the ANS.
duced to the general diabetic population more catastrophic event that could even- DAN affects sensory, motor, and vasomo-
are difficult to sustain and consequently tually occur. tor fibers innervating a large number of
less than effective. This is due, in part, to Despite research evidence that clini- organs. DAN may thus affect a number of
the long-term commitment that must be cal observations (whether they be symp- different organ systems (e.g., cardiovas-
made to the practice of preventive mea- toms or routine vital signs) should not be cular, GI, and genitourinary).
sures. Although individuals with diabetes the sole basis for the diagnosis of cardio- Diabetic neuropathy – “A descriptive
are faced with the immediate pressures of vascular autonomic dysfunction, screen- term meaning a demonstrable disorder,
disease management on a day-to-day ba- ing for abnormalities is infrequently either clinically evident or subclinical,
sis, it is the long-term risks of micro- and done. This is also despite the fact that of- that occurs in the setting of diabetes mel-
macrovascular complications that pose fice-based commercially available instru- litus without other causes for peripheral
the most serious risks (191). The ability to mentation for detection is readily neuropathy. The neuropathic disorder in-
determine early stages of autonomic dys- available. cludes manifestations in the somatic
function could intensify the salience of Given the clinical and economic im- and/or autonomic parts of the peripheral
measures such as diet and exercise that pact of this complication, testing of dia- nervous system” (3).
directly affect efforts to establish tight gly- betic individuals for cardiovascular Heart rate variability (HRV) – The mag-
cemic control and delay the development autonomic dysfunction should be part of nitude of heart rate fluctuations (R-R
of autonomic dysfunction. Colloquial pa- their standard of care. Such a recommen- interval) around the mean heart rate that
tient management strategies could be in- dation does not diminish the importance are modulated by the ANS. HRV is con-
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1573
Technical Review
sidered the earliest indicator and most Table A1—Summary of HRV test performance
frequent finding in symptomatic cardio-
vascular autonomic dysfunction. E:I ratio Valsalva ratio Standing (30:15) ratio
Parasympathetic nervous system – The
portion of the ANS concerned with con- Sensitivity 0.93 0.98 0.93
servation and restoration of energy. It Specificity 0.93 0.91 0.93
causes a reduction in heart rate and blood Positive predictive value 0.93 0.91 0.92
pressure, facilitates the digestion and ab- Negative predictive value 0.94 0.98 0.93
sorption of nutrients, and facilitates the From A.I. Vinik and M. Risk, unpublished data.
excretion of waste products from the
body. ing standardized algorithms and an offsite constant pressure at 40 ml over the 15-s
Sympathetic nervous system – The por- processing center. These currently un- interval. This causes a sudden transient
tion of the ANS that enables the body to published data (from A.I.V. and Risk) increase in intrathoracic and intra-
be prepared for fear, flight, or fight. Sym- were based on standardized testing of abdominal pressure and a consequent he-
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
pathetic responses include increases in 205 normal subjects and 3,516 patients modynamic response. Healthy patients
heart rate, blood pressure, and cardiac with type 1 or type 2 diabetes from 42 develop tachycardia and peripheral vaso-
output and diversion of blood flow from constriction during the strain and an
the skin and splanchnic vessels to those centers.
overshoot in blood pressure and brady-
supplying skeletal muscle. cardia on release. However, in patients
E:I ratio
The beat-to-beat HRV assesses the heart with autonomic damage from diabetes,
rate response to an autonomic reflex arc the reflex pathways are damaged, result-
APPENDIX: ing in a slow and steady decline in blood
STANDARDIZED TESTS OF using an electrocardiography and a means
for standardizing the patient’s breathing pressure during strain, followed by grad-
AUTONOMIC FUNCTION ual return to normal after release. Heart
The important criteria for appraising clin- rate (e.g., visual cues to guide inspiration
and expiration). The time intervals be- rate responses are often unchanged in this
ical tests of autonomic function include situation.
reliability, reproducibility, general corre- tween R-waves of the QRS complexes are
measured in milliseconds. This measure- The Valsalva ratio is the longest R-R
lation with each other and with tests of divided by the shortest R-R occurring
peripheral somatic nerve function, well- ment should be obtained using the deep
respiration test and the results evaluated within 45 s of peak heart rate and is in-
established normal values, and demon- dicative of overall condition of the para-
strated prognostic value. Three tests of by determining the E:I ratio.
To perform the test, the subject re- sympathetic and sympathetic fibers.
cardiovascular autonomic nerve function
that fulfill these criteria are 1) the E:I ratio mains supine and breathes deeply at the
(obtained from R-R variations), 2) the Val- rate of one breath per 10 s (i.e., six breaths Heart rate response to standing
salva ratio, and 3) the standing 30:15 ra- per minute) for 1 min while being moni- To test the heart rate response to standing,
tio. These tests use deep breathing, the tored by ECG. The E:I is the ratio of the the patient is connected to the heart rate
Valsalva maneuver, and standing from a mean of the longest R-R intervals during monitor while in the supine position. The
supine position, respectively, as provoca- deep expirations to the mean of the short- patient then stands to a full upright posi-
tive stimuli. For purposes of reimburse- est R-R intervals during deep inspirations. tion, and the ECG is monitored for an
ment, the three tests are grouped together The E:I ratio is significantly affected by additional period while standing. Stand-
under Current Procedural Terminology shifting of the heart rate and regularity of ing causes an immediate rapid increase in
code 95921. At least two of these three the respiratory cycling. HRV decreases heart rate with the maximum rate gener-
tests should be performed to provide ad- with increasing respiration rate, with the ally found at or around the 15th beat after
equate diagnostic information and to sup- greatest variation occurring at a respira- standing. The heart rate slows at or
port reimbursement claims. tory rate of six breaths per minute. Respi- around the 30th beat. The heart rate trac-
An abnormal result for each test is ration should therefore be standardized at ing is used to calculate the ratio of the
defined as HRV below that of the 5th six breaths per minute to optimize test longest R-R interval (about beat 30) after
percentile of the normal age-matched results. E:I ratios are based on the fact that the stand to the shortest R-R interval
population. Abnormal HRV in one test inspiration shortens R-R intervals while (about beat 15). This measure, called the
is indicative of early autonomic neurop- expiration lengthens them. 30:15 ratio, reflects the overall condition
athy. of the parasympathetic fibers. Normal
Because of the technical requirements Valsalva maneuver ranges are age dependent.
for these tests, they should be performed The complex effect of the Valsalva maneu-
at the point-of-care office or in a clinical ver on cardiovascular function is the basis
References
laboratory setting. The tests are not cur- of its usefulness as a measure of auto- 1. Vinik AI, Erbas T: Recognizing and
rently appropriate for nonclinical screen- nomic function. In the standard Valsalva treating diabetic autonomic neuropathy.
ing venues. maneuver, the supine patient, connected Cleve Clin J Med 68:928 –944, 2001
The sensitivity, specificity, and posi- to an ECG monitor, forcibly exhales for 2. Freeman R: The peripheral nervous sys-
tive/negative predictive values listed in 15 s against a fixed resistance with an tem and diabetes. In Joslin’s Diabetes Mel-
Table A1 summarize results obtained us- open glottis. The patient should maintain litus. Weir G, Kahn R, King GL, Eds.
1574 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
Philadelphia, Lippincott, 2002 ezevic-Cuca J: Autoimmune mecha- neuropathy. Q J Med 49:95–108, 1980
3. American Diabetes Association and nisms in the pathogenesis of diabetic 32. Ewing DJ, Campbell IW, Clark BF: As-
American Academy of Neurology: Re- neuropathy. In Molecular Mechanisms of sessment of cardiovascular effects in
port and recommendations of the San Endocrine and Organ Specific Autoimmu- diabetic autonomic neuropathy and
Antonio Conference on diabetic neurop- nity. Eisenbarth G, Ed. Austin, TX, R.G. prognostic implications. Ann Intern Med
athy (Consensus Statement). Diabetes Landes, 1999, p. 217–251 92:308 –311, 1980
37:1000 –1004, 1988 18. Sundkvist G, Lind P, Bergstrom B, Lilja 33. Hulper B, Willms B: Investigations of
4. Ziegler D: Cardiovascular autonomic B, Rabinowe SL: Autonomic nerve anti- autonomic diabetic neuropathy of the
neuropathy: clinical manifestations and bodies and autonomic nerve function in cardiovascular system. Horm Metab Res
measurement. Diabetes Reviews 7:300 – type 1 and type 2 diabetic patients. J In- Suppl 9:77– 80, 1980
315, 1999 tern Med 229:505–510, 1991 34. Dyrberg T, Benn J, Christiansen JS,
5. Pfeifer MA, Weinberg CR, Cook DL, Re- 19. Apfel SC, Arezzo JC, Brownlee M, Fed- Hilsted J, Nerup J: Prevalence of diabetic
enan A, Halter JB, Ensinck JW, Porte D eroff H, Kessler JA: Nerve growth factor autonomic neuropathy measured by
Jr: Autonomic neural dysfunction in re- administration protects against experi- simple bedside tests. Diabetologia 20:
cently diagnosed diabetic subjects. Dia- mental diabetic sensory neuropathy. 190 –194, 1981
betes Care 7:447– 453, 1984 Brain Res 634:7–12, 1994 35. Xueli Z, Baidi Z, Guoxian H, Xixing Z, et
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
6. Ewing DJ: Cardiovascular reflexes and 20. Horrobin DF: Essential fatty acids in the al.: Peripheral and autonomic nerve
autonomic neuropathy. Clin Sci Mol Med management of impaired nerve function function tests in early diagnosis of dia-
55:321–327, 1978 in diabetes. Diabetes 46 (Suppl. 2):S90 – betic neuropathy. Chinese Med J 94:495–
7. Clarke BF, Ewing DJ, Campbell IW: Di- S93, 1997 502, 1981
abetic autonomic neuropathy. Diabetolo- 21. Brownlee M: Glycation products and the 36. O’Brien IA, McFadden JP, Corrall RJ:
gia 17:195–212, 1979 pathogenesis of diabetic complications. The influence of autonomic neuropathy
8. Vinik AI: Diagnosis and management of Diabetes Care 15:1835–1843, 1992 on mortality in insulin-dependent dia-
diabetic neuropathy. Clin Geriatr Med 22. Obrosova IG: How does glucose gener- betes. Q J Med 79:495–502, 1991
15:293–320, 1999 ate oxidative stress in peripheral nerve? 37. DCCT Research Group: The effect of in-
9. Greene DA, Lattimer SA: Impaired rat Intern Review Neurobiology 50:3–35, 2002 tensive diabetes therapy on measures of
sciatic nerve sodium-potassium adeno- 23. Pacher P, Liaudet L, Soriano FG, Mabley autonomic nervous system function in
sine triphosphatase in acute streptozocin JG, Szabo E, Szabo C: The role of poly- the Diabetes Control and Complications
diabetes and its correction by dietary (ADP-ribose) polymerase activation in Trial (DCCT). Diabetologia 41:416 –423,
myo-inositol supplementation. J Clin In- the development of myocardial and en- 1998
vest 72:1058 –1063, 1983 dothelial dysfunction in diabetes. Diabe- 38. Neil HA, Thompson AV, John S, et al.:
10. Greene DA, Lattimer SA, Sima AA: Are tes 51:514 –521, 2002 Diabetic autonomic neuropathy: the
disturbances of sorbitol, phosphoinosi- 24. Ziegler D, Gries FA, Spuler M, Lessmann prevalence of impaired heart rate vari-
tide, and Na⫹-K⫹-ATPase regulation F, Diabetic Cardiovascular Autonomic ability in a geographically defined pop-
involved in pathogenesis of diabetic Neuropathy Multicenter Study Group: ulation. Diabet Med 6:20 –24, 1989
neuropathy? Diabetes 37:688 – 693, 1988 The epidemiology of diabetic neuropa- 39. O’Brien IA, O’Hare JP, Lewin IG, Corrall
11. Veves A, King GL: Can VEGF reverse di- thy. J Diabetes Complications 6:49 –57, RJ: The prevalence of autonomic neu-
abetic neuropathy in human subjects? 1992 ropathy in insulin-dependent diabetes: a
J Clin Invest 107:1215–1218, 2001 25. Kennedy WR, Navarro X, Sutherland controlled study based on heart rate
12. Cameron NE, Cotter MA: Metabolic and DER: Neuropathy profile of diabetic pa- variability. Q J Med 61:957–967, 1986
vascular factors in the pathogenesis of tients in a pancreas transplantation pro- 40. Verrotti A, Chiarelli F, Blasetti A,
diabetic neuropathy. Diabetes 46 (Suppl. gram. Neurology 45:773–780, 1995 Morgese G: Autonomic neuropathy in
2):31S–37S, 1997 26. Sharpey-Schafer EP, Taylor PJ: Absent diabetic children. J Paediatr Child Health
13. Low PA, Nickander KK, Tritschler HJ: circulatory reflexes in diabetic neuritis. 31:545–548, 1995
The roles of oxidative stress and antiox- Lancet 1:559 –562, 1960 41. Ewing DJ: Cardiac autonomic neuropa-
idant treatment in experimental diabetic 27. Ewing DJ, Irving JB, Kerr F, et al.: Car- thy. In Diabetes and Heart Disease. Jarret
neuropathy. Diabetes 46 (Suppl. 2):S38 – diovascular responses to sustained hand- RJ, Ed. Amsterdam, the Netherlands,
S42, 1997 grip in normal subjects and in patients Elsevier, 1984, p. 99 –132
14. Hoeldtke RD, Bryner KD, McNeill DR, with diabetes mellitus: a test of auto- 42. Maser RE, Lenhard MJ, DeCherney GS:
Hobbs GR, Riggs JE, Warehime SS, nomic function. Clin Sci Mol Med 46: Cardiovascular autonomic neuropathy:
Christie I, Ganser G, Van Dyke K: Nitro- 295–306, 1974 the clinical significance of its determina-
sative stress, uric acid, and peripheral 28. Morley JE, Asvat MS, Klein C, Lowenthal tion. Endocrinologist 10:27–33, 2000
nerve function in early type 1 diabetes. MN: Autonomic neuropathy in black di- 43. Schumer MP, Joyner SA, Pfeifer MA:
Diabetes 51:2817–2825, 2002 abetic patients. S Afr Med J 52:115–116, Cardiovascular autonomic neuropathy
15. Vinik AI, Erbas T, Tae S, Stansberry K, 1977 testing in patients with diabetes. Diabe-
Scanelli JA, Pittenger GL: Dermal neuro- 29. Hilsted J, Jensen SB: A simple test for tes Spectrum 11:227–231, 1998
vascular dysfunction in type 2 diabetes. autonomic neuropathy in juvenile dia- 44. Ziegler D: Diabetic cardiovascular auto-
Diabetes Care 24:1468 –1475, 2001 betics. Acta Med Scand 205:385–387, nomic neuropathy: prognosis, diagnosis
16. Pittenger GL, Malik RA, Burcus N, Boul- 1979 and treatment. Diabetes Metab Rev 10:
ton AJ, Vinik AI: Specific fiber deficits in 30. Mackay JD, Page MM, Cambridge J, 339 –383, 1994
sensorimotor diabetic polyneuropathy Watkins PJ: Diabetic autonomic neurop- 45. Vinik AI, Erbas T: Neuropathy. In Hand-
correspond to cytotoxicity against neu- athy: the diagnostic value of heart rate book of Exercise in Diabetes. Ruderman N,
roblastoma cells of sera from patients monitoring. Diabetologia 18:471– 478, Devlin JT, Schneider SH, Kriska A, Eds.
with diabetes. Diabetes Care 22:1839 – 1980 Alexandria, VA, American Diabetes As-
1844, 1999 31. Ewing DJ, Campbell IW, Clarke BF: The sociation, p. 463– 496, 2002
17. Vinik AI, Pittenger GL, Milicevic Z, Kn- natural history of diabetic autonomic 46. Kahn J, Zola B, Juni J, Vinik AI: De-
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1575
Technical Review
creased exercise heart rate in diabetic 61. Vinik AI: Diabetic neuropathy: patho- NA, Dar MA, Hayat A, Abbas SM: Silent
subjects with cardiac autonomic neu- genesis and therapy. Am J Med 107:17S– myocardial ischemia and cardiac auto-
ropathy. Diabetes Care 9:389 –394, 1986 26S, 1999 nomic neuropathy in diabetics. J Assoc
47. Roy TM, Peterson HR, Snider HL, Cyrus 62. Freeman R: Diabetic autonomic neurop- Physicians India 47:767–769, 1999
J, et al.: Autonomic influence on cardio- athy: an overview. In Clinical Manage- 74. Valensi P, Sachs RN, Harfouche B,
vascular performance in diabetic sub- ment of Diabetic Neuropathy. Veves A, Ed. Lormeau B, Paries J, Cosson E, Paycha F,
jects. Am J Med 87:382–388, 1989 Totowa, NJ, Humana Press, 1998, p. Leutenegger M, Attali JR: Predictive
48. Burgos LG, Ebert TJ, Asiddao C, Turner 181–208 value of cardiac autonomic neuropathy
LA, et al.: Increased intraoperative car- 63. Niakan E, Harati Y, Rolak LA, Comstock in diabetic patients with or without si-
diovascular morbidity in diabetics with JP, Rokey R: Silent myocardial infarction lent myocardial ischemia. Diabetes Care
autonomic neuropathy. Anesthesiology and diabetic cardiovascular autonomic 24:339 –343, 2001
70:591–597, 1989 neuropathy. Arch Intern Med 146:2229 – 75. Ambepityia G, Kopelman PG, Ingram D,
49. Kitamura A, Hoshino T, Kon T, et al.: 2230, 1986 Swash M, Mills PG, Timmis AD: Exer-
Patients with diabetic neuropathy are at 64. Hume L, Oakley GD, Boulton AJ, Hard- tional myocardial ischemia in diabetes: a
risk of a greater intraoperative reduction isty C, Ward JD: Asymptomatic myo- quantitative analysis of anginal percep-
in core temperature. Anesthesiology 92: cardial ischemia in diabetes and its tual threshold and the influence of auto-
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
1311–1318, 2000 relationship to diabetic neuropathy: an nomic function. J Am Coll Cardiol 15:72–
50. Sobotka PA, Liss HP, Vinik AI: Impaired exercise electrocardiography study in 77, 1990
hypoxic ventilatory drive in diabetic pa- middle-aged diabetic men. Diabetes Care 76. Marchant B, Umachandran V, Stevenson
tients with autonomic neuropathy. J Clin 9:384 –388, 1986 R, Kopelman PG, Timmis AD: Silent
Endocrinol Metab 62:658 – 663, 1986 65. Murray DP, O’Brien T, Mulrooney R, myocardial ischemia: role of subclinical
51. Position paper: Orthostatic hypoten- O’Sullivan DJ: Autonomic dysfunction neuropathy in patients with and without
sion, multiple system atrophy (the Shy and silent myocardial ischaemia on ex- diabetes. J Am Coll Cardiol 22:1433–
Drager syndrome) and pure autonomic ercise testing in diabetes mellitus. Diabet 1437, 1993
failure. J Auton Nerv Syst 58:123–124, Med 7:580 –584, 1990 77. Hikita H, Kurita A, Takase B, Nagayoshi
1996 66. Langer A, Freeman MR, Josse RG, H, Uehata A, Nishioka T, Mitani H,
52. Low PA, Walsh JC, Huang CY, McLeod Steiner G, Armstrong PW: Detection of Mizuno K, Nakamura H: Usefulness
JG: The sympathetic nervous system in silent myocardial ischemia in diabetes of plasma beta-endorphin level, pain
diabetic neuropathy: a clinical and mellitus. Am J Cardiol 67:1073–1078, threshold and autonomic function in
pathological study. Brain 98:341–356, 1991 assessing silent myocardial ischemia in
1975 67. O’Sullivan JJ, Conroy RM, MacDonald patients with and without diabetes mel-
53. Hilsted J, Parving HH, Christensen NJ, K, McKenna TJ, Mauerer BJ: Silent isch- litus. Am J Cardiol 72:140 –143, 1993
Benn J, Galbo H: Hemodynamics in di- emia in diabetic men with autonomic 78. Langer A, Freeman MR, Josse RG, Arm-
abetic orthostatic hypotension. J Clin In- neuropathy. Br Heart J 66:313–315, 1991 strong PW: Metaiodobenzylguanidine
vest 68:1427–1434, 1981 68. Koistinen MJ, Airaksinen KE, Huikuri imaging in diabetes mellitus: assessment
54. Hilsted J, Galbo H, Christensen NJ: HV, Pirttiaho H, Linnaluoto MK, Ika- of cardiac sympathetic denervation and
Impaired cardiovascular responses to heimo MJ, Takkunen JT: Asymptomatic its relation to autonomic dysfunction
graded exercise in diabetic autonomic coronary artery disease in diabetes: asso- and silent myocardial ischemia. J Am
neuropathy. Diabetes 28:313–319, 1979 ciated with autonomic neuropathy? Acta Coll Cardiol 25:610 – 618, 1995
55. Cryer PE, Silverberg AB, Santiago JV, Diabetol 28:199 –202, 1992 79. Airaksinen KEJ, Koistinen MJ: Associ-
Shah SD: Plasma catecholamines in dia- 69. Hartmann A, Schlottog B, Jungmann E, ation between silent coronary artery
betes: the syndromes of hypoadrenergic Bohm BO, Usadel KH, Kaltenbach M: disease, diabetes, and autonomic neu-
and hyperadrenergic postural hypoten- Somatic pain threshold and reactive hy- ropathy. Diabetes Care 15:288 –292, 1992
sion. Am J Med 64:407– 416, 1978 peremia in autonomic diabetic neuropa- 80. Airaksinen KE, Ikaheimo MJ, Linnaluoto
56. Tohmeh JF, Shah SD, Cryer PE: The thy and silent myocardial ischemia. Int MK, Niemela M, Takkunen JT: Impaired
pathogenesis of hyperadrenergic pos- J Cardiol 42:121–127, 1993 vagal heart rate control in coronary ar-
tural hypotension in diabetic patients. 70. Jermendy G, Davidovits Z, Khoor S: Si- tery disease. Br Heart J 58:592–597,
Am J Med 67:772–778, 1979 lent coronary artery disease in diabetic 1987
57. Page MM, Watkins PJ: Provocation of patients with cardiac autonomic neu- 81. Campbell IW, Ewing DJ, Clarke BF:
postural hypotension by insulin in dia- ropathy. Diabetes Care 17:1231–1232, Painful myocardial infarction in severe
betic autonomic neuropathy. Diabetes 1994 diabetic autonomic neuropathy. Acta
25:90 –95, 1976 71. Zarich S, Waxman S, Freeman RT, Diabetol Lat 15:210 –214, 1978
58. Mathias CJ, da Costa DF, Fosbraey P, Mittleman M, Hegarty P, Nesto RW: Ef- 82. Sampson MJ, Wilson S, Karagiannis P,
Christensen NJ, Bannister R: Hypoten- fect of autonomic nervous system dys- Edmonds M, Watkins PJ: Progression of
sive and sedative effects of insulin in au- function on the circadian pattern of diabetic autonomic neuropathy over a
tonomic failure. Br Med J (Clin Res Ed) myocardial ischemia in diabetes melli- decade of insulin-dependent diabetics.
295:161–163, 1987 tus. J Am Coll Cardiol 24:956 –962, 1994 Q J Med 75:635– 646, 1990
59. Winocour PH, Dhar H, Anderson DC: 72. Milan Study on Atherosclerosis and 83. Ewing DJ, Boland O, Neilson JM, Cho
The relationship between autonomic Diabetes (MiSAD) Group: Prevalence CG, Clarke BF: Autonomic neuropathy,
neuropathy and urinary sodium and al- of unrecognized silent myocardial QT interval lengthening, and unex-
bumin excretion in insulin-treated dia- ischemia and its association with athero- pected deaths in male diabetic patients.
betics. Diabet Med 3:436 – 440, 1986 sclerotic risk factors in noninsulin-de- Diabetologia 34:182–185, 1991
60. Freeman R: Cardiovascular autonomic pendent diabetes mellitus. Am J Cardiol 84. Jermendy G, Toth L, Voros P, Koltai MZ,
neuropathy. In Diabetic Neuropathy. 2nd 79:134 –139, 1997 Pogatsa G: Cardiac autonomic neuropa-
ed. Dyck PJ, Thomas PK, Eds. Philadel- 73. Jalal S, Alai MS, Khan KA, Jan VM, thy and QT interval length: a follow-up
phia, WB Saunders, 1999, p. 541–554 Rather HA, Iqbal K, Tramboo NA, Lone study in diabetic patients. Acta Cardiol
1576 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
46:189 –200, 1991 95. Ewing DJ, Martyn CN, Young RJ, Clarke diabetes on mortality after the first myo-
85. Rathmann W, Ziegler D, Jahnke M, et al.: BF: The value of cardiovascular auto- cardial infarction: The FINMONICA
Mortality in diabetic patients with car- nomic function tests: 10 years experi- Myocardial Infarction Register Study
diovascular autonomic neuropathy. Dia- ence in diabetes. Diabetes Care 8:491– Group. Diabetes Care 21:69 –75, 1998
bet Med 10:820 – 824, 1993 498, 1985 108. Fava S, Azzopardi J, Muscat HA, Fen-
86. Hathaway DK, El-Gebely S, Cardoso 96. Page MM, Watkins PJ: Cardiorespiratory nech FF: Factors that influence outcome
SS, Elmer DS, Gaber AO: Autonomic arrest and diabetic autonomic neuropa- in diabetic subjects with myocardial in-
control dysfunction in diabetic trans- thy. Lancet 1:14 –16, 1978 farction. Diabetes Care 16:1615–1618,
plant recipients succumbing to sud- 97. Maser RE, Pfeifer MA, Dorman JS, Kuller 1993
den cardiac death. Transplantation 59: LH, Becker DJ, Orchard TJ: Diabetic au- 109. Katz A, Liberty IF, Porath A, Ovsyshcher
634 – 637, 1995 tonomic neuropathy and cardiovascular I, Prystowsky EN: A simple beside test of
87. Orchard TJ, Lloyd CE, Maser RE, Kuller risk: Pittsburgh Epidemiology of Diabe- 1-minute heart rate variability during
LH: Why does diabetic autonomic neu- tes Complications Study III. Arch Intern deep breathing as a prognostic index af-
ropathy predict IDDM mortality? An Med 150:1218 –1222, 1990 ter myocardial infarction. Am Heart J
analysis from the Pittsburgh Epidemiol- 98. Spallone V, Maiello MR, Cicconetti E, 138:32–38, 1999
ogy of Diabetes Complications Study. Menzinger G: Autonomic neuropathy 110. Toyry JP, Niskanen LK, Lansimies EA,
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
Diabetes Res Clin Pract 34 (Suppl.): and cardiovascular risk factors in insu- Partanen KPL, Uusitupa MIJ: Autonomic
S165–S171, 1996 lin-dependent and non insulin-depen- neuropathy predicts the development of
88. Sawicki PT, Bender DR, Berger M: Pro- dent diabetes. Diabetes Res Clin Pract 34 stroke in patients with non-insulin-de-
longed QT interval as a predictor of (Suppl. 3):169 –179, 1997 pendent diabetes mellitus. Stroke 27:
mortality in diabetic nephropathy. Dia- 99. Cohen JA, Jeffers BW, Faldut D, 1316 –1318, 1996
betologia 39:77– 81, 1996 Marcoux M, Schrier RW: Risks for sen- 111. Ewing DJ: Diabetic autonomic neuropa-
89. Navarro X, Kennedy WR, Aeppli D, sorimotor peripheral neuropathy and thy and the heart. Diabetes Res Clin Pract
Sutherland DE: Neuropathy and mortal- autonomic neuropathy in non-insulin- 30 (Suppl.)S31–S36, 1996
ity in diabetes: influence of pancreas dependent diabetes mellitus (NIDDM). 112. Fraser DM, Campbell IW, Ewing DJ,
transplantation. Muscle Nerve 19:1009 – Muscle Nerve 21:72– 80, 1998 Murray A, Neilson JM, Clarke BF: Pe-
1016, 1996 100. Menzinger G, Gambardella S, Spallone ripheral and autonomic nerve function
90. Toyry JP, Niskanen LK, Mantysaari MJ, V: The relationship of autonomic neu- in newly diagnosed diabetes mellitus.
Lansimies EA, Uusitupa MIJ: Occur- ropathy to other diabetic complications. Diabetes 26:546 –550, 1977
rence, predictors, and clinical signifi- Diabet Med 10 (Suppl. 2):74S–76S, 1993 113. Vinik AI, Milicevic Z: Recent advances in
cance of autonomic neuropathy in 101. Sivieri R, Veglio M, Chinaglia A, et al.: the diagnosis and treatment of diabetic
NIDDM: ten-year follow-up from the di- Prevalence of QT prolongation in a type neuropathy. Endocrinologist 6:443– 461,
agnosis. Diabetes 45:308 –315, 1996 1 diabetic population and its association 1996
91. Sawicki PT, Kiwitt S, Bender R, Berger with autonomic neuropathy. Diabet Med 114. Javorka K, Javorkova J, Petraskova M, et
M: The value of QT interval dispersion 10:920 –924, 1993 al.: Heart rate variability and cardiovas-
for identification of total mortality risk in 102. Veglio M, Borra M, Stevens LK, Fuller cular tests in young patients with diabe-
non-insulin-dependent diabetes melli- JH, et al.: The relation between QTc tes mellitus type 1. J Pediatr Endocrinol
tus. J Intern Med 243:49 –56, 1998 interval prolongation and diabetic com- Metab 12:423– 431, 1999
92. Veglio M, Sivieri R, Chinaglia A, Scagli- plications: the EURODIAB IDDM Com- 115. Young RJ, Ewing DJ, Clarke BF: Nerve
one L, Cavallo-Perin P: QT interval pro- plications Study Group. Diabetologia 42: function and metabolic control in teen-
longation and mortality in type 1 68 –75, 1999 age diabetics. Diabetes 32:142–147, 1983
diabetic patients: a 5-year cohort pro- 103. Kahn JK, Sisson JC, Vinik AI: Predic- 116. Ewing DJ, Clarke BF: Diabetic auto-
spective study: Neuropathy Study tion of sudden cardiac death in diabetic nomic neuropathy: a clinical viewpoint.
Group of the Italian Society of the Study autonomic neuropathy. J Nucl Med 29: In Diabetic Neuropathy. Dyck PJ, Thomas
of Diabetes, Piemonte Affiliate. Diabetes 1605–1606, 1988 PK, Asbury AK, Weingrad AI, Porte D,
Care 23:1381–1383, 2000 104. Stevens MJ, Raffel DM, Allman KC, Eds. Philadelphia, WB Saunders, 1987,
93. Gerritsen J, Dekker JM, ten Voorde BJ, Dayanikli F, Ficaro E, Sandford T, Wie- p. 66 – 88
Kostense PJ, Heine RJ, Bouter LM, land DM, Pfeifer MA, Schwaiger M: 117. Karavanaki K, Baum JD: Prevalence of
Heethaar RM, Stehouwer CD: Impaired Cardiac sympathetic dysinnervation in microvascular and neurologic abnor-
autonomic function is associated with diabetes: implications for enhanced car- malities in a population of diabetic chil-
increased mortality, especially in sub- diovascular risk. Circulation 98:961–968, dren. J Pediatr Endocrinol 12:411– 422,
jects with diabetes, hypertension, or a 1998 1999
history of cardiovascular disease: the 105. Suarez GA, Kottke TE, Callahan MJ, 118. Low PA, Fealey RD: Sudomotor neurop-
Hoorn Study. Diabetes Care 24:1793– Norell JE, O’Brien PC, Dyck PJ: Is auto- athy: In Diabetic Neuropathy. Dyck PJ,
1798, 2001 nomic neuropathy an important cause of Thomas PK, Asbury AK, Weingrad AI,
94. Chen HS, Hwu CM, Kuo BI, Chiang SC, sudden death in diabetes mellitus? (Ab- Porte D, Eds. Philadelphia, WB Saun-
Kwok CF, Lee SH, Lee YS, Weih MJ, stract) Neurology 56 (Suppl. 3):A208, ders, 1987, p. 140 –145
Hsiao LC, Lin SH, Ho LT: Abnormal car- 2001 119. DePonti F, Fealey RD, Malagelada JR:
diovascular reflex tests are predictors of 106. Johnson BF, Nesto R, Pfeifer M, Slater Gastrointestinal syndromes due to dia-
mortality in type 2 diabetes mellitus. W, Vinik A, Wackers F, Young L: betes mellitus. In Diabetic Neuropathy.
Diabet Med 18:268 –273, 2001 Systolic and diastolic dysfunction in di- Dyck PJ, Thomas PK, Asbury AK, Wein-
94a.Maser RE, Mitchell BD, Vinik AI, Free- abetic patients with neuropathy (Ab- grad AI, Porte D, Eds. Philadelphia, WB
man R: The association between cardio- stract). Diabetes 46 (Suppl. 1):314A, 1997 Saunders, 1987, p. 155–161
vascular autonomic neuropathy and 107. Miettinen H, Lehto S, Salomaa V, Ma- 120. Smith SA, Smith SE: Assessment of pu-
mortality in individuals with diabetes. honen M, Niemela M, Haffner SM, pillary function in diabetic neuropathy.
Diabetes Care. In press Pyorala K, Tuomilehto J: Impact of In Diabetic Neuropathy. Dyck PJ, Thomas
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1577
Technical Review
PK, Asbury AK, Weingrad AI, Porte D, 135. McCulloch DK, Campbell IW, Wu FC, 147. Cryer PE: Iatrogenic hypoglycemia as a
Eds. Philadelphia, WB Saunders, 1987, Prescott RJ, Clarke BF: The prevalence cause of hypoglycemia-associated auto-
p. 134 –139 of diabetic impotence. Diabetologia 18: nomic failure in IDDM: a vicious cycle.
121. Levitt NS, Stansberry KB, Wynchank S, 279 –283, 1980 Diabetes 41:255–260, 1992
Vinik AI: The natural progression of au- 136. Feldman HA, Goldstein I, Hatzichristou 148. Dagogo-Jack SE, Craft S, Cryer PE:
tonomic neuropathy and autonomic DG, Krane RJ, McKinlay JB: Impotence Hypoglycemia-associated autonomic
function tests in a cohort of people with and its medical and psychosocial corre- failure in insulin-dependent diabetes
IDDM. Diabetes Care 19:751–754, 1996 lates: results of the Massachusetts Male mellitus: recent antecedent hypoglyce-
122. Farup CE, Leidy NK, Murray M, Wil- Aging Study. J Urol 151:54 – 61, 1994 mia reduces autonomic responses to,
liams GR, Helbers L, Quigley EMM: Ef- 137. Bacon CG, Hu FB, Giovannucci E, symptoms of, and defense against subse-
fect of domperidone on the health- Glasser DB, Mittleman MA, Rimm EB: quent hypoglycemia. J Clin Invest 91:
related quality of life of patients with Association of type and duration of dia- 819 – 828, 1993
symptoms of diabetic gastroparesis. Di- betes with erectile dysfunction in a large 149. Cryer PE: Hypoglycemia-associated
abetes Care 21:1699 –1706, 1998 cohort of men. Diabetes Care 25:1458 – autonomic failure in diabetes. Am J
123. Channer KS, Jackson PC, O’Brien I, Cor- 1463, 2002 Physiol Endocrinol Metab 281:E1115–
rall RJ, Coles DR, Davies ER, Virjee JP: 138. Vinik AI, Richardson D: Erectile dys- E1121, 2001
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
Oesophageal function in diabetes melli- function in diabetes. Diabetes Reviews 150. Hoeldtke RD, Boden G: Epinephrine
tus and its association with autonomic 6:16 –33, 1998 secretion, hypoglycemia unawareness,
neuropathy. Diabet Med 2:378 –382, 1985 139. Enzlin P, Mathieu C, Vanderschueren D, and diabetic autonomic neuropathy.
124. Kong MF, Horowitz M, Jones KL, Demyttenaere K: Diabetes mellitus and Ann Intern Med 120:512–517, 1994
Wishart JM, Harding PE: Natural history female sexuality: a review of 25 years’ 151. Stephenson JM, Kempler P, Perin PC,
of diabetic gastroparesis. Diabetes Care research. Diabet Med 15:809 – 815, 1998 Fuller JH: Is autonomic neuropathy a
22:503–507, 1999 140. Bosman DR, Osborne CA, Marsden JT, risk factor for severe hypoglycaemia?
125. Horowitz M, Edelbroek M, Fraser R, Macdougall IC, Gardner WN, Watkins The EURODIAB IDDM Complications
Maddox A, Wishart J: Disordered gastric PJ: Erythropoietin response to hypoxia Study. Diabetologia 39:1372–1376, 1996
motor function in diabetes mellitus: in patients with diabetic autonomic neu- 152. Low P, Lagerlund TD, McManis PG:
recent insights into prevalence, patho- ropathy and non-diabetic chronic renal Nerve blood flow and oxygen delivery in
physiology, clinical relevance and treat- failure. Diabet Med 19:65– 69, 2002 normal, diabetic, and ischemic neurop-
ment. Scand J Gastroenterol 26:673– 684, 141. Robertson D, Krantz SB, Biaggioni I, athy. Int Rev Neurobiol 31:355– 438, 1989
1991 Robertson D: The anemia of micrograv- 153. Stansberry KB, Hill MA, Shapiro SA, Mc-
126. Schiller LR, Santa Ana CA, Schmulen ity and recumbency: role of sympathetic Nitt PM, Bhatt BA, Vinik AI: Impairment
AC, Hendler RS, Harford WV, Fordtran neural control of erythropoietin produc- of peripheral blood flow responses in di-
JS: Pathogenesis of fecal incontinence in tion. Acta Astronautica 33:137–141, 1994 abetes resembles an enhanced aging ef-
diabetes mellitus: evidence for internal- 142. Ryder RE, Owens DR, Hayes TM, Gha- fect. Diabetes Care 20:1711–1716, 1997
anal-sphincter dysfunction. N Engl J Med tei MA, Bloom SR: Unawareness of 154. Stansberry KB, Peppard HR, Babyak LM,
307:1666 –1671, 1982 hypoglycaemia and inadequate hypo- Popp G, McNitt PM, Vinik AI: Primary
127. Neumann C, Schmid H: Relationship glycaemic counterregulation: no causal nociceptive afferents mediate the blood
between the degree of cardiovascular au- relation with diabetic autonomic neu- flow dysfunction in non-glabrous (hairy)
tonomic dysfunction and symptoms of ropathy. Br Med J 301:783–787, 1990 skin of type 2 diabetes: a new model for
neuropathy and other complications of 143. Hepburn DA, Patrick AW, Eadington the pathogenesis of microvascular dys-
diabetes mellitus. Braz J Med Biol Res 28: DW, Ewing DJ, Frier BM: Unawareness function. Diabetes Care 22:1549 –1554,
751–757, 1995 of hypoglycaemia in insulin-treated dia- 1999
128. Blaivas JG: The neurophysiology of mic- betic patients: prevalence and relation- 155. Boyko EJ, Ahroni JH, Stensel V, Forsberg
turition: a clinical study of 550 patients. ship to autonomic neuropathy. Diabet RC, Davignon DR, Smith DG: A pro-
J Urol 127:958 –963, 1982 Med 7:711–717, 1990 spective study of risk factors for diabetic
129. Ellenberg M: Development of urinary 144. Bottini P, Boschetti E, Pampanelli S, foot ulcer: the Seattle Diabetic Foot
bladder dysfunction in diabetes melli- Ciofetta M, Del Sindaco P, Scionti L, Study. Diabetes Care 22:1036 –1042,
tus. Ann Intern Med 92:321–323, 1980 Brunetti P, Bolli GB: Contribution of au- 1999
130. Bradley WE: Diagnosis of urinary blad- tonomic neuropathy to reduced plasma 156. Young MJ, Marshall A, Adams JE, Selby
der dysfunction in diabetes mellitus. adrenaline responses to hypoglycemia in PL, Boulton AJM: Osteopenia, neurolog-
Ann Intern Med 92:323–326, 1980 IDDM: evidence for a nonselective de- ical dysfunction, and the development
131. Beylot M, Marion D, Noel G: Ultrasono- fect. Diabetes 46:814 – 823, 1997 of charcot neuroarthropathy. Diabetes
graphic determination of residual urine 145. Fanelli C, Pampanelli S, Lalli C, Del Sin- Care 18:34 –38, 1995
in diabetic subjects: relationship to neu- daco P, Ciofetta M, Lepore M, Porcellati 157. American Diabetes Association and
ropathy and urinary tract infection. Dia- F, Bottini P, Di Vincenzo A, Brunetti P, American Academy of Neurology: Pro-
betes Care 5:501–505, 1982 Bolli GB: Long-term intensive therapy ceedings of a consensus development
132. Norden G, Granerus G, Nyberg G: Dia- of IDDM patients with clinically overt conference on standardized measures in
betic cystopathy: a risk factor in diabetic autonomic neuropathy: effects on hypo- diabetic neuropathy. Diabetes Care 15:
nephropathy? J Diabet Complications glycemia awareness and counterregula- 1080 –1107, 1992
2:203–206, 1988 tion. Diabetes 46:1172–1181, 1997 158. Pfeifer MA, Cook D, Brodsky J, Tice D,
133. Frimodt-Moller C, Mortensen S: Treat- 146. Meyer C, Grossmann R, Mitrakou A, Reenan A, Swedine S, Halter JB, Porte D
ment of diabetic cystopathy. Ann Intern Mahler R, Veneman T, Gerich J, Bretzel Jr: Quantitative evaluation of cardiac
Med 92:327–328, 1980 RG: Effects of autonomic neuropathy on parasympathetic activity in normal and
134. Ioanid CP, Noica N: Incidence and diag- counterregulation and awareness of hy- diabetic man. Diabetes 31:339 –345, 1982
nostic aspects of the bladder disorders in poglycemia in type 1 diabetic patients. 159. Ewing DJ, Campbell IW, Murray H,
diabetics. Eur Urol 7:211–214, 1981 Diabetes Care 21:1960 –1966, 1998 Neilson JM, Clarke BF: Immediate heart-
1578 DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003
Vinik and Associates
rate response to standing: simple test for 1217–1221, 1980 and future. Diabetes 44:1355–1361,
autonomic neuropathy in diabetes. BMJ 171. Sundkvist G: Autonomic nervous func- 1995
1:145–147, 1978 tion in asymptomatic diabetic patients 183. Feldman EL, Stevens MJ, Greene DA:
160. Borst C, Weiling W, van Brederode JFM, with signs of peripheral neuropathy. Di- Pathogenesis of diabetic neuropathy.
Hond A, DeRijk LG, Dunning AJ: Mech- abetes Care 4:529 –534, 1981 Clin Neurosci 4:365–370, 1997
anisms of initial heart rate response to 172. Weinberg CR, Pfeifer MA: Development 184. Low PA, Nickander KK: Oxygen free
postural change. Am J Physiol 243: of a predictive model for symptomatic radical effects in sciatic nerve in experi-
H676 –H681, 1982 neuropathy in diabetes. Diabetes 35: mental diabetes. Diabetes 40:873– 877,
161. Ziegler D, Laux G, Dannehl K, Spuler M, 873– 880, 1986 1991
et al.: Assessment of cardiovascular au- 173. Mustonen J, Uusitipa M, Mantysaari M, 185. Ziegler D, Reljanovic M, Mehnert H,
tonomic function: age-related normal et al.: Changes in autonomic nervous Gries FA: Alpha-lipoic acid in the treat-
ranges and reproducibility of spectral function during the 4-year follow-up in ment of diabetic polyneuropathy in Ger-
analysis, vector analysis, and standard middle-aged diabetic and nondiabetic many: current evidence from clinical
tests of heart rate variation and blood subjects initially free of coronary heart trials. Exp Clin Endocrinol Diabetes 107:
pressure responses. Diabet Med 9:166 – disease. J Intern Med 241:227–235, 1997 421– 430, 1999
175, 1992 174. Knowler WC, Barrett-Connor E, Fowler 186. Manzella D, Barbieri M, Ragno E,
Downloaded from http://diabetesjournals.org/care/article-pdf/26/5/1553/592892/dc0503001553.pdf by guest on 03 November 2022
162. Sandroni P, Benarroch EE, Low PA: SE, Hamman RE, Lachin JM, Walker EA, Paolisso G: Chronic administration of
Pharmacological dissection of compo- Nathan DM: Reduction in the incidence pharmacologic doses of vitamin E im-
nents of the Valsalva maneuver in ad- of type 2 diabetes with lifestyle interven- proves the cardiac autonomic nervous
renergic failure. J Appl Physiol 71: tion or metformin. N Engl J Med 346: system in patients with type 2 diabetes.
1563–1567, 1991 393– 403, 2002 Am J Clin Nutr 73:1052–1057, 2001
163. American Academy of Neurology Ther- 175. Wein TH, Albers JW: Diabetic neuropa- 187. Kontopoulos AG, Athyros VG, Didange-
apeutics and Technology Assessment thies. Phys Med Rehabil Clin N Am 12: los TP, Papageorgiou AA, Avramidis MJ,
Subcommittee: Assessment: clinical au- 307–320, 2001 Mayroudi MC, Karamitsos DT: Effect of
tonomic testing report. Neurology 46: 176. Karavanaki-Karanassiou K: Autonomic chronic quinapril administration on
873– 880, 1996 neuropathy in children and adolescents
heart rate variability in patients with di-
164. Pfeifer MA, Schumer MP, Gelber DA: Al- with diabetes mellitus. J Pediatr Endocri-
abetic autonomic neuropathy. Diabetes
dose reductase inhibitors: the end of an nol Metab 14 (Suppl. 5):1379 –1386,
Care 20:355–361, 1997
era or the need for different trial designs? 2001
188. Malik RA, Williamson S, Abbott C, Car-
Diabetes 46 (Suppl. 2):S82–S89, 1997 177. Massin MM, Derkenne B, Tallsund M,
rington AL, Iqbal J, Schady W, et al.:
165. Task Force of the European Society of Rocour-Brumioul D, Ernould C, Leb-
Effect of angiotensin-converting-en-
Cardiology and the North American So- rethon MC, Bourguignon JP: Cardiac
ciety of Pacing and Electrophysiology: autonomic dysfunction in diabetic chil- zyme (ACE) inhibitor trandolapril on
Heart rate variability: standards of dren. Diabetes Care 22:1845–1850, 1999 human diabetic neuropathy: random-
measurement, physiological interpre- 178. DCCT Research Group: Factors in de- ised double-blind controlled trial. Lancet
tation and clinical use. Circulation 93: velopment of diabetic neuropathy. Base- 352:1978 –1981, 1998
1043–1065, 1996 line analysis of neuropathy in feasibility 189. Ebbehoj E, Poulsen PL, Hansen KW,
166. Freeman R, Saul P, Roberts M, Berger phase of Diabetes Control and Compli- Knudsen ST, Molgaard H, Mogensen
RD, Broadbridge C, Cohen R: Spectral cations Trial (DCCT). Diabetes 37:476 – CE: Effects on heart rate variability of
analysis of heart rate in diabetic auto- 481, 1988 metoprolol supplementary to on going
nomic neuropathy. Arch Neurol 48:185– 179. Jaffe RS, Aoki TT, Rohatsch PL, Disbrow ACE-inhibitor treatment in type I dia-
190, 1991 EA, Fung DL: Predicting cardiac auto- betic patients with abnormal albumin-
167. Howorka K, Pumprla J, Schabmann A: nomic neuropathy in type 1 (insulin-de- uria. Diabetologia 45:965–975, 2002
Optimal parameters for short-term heart pendent) diabetes mellitus. Clin Auton 190. Singleton JR, Smith AG, Bromberg MB:
rate spectrogram for routine evaluation Res 5:155–158, 1995 Painful sensory polyneuropathy associ-
of diabetic cardiovascular autonomic 180. May O, Arildsen H, Damsgaard EM, ated with impaired glucose tolerance.
neuropathy. J Auton Nerv Syst 69:164 – Mickley H: Cardiovascular autonomic Muscle Nerve 24:1225–1228, 2001
172, 1998 neuropathy in insulin-dependent diabe- 191. Sochett E, Daneman D: Early diabetes-
168. Vinik AI, Suwanwalaikorn S: Autonomic tes mellitus: prevalence and estimated related complications in children and
neuropathy. In Current Therapy of Dia- risk of coronary heart disease in the gen- adolescents with type 1 diabetes: impli-
betes Mellitus. De Fronzo RM, Ed. St. eral population. J Intern Med 248:483– cations for screening and intervention.
Louis, MO, Yearbook, 1997, p. 165–176 491, 2000 Endocrinol Metab Clin North Am 28:865–
169. Vinik AI, Holland MT, Le Beau JM, Li- 181. Clark CM, Vinicor F: Introduction: 882, 1999
uzzi FJ, Stansberry KB, Colen LB: Dia- Risks and benefits of intensive manage- 192. Howorka K, Pumprla J, Haber P, et al.:
betic neuropathies. Diabetes Care 15: ment in non-insulin-dependent diabetes Effects of physical training on heart rate
1926 –1975, 1992 mellitus: the fifth Regenstrief confer- variability in diabetic patients with vari-
170. Battle WM, Snape WJ Jr, Alavi A, Cohen ence. Ann Intern Med 124:81– 85, 1996 ous degrees of cardiovascular autonomic
S, Braunstein S: Colonic dysfunction in 182. Pfeifer MA, Schumer MP: Clinical trials neuropathy. Cardiovascular Res 34:206 –
diabetes mellitus. Gastroenterology 79: of diabetic neuropathy: past, present, 214, 1997
DIABETES CARE, VOLUME 26, NUMBER 5, MAY 2003 1579
You might also like
- Direct Social Work Practice Theory and Skills 10th Edition Hepworth Test BankDocument7 pagesDirect Social Work Practice Theory and Skills 10th Edition Hepworth Test BankCrystalBrowncpzky100% (17)
- Hypnotherapy ScriptsDocument109 pagesHypnotherapy ScriptsSabina Lupasco97% (30)
- How To Start A Niche Staffing or Recruiting Business - Discover Your NicheDocument30 pagesHow To Start A Niche Staffing or Recruiting Business - Discover Your NicheDee Williams67% (3)
- Jurnal Fix IpdDocument4 pagesJurnal Fix IpdDea Melinda SabilaNo ratings yet
- Evaluation of Chronic Renal Disease, A Staged ApproachDocument8 pagesEvaluation of Chronic Renal Disease, A Staged Approachtaner_soysurenNo ratings yet
- Cleveland Clinic Journal of Medicine 2008 KIMYOUNOSSI 721 8faal2Document8 pagesCleveland Clinic Journal of Medicine 2008 KIMYOUNOSSI 721 8faal2wira_meganNo ratings yet
- Drug Liver InjuryDocument21 pagesDrug Liver Injurymade dedyNo ratings yet
- TVP-2020-1112 Managing Feline Urethral ObstructionDocument6 pagesTVP-2020-1112 Managing Feline Urethral ObstructionLucas Dos Santos MacedoNo ratings yet
- 2011 - AASLD - Management of Acute Liver FailureDocument22 pages2011 - AASLD - Management of Acute Liver FailuremohamedelsayedelmenyawyNo ratings yet
- Merec Briefing No32Document8 pagesMerec Briefing No32Riefka Ananda ZulfaNo ratings yet
- Harrisons Principles of Internal Medicine 21st Edition Vol 1 Vol Split PDF 1694700703964Document73 pagesHarrisons Principles of Internal Medicine 21st Edition Vol 1 Vol Split PDF 1694700703964Clorinda RodriguezNo ratings yet
- Tgi Erc 2Document13 pagesTgi Erc 2Adrian LaimeNo ratings yet
- Chronic Kidney Disease: SeminarDocument16 pagesChronic Kidney Disease: SeminarMichael Meng100% (1)
- HshsjneDocument5 pagesHshsjneyunia habsariNo ratings yet
- Geographical Differences The Prevalence of Dyspepsia: Key WordsDocument8 pagesGeographical Differences The Prevalence of Dyspepsia: Key WordsAndhi Riawan Eko WiikramatunggadewaNo ratings yet
- Early Detection of Eating Disorders in General PracticeDocument7 pagesEarly Detection of Eating Disorders in General PracticeManny RosengallegosNo ratings yet
- Epidemiology of Chronic Kidney Disease Among Older Adults: A Focus On The Oldest OldDocument8 pagesEpidemiology of Chronic Kidney Disease Among Older Adults: A Focus On The Oldest Oldkhangha.ptNo ratings yet
- Diagnosis and Management of Acute Pancreatitis andDocument11 pagesDiagnosis and Management of Acute Pancreatitis andMarcelitaTaliaDuwiriNo ratings yet
- Higado GrasoDocument13 pagesHigado GrasoMarisol MolinaNo ratings yet
- Review: Treatment of Constipation in Older PeopleDocument8 pagesReview: Treatment of Constipation in Older PeopleMohd ZulAmirulNo ratings yet
- ACG Clinical Guideline: Chronic PancreatitisDocument18 pagesACG Clinical Guideline: Chronic PancreatitisRene CordovaNo ratings yet
- Nejmcp 2114026Document10 pagesNejmcp 2114026Engin AltınkayaNo ratings yet
- Insuficiencia Renal CronicaDocument13 pagesInsuficiencia Renal CronicaCarlos DNo ratings yet
- Pruebas de Funcion Hepatica AnormalDocument17 pagesPruebas de Funcion Hepatica AnormalMedicina InternaNo ratings yet
- The British Society of Gastroenterology/UK-PBC Primary Biliary Cholangitis Treatment and Management GuidelinesDocument27 pagesThe British Society of Gastroenterology/UK-PBC Primary Biliary Cholangitis Treatment and Management GuidelinesAnonymous zZrGTONhNo ratings yet
- IsbelDocument7 pagesIsbelCaity YoungNo ratings yet
- Erge NejmDocument10 pagesErge Nejmliz salcedoNo ratings yet
- Nonalcoholic Fatty Liver Disease: NafldDocument1 pageNonalcoholic Fatty Liver Disease: NafldleandroNo ratings yet
- Pharmacotherapy in Chronic Kidney Disease Patients Presenting With Acute Coronary SyndromeDocument27 pagesPharmacotherapy in Chronic Kidney Disease Patients Presenting With Acute Coronary SyndromeaudiNo ratings yet
- Harrisons Principles of Internal Medicine Vol.1 Vol.2 20th Edition2018 Original PDF 3 157 167Document11 pagesHarrisons Principles of Internal Medicine Vol.1 Vol.2 20th Edition2018 Original PDF 3 157 167William MilesNo ratings yet
- GatroDocument48 pagesGatronainggolan Debora15No ratings yet
- Functional Dyspepsia: Review ArticleDocument11 pagesFunctional Dyspepsia: Review Articlejenny puentesNo ratings yet
- NAFLD-dr. Masrul KuliahDocument103 pagesNAFLD-dr. Masrul KuliahAndrie WigunaNo ratings yet
- Nejmcp 2114026Document10 pagesNejmcp 2114026Cristina Adriana PopaNo ratings yet
- Perlemakan Hati Non-AlkoholikDocument5 pagesPerlemakan Hati Non-AlkoholikChristinaNo ratings yet
- British Society of Gastroenterology Guidelines On The Management of Functional DyspepsiaDocument27 pagesBritish Society of Gastroenterology Guidelines On The Management of Functional DyspepsiaRicardo PaterninaNo ratings yet
- Glomerulonefritis Primaria Medicine 2015Document6 pagesGlomerulonefritis Primaria Medicine 2015Francisco Rebollar GarduñoNo ratings yet
- Simoneau 1994Document11 pagesSimoneau 1994Monica ViverosNo ratings yet
- Diabetic Neuropathy in ChildrenDocument14 pagesDiabetic Neuropathy in Childrensucca07No ratings yet
- Emergency in KADDocument4 pagesEmergency in KADxbkjbhrqkjNo ratings yet
- Pamw 2011-1-2 48-Stompor 0Document6 pagesPamw 2011-1-2 48-Stompor 0Ners SenNo ratings yet
- Standard Baru Kriteria Diabetes 2010Document51 pagesStandard Baru Kriteria Diabetes 2010Tina MultazamiNo ratings yet
- Clinical - Liver: Simple Noninvasive Systems Predict Long-Term Outcomes of Patients With Nonalcoholic Fatty Liver DiseaseDocument12 pagesClinical - Liver: Simple Noninvasive Systems Predict Long-Term Outcomes of Patients With Nonalcoholic Fatty Liver Disease走过一些路No ratings yet
- HIgado GrasoDocument6 pagesHIgado GrasoWilson Suarez VenturaNo ratings yet
- Ibs JurnalDocument11 pagesIbs JurnalimuhammadfahmiNo ratings yet
- Headache: General PrinciplesDocument5 pagesHeadache: General PrinciplesAl Glen EgarleNo ratings yet
- Advances in Understanding The Progression of Non-Alcoholic Fatty Liver Disease To Non-Alcoholic Steatohepatitis: A Comprehensive ReviewDocument7 pagesAdvances in Understanding The Progression of Non-Alcoholic Fatty Liver Disease To Non-Alcoholic Steatohepatitis: A Comprehensive ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- British Society Guidelines Functional DyspepsiaDocument27 pagesBritish Society Guidelines Functional DyspepsiagigiNo ratings yet
- Desórdenes GastrointestinalesDocument11 pagesDesórdenes GastrointestinalesSMIBA MedicinaNo ratings yet
- A Clinical Overview of Non-Alcoholic Fatty Liver Disease A GuideDocument12 pagesA Clinical Overview of Non-Alcoholic Fatty Liver Disease A GuideAnindya RosmaNo ratings yet
- Piis0016508507005914 PDFDocument23 pagesPiis0016508507005914 PDFHeidy Bravo RamosNo ratings yet
- DispepsiaDocument11 pagesDispepsiaPendikNo ratings yet
- CKD PDFDocument6 pagesCKD PDFmkafabillahNo ratings yet
- Nash: Advances in Evaluation and Management: Rakesh K TandonDocument6 pagesNash: Advances in Evaluation and Management: Rakesh K TandonSrinivas GokulnathNo ratings yet
- CKD Lancet 2021Document17 pagesCKD Lancet 2021Fabiola AlonsoNo ratings yet
- 10 1056@NEJMra1505202 PDFDocument10 pages10 1056@NEJMra1505202 PDFFiorella ChambiNo ratings yet
- Canine Chronic Kidney Disease Current Diagnostics & Goals For Long-Term ManagementDocument7 pagesCanine Chronic Kidney Disease Current Diagnostics & Goals For Long-Term ManagementJuni ClaudiaNo ratings yet
- Restoring Chronic Kidney Disease : Restoring, Preserving, and Improving CKD to Avoid DialysisFrom EverandRestoring Chronic Kidney Disease : Restoring, Preserving, and Improving CKD to Avoid DialysisNo ratings yet
- Liver Cell CancerFrom EverandLiver Cell CancerH.M. CameronRating: 5 out of 5 stars5/5 (1)
- Evidence-Based Gastroenterology and HepatologyFrom EverandEvidence-Based Gastroenterology and HepatologyJohn W. D. McDonaldNo ratings yet
- Eia Assignment No. 2Document8 pagesEia Assignment No. 2Swati GuptaNo ratings yet
- Ma 4001 Lyo 5 DcuiDocument2 pagesMa 4001 Lyo 5 DcuirestandcleanaguachicaNo ratings yet
- Ivermectin Potential Candidate For The Treatment of Covid 19Document3 pagesIvermectin Potential Candidate For The Treatment of Covid 19glenwell sentosaNo ratings yet
- Errors and The CBC Result 2.0Document43 pagesErrors and The CBC Result 2.0Ella OrtegaNo ratings yet
- Latin American Forensic Odontology: A Scoping Review of Its Current Research and The Objective/Subjective Nature of Its StudiesDocument12 pagesLatin American Forensic Odontology: A Scoping Review of Its Current Research and The Objective/Subjective Nature of Its StudiesTarsila LopesNo ratings yet
- BOSH Lecture 1 - HistoryDocument12 pagesBOSH Lecture 1 - HistoryVitaliana VillaverdeNo ratings yet
- Macro Calculator - Anna VictoriaDocument2 pagesMacro Calculator - Anna VictoriaDonnaNo ratings yet
- Nurs490 Safety Performance Improvement Paper Neuburg IntroDocument2 pagesNurs490 Safety Performance Improvement Paper Neuburg Introapi-452041818No ratings yet
- Patho QuestDocument4 pagesPatho QuestRosel Ann BontiaNo ratings yet
- Quiz MH, Rhabdo, PRISDocument1 pageQuiz MH, Rhabdo, PRISRicky JalecoNo ratings yet
- Amiodarone Guideline For Use and MonitoringDocument8 pagesAmiodarone Guideline For Use and MonitoringTania NicolaescuNo ratings yet
- Behavioural Management in Children (Compatibility Mode)Document25 pagesBehavioural Management in Children (Compatibility Mode)haneeneeNo ratings yet
- The Language Instinct (Steven Pinker) : Chapter 1: An Instinct To Acquire An ArtDocument4 pagesThe Language Instinct (Steven Pinker) : Chapter 1: An Instinct To Acquire An ArtPablo MartínNo ratings yet
- CHED Regional Memorandum No. 3, S. 2021Document6 pagesCHED Regional Memorandum No. 3, S. 2021Amy uretaNo ratings yet
- Multiple Pregnancy NOR PosterDocument1 pageMultiple Pregnancy NOR PosterbigbossNo ratings yet
- Research MethodologyDocument34 pagesResearch MethodologyAkash mathewNo ratings yet
- HrishabhDocument1 pageHrishabhPramathesh SharmaNo ratings yet
- Kiran Mazumdar ShawDocument13 pagesKiran Mazumdar ShawInjimamul IslamNo ratings yet
- TFS Audit Program V2.0Document29 pagesTFS Audit Program V2.0kanji63No ratings yet
- Rad - Tech CpdprogramDocument11 pagesRad - Tech CpdprogramPRC BoardNo ratings yet
- Healthcare Project in AdidomeDocument20 pagesHealthcare Project in Adidomeamode idowuNo ratings yet
- Natural Language Processing and ML Based Student Mental Health Analysis Using Non Clinical Texts PDFDocument53 pagesNatural Language Processing and ML Based Student Mental Health Analysis Using Non Clinical Texts PDFRakibul Îslam DeepuNo ratings yet
- Grievance StatusDocument2 pagesGrievance StatusfirmarnahikhayegatuNo ratings yet
- Plab 1 Mock 5th March 2017Document35 pagesPlab 1 Mock 5th March 2017RabeeyaNo ratings yet
- Simpson AffidavitDocument55 pagesSimpson AffidavitCalgary HeraldNo ratings yet
- Lapsus - Asrarudin - BPHDocument18 pagesLapsus - Asrarudin - BPHAsrarudin HamidNo ratings yet
- Lesson 01 - PE and Health 4Document6 pagesLesson 01 - PE and Health 4Andrea Gamutan100% (1)