Professional Documents
Culture Documents
Postural Instability in Patients with Diabetic Sensory Neuropathy
Uploaded by
Monica ViverosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Postural Instability in Patients with Diabetic Sensory Neuropathy
Uploaded by
Monica ViverosCopyright:
Available Formats
N A L A R T I C L E
Postural Instability in
Patients with Diabetic
I t is well known to those who treat pa-
tients with diabetic distal symmetrical
polyneuropathy that these patients will
occasionally complain of instability while
walking or standing (1,2). Instability
Sensory Neuropathy could have many causes (such as central
nervous system [CNS] dysfunction, de-
GUY G. SIMONEAU, PHD MARY B. BECKER, RN creased lower-extremity strength, visual
JAN S. ULBRECHT, MB, BS PETER R. CAVANAGH, PHD deficits, etc.), but in the diabetic patient
JANICE A. DERR, PHD with sensory neuropathy, it is usually at-
tributed principally to the lack of ade-
quate proprioceptive feedback from the
OBJECTIVE — Recent survey evidence suggests that sensory ataxia due to diabetic lower extremities and is labeled sensory
neuropathy may be a more frequent and serious problem than is commonly recog- ataxia (1,2). Although significant anec-
nized. This view is further supported by research that confirms the major contribution dotal evidence of this problem exists (2),
of the somatosensory system to the control of posture. We therefore sought to deter- there is, at present, little quantitative evi-
mine the effects of significant diabetic distal symmetrical polyneuropathy on the con- dence in a well-characterized sample to
trol of posture. determine the magnitude of the effect ( 3 -
RESEARCH DESIGN A N D M E T H O D S — Fifty-one subjects, divided into 5). In addition, clinically significant sen-
three groups, participated in this study. Seventeen had diabetes and significant sensory sory ataxia is thought to be relatively rare
neuropathy, 17 had diabetes and no neuropathy, and 17 had neither diabetes nor (1,2), a perspective that may not be cor-
neuropathy. The subjects were matched across groups, and stringent exclusion criteria rect (4). In this study, therefore, we set
were applied. Postural stability during quiet standing was measured using a force out to measure postural stability among
platform. In addition to electrophysiological and quantitative sensory tests of neurop- patients with diabetic distal symmetrical
athy, a number of physical and functional characteristics were measured for all subjects. polyneuropathy during stance and to de-
termine the physical and sensory charac-
RESULTS— Postural instability was found to be significantly associated with sen- teristics that may be most predictive of
sory neuropathy, but not with diabetes per se. Patients with sensory neuropathy dem- instability in this population. The patients
onstrated between 66 and 117% more instability than did control subjects (depending were not selected for complaints of insta-
on the testing condition). Based on multiple linear regression analyses, the most sig- bility.
nificant correlates of instability were the quantitative sensory measures of neuropathy
and age.
CONCLUSIONS — The loss of sensory perception secondary to diabetic distal RESEARCH DESIGN AND
symmetrical sensory neuropathy has a markedly detrimental effect on postural stabil- M E T H O D S — Fifty-one subjects, di-
ity. The deficit is greatest when visual or vestibular cues are absent or degraded. vided into three groups (n = 17 per
Patients with neuropathy need to be informed of the postural consequences of this group), were studied. Group 1 was se-
condition to limit the potential morbidity caused by falls. lected to have diabetes and neuropathy
(DM-NP), group 2 to have diabetes but no
significant neuropathy (DM-nonNP), and
From the Program in Physical Therapy (G.G.S.), Marquette University, Milwaukee, Wisconsin, group 3 to have neither diabetes nor neu-
and The Center for Locomotion Studies (J-S.U., M.B.B., P.R.C.) and the Department of Statistics ropathy (nonDM). The majority of the
(J.A.D.), Penn State University, University Park, Pennsylvania. subjects with diabetes were recruited
Address correspondence and reprint requests to Peter R. Cavanagh, PhD, The Center for from a specialty diabetes clinic, and a few
Locomotion Studies, Room 10, Intramural Building, Penn State University, University Park, PA
16802. subjects with diabetes and all of the non-
Received for publication 12 December 1993 and accepted in revised form 30 June 1994. diabetic control subjects were recruited
CNS, central nervous system; DM-NP, subjects with diabetes and neuropathy; DM-nonNP, through advertising. Significant periph-
subjects with diabetes and no significant neuropathy; nonDM, subjects with neither diabetes nor eral sensory neuropathy was defined as
neuropathy; VPT, vibratory perception threshold; NIDDM, non-insulin-dependent diabetes the average vibratory perception thresh-
mellitus; IDDM, insulin-dependent diabetes mellitus; SLR, sensory latency response; MNCV,
motor nerve conduction velocity; SW, Semmes-Weinstein; JMPT, joint movement perception old (VPT) for the halluces being equal to,
threshold; VCS, visual contrast sensitivity; ROM, range of movement; CoP, center of pressure; or exceeding, the age-adjusted normal
ANOVA, analysis of variance. VPT values published by Bloom et al. (7)
(the upper limit of normal was defined by
DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994 1411
Posture and diabetic sensory neuropathy
Table 1—Exclusion criteria measured in the diabetic subjects. Motor
1. Regular use of medications affecting the central or peripheral nervous system or muscular function tests included manual and hand-
function and likely to have an impact on postural stability measurements (medications held dynamometric assessment of
allowed were limited to angiotensin-converting enzyme inhibitors, antiarrhythmics, strength of the lower-extremity muscula-
antibiotics, nonsteroidal anti-inflammatory drugs, calcium channel blockers, cardiac ture together with motor nerve conduc-
glycosides, diuretics, H2 receptor blockers, hormones, lipid-lowering agents, nitrates) tion velocity (MNCV) testing of the pero-
2. Significant weakness of the lower-extremity musculature, including weakness due to neal nerve in the DM groups.
diabetic distal motor neuropathy or disuse
VPT on the plantar surface of both
3. A history of neurological diseases (other than peripheral neuropathy attributed to
halluces was tested using a fixed-fre-
diabetes) likely to affect lower-extremity function or posture, including, but not limited
to, peripheral nerve compression, focal neuropathies, radiculopathies, strokes, and quency (60 Hz) variable amplitude vibro-
Parkinson's disease meter (Biothesiometer, Bio-Medical In-
4. Visual acuity <20/100, loss of binocular vision, or presence of double vision (diabetic strument, Newbury, OH) using the
retinopathy per se was not an exclusion) method of limits protocol (7,9), with an
5. Abnormal clinical evaluation of vestibular function upper limit value of 50 V. The full set of
6. Weight outside - 2 0 to - 3 3 % ideal body weight (46) 20 Semmes-Weinstein (SW) monofila-
7. Inability to abstain from alcohol on the day of testing; history of drug or alcohol ments (ranging from 1.65 to 6.65: these
dependency or of medical treatment for drug or alcohol dependency numbers represent logg of 10 times the
8. Inability to abstain from caffeine for 6 h before testing of postural stability
buckling force in grams; the higher the
9. A history of psychological/psychiatric conditions requiring medical attention
10. Clinically apparent significant abnormalities (deformity, abnormal range of motion, etc.)
number, the worse the neuropathy) was
of the back, hip, knee, ankle, or foot used for evaluating touch-pressure sensa-
11. Any arthritic conditions causing frequent pain, discomfort, and difficulty walking or tion following the protocol of Sosenko et
standing al. (10). For data analysis, the SW rating
12. A history of major surgical procedures, major fractures, or other musculoskeletal and VPT values obtained for the right and
problems likely to affect lower-extremity function and posture left halluces were averaged.
13. Any previous illness, surgery, or other characteristic(s) that might, in the opinion of the To quantify joint movement per-
investigator, interfere with lower-extremity function, postural mechanism, or the subject's
ception threshold (JMPT) at the ankle in a
adequate participation in the study protocol
14. For the nonDM subjects, a blood glucose value >6.72 mmol/1 more than 2 h after a meal
weight-bearing condition, we used a de-
15. Severe exercise-induced claudication vice that was specially designed for this
purpose. The apparatus consisted of two
individually movable foot plates that
could be tilted up (for dorsiflexion) or
Bloom et al. as mean + 2 SD of their dependent diabetes mellitus (NIDDM),
down (for plantarflexion) through the use
healthy subjects at each age). To control and subjects with onset of diabetes when
of an electromagnetic actuator (11). Test-
for possible effects of multiple other char- younger than age 40 years who were ing was performed for plantarflexion and
acteristics on postural stability, the sub- treated with insulin within 2 years of di- dorsiflexion at an angular velocity of
jects were matched across the groups by agnosis were considered to have insulin- 0.25% using the method of limits. For
gender, age (limited to 4 0 - 7 0 years), dependent diabetes mellitus (IDDM). data analysis, JMPTs of the right and left
weight in relationship to height, and du- ankles were averaged after adding plan-
ration of diabetes. Each triplet of subjects Neuropathy assessment tarflexion and dorsiflexion threshold val-
was matched as closely as possible for all It has been suggested that to fully assess ues together.
four characteristics. The exclusion criteria neuropathy, multiple measures of sen- Knee extensor and flexor and an-
applied during subject selection were de- sory and motor function should be used kle plantarflexor and dorsiflexor strength
signed to limit the possible influence of (8). This approach was particularly rele- testing was performed with a hand-held
factors other than diabetes and neuropa- vant in this study because one of the ques- dynamometer (12,13). These measure-
thy on postural stability (Table 1). Diabe- tions being asked was, What measure of ments were converted into torque values
tes type was assigned as follows: subjects neuropathy might best predict instability? by multiplying the force applied (in kg)
with onset of diabetes when older than Somatosensory function tests included and the distance between the point of ap-
age 40 years and those with onset when the evaluation of vibratory, touch-pres- plication and the center of rotation of the
younger than age 40 years who were not sure, and ankle joint movement percep- joint (in cm). In addition, the strength of
treated with insulin within 2 years of on- tion thresholds. The sensory latency re- the ankle evertors and invertors and flex-
set were considered to have non-insulin- sponse (SLR) of the sural nerve was also ors of the toes, including the halluces,
1412 DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994
Simoneau and Associates
were tested subjectively using manual
muscle testing (14).
B
Conventional electrophysiologi-
cal methods (15) were used to measure
MNCV and SLR.
Other subject characteristics
Since it is known that quality of the visual
input can have an impact on stability
(16), a rather extensive evaluation of vi-
sion was performed. These tests included
standard corrected binocular visual acu-
ity. Visual contrast sensitivity (VCS) at
five spatial frequencies (1.5, 3, 6, 12, and
18 cycles/degree of visual angle) was as-
sessed using three Vistech charts (Vistech
Consultants, Dayton, OH). The assess-
ment of VCS has been reported to provide
a better and more comprehensive mea-
surement of visual function than the as-
Medio-Lateral
sessment of visual acuity (17). The aver-
age luminance for the charts was ~40
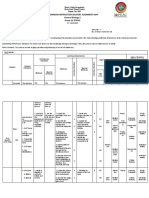
candelas/m (2). Because it has been sug- Figure 1—A: A subject standing on a force platform during a stability test. Postural stability is tested
gested that peripheral vision is most rele- here while the subject is standing barefoot and looking straight ahead with her eyes open for a period of
vant to the maintenance of upright pos- 30 s. The structure surrounding the subject provides a standard visual environment. B: A typical CoP
ture (18), visual peripheral field for each excursion signal output obtained over the 30 s of data collection. One division on both axes represents a
eye of each subject was tested using stan- 1-cm excursion of the CoP. The length of this path is used to quantify stability. This approach can be
dard equipment for every 45° of periph- thought of as a quantitative Romberg test.
eral vision. Clinical evaluation of the ves-
tibular system, the third sensory system
actively involved in the control of pos-
ture, was performed in the laboratory by barefoot and as still as possible for 30 s value, the less stable the individual
using four standard tests of vestibulo- (Kistler type 9261A on-line to an SMS (22,23).
ocular function (19) and the stepping test minicomputer) (Fig. 1A). This platform, The force platform was located at
as described by Fukuda (20). Ranges of which is level with the floor surface, is the center of a volume (6 ft by 16 ft by 10
movement (ROMs) of the ankle, subtalar equipped with force transducers that ft high) specifically built to control the
joint, knee, and first metatarsophalangeal measure the magnitude and the direction visual environment (Fig. 1A), which con-
joint were measured using standard go- of the forces applied to it. The center of sisted of vertical 3-inch gray/white alter-
niometric techniques (21). All subjects pressure (CoP) signal (Fig. IB), corre- nating stripes (optimal for the mainte-
completed an activity level questionnaire sponding to the point of application of the nance of stable posture [241). Lighting
that also contained questions regarding resultant force between the feet and force was constant, with a mean luminance of
their subjective ability to perform various platform, can therefore be measured and 20 candelas/m (2). A pure vertical visual
daily tasks such as walking, getting up reflects the stability of each subject during cue pattern was obtained using noncor-
from a chair, and going up and down stance (22,23). The CoP signal was sam- rective lenses that allowed full peripheral
stairs. Blood pressure was measured after pled at a rate of 100 Hz for a period of 30 vision with the exception of the white
3 min of sitting and then after 1 and 3 min s. Before analysis, the data were filtered ceiling and black floor. A standard foot
of standing. with a 4th-order, zero-phase shift, Butter- position with the heels 15 cm apart and
worth-type low-pass filter with a cutoff the feet toeing-out 10° was used.
frequency of 5 Hz (24). For the purpose For the diabetic subjects, blood
Stability measures of these experiments, only the total excur- glucose levels were measured before and
Measurements of stability were per- sion of the path of the CoP signal was every 30 min during the experiment.
formed with the subjects standing quietly used to quantify stability: the larger this Minimum and maximum acceptable lev-
DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994 1413
Posture and diabetic sensory neuropathy
Table 2—Subject characteristics used for matching tarsophalangeal joint ROM in extension,
and amount of body rotation and dis-
DM-NP DM-nonNP nonDM placement obtained with the Fukuda test.
Next, a series of multiple linear regression
Number of subjects 17 17 17 models were fit to this set of predictor
Gender (female/male) 4/13 4/13 4/13
variables. The log transform of total CoP
Age (years) 55.0 ± 7.9 54.2 ± 8.1 54.7 ± 8.5
Weight (kg) 91.6 ± 14.5 86.8 ± 11.7 87.3 ± 9.4 excursion was used as the dependent
Height (cm) 180.0 ± 7.5 177.2 ± 5.3 177.5 ± 7.9 variable to stabilize the error variance.
Duration of diabetes (years) 16.0 ± 9.9 13.4 ± 9.8 NA Predictor variables were sequentially ex-
Age at diabetes onset (years) 39.3 ± 16.3 40.8 ± 11.1 NA cluded from the model using a criterion
Data are means ± SD. No statistically significant differences were found among the three groups for any of for P values that decreased at every pass
the variables (P > 0.05). through the data from P = 0.30-0.20 to
0.10-0.05.
A second group of linear regres-
sion equations using age and quantitative
els of blood glucose were defined as 4.48 characteristics. Each block in the design sensory measurements as predictor vari-
and 22.40 mmol/1, respectively. Testing was made up of the three matched sub- ables of CoP excursion while standing
was started a maximum of 1 h after a meal jects, one from each group. An ANOVA with eyes open/head forward was calcu-
and lasted ~ 2 h. was also used to estimate differences in lated for the subset of 34 diabetic sub-
the CoP total excursion among the three jects, to provide potentially clinically use-
Experimental conditions groups and among the four experimental ful reference tables from which prediction
To assess the effects on stability of so- testing conditions. For all analyses, the of problems of stability in patients with
matosensory deficits caused by neuropa- ANOVA was followed by post hoc com- various degrees of neuropathy might be
thy in conjunction with deficits in vision parisons among model means when sig- possible, while taking into account the
and/or vestibular function, we tested all nificant differences were found. age of the patients. All sets of prediction
subjects under four conditions: eyes To determine the best-fitting lin- equations were inspected for model R2
open/head straight, eyes open/head back, ear regression model predicting CoP total and significance of coefficients.
eyes closed/head straight, and eyes excursion of all 51 subjects while stand- Finally, because age and sensory
closed/head back. In the head back posi- ing with eyes open/head forward, a statis- functions were the best predictors of in-
tion, which is believed to reduce the ef- tical search was conducted in several stability, possible interactions between
fectiveness of vestibular information for steps. First, the correlation matrix of the these two variables in predicting CoP ex-
the control of posture (25), neck/head ex- full set of predictor variables was in- cursion were investigated within the
tension was standardized to be 45°. For spected. The objective of this inspection ANOVA model and by using the interac-
each trial with eyes open, the subjects was to reduce the number of predictor tion terms in the regression models.
were instructed to fix their gaze on a sta- variables in the search set while including
tionary target in the center of their field of representative measures of vision, neu-
vision. Each subject was tested under all ropathy, joint movement perception, ves- RESULTS
four conditions using a randomized bal- tibular function, and subject demo-
anced design; three trials were averaged graphic characteristics. Sets of highly General subject characteristics
under each condition. correlated and functionally related vari- The physical characteristics of the
ables, such as the several measures of vi- DM-NP (diabetic neuropathic), DM-
Statistical analysis sual acuity, were represented by one vari- nonNP (diabetic not significantly neuro-
The SAS software package (26) on the able per set. The initial set of predictors pathic), and nonDM (neither diabetic nor
mainframe computer of The Pennsylvania included 19 variables: age, weight, neuropathic) groups on which matching
State University was used for data analy- height, gender, diabetes, retinopathy, of the subjects was based are shown in
sis. An analysis of variance (ANOVA) for a VPT and an indicator for off-scale read- Table 2. There were no statistically signif-
randomized block design was used to de- ings, SW rating and an indicator for off- icant differences (P > 0.05) among the
termine whether there were any statisti- scale readings, VCS at 1.5 cycles/degree, groups in terms of these attributes. There
cally significant differences among the JMPT, ankle plantarflexion torque, ROM were five subjects with IDDM in the
three groups for all measurements of neu- for ankle dorsiflexion measured with the DM-NP group and six in the DM-nonNP
ropathy as well as for measurements of knee extended, manual muscle testing for group. Of the subjects with NIDDM,
other sensory functions and physical the foot, subtalar joint ROM, first meta- eight in the DM-NP group and seven in
1414 DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994
Simoneau mid Associates
Table 3—Neuropathy characteristics ity, visual contrast sensitivity at higher
frequencies, and peripheral visual field
DM-NP DM-nonNP NonDM testing. The differences in retinopathy
were reflected by a statistically significant
VPT (Vs) 47.4 ± 3.3 13.9 ± 6.4 11.8 ± 4 . 7
reduction (P < 0.05) in visual contrast
Touch-pressure perception (SW rating) 4.6 ± 1.4 3.3 ± 0.5 2.9 ± 0.5
JMPT (degrees) 3.8 ± 3.6 1.5 ± 1.0 1.8 ± 1.4
sensitivity at the low spatial frequencies
SLR of sural nerve (ms) 6.3 ± 2.0 4.7 ± 1.1 NA (Table 4).
MNCV of peroneal nerve (m/s) 36.1 ±8.3 42.3 ± 5.1 NA No statistically significant differ-
Strength ences were found among the three groups
Ankle dorsiflexion (kg • cm) 305 ± 109 317 ± 122 397 ± 117 for passive knee ROM, ankle dorsiflexion
Ankle plantarflexion (kg • cm) 301 ± 98 312 ±97 370 ± 91 measured with the knee at 90°, ankle
Knee flexion (kg • cm) 551 ± 225 523 ± 207 576 ± 246
plantarflexion and metatarsophalangeal
Knee extension (kg • cm) 1324 ± 541 1282 ± 443 1544 ± 490
joint flexion. The two groups with diabe-
Data are means ± SD. In the DM-NP group there were 6 off-scale measures for VPT (50 V), 4 for SW rating
(6.65), and none for JMP; these values are included in the data in the table. In four subjects in the DM-NP tes were found to have significantly less (P
and one in the DM-nonNP groups, SLR could not be measured; they are not included in the data in this table. < 0.05) first metatarsophalangeal joint
Differences between the DM-NP and the other two groups for VTP, touch-pressure perception, and JMPT are extension (DM-NP = 76.6 ± 19.6°; DM-
statistically significant (P < 0.01). Difference between the DM-NP and the DM-nonNP group for SLR of sural nonNP = 83.7 ± 11.2°; nonDM = 92.0
nerve and MNCV of peroneal nerve is statistically significant (P < 0.05). Differences between the nonDM and
the two DM groups for ankle dorsiflexion and ankle plantarflexion are statistically significant (P < 0.05).
± 12.4°) and ankle dorsiflexion when
measured with the knee extended (DM-
NP = 5.6 ± 4.0°; DM-nonNP = 5.9 ±
3.3°; nonDM = 8.6 ± 4.8°) than the
the DM-nonNP group were being treated mal strength (4/5 in one case), and the nonDM group. A significant difference
with insulin at the time of the study. nonDM subjects all had normal strength. was also found between the two diabetic
groups for subtalar joint mobility (DM-
Measures of neuropathy Other subject characteristics NP = 25.1 ± 5.8°; DM-nonNP = 29.7 ±
The values for VPT, touch-pressure sen- Four subjects in the DM-NP group had 6.2°; nonDM = 28.1 ± 3.8°). These dif-
sation perception threshold (SW rating), background retinopathy and four others ferences in joint mobility were expected
ankle JMPT, MNCV of the peroneal had prior laser surgery, compared with because others have shown that limited
nerve, and SLR of the sural nerve are one subject with background retinopathy joint mobility is a feature of diabetes
shown in Table 3. There were statistically and one subject with prior laser surgery in (27,28).
significant differences between the the DM-nonNP group (Table 4). There All subjects had normal vestibulo-
DM-NP group and the two control were no statistically significant differences ocular function based on the clinical and
groups, such that the DM-NP group had a (P > 0.05) among groups for visual acu- the Fukuda tests (data not shown). Based
significant amount of neuropathy com-
pared with the control groups. There
were no statistically significant differences Table 4—Visual function characteristics
(P > 0.05) between the DM-nonNP and
nonDM groups in terms of neuropathy.
DM-NP DM-nonNP nonDM
Torque values for the ankle and
knee musculature are also listed in Table Retinopathy (background/laser) 4/4 1/1 NA
3. Strength at the knee was not signifi- Corrected visual acuity (X/20) 25.4 ± 11.6 21.8 ± 7.8 21.2 ± 5.3
cantly different among the groups (P > Visual field (degrees)
0.05). At the ankle, both DM groups were Left eye 63.3 ± 4.6 63.5 ± 3.9 63.8 ± 4.5
significantly weaker than the nonDM Right eye 65.4 ± 5.9 66.7 ± 5.6 66.5 ± 3.0
Visual contrast sensitivity
group (P < 0.05), but the two DM groups
1.5 cycles/degree 62.1 ± 24.9 78.2 ± 22.0 81.9 ± 23.5
were not statistically significantly differ-
3 cycles /degree 102.6 ± 45.8 136.8 ± 36.3 138.6 ± 40.0
ent from each other (P > 0.05). Of the 17 6 cycles /degree 91.3 ± 51.4 121.6 ±38.2 126.8 ± 59.4
DM-NP subjects, 4 had minimal weak- 12 cycles /degree 45.4 ± 29.5 58.4 ± 33.2 55.4 ± 30.7
ness (manual muscle rating of 4/5) of the 18 cycles/degree 13.9 ± 9.2 15.8 ± 10.3 17.5 ± 12.8
hallux or toe flexors of either foot. All but Data are means ± SD. Differences between the DM-NP and the other two groups for visual contrast sensi-
one of the DM-nonNP subjects had nor- tivity at 1.5, 3, and 6 cycles/degree are statistically significant (P < 0.05)
DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994 1415
Posture and diabetic sensory neuropathy
on the activity profile questionnaire, the Table 5—Blood pressure by group 117% less stable than the nonDM group.
groups were well matched in terms of ac- Note that as visual or vestibular inputs
tivities and abilities to perform routine 3 min 1 min 3 min were degraded or removed (e.g., in the
daily tasks. sitting standing standing eyes closed/head back condition) the
The average blood glucose levels neuropathic patients experienced much
DM-NP 143V81 141/81 142/82
during postural testing were 10.70 and greater percentage declines in stability
(20/7) (27/8) (29/8)
11.20 mmol/1 for the DM-NP and DM- DM-nonNP 144V86 139/86 141/86
than did the other groups. No significant
nonNP groups, respectively. These values (22/12) (22/10) (22/11) differences were found between the DM-
were 10.98 and 11.48 mmol/1 at the start nonNP and nonDM groups under any of
of the experiments and 10.19 and 10.98 nonDM 128/84 127/83 131/85 the test conditions (P > 0.05). Thus, sen-
mmol/1 after 90 min, respectively. These (15/7) (14/7) (18/7) sory neuropathy had a significant adverse
values were not significantly different be- Values are averages (SD). * Systolic blood pressure effect on stability while standing, but dia-
tween the two groups with diabetes at any in the DM group statistically significantly different betes per se had no effect.
time. from nonDM group; changes from sitting to stand-
ing are not statistically significantly different.
HbAlc values were not obtained
Association between instability and
as part of the formal protocol. Clinical re-
sensory and physical characteristics
sults were available for 13 subjects in the
The influence of sensory deficits as repre-
DM-NP group and for 12 subjects in the
were no significant differences between sented by the different sensory measures,
DM-nonNP group. The average values
the three groups in the change in systolic as well as of all the other physical charac-
(mean ± SD) were 8.1 ± 2.2 and 6.9 ±
and diastolic blood pressure from sitting teristics on the control of posture were
2.0%, respectively, and these were not
to standing after 1 and 3 min. The lowest investigated by grouping all 51 subjects
statistically different from each other (P =
recorded standing systolic blood pressure together and using regression analysis
0.19). These results do provide some in-
was coincidentally identical in the three techniques. Thereby, possible contribu-
dication of the level of control of diabetes tions of measures that were found to be
groups at 104 mmHg. No patients had
among our subjects at the time of these different among groups (ankle strength
CNS symptoms upon standing (symp-
experiments. As has been the case in most tomatic postural hypotension was an ex- and visual contrast sensitivity at low fre-
studies of diabetes complications, we did clusion criterion). Thus, no differences in quencies) and of variables that although
find a significant positive correlation be- postural hypotension existed among the not different among the groups could in-
tween the HbAlc values and neuropathy three groups. fluence control of posture (age, for exam-
measures (r = 0.31-0.43) ple) could be determined. In a multiple
Therefore, with the exception of
Patients receiving antihyperten- linear regression model in which all mea-
small deficits in some aspects of visual
sive therapy during the study were as fol- sures of sensation as well as age, weight,
function, minor differences in ankle and
lows: six in the DM-NP group (two were height, duration of diabetes, retinopathy
foot mobility, small deficits in ankle and
receiving diuretics only); three in the DM- status, measures of vision, strength at the
foot musculature strength, and a differ-
nonNP; and one in the nonDM group. ankle, and range of motion of several
ence in systolic blood pressure after 3 min
Blood pressure values for the three groups of sitting, the three groups of subjects joints of the foot were tested, only mea-
are shown in Table 5. There was a trend were considered to have very similar sures of sensory neuropathy and age con-
for the systolic blood pressure to be physical characteristics except for the tributed significantly to the fit of the
higher in the diabetes groups when com- quality of somatosensory perception in model (Eq. 1)
pared with the nonDM group, and this the distal end of the lower extremities.
difference was statistically significant (P Instability = exp (1.89 + 0.018
< 0.05, DM-NP versus nonDM and DM- age + 0.010 VPT
nonNP versus nonDM) in the 3-min sit- Instability and diabetic neuropathy + 0.396 SW off-scale) (1)
ting blood pressure. However, when the The postural stability results for each
two diabetes groups were compared, the group under the four testing conditions withR2 = 63.3% (Pearson r = 0.80). (For
largest difference between them in sys- are graphically represented in Fig. 2. The Eqs. 1 through 4, coefficients are signifi-
tolic blood pressure was only 2 mmHg, so DM-NP subjects were found to be signif- cant at P < 0.05, unless otherwise stated;
that these two groups can be considered icantly less stable (greater CoP excursion) instability corresponds to the CoP excur-
well matched in terms of systolic blood under all conditions than either the DM- sion in cm over 30 s in the eyes open/head
pressure. There were no significant differ- nonNP or nonDM subjects (P < 0.01). forward condition; the indicator variable
ences between the groups in diastolic These differences were large: the DM-NP SW off-scale has a value of 0 if the SW
blood pressure. Most importantly, there group was, on average, between 66 and rating is ^6.65 and a value of 1 if it is
1416 DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994
Simoneau and Associates
lating instability to age and SW rating in
the diabetic patients is
Instability = exp (1.46 + 0.023
age + 0.118 SW rating
+ 0.218 SW off-scale) (3)
where R2 = 54.7% (Pearson r = 0.74).
The SW off-scale variable was included in
the model to account for the upper limit
in the measurement despite its P value
being >0.05.
The linear regression equation re-
lating instability to age and ankle JMPT in
the diabetic patients is
Instability = exp (2.07 4- 0.0182
age + 0.0697 JMPT) (4)
Eyes Eyes Eyes Eyes where R2 = 51.9% (Pearson r = 0.72).
open/Head open/Head closed/Head closed/Head Equations for MNCV and SLR are
straight back straight back not shown because MNCV did not pre-
dict sway and SLR did so with an R? value
Testing Conditions
of only 4.4%.
Figure 2—Postural instability for the three groups of subjects under the jour testing conditions. A Tables 6, 7, and 8, developed
statistically significant difference (P < 0.01) was found between the DM-NP group and the two other from Eqs. 2, 3, and 4, provide a simple
groups jor all conditions. No statistically significant difference was found between the DM-nonNP and reference chart to determine the level of
nonDM groups (P > 0.05). Also note the similarity in instability between the DM-NP subjects standing
instability of individuals between 40 and
with eyes openAooking ahead and the nonDM group when standing with eyes closed/head back. The solid
65 years of age with various levels of sen-
line above each bar represents 1 SD.
sory losses measured in different ways.
The shaded areas correspond to the com-
bination of age and sensory loss in an in-
greater and therefore off scale; the indica- ered reasonable to provide an equation dividual with diabetes that would predict
tor variable VPT off-scale has a value of 0 for each sensory measurement technique more instability during stance than ex-
if the VPT is < 50 V and a value of 1 if it is because clinicians, in the absence of a rec- pected when compared with a healthy
greater and therefore off scale. The base of ognized standard measurement of sen- person between the ages of 40 and 60.
the natural logarithm [exp] is ~2.7182.) sory neuropathy, will often limit their as- The criterion value for normal stability
The type of diabetes, treatment sessment of sensory function to any one (determined to be 27.1 cm) is based on
method, and blood glucose level at the of these tests. the average CoP excursion (18.55 cm)
time of the experiment were not signifi- The linear regression equation re- plus 2 SD (8.54 cm) for the 13 nonDM
cantly related to postural stability. lating instability to age and VPT in the subjects between the ages of 40 and 60.
diabetic patients is
Prediction of instability from age CONCLUSIONS
and single measurements of Instability = exp (1.63 + 0.024
neuropathy age + 0.010 VPT Instability and diabetic neuropathy
The individual linear regression models + 0.079 VPT off-scale) (2) The major finding of this study is that di-
to predict instability for the eyes open/ abetic patients with distal symmetrical
head forward condition using age in con- where R2 = 53.6% (Pearson r = 0.73). sensory neuropathy not selected for any
junction with three different quantitative The VPT off-scale variable was kept in the complaint of instability are significantly
sensory tests of neuropathy as predictor model to adjust for the upper limit of VPT less stable during quiet standing than ei-
variables are presented below. These measurement despite its P value being > ther age-matched diabetic patients with-
equations were derived from the data of 0.05. out marked sensory neuropathy or age-
the 34 diabetic subjects. It was consid- The linear regression equation re- matched nondiabetic control subjects.
DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994 1417
Posture and diabetic sensory neuropathy
Table 6—Prediction of instability for diabetic individuals standing with eyes open and symptoms, and some had a history of foot
looking forward based on VPT and age ulceration. Even though they did not
complain of instability, we found them to
VPT (Vs) be quite unstable. In a survey of younger
patients with neuropathy, we found re-
Age (years) 10 20 30 40 50 cently that similar patients did report
40 14.49 16.00 17.67 19.52 21.55 problems when questioned directly (6).
45 16.30 18.00 19.88 21.96 24.25 Therefore, we suspect that this is a clinical
50 18.34 20.26 22.37 24.71 27.29 problem that is underreported, perhaps
55 20.64 22.80 25.18 27.80 30.71 because patients consider it to be a part of
60 23.23 25.65 28.33 31.29 34.55 normal aging. Instability may also not be
65 26.14 28.86 31.88 35.21 38.88 as disturbing as neuropathic pain or as
Instability = exp(1.63 4- 0.024 age + 0.010 VPT + 0.079 VPT-offscale). A value of 27.1 cm represents the visible as ulceration. We suggest, how-
upper 95% confidence interval for stability in healthy adults between 40 and 60 years of age (mean + 2 SD
ever, that clinicians must consider insta-
[18.55 + 2 X 4.27]). All values in excess of 27.1 cm are shaded, indicating that individuals with these
combinations of age and sensory losses are outside the normal 95% confidence interval. Therefore, this table bility in dealing with their patients with
can be used clinically to establish the level of instability of patients based solely on VPT testing and age, neuropathy.
eliminating the need to perform a test of stability with sophisticated equipment.
Consequences of instability
Diabetes per se has no effect on postural tually be much worse than what we have There is, in fact, additional circumstantial
stability. While the results have implica- observed in this study. In the clinical set- evidence in the literature to suggest that
tions for posture control theory, there are ting, neuropathic patients are likely to be instability may be clinically important
a number of potentially significant clini- encountered with a variety of conditions, among patients with diabetic neuropathy.
cal consequences of these findings. e.g., medications that act on the CNS, sig- Heath et al. (31) reported an increased
With eyes open/head straight the nificant weakness and/or other lower- incidence of leg/ankle fractures in dia-
patients with sensory loss were found to extremity dysfunction, uncorrected vi- betic women compared with age-
sway 66% more than did the healthy con- sual deficits, or obesity (29,30), that matched nondiabetic control subjects (al-
trol subjects. This is approximately the would cause additional instability. though neuropathy was not measured in
same degree of instability seen in healthy As noted, these neuropathic pa- their study). Selby (32), based on a review
people of a similar age when standing tients were not selected based on any of several publications, indicated that the
with their eyes closed/head back (Fig. 2). complaints of instability, but simply on incidence of diabetes among patients with
In the eyes closed/head back position the basis of having neuropathy. A few femoral neck fractures is greater than ex-
(such as might be encountered by a per- were experiencing painful dysesthetic pected based on the incidence of diabetes
son with cataracts in poor lighting look-
ing up to reach a high shelf), the patients
with sensory neuropathy were found to Table 7—Prediction of instability for diabetic individuals standing with eyes open and
be approximately twice as unstable as an looking forward, based on SW rating and age
average healthy person under the same
circumstances (Fig. 2). Semmes-Weinstein monofilament (SW rating)
Because of the rigorous exclusion
criteria used in this study, we were able to Age (years) 1.65 3.22 4.31 5.18 6.65
recruit neuropathic patients with no 40 13.34 16.05 18.26 20.23 24.06
likely reason for instability other than 45 14.99 18.05 20.52 22.74 27.05
neuropathy. Specifically, patients with all 50 16.86 20.29 23.07 25.57 30.41
the other known clinically important con- 55 18.95 22.80 25.93 28.74 34.18
tributors to instability (29,30) were ex- 60 21.30 25.64 29.15 32.31 38.42
cluded. In addition, the visual environ- 65 23.94 28.82 32.77 36.32 43.19
ment was optimized for the maintenance Instability = exp (1.46 + 0.023 AGE + 0.118 SW-rating + 0.218 SW-offscale). A value of 27.1 cm
of posture in our experiments. This im- represents the upper 95% confidence interval for stability in healthy adults between 40 and 60 years of age
(mean + 2 SD [18.55 + 2 X 4.27]). All values in excess of 27.1 cm are shaded, indicating that individuals
plies that in clinical situations, the degree
with these combinations of age and sensory losses are outside the normal 95% confidence interval. There-
of postural instability among patients fore, this table can be used clinically to establish the level of instability of patients based solely on SW
with diabetic sensory neuropathy may ac- monofilament testing and age, eliminating the need to perform a test of stability with sophisticated equipment.
1418 DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994
Simoneau and Associates
Table 8—Prediction of instability for diabetic individuals standing with eyes open and touch) would have greater instability than
looking forward, based on JMPT and age would a 73-year-old individual with nor-
mal age-adjusted sensory function.
Ankle JMPT (degrees) A major goal of the regression
analysis was to provide the clinician with
Age (years) 0.5 2.25 4 5.75 7.5 a method to predict instability in diabetic
40 16.99 19.20 21.69 24.50 27.68 patients without the use of force plat-
45 18.61 21.03 23.76 26.84 30.32 forms, which are rarely available in a clin-
50 20.39 23.03 26.02 29.39 33.21 ical setting. Equation 1 appears to provide
55 22.33 25.22 28.50 32.19 36.37 such a tool, because a large percentage of
60 24.46 27.63 31.21 35.26 39.84 the variance in the measurement of stabil-
65 26.79 30.26 34.19 38.62 43.63 ity (R2 = 63.3%) is accounted for by age
Instability = exp (2.07 + 0.0182 AGE + 0.0697 JMPT). A value of 27.1 cm represents the upper 95% and only two clinically measurable inde-
confidence interval for stability in healthy adults between the ages of 40 and 60 (mean 4- 2 SD [18.55 + 2
X 4.27]). All values in excess of 27.1 cm are shaded, indicating that individuals with these combinations of
pendent variables: VPT and SW off-scale.
age and sensory losses are outside the normal 95% confidence interval. Therefore, this table can be used The determination of these factors, using
clinically to establish the level of instability of patients based solely on ankle JMPT testing and age, elimi- a vibrometer and a single SW mono fila-
nating the need to perform a test of stability with sophisticated equipment. ment, can be easily performed in the phy-
sician's office and takes ~ 5 min using
simple and affordable equipment.
in the population, although there is some during standing would be even more af- Prediction of instability from age
debate over whether diabetic osteopenia fected and that gait and ability to recover and single measurements of
or diabetic neuropathy is responsible. We from slipping or tripping may also be al- neuropathy
have found radiographic evidence of foot tered. A secondary hypothesis for this study was
fractures to be much more prevalent in that a particular measure of neuropathy
neuropathic diabetic patients (33), and, Association between instability and may be better associated with instability
in the recent interview study already sensory and physical characteristics than all others. To test this hypothesis and
mentioned, neuropathic patients self- From the regression analyses performed to further simplify the prediction of insta-
reported 15 times more injuries during on the data, instability observed among bility, three equations were developed,
gait and felt significantly less safe in un- the DM-NP group was largely related to each making use of age and a single mea-
usual conditions than did non-neuro- sensory neuropathy and aging (the com- sure of neuropathy (Eqs. 2, 3, and 4).
pathic diabetic patients (6). Finally, Rich- bined R2 of Eq. 1 was 63.3%) and not Each of these three equations accounts for
ardson et al. (34) reported that peripheral significantly related to diabetes or any a similar amount of variance, with R? val-
neuropathy was significantly associated other physical or functional characteris- ues of 53.6, 54.7, and 51.9%, respec-
with falling and repetitive falls. tics assessed in this study (Eq. 1). Specif- tively. The similarity in the R2 values sup-
Falls have been linked to instabil- ically, the effects of mild ankle muscle ports the use of any one of these three
ity by others (35-39), and the awareness weakness and vision deficits in the group quantitative sensory tests for prediction
of the problem of falls among the elderly with neuropathy did not confound our of instability.
is presently heightened because the se- results. Among the measures of neuropa- Tables 6-8, developed from these
quelae of falls are becoming increasing thy, the best predictors of instability were equations, represent an attempt to pro-
causes of morbidity and mortality and an the three quantitative sensory tests. It is vide a quick, clinically useful guide for
increasing burden on the health care sys- noteworthy that stability was very poorly prediction of instability based on these
tem (29,40-42). Based on our findings, it related to the electrophysiological tests, a single measures of neuropathy. We recog-
is possible that diabetic neuropathic significant point in favor of the continued nize that these predictions are based on a
ataxia is a significant contributing factor use of quantitative sensory tests to assess small number of patients, and yet we feel
to injuries from falls in the elderly, and sensory neuropathy. The increase in pos- they are useful. For all three measures of
this clearly deserves further investigation. tural instability related to aging predicted neuropathy, the general rule appears to
In this study, we investigated the effects of in Eq. 1 has been previously documented be that at <50 years of age, very severe
distal symmetrical diabetic polyneuropa- (45). It is of note, however, that using Eq. neuropathy (such as that represented by
thy on posture in a very simple situa- 1, a 30-year-old diabetic patient with sig- off-scale measurements for both monofil-
tion—quiet stance. It is likely that recov- nificant neuropathy (off-scale measure- ament testing and VPT) is required to
ery from a disturbing force (43,44) ment of vibration and perception to cause significant instability. However,
DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994 1419
Posture and diabetic sensory neuropathy
above this age, even mild neuropathy will 10. Sosenko JM, Kato M, Soto R, Bild DE:
Acknowledgments—This work was per- Comparison of quantitative sensory-
render the patient's postural stability ab-
formed at the Center for Locomotion Studies threshold measures for their association
normal, and severe neuropathy results in
(CELOS) at Penn State University and was with foot ulceration in diabetic patients.
dramatic deficits in stability. Table 8 is of
partially supported by a grant from the Amer- Diabetes Care 13:1057-1061, 1990
special interest because ankle JMPT is the
ican Diabetes Association.
only test that allows the establishment of 11. Simoneau GG, Ulbrecht JS, Becker MB,
The results were first presented in abstract
an abnormally high level of sway in the Derr JA, Cavanagh PR: Design and pre-
form at the 1992 Annual Meeting and Scien-
younger population. This is no doubt due liminary testing of a device to quantify
tific Sessions of the American Diabetes Associ-
to the fact that it is the only test of neu- ankle joint proprioceptive function dur-
ation, San Antonio, Texas.
ropathy used here that does not have a ing weightbearing. In Posture and Gait:
finite upper limit. Control Mechanisms. Proc Xlth Interna-
References tional Symposium ojthe Society for Postural
Which specific somatosensory re-
1. Greene DA, Sima AAF, Albers JW, Pfeifer and Gait Research, Portland, OR, 24-27
ceptors are most responsible for the main-
MA: Diabetic neuropathy. In Elknberg May 1992. Woollacott M, Horak F, Eds.
tenance of normal posture is not com-
and Rijkin's Diabetes Mellitus: Theory and Eugene, University of Oregon Books,
pletely understood, and this study did not 1992,p.428-431
address that issue. The proprioceptors Practice. 4th ed. Rifkin H, Porte D Jr, Eds.
New York, Elsevier, 1990, p. 710-755 12. Bohannon RW, Andrews AW: Interrater
that may be involved include cutaneous
2. Thomas PK, Brown MJ: Diabetic polyneu- reliability of hand-held dynamometry.
pressure receptors, joint receptors, Golgi
ropathy. In Diabetic Neuropathy. Dyck PJ, PhysTher 67:931-933, 1986
tendon organs, and muscle spindles. Our
Thomas PK, Asbury AK, Winegrad AI, 13. Wadsworth CT, Krishnan R, Sear M, Har-
JMPT test was actually a test of all of the
Porte D, Eds. Philadelphia, Saunders, rold J, Nielsen DH: Intrarater reliability of
above receptors potentially functioning
1987,p.56-65 manual muscle testing and hand-held dy-
together, while VPT and monofilament 3. Ojala JM, Matikainen E, Groop L: Body namometric muscle system. Phys Ther 67:
testing addressed primarily skin recep- sway in diabetic neuropathy. ] Neurol 1343-1347, 1986
tors. The fact that these three measures of 232:188-193, 1985 14. Kendall FP, McCreary EK: Muscles: Test-
neuropathy were all equally associated 4. Mimori Y, Nakamura M, Kameyama M, ing and Function. 3rd ed. Baltimore, MD,
with instability does not help address the Sako Y, Yamao S, Miyoshi T: Statokinesi- Williams & Wilkins, 1983
issue: abnormalities in one measure of gram of patients with diabetic neuropa- 15. Nelson C: Electrical evaluation of nerve
neuropathy may simply be a surrogate for thy. In Proc International Symposium on Di- and muscle excitability. In Electrotherapy
abnormalities in the pathway actually re- abetic Neuropathy and Its Treatment. Goto in Rehabilitation. Gersh MR, Ed. Philadel-
sponsible. Thus, understanding of this as- Y, Horiuchi A, Kogure K, Eds. New York, phia, Davis, 1992, p. 101-148
pect of posture control awaits further re- Excerpta Medica, 1982, p. 168-172 16. Brandt T: Sensory function and posture.
search. 5. Lord SR, Caplan GA, Colagiuri R, Colagi- In Posture and Gait: Development, Adapta-
In conclusion, we demonstrate in uri S, Ward JA: Sensori-motor function in tion and Modulation. Proc 9th International
this study of diabetic patients with distal older persons with diabetes. Diabetic Med Symposium on Postural and Gait Research,
symmetrical predominantly sensory neu- 10:614-618, 1993 Marseille, France, 29 May-] ]une, 1988.
ropathy, but without a particular com- 6. Cavanagh PR, DerrJA, UlbrechtJS, Maser Amblard B, Berthoz A, Clarac F, Eds. New
RE, Orchard TJ: Problems with gait and York, Excerpta Medica, 1988, p. 127-136
plaint of instability, that such neuropathy
does lead to significant instability during posture in neuropathic patients with in- 17. National Research Council: Emergent
sulin-dependent diabetes mellitus. Dia- Techniques for Assessment of Visual Perfor-
quiet standing. Increased instability is
betic Med 9:469-474, 1992 mance. Washington, DC, National Acad-
thought to be associated with an in-
7. Bloom S, Till S, Sonksen P, Smith S: Use emy Press, 1985, p. 2-14
creased risk of falling. Our findings, taken
of a biothesiometer to measure individual 18. Post RB, Leibowitz HW: Two modes of
together with previous research that has
vibration thresholds and their variation in processing visual information: implica-
suggested that patients with neuropathy tions for assessing visual impairment. Am
519 non-diabetic subjects. Br Med] 288:
may indeed have more falls, should lead 1793-1795, 1984 ] Optom Physiol Optics 63:94-96, 1986
to increased clinical vigilance and patient 8. Asbury AK, Porte D: Report and recom- 19. Herdman SJ: Assessment and treatment of
education about the problem, particularly mendations of the San Antonio Confer- balance disorders in the vestibular-defi-
in the elderly or in patients with addi- ence on diabetic neuropathy. Diabetes cient patient. In Balance. Proc APTA Fo-
tional risk factors for instability. It should Care 11:592-597, 1988 rum, Nashville, TN, 13-15 June, 1989.
also lead to increased research efforts in 9. Gerr FE, Letz R: Reliability of a widely used Duncan PW, Ed. Alexandria, VA, APTA,
this field directed both at a greater under- test of peripheral cutaneous vibration sensi- 1989,p.87-94
standing of the problem and at strategies tivity and a comparison of two testing pro- 20. Fukuda T: The stepping test. Ada Otolar-
aimed at injury risk reduction. tocols. Br] Ind Med 45:635-639,1987 yngol 50:95-108, 1959
1420 DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994
Simoneau and Associates
21. Norkin CC, White DJ: Measurement of factors for falls among elderly persons liv- postural imbalance. Br MedJ 1:261-264,
Joint Motion: A Guide to Goniometry. Phil- ing in the community. N EnglJ Med 319: 1977
adelphia, Davis, 1985, p. 88-112 1701-1707, 1988 38. Robbins AS, Rubenstein LZ, Josephson
22. Lucy SD, Hayes KC: Postural sway pro- 30. Speechley M, Tinetti M: Assessment of KR, Schulman BL, Osteirweil D, Fine G:
files: normal subjects and subjects with risk and prevention of falls among elderly Predictors of falls among elderly people.
cerebellar ataxia. Physiother Can 37:140- persons: role of the physiotherapist. Phys- ArchlntemMed 149:1628-1633, 1989
148,1985 iother Can 42:75-79, 1990 39. Brocklehurst JC, Robertson D, James-
23. Kirby RL, Price NA, MacLeod DA: The 31. Heath H, Melton LJ, Chu CP: Diabetes Groom P: Clinical correlates of sway in
influence of foot position on standing bal- mellitus and risk of skeletal fracture. N old age-sensory modalities. Age Aging 11:
ance. J Biomech 20:423-427, 1987 EnglJ Med 303:567-570,1980 1-10, 1982
24. Simoneau GG, Cavanagh PR, UlbrechtJS, 32. Selby PL: Osteopenia and diabetes. Dia- 40. Sorock GS: Falls among the elderly: epi-
Leibowitz HW, Tyrrell RA: The effects of betic Med 5:423-428, 1988 demiology and prevention. AmJ Prev Med
visual factors and head orientation on 33. Cavanagh PR, Young MJ, Adams JE, Vick- 4:282-288, 1988
postural steadiness in women 55 to 70 years ers KL, Boulton AJM: Radiographic ab- 41. National Safety Council: Accident Facts.
of ageJGerontol 47:M151-M158,1992 normalities in the feet of patients with di- Chicago, National Safety Council, 1987
25. Brandt T, Krafczyk S, Malsbenden I: Pos- abetic neuropathy. Diabetes Care 17:201- 42. Baker SP, Harvey AH: Fall injuries in the
tural imbalance with head extension: im- 209,1994 elderly. Clin Geriatr Med 1:501-512,
provement by training as a model for 34. Richardson JK, Ching C, Hurvitz EA: The 1985
ataxia therapy. Ann NYAcad Sri 374:636- relationship between electromyographi- 43. Diener HC, Dichgans J, Bootz F, Bacher
649, 1981 cally documented peripheral neuropathy M: Early stabilization of human posture
2 6. SAS/STAT User's Guide: Statis tics. Version and falls. J Am Gerontol Soc 40:1008- after a sudden disturbance: influence of
6, 4th ed., vol. 2. Cary, NC, SAS, 1989 1012, 1992 rate and amplitude of displacement, lixp
27. Rosenbloom AL, Silverstein JH, Lezotte 35. Campbell AJ, Borrie MJ, Spears GF: Risk Brain Res 56:126-134, 1984
DC, Richardson K, McCallum M: Limited factors for falls in a community-based 44. Hansen PD, Woollacott MH, Debu B: Pos-
joint mobility in childhood diabetes mel- prospective study of people 70 years and tural responses to changing task condi-
litus indicates increased risk for microvas- olderj Gerontol 44:M112-M117, 1989 tions. Exp Brain Res 73:627-636, 1988
cular disease. N EnglJ Med 305:191-194, 36. Fernie GR, Gryfe CI, Holliday PJ, 45. Sheldon JH: The effect of age on the con-
1981 Llewellyn A: The relationship of postural trol of sway. Gerontol Clin 5:129-138,1963
28. Shinabarger NL: Limited joint mobility in sway in standing to the incidence of falls in 46. Andres R, Elahi D, Tobin DJ, Muller
adults with diabetes mellitus. Phys Ther geriatric subjects. Age Aging 11:11-16,1982 DC, Brant L: Impact of age on weight
67:215-218, 1987 37. Overstall PW, Exton-Smith AN, Imms FJ, goals. Ann Intern Med 103:1030-1033,
29. Tinetti ME, Speechley M, Ginter SF: Risk Johnson AL: Falls in the elderly related to 1985
DIABETES CARE, VOLUME 17, NUMBER 12, DECEMBER 1994 1421
You might also like
- Chapter 15Document10 pagesChapter 15Aryanto AntoNo ratings yet
- Handicap Vestibular en Polineuropatia DiabeticaDocument6 pagesHandicap Vestibular en Polineuropatia DiabeticaPedro César Saavedra MartínezNo ratings yet
- A Practical Two-Step Quantitative Clinical and Electrophysiological Assessment For The Diagnosis and Staging of Dianetic NeuropathyDocument9 pagesA Practical Two-Step Quantitative Clinical and Electrophysiological Assessment For The Diagnosis and Staging of Dianetic NeuropathyGhislaino ItabgaNo ratings yet
- Gait Abnormalities in Diabetic Neuropathy: Pathophysiology/ComplicationsDocument4 pagesGait Abnormalities in Diabetic Neuropathy: Pathophysiology/ComplicationschindyafisaNo ratings yet
- No Diabetic Lumbosacral RadiculopathyDocument11 pagesNo Diabetic Lumbosacral RadiculopathyHamza JubranNo ratings yet
- Evaluation and Prevention of Diabetic NeuropathyDocument6 pagesEvaluation and Prevention of Diabetic Neuropathyvivek_win95No ratings yet
- 1793Document5 pages1793onlyforu_3No ratings yet
- Approach To Peripheral Neuropathy For Primary Care ClinicianDocument7 pagesApproach To Peripheral Neuropathy For Primary Care ClinicianGevania ArantzaNo ratings yet
- Balducci2006 PDFDocument8 pagesBalducci2006 PDFDimasBanyakRejekiNo ratings yet
- Neuropatias PeriféricasDocument15 pagesNeuropatias PeriféricasGustavo Rodrigues de RezendeNo ratings yet
- 91 Diabetic Striatopathy EndotextDocument10 pages91 Diabetic Striatopathy EndotextReena SinghNo ratings yet
- Behaviour in Frontotemporal Dementia, Alzheimer's Disease and Vascular DementiaDocument13 pagesBehaviour in Frontotemporal Dementia, Alzheimer's Disease and Vascular DementiaFrancisco Ribeiro RachinasNo ratings yet
- Examination of Peripheral Nerve InjuriesDocument9 pagesExamination of Peripheral Nerve InjuriessarandashoshiNo ratings yet
- Millimeter Wave Treatment of Diabetic Sensorymotor Polyneuropathy1Document6 pagesMillimeter Wave Treatment of Diabetic Sensorymotor Polyneuropathy1olgaremonNo ratings yet
- 118a - Alteration in Neurologic FunctionDocument35 pages118a - Alteration in Neurologic FunctionJoanna TaylanNo ratings yet
- Alteration in Neurologic FunctionDocument35 pagesAlteration in Neurologic FunctionJoanna Taylan100% (1)
- Diabetic Neuropathy: Neuropatia DiabéticaDocument6 pagesDiabetic Neuropathy: Neuropatia DiabéticaElizabeth RuttinaNo ratings yet
- 4 Jpma Oa NCSDocument6 pages4 Jpma Oa NCSpunit lakraNo ratings yet
- Huizinga DAN PELTIER 2007Document10 pagesHuizinga DAN PELTIER 2007TriNo ratings yet
- Konduksi DSP NcsDocument7 pagesKonduksi DSP NcsMutiara Kristiani PutriNo ratings yet
- Neuropathy-in-diabetes_2015_MedicineDocument7 pagesNeuropathy-in-diabetes_2015_MedicineKaterinee Masielly Flores BlandónNo ratings yet
- Autoimmune Axonal Neuropathies. 2023Document15 pagesAutoimmune Axonal Neuropathies. 2023Arbey Aponte PuertoNo ratings yet
- Diabetic Neuropathies Update On Definitions Diagnostic Criteria Estimation of Severity and TreatmentsDocument34 pagesDiabetic Neuropathies Update On Definitions Diagnostic Criteria Estimation of Severity and TreatmentsHumberto RuelasNo ratings yet
- Chronic Axonal PolyneuropathyDocument19 pagesChronic Axonal PolyneuropathyzhoujNo ratings yet
- Diabetic NeuropathyDocument4 pagesDiabetic NeuropathyAsish GeiorgeNo ratings yet
- Narisetti, 2017Document9 pagesNarisetti, 2017Rizki Muhammad RanandaNo ratings yet
- Cerebral Palsy: Causes and Treatment Alternatives, Based On The Evidence Provided by Gait Analysis - Rupcich M, Bravo RDocument2 pagesCerebral Palsy: Causes and Treatment Alternatives, Based On The Evidence Provided by Gait Analysis - Rupcich M, Bravo RRicardo BravoNo ratings yet
- Research Article Electrophysiological Characterization of Neuropathy Complicating Type 1 Diabetes MellitusDocument7 pagesResearch Article Electrophysiological Characterization of Neuropathy Complicating Type 1 Diabetes MellitusMutiara Kristiani PutriNo ratings yet
- Research Article Electrophysiological Characterization of Neuropathy Complicating Type 1 Diabetes MellitusDocument7 pagesResearch Article Electrophysiological Characterization of Neuropathy Complicating Type 1 Diabetes MellitusMutiara Kristiani PutriNo ratings yet
- WNL 0000000000011792Document12 pagesWNL 0000000000011792jose JimenezNo ratings yet
- Stiff Person 2014Document10 pagesStiff Person 2014Pablo Sebastián SaezNo ratings yet
- Postreading Self-Assessment and CME Test-Preferred ResponsesDocument10 pagesPostreading Self-Assessment and CME Test-Preferred ResponsesFlea CidNo ratings yet
- Painless Diabetic Motor NeuropathyDocument12 pagesPainless Diabetic Motor NeuropathyHamza JubranNo ratings yet
- Vascular Dysfunction and Autonomic Neuropathy in Type 2 DiabetesDocument6 pagesVascular Dysfunction and Autonomic Neuropathy in Type 2 DiabetesaudiNo ratings yet
- Muscle Weakness and Other Late Complications of Diabetic PolyneuropathyDocument6 pagesMuscle Weakness and Other Late Complications of Diabetic Polyneuropathyrizki laluNo ratings yet
- A Case of Patient With Cerebellar Variant of Stiff Person SyndromeDocument4 pagesA Case of Patient With Cerebellar Variant of Stiff Person SyndromelaraviNo ratings yet
- Prevalencia de Neuropatía Periférica en Diabéticos Tipo 2 en El Primer Nivel de AtenciónDocument6 pagesPrevalencia de Neuropatía Periférica en Diabéticos Tipo 2 en El Primer Nivel de AtenciónNayely GuadalupeNo ratings yet
- Utah Neuropathy ScaleDocument10 pagesUtah Neuropathy ScaleRiko JumattullahNo ratings yet
- Neuro 1st WeekDocument70 pagesNeuro 1st WeekMel PajantoyNo ratings yet
- 2021 JinDocument9 pages2021 Jingzou2013No ratings yet
- Wenisch, 2013 Perfil de 31 PacientesDocument6 pagesWenisch, 2013 Perfil de 31 PacientesRicardo Jose De LeonNo ratings yet
- 28sici 291096 9136 28199802 2915 3A2 3C97 3A 3aaid Dia523 3e3.0.co 3B2 5 PDFDocument16 pages28sici 291096 9136 28199802 2915 3A2 3C97 3A 3aaid Dia523 3e3.0.co 3B2 5 PDFHesbon MomanyiNo ratings yet
- Surgical Therapies For Parkinson DiseaseDocument13 pagesSurgical Therapies For Parkinson DiseaseAnali Durán CorderoNo ratings yet
- The Rochester Diabetic Neuropathy StudyDocument10 pagesThe Rochester Diabetic Neuropathy StudyMonica ViverosNo ratings yet
- Benedict 2020Document12 pagesBenedict 2020HannaNo ratings yet
- Approach To Neurologic DisordersDocument6 pagesApproach To Neurologic DisordersSam VattaraiNo ratings yet
- Coma and Disorders of Consciousness: Scienti Fic Advances and Practical Considerations For CliniciansDocument8 pagesComa and Disorders of Consciousness: Scienti Fic Advances and Practical Considerations For ClinicianspipikafiyaNo ratings yet
- Algoritmo diferencial de la ataxia sensitiva en mielopatia por cobre secundaria a celiaquiaDocument7 pagesAlgoritmo diferencial de la ataxia sensitiva en mielopatia por cobre secundaria a celiaquiaFarid Santiago Abedrabbo LombeydaNo ratings yet
- 2017 - Déficits Vestibulares em Distúrbios NeurodegenerativosDocument9 pages2017 - Déficits Vestibulares em Distúrbios NeurodegenerativosDenise MaiaNo ratings yet
- Brismar Et Al. - 2007 - Predictors of Cognitive Impairment in Type 1 DiabetesDocument11 pagesBrismar Et Al. - 2007 - Predictors of Cognitive Impairment in Type 1 DiabetesJuan Pablo PérezNo ratings yet
- Obstructive Sleep Apnea Syndrome in Parkinson's Disease and Other ParkinsonismsDocument5 pagesObstructive Sleep Apnea Syndrome in Parkinson's Disease and Other ParkinsonismsTri Eka JuliantoNo ratings yet
- Diabetic NeuropathyDocument10 pagesDiabetic NeuropathyIrma Sari RasyidNo ratings yet
- Systematic Review: Balance Interventions For Diabetic Peripheral Neuropathy: A Systematic ReviewDocument8 pagesSystematic Review: Balance Interventions For Diabetic Peripheral Neuropathy: A Systematic ReviewJorge Luis Cifuentes EsparzaNo ratings yet
- ww24 Med12Document1 pageww24 Med12m0rinskiNo ratings yet
- Hepaticka Encefalopatija I ManganDocument12 pagesHepaticka Encefalopatija I ManganIvan MihailovicNo ratings yet
- An Easy Approach To Evaluating Peripheral NeuropathyDocument11 pagesAn Easy Approach To Evaluating Peripheral NeuropathyShahabuddin ShaikhNo ratings yet
- Review Article: Aristidis Veves, MD, Miroslav Backonja, MD, and Rayaz A. Malik, MB, PHDDocument15 pagesReview Article: Aristidis Veves, MD, Miroslav Backonja, MD, and Rayaz A. Malik, MB, PHDsrinivasNo ratings yet
- Neurology Multiple Choice Questions With Explanations: Volume IFrom EverandNeurology Multiple Choice Questions With Explanations: Volume IRating: 4 out of 5 stars4/5 (7)
- Clinical Autonomic and Mitochondrial Disorders: Diagnosis, Prevention, and Treatment for Mind-Body WellnessFrom EverandClinical Autonomic and Mitochondrial Disorders: Diagnosis, Prevention, and Treatment for Mind-Body WellnessNo ratings yet
- Decoding the Brain: A Comprehensive Introduction to Neurocognitive DisordersFrom EverandDecoding the Brain: A Comprehensive Introduction to Neurocognitive DisordersNo ratings yet
- Does Somatosensory Loss Induce Adaptation of The Gait Initiation Process?Document4 pagesDoes Somatosensory Loss Induce Adaptation of The Gait Initiation Process?Monica ViverosNo ratings yet
- Clinical stabilometry standardizationDocument3 pagesClinical stabilometry standardizationMonica ViverosNo ratings yet
- Vitamin B12, Demyelination, Remyelination and Repair in Multiple SclerosisDocument5 pagesVitamin B12, Demyelination, Remyelination and Repair in Multiple SclerosisMonica ViverosNo ratings yet
- Specifications For Building A Verticalforce Platform Designed Forclinical StabilometryDocument3 pagesSpecifications For Building A Verticalforce Platform Designed Forclinical StabilometryMonica ViverosNo ratings yet
- Salsa Bili 487Document12 pagesSalsa Bili 487Monica ViverosNo ratings yet
- Fitzpatrick 1994Document14 pagesFitzpatrick 1994Monica ViverosNo ratings yet
- Gait & Posture: Ana Flavia Gomes Paiva, Philippe Thoumie, Besma MissaouiDocument4 pagesGait & Posture: Ana Flavia Gomes Paiva, Philippe Thoumie, Besma MissaouiMonica ViverosNo ratings yet
- Study of Intra-Subject Random Variations of Stabilometric ParametersDocument3 pagesStudy of Intra-Subject Random Variations of Stabilometric ParametersMonica ViverosNo ratings yet
- Group II Spindle Fibres and Afferent Control of Stance. Clues From Diabetic NeuropathyDocument11 pagesGroup II Spindle Fibres and Afferent Control of Stance. Clues From Diabetic NeuropathyMonica ViverosNo ratings yet
- Name: Teacher: Date: Score:: Fractions WorksheetsDocument2 pagesName: Teacher: Date: Score:: Fractions WorksheetsMonica ViverosNo ratings yet
- Applicability of Smartphone For Dynamic Postural Stability EvaluationDocument7 pagesApplicability of Smartphone For Dynamic Postural Stability EvaluationMonica ViverosNo ratings yet
- Organization of Postural Responses Following A Rotational Support Surface Perturbation, After TKA: Sagittal Plane RotationsDocument9 pagesOrganization of Postural Responses Following A Rotational Support Surface Perturbation, After TKA: Sagittal Plane RotationsMonica ViverosNo ratings yet
- Write The Correct Comparison Symbol (, or ) in Each BoxDocument2 pagesWrite The Correct Comparison Symbol (, or ) in Each BoxMonica ViverosNo ratings yet
- Reliability Analysis of A Sensitive and Independent Stabilometry Parameter SetDocument14 pagesReliability Analysis of A Sensitive and Independent Stabilometry Parameter SetMonica ViverosNo ratings yet
- Fitzpatrick 1994Document14 pagesFitzpatrick 1994Monica ViverosNo ratings yet
- Applicability of Smartphone For Dynamic Postural Stability EvaluationDocument7 pagesApplicability of Smartphone For Dynamic Postural Stability EvaluationMonica ViverosNo ratings yet
- The Rochester Diabetic Neuropathy StudyDocument10 pagesThe Rochester Diabetic Neuropathy StudyMonica ViverosNo ratings yet
- Name: Teacher: Date: Score:: Fractions WorksheetsDocument2 pagesName: Teacher: Date: Score:: Fractions WorksheetsMohd Haniff Hafszal SemanNo ratings yet
- Fractions, Decimals, and PercentsDocument4 pagesFractions, Decimals, and PercentsMonica ViverosNo ratings yet
- Name: Teacher: Date: Score:: Fractions WorksheetsDocument1 pageName: Teacher: Date: Score:: Fractions WorksheetsZai SulaimanNo ratings yet
- Grade 4 Fractions To Decimals ADocument2 pagesGrade 4 Fractions To Decimals AMonica ViverosNo ratings yet
- Equivalent FractionsDocument2 pagesEquivalent FractionsMonica ViverosNo ratings yet
- Grade 5 Multiplying Decimals Mentally ADocument2 pagesGrade 5 Multiplying Decimals Mentally AMonica ViverosNo ratings yet
- Convert Between Fractions and Decimals NumbersDocument2 pagesConvert Between Fractions and Decimals NumbersMonica ViverosNo ratings yet
- Fraction To DecimalDocument2 pagesFraction To DecimalMonica ViverosNo ratings yet
- Name: Teacher: Date: Score:: Fractions WorksheetsDocument2 pagesName: Teacher: Date: Score:: Fractions WorksheetsMohd Haniff Hafszal SemanNo ratings yet
- Write The Correct Comparison Symbol (, or ) in Each BoxDocument2 pagesWrite The Correct Comparison Symbol (, or ) in Each BoxMonica ViverosNo ratings yet
- Decimal ComparisonDocument2 pagesDecimal ComparisonMonica ViverosNo ratings yet
- Percentage of Number Worksheet: Calculate The PercentagesDocument2 pagesPercentage of Number Worksheet: Calculate The PercentagesMonica ViverosNo ratings yet
- Woodworth (1899) The Accuracy of Voluntary MovementDocument120 pagesWoodworth (1899) The Accuracy of Voluntary MovementInacioRabaioli0% (2)
- Sodium Stibogluconate Pentamidine IsetionateDocument10 pagesSodium Stibogluconate Pentamidine IsetionateThunder BoltNo ratings yet
- Etiology of Psoriasis PDFDocument2 pagesEtiology of Psoriasis PDFAshleyNo ratings yet
- History-The Beginning of An IndustryDocument20 pagesHistory-The Beginning of An IndustryAnil BatraNo ratings yet
- The Living Embryo and Making of Whole Mounts 72Document7 pagesThe Living Embryo and Making of Whole Mounts 72joemark_narsico5796100% (1)
- Austin and Seebohar - Performance Nutrition. Nutrient TimingDocument200 pagesAustin and Seebohar - Performance Nutrition. Nutrient Timingmax7booxNo ratings yet
- Medicina Mitocondrial Vol 1Document485 pagesMedicina Mitocondrial Vol 1ArianPedrozaNo ratings yet
- Essentials of Medical Language 3rd Edition Allan Test BankDocument143 pagesEssentials of Medical Language 3rd Edition Allan Test BankDebbieCollinsokpzd100% (14)
- 1 - ATP-ADP - CycleDocument32 pages1 - ATP-ADP - CycleLearni J. EscoteNo ratings yet
- TBI QuizletDocument4 pagesTBI QuizletLoraine CometaNo ratings yet
- 12.1 Pediatri - Sirkulasi FetalDocument22 pages12.1 Pediatri - Sirkulasi Fetalwa ode nur salsabilahNo ratings yet
- CP 2Document24 pagesCP 2Bandameedi RamuNo ratings yet
- Aqa Bly3h W MS Jun 2012Document11 pagesAqa Bly3h W MS Jun 2012Rubab ZahraNo ratings yet
- 2022 Anatmoy and Physiology Cheat Sheet!Document3 pages2022 Anatmoy and Physiology Cheat Sheet!Estella BrockwellNo ratings yet
- Guide to Physical Assessment DocumentationDocument3 pagesGuide to Physical Assessment Documentationsandaman2225No ratings yet
- 10k Training Program (Interval, Cruise and Long Dist)Document6 pages10k Training Program (Interval, Cruise and Long Dist)kevinalmerNo ratings yet
- IbuprofenDocument31 pagesIbuprofenjalan jalanNo ratings yet
- Classroom Instruction Delivery Alignment Map General Biology 1 Grade 11 (STEM)Document6 pagesClassroom Instruction Delivery Alignment Map General Biology 1 Grade 11 (STEM)Julius Memeg PanayoNo ratings yet
- Gits Systems Anaphy DisordersDocument23 pagesGits Systems Anaphy DisordersIlawNo ratings yet
- Coenzymes and CofactorsDocument11 pagesCoenzymes and CofactorsGovindaraju ShruthiNo ratings yet
- CVS and RSDocument132 pagesCVS and RSclareawambuiNo ratings yet
- Pathfast PresepsinDocument6 pagesPathfast PresepsinWulan Ervinna SimanjuntakNo ratings yet
- Seretide Accuhaler Provides Effective Asthma ReliefDocument17 pagesSeretide Accuhaler Provides Effective Asthma ReliefSagacious Veracity0% (1)
- 1.05 Psychobiology: Niels Birbaumer University of Tuèbingen, Germany and Herta Flor Humboldt-University, Berlin, GermanyDocument58 pages1.05 Psychobiology: Niels Birbaumer University of Tuèbingen, Germany and Herta Flor Humboldt-University, Berlin, GermanySandra Carolina Valencia LaraNo ratings yet
- SaudiJHealthSci4142-1740933 045009Document9 pagesSaudiJHealthSci4142-1740933 045009Ramona BordeaNo ratings yet
- Anatomy 7062113972923606793Document4 pagesAnatomy 7062113972923606793Domato Ayaon NawalNo ratings yet
- Normal Lab Values Guide Under 40 CharactersDocument2 pagesNormal Lab Values Guide Under 40 CharactersPrashanth RajuNo ratings yet
- Micro Organisms ReviewerDocument72 pagesMicro Organisms ReviewerdavenNo ratings yet
- Stress (Biology) - Wikipedia, The Free Encyclopedia PDFDocument8 pagesStress (Biology) - Wikipedia, The Free Encyclopedia PDFBruno JeronimoNo ratings yet
- Changed Processing of Visual Sexual Stimuli Under GnRH-therapy - A Single Case Study in Pedophilia Using Eye Tracking and fMRIDocument13 pagesChanged Processing of Visual Sexual Stimuli Under GnRH-therapy - A Single Case Study in Pedophilia Using Eye Tracking and fMRIEmy Noviana SandyNo ratings yet