Professional Documents
Culture Documents
Zwab061 446
Zwab061 446
Uploaded by
JOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Zwab061 446
Zwab061 446
Uploaded by
JCopyright:
Available Formats
European Journal of Preventive Cardiology 2021, 28, Suppl 1 i433
Health Economics
How consistent are cost-effectiveness estimates of a cardiovascular polypill strategy
for the secondary prevention of cardiovascular disease across different cardiovascular
risk equations?
Rubio G.1; Aguiar C.2; Araujo F.3; Carcedo D.4; Abreu-Oliveira TP.5; Paz S.6; Castellano JM.7
1Ferrer Internacional, Barcelona, Spain
Downloaded from https://academic.oup.com/eurjpc/article/28/Supplement_1/zwab061.446/6273811 by guest on 21 December 2022
2Hospitalde Santa Cruz, Serviço de Cardiologia, Carnaxide, Portugal
3Hospital Beatriz Angelo, Serviço de Medicina Interna, Loures, Portugal
4Hygeia Consulting, Madrid, Spain
5Ferrer Portugal, Regulatory Affairs, Lisbon, Portugal
6Smartwriting4u, Benicassim, Spain
7National Centre for Cardiovascular Research (CNIC), Madrid, Spain
Funding Acknowledgements: Type of funding sources: Private company. Main funding source(s): Ferre Internacional
Background: Risk equations (RE) are crucial to individualise estimates and properly adjust preventive treatments in patients with previous
cardiovascular (CV) disease. RE are also routinely incorporated into health economic assessments but it is unknown if the cost-effective-
ness results vary according to the RE applied.
Purpose: To determine the cost-effectiveness of a CV polypill (ASA 100mg, atorvastatin 20/40mg and ramipril 2.5/5/10mg) strategy com-
pared to usual practice of combining monocomponents in the prevention of recurrent events in patients with previous coronary heart disease
(CHD) or stroke applying two different CV RE: SMART and FRAMINGHAM, respectively.
Methods: A Markov cost-effectiveness model (1-year cycles; 4 health states: stable disease, subsequent CHD, subsequent stroke; death;
payer perspective; direct medical costs; lifetime horizon; 4% discount rate) was developed for Portugal. Transition probability between health
states was based on the SMART RE and an adaptation for secondary CV prevention of the FRAMINGHAM RE, respectively. Cost-effective-
ness was calculated for a mixed cohort of secondary prevention patients (weighed post-CHD: 57.9%; post-stroke: 42.1%). Systematic litera-
ture reviews, Portuguese registries, mortality tables and official reports ware used to identify effectiveness, epidemiological, costs and utility
data. Outcomes were costs (€, 2020) per life year (LY) and Quality Adjusted Life Year (QALY) gained. One-way (OWA) and probabilistic
(PSA) sensitivity analyses tested the consistency of results. Assumptions were validated by experts.
Results: Applying the SMART RE, the incremental cost-effectiveness ratio (ICER) is 1,555€/LY gained and the incremental cost-utility ratio
(ICUR) is 1,785€/QALY gained for the polypill strategy. The incremental costs of adopting the polypill strategy are 171,378€. Recurrent CV
events (550.68 vs 642.13) and CV deaths (106.05 vs 122.81) are also less frequent with the polypill strategy compared with monocompo-
nents. Assuming a willingness-to-pay (WTP) threshold of 30.000 €/QALY gained, there is a 77.80% probability for the polypill strategy to be
cost-effective and 43.00% chances to be costs saving when used in a mixed cardiovascular and cerebrovascular disease population. Apply-
ing the FRAMINGHAM RE, the ICER is 998€/LY gained and the ICUR is 1,242€/QALY. The incremental costs amount 175,122€. Recurrent
CV events (452.66 vs 563.48) and CV deaths (104.77 vs 127.32) are less frequent with the polypill strategy. The PSA shows a 99.5% proba-
bility for the polypill strategy to be cost-effective and 46.8% chances to be costs saving.
Conclusion: Both risk equations result in comparable results on the cost-effectiveness of interventions for the secondary prevention of CV
disease. The polypill strategy remains cost-effective compared to the common practice of using individual monocomponents concomitantly,
reducing recurrent CV events at a moderately higher cost.
You might also like
- Raja Nand Kumar CaseDocument3 pagesRaja Nand Kumar CaseCAptain Sparrow0% (1)
- MUS-361U Syllabus (Summer 2017) Jon Newton Portland State University History of Rock MusicDocument4 pagesMUS-361U Syllabus (Summer 2017) Jon Newton Portland State University History of Rock MusicHardlyNo ratings yet
- 1 s2.0 S2254887421001107 MainDocument9 pages1 s2.0 S2254887421001107 MainSergio de LeonNo ratings yet
- LatinoDocument1 pageLatinojoseNo ratings yet
- RARE & Orphan Diseases - Epidemiology & Public HealthDocument1 pageRARE & Orphan Diseases - Epidemiology & Public HealthMichael John AguilarNo ratings yet
- Diagnostics: Automated Systems For Calculating Arteriovenous Ratio in Retinographies: A Scoping ReviewDocument14 pagesDiagnostics: Automated Systems For Calculating Arteriovenous Ratio in Retinographies: A Scoping ReviewokuwobiNo ratings yet
- BJOphthalmol 2020 316594.fullDocument6 pagesBJOphthalmol 2020 316594.fullunidadoftalmologia.dsmNo ratings yet
- Contrato Riesgos Compartidos PDFDocument4 pagesContrato Riesgos Compartidos PDFSergio TerrasaNo ratings yet
- Articulo Linfoma y FragilidadDocument10 pagesArticulo Linfoma y FragilidadLuis VasquezNo ratings yet
- Algoritmo Diabetes 2021Document8 pagesAlgoritmo Diabetes 2021cochipinkNo ratings yet
- PDFDocument11 pagesPDFNico IonaşcuNo ratings yet
- Bertoldi 2011Document7 pagesBertoldi 2011Luba D'AndreaNo ratings yet
- PIIS2666776222001892Document14 pagesPIIS2666776222001892Maribel GodoyNo ratings yet
- AbstractsDocument2 pagesAbstractsAnisaNo ratings yet
- International Journal of Cardiology: A B C K D A A e F G H I J ADocument9 pagesInternational Journal of Cardiology: A B C K D A A e F G H I J ASari ChaerunisahNo ratings yet
- Procalcitonin To Reduce Long-Term Infection-Associated AE in Sepsis 2020Document61 pagesProcalcitonin To Reduce Long-Term Infection-Associated AE in Sepsis 2020Christopher TorresNo ratings yet
- Healthcare 10 01438 v3Document14 pagesHealthcare 10 01438 v3Zeera MohamadNo ratings yet
- Prediction of Mortality and Heart Failure Hospitalisations in Patients UndergoinDocument23 pagesPrediction of Mortality and Heart Failure Hospitalisations in Patients UndergoinAlberto PolimeniNo ratings yet
- Alsoufi 2018Document2 pagesAlsoufi 2018nidaakkusNo ratings yet
- Makalah KesehatanDocument9 pagesMakalah KesehatanNini RahmiNo ratings yet
- Predicting 30-DayMortality For PatientsWith AcuteHeart Failure in The EmergencyDepartmentDocument14 pagesPredicting 30-DayMortality For PatientsWith AcuteHeart Failure in The EmergencyDepartmentRoberto López MataNo ratings yet
- A Machine Learning Approach To Management of Heart Failure PopulationsDocument10 pagesA Machine Learning Approach To Management of Heart Failure PopulationsS. M MEHEDI ZAMAN, 180021128No ratings yet
- 1 s2.0 S0007091217542075 MainDocument11 pages1 s2.0 S0007091217542075 Maineny_sumaini65No ratings yet
- Development and Implementation of A Computerized Medical Decision Support System To Reduce Polypharmacy and Drug-Drug Interactions in Hospitalized Patients.Document11 pagesDevelopment and Implementation of A Computerized Medical Decision Support System To Reduce Polypharmacy and Drug-Drug Interactions in Hospitalized Patients.Guido GiuntiNo ratings yet
- PrintArticle 72003Document7 pagesPrintArticle 72003Sadhi RashydNo ratings yet
- Cortejoso2016 Cost-Effectiveness of Screening For DPYD Polymorphisms To Prevent NeutropeniaDocument6 pagesCortejoso2016 Cost-Effectiveness of Screening For DPYD Polymorphisms To Prevent NeutropeniaSandra KneževićNo ratings yet
- Desmedt2019Document27 pagesDesmedt2019Nathaly Baldeon CamposNo ratings yet
- Novel Biomarkers of Cardiovascular Disease. Aplications in Clinical PracticeDocument29 pagesNovel Biomarkers of Cardiovascular Disease. Aplications in Clinical PracticeSofia AraujoNo ratings yet
- Building Your Peripheral Artery Disease Toolkit MDocument11 pagesBuilding Your Peripheral Artery Disease Toolkit MehaffejeeNo ratings yet
- Machine Learning Based Models To Support Decision Maki - 2021 - International JoDocument7 pagesMachine Learning Based Models To Support Decision Maki - 2021 - International JobasubuetNo ratings yet
- Performance of A Novel Risk Model For Deep Sternal Wound Infection After Coronary Artery Bypass GraftingDocument8 pagesPerformance of A Novel Risk Model For Deep Sternal Wound Infection After Coronary Artery Bypass GraftingMartha CeciliaNo ratings yet
- ResearchDocument4 pagesResearchCarl Dela CruzNo ratings yet
- A Systematic and Universal Artificial Intelligence Screening Method For Oropharyngeal Dysphagia - Improving Diagnosis Through Risk ManagementDocument14 pagesA Systematic and Universal Artificial Intelligence Screening Method For Oropharyngeal Dysphagia - Improving Diagnosis Through Risk ManagementAlvina RusliNo ratings yet
- The Re-Endo Registry: A Prospective, Interoperable, Standardised Clinical Registry of Infective Endocarditis PatientsDocument4 pagesThe Re-Endo Registry: A Prospective, Interoperable, Standardised Clinical Registry of Infective Endocarditis PatientsJéssicaLopesNo ratings yet
- 873 3010 2 PBDocument5 pages873 3010 2 PBandreaNo ratings yet
- PRO49 DEVELOPMENT OF AN ALGORITHM TO IDENTIFY CLINICAL PROFILE - 2020 - Value inDocument1 pagePRO49 DEVELOPMENT OF AN ALGORITHM TO IDENTIFY CLINICAL PROFILE - 2020 - Value inMichael John AguilarNo ratings yet
- Multidisciplinary Practice Guidelines For The Diagnosis, Genetic Counseling and Treatment of Pheochromocytomas and ParagangliomasDocument19 pagesMultidisciplinary Practice Guidelines For The Diagnosis, Genetic Counseling and Treatment of Pheochromocytomas and ParagangliomasLaura Marina IlincaNo ratings yet
- Guideline - Diagnosis - Genetic - Pheochromocytomas 2021Document25 pagesGuideline - Diagnosis - Genetic - Pheochromocytomas 2021mehidimed1889No ratings yet
- Early ViewDocument34 pagesEarly Viewyesid urregoNo ratings yet
- Covid19 Prediction Model With Hybrid Approach A ReviewDocument6 pagesCovid19 Prediction Model With Hybrid Approach A ReviewIJRASETPublicationsNo ratings yet
- International Journal of Cardiology: Contents Lists Available atDocument6 pagesInternational Journal of Cardiology: Contents Lists Available atdanfer_99No ratings yet
- Risk Factors For Physical Disability Upon Release FromDocument9 pagesRisk Factors For Physical Disability Upon Release FromRODOLFO JOSÉ DE OLIVEIRA MOREIRANo ratings yet
- Epidemiology of Chronic Rhinosinusitis: Prevalence and Risk FactorsDocument9 pagesEpidemiology of Chronic Rhinosinusitis: Prevalence and Risk FactorsChristian VieryNo ratings yet
- Mechanical Thrombectomy Is Cost-Effective Versus Medical Management Alone Around Europe in Patients With Low ASPECTSDocument5 pagesMechanical Thrombectomy Is Cost-Effective Versus Medical Management Alone Around Europe in Patients With Low ASPECTSRafika Ayu NadiaNo ratings yet
- PSY56 REAL WORLD DATA FOR HAEMOPHILIA A SYSTEMATIC APPROACH - 2019 - Value inDocument1 pagePSY56 REAL WORLD DATA FOR HAEMOPHILIA A SYSTEMATIC APPROACH - 2019 - Value inMichael John AguilarNo ratings yet
- Clinical Nutrition As Part Treatment Pathway Pancreatic Cancer Patients An Expert Consensus 2022Document15 pagesClinical Nutrition As Part Treatment Pathway Pancreatic Cancer Patients An Expert Consensus 2022Eva Lanza VallsNo ratings yet
- A Prospective Cohort Study in Patients With Type 2 Diabetes Mellitus For Validation of Biomarkers (PROVALID) - Study Design and Baseline CharacteristicsDocument10 pagesA Prospective Cohort Study in Patients With Type 2 Diabetes Mellitus For Validation of Biomarkers (PROVALID) - Study Design and Baseline CharacteristicsdianNo ratings yet
- Melatonina (2020) Rubio M, IV, CoVid 5 MGDocument3 pagesMelatonina (2020) Rubio M, IV, CoVid 5 MGAlumno del Doctorado FarmacologiaNo ratings yet
- UntitledDocument15 pagesUntitledMARTIN DANIEL COLMENAREZ RODRIGUEZNo ratings yet
- Version of Record:: ManuscriptDocument38 pagesVersion of Record:: Manuscriptutkarsh PromotiomNo ratings yet
- Covid 19 Health Prediction Using Supervised Learning With OptimizationDocument5 pagesCovid 19 Health Prediction Using Supervised Learning With OptimizationEditor IJTSRDNo ratings yet
- Seizure: European Journal of Epilepsy: SciencedirectDocument8 pagesSeizure: European Journal of Epilepsy: SciencedirectNicolás Robertino LombardiNo ratings yet
- TITLE: Real-World Effectiveness of Hydroxychloroquine, Azithromycin, and Ivermectin AmongDocument25 pagesTITLE: Real-World Effectiveness of Hydroxychloroquine, Azithromycin, and Ivermectin AmongMigjofNo ratings yet
- s12962 021 00295 3Document11 pagess12962 021 00295 3alfredopalacios77No ratings yet
- ArticleDocument7 pagesArticleDriss AbleNo ratings yet
- PRO10 THE COST ANALYSIS OF EMICIZUMAB VERSUS ACTIVATED PROTHROMB - 2020 - ValueDocument1 pagePRO10 THE COST ANALYSIS OF EMICIZUMAB VERSUS ACTIVATED PROTHROMB - 2020 - ValueMichael John AguilarNo ratings yet
- Practical Guide SPFADocument64 pagesPractical Guide SPFArafaelomar89No ratings yet
- Stroids Meta 2023Document14 pagesStroids Meta 2023Sachin KumarNo ratings yet
- Actualización-Endocarditis-bacteriana AmJMed 2020Document6 pagesActualización-Endocarditis-bacteriana AmJMed 2020msq.cv5919No ratings yet
- Umapathy 2017Document11 pagesUmapathy 2017Karinaayu SerinNo ratings yet
- Nurse Navigator Development of A ProgramDocument14 pagesNurse Navigator Development of A Programlindaflor13No ratings yet
- What Is BREXIT?Document3 pagesWhat Is BREXIT?yash nigamNo ratings yet
- Application of Machine Learning On Power System Dynamic Security AssessmentDocument6 pagesApplication of Machine Learning On Power System Dynamic Security AssessmenthuskeeNo ratings yet
- PDF Yamaha PSR Gx76 CompressDocument39 pagesPDF Yamaha PSR Gx76 Compressdaniel123estradaNo ratings yet
- 4677-Article Text-19529-1-10-20220528 PDFDocument16 pages4677-Article Text-19529-1-10-20220528 PDFMUHAMMAD FAZRIELNo ratings yet
- SCM Quiz No 2Document2 pagesSCM Quiz No 2MUHAMMAD -No ratings yet
- General Requirements For Welding of PipingDocument8 pagesGeneral Requirements For Welding of PipingMuhammedHafisNo ratings yet
- Appendix - Final Survey Questions - Yoga Australia - QualtricsDocument9 pagesAppendix - Final Survey Questions - Yoga Australia - QualtricsThảo NhiNo ratings yet
- SRDC Construction GuidelinesDocument27 pagesSRDC Construction GuidelinesRowell Ian Gana-anNo ratings yet
- TDL Language EnhancementsDocument111 pagesTDL Language EnhancementsJasim MuhammedNo ratings yet
- About Malaysia: Kuala LumpurDocument13 pagesAbout Malaysia: Kuala LumpurRajaghuru SomaguruNo ratings yet
- HazpakDocument20 pagesHazpakqhseconsultNo ratings yet
- Mobile Id Client Reference Guide V 2 7 PDFDocument49 pagesMobile Id Client Reference Guide V 2 7 PDFNyamdorj PurevbatNo ratings yet
- Kepimpinan Strategik Dan Hubungannya Dengan Kualiti Pengajaran GuruDocument13 pagesKepimpinan Strategik Dan Hubungannya Dengan Kualiti Pengajaran GuruGunalatcumy KarunanitheNo ratings yet
- 21612Document3 pages21612Prashant27992No ratings yet
- Learner AnalysisDocument6 pagesLearner Analysisapi-252604284No ratings yet
- Weekly Current Affairs May 2023 Week 01 - CompressedDocument31 pagesWeekly Current Affairs May 2023 Week 01 - Compressedsailesh singhNo ratings yet
- Science, Technology and SocietyDocument67 pagesScience, Technology and SocietyMae-ann P. MarcelinoNo ratings yet
- The Chhattisgarh Land Revenue Code 1959 Complete Act - Citation 134590 - Bare AcDocument175 pagesThe Chhattisgarh Land Revenue Code 1959 Complete Act - Citation 134590 - Bare AcKshitij NawarangNo ratings yet
- ENTP. Per TOPICDocument13 pagesENTP. Per TOPICeffendyNo ratings yet
- NetView For ZOS Programming PipesDocument394 pagesNetView For ZOS Programming Pipesrobhal01No ratings yet
- Qra HPCL Jalandhar Ird-Draft r1Document92 pagesQra HPCL Jalandhar Ird-Draft r1PABNo ratings yet
- Catalog Greiner - 980042 - GBO-PA - Catalogue - EN - 05.12.2023Document186 pagesCatalog Greiner - 980042 - GBO-PA - Catalogue - EN - 05.12.2023victor55stanNo ratings yet
- Well-Organized Modular Kitchen. ORIGINA POSTED On - by Itnseo75 - Mar, 2024 - MediumDocument6 pagesWell-Organized Modular Kitchen. ORIGINA POSTED On - by Itnseo75 - Mar, 2024 - Mediumitnseo75No ratings yet
- 4-Bus Mixing Console L Series Mixers: General Description FeaturesDocument3 pages4-Bus Mixing Console L Series Mixers: General Description FeaturesBanda SBANo ratings yet
- Video Journalism Project (Edited For Teacher)Document3 pagesVideo Journalism Project (Edited For Teacher)Bin RenNo ratings yet
- Tiang PJU Oktagonal H-06M SP (Bottom 160mm) Sock 2 Inch RevDocument1 pageTiang PJU Oktagonal H-06M SP (Bottom 160mm) Sock 2 Inch Revkusnadi st100% (1)
- Chapter 2 Strategy and Tactics of Distributive Bargaining 2020-09-28 09 - 52 - 18Document31 pagesChapter 2 Strategy and Tactics of Distributive Bargaining 2020-09-28 09 - 52 - 18fbm2000No ratings yet
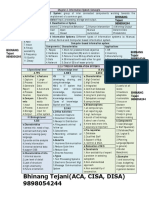
- Isca Chap 2 Revision ChartDocument2 pagesIsca Chap 2 Revision ChartKumar SwamyNo ratings yet