Professional Documents
Culture Documents
Bioethics, Pandemic and The Duty To Treat: Discussing The Allocation of Scarce Resources
Uploaded by
IJAERS JOURNALOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bioethics, Pandemic and The Duty To Treat: Discussing The Allocation of Scarce Resources
Uploaded by
IJAERS JOURNALCopyright:
Available Formats
International Journal of Advanced Engineering Research and
Science (IJAERS)
Peer-Reviewed Journal
ISSN: 2349-6495(P) | 2456-1908(O)
Vol-9, Issue-12; Dec, 2022
Journal Home Page Available: https://ijaers.com/
Article DOI: https://dx.doi.org/10.22161/ijaers.912.15
Bioethics, pandemic and the duty to treat: Discussing the
allocation of scarce resources
Letícia Almeida de Assunção1, Eliana Maria dos Santos2, Sarah Jacqueline Costa do
Lago3, Claudeth Freitas da Costa4, José Gustavo Monteiro Penha5, Leonardo Silva da
Costa6, Milton Nazareno de Quadros Miranda7, Francielma Pinheiro das Chagas8, Regina
Racquel dos Santos Jacinto9, Carla Monique Lavareda Costa10, Elane Magalhães
Oliveira11, Josiane Macedo de Oliveira Rupf12, Adams Brunno Silva13, Sonia Maria dos
Santos Farias14, Yasmin Pacheco Ribeiro15, Carla Caroline Motta Castilho16, Taynnara de
Oliveira do Espírito Santo Cunha17, Ivonete Vieira Pereira Peixoto18, Lucineia Ferreira
Ferreira19, Alessandra Evangelista20, Jhennifer Pereira Rodrigues21, Luceme Martins
Silva22, Marilene de Sousa Costa23, Edioneise Dantas de Souza24, Luana Priscila
Assunção25, Tainá Sayuri Onuma de Oliveira26, Erick Bruno Monteiro Costa27, Tarsila
Fagury Videira Secco Carvalho28, Liana de Oliveira Araújo29, Ana Caroline Guedes
Souza Martins30
1Nurse. Master Student in Oncology and Medical Sciences at Federal University of Pará (UFPA), Belém, Pará, Brazil.
2 Nurse. Master in Pharmaceutical Sciences from UFPA. Post-graduation in Teaching in Higher Education and in Occupational Nursing.
Professor at the University of São Paulo (UNIP). Belém, Pará, Brazil.
3 Nurse at Hospital Universitário Walter Cantídio- Universidade Federal do Ceará. Fortaleza, Ceará, Brazil.
4 Nurse. Specialist in Family Health., São Luís, Maranhão, Brazil.
5 Nurse. State University of Piauí. Specialist in Neonatal and Pediatric Nursing from the Pernambucana School of Health - FPS. Graduate in
Nursing in Urgency and Emergency by the Brazilian Institute of Postgraduate and Extension - IBPEX. Postgraduate in Preceptorship in
Health by UFRN. Specialization in Health Services Management by UniBF Faculdade. Master in Nursing by the Graduate Program in
Nursing/Health by FURG.
6 Nurse. Specialist in gynecology and obstetricsBelém, Pará, Brazil.
7 Nurse. Specialist_ occupational nursing, neonatology, obstetrics and auditing, Belém, Pará, Brazil.
8 Nurse. Epecialist in obstetrics and neonatology and occupational nursing. Belém, Pará, Brazil.
9 Nurse. Specialist in Obstetrics and Neonatology from INESUl Instituto Superior de Londrina and Maternal and Child Health from the
Federal University of Maranhão. Belém, Pará, Brazil.
10 Nurse. Specialist in Indigenous Health from the Venda Nova do Imigrante College – FAVENI; Specialist in Integrated Clinic at the Federal
University of Pará – UFPA; Specialist in Obstetric and Gynecological Nursing by Escola Superior da Amazônia – ESAMAZ; Master in
Nursing – UFPA. Belém, Pará, Brazil
11 Nurse. Assistant Nurse at the Infectious and Parasitic Diseases Unit at the João de Barros Barreto University Hospital/ CHU - UFPA. Post-
Graduation in Infectious Diseases Nursing by Faculdade Integrada de Brasília, Post-Graduation in Pediatric and Neonatal ICU Nursing by
IBRA College and Post-Graduation in Nursing in ICU - Intensive Care Unit by FAECHBelém, Pará, Brazil.
12 Nurse. Specialist in Epidemiology and Hospital Infection Control; Specialist in Quality and Patient Safety and Specialist and Nursing in
Intensive Care; Master's student in Tropical Diseases. Belém, Pará, Brazil.
13 Nurse. Nurse in surgical Clinic. Master in Nursing at UEPA. Belém, Pará, Brazil.
14 Social Worker. Master in Science and Environment at UFPA. Belém, Pará, Brazil.
15 Biomedical. Master in Parasite Biology in the Amazon from the State University of Pará (UEPA)Ananindeua, Pará, Brazil.
16 Nurse. University of the Amazon - Unama. Specialist in Nursing in Nephrology and Urology – Finama. Belém, Pará, Brazil.
www.ijaers.com Page | 131
Assunção et al. International Journal of Advanced Engineering Research and Science, 9(12)-2022
17 Nurse. Master's student at the Health Education Program in the Amazon – ESA-UEPA. Postgraduate in Management and Auditing in
Health Services and Occupational Nursing. Nurse at the Department of Health and Quality of Life at the Federal Institute of Pará (IFPA).
18 Nurse. Postdoctoral Student at Instituto Evandro Chagas. PhD in Nursing from the Federal University of Rio de Janeiro. Adjunct Professor
at UEPA. Professor of the Master's Degree in Nursing and the Master's Degree in Health Education in the Amazon at UEPA, Belém, Pará,
Brazil.
19 Nurse Student. State University of Pará -UEPA. Belém, Pará, Brazil
20 Nurse at the University of the Amazon (UNAMA). Belém, Pará, Brazil
21 Nurse. State University of Pará -UEPA- Belém, Pará, Brazil
22 Nurse. University of the Amazon-UNAMA. Belém, Pará, Brazil.
23 Nurse. Post graduate. Nurse at Santa Casa foundation, Ananindeua, Pará, Brazil.
24 Nurse.Specialit in obstetrical nursing and gynecology. Coordinator of the CME of Dom Vicente Zico rear hospital. Belém, Pará, Brazil.
25 Nurse.Universidade da Amazônia. Belém, Pará, Brazil.
26 2 Nurse. Master’s Student in Nursing at UFPA. Postgraduate in ICU and Occupational Nursing. Assistant Nurse at the Institute of Health
Care for Public Servants of the Municipality of Belém - IASB. Belém, Pará, Brazil.
27 Nurse at the University of the Amazon – UNAMA. Master's student in Knowledge Management for Socio-environmental Development at
the University of Amazonia – UNAMA Ananindeua, Pará, Brazil
28 Graduated in Physiotherapy from the University of the Amazon (UNAMA). Master in Gerontology - Catholic University of Brasilia.
Hospital Bettina Ferro, Belém, Pará, Brazil.
29 Nurse. Post graduate in urgency and emergency. Brasília, Distrito federal, Brazil.
30 Nurse. Doctoral Student in Clinical Research in Infectious Diseases at National Institute of Infectious Diseases-INI-FIOCRUZ-RJ.
Professor at UEPA, Belém, Pará, Brazil.
Received: 15 Nov 2022, Abstract — Objectives: To know the ethical parameters in relation
Receive in revised form: 05 Dec 2022, to the allocation of scarce resources in the midst of the pandemic.
Method: This is an integrative literature review that included
Accepted: 12 Dec 2022,
articles published in 2020, during the Covid-19 pandemic, in
Available online: 19 Dec 2022 journals indexed in Lilacs and Scielo databases, available for free,
©2022 The Author(s). Published by AI Publication. and studies discussed in international bioethics forums focused on
This is an open access article under the CC BY discussing ethical dilemmas during the pandemic. Results: There
license are strong justifications for the development and application of
(https://creativecommons.org/licenses/by/4.0/). triage protocols in case the pandemic exceeds the capacity to
provide intensive care to all patients. Conclusion: It is important
Keywords— Pandemic. Bioethics. Health
that hospitals take immediate steps to develop a decision-making
Economics.
process, anticipate what will be the priority criteria in this
pandemic moment and involve the ethics team in the institutions,
in order to take the burden off the decision of health professionals,
which are already overloaded.
I. INTRODUCTION communities, even if the ability to provide care is sufficient,
COVID-19 is an infectious disease that spread rapidly a priority must be on the goals of care in the setting of acute
and required resources beyond what healthcare systems can life-threatening illness, especially for patients. with life-
handle. This new infection with severe clinical limiting chronic diseases. [2,5]
manifestations, including death, has reached at least 124 According to the Brazilian Ministry of Health, as of
countries and territories [1,3,6]. While the ultimate course April 28, 2020, 71,886 confirmed cases and 5,017 deaths
and impact of Covid-19 is uncertain, this pandemic is from the disease were recorded in Brazil, according to
challenging healthcare systems around the world and raising information provided by the State Health Departments
important ethical questions, especially with regard to the across the country. In the last 24 hours, there were 5,385
potential need for rationing. [1] new cases and 474 new deaths. Of the 71,886 confirmed
The Covid-19 pandemic has led to a severe shortage of cases, 32,544 are considered recovered (45%) and 34,325
many essential goods and services, from hand sanitizers and are under follow-up. There are still 1,156 deaths under
N-95 masks to Intensive Care Unit (ICU) beds and investigation. [15]
ventilators1. The Covid-19 outbreak has posed critical The SUS does not have enough ICU beds for the demand
challenges for the public health, research and medical of the pandemic, most Brazilian states are unprepared to
www.ijaers.com Page | 132
Assunção et al. International Journal of Advanced Engineering Research and Science, 9(12)-2022
serve the serious cases of patients infected by the Articles published in 2020, during the Covid-19
coronavirus in the public network. In total, counting SUS pandemic, in journals indexed in Lilacs and Scielo
and private ICUs, Brazil has about 47,000 beds, divided in databases available in full, and studies discussed in
half in each system. Adding the two together, the average international bioethics forums aimed at discussing ethical
rises to 2.1 for every 10,000 people, below the need dilemmas during the pandemic were included in this study.
observed in the most affected countries. [14,15] Through this, it was possible to carry out a more detailed
This raises important ethical questions about how we analysis of bioethics experts, on how to proceed in relation
decide who has access to critical care when we cannot to the allocation of scarce resources in health services
provide it to everyone, during a pandemic, we need to around the world.
respect individual rights and freedoms, considering the Thus, in order to refine it, the following inclusion
needs of the general public. Decisions made in these criteria were defined: scientific articles that explained the
exceptional times must consider the principles of medical methodological trajectory adopted; written in Portuguese,
bioethics.[5,9] English or Spanish without restriction to the year of
From the perspective of this study, the objective is to publication and relate to terminally ill patients or end-of-life
know, through the literature, the ethical dilemmas in patients. Articles that included literature reviews, editorials
relation to the allocation of scarce resources in the midst of and proceedings abstracts were excluded.
the pandemic. For data analysis, only studies that were related to the
proposed theme were evaluated and selected, initially 16
studies were identified. After reading the abstracts,
II. METHOD
following the inclusion and exclusion criteria, 9 studies
In order to reach the objective of this study, an were effectively analyzed because they referred in the
integrative literature review was chosen, which makes it results to the bioethics theme in the allocation of health
possible to gather and synthesize results from multiple resources in the covid-19 pandemic.
published studies on a delimited topic in a systematic and
orderly manner, contributing to the deepening of the
investigated topic4. It was developed in six stages: III. RESULTS
establishment of the theme and research question; definition A summary of the selected articles is presented in the
of inclusion and exclusion criteria for sample selection; following table (table 1).
categorization of studies; evaluation of included studies;
interpretation of results and presentation of the review.
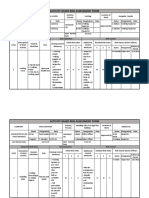
Table 1 – Distribution of studies according to numbering, research objective and research findings. Brasil, 2020.
N Author / year of Article title Periodical Objetives Main Results
Publication
1 PAULS; Ethical Canadian Discuss ethical In the midst of the
MIGNEAULT & considerations in Jounal issues about pandemic, advance
of Emergency decisions related directives of will
BAKEWELL, 2020 the allocation of to show how an
critical care Medicine important allies to the
distribution of
resources when ICU beds and management of the
respirators amid Canadian health
capacity is service.
the pandemic
overwhelmed.
of COVID-19.
www.ijaers.com Page | 133
Assunção et al. International Journal of Advanced Engineering Research and Science, 9(12)-2022
2 CURTIS; KROSS The Importance JAMA Discuss do not The importance that
& of Addressing Network Resuscitate clinicians have high
STAPLETON, 2020 orders on of the discussions quality,
Advance Care COVID-19 as much over the
Planning and pandemic planning advanced of
Decisions About service to individuals
Do-Not- of community,
especially those aged
Resuscitate more advanced and
Orders During with diseases
Novel chronicles.
Coronavirus 2019
(COVID-19)
3 TROUG, The Toughest The new Evaluate the the doctors of United
MITCHELL & Triage — England screening States can take
DALEY, 2020 Jounal of made in relation decisions that never
Allocating had before and for
Ventilators in a Medicine to the fans which many of them
Pandemic mechanics in will not be
United States. prepared.
4 EMANUEL Fair Allocation of The new analyze the Guidelines can
et al., 2020 Scarce Medical England capacity of ensure that doctors
Jounal of management of and nurses don't have
Resources in the the task of decide,
Medicine health system
Time of Covid-19 without help, which
in the states patients
united and the
possible choices Receive treatment
that doctors and that save lives and
nurses must do. which not.
5 GOSTIN; Responding to The Hastings To discuss In a moment of vast
FRIEDMAN & COVID-19: How Center Report ethically about inequalities, we are
the division and all so safe as the most
WETTER, 2020 to Navigate a asset allocation vulnerable between
Public Health and services for us United States and
Emergency population in in the world. If poor
midst of the members or
Legally and pandemic. disadvantaged of ours
Ethically. community no can
practice detachment
physical or access
health services, we
will all run a greater
risk.
6 BELINGER et al., Ethical The Hastings The study aims The institutions of
2020 Framework for Center to health are crucial to
Health Care help structure resist and if recover
discussions in from emergencies of
Institutions & progress of public health. O
Guidelines for worries practice support
Institutional ethical and ethics is crucial to the
Ethics Services predictable integrity and the
under levels of strength well-being
Responding to the contingency of
Coronavirus service and of work.
potentially
www.ijaers.com Page | 134
Assunção et al. International Journal of Advanced Engineering Research and Science, 9(12)-2022
Pandemic crisis patterns of
attendance.
7 POOLE et al., 2020 Responding to the The Analyze better Interventions under
COVID-19 Hastings Forms of tailored to the needs of
pandemic in Center interventions in crisis-affected
complex order to populations, provided
humanitarian maximize the with transparent
crises effectiveness of information, in the
actions during context of inclusive
the covid-19 governance practices,
pandemic. are urgently needed in
the global response to
the coronavirus
pandemic.
COVID-19.
8 HICK et al., 2020 Duty to Plan: National Discuss the Health facilities
Health Care, Academy of application of should develop
Crisis Standardsof Medicine the standards of proactive, layered
Care, and Novel care for strategies, using the
Coronavirus outpatient and best clinical
SARS-CoV-2 emergency information available
capacity, placed and building on their
by the existing outbreak
coronavirus or capacity plans to
other major optimize resource use
epidemic or in the event that the
pandemic event. current outbreak
spreads and creates
severe health
demands.
resources.
9 KRAMER; Ethics in the Time Journal of the The purpose of The COVID-19
BROWN& of Coronavirus: American this work was to pandemic is full of
KOPAR, 2020 Recommendatios Collegeof examine and uncertainties. Despite
in the COVID-19 Surgeons. provide being in the early
Pandemic. recommendatio stages of the
ns for several of challenges of this
the most crisis, lessons from
pressing ethical the HIV/AIDS
challenges, pandemic and the
making a
models of allocation
comparing the of scarce resources.
HIV pandemic
with the
coronavirus
(COVID-19)
pandemic.
Source: Research Protocol, 2022.
www.ijaers.com Page | 135
Assunção et al. International Journal of Advanced Engineering Research and Science, 9(12)-2022
The articles selected in the table above were carefully Bioethics and the duty to treat: the battle for mechanical
evaluated and grouped into categories: 1) A stressed health respirators.
system: response to the allocation of scarce resources amid Unlike decisions related to other forms of life-
the pandemic; 2) Bioethics and the duty to treat: the battle sustaining treatment, the decision to start or stop mechanical
for mechanical respirators; 3) Maximizing benefits is key in ventilation is often a life-or-death choice, because when
a pandemic; 4) Why palliative care in the covid-19 patients' breathing deteriorates to the point that they need a
pandemic? ventilator, they usually there is only a limited window
during which they can be saved. And when the machine is
IV. DISCUSSION taken from patients who are totally ventilator-dependent,
they usually die in a matter of minutes. [2,3]
A stressed health system: response to the allocation of
scarce resources amid the pandemic In normal times, outside of a health crisis, intensive
care beds and technology are properly allocated, first-come,
During a pandemic, when demand increases and
first-served. This is unsatisfactory when existing supply is
resources are overloaded, it is necessary to question which
outstripped by demand, as is happening in the Covid-19
decision-making structures will be adopted in relation to the
pandemic.[10]
division of health goods and services for the
population5,6,7,8 And how to carry out an ethical screening Decisions to withdraw ventilators during a pandemic
in this distribution when we are facing a pandemic? Or how in order to make the resource available to another patient
to deal with the fact that patients who could benefit from cannot be justified in any of the following ways: they are
intensive care or who would have received this care under not being taken at the request of the patient or their
different circumstances, and now would be denied this representative, nor can it be said that treatment is useless.
care.[1] Once patients have already been placed on mechanical
ventilation, decisions to withdraw it are especially difficult.
In the United States, many states have developed
[5,6,7]
rationing strategies during this pandemic. In Italy, Italian
guidelines have given a higher priority to access to intensive As circumstances change and the availability of
care, to younger patients with severe illness than to elderly ventilators and other medical resources increases or
patients. In Canada, much has been said about the decreases, the ethics committee may adjust its rationing
importance of advance directives and the participation of criteria to produce the best results. [2] Finally, when a
bioethics experts in the screening process.[3,6] hospital is placed to make decisions that may harm some
patients, the use of a committee removes the weight of those
There are strong ethical rationales for developing and
options from any individual, spreading the burden among
applying robust systems and screening protocols in the
all committee members.[3,11,12]
event that a pandemic overwhelms the ability to provide
critical care to all patients. Criteria such as age, life stage, In addition to removing responsibility for triage
mental capacity, physical capacity or disability should not decisions from bedside physicians, committee members
be used alone as an allocation criterion. The moral worth must also take on the task of communicating the decision to
and dignity of all people is equal, regardless of these the family, treating physicians may be motivated to try to
criteria. [5] comfort the family by telling them that mechanical
ventilation is not being provided because it would be useless
Choosing to set limits on access to treatment is not a
and assuring them that everything has been done. However,
discretionary decision, but a necessary response to the
it would be up to the committee members to communicate
overwhelming effects of a pandemic1. This process must be
these decisions, as it would ensure that the message was
evidence-based, and a transparent set of rules to decide who
clear and precise, helping to avoid confusion or
is critical and who is not., healthcare institutions need to
misunderstandings.[1,2,12]
take a clear stand by supporting the frontline who make
these decisions. [7] Maximizing benefits is key in a pandemic
Institutional ethics services, such as clinical ethics The value of maximizing benefits during the pandemic
consultant teams and ethics committees5, respond to this is most important, as this value reflects the importance of
practical reality by helping professionals, formulating responsible stewardship of resources, with the aim of saving
protocols to help apply guidelines, which ensure that health the greatest number of lives as well as improving the quality
professionals are not faced with the terrible task of of life after treatment for individuals.[12,13] Maximizing
improvise decisions about who to treat or make these benefits means that priority is given to those who are sick,
decisions in isolation. [9,10] but who have a greater chance of recovery and successful
www.ijaers.com Page | 136
Assunção et al. International Journal of Advanced Engineering Research and Science, 9(12)-2022
treatment, compared to those who would hardly recover, slow transmission of illness means that patients who die
even if treated, or even those who can recover without from COVID-19 are often left without their loved ones, who
treatment. [5,6,7] in turn will be unable to say goodbye or perform traditional
As maximizing benefits is critical in a pandemic, mourning rituals.[1,2]
removing a patient from a ventilator or an ICU bed to In this sense, PC and life-saving treatment should not
provide them to others who have a better chance of recovery be considered separate, saving lives is a crucial way to
is also justifiable, and patients should be made aware of this achieve this goal, but it is not the only one. Therefore, the
possibility in the future. admission.[10,11] However, many prevention and relief of suffering must be offered to anyone
guidelines agree that the decision to withdraw a scarce who suffers physically, psychologically, socially or
resource to save others in a pandemic context is not an act spiritually and not just to those with life-threatening
of killing and does not require patient consent.[11,13] conditions. [10]
On the other hand, ICU beds and ventilators are Practical steps can be taken such as ensuring access to
curative rather than preventive. Patients who need them face medications (such as opioids) and protective equipment,
life-threatening conditions, maximizing benefits requires considering greater use of telemedicine and video,
consideration of prognosis, how long the patient is likely to discussing advanced care plans, providing better training
live if treated, which may mean prioritizing younger and preparedness across the health workforce, and the role
patients and those with fewer coexisting conditions. of lay caregivers and the community in general.[2,3,5]
Fair allocation of resources that prioritizes the value of
maximizing benefits applies to all patients in need of V. FINAL CONSIDERATIONS
resources.1 For example, an allergic physician who
In the face of a pandemic, planning is necessary that
experiences anaphylactic shock and needs intubation and
includes strategies such as preparing, conserving, replacing,
life-saving ventilatory support should take priority over
adapting, reusing and reallocating resources. It is important
Covid-19 patients who are not first-line healthcare
for hospitals to take steps now to develop a decision-making
workers.[9]
process, anticipate what the priority criteria will be at this
Why palliative care in the covid-19 pandemic? time, and involve the ethics in institutions in order to take
Any triage system that does not integrate palliative the weight off the decision of health professionals, who are
care principles is unethical, patients who have no chance of already overloaded.
survival should not be abandoned, but should receive The urgency with which our practical decisions and
palliative care as a human right. Humanitarian responses organizational protocols are being reconfigured necessarily
that do not include Palliative Care (PC) are clinically infuses considerable uncertainty into patient care and leads
deficient and ethically indefensible. [7,8] to considerable variation in treatment. Being told to "do the
Palliative Care by definition is a multidisciplinary best you can", while understandable in the current situation,
approach that prevents and alleviates suffering through is a suboptimal alternative to carefully considered and
early identification, correct assessment and treatment of systematically enacted guidelines for action.
pain and other problems, whether physical, psychosocial or
spiritual, intended for any patient who has a health condition
REFERENCES
that threatens or limit your life.[5,7,8,9]
[1] Merril Pauls, et al. Ethical considerations in the allocation of
The current context frequently and urgently requires
critical care resources when capacity is overwhelmed.
health professionals who are in the field to make difficult Canadian journal of emergency medicine.2020;1-3.DOI:
decisions that involve ethical and technical issues in the face https://doi.org/10.1017/cem.2020.354.
of a disease with little scientific evidence. But COVID-19 [2] Curtis J. Randall, Kross Erin K., Stapleton Renee D. The
makes this more difficult.[10] Time is short when patients Importance of Addressing Advance Care Planning and
rapidly deteriorate and healthcare workers are Decisions About Do-Not-Resuscitate Orders During Novel
overwhelmed, isolation is mandatory and families are Coronavirus 2019 (COVID-19). JAMA Network [Internet].
advised not to touch or even be in the same room as their 2020;1-3. DOI 10.1001/jama.2020.4894.
[3] Truog Robert, Mitchell Christine, Daley George Q. The
loved ones. dear.[4,5]
Toughest Triage? Allocating Ventilators in a Pandemic. The
During the COVID-19 pandemic, access to essential New England Journal of Medicine. 2020;1-3.DOI
palliative care at the end of life, including bereavement 10.1056/NEJMp2005689. Available from:
support, will be limited in the face of high demands in all https://www.nejm.org/doi/full/10.1056/NEJMp2005689
countries10,12,13. Strict physical distancing regulations to
www.ijaers.com Page | 137
Assunção et al. International Journal of Advanced Engineering Research and Science, 9(12)-2022
[4] Mendes Karina Dal Sasso, Silveira Renata Cristina de 10.1056/NEJMsb2005114. Available from:
Campos Pereira, Galvão Cristina Maria. Revisão integrativa: https://www.nejm.org/doi/full/10.1056/NEJMsb2005114
método de pesquisa para a incorporação de evidências na [14] Cazian Fernando. SUS não tem leitos de UTI para enfrentar
saúde e na enfermagem. Texto & Contexto- Enfermagem. coronavírus. Folha de São Paulo. 2020;1-3. Available from:
2008;17. DOI https://doi.org/10.1590/S0104- https://www1.folha.uol.com.br/equilibrioesaude/2020/03/sus
07072008000400018. Available from: -nos-estados-nao-tem-leitos- de-uti-contra-o-
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S01 coronavirus.shtml.
04-07072008000400018 [15] Ministério da Saúde: Brasil registra 71.886 casos de
[5] Gostin Lawrence O., Friedman Eric A., Wetter Sarah A. coronavírus e 5.017 mortes da doença. 2020. Available from:
Responding to Covid-19: How to Navigate a Public Health https://www.saude.gov.br/noticias/agencia-saude/46806-
Emergency Legally and Ethically. The Hastings Center brasil-registra-71-886-casos-de- coronavirus-e-5-017-
Report [Internet]. 2020;50(2):1-5. DOI mortes-da-doenca Acess: 22 oct 2022.
https://doi.org/10.1002/hast.1090. Available from:
https://www.ncbi.nlm.nih.gov/pubmed/32219845
[6] Berlinger Nancy, et al. Ethical Framework for Health Care
Institutions & Guidelines for Institutional Ethics Services
Responding to the Coronavirus Pandemic. The Hastings
Center. 2020;1-12. Available from:
https://www.thehastingscenter.org/ethicalframeworkcovid19
/.
[7] Miller Franklin G. Why I Support Age-Related Rationing of
Ventilators for Covid-19 Patients. The Hastings Center.
2020;1-5. Available from:
https://www.thehastingscenter.org/why-i-support-age-
related-rationing-of- ventilators-for-covid-19-patients/.
[8] Poole Danielle N., et al. Responding to the COVID-19
pandemic in complex humanitarian crises. International
Journal for equity in health. 2020;41:1-2. DOI
https://doi.org/10.1186/s12939-020-01162-y. Available
from:
https://equityhealthj.biomedcentral.com/articles/10.1186/s12
939-020-01162-y
[9] Steinberg E, et al. Calculated decisions: COVID-19
calculators during extreme resouce-limited situations. Emerg
Med Pract [Internet]. 2020;4:1-5. Available from:
https://www.ncbi.nlm.nih.gov/pubmed/32259419
[10] Kramer Jessica B., Brown Douglas E. Ethics in the Time of
Coronavirus: Recommendations in the COVID-19 Pandemic.
Journal of the American College of Surgeons. 2020;230(6),
1114. DOI
https://doi.org/10.1016/j.jamcollsurg.2020.04.004. Available
from: https://www.journalacs.org/article/S1072-
7515(20)30309-4/fulltext
[11] Fauci Anthony S., Lane Clifford, Redfield Robert R. Covid-
19? Navigating the Uncharted. The New England Journal of
Medicine. 2020;382(13), 1268-1269 DOI:
10.1056/NEJMe2002387. Available from:
https://www.nejm.org/doi/full/10.1056/NEJMe2002387
[12] Hick John L., et al. Duty to Plan: Health Care, Crisis
Standards of Care, and Novel Coronavirus SARS-CoV-2.
National Academy of Medicine. 2020;1-13. DOI
https://doi.org/10.31478/202003b. Available from:
https://nam.edu/duty-to-plan-health-care-crisis-standards-of-
care-and-novel-coronavirus- sars-cov-2/.
[13] Emanuel Ezekiel J., et al. Fair Allocation of Scarce Medical
Resources in the 4. Time of Covid-19. The New England
Journal of Medicine. 2020;1-5. DOI
www.ijaers.com Page | 138
You might also like
- Extracardiac Signs of Fluid Overload in The Critically IllDocument13 pagesExtracardiac Signs of Fluid Overload in The Critically IllBlanca Herrera MoralesNo ratings yet
- FOR REVISION 3 Chapter 1 2 GROUP 6 N31Document55 pagesFOR REVISION 3 Chapter 1 2 GROUP 6 N31st michael machine shop100% (1)
- Lessons Learned From The Dog GenomeDocument11 pagesLessons Learned From The Dog GenomebellonicoNo ratings yet
- Covid 19 Vaccine ResearchDocument49 pagesCovid 19 Vaccine Researchcassandra67% (3)
- Veolia Water Tech AUS PharmaDocument7 pagesVeolia Water Tech AUS Pharmamanojdhamne5802No ratings yet
- Co2 Laser CatalogueDocument24 pagesCo2 Laser CatalogueBlin RodsNo ratings yet
- Nurses' Burnout and AssociatedDocument18 pagesNurses' Burnout and AssociatedTalipNo ratings yet
- Cleaning Validation Guidelines - Health CanadaDocument7 pagesCleaning Validation Guidelines - Health Canadahafeez50No ratings yet
- Nurses and Care Management in Clinical Emergencies: Bibliographic ReviewDocument7 pagesNurses and Care Management in Clinical Emergencies: Bibliographic ReviewIJAERS JOURNALNo ratings yet
- The Use of Technology in The Classification of Obstetric Risk: An Integrative Literature ReviewDocument7 pagesThe Use of Technology in The Classification of Obstetric Risk: An Integrative Literature ReviewIJAERS JOURNALNo ratings yet
- Morbimortality in American Cutaneous Leishmaniasis in The Xingú Region - Pará: Elaboration of A Digital Booklet For Health ProfessionalsDocument6 pagesMorbimortality in American Cutaneous Leishmaniasis in The Xingú Region - Pará: Elaboration of A Digital Booklet For Health ProfessionalsIJAERS JOURNALNo ratings yet
- 110 ArticleText 781 2 10 20200713Document6 pages110 ArticleText 781 2 10 20200713Temesgen OloloNo ratings yet
- Pathogens 11 01248Document13 pagesPathogens 11 01248Ngọc Minh Anh NguyễnNo ratings yet
- Unveiling The Meaning Attributed To Nursing Care at The Perspective of Person With CancerDocument8 pagesUnveiling The Meaning Attributed To Nursing Care at The Perspective of Person With CancerIJAERS JOURNALNo ratings yet
- Jurnal Inter7Document6 pagesJurnal Inter7Mhd FirdausNo ratings yet
- CHAPTER 1 3 SampleDocument41 pagesCHAPTER 1 3 SampleChua CandiceNo ratings yet
- Level of Anxiety Caused by Covid 19 Pandemic To The Nurses in Surigao CityDocument44 pagesLevel of Anxiety Caused by Covid 19 Pandemic To The Nurses in Surigao CityMichelle SunicoNo ratings yet
- COVID 19 Affect and Dimensions of Health of Mother During PregnancyDocument4 pagesCOVID 19 Affect and Dimensions of Health of Mother During PregnancyEditor IJTSRDNo ratings yet
- Issn: Issn:: Aquichan 1657-5997 2027-5374 Universidad de La SabanaDocument22 pagesIssn: Issn:: Aquichan 1657-5997 2027-5374 Universidad de La SabanaDavid Alejandro MorinNo ratings yet
- Assessment of The Nursing Educator's Role During (Covid-19) Outbreak in SudanDocument7 pagesAssessment of The Nursing Educator's Role During (Covid-19) Outbreak in SudanInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impacts of Social Distancing On The Incidence of Covid-19 in A Municipality in The Brazilian AmazonDocument6 pagesThe Impacts of Social Distancing On The Incidence of Covid-19 in A Municipality in The Brazilian AmazonIJAERS JOURNALNo ratings yet
- Nursing Care For Patients With Laryngeal Cancer: An Integrative ReviewDocument9 pagesNursing Care For Patients With Laryngeal Cancer: An Integrative ReviewIJAERS JOURNALNo ratings yet
- The Role of Chemistry in Sanitization and Personal Hygiene in Context of Covid-19Document8 pagesThe Role of Chemistry in Sanitization and Personal Hygiene in Context of Covid-19Central Asian StudiesNo ratings yet
- At The Epicenter of COVID-19-the Tragic Failure of The Global Supply Chain For Medical SuppliesDocument9 pagesAt The Epicenter of COVID-19-the Tragic Failure of The Global Supply Chain For Medical SuppliesIpuk WidayantiNo ratings yet
- ResearchDocument36 pagesResearchSajithShuraneNo ratings yet
- Global Clinical Journal Volume 3 December 2020 en DigitalDocument36 pagesGlobal Clinical Journal Volume 3 December 2020 en DigitalRicardo Mello CordeiroNo ratings yet
- 17 Preprints202003.0001.v2 TFR-COVID-19Document76 pages17 Preprints202003.0001.v2 TFR-COVID-19Zura JijelavaNo ratings yet
- Management of The Nursing Processes of Internal Students in The Confrontation of The COVID-19Document8 pagesManagement of The Nursing Processes of Internal Students in The Confrontation of The COVID-19Maria Liliana Calderon MaciasNo ratings yet
- Journal Homepage: - : IntroductionDocument2 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Idr 13 00064Document15 pagesIdr 13 00064Dmytro DemashNo ratings yet
- Coronavirus Disease 2019 - COVID-19: April 2020Document76 pagesCoronavirus Disease 2019 - COVID-19: April 2020ASHWIN BALAJI RNo ratings yet
- Health Science Reports - 2022 - SeyedAlinaghi - Impact of COVID 19 Pandemic On Routine Vaccination Coverage of Children andDocument12 pagesHealth Science Reports - 2022 - SeyedAlinaghi - Impact of COVID 19 Pandemic On Routine Vaccination Coverage of Children andArumm88No ratings yet
- Community-Acquired Pneumonia in Critically Ill Very Old Patients: A Growing ProblemDocument16 pagesCommunity-Acquired Pneumonia in Critically Ill Very Old Patients: A Growing ProblemTeju SutejoNo ratings yet
- Innovations For Tackling Tuberculosis in The Time of Covid - 19Document13 pagesInnovations For Tackling Tuberculosis in The Time of Covid - 19Minsarnawati TanacaNo ratings yet
- Developments in Medical Education in Response To The COVID-19 Pandemic: A Rapid BEME Systematic Review: BEME Guide No. 63Document15 pagesDevelopments in Medical Education in Response To The COVID-19 Pandemic: A Rapid BEME Systematic Review: BEME Guide No. 63Idiani DarmawatiNo ratings yet
- Objective Structured Clinical Examination (OSCE) : Perceptions of Nursing Students in Tuberculosis DiagnosisDocument8 pagesObjective Structured Clinical Examination (OSCE) : Perceptions of Nursing Students in Tuberculosis DiagnosisIJAERS JOURNAL100% (1)
- B12.Knowledge and Perceptions About COVID-19 Among The Medical and Allied Health Science Students in IndiaDocument6 pagesB12.Knowledge and Perceptions About COVID-19 Among The Medical and Allied Health Science Students in IndiaWislianaNo ratings yet
- Coronavirus Disease 2019 COVID19 Pandemic and PregnancyDocument47 pagesCoronavirus Disease 2019 COVID19 Pandemic and PregnancynoorulaminNo ratings yet
- Covid-19 Diagnosis AnnouncementDocument8 pagesCovid-19 Diagnosis AnnouncementIJAR JOURNALNo ratings yet
- Construction of A Classifying Technology For Geriatric Emergency Care For Caregivers of The ElderlyDocument8 pagesConstruction of A Classifying Technology For Geriatric Emergency Care For Caregivers of The ElderlyIJAERS JOURNALNo ratings yet
- Knowledge and Practice of Nursing Personnel On COVID-19 OnLINE DESCRIPTIVE STUDYDocument8 pagesKnowledge and Practice of Nursing Personnel On COVID-19 OnLINE DESCRIPTIVE STUDYInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Estres en CovidDocument7 pagesEstres en CovidcristhianNo ratings yet
- Level of Trust of The Population in The Unified HeDocument13 pagesLevel of Trust of The Population in The Unified HeMary Ashley Martinez ParcareyNo ratings yet
- Thesis On Biomedical Waste ManagementDocument8 pagesThesis On Biomedical Waste Managementtinawilliamsjackson100% (2)
- Clinical Presentation and Outcomes of Pregnant Women With Coronavirus Disease 2019: A Systematic Review and Meta-AnalysisDocument13 pagesClinical Presentation and Outcomes of Pregnant Women With Coronavirus Disease 2019: A Systematic Review and Meta-AnalysisanggipuspaNo ratings yet
- 17 Preprints202003.0001.v2 TFR-COVID-19Document76 pages17 Preprints202003.0001.v2 TFR-COVID-19Md Nadim MiahNo ratings yet
- Nursing Education in A Pandemic: Academic Challenges in Response To COVID-19Document4 pagesNursing Education in A Pandemic: Academic Challenges in Response To COVID-19Renzo GabrielNo ratings yet
- Knowledge of Nursing Students To Adhering Safety ProtocolsDocument74 pagesKnowledge of Nursing Students To Adhering Safety ProtocolsHareen “areshapesgay-” AdlaonNo ratings yet
- Do Medical Interns Feel Prepared To Work in The COVID-19 Pandemic?Document6 pagesDo Medical Interns Feel Prepared To Work in The COVID-19 Pandemic?Raul SousaNo ratings yet
- Nursing Leadership For 21st CenturyDocument2 pagesNursing Leadership For 21st CenturyCarlen Mae L. YacapinNo ratings yet
- Thesis ProposalDocument28 pagesThesis ProposalElla B. CollantesNo ratings yet
- Pakistan, Knowledge Attitude and PracticeDocument26 pagesPakistan, Knowledge Attitude and PracticeAprilianaNo ratings yet
- Research in Social and Administrative PharmacyDocument7 pagesResearch in Social and Administrative PharmacymuftiaNo ratings yet
- The Difficulties of Implementing Palliative CareDocument8 pagesThe Difficulties of Implementing Palliative CareIJAERS JOURNALNo ratings yet
- Ipc PreparednessDocument14 pagesIpc PreparednessSala MusikaNo ratings yet
- College Students' Knowledge, Attitude, and Practices On COVID-19 Prevention Post E-Health Education ProgramDocument8 pagesCollege Students' Knowledge, Attitude, and Practices On COVID-19 Prevention Post E-Health Education ProgramIJPHSNo ratings yet
- Indian LitratureDocument8 pagesIndian LitraturerenuNo ratings yet
- Knowledge, Attitude, and Practice Towards COVID 19 Among People Living With HIV/AIDS in Kigali, RwandaDocument6 pagesKnowledge, Attitude, and Practice Towards COVID 19 Among People Living With HIV/AIDS in Kigali, RwandamadawiNo ratings yet
- Wadh0022 Assignment 4 With FeedbackDocument39 pagesWadh0022 Assignment 4 With FeedbackViswaVittal's TheHiddenWorldNo ratings yet
- Vaccines 10 00059Document9 pagesVaccines 10 00059wahid.hasyimNo ratings yet
- Preventing Hospital Infections Real World Problems Realistic Solutions 2Nd Edition Jennifer Meddings Download PDF ChapterDocument52 pagesPreventing Hospital Infections Real World Problems Realistic Solutions 2Nd Edition Jennifer Meddings Download PDF Chaptermary.schoonmaker770100% (9)
- CELEST (2020) Issue 2 Telemedicine in Malaysia During Covid-19 PandemicDocument11 pagesCELEST (2020) Issue 2 Telemedicine in Malaysia During Covid-19 PandemicDrSuthan kaveriNo ratings yet
- Strategies For The Assessment of Tuberculosis Contacts: An Integrative Literature ReviewDocument9 pagesStrategies For The Assessment of Tuberculosis Contacts: An Integrative Literature ReviewIJAERS JOURNALNo ratings yet
- Group 6 Final Revision 2 1Document14 pagesGroup 6 Final Revision 2 1ANGELICA JOY GATDULANo ratings yet
- COVID-19: Tackling Global Pandemics through Scientific and Social ToolsFrom EverandCOVID-19: Tackling Global Pandemics through Scientific and Social ToolsS. ChatterjeeNo ratings yet
- Beef Cattle Farmers' Economic Behavior in The Minahasa Tenggara Regency, IndonesiaDocument7 pagesBeef Cattle Farmers' Economic Behavior in The Minahasa Tenggara Regency, IndonesiaIJAERS JOURNALNo ratings yet
- Impacts On The Mental Health of Professionals in A Prisonal System in Alagoas During The Covid-19 PandemicDocument7 pagesImpacts On The Mental Health of Professionals in A Prisonal System in Alagoas During The Covid-19 PandemicIJAERS JOURNALNo ratings yet
- Enhancing Cybersecurity: The Power of Artificial Intelligence in Threat Detection and PreventionDocument6 pagesEnhancing Cybersecurity: The Power of Artificial Intelligence in Threat Detection and PreventionIJAERS JOURNALNo ratings yet
- Playfulness in Early Childhood EducationDocument7 pagesPlayfulness in Early Childhood EducationIJAERS JOURNALNo ratings yet
- Climatic Rhythms and Prevalence of Malaria in The Municipality of Sinende in Northern BeninDocument8 pagesClimatic Rhythms and Prevalence of Malaria in The Municipality of Sinende in Northern BeninIJAERS JOURNALNo ratings yet
- Analysis Damage To The Inpres Elementary School Building Village Asilulu Central Maluku RegencyDocument5 pagesAnalysis Damage To The Inpres Elementary School Building Village Asilulu Central Maluku RegencyIJAERS JOURNALNo ratings yet
- Breastfeeding and Factors Associated With The Prevention of Childhood Obesity: An Integrative Literature ReviewDocument16 pagesBreastfeeding and Factors Associated With The Prevention of Childhood Obesity: An Integrative Literature ReviewIJAERS JOURNALNo ratings yet
- Constructed Wetlands: Technology For Removing Drug Concentration From WaterDocument12 pagesConstructed Wetlands: Technology For Removing Drug Concentration From WaterIJAERS JOURNALNo ratings yet
- Business Logistics and The Relationship With Organizational SuccessDocument4 pagesBusiness Logistics and The Relationship With Organizational SuccessIJAERS JOURNALNo ratings yet
- The Economic Impact of Coronavirus Disease (COVID-19) : A Study On Tourism Indicators in The Kingdom of Saudi ArabiaDocument4 pagesThe Economic Impact of Coronavirus Disease (COVID-19) : A Study On Tourism Indicators in The Kingdom of Saudi ArabiaIJAERS JOURNALNo ratings yet
- Study of The Extraction Process of The Pleurotus Citrinopileatus Mushroom and Evaluation of The Biological Activity of The ExtractDocument8 pagesStudy of The Extraction Process of The Pleurotus Citrinopileatus Mushroom and Evaluation of The Biological Activity of The ExtractIJAERS JOURNALNo ratings yet
- Associativism As Strategy of Reaching Territorial Rights, Programs, Projects and Public Policies of Rural Development: The Case of The São Francisco Do Mainã Community, Manaus, AMDocument9 pagesAssociativism As Strategy of Reaching Territorial Rights, Programs, Projects and Public Policies of Rural Development: The Case of The São Francisco Do Mainã Community, Manaus, AMIJAERS JOURNALNo ratings yet
- Analysis of The Thermal Behavior of Masonry Concrete Block With Internal Natural Element CoatingDocument11 pagesAnalysis of The Thermal Behavior of Masonry Concrete Block With Internal Natural Element CoatingIJAERS JOURNALNo ratings yet
- Morphometric Analysis of The Ekole River As A Consequence of Climate Change: A Case Study in Yenagoa, Bayelsa State, NigeriaDocument9 pagesMorphometric Analysis of The Ekole River As A Consequence of Climate Change: A Case Study in Yenagoa, Bayelsa State, NigeriaIJAERS JOURNALNo ratings yet
- Childhood/ Pediatric Cancer: Nursing Care in Oncopediatrics With A Central Focus On HumanizationDocument12 pagesChildhood/ Pediatric Cancer: Nursing Care in Oncopediatrics With A Central Focus On HumanizationIJAERS JOURNALNo ratings yet
- VCO Rancidity Analysis Refers To Fermentation Time That Produced by Gradual Heating MethodDocument6 pagesVCO Rancidity Analysis Refers To Fermentation Time That Produced by Gradual Heating MethodIJAERS JOURNAL100% (1)
- Water Quality Assessment Using GIS Based Multi-Criteria Evaluation (MCE) and Analytical Hierarchy Process (AHP) Methods in Yenagoa Bayelsa State, NigeriaDocument11 pagesWater Quality Assessment Using GIS Based Multi-Criteria Evaluation (MCE) and Analytical Hierarchy Process (AHP) Methods in Yenagoa Bayelsa State, NigeriaIJAERS JOURNALNo ratings yet
- Process Sequence Optimization and Structural Analysis of Nanoscale Heterostructure Using Compound Semiconductors AlAsSb/In0.59Ga0.41As/GaAs0.53Sb0.47Document5 pagesProcess Sequence Optimization and Structural Analysis of Nanoscale Heterostructure Using Compound Semiconductors AlAsSb/In0.59Ga0.41As/GaAs0.53Sb0.47IJAERS JOURNALNo ratings yet
- Komla Uwolowudu Amegna: International Journal of Advanced Engineering Research and Science (IJAERS)Document9 pagesKomla Uwolowudu Amegna: International Journal of Advanced Engineering Research and Science (IJAERS)IJAERS JOURNALNo ratings yet
- Association of Bacterial Vaginosis To Atypia in Squamous Cells of The CervixDocument15 pagesAssociation of Bacterial Vaginosis To Atypia in Squamous Cells of The CervixIJAERS JOURNALNo ratings yet
- Multiprofessional Care For A Patient With Gestational DiabetesDocument12 pagesMultiprofessional Care For A Patient With Gestational DiabetesIJAERS JOURNALNo ratings yet
- Design and Building of Servo Motor Portable Coconut Peller MachineDocument5 pagesDesign and Building of Servo Motor Portable Coconut Peller MachineIJAERS JOURNALNo ratings yet
- Does Blended Learning Approach Affect Madrasa Students English Writing Errors? A Comparative StudyDocument12 pagesDoes Blended Learning Approach Affect Madrasa Students English Writing Errors? A Comparative StudyIJAERS JOURNALNo ratings yet
- Humanization in Undergraduate Medical Education: The Brazilian Learner's PerspectiveDocument12 pagesHumanization in Undergraduate Medical Education: The Brazilian Learner's PerspectiveIJAERS JOURNALNo ratings yet
- Mining and Its Impacts On Environment and Health With Special Reference To Ballari District, Karnataka, IndiaDocument7 pagesMining and Its Impacts On Environment and Health With Special Reference To Ballari District, Karnataka, IndiaIJAERS JOURNALNo ratings yet
- Sociodemographic and Clinical Profile of Women With Uterine Cervical Cancer Attended in An Oncological Hospital in The State of Acre, BrazilDocument9 pagesSociodemographic and Clinical Profile of Women With Uterine Cervical Cancer Attended in An Oncological Hospital in The State of Acre, BrazilIJAERS JOURNALNo ratings yet
- Modeling of Geological and Geophysical Data, Onshore Field of Potiguar Basin, Northeastern BrazilDocument5 pagesModeling of Geological and Geophysical Data, Onshore Field of Potiguar Basin, Northeastern BrazilIJAERS JOURNALNo ratings yet
- Assessment of The Risk of Cardiovascular Diseases and Its Relationship With Heart Rate Variability in Physically Active and Sedentary IndividualsDocument13 pagesAssessment of The Risk of Cardiovascular Diseases and Its Relationship With Heart Rate Variability in Physically Active and Sedentary IndividualsIJAERS JOURNALNo ratings yet
- Detection and Control of Bacterial BiofilmsDocument15 pagesDetection and Control of Bacterial BiofilmsIJAERS JOURNALNo ratings yet
- The Psychologist's Role in The Process of Listening To Children Victims of Sexual Violence in Legal ProceedingsDocument8 pagesThe Psychologist's Role in The Process of Listening To Children Victims of Sexual Violence in Legal ProceedingsIJAERS JOURNALNo ratings yet
- Neonatology Short Case History Taking Format by SPKathankar 1Document5 pagesNeonatology Short Case History Taking Format by SPKathankar 1HkNo ratings yet
- 1 Identification: Acc. To OSHA HCSDocument10 pages1 Identification: Acc. To OSHA HCSbinaccaNo ratings yet
- L113 Independent Project Final ProposalDocument3 pagesL113 Independent Project Final ProposalAmelia RoebuckNo ratings yet
- Essay For TBIDocument7 pagesEssay For TBINatalie DrubachNo ratings yet
- ListeningDocument7 pagesListeningPallavi JNo ratings yet
- Resume Danika AcostaDocument2 pagesResume Danika Acostaapi-508877504No ratings yet
- Effectiveness and Neural Mechanisms of Home-BasedDocument5 pagesEffectiveness and Neural Mechanisms of Home-BasedMuhammad ImronNo ratings yet
- Backwardness of Women Leads To Backwardness of The Nation PDFDocument3 pagesBackwardness of Women Leads To Backwardness of The Nation PDFMuhammad ShahZadNo ratings yet
- How To Be Eco-FriendlyDocument18 pagesHow To Be Eco-Friendlyhannah courseyNo ratings yet
- Npi NCMHDocument6 pagesNpi NCMHJoshua DauzNo ratings yet
- Perbandingan Kasus Fatal Akibat Covid-19 Pada Beberapa Negara Asia TenggaraDocument6 pagesPerbandingan Kasus Fatal Akibat Covid-19 Pada Beberapa Negara Asia Tenggarasofia uyNo ratings yet
- Angelina Hull Student - Heritagehs - Argumentative Essay - Student Name - Class Period - Spring 19 - H English 1Document5 pagesAngelina Hull Student - Heritagehs - Argumentative Essay - Student Name - Class Period - Spring 19 - H English 1api-461590822No ratings yet
- Nota Bene For My ReviewersDocument4 pagesNota Bene For My ReviewersYomadoNo ratings yet
- Data Peserta Gartheting LT 3aumst Final 2022Document11 pagesData Peserta Gartheting LT 3aumst Final 2022Doni IrawanNo ratings yet
- Full Length Research Article: ISSN: 2230-9926Document5 pagesFull Length Research Article: ISSN: 2230-9926Nisarg SutharNo ratings yet
- Operating Room Personnel OrganizationDocument4 pagesOperating Room Personnel OrganizationantihistamiiineNo ratings yet
- Eye Drops and Dispensing Aids: A GuideDocument37 pagesEye Drops and Dispensing Aids: A GuideAamna ShahNo ratings yet
- Digi T Vigilance TestDocument6 pagesDigi T Vigilance TestJillianne FrancoNo ratings yet
- History of Perioperative Nursing 2023Document10 pagesHistory of Perioperative Nursing 2023Boniface MogakaNo ratings yet
- Daftar PustakaDocument5 pagesDaftar PustakaR Handi BramantoNo ratings yet
- The Ladli Scheme in India ReportDocument26 pagesThe Ladli Scheme in India ReportManoj BhalaniNo ratings yet
- Activity-Based Risk Assessment Form: Wearing InspectorDocument3 pagesActivity-Based Risk Assessment Form: Wearing InspectorSherly MagatNo ratings yet
- Faradic: Reference ManualDocument19 pagesFaradic: Reference ManualrobertNo ratings yet
- ABCDEFGHI Systematic Approach To Wound Assessment and ManagementDocument36 pagesABCDEFGHI Systematic Approach To Wound Assessment and ManagementsaerodinNo ratings yet
- EntDocument11 pagesEntkhuzaima9No ratings yet