Professional Documents
Culture Documents
Anti G
Uploaded by
DR.RAJESWARI SUBRAMANIYANOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anti G
Uploaded by
DR.RAJESWARI SUBRAMANIYANCopyright:
Available Formats
case study [transfusion medicine | immunology | hematology] Drug History
Enoxaparin, switched to heparin at 36 weeks of gestation;
Is It Really Anti-D and Anti-C nitrofurantoin; iron supplementation; and prenatal vitamins.
or Is It Anti-G?
Nada Rikabi, MD,1 Lisa Dunn-Albanasse, MD,2 Obstetrical History
Dave Krugh, MT(ASCP)SBB,1 Diane Snider, MT(ASCP),1 [T2]
Kristi Frenken, RN,2 Karen Rossi, RN,2
Richard O’Shaughnessy, MD,2 Melanie S. Kennedy, MD1 Principal Laboratory Findings
Departments of 1Pathology and 2Obstetrics & Gynecology, Maternal- [T3]
Fetal Medicine, The Ohio State University, Columbus, OH
Results of Additional Diagnostic Procedures
DOI: 10.1309/VQVYA7WY3T8HH7P4
An amniocentesis was performed at 20 weeks gestational age
(G.A.) and a delta OD450 analysis performed on amniotic
Patient fluid yielded a value of 0.07 (with a hemoglobin peak present
36-year-old Caucasian woman. in the scan), corresponding to a Liley chart zone of 1 (ie, un-
affected or mildly affected fetus for intrauterine hemolysis).
Downloaded from http://labmed.oxfordjournals.org/ by guest on February 29, 2016
History of Present Illness Fetal cells in the amniotic fluid were tested by polymerase
The patient is a G3P3, group B Rh(D) negative woman, chain reaction (PCR) for gene sequences corresponding to Rh
treated appropriately with Rh(D) immune globulin (RhIg) antigens. PCR testing was positive for D and negative for C
therapy after the birth of her first and second infants. The pa- antigen gene sequences. At 24 weeks and 2 days G.A. (ie, 24
tient presented in her third pregnancy at 12 2/7 weeks of ges- 2/7), anti-G and anti-C were identified in the patient’s serum.
tation with a positive antibody screen for anti-D and anti-C. At 27 6/7 weeks G.A., RhIg was administered to the mother.
The titer against R1R1 cells initially was 1:8, increasing to
1:16. The anti-D titer against R2R2 cells was 1:4. Questions:
1. Should all prenatal patients presenting with possible anti-D
Medical History and anti-C in their serum be routinely evaluated to deter-
Thrombotic thrombocytopenia purpura (TTP), treated on mine the presence of anti-G rather than anti-D?
multiple occasions with plasma exchange and with plasma 2. How can anti-G be identified in the laboratory?
infusions [T1], deep venous thrombosis, supraventricular 3. What is the risk for hemolytic disease of the newborn (HDN)
tachycardia, and adenomatous polyps of the small bowel. in prenatal patients with anti-G as opposed to anti-D?
4. In this case, if the infant required an intrauterine transfu-
Surgical History sion or an exchange transfusion, what type of blood would
Splenectomy. be appropriate for transfusion?
5. How could the identification of anti-G in a prenatal patient
Family History with an apparent anti-D and anti-C be of help in some
Divorced, remarried with 3 children. The patient is adopted and legal issues?
therefore had no knowledge of her family’s medical history. 6. Is the patient a Rh(D) immune globulin (RhIg) candidate?
Patient’s Transfusion History
Year/Month of Transfusion and Number of Units Transfused
T1
Blood Component 1992 1993 1994 1996 1997 1998 1999 2000 193
Transfused Aug Oct Dec Jan Feb Apr May Feb Feb Jul Aug Sep
Platelet pheresis units 1a 0 0 0 0 0 0 0 0 0 0 0
Pooled platelets 1a 0 0 0 0 0 0 0 0 0 0 0
FFP 12 43 0 0 14 2 2 0 0 0 0 0
CPP 0 0 6 6 124 62 12 91 2 8 80 0
RBCs 4a + 1b 0 0 0 2a 2a 0 1a 2a 0 2b 3a
aB Rh(D) negative. bO Rh(D) negative. FFP, fresh frozen plasma; CPP, cryoprecipitate-poor plasma; RBCs, red blood cells
© laboratorymedicine> march 2003> number 3> volume 34
Patient’s Obstetrical History
Mother Neonate(s)a
T2
Pregnancya Ab Screen G.A. @ Delivery RhIg Givenb Probable HDN Status Rh(D) Type
Paternal Genotype
G1P1 Neg 40 Yes n.a. Unaffected Positive
G2P3 Neg 40 Yes n.a. Unaffected Negative (twins)
G3P4 Pos 39 Yes R2r Unaffected Positive
aEach pregnancy resulted from 3 different men. bRh(D) immune globulin (RhIg) was administered at ~28 weeks gestational age (G.A.) or at delivery for all three pregnancies. Ab,
antibody; HDN, hemolytic disease of the newborn; n.a., not available
T3
Patient’s Antibody Screening Results at Various Gestational Ages
Downloaded from http://labmed.oxfordjournals.org/ by guest on February 29, 2016
Antibody Titer at Gestational Age, wk
Ab Testing Phasea 12 2/7 16 3/7 22 22 25 2/7 27 6/7 32 1/7
Saline Neg Neg Neg Neg Neg Neg Neg
AHG 1:8 1:16 1:4 1:16 1:16 1:8 1:8
aAntibody (Ab) screening cells were genotype R1R1 for all maternal serum Ab screening performed at all gestational ages (G.A.) except at 22 weeks G.A. when both R1R1 and R2R2 cells
were used. AHG, anti-human globulin
Possible Answers: ing by adsorption/elution techniques in the presence of poly-
1. Yes. Routine evaluation to differentiate anti-D, anti-C, and ethylene glycol (PEG) using R0r, r’r, and rGr red blood cells.
anti-G should be done on alloimmunized pregnant women Anti-C and anti-G with no anti-D were noted in 4 of 27
presenting serologically with an apparent anti-D and anti-C in (14.8%) samples.3 In our case, anti-G was suspected due to
their serum. Anti-G should be suspected when (1) the obstet- higher titers of anti-D and anti-C compared with anti-D, as
rical and transfusion history conflicts with formation of anti- well as the lack of history of sensitization [all red blood cells
D and -C, (2) the pregnant woman has received appropriate transfused were Rh(D) negative and RhIg was administered
Rh(D) immune globulin (RhIg) therapy, (3) the biological appropriately when indicated]. Since the differentiation of
father of the infant is Rh(D) negative, and/or (4) the antibody anti-D and anti-G is important in the management and prog-
titer of anti-C is significantly higher than the anti-D titer. In nosis of a pregnancy complicated by the presence of these
one case report, the laboratory investigation of a G7P3 antibodies, it should be performed whenever anti-D and anti-
woman, who received appropriate RhIg therapy after her last C are identified.
pregnancy, presented with a positive antibody screen with an
apparent anti-D and anti-C. Anti-G was suspected because 2. By testing serum with an appropriate panel of genotypic
more reactivity was observed with the C(+)D(-) red blood red blood cells. The G antigen is present on all red blood
cell sample than with the C(-)D(+) red blood cell sample. cells that are C+, since C(+)G(-) red blood cells have not
Further testing with D(+)G(-) red blood cells showed no reac- been found. The G antigen is present also on most (not all) D
tivity, leading to the exclusion of anti-D.1 In another study, a antigen positive red blood cells, since D(+)G(-) red blood
G4P1 pregnant woman who had received RhIg therapy when cells have been found. The G antigen (weak) is present on
indicated was shown to have anti-D and anti-C with a higher Rh(D) positive weak red blood cells. In summary, the G anti-
194 titer of anti-C than anti-D (1:32 versus 1:4, respectively). Ad- gen would be absent from C(-)D(-) red blood cells and would
sorption and elution studies proved that the patient had anti-C be present on most C+ or D+ red blood cells. Because of the
and anti–G, but no anti-D. Retrospective analysis of sera way these 3 antigens are expressed, anti-G appears serologi-
from 6 other pregnant women with anti-D and anti-C was cally identical to anti-D and anti-C. In a pregnant patient with
done; 2 had anti-D, anti-C, and anti-G, 3 had anti-D and anti- an apparent anti-D and anti-C, sequential adsorption and elu-
G with no anti-C, and 1 had anti-C and anti-G with no anti- tion studies using r’r (Cde) and R0r (cDe) red blood cells can
D.2 In another report, 27 pregnant women who were initially be done to confirm the presence or absence of anti-G [T4]. It
identified as having anti-D and anti-C underwent further test- is important to mention that rarely, individuals may have red
laboratorymedicine> march 2003> number 3> volume 34 ©
Antibodies Remaining After Sequential Reaction of Serum Containing Anti-D, Anti-C, and/or Anti–G
Antibodies With R0r and r’r Genotype-Specific Red Blood Cells
T4
Antibodies Remaining After Reaction With R0r and r’r Cells
R0r (cDe, G positive) r’r (Cde, G positive)
Serum Containing the Antibodies 1st Adsorption ➙ 1st Elution ➙ 2nd Adsorption ➙ 2nd Elution
D, C, and G D and G D and G G G
D and C D D None None
blood cells that are D negative, C negative, but G positive. was thought to have anti-D and anti-C. Prenatal workup re-
These cells may have a C-like component known as (CG) that vealed that the patient had an anti-G rather than an anti-D.
can react with anti-C. Because of the possibility of this reac- At 32.5 weeks of gestation, the mother delivered an affected
Downloaded from http://labmed.oxfordjournals.org/ by guest on February 29, 2016
tion, these rare cells should not be used to detect the presence fetus with moderately severe HDN.6 We conclude that even
or absence of anti-G.2 though hemolytic HDN due to anti-G is very uncommon, it
should still be considered when more reactivity is observed
3. The risk of HDN is small but finite. The number of case with C(+)D(-) than with the C(-)D(+) antibody screening
reports of anti-C and/or anti-G without a concomitant anti- red blood cells.
D during pregnancy is limited, precluding a complete evalu-
ation of the risk for HDN in these patients. However, it is 4. Cytomegalovirus (CMV) seronegative, irradiated group O
known that anti-C alloimmunization occurs less frequently Rh(D) negative (rr) red blood cells would be indicated. The
than anti-D and even though anti-C may cause serious transfused red blood cells must be D and C antigen negative
HDN, it is usually less severe. Anti-G rarely presents with a and consequently G antigen negative. The differentiation of
high titer that may affect the fetus and require medical in- anti-D, anti-C, and anti-G for routine transfusion is not nec-
tervention (ie, amniocentesis or intrauterine transfusion). In essary, since most Rh(D) negative, C antigen negative red
one study, adsorption and elution testing was performed on blood cells would be G antigen negative. If the mother is the
serum from 27 pregnant women with apparent anti-D and donor for intrauterine transfusion, frozen deglycerolized red
anti–C and 4 of the 27 samples (14.8%) showed anti-G and blood cells allows multiple aliquots to be frozen and then
anti-C without anti-D. None of the newborn children from thawed as needed.
these pregnancies were affected with HDN or needed post-
partum management.3 In another case report, a 35-year-old 5. When the medical and transfusion history are inconsistent
Rh(D) negative primigravida who had received 4 units of with the finding of an apparent anti-D and anti-C in an Rh(D)
Rh(D) negative allogeneic red blood cells had a history of negative pregnant woman and the biological father is Rh(D)
positive anti-D and anti-C antibody screens as part of her negative. In such cases, questions about paternity may arise.
prenatal workup. Additional studies by a different labora- If anti-D is not present (only anti-C and/or anti-G) RhIg
tory showed the presence of anti-G and possible anti-C with should be given at appropriate times. Therefore, correct anti-
no anti-D. At 22 weeks gestation, titers were 1:64 against r’r body identification and appropriate RhIg administration are
red blood cells and 1:16 against R2R2 red blood cells. Am- extremely important in preventing medicolegal situations.3
niocentesis indicated that the fetus did not appear to be af-
fected by intrauterine hemolysis. The mother delivered a 6. Yes. Pregnant women with anti-G and without anti-D in
healthy infant at 36 weeks gestation. The infant had a posi- their serum are considered candidates for prophylactic RhIg
tive direct antiglobulin test (DAT) with an acid eluate therapy at 28 weeks gestation, at delivery if the infant is
revealing the presence of anti-G. The total bilirubin (highest Rh(D) positive, and when clinically indicated (eg, for the risk
value) was 11.9 mg/dL at 5 days postpartum and no further of sensitization with amniocentesis) to prevent formation of
management was needed.4 In contrast to these findings, anti-D and potential severe complications in future pregnan- 195
among 28 sera from alloimmunized women with anti-D and cies. In our case, the patient continued to receive RhIg ther-
anti-C, 2 contained titers of anti-G consistent with moderate apy, which could have been erroneously excluded if the
to severe HDN by the chemiluminescence test. It was also possibility of an existing anti-G rather than an anti-D
noted in this study that fetal hemolysis due to anti-G was antibody was not considered. Our patient delivered a healthy
more likely to occur in r’r (C-positive, D-negative) fetuses.5 newborn at 39 weeks gestation who typed as A Rh(D) posi-
In another study, an Rh(D) negative woman with a history tive and had a negative DAT. No therapeutic interventions
of multiple transfusions of Rh(D) negative blood in the past were required.
© laboratorymedicine> march 2003> number 3> volume 34
Keywords: anti-D, anti-C, anti-G, Rh immune globulin, 3. Palfi M, Gunnarsson C. The frequency of anti-C and anti-G in the absence of
hemolytic disease of the newborn anti-D in alloimmunized pregnancies. Transfusion Med. 2001;11:207-210.
4. Cash K, Brown T, Strupp A, et al. Anti-G in a pregnant patient. Transfusion.
1999;39:531-533.
1. Judd J. Summary of RAP Session Serologic Controversies (Two G, not CD). 5. Hadley AG, Poole GD, Poole J, et al. Hemolytic disease of the newborn due to
AABB News. December 2000. anti-G. Vox Sang. 1996;71:108-112.
2. Shirey R, Mirabella D, Lumadue J, et al. Differentiation of anti-D, -C, and-G: 6. Yesus YW, Akhter JE. Hemolytic disease of the newborn due to anti-C and anti-
clinical relevance in alloimmunized pregnancies. Immunohematology. G masquerading as anti-D. Am J Clin Pathol. 1985;84:769-72.
1997;37:493.
Downloaded from http://labmed.oxfordjournals.org/ by guest on February 29, 2016
196
laboratorymedicine> march 2003> number 3> volume 34 ©
You might also like
- Immunohematology and Transfusion Medicine: A Case Study ApproachFrom EverandImmunohematology and Transfusion Medicine: A Case Study ApproachNo ratings yet
- Tmp305e TMPDocument3 pagesTmp305e TMPFrontiersNo ratings yet
- Ultrasound in Obstet Gyne - 2002 - Senat - Management of Single Fetal Death in Twin To Twin Transfusion Syndrome A RoleDocument4 pagesUltrasound in Obstet Gyne - 2002 - Senat - Management of Single Fetal Death in Twin To Twin Transfusion Syndrome A RoleBramantyo Dwi HandjonoNo ratings yet
- Applied Peritoneal Dialysis: Improving Patient OutcomesFrom EverandApplied Peritoneal Dialysis: Improving Patient OutcomesAnjay RastogiNo ratings yet
- Jurnal Vox Sanguinis - 2023 - Malhotra - Autoimmune Anti D in An RHD Positive Young Infant Learning From A Rare CaseDocument4 pagesJurnal Vox Sanguinis - 2023 - Malhotra - Autoimmune Anti D in An RHD Positive Young Infant Learning From A Rare CaseFauzan.ANo ratings yet
- Safety and Efficacy of Packed Red Blood Cell Transfusions at Different Doses in Very Low Birth Weight InfantsDocument3 pagesSafety and Efficacy of Packed Red Blood Cell Transfusions at Different Doses in Very Low Birth Weight InfantsVidini Kusuma AjiNo ratings yet
- Case Series: Newborn Haemorrhagic Disorders: About 30 CasesDocument8 pagesCase Series: Newborn Haemorrhagic Disorders: About 30 CasesNasriNo ratings yet
- Robert J. Adderley, MD, FRCP (C) Paul C.J. Rogers, T MB, MRCP, FRCP (C) Dorothy Shaw,. MB, FRCP (Ci Louis D. Wadsworth, MB, FRCP (C)Document3 pagesRobert J. Adderley, MD, FRCP (C) Paul C.J. Rogers, T MB, MRCP, FRCP (C) Dorothy Shaw,. MB, FRCP (Ci Louis D. Wadsworth, MB, FRCP (C)Sri HariNo ratings yet
- Blood Component TherapyDocument13 pagesBlood Component Therapymcbenze1607No ratings yet
- 5image BBDocument44 pages5image BBCaleb Joshua MendozaNo ratings yet
- Brmedj00461 0017Document4 pagesBrmedj00461 0017muhammad24fayazNo ratings yet
- HDN - Dr. SumadionoDocument4 pagesHDN - Dr. SumadionoJamaluddin Ahmad A.MNo ratings yet
- Ma 70 408Document5 pagesMa 70 408Zahra AfifahNo ratings yet
- Bloodproducttransfusions Andreactions: Jessica L. Osterman,, Sanjay AroraDocument12 pagesBloodproducttransfusions Andreactions: Jessica L. Osterman,, Sanjay AroraAdi ParamarthaNo ratings yet
- Acquired B Phenomenon in A Neonate Presenting Wit - 2019 - Transfusion and ApherDocument2 pagesAcquired B Phenomenon in A Neonate Presenting Wit - 2019 - Transfusion and ApherFrankenstein MelancholyNo ratings yet
- 2001-Haemolytic Disease of Newborn.Document6 pages2001-Haemolytic Disease of Newborn.蔡黑面No ratings yet
- Diagnostic Accuracy of Fetal Rhesus D Genotyping Using Cell-Free Fetal DNA During The First Trimester of PregnancyDocument5 pagesDiagnostic Accuracy of Fetal Rhesus D Genotyping Using Cell-Free Fetal DNA During The First Trimester of PregnancyRahmayani IsmaNo ratings yet
- Adverse Transfusion Reaction Form: Ministry of Health Pharmacy and Poisons Board P.O. Box 27663-00506 NAIROBIDocument1 pageAdverse Transfusion Reaction Form: Ministry of Health Pharmacy and Poisons Board P.O. Box 27663-00506 NAIROBIkrunalNo ratings yet
- Management of Blood Donors and Blood Donations From Individuals Found To Have A Positive Direct Antiglobulin TestDocument11 pagesManagement of Blood Donors and Blood Donations From Individuals Found To Have A Positive Direct Antiglobulin TestLuis Enrique Tinoco JuradoNo ratings yet
- Autoimmune Haemolytic Anaemia in A Newborn Infant: Case ReportDocument2 pagesAutoimmune Haemolytic Anaemia in A Newborn Infant: Case ReportFanny TangkudungNo ratings yet
- The Impact of in Utero Transfusions On Perinatal Outcomes in Patients With Alpha Thalassemia MajorDocument11 pagesThe Impact of in Utero Transfusions On Perinatal Outcomes in Patients With Alpha Thalassemia Majoraulia firdausNo ratings yet
- Overcoming A Positive Crossmatch in Living-Donor Kidney TransplantationDocument7 pagesOvercoming A Positive Crossmatch in Living-Donor Kidney TransplantationPratik TripathiNo ratings yet
- Effect and Clinical Value of Coagulation Test On Adverse Reactions of Blood Transfusion in Patients With Major Bleeding in Ectopic PregnancyDocument5 pagesEffect and Clinical Value of Coagulation Test On Adverse Reactions of Blood Transfusion in Patients With Major Bleeding in Ectopic PregnancyRifky TaniyoNo ratings yet
- Identification of Hepatitis B Surface Antigen Variants With Alterations Outside The "A" Determinant in Immunized Singapore InfantsDocument5 pagesIdentification of Hepatitis B Surface Antigen Variants With Alterations Outside The "A" Determinant in Immunized Singapore InfantsWa Nur Arlin RahmadhantyNo ratings yet
- DAT NeonatalDocument5 pagesDAT NeonatalAji DwijayantoNo ratings yet
- 2003 - 01 - 01 Steinborn-Scharf-Soluble HLA-DR Levels in The Maternal CirculationDocument7 pages2003 - 01 - 01 Steinborn-Scharf-Soluble HLA-DR Levels in The Maternal CirculationAlexander ScharfNo ratings yet
- Caos PaperDocument6 pagesCaos PaperMauricio Lopez MejiaNo ratings yet
- Aboi ModuleDocument38 pagesAboi ModuleRANJANEE MUTHUNo ratings yet
- Fetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaDocument4 pagesFetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaMuhammad AdithiaNo ratings yet
- Thrombocytopenia in Late Preterm and Term Neonates After Perinatal AsphyxiaDocument10 pagesThrombocytopenia in Late Preterm and Term Neonates After Perinatal AsphyxiaTammy Utami DewiNo ratings yet
- NIH Public Access: Author ManuscriptDocument12 pagesNIH Public Access: Author ManuscriptIvan HoNo ratings yet
- Hemolysis Following Platelet Transfusions From ABO-incompatible DonorsDocument3 pagesHemolysis Following Platelet Transfusions From ABO-incompatible Donorsmy accountNo ratings yet
- Transfusion and Apheresis Science: Ravneet Kaur Bedi, Kshitija Mittal, Tanvi Sood, Rakesh Kumar, Ajay S. PraveenDocument3 pagesTransfusion and Apheresis Science: Ravneet Kaur Bedi, Kshitija Mittal, Tanvi Sood, Rakesh Kumar, Ajay S. PraveenLuis Enrique Tinoco JuradoNo ratings yet
- Transfusion Medicine QuestionsDocument32 pagesTransfusion Medicine QuestionsMahmoud RamlawiNo ratings yet
- Aiha 3Document5 pagesAiha 3Andi WahyudiNo ratings yet
- E361 FullDocument12 pagesE361 FullGi PainNo ratings yet
- Rhesus IsoimmunisationDocument27 pagesRhesus IsoimmunisationMuwanga faizoNo ratings yet
- Alloimmunization in Pregnancy: Brooke Grizzell, M.DDocument40 pagesAlloimmunization in Pregnancy: Brooke Grizzell, M.DhectorNo ratings yet
- Prenatal Imaging Features Suggestive of Liver Gestational Allo Immune DiseaseDocument4 pagesPrenatal Imaging Features Suggestive of Liver Gestational Allo Immune DiseaseEuis NoorhayatyNo ratings yet
- Casos Clinicos en Ingles NeonatologiaDocument3 pagesCasos Clinicos en Ingles NeonatologiaLourdes RamírezNo ratings yet
- Uso de TTPA para Diagnostico de SCDocument7 pagesUso de TTPA para Diagnostico de SCdrirrazabalNo ratings yet
- Evidence For Feasibility of Fetal Trophoblastic Cell-Based Noninvasive Prenatal TestingDocument11 pagesEvidence For Feasibility of Fetal Trophoblastic Cell-Based Noninvasive Prenatal TestingCavin PengNo ratings yet
- Coagulation Changes in Individuals With Sickle Cell TraitDocument6 pagesCoagulation Changes in Individuals With Sickle Cell TraitMohaNo ratings yet
- Transfusi BlokDocument96 pagesTransfusi BlokTutde SedanaNo ratings yet
- Transfusion: Practices in NicuDocument80 pagesTransfusion: Practices in NicuPranay MallNo ratings yet
- Umbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialDocument5 pagesUmbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialAffah MustafaNo ratings yet
- NIAP S1 ProspectiveDocument9 pagesNIAP S1 ProspectiveA ANo ratings yet
- Clinical Reviews in Emergency MedicineDocument10 pagesClinical Reviews in Emergency MedicineJanetta RheaNo ratings yet
- Jipmer Sample Questions 2019 DR Vandana: A. Gabra 1Document16 pagesJipmer Sample Questions 2019 DR Vandana: A. Gabra 1adiNo ratings yet
- Amoxicillin and Ceftriaxone As Treatment Alternatives To Penicillin For Maternal Syphilis 2017Document3 pagesAmoxicillin and Ceftriaxone As Treatment Alternatives To Penicillin For Maternal Syphilis 2017Jose Luis Morales BautistaNo ratings yet
- Case StudyDocument7 pagesCase StudyNikitha HeleenaNo ratings yet
- Case StudyDocument7 pagesCase StudyNikitha HeleenaNo ratings yet
- Podocyturia As A DiagnosticMarker For Preeclampsia 2012Document6 pagesPodocyturia As A DiagnosticMarker For Preeclampsia 2012Diapositivas08No ratings yet
- A Practical Guide To Red Blood Cell Transfusion in ChildrenDocument6 pagesA Practical Guide To Red Blood Cell Transfusion in ChildrendovaNo ratings yet
- 2006-Intravenous Immunoglobulin in ABO and RH Hemolytic Diseases of NewbornDocument4 pages2006-Intravenous Immunoglobulin in ABO and RH Hemolytic Diseases of Newborn蔡黑面No ratings yet
- Cureus 0012 00000007812Document6 pagesCureus 0012 00000007812taufik.abdiNo ratings yet
- PR 1990572Document6 pagesPR 1990572OSUPLENTE AMARELONo ratings yet
- Platelet in DengueDocument5 pagesPlatelet in Denguekarina nilasariNo ratings yet
- Prognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisDocument6 pagesPrognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisWulan CerankNo ratings yet
- CLASS-3 MATHS Money WORKSHEETDocument7 pagesCLASS-3 MATHS Money WORKSHEETDR.RAJESWARI SUBRAMANIYANNo ratings yet
- 2004 - BJH A Physician's Guide To Transfusion in Autoimmune HaemolyticDocument5 pages2004 - BJH A Physician's Guide To Transfusion in Autoimmune HaemolyticMayada Rakhmima KarizkiNo ratings yet
- AABB Pediatric Transfusion - Risks and GuidelinesDocument57 pagesAABB Pediatric Transfusion - Risks and GuidelinesDR.RAJESWARI SUBRAMANIYANNo ratings yet
- CEO Previous Year For Class 3Document7 pagesCEO Previous Year For Class 3DR.RAJESWARI SUBRAMANIYANNo ratings yet
- HCP English Stage3 WB SampleDocument7 pagesHCP English Stage3 WB SampleDR.RAJESWARI SUBRAMANIYANNo ratings yet
- 2007 JulyAug Plasma TransfusionDocument9 pages2007 JulyAug Plasma TransfusionDR.RAJESWARI SUBRAMANIYANNo ratings yet
- Dat 3728Document2 pagesDat 3728DR.RAJESWARI SUBRAMANIYANNo ratings yet
- Using Preposition To Complete A SentenceDocument2 pagesUsing Preposition To Complete A SentenceDR.RAJESWARI SUBRAMANIYANNo ratings yet
- Geographical Features in English - Clark and MillerDocument39 pagesGeographical Features in English - Clark and MillerDR.RAJESWARI SUBRAMANIYANNo ratings yet
- Food We Eat Class 2 Evs Worksheet 7Document1 pageFood We Eat Class 2 Evs Worksheet 7DR.RAJESWARI SUBRAMANIYANNo ratings yet
- Big 1988Document145 pagesBig 1988Tony EmmerNo ratings yet
- Make Her Make MoveDocument32 pagesMake Her Make MoveAlfredo GomezNo ratings yet
- Gutierrez Hermanos vs. Court of Appeals, 178 SCRA 37Document11 pagesGutierrez Hermanos vs. Court of Appeals, 178 SCRA 37fjl_302711No ratings yet
- Perfecto Vs Esidera DigestDocument1 pagePerfecto Vs Esidera DigestCharmaine GraceNo ratings yet
- High School Brag Sheet TemplateDocument4 pagesHigh School Brag Sheet TemplateOkey OtamNo ratings yet
- Cause and Effect Sutra English and ChineseDocument84 pagesCause and Effect Sutra English and ChineseVendyChenNo ratings yet
- Causes of The Trojan War PDFDocument3 pagesCauses of The Trojan War PDFTanaya DeoNo ratings yet
- CRPC Bail PresentationDocument8 pagesCRPC Bail PresentationDishant ThakkarNo ratings yet
- Maharishi Arvind Institute of Engineering and Technology, JaipurDocument14 pagesMaharishi Arvind Institute of Engineering and Technology, JaipurDivaksh JainNo ratings yet
- Unit 1 Tpde & Pde Lecture Notes PDFDocument36 pagesUnit 1 Tpde & Pde Lecture Notes PDFpoojaabanindranNo ratings yet
- Jawaban Uts-Bahasa Inggris Bisnis IDocument3 pagesJawaban Uts-Bahasa Inggris Bisnis IAidaNo ratings yet
- CFG (31 34)Document78 pagesCFG (31 34)Abdul Sattar KianiNo ratings yet
- Evening PrayerDocument3 pagesEvening PrayerVinz B. SalmazanNo ratings yet
- Curriculum Vitea TEMPLATEDocument11 pagesCurriculum Vitea TEMPLATEHarveyNo ratings yet
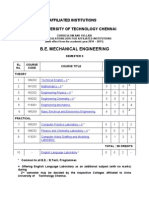
- B.E. Mechanical Engineering: Affiliated Institutions Anna University of Technology ChennaiDocument17 pagesB.E. Mechanical Engineering: Affiliated Institutions Anna University of Technology Chennaivit_mechNo ratings yet
- Generics - The Swift Programming Language (Swift 5.7)Document28 pagesGenerics - The Swift Programming Language (Swift 5.7)jomi86No ratings yet
- Baru PDFDocument4 pagesBaru PDFshribarathiNo ratings yet
- Why This App? How Educators Choose A Good Educational AppDocument17 pagesWhy This App? How Educators Choose A Good Educational AppTien ELNo ratings yet
- Fixed Income Portfolio Benchmarks 2012 01Document10 pagesFixed Income Portfolio Benchmarks 2012 01Grimoire HeartsNo ratings yet
- Stage 1 English Curriculum Framework PDFDocument2 pagesStage 1 English Curriculum Framework PDFMangunatun KhasanahNo ratings yet
- Victims and Perpetrators Testimony of Young Khmer Rouge ComradesDocument83 pagesVictims and Perpetrators Testimony of Young Khmer Rouge Comradesagarratecatalina100% (2)
- Fundamentals IKS SyllabusDocument2 pagesFundamentals IKS Syllabuspurushotampandit1No ratings yet
- Classical Psychoanalytic TheoryDocument18 pagesClassical Psychoanalytic TheoryDelonix Cattleya RegiaNo ratings yet
- Fundamental of Software Engineering: Faculty of Technology Department of Computer Science Debre Tabor UniversityDocument17 pagesFundamental of Software Engineering: Faculty of Technology Department of Computer Science Debre Tabor UniversityBethelhem YetwaleNo ratings yet
- St. Paul City Council Legislation TextDocument3 pagesSt. Paul City Council Legislation TextPGurusNo ratings yet
- Essential Drugs FlowchartsDocument10 pagesEssential Drugs FlowchartsanilkumarappapurapuNo ratings yet
- Para MidtermsDocument126 pagesPara Midtermshezekiah hezNo ratings yet
- Materi TOEFL 02 AprilDocument66 pagesMateri TOEFL 02 AprilamelianurlaelasariNo ratings yet
- Tara LagnaDocument10 pagesTara LagnaNarotham Reddy100% (1)
- TOS For EIM Grade 9 & 10Document2 pagesTOS For EIM Grade 9 & 10Sanja Shishin100% (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (20)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet