Professional Documents
Culture Documents
Ultrasound in Obstet Gyne - 2002 - Senat - Management of Single Fetal Death in Twin To Twin Transfusion Syndrome A Role
Uploaded by
Bramantyo Dwi HandjonoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ultrasound in Obstet Gyne - 2002 - Senat - Management of Single Fetal Death in Twin To Twin Transfusion Syndrome A Role
Uploaded by
Bramantyo Dwi HandjonoCopyright:
Available Formats
Ultrasound Obstet Gynecol 2002; 20: 360 – 363
Management of single fetal death in twin-to-twin transfusion
Blackwell Science, Ltd
syndrome: a role for fetal blood sampling
M.-V. SENAT*, J.-P. BERNARD*, S. LOIZEAU* and Y. VILLE*
*Department of Obstetrics and Gynecology, Paris-Ouest University, CHI Poissy-St-Germain, France
KEYWORDS: Fetal blood sampling, Intrauterine transfusion, Single fetal death, Twin–twin transfusion
ABSTRACT INTRODUCTION
Objective Intrauterine death of one twin in monochorionic Twins have a higher mortality and morbidity than singletons
pregnancies is associated with an increased mortality and mor- and among twin pregnancies the risks are even higher when
bidity of the cotwin. This is likely to occur as a consequence of they are monochorionic1–7. The mechanism of intrauterine
acute hemodynamic changes due to feto–fetal hemorrhage at death in one monochorionic twin and its association with
the time of death of the cotwin. We assessed the role of fetal increased mortality and morbidity in the surviving cotwin is
blood sampling and intrauterine transfusion to rescue the still debated, although two theories have been proposed. The
survivor. embolization theory suggests that the injuries observed among
survivors are related to the passage of thromboplastic
Materials and methods We managed 12 cases of single material from the dead twin to the live one via the placental
intrauterine death at between 17 and 26 weeks’ gestation in anastomoses leading to the development of disseminated
monochorionic twins complicated by twin-to-twin transfusion intravascular coagulation (DIVC)8–10. The second and most
syndrome (TTTS). All these cases had been treated either by convincing theory involves exsanguination of the survivor
laser therapy or by serial amniodrainage. When the demise of into the dead fetus just before or at the time of death when
one twin occurred, ultrasound-guided fetal blood sampling its blood pressure drops dramatically11–14. If this mechanism
was performed in the surviving twin using a 20-gauge needle is mainly responsible for the morbidity seen in the survivor,
within 24 h of death. Intrauterine transfusion was performed it may then be reasonable to assume that early intervention
at the same time in cases where the survivor was anemic. All could largely prevent the morbid consequences. Twin-to-twin
survivors were assessed in the neonatal period and at 1 year transfusion syndrome (TTTS) is characterized by a more
of age. severe form of hemodynamic imbalance and instability. In
Results Six of the 12 surviving fetuses were found to be TTTS treated by either laser coagulation15 or amniodrainage
anemic and underwent intrauterine transfusion. All fetuses one could argue that occlusion of some anastomoses is totally
survived the procedure. Four of these fetuses had normal lacking with the latter technique, but could still be incomplete
neurological development at 1 year of age. Periventricular following laser coagulation owing to technical difficulties.
leukomalacia developed in one case and the patient under- The management of intrauterine death of one twin by fetal
went termination of pregnancy at 34 weeks. In one case blood sampling and subsequent intrauterine transfusion
delivery occurred at 34 weeks’ gestation and the baby devel- (IUT) of the anemic survivors may therefore rescue these
oped periventricular leukomalacia at 1 month of age. In all fetuses from prolonged hypovolemia/anemia.
six non-anemic fetuses pediatric examination was normal at The aim of this study was to assess the role of fetal blood
birth and at 1 year of age. sampling and IUT to rescue the survivor within 24 h of the
death of one monochorionic cotwin in TTTS.
Conclusion Intrauterine death of one monochorionic twin
in TTTS puts the survivor at high risk of intrauterine death or
MATERIALS AND METHODS
of developing ischemic/hypoxic lesions. Our results suggest
that fetal blood sampling is a useful diagnostic tool to identify Over a 2-year period we reviewed 12 cases of single intrauterine
those fetuses that are not anemic and hence unlikely to be at death in monochorionic pregnancies complicated by TTTS
risk of developing a cerebral lesion. occurring between 17 and 26 weeks’ gestation. All these
Correspondence: Prof Y. Ville, Service de Gynécologie Obstétrique, Hôpital de Poissy, Rue du Champ Gaillard, 78300 Poissy, France
(e-mail: yville@wanadoo.fr)
Accepted 7-5-02
360 ORIGINAL PAPER
14690705, 2002, 4, Downloaded from https://obgyn.onlinelibrary.wiley.com/doi/10.1046/j.1469-0705.2002.00815.x by Nat Prov Indonesia, Wiley Online Library on [17/02/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Single fetal death in TTTS Senat et al.
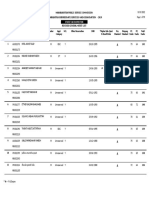
Table 1 Summary of clinical and hematological characteristics of the 12 survivors following intrauterine death of their monochorionic cotwin in twin-
to-twin transfusion syndrome
Treatment L L L L L L A A A A A+L L+C
GA at treatment (weeks) 22 21 21 23 20 18 26 24 20 17 (22,24) (20,25)
Dead twin (D/R) R R R D R D R R D D D R
Ultrasound markers of fetal anemia minor minor minor none none none none major none none major none
(1) (1) (1) (2) (2)
Hb pretransfusion (g /dL) 16 11 12 14 6.8 20 6.1 5.1 13.2 3.8 7.0 8.0
Hb post-transfusion (g /dL) NA NA NA NA 11.5 NA 12.6 12.8 NA 11.9 13 12
Intrauterine transfusion no no no no yes no yes yes no yes yes yes
GA at delivery (weeks) 38 37 35 34 36 38 28 34 37 34 PVL 36 29
TOP
Morbidity at 1 year of age no no no no no no no PVL no no no
L, laser; A, amniodrainage; C, cord coagulation; GA, gestational age; R, recipient; D, donor; Hb, hemoglobin concentration; PVL, periventricular
leukomalacia; TOP, termination of pregnancy; (1) frontal edema, echogenic bowel; (2) ascites and/or generalized edema.
pregnancies had been treated either with laser coagulation or was performed in six cases at 18–23 weeks’ gestation. One
with serial amniodrainage following prenatal diagnosis patient had an amniodrainage at 22 weeks and a laser pro-
(Table 1). When the demise of one twin occurred, fetal blood cedure 2 weeks later. One patient had a laser procedure at
sampling was performed in the surviving twin with a 20-gauge 20 weeks’ gestation followed by cord coagulation in one twin
needle within 24 h. IUT was performed under ultrasound at 25 weeks’ gestation. Seven recipients and five donors died.
guidance in cases where the survivor was anemic, with the aim All deaths occurred within 3 days of the procedure. Six of the
of correcting the effect of hypovolemia/anemia in the devel- 12 surviving fetuses were found to be anemic and IUT was
opment of tissue ischemia. The site of sampling was the placental then performed (Figure 1). The volume of blood that was
cord insertion in all cases. Fetal hematology was assessed transfused was calculated according to the concentration of
with hemo-cue and compatible ORh-irradiated adult blood the donor blood, the fetal hemoglobin concentration and the
was used for IUT when indicated. Confirmation of fetal estimated fetal weight16. Of these six fetuses only two had
hematology was obtained later through the usual techniques major ultrasound markers of fetal anemia with an otherwise
from the hematology laboratory. Weekly anomaly scans normal biophysical profile: frontal edema, mild ascites,
and Doppler investigations were performed following IUT hyperechogenic bowel, absent or reversed flow during atrial
and magnetic resonance imaging (MRI) was performed at contraction in the ductus venosus. All fetuses survived the
32 weeks’ gestation. At the time of delivery the neonates under- procedure. In one case ultrasound and MRI follow-up
went a complete clinical examination as well as transfont- showed periventricular leukomalacia at 34 weeks’ gestation
anellar ultrasound at birth. All survivors were re-assessed and the patient underwent termination of pregnancy. In two
at the age of 1 year. Placentae all underwent histological cases delivery was close to term and these fetuses had a
examination. normal neurological development at 1 year of age. In two
cases delivery occurred 2 and 4 weeks following IUT. These
fetuses were born prematurely at 28 and 29 weeks’ gestation,
RESULTS
respectively. They also had normal neurological development
Amniodrainage was performed in four cases at 17, 20, 24 and at 1 year of age. In one case delivery occurred at 34 weeks’
26 weeks’ gestation, respectively. Laser coagulation alone gestation and the baby developed periventricular leukomalacia
at the age of 1 month, despite normal weekly ultrasound and
MRI antenatal follow-up and normal antenatal MRI. The
neonatal brain scan was also normal in that case. In the six
non-anemic fetuses follow-up anomaly scans and Doppler
remained normal and the pregnancies were uneventful.
Spontaneous delivery occurred between 34 and 38 weeks of
gestation. Pediatric examination was normal at birth and at
1 year of age. There was no evidence of hypoxic or ischemic
brain injury. Results are summarized in Table 1.
Histological examination of the placentae confirmed
monochorionicity in all cases.
D ISC U SSIO N
In the present series of 12 cases of single intrauterine death
Figure 1 Hemoglobin pretransfusion (䉭) and post-transfusion (䉱) in in monochorionic twins complicated by TTTS, there were 10
relation to gestational age. healthy survivors including four anemic fetuses managed
Ultrasound in Obstetrics and Gynecology 361
14690705, 2002, 4, Downloaded from https://obgyn.onlinelibrary.wiley.com/doi/10.1046/j.1469-0705.2002.00815.x by Nat Prov Indonesia, Wiley Online Library on [17/02/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Single fetal death in TTTS Senat et al.
with IUT and six non-anemic fetuses who underwent fetal occluded placental anastomoses in five and three cases,
blood sampling without transfusion. One of the anemic respectively. This is likely to prevent at least partly profound
fetuses survived but developed periventricular leukomalacia hypovolemia/hypotension from occurring in the survivor.
at 1 month of age despite IUT within 24 h after the death Indeed in the amniodrainage group, two survivors out of
of its cotwin. This study supports the data of Nicolini et al. three developed periventricular leukomalacia despite IUT,
who found that in non-occlusive management all survivors whereas none of the three anemic fetuses did in the laser
sampled within 24 h after death of the cotwin were group. However, such small numbers do not allow for any
anemic14. Okamura et al. also described three of five sur- meaningful statistics to be done.
vivors with anemia when sampled within 24 h of death of Intrauterine death of one monochorionic twin therefore
their cotwin13. puts the survivor at a high risk of intrauterine death or of
Intrauterine death of one twin is associated with an in- developing ischemic/hypoxic lesions. Fetal blood sampling
creased neurological morbidity in the cotwin when it survives17. can be performed to evaluate the hematological condition of
Cerebral and renal damage following hemorrhage-related hypo- the survivor since ultrasound cannot always show markers of
tension are the main factors of morbidity17,18. The hypothesis fetal anemia. Frontal edema and hypoechogenic bowel can be
that there is a passage of thromboplastin-like substances mistaken for subtle signs of fetal anemia in the context of
from the dead twin to the surviving twin through placental intrauterine death of the cotwin. However, when this occurs
vascular anastomoses, leading to intrauterine DIVC8–10, after laser coagulation, it is also likely to reflect transient fetal
has never been shown by fetal or neonatal investigations. hypertension following ablation of placental vessels23.
This hypothesis is only based on postmortem findings of Indeed in our series three non-anemic survivors presented
areas of infarction and necrosis in the brain and kidneys these ultrasound features following laser therapy. The non-
of dead monochorionic twins. Moreover the coagulation anemic group had a good outcome. Our results suggest that
profile in the surviving fetuses after the death of the cotwin fetal blood sampling is a useful diagnostic tool following the
were found to be normal at fetal blood sampling11,13,20. death of a twin in TTTS to identify fetuses that are not anemic
In constrast, well-documented papers support that morbid- and hence unlikely to be at risk of developing a cerebral
ity in the surviving fetus is due to acute hemodynamic lesion. Fetuses that are anemic remain at high risk, especially
decompensation just before or at the time of death of the when no occlusive technique has been used initially to de-
cotwin when its blood pressure drops, leading to exsanguina- crease feto–fetal exsanguination. After extensive counseling
tion of the live fetus into the dead one across placental regarding the risks of these invasive procedures, fetal blood
anastomoses11–14. Consequently acute and profound sampling and IUT may therefore prove to be a useful inter-
hemodynamic changes with hypovolemia and anemia can vention. This observation will need to be confirmed in a
occur in the survivor and may be responsible for the develop- larger series.
ment of ischemic lesions and particularly periventricular
leukomalacia. This acute phenomenon is probably even more
REFERENCES
marked in monochorionic twins with TTTS, and will depend
on the number and size of vascular placental anastomoses 1 Ho SK, Wu Pyk. Perinatal factors and neonatal morbidity in twin
pregnancy. Am J Obstet Gynecol 1975; 122: 979– 87
since large quantities of fetal blood can rapidly be transferred
2 Naeye RL, Tafari N, Judge D, Marboe CC. Twins: causes of peri-
across these vessels. An unfavorable outcome was reported natal death in 12 US cities and in one African city. Am J Obstet Gynecol
in monochorionic twins with the association of unidirec- 1978; 131: 267– 72
tional artery–vein anastomoses and artery–artery superficial 3 Derom R, Vlietnik R, Derom C, Thiery M, Van Maele G, Vanden-
anastomoses on monochorionic placentae20. Laser treat- Berghe H. Perinatal mortality in the east Flanders prospective twin
survey. Eur J Obstet Gynecol Reprod Biol 1991; 41: 25– 6
ment aims at occluding all placental vascular anastomoses,
4 Potter EL. Twin zygocity and placental form in relation to the
which is not always entirely feasible, while amniodrainage outcome of pregnancy. Am J Obstet Gynecol 1963; 87: 566–77
should have no occluding effect. The hemodynamic theory 5 Myrianthopoulos MC. An epidemiologic survey of twins in a large
was proposed by Fusi et al. as one of the recipients was prospectively studied population. Am J Hum Genet 1970; 22: 611– 29
found to be anemic after the death of the donor twin11. This 6 Nylander PPS. Perinatal mortality in twins. Acta Genet Med Gemel-
lol 1979; 28: 263
was later confirmed by Okamura et al.13. In our study the
7 Pharoah POD, Adi Y. Consequences of in-utero death in a twin
prognosis of the surviving twin seems to be better than in pregnancy. Lancet 2000; 355: 1597– 602
other series12–14,22,23. Indeed only two children out of 12 8 Benirschke K. Twin placenta in perinatal mortality. N Y State
developed periventricular leukomalacia. Only one recent J Med 1961; 1: 1499–507
study reported similar management in single intrauterine 9 Schinzel AAGL, Smith DW, Miller JR. Monozygotic twinning and
structural defects. J Pediatr 1979; 95: 921– 30
death in seven cases of TTTS22. These fetuses underwent
10 Moore CM, McAdams AJ, Sutherland J. Intrauterine disseminated
IUT within 24 h following the demise of the cotwin. Two intravascular coagulation: a syndrome of multiple pregnancy with a
fetuses died in utero and two fetuses developed cerebral dead twin fetus. J Pediatr 1969; 74: 523– 8
lesions and termination of pregnancy was performed. There 11 Fusi L, McParland P, Fisk P, Nicolini U, Wigglesworth J. Acute
was one neonatal death and only two fetuses were born alive twin–twin transfusion syndrome: possible mechanism for brain
damaged survivors after intrauterine death of a monochorionic twin.
and had a favorable outcome. The main difference with our
Obstet Gynecol 1991; 78: 517– 20.
series is that laser was performed in eight cases out of 12 and 12 Fusi L, Gordon H. Twin pregnancy complicated by single intra-
only three survivors were anemic in this group. One can uterine death. Problems and outcome with conservative management.
therefore assume that laser had completely or partially Br J Obstet Gynaecol 1990; 97: 511– 6
362 Ultrasound in Obstetrics and Gynecology
14690705, 2002, 4, Downloaded from https://obgyn.onlinelibrary.wiley.com/doi/10.1046/j.1469-0705.2002.00815.x by Nat Prov Indonesia, Wiley Online Library on [17/02/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Single fetal death in TTTS Senat et al.
13 Okamura K, Murotsuki J, Tanigawara S, Uehara S, Yajima A. 19 Prompeler HJ, Madjar H, Klosa W, Dubois A, Zahradnik HP,
Funipuncture for evaluation of hematologic and coagulation indices Schillinger H, Breckwoldt M. Twin pregnancies with single fetal
in the surviving twin following co-twin’s death. Obstet Gynecol death. Acta Obstet Gynecol Scand 1994; 73: 205– 8
1994; 83: 975 – 8 20 Weeks AD, Davies NP, Sprigg A, Fairlie FM. The sequential in utero
14 Nicolini U, Pisoni MP, Cela E, Roberts A. Fetal blood sample imme- death of heterokaryotic monozygotic twins. A case report and
diately before and within 24 hours of death in monochorionic twin literature review. Prenat Diagn 1996; 16: 657– 663
pregnancies complicated by single intrauterine death. Am J Obstet 21 Bajoria R, Wee L, Anwar S, Ward S. Outcome of twin pregnancies
Gynecol 1998; 179: 800 – 3 complicated by single intrauterine death in relation to vascular
15 Ville Y, Hecher K, Gagnon A, Sabire N, Hyett J, Nicolaides I. Endo- anatomy of the monochorionic placenta. Hum Reprod 1999; 8:
scopic laser coagulation in the management of severe twin-to-twin 2124–30
transfusion syndrome. Br J Obstet Gynaecol 1998; 105: 446– 53 22 Saito K, Ohtsu Y, Amano K, Nishijima M. Perinatal outcome and
16 Nicolaides KH, Rodeck CH, Misbasham RS, Kemp JR. Have Liley management of single fetal death in twin pregnancy. A case series and
charts outlived their usefulness? Am J Obstet Gynecol 1985; 152: review. J Perinat Med 1999; 27: 473– 7
341– 9 23 Tanawattanacharoen S, Taylor MJO, Letsky E, Cox P, Cowan F,
17 Petterson B, Nelson KB, Watson L, Stanley F. Twins, triplets and Fisk N. Intrauterine rescue transfusion in monochorionic multiple
cerebral palsy in births in Western Australia in the 1980s. Br Med J pregnancies with recent single intrauterine death. Prenat Diagn
1993; 307: 1239 – 943 2001; 21: 274– 8
18 Isimatu J, Hori D, Miyajima S, Hamada T, Yakushiji M, Nishimi T. 24 Zikulnig L, Hecher K, Bregenzer T, Baz E, Hackeloer BJ. Prognostic
Twin pregnancies complicated by the death of one fetus in the second factors in severe twin–twin transfusion syndrome treated by endoscopic
or third trimester. J Matern Fetal Invest 1994; 4: 141– 4 laser surgery. Ultrasound Obstet Gynecol 1999; 14: 380 –7
Ultrasound in Obstetrics and Gynecology 363
You might also like
- Introduction To Occupational Therapy PDFDocument291 pagesIntroduction To Occupational Therapy PDFMurat Hasan BaşaranNo ratings yet
- Book - MOSBY'S DENTAL DRUG REFERENCE PDFDocument1,496 pagesBook - MOSBY'S DENTAL DRUG REFERENCE PDFMohamed Faizal78% (9)
- Musculoskeletal Clinical Translation FrameworkDocument1 pageMusculoskeletal Clinical Translation FrameworkRafaelNo ratings yet
- EFT GuideDocument11 pagesEFT Guidenokaion19% (26)
- Prognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisDocument6 pagesPrognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisWulan CerankNo ratings yet
- The Diagram Shows How A Company Called HB Office RDocument1 pageThe Diagram Shows How A Company Called HB Office RbugakNo ratings yet
- Snake Bite SOPDocument5 pagesSnake Bite SOPRaza Muhammad SoomroNo ratings yet
- FEDIAF Nutritional Guidelines 2020 20200917Document96 pagesFEDIAF Nutritional Guidelines 2020 20200917luciana ribeiroNo ratings yet
- Intraventricular HemorrhageDocument11 pagesIntraventricular HemorrhagemeraivyNo ratings yet
- 1 s2.0 S1028455920301753 MainDocument4 pages1 s2.0 S1028455920301753 MainAditi SoniNo ratings yet
- Case Series: Newborn Haemorrhagic Disorders: About 30 CasesDocument8 pagesCase Series: Newborn Haemorrhagic Disorders: About 30 CasesNasriNo ratings yet
- Prenatal Imaging Features Suggestive of Liver Gestational Allo Immune DiseaseDocument4 pagesPrenatal Imaging Features Suggestive of Liver Gestational Allo Immune DiseaseEuis NoorhayatyNo ratings yet
- Hydatidiform Mole Vs PMDDocument6 pagesHydatidiform Mole Vs PMDNADIANo ratings yet
- Caos PaperDocument6 pagesCaos PaperMauricio Lopez MejiaNo ratings yet
- Uterine Rupture at 21 Weeks in Twin Pregnancy WithDocument5 pagesUterine Rupture at 21 Weeks in Twin Pregnancy WithGatoso OsoNo ratings yet
- DIC in Abruptio 2Document5 pagesDIC in Abruptio 2HoneylynNo ratings yet
- C. Eckmann-Scholz, J. Mallek, A. Caliebe, S. HeidemannDocument2 pagesC. Eckmann-Scholz, J. Mallek, A. Caliebe, S. HeidemannKeith Mark AlmarinesNo ratings yet
- J. Hackett, L. Hall, M. Sadiq, M. Putheran, B. Hall, S. Burn, A. Sharp, Z. Alfirevic, U. AgarwalDocument7 pagesJ. Hackett, L. Hall, M. Sadiq, M. Putheran, B. Hall, S. Burn, A. Sharp, Z. Alfirevic, U. AgarwalerasmohuertasNo ratings yet
- Janiak Et Al-2014-Ultrasound in Obstetrics & GynecologyDocument1 pageJaniak Et Al-2014-Ultrasound in Obstetrics & GynecologyWira PutriNo ratings yet
- Umbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialDocument5 pagesUmbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialAffah MustafaNo ratings yet
- NONIMMUNE HYDROPS FETALIS Journal of Clinical MedicineDocument8 pagesNONIMMUNE HYDROPS FETALIS Journal of Clinical MedicineTifanny TantosoNo ratings yet
- Perinatal Transient Myeloproliferative Disorder in Trisomy 21Document11 pagesPerinatal Transient Myeloproliferative Disorder in Trisomy 21Carina SuarezNo ratings yet
- Cog NTDocument11 pagesCog NTFabiolaQuijaiteNo ratings yet
- Fonc 11 803994Document13 pagesFonc 11 803994zahra abdurrazakNo ratings yet
- Uog 232Document7 pagesUog 232anon_118437533No ratings yet
- Leukapheresis in Management of Hyperleukocytosis in Children's LeukemiasDocument5 pagesLeukapheresis in Management of Hyperleukocytosis in Children's LeukemiasMira SrikandiNo ratings yet
- Hom 3Document7 pagesHom 3Mira SrikandiNo ratings yet
- Endovaginal Ultrasound and Doppler Findings After First-Trimester Abortion (Journal of Diagnostic Medical Sonography, Vol. 9, Issue 2) (1993)Document1 pageEndovaginal Ultrasound and Doppler Findings After First-Trimester Abortion (Journal of Diagnostic Medical Sonography, Vol. 9, Issue 2) (1993)Orchid LandNo ratings yet
- Vitelline Duct Pathogenesis in NeonatesDocument5 pagesVitelline Duct Pathogenesis in NeonatesRonjavafantillanNo ratings yet
- The Use of Plasma Exchange in A Very Earlyonset and Life Threatening Hemolysis Elevated Liver Enzymes and Low Platelet Hellp Syndr 2161 0932 1000387Document4 pagesThe Use of Plasma Exchange in A Very Earlyonset and Life Threatening Hemolysis Elevated Liver Enzymes and Low Platelet Hellp Syndr 2161 0932 1000387Alfa FebriandaNo ratings yet
- Spontaneous Rupture of The Uterine Artery in An Otherwise Normal PregnancyDocument7 pagesSpontaneous Rupture of The Uterine Artery in An Otherwise Normal PregnancyhendrayatiranyNo ratings yet
- The Impact of in Utero Transfusions On Perinatal Outcomes in Patients With Alpha Thalassemia MajorDocument11 pagesThe Impact of in Utero Transfusions On Perinatal Outcomes in Patients With Alpha Thalassemia Majoraulia firdausNo ratings yet
- Safety and Efficacy of Packed Red Blood Cell Transfusions at Different Doses in Very Low Birth Weight InfantsDocument3 pagesSafety and Efficacy of Packed Red Blood Cell Transfusions at Different Doses in Very Low Birth Weight InfantsVidini Kusuma AjiNo ratings yet
- Anti GDocument4 pagesAnti GDR.RAJESWARI SUBRAMANIYANNo ratings yet
- Jsafog 13 137Document5 pagesJsafog 13 137Elizabeth Duprat GaxiolaNo ratings yet
- Hmole Case ReviewDocument5 pagesHmole Case ReviewJonalyn EtongNo ratings yet
- 2009 DV Aortic Isthmus FGR Blood Flow GratacosDocument5 pages2009 DV Aortic Isthmus FGR Blood Flow GratacosRibeiro SáNo ratings yet
- Supportive Management of Pregnancy-Associated Aplastic AnemiaDocument6 pagesSupportive Management of Pregnancy-Associated Aplastic AnemiaAs YuYu MustafaNo ratings yet
- Selective Feticide in Complicated Monochorionic Twin Pregnancies Using Ultrasound-Guided Bipolar Cord CoagulationDocument5 pagesSelective Feticide in Complicated Monochorionic Twin Pregnancies Using Ultrasound-Guided Bipolar Cord CoagulationDesyHandayaniNo ratings yet
- Monoamniotic Twin Pregnancies: Antenatal Management and Perinatal Results of 19 Consecutive CasesDocument6 pagesMonoamniotic Twin Pregnancies: Antenatal Management and Perinatal Results of 19 Consecutive CasesNovd NovitaNo ratings yet
- 10.7556 Jaoa.2019.032Document4 pages10.7556 Jaoa.2019.032Luana MesquitaNo ratings yet
- 2001-Haemolytic Disease of Newborn.Document6 pages2001-Haemolytic Disease of Newborn.蔡黑面No ratings yet
- Updates in Red Blood Cell and Platelet Transfusions in Preterm NeonatesDocument4 pagesUpdates in Red Blood Cell and Platelet Transfusions in Preterm NeonatesEmilio Emmanué Escobar CruzNo ratings yet
- Neonatal Anemia (About 162 Cases)Document4 pagesNeonatal Anemia (About 162 Cases)IJAR JOURNALNo ratings yet
- Dev Riend T 1998Document5 pagesDev Riend T 1998Sarly FebrianaNo ratings yet
- Fetomaternal Hemorrhage (FMH), An Update Review of LiteratureDocument35 pagesFetomaternal Hemorrhage (FMH), An Update Review of LiteratureEugenia Jeniffer JNo ratings yet
- Prenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromaDocument5 pagesPrenatal Management, Pregnancy and Pediatric Outcomes in Fetuses With Septated Cystic HygromawitaNo ratings yet
- Red Cell AlloimmunizationDocument54 pagesRed Cell Alloimmunizationበአምላክ ጋሻዬ በዛNo ratings yet
- Multifetal PregnancyDocument42 pagesMultifetal PregnancyRisman TangdiNo ratings yet
- Neonatal Transfusion PracticeDocument6 pagesNeonatal Transfusion Practicemaag67No ratings yet
- Hemorrhagic Disease of Newborn: A Prospective Study of Clinical Features and OutcomeDocument5 pagesHemorrhagic Disease of Newborn: A Prospective Study of Clinical Features and OutcomeIan SutejaNo ratings yet
- Kovac 2020 Pregnancy After Kidney TransplantationDocument5 pagesKovac 2020 Pregnancy After Kidney TransplantationBCR ABLNo ratings yet
- Twin PregnancyDocument73 pagesTwin Pregnancykrishna mandalNo ratings yet
- Fped 09 801955Document9 pagesFped 09 801955YandiNo ratings yet
- Case Report - : Fetal Surface Placental Hematomas: The Clue in The Diagnosis of A Bleeding DyscrasiaDocument3 pagesCase Report - : Fetal Surface Placental Hematomas: The Clue in The Diagnosis of A Bleeding DyscrasiaCostin VrabieNo ratings yet
- Seminar: Michael J Seckl, Neil J Sebire, Ross S BerkowitzDocument13 pagesSeminar: Michael J Seckl, Neil J Sebire, Ross S BerkowitzFelicia HalimNo ratings yet
- 194 265 1 SMDocument5 pages194 265 1 SMAdkhiatul MuslihatinNo ratings yet
- J J Gynec Obst 2 3 020 PDFDocument4 pagesJ J Gynec Obst 2 3 020 PDFAnonymous nz9rhHNo ratings yet
- Outcome of Pregnancies With Hellp Syndrome Complicated by Acute Renal Failure 1989 1999Document10 pagesOutcome of Pregnancies With Hellp Syndrome Complicated by Acute Renal Failure 1989 1999ugidimasNo ratings yet
- Twin-To-Twin Transfusion Syndrome (TTTS)Document28 pagesTwin-To-Twin Transfusion Syndrome (TTTS)Chandeep VasuNo ratings yet
- Kobayashi 2014Document7 pagesKobayashi 2014Mauricio Lopez MejiaNo ratings yet
- Multifetal Pregnancy: Early Diagnosis and ManagementDocument33 pagesMultifetal Pregnancy: Early Diagnosis and ManagementjasmniaNo ratings yet
- 2851-26. 31 Rasheed Eclampsia-1625840448Document3 pages2851-26. 31 Rasheed Eclampsia-1625840448Umair HasanNo ratings yet
- 182 FullDocument15 pages182 FullSonia BalintNo ratings yet
- Effect of Association of Thrombocytopenia With Anemia On Feto-Maternal OutcomeDocument8 pagesEffect of Association of Thrombocytopenia With Anemia On Feto-Maternal OutcomeIJAR JOURNALNo ratings yet
- Ectopic Abdominal Pregnancies: About 2 CasesDocument10 pagesEctopic Abdominal Pregnancies: About 2 CasesIJAR JOURNALNo ratings yet
- Diagnosis Dan Penatalaksanaan Limfoma Orbita. Lohita Cakrawarti AzDocument11 pagesDiagnosis Dan Penatalaksanaan Limfoma Orbita. Lohita Cakrawarti AzBramantyo Dwi HandjonoNo ratings yet
- Post-Infectious Guillain-Barré Syndrome Related To SARS-CoV-2 Infection A Systematic ReviewDocument16 pagesPost-Infectious Guillain-Barré Syndrome Related To SARS-CoV-2 Infection A Systematic ReviewBramantyo Dwi HandjonoNo ratings yet
- 2018 Guidelines For The Management of Dyslipidemia: Correspondence To In-Kyung Jeong, M.DDocument49 pages2018 Guidelines For The Management of Dyslipidemia: Correspondence To In-Kyung Jeong, M.DBramantyo Dwi HandjonoNo ratings yet
- Hyperlipidemia: Practice GapsDocument12 pagesHyperlipidemia: Practice GapsBramantyo Dwi HandjonoNo ratings yet
- Hypercholesterolaemia and Its Management: Clinical ReviewDocument6 pagesHypercholesterolaemia and Its Management: Clinical ReviewAchmad Faiz SulaimanNo ratings yet
- Special Communication: Risk Assessment: First Step in Risk ManagementDocument12 pagesSpecial Communication: Risk Assessment: First Step in Risk ManagementBramantyo Dwi HandjonoNo ratings yet
- Inguinal Hernias: BMJ (Online) March 2008Document5 pagesInguinal Hernias: BMJ (Online) March 2008Karl PinedaNo ratings yet
- Company Name: Aims Industries LTDDocument40 pagesCompany Name: Aims Industries LTDkishoreNo ratings yet
- Diana Barnett Course Critique n5327 RDocument4 pagesDiana Barnett Course Critique n5327 Rapi-308950624No ratings yet
- Example of A NHS Risk Rating MatrixDocument2 pagesExample of A NHS Risk Rating MatrixRochady SetiantoNo ratings yet
- Drug Study 1Document2 pagesDrug Study 1Hafza MacabatoNo ratings yet
- ProQual Fees Schedule June 2021Document19 pagesProQual Fees Schedule June 2021Sohail SNo ratings yet
- Assess PDFDocument9 pagesAssess PDFJov'z GuerreroNo ratings yet
- (Yabanci Dil Testi) : T.C. Millî Eğitim Bakanliği Ölçme, Değerlendirme Ve Sinav Hizmetleri Genel MüdürlüğüDocument22 pages(Yabanci Dil Testi) : T.C. Millî Eğitim Bakanliği Ölçme, Değerlendirme Ve Sinav Hizmetleri Genel Müdürlüğücem kayaNo ratings yet
- SR - Hse Officer (8104)Document5 pagesSR - Hse Officer (8104)Nijo Joseph100% (1)
- MSDS Aceite CastorDocument6 pagesMSDS Aceite CastorwaddydiNo ratings yet
- Back Pain During PregnancyDocument3 pagesBack Pain During PregnancyDr. Sadhana KalaNo ratings yet
- Anxiety Disorder by SlidesgoDocument55 pagesAnxiety Disorder by SlidesgoShey DraftsNo ratings yet
- Types Causes Signs and Symptomps Intellectual DisabilityDocument2 pagesTypes Causes Signs and Symptomps Intellectual DisabilityMae Ann Jean JustolNo ratings yet
- Migraine HeadachesDocument15 pagesMigraine Headachesdheeksha puvvadaNo ratings yet
- Covid-19 RT-PCR Test Report & Certification: Certificate IssuedDocument1 pageCovid-19 RT-PCR Test Report & Certification: Certificate IssuedJerome OliverosNo ratings yet
- Trail Mix Cookies IKDocument24 pagesTrail Mix Cookies IKDwi Intan WNo ratings yet
- Calories Needed For A 17 Year Old, 70 KG MaleDocument7 pagesCalories Needed For A 17 Year Old, 70 KG Maleboom boomNo ratings yet
- CephalosporinsDocument20 pagesCephalosporinsBianca Andrea RagazaNo ratings yet
- Maharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019Document59 pagesMaharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019S KatyarmalNo ratings yet
- Factitious DisorderDocument6 pagesFactitious DisorderRon JaredNo ratings yet
- Lab Report 15438869 20231127064225Document1 pageLab Report 15438869 20231127064225carilloabhe21No ratings yet
- Acupuncture LectureDocument10 pagesAcupuncture Lectureapi-5481010020% (1)
- Unit - 1 Concepts and Definitions 1.1 Disaster (I)Document25 pagesUnit - 1 Concepts and Definitions 1.1 Disaster (I)RISHITHA LELLANo ratings yet