Professional Documents
Culture Documents
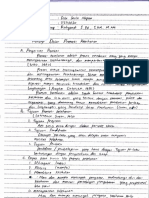
Lampiran
Lampiran
Uploaded by
dila laila nafisa0 ratings0% found this document useful (0 votes)
15 views18 pagesOriginal Title
2. Lampiran
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
15 views18 pagesLampiran
Lampiran
Uploaded by
dila laila nafisaCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 18
‘The cent issue a il ext achive of hs journal is availabe on eral Isght at:
srr emeralinsight.com2586-840X htm
352
‘eee ee 8
Effectiveness of the intervention
program for dengue hemorrhagic
fever prevention among rural
communities in Thailand
A quasi-experimental study
Suda Hanklang
Faculty of Nursing, Vongchavalitkul University, Nakhon Ratchasima, Thailand
Paul Ratanasiripong
California State University, Long Beach, California, USA, and
Suleegorn Sivasan
Faculty of Nursing, Vongchavalitkul University, Nakhon Ratchasima, Thailand
Abstract,
Purpose — The purpose of this paper isto evaluate the effectiveness ofthe intervention program for dengue
fever preveation azn peopl nul companies.
Designimethodology/approsch ~ A quasvexperimental study was designed for two groups
iBlerveation group recived
Ienowiedge broadcast, campaign, model house contest ané group edcaton, The ¢
any the tal sare of health promoting hospitals. The primary expected ostoomes were changes in
Knowledge, perceived susceptbilty, pesceived severity, perceived. benefit perceived baits and
preventive’ action from bastline data, postinterveation and threesvonth followup, along with
Eamparison between the two groups. The secondary expected outcomes were changes i house index
(i) irom baseline to postantervention and threem
"he eo groupe.
Findings — From the total of 64 participants, 32 were randomly assigned tothe cots) group and 32 were
Fandomly assigned to the intervention group, There wee significant differences in knowledge, perclved
fuscepubiity, perceived severity, perceved beneit, perceived barriers, preventive action and HI ts the
intervention group afer recesred the iveweek intervention program and at theeemionth follow-up
2003,
Griginaltyivalue — Dengue hemwrhagie prevention program based on the Health Bali Model was
fictive in lowering HL and improving knowledge, peesved stscetblty, perceived severity, perceived
benefit, perceived buries and preventive acioh hong people in rwal cammniies. The intervention
‘rogram may be beneficial in primary care in sucha rural comm
Commons Attribution (CC BY 40) licence. Anyone may reproduce, distribute, translate and «
Gerivative works of ths article (or bots commercial and noncommercial purposes), subject to f
attribution fo the orginal pablcaion and authors. The ful rms
‘reativecommons ogiicence/by/t Oegalcode
“The authore declared no potential conflicts of interest with respect to the research, authorship
andlor publication ofthis paper. The authors are grateful to Maharat Nakhon Ratchasima Hospital
tnd Health Provineial Osfice for coordinating and supporting data collections, The authors thank all
village bealth volunteers for assistance with data collecting and all staff at Sub-District Health
Promoting Hospital
Introduction
Dengue is a mosquite-borme disease found mainly in countries with tropical and
subtropical climates. The global prevalence of dengue has grown dramatically in recent
decades. Currently, about half of the world’s population is at risk of infection{1], Globally,
one recent estimate indicates 390m dengue infections per year (95 percent credible interval
of 284-528m), of which 96m (67—136m) manifest clinical symptoms{2}. An estimated
500,000 people with severe dengue require hospitalization each year and about 25 percent
of those infected dies(I]
Dengue fever is a disease caused by the dengue virus. The main cause of dengue virus
infection in human is through bites from infected female mosquitoes (Aedes aegypti)
Dengue virus is a carvier disease found in all age groups(3}, The symptoms of dengue
fever include high fever, chils, fatigue, rash, nausea, vomiting, headache, sore throat and
pain (muscle, back, joint and abdomen areas)[d] In severe cases, it can be life threatening
due to serious bleeding and shock{4], The most effective intervention is to prevent
mosquito bites(5}
Thailand is still suffering from dengue fever nationwide and during all seasons.
In 2017, Thailand has reported 52,049 dengue cases from all 77 provinces, including
62 deaths(6). The Ministry of Public Health has adopted a policy to control dengue
hemorrhagic fever in the National Health Development Plan No, 11 (2012-2016) which
targeted the reduction of dengue hemorrhagic fever rate to not more than 25 percent
‘of the median in the past five years and the reduction of morbidity rate to not more than
0.02 percent{7}.
‘The Northeastern region of Thailand has the largest land area. Nakhon Ratchasima
province has the highest population in the Northeast region and the second highest
population in the country, The incidence of dengue hemorrhagic fever in Nakhon
Ratchasima in the past five years (2013-2017) were 269.29, 33.58, 27453, 62.45, 65.38 per
100,000 population, respectively. In 2017, the prevalence of dengue hemorrhagic fever in
Nakhon Ratchasima were 1,716 cases with the morbidity rate of 65:38 per 100,000
population and two cases of death by dengue hemorrhagic fever, giving the mortality rate of
0.08 per 100,000 population(6}. The model forecasting of dengue hemorrhagic fever in 2017
showed that Nakhon Ratchasima was the high-risk area to monitor the disease(8]
It is believed that the outbreak of dengue hemorrhagic fever is mainly from mosquitoes
and by the general nature of mosquitoes, like laying eggs in containers of water inside and
outside the house. This is due to the behaviors of local rural people. Some behaviors that
may not be appropriate include disorganized house, inadequate lighting management.
hanging dirty clothes in the house, not covering water storage container and leaving wet
waste with water, As a result, mosquito breeding becomes widespread®]
Dengue morbidity can be reduced by applying effective communication that can achieve
behavioral outcomes that augment prevention programs{10] At present, the main method to
control or prevent the transmission of dengue virus isto combat vector mosquitoes through
preventing mosquitoes from accessing egg-laying habitats by environmental management
and modification, active monitoring and surveillance of vectors to determine the
effectiveness of control interventions, 10]
‘The Health belief model (HBM), developed from the theory of social psychology.
describes the behavior of individuals{11], The HEM believes that people who change their
behavior must perceive their susceptibility, perceived severity, perceived benefits of
modifying health behaviors and perceived fewer barriers of preventive behaviors, cues to
action, modifying factors and health motivation{11, 12), Therefore, from HBM constructs,
the researcher expected to apply the theory of HEM to use in the prevention of dengue
disease because theory says individuals will eek ways to follow the recommendations for
prevention and rehabilitation as long as the disease prevention practice is more positive
Effectiveness
of the
intervention
program,
353
354
Figure 1
‘Thecretcalfmewore
athe iy
than the difficulty(11), By following these theory instructions, a person aust feel fear for
the disease or feel threatened. In addition, a person must feel to have an ability for disease
prevention(13) Previous studies in Thailand have adopted the HBM to modify dengue
prevention behaviors and received good results(14, 15}, Therefore, this research is based
on the HBM as a theoretical framework for the prevention measures and for designing
intervention activities,
It is necessary to encourage people in the community to receive knowledge about the
disease, promote risk perception and benefits of disease prevention so that people can find
solutions to reduce the barriers to disease prevention then take action to prevent dengue
fever. The dengue hemorrhagic disease prevention in the community must be supported
by the community and apply the campaign for community awareness of the dengue
problem, Previous studies have focused mainly on source reduction of water containers in
a household and vector controlf16-18], These studies earlier did not investigate the
combination of vector control activities, and the behavior changing based on the HBM for
dengue fever prevention, For this study, the researchers are interested in examining the
effects of the dengue hemorrhagic fever prevention intervention program in rural
communities. The data from this study will lead to health promotion planning for dengue
hemorrhagic prevention in rural communities, The focus is on promoting knowledge in
disease prevention, raising awareness of risk and severity of disease, encouraging the
benefits of disease prevention and reducing barriers to disease prevention. The main
objective of the community intervention program is for eradicating dengue hemorrhagic
fever which is a major public health problem in Thailand.
Research objective
‘The purpose of this study is to examine the effectiveness of the intervention program for
dengue hemorrhagic fever prevention among rural communities in Thailand based on the
theory of HBM (Figure 2).
Study design
This is a quasiexperimental study that examined the effect of dengue hemorrhagic fever
‘prevention intervention in rural communities. Participants were randomly divided into two
sue emu Dee re (Keowee of gue beonag fe
teva cteapeit mae eg gl fees i
‘Sitostoet nde fH veosot
(U0) Providing the knowledge of dengue 00 Reser
‘Shona teh €23)Pasna ty
comnany (2.3) Perocived benefits of protection
(24 Pesved bats to proton
(6) Comore fr safety donee ose Bean men eanpistemertacs
(2) Grp eduction (4) House idee (ithe percentage of
sroups as explained below. The experimental group received a five-week intervention Effectiveness
contol group contined fe as Usa. Variables Were measured before the of the
atte the five wek intervention, and at thtee-month followup
intervention
rogram
Sample size Progr:
The sample size was calculated by the following formula(29}
355
yy _ WeawZa)* x08 _20.98-+084? x BAI? _ 5p
a 38)" °
amples percentile vakte (100-(a2) percent under the normal curve set at
005=195 (Wwortaled); 0=020, Z.=084; 4=7;—z;, mean difference of preventive
practice score for dengue fever prevention from previous studied 4] =2.38, o= standard
deviation of mean difference of preventive practice score for dengue fever prevention from
previously studied l4]=3.41
‘The sample size needed for this study was 32 for each group,
Participant inclusion criteria include: atleast 20 years old; Thai nationality; both male
and female; has lived inthe community for more than six months, able to answer questions,
no problem speaking, listening and communicating; no training on educational program for
dengue hemorrhagic fever prevention in the previous six months; willing to participate in
this study; and able to sign the informed consent form.
‘The criteria for exchiding participants from this step are: participants who have
ficulties communicating in Thaf, and participants who are not available at the time of
data collection (Figure 2}
Participants
Two districts were randomly selected irom Nakhon Ratchasima province. Then, two
sub-distriets from two districts were randomly chosen. Further, two villages were randomly
selected from the two sub-distrits to be part of the study. To prevent the contamination of
data, the entire village was randomly assigned as either experimental group or control
group. Individual household from each village is randomly selected to be inchuded in the
study. They were excluded if they had lived in the community less than six months, had
Symptoms or illnesses that limit activity, of had partiipated in any education program for
dengue prevention during the prior six months
Data collection
Participants were randomly divided into two groups (intervention group, n = 33; control
group, n=33). The intervention group was assigned to a five-week program
The control group received the usual health education érom public health personnel
Evaluations by questionnaire were measured three times for both groups. The
questionnaire consisted of 52 questions that took approximately 45min for respondents to
complete. Written consent forms were obtained irom participants prior to data collection
This study was approved by the Committee of Human Ethical Research, Makarat
Hospital, Nakhon Ratchasima,
Research instrument
Part 1: demographic information included seven items on gender, age, marital status,
highest education, occupation, income and information obtained from the community
356
Figure 2
Flow dagram
ofthe stacy
Eseates n= 28)
1 Sesto
{ hocene stnsed arent an 38) Sanit 3)
[eats ewig Teste lonap ge rsros)n=
Disorientation gh esos in Dicartned etrenan ove reer) n=O)
Doan 38)
{Exled ton aes gh eso n= evra ve rents f=)
Part 2: knowledge about dengue hemorrhagic fever included 20 items that assessed
participant's knowledge af the causes of dengue fever, signs and symptoms, treatment aad
prevention. The score of 1 point was given for each correct answer and 0 point for each
‘wrong answer,
Part 3: perception of dengue hemorrhagic fever prevention included 20 items which
derived from four main constructs of HBM: perceived susceptibility, perceived severity,
perceived benefits, and perceived barriers to prevention. Perception measurement utilized a
three-point Likert scale that inchided disagree (1), neither agree nor disagree (2) and agree 3)
Part 4: dengue fever prevention practices were measured using five items derived from.
principle for dengue hemorrhagic fever prevention practices from the Department of
Disease Control, Ministry of Public Health, Thailand|20),
Intervention
Participants in the control group did not receive any interventions. Participants
jn the experimental group were enrolled in the intervention program based on
the HBM theory. The HBM has four constructs representing the perceived threat and net
benefits: perceived susceptibility, perceived severity, perceived benefits and perceived
barries[12). The specific intervention program included four main activities based on
HBM theory.
Activity 1: providing knowledge of dengue hemorrhagic fever
Implementation timeframe: Weeks 1-5,
“The objective of tis activity was to provide the knowledge of dengue hemorrhagic fever
through the daily community broadcast. The messages were based on HBM constructs as
described below:
(1) Raise the perceived susceptibility: “dengue is @ problem in com
‘eroup.”
2) Raise the perceived severity: “it is alittle one but itis the one that can kill you.”
nity for all age
Raise the perceived benelits: “take care of the house environment, then the safe
environment will protect your family from dengue hemorrhagic fever
(1) Reduce the perceived barriers: ust few minutes for easy clean-up can reduce many
risks from dengue
Activity 2: dengue hemorrhagic fever campaign
Implementation timeframe: Week 2.
"The emphasis is on individuals to receive information through campaign activities:
(0), The individuals who took part in the campaign consisted of the head ofthe village,
assistant head of the village, vlage health volunteer, adults in the village and
students in the village. Mosquito mascot and cartoons were also part of the
campaign parade
2) Poster boards were used during campaign parade to raise awareness of
dengue hemorthagic fever such as principle for dengue hemorthagic fever
prevention practices fom the Department of Disease Cantsol20] and mosquito
life eye
@) Campaign announcements about practices to eradicate larvae using temephos or
abate sand and using mosquito repel
#)_ Distribution of leaflet and messages on dengue hemorrhagic fever, such as signs and
‘symptoms of dengue hemorrhagic fever.
(6) All participants in the parade campaign went to all the houses in the village to
identify mosquito breeding sites. If an open water container was found, the
participants removed all the water étom it,
Activity 3: a contest for safety dengue house
Implementation timeframe: Weeks 3-1 and announcement of the winner during Week 5.
‘The objective ofthis activity was to find a model house that is safe from dengue and to
encourage villagers to see the importance of environmental management and create good
examples for their neighbors:
(1) Defined the attributes of the house that is safe from dengue on the basis of the
hygienic and clean house assessment from the Department of Disease Control,
‘Thailand|20] then selected major topics in the assessment, An award-winning house
thas to show the important features ofall attributes.
@) Assigned the committee to evaluate the houses that participate in community
Contest. The committee consisted of seven representatives of the community,
Effectiveness
of the
intervention
program,
357
358
including the village head (one), the assistant village heads (two) and village health
‘volunteers (four)
(Public announcement
the rules of the contest.
ecruit people in the community tothe contest and to inform
valuation process,
(©) The announcement of the award for the winner and the second place during the
‘group activity atthe village hal
(©) The winners received a large catifcate to display at the front oftheir houses to be
examples to neighbors and motivate them to be safe from dengue.
Activity 4: group education
Implementation timeframe: Week 5,
“The objective ofthis activity was to provide knowledge about dengue hemorrhagic fever.
Activity was set in the comunity hall with the following activities:
(2) knowledge exhibition about dengue, mosquito's repellent and methods for
exadicating mosquitos; and
(@) stage play and role play that reflected the susceptibility for risks, the dengue
severity, the benefits of prevention, and reduction in barriers to prevent dengue
hemorthagic fever.
Validity and reliability of research instruments
The intervention program and research instrument were adapted from the literature
review based on the HBM theory and were reviewed by experts inthe field, Content validity:
a panel of three experts evaluated the content validity of the intervention program and
research instrument. For content validity testing, CVI was analyzed and found to be 029.
Reliabilty: the questionnaire was tested for reliability with 30 people with similar
characteristics to the samples, For internal consistency reliability testing, Cronbach's a
coefficient was analyzed. All scales had good levels of internal consistency of more
than 0.70,
Data analyses
Statistical Packet for the Social Sciences 23.0 was used for data analyses. Descriptive
statistics were calculated to describe demographic characteristics and other backgrounds of
the participants. To compare the data between the two groups, /-test and 7” test were used,
Two-way repeated measures ANOVA was used to analyze the difference in the total scores
of six scales for dengue hemorrhagic fever prevention between the two groups actoss times
of measure. The 7 test was used for analyzing the difference in the number of house index
GD between the two groups,
Results
A total of 64 of the initial 66 participants completed the study questionnaires
at three timeframes, Thus, data analyses were performed using 64 subjects, At baseline,
there were no significant differences in general characteristics between the intervention
group and control group. However, there was a significant difference in gender
(see Table Dy
Effectiveness
Intervention gop n= 32) Coto group (»=32) 2
Demographic data Nunber Percent Number Percent ort _pevalue of the
‘Gnd intervention
Male 2 63 cry 0.005 program
Female a ss 5
Age ear) gnean:t SD) conn 118t Liss os 359
Mania status
Since 1 a1 o 00 0003
Mortiea B no as
Widowed 7 no a1
Diver i 3 a1
Tight education
Primary sca 2 a3 ms 206 0518
Dh schal 4 25 3 °4
igh 2 33 Q 90
xcpation
Famer a eas mo ws
Tracer 3 3 4s
ied 2 a3 3 94
Official 0 00 1 31 co Rie
Fosse work 3 o4 ‘ 25. evan
Other 4 ns 0 00 seneral characterise
Income sse2s0.2 627882 02s.26sa588 oxo ommy age eteeentn
Note: *p<005 ‘bate
‘Table Il showed HI decreased in both groups at the end of the intervention program and
revealed a significant difference between groups for both the post-intervention and the
follow-up.
Comparison of the groups before starting intervention revealed no significant difference
in the scores of knowledge, perceived susceptibility, perceived severity, perceived benefits
perceived barriers and preventive action (see Table I.
‘The intervention group had increases in the scores of knowledge, perceived
susceptibility, perceived severity, perceived benefits, perceived barriers and preventive
action aiter mtervention. Only preventive action showed the interaction between group and
time (F=11.19, p-value < 0.001) (Table IV),
Discussion
A quasiexperimental study was designed to assess the effectiveness of the
intervention program based on HBM to prevent dengue hemorrhagic fever
Intervention group (v=32)—_Contol group (x= 32) use idee
Measuring tine Found arvae(n) Found larvae (o) ih (percentage of
houses infested it
Preinterventon 2 3750 uw 0058 larvae andlor pupae
Pestintervention ° ° 0 1185 Betiveeninlervetion
Followssp 6 ° 2 14769 ‘snd conta groups
360
‘Table HL.
Comparison of study
‘arabes between
rope at aselne
Results demonstrated that this intervention program significantly increased the
knowledge, perceived susceptibility, perceived severity, perceived benefits,
perceived barriers and preventive action. This finding supported the assumption that
applying the HBM to the intervention in rural communities can promote the preventive
actions and may be beneficial in the primary care of people with a high risk of dengue
hemorrhagic fever
The intervention program was created to meet the HBM theory because
protective behavior is related to the knowledge, perceived susceptibility, perceived
severity, perceived benefits and perceived barriers. Although education campaigns have
increased people's awareness of dengue, it remains unclear to what extent this knowledge
js put into practice, and to what extent this practice actually reduces mosquito
‘populations. In this study, the intervention encouraged the practice of participants in
many ways. The knowledge was provided via daily broadcast to the community, dengue
campaign and group education atthe village hall Cues-to-action was implemented via the
contest for a model house for safety from dengue, which was in line with an earlier
research suggestion(13] that there is a greater likelihood of positive outcomes for
preventive actions when the participants are supported and encouraged by the good
‘model in the community.
‘After the intervention program, the total scores on the six scales for dengue hemorrhagic
{ever prevention were significantly higher in the intervention group than those inthe control
group. These results support the effectiveness of the intervention program direct
However, in the follow-up phase, some scores were decreased; this may be because the
community engagement tends to be insufficient, Thus, the approach toward enkancing
community involvement is important.
‘The results of this study showed that the HI for the intervention group deczeased for
‘both postintervention and follow-up. The effectiveness ofthe program on preventive action
is consistent with the earlier studied that showed the direct link between knowledge of
dengue preventive measures and container protection practice{21] In order to decrease the
brooding site of mosquitoes, itis necessary for people in the community to change the
behaviors for the dengue hemorrhagic fever prevention,
Conclusions
Dengue hemorrhagic fever is pervasive among rural communities, In the present study,
We conducted a quasiexperimental study to investigate the effectiveness of the
intervention program. The effects were measured by the knowledge, perceived
susceptibility, perceived severity, perceived benefits, perceived barriers and preventive
action. After participation in the intervention program, the five scales showed a
significant increase; therefore, the intervention program may be beneficial in primary care
in such a rural community
Variables ezvention group X SD) Contzol group F
Knowledge 1528 223 ust gs) ox
Perceived susceptity 1328 (119 1316 014) 0433
Perceived seventy 1216 (125) 9564
Peteived benefit 1347 (105 030
Perceived barrie 14.09 (093)
Preventive action 441 078) O78
Note: n=64
000) srtt
ao00>) 9899
ves
ier
at
$288 BOEPERGES
g 55 Peal
SB 2 ESE
a oad
Spoon
pe aang
ero eco (eaco) 2x (a0) TE 0) FFE sug passag
(S50) 0ceT SRO GEST
Geo 980 asta) zet soar crDoorr cone sugag pasameg
(eoeter Us Hest we
Gio sro (e100) sav io) ese oyna Suias posrg
(e50) seer sin
‘osyo) ovo 100 «zor (SoU iret ones yadooms passing
(se 6st 09
wea art ta9>) ze 60) zzt some spatnonsy
wea mo aA
yx dno ma, nog
362
References
1, World Heath Organization [WHO] Dengue and severe dent D1). (update 2017 Apr: ce
2018 Mar 24}. Avaiable for: worw.who ntimedicrntefiacts bets lead
2 Bhat S,Gething PW, Brady 0) Masia JP, Baio AM, Moyes CL, Drake JM, Brownstein JS
Hoen AG, Sak 0, Myers ME, George DB, nich , Wiliam Wint GR Simons CP, Seat FW.
Fara J) Hay SL The gba dsbution ad burden of dengue Nate 2013 Ape 25496 (445)
5067, di 102088nattze12060
3. Guerdan BR. Dengue feverengue hemor fver, A.J Me 2010 Spring: 72 513
4. Singh, Kssoon N, Bansal A Dengue and dengue hema fever management ise in an
inensve cate it de Pediat, 207 €80)2235
5. Ballenge-Browning KK & Elder JP. Mulismodel Aedes aegypti mnsqito ection interventions
and dengue fever prevention. Trp Med lt Heakh. 208, 1403) 19421591
6 Department of Disease Control Ministry of Pubic Healt, Thailand. Dengue hemorrhagic fever
report 2017 (2017) update: 2018 Jan ted 2018 Max 2 Available ems www tad org
Stoiesiiew 2804
7 Ministry of Public Health, Thailand. Guideline fr surveilance prevention and contol of dengue
ee: 2077 pated 2016 Ju 23 ced 208 Mar 4} Avalable Su pry have nto
Stele PDF Afi uDengeDengue 2033158" 204 Fan fo. 201}pd¢
8 Department of Disease Cottol, Ministry of ble Healt, Thad. The model forecasting of
dengue heorragi ever in 20472017 {spdatd: 2017 ced 2018 Mar 2) Avaliable rr wir
Uhavidergivupladsfielle PDF Dengue 2bldengue forecast 60 pa
9. Samuel PP, Thenmoshi V. Nagar] Dilp Kumar, Tyagi BK Dengue vectors prevalence andthe
rented sk frtors involved the transmission of dengue i Thiwvanesthapwrars ditt,
Kerb, Soth Inia, Vector Bore Dis 20% 31 3138
10, World Heath Organization (WTIO], Global strategy for dengue prevention and contol
Worl Heats Orgatization, WHO Press, Geneva: 2012
1, Strether V]Rosetock IM, The health ef model In: Glnz , Lewis FM, Rimes BK editors
leah behavior ad helt education: her, research and rece, 2nd ed San Frencisen, Ch
dossey Bas, 1997 1158
12, Rosenstock I Historie ois ofthe heath bef mode, Health Bae Monoge. 1974 2
33,
18, Lennon JL. The use ofthe Heats Ble model in dengue health edcation, Dengue Bulletin. 2005;
p78
1, Auttapoom K,Ratenasuwan W, Suizarat D, Tayamonglgel M. The etctveness ofthe
health beet ode aad the particpatio ofthe conemunty i controling most larvae
Khuramuang Dt, Kalass Province, Proceeding of 1th Naesuan Research Conteence o a
21-22, 216, Narestan Univers, Pisano Province,
15, Saengkae H. The elect of health edsaton program for prevention and contra of, dengue
emer fever infamy coe leaders, Maangpha Sbtiste, Aranyaprathel Dis, Srakaeo
Prosnce. PRR) 2015, 100) 6581
16, Phuanukoonnon $, Mueler J Bryan JL. Btetveness of dengue contol practices in household
vate containers in Nortbeast Thane, TM eI, 205; 108) 75.68
17, Chaooiatana A, Chanruang S, PotbaledP. A comparison of dengue hemorrhagic fever contol
interventions in northeaser Thailand. Southeast Asian J Top Med Public Healt, 2008, 35)
erat
18, Ballenger Browning KK Elder JP Multimode] Andes aegyt mosqito reduction interventions and
denge ever prevention TM & IH. 2008, 1402 154281
19, Polit DE, Hungler BP, Nursing Research: Principles and methods. Sof, Philadephia, OA
Lappinot 1987
20, Department af Disease Control, Ministry of Public Health, Thailand. Manual for guiding cognizant
of diseases and healt hazards for the pubic people. The Bureau of Risk Communication and
Behavioral Health Development. Ist ed The Agricultural Federative Coaperation of Thailand
Limite, Bangkok, 2013: 20-25,
21, Koentaadt CIM, Tuiten W, Sihiprasasna R Kijchalao U, Jones JW, Scot TW. Dengue knowledge
and practies and their impact on Aedes aegypti populations in Kamphaeng Phe, Thailand. An J
‘Trop. Med. Hyg. 2006, 744) 692.700,
Corresponding author
Suda Hanklang can be contacted at: en101_987654@hotmailcom
For instructions on bow to order reprints of this article please visi our webs
‘www.emeraldgrouppublishing comflicensing/reprints htm
Or contact us fr further details: permissions @emeraldinsight.com
Effectiveness
of the
intervention
program,
363
The Joanna Briggs Institute Critical Appraisal tools
for use in JBI Systematic Reviews.
Checklist for
Quasi-Experimental Studies
(non-randomized experimental studies)
http://joannabriggs.org/research/critical-appraisal-tools.html
www.joannabriggs.org
>
JBI Critical Appraisal Checklist for Quasi-Experimental Studies
(non-randomized experimental studies)
Reviewer. _Date__
Author Year _Record Number.
Yes No Unclear Not
applicable
1, sit clear in the study what is the ‘cause’ and what is the ‘effect’
(ie, there is no confusion about which variable comes first)?
oO
2. Were the participants included in any comparisons similar?
3, Were the participants included in any comparisons receiving
similar treatment/care, other than the exposure or intervention
of interest?
4, Was there a control group?
5. Were there multiple measurements of the outcome both pre
‘and post the intervention/exposure?
6. Was follow up complete and if not, were differences between
groups in terms of their follow up adequately described and
analyzed?
7. Were the outcomes of participants included in any comparisons
‘measured in the same way?
8. Were outcomes measured in a reliable way?
OOo0dcOdUvOdUmdondlmUmcde hc
Oo00dUdmUCUODWUOUUODUcUODlUco lm
OoOoddcvUuodmUmUDUcUlUmce lo
OocU0ndoUdmUODUcUOUUDODULcUDlhUmO
9, Was appropriate statistical analysis used?
Overall appraisal include LC] txctude C1 seek further info C1
Comments (Including reason for exclusion)
© Joanna Briggs Institute 2017 Critical Appraisal Checklist | 3
for Quasi-Experimental Studies
sS-
Explanation for the critical appraisal tool for Quasi-Experimental Studies
(experimental studies without random allocation)
How to cite: Tufanaru C, Munn 2, Aromataris E, Campbell J, Hopp L. Chapter 3: Systematic reviews of
effectiveness. In: Aromataris E, Munn Z (Editors). Joanna Briggs Institute Reviewer's Manual. The Joanna
Briggs Institute, 2017. Available from https://reviewersmanual.joannabriges.or
Critical Appraisal Tool for Quasi-Experimental Studies
{experimental studies without random allocation)
Answers: Yes, No, Unclear or Not Applicable
1, Isit clear in the study what is the ‘cause’ and what is the ‘effect’ (i.e. there is no confusion
about which variable comes first)?
‘Ambiguity with regards to the temporal relationship of variables constitutes a threat to the
internal validity of a study exploring causal relationships. The ‘cause’ (the independent variable,
thattis, the treatment or intervention of interest) should occur in time before the explored ‘effect’
(the dependent variable, which is the effect or outcome of interest). Check if it is clear which
variable is manipulated as a potential cause. Check if itis clear which variable is measured as the
effect of the potential cause. Is it clear that the ‘cause’ was manipulated before the occurrence
of the ‘effect’?
2. Were the participants included in any comparisons similar?
The differences between participants included in compared groups constitute a threat to the
internal validity of a study exploring causal relationships. If there are differences between
participants included in compared groups there is a risk of selection bias. If there are differences
between participants included in the compared groups maybe the ‘effect’ cannot be attributed
to the potential ‘cause’, as maybe it is plausible that the ‘effect’ may be explained by the
differences between participants, that is, by selection bias. Check the characteristics reported for
participants. Are the participants from the compared groups similar with regards to the
characteristics that may explain the effect even in the absence of the ‘cause’, for example, age,
severity of the disease, stage of the disease, co-existing conditions and so on? [NOTE: In one
single group pre-test/post-test studies where the patients are the same (the same one group) in
any pre-post comparisons, the answer to this question should be ‘yes.]
3. Were the participants included in any comparisons receiving similar treatment/care, other
n of interest?
than the exposure or interven
In order to attribute the ‘effect’ to the ‘cause’ (the exposure or intervention of interest),
assuming that there is no selection bias, there should be no other difference between the groups
in terms of treatments or care received, other than the manipulated ‘cause’ (the intervention of
© Joanna Briggs Institute 2017 Critical Appraisal Checklist | 4
for Quasi-Experimental Studies
>
interest). If there are other exposures or treatments occurring in the same time with the ‘cause’,
other than the intervention of interest, then potentially the ‘effect’ cannot be attributed to the
intervention of interest, as it is plausible that the ‘effect’ may be explained by other exposures
or treatments, other than the intervention of interest, occurring in the same time with the
intervention of interest. Check the reported exposures or interventions received by the
compared groups. Are there other exposures or treatments occurring in the same time with the
intervention of interest? Is it plausible that the ‘effect’ may be explained by other exposures or
treatments occurring in the same time with the intervention of interest?
4, Was there a control group?
Control groups offer the conditions to explore what would have happened with groups exposed
to other different treatments, other than to the potential ‘cause’ (the intervention of interest).
The comparison of the treated group (the group exposed to the examined ‘cause’, that is, the
group receiving the intervention of interest) with such other groups strengthens the examination
of the causal plausibility. The validity of causal inferences is strengthened in studies with at least
one independent control group compared to studies without an independent control group.
Check if there are independent, separate groups, used as control groups in the study. (Note: The
control group should be an independent, separate control group, not the pre-test group ina single
group pre-test post-test design.]
5. Were there multiple measurements of the outcome both pre and post the
intervention/exposure?
In order to show that there is a change in the outcome (the ‘effect’) as a result of the
intervention/treatment (the ‘cause’) it is necessary to compare the results of measurement
before and after the intervention/treatment. If there is no measurement before the treatment
and only measurement after the treatment is available it is not known if there is a change after
the treatment compared to before the treatment. If multiple measurements are collected before
the intervention/treatment is implemented then it is possible to explore the plausibility of
alternative explanations other than the proposed ‘cause’ (the intervention of interest) for the
observed ‘effect’, such as the naturally occurring changes in the absence of the ‘cause’, and
changes of high (or low) scores towards less extreme values even in the absence of the ‘cause’
(sometimes called regression to the mean). If multiple measurements are collected after the
intervention/treatment is implemented it is possible to explore the changes of the ‘effect’ in time
in each group and to compare these changes across the groups. Check if measurements were
collected before the intervention of interest was implemented. Were there multiple pre-test
measurements? Check if measurements were collected after the intervention of interest was
implemented. Were there multiple post-test measurements?
© Joanna Briggs Institute 2017 Critical Appraisal Checklist | 5
for Quasi-Experimental Studies
>
6. Was follow up complete and if not, were differences between groups in terms of their follow
up adequately described and analyzed?
If there are differences with regards to the loss to follow up between the compared groups these
differences represent a threat to the internal validity of a study exploring causal effects as these
differences may provide a plausible alternative explanation for the observed ‘effect’ even in the
absence of the ‘cause’ (the treatment or exposure of interest). Check if there were differences
with regards to the loss to follow up between the compared groups. If follow up was incomplete
(that is, there is incomplete information on all participants), examine the reported details about
the strategies used in order to address incomplete follow up, such as descriptions of loss to follow
up (absolute numbers; proportions; reasons for loss to follow up; patterns of loss to follow up)
and impact analyses (the analyses of the impact of loss to follow up on results). Was there a
description of the incomplete follow up (number of participants and the specific reasons for loss
to follow up)? If there are differences between groups with regards to the loss to follow up, was
there an analysis of patterns of loss to follow up? If there are differences between the groups
with regards to the loss to follow up, was there an analysis of the impact of the loss to follow up
on the results?
7. Were the outcomes of participants included in any comparisons measured in the same way?
If the outcome (the ‘effect’) is not measured in the same way in the compared groups there is a
threat to the internal validity of a study exploring a causal relationship as the differences in
‘outcome measurements may be confused with an effect of the treatment or intervention of
interest (the ‘cause’). Check if the outcomes were measured in the same way. Same instrument
or scale used? Same measurement timing? Same measurement procedures and instructions?
8, Were outcomes measured in a reliable way?
Unreliability of outcome measurements is one threat that weakens the validity of inferences
about the statistical relationship between the ‘cause’ and the ‘effect’ estimated in a study
exploring causal effects. Unreliability of outcome measurements is one of different plausible
explanations for errors of statistical inference with regards to the existence and the magnitude
of the effect determined by the treatment (‘cause’). Check the details about the reliability of
measurement such as the number of raters, training of raters, the intra-rater reliability, and the
inter-raters reliability within the study (not to external sources). This question is about the
reliability of the measurement performed in the study, it is not about the validity of the
measurement instruments/scales used in the study. (Note: Two other important threats that
weaken the validity of inferences about the statistical relationship between the ‘cause’ and the
‘effect’ ore low statistical power and the violation of the assumptions of statistical tests. These
other threats are not explored within Question 8, these are explored within Question 9.]
© Joanna Briggs Institute 2017 Critical Appraisal Checklist | 6
for Quasi-Experimental Studies
>
9. Was appropriate statistical analysis used?
Inappropriate statistical analysis may cause errors of statistical inference with regards to the
existence and the magnitude of the effect determined by the treatment (‘cause’). Low statistical
power and the violation of the assumptions of statistical tests are two important threats that
weakens the validity of inferences about the st
‘effect’. Check the following aspec
ical relationship between the ‘cause’ and the
if the assumptions of statistical tests were respected; if
appropriate statistical power analysis was performed; if appropriate effect sizes were used; if
appropriate statistical procedures or methods were used given the number and type of
dependent and independent variables, the number of study groups, the nature of the
relationship between the groups (independent or dependent groups), and the objectives of
statistical analysis (association between variables; prediction; survival analysis etc.)
© Joanna Briggs Institute 2017 Critical Appraisal Checklist | 7
for Quasi-Experimental Studies
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pedoman Internal Ispa KlabangDocument15 pagesPedoman Internal Ispa Klabangdievara.deddy50% (2)
- Rumah Dan LingkunganDocument6 pagesRumah Dan Lingkungandila laila nafisaNo ratings yet
- Bab Ii-1Document27 pagesBab Ii-1dila laila nafisaNo ratings yet
- Kesehatan Ibu Dan AnakDocument6 pagesKesehatan Ibu Dan Anakdila laila nafisaNo ratings yet
- Bab I-1Document3 pagesBab I-1dila laila nafisaNo ratings yet
- Bab IiDocument28 pagesBab Iidila laila nafisaNo ratings yet
- Lembar 1Document1 pageLembar 1dila laila nafisaNo ratings yet
- Bab IDocument6 pagesBab Idila laila nafisaNo ratings yet
- Surat Peminjaman LabDocument1 pageSurat Peminjaman Labdila laila nafisaNo ratings yet
- KESWADocument12 pagesKESWAdila laila nafisaNo ratings yet
- BAB II Pake p2pDocument15 pagesBAB II Pake p2pdila laila nafisaNo ratings yet
- Daftar PustakaDocument1 pageDaftar Pustakadila laila nafisaNo ratings yet
- Bab IDocument6 pagesBab Idila laila nafisaNo ratings yet
- Kata Pengantar, Daftar Isi, Daftar Tabel, Daftar Singkatan, LampiranDocument9 pagesKata Pengantar, Daftar Isi, Daftar Tabel, Daftar Singkatan, Lampirandila laila nafisaNo ratings yet
- Ijo 04 05 508Document5 pagesIjo 04 05 508dila laila nafisaNo ratings yet
- TBC Dapat Dicegah Penularannya !Document10 pagesTBC Dapat Dicegah Penularannya !dila laila nafisaNo ratings yet
- Occupational Sunlight Exposure, Polymorphism of Glutathione S-Transferase M1, and Senile Cataract RiskDocument2 pagesOccupational Sunlight Exposure, Polymorphism of Glutathione S-Transferase M1, and Senile Cataract Riskdila laila nafisaNo ratings yet
- Kata Pengantar KesproDocument2 pagesKata Pengantar Kesprodila laila nafisaNo ratings yet
- Lembar Kegiatan Harian BaruDocument4 pagesLembar Kegiatan Harian Barudila laila nafisaNo ratings yet
- Jurnal Translate2Document12 pagesJurnal Translate2dila laila nafisaNo ratings yet
- Ijmsv 01 P 0165Document5 pagesIjmsv 01 P 0165dila laila nafisaNo ratings yet
- Ukk CampakamulyaDocument18 pagesUkk Campakamulyadila laila nafisaNo ratings yet
- Laporan Baru EpidlapDocument24 pagesLaporan Baru Epidlapdila laila nafisaNo ratings yet
- p2bb Zoonosis Desember 2022Document4 pagesp2bb Zoonosis Desember 2022dila laila nafisaNo ratings yet
- Katarak Merupakan Penyebab Sedikitnya 50 Salinan SalinanDocument41 pagesKatarak Merupakan Penyebab Sedikitnya 50 Salinan Salinandila laila nafisaNo ratings yet
- Program TB JuliDocument4 pagesProgram TB Julidila laila nafisaNo ratings yet
- Perkesmas Juni 2022Document5 pagesPerkesmas Juni 2022dila laila nafisaNo ratings yet
- Kesja September 2022Document6 pagesKesja September 2022dila laila nafisaNo ratings yet
- SKDR NaringgulDocument2 pagesSKDR Naringguldila laila nafisaNo ratings yet
- Kesehatan Indra Bulan JUNIDocument4 pagesKesehatan Indra Bulan JUNIdila laila nafisaNo ratings yet