Professional Documents
Culture Documents
Antipsikotik Vs Behaviour Therapy Pada Pasien Psikotik
Uploaded by
Dewi NofiantiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antipsikotik Vs Behaviour Therapy Pada Pasien Psikotik
Uploaded by
Dewi NofiantiCopyright:
Available Formats
Articles
Antipsychotic drugs versus cognitive behavioural therapy
versus a combination of both in people with psychosis:
a randomised controlled pilot and feasibility study
Anthony P Morrison, Heather Law, Lucy Carter, Rachel Sellers, Richard Emsley, Melissa Pyle, Paul French, David Shiers, Alison R Yung,
Elizabeth K Murphy, Natasha Holden, Ann Steele, Samantha E Bowe, Jasper Palmier-Claus, Victoria Brooks, Rory Byrne, Linda Davies,
Peter M Haddad
Summary
Background Little evidence is available for head-to-head comparisons of psychosocial interventions and pharmacological Lancet Psychiatry 2018
interventions in psychosis. We aimed to establish whether a randomised controlled trial of cognitive behavioural Published Online
therapy (CBT) versus antipsychotic drugs versus a combination of both would be feasible in people with psychosis. March 28, 2018
http://dx.doi.org/10.1016/
S2215-0366(18)30096-8
Methods We did a single-site, single-blind pilot randomised controlled trial in people with psychosis who used services
See Online/Comment
in National Health Service trusts across Greater Manchester, UK. Eligible participants were aged 16 years or older; http://dx.doi.org/10.1016/
met ICD-10 criteria for schizophrenia, schizoaffective disorder, or delusional disorder, or met the entry criteria for an S2215-0366(18)30123-8
early intervention for psychosis service; were in contact with mental health services, under the care of a consultant Division of Psychology and
psychiatrist; scored at least 4 on delusions or hallucinations items, or at least 5 on suspiciousness, persecution, or Mental Health
grandiosity items on the Positive and Negative Syndrome Scale (PANSS); had capacity to consent; and were help- (Prof A P Morrison ClinPsyD,
H Law PhD, L Carter PhD,
seeking. Participants were assigned (1:1:1) to antipsychotics, CBT, or antipsychotics plus CBT. Randomisation was R Sellers PhD, M Pyle PhD,
done via a secure web-based randomisation system (Sealed Envelope), with randomised permuted blocks of 4 and 6, Prof P French PhD,
stratified by gender and first episode status. CBT incorporated up to 26 sessions over 6 months plus up to four booster D Shiers MBChB,
sessions. Choice and dose of antipsychotic were at the discretion of the treating consultant. Participants were followed Prof A R Yung PhD,
J Palmier-Claus PhD, R Byrne PhD,
up for 1 year. The primary outcome was feasibility (ie, data about recruitment, retention, and acceptability), and the Prof P M Haddad MD), Division
primary efficacy outcome was the PANSS total score (assessed at baseline, 6, 12, 24, and 52 weeks). Non-neurological of Population Health, Health
side-effects were assessed systemically with the Antipsychotic Non-neurological Side Effects Rating Scale. Primary Services Research and Primary
analyses were done by intention to treat; safety analyses were done on an as-treated basis. The study was prospectively Care (Prof R Emsley PhD,
Prof L Davies PhD), and
registered with ISRCTN, number ISRCTN06022197. Manchester Academic Health
Science Centre Clinical Trials
Findings Of 138 patients referred to the study, 75 were recruited and randomly assigned—26 to CBT, 24 to Unit (Prof R Emsley), University
of Manchester, Manchester
antipsychotics, and 25 to antipsychotics plus CBT. Attrition was low, and retention high, with only four withdrawals
Academic Health Science
across all groups. 40 (78%) of 51 participants allocated to CBT attended six or more sessions. Of the 49 participants Centre, Manchester, UK; and
randomised to antipsychotics, 11 (22%) were not prescribed a regular antipsychotic. Median duration of total Greater Manchester Mental
antipsychotic treatment was 44·5 weeks (IQR 26–51). PANSS total score was significantly reduced in the combined Health NHS Foundation Trust,
Manchester, UK
intervention group compared with the CBT group (–5·65 [95% CI –10·37 to –0·93]; p=0·019). PANSS total scores did
(Prof A P Morrison, H Law,
not differ significantly between the combined group and the antipsychotics group (–4·52 [95% CI –9·30 to 0·26]; L Carter, R Sellers, M Pyle,
p=0·064) or between the antipsychotics and CBT groups (–1·13 [95% CI –5·81 to 3·55]; p=0·637). Significantly fewer P French, D Shiers, Prof A R Yung,
side-effects, as measured with the Antipsychotic Non-neurological Side Effects Rating Scale, were noted in the CBT E K Murphy ClinPsyD,
N Holden DClinPsy, A Steele PhD,
group than in the antipsychotics (3·22 [95% CI 0·58 to 5·87]; p=0·017) or antipsychotics plus CBT (3·99 [95% CI
S E Bowe DClinPsy,
1·36 to 6·64]; p=0·003) groups. Only one serious adverse event was thought to be related to the trial (an overdose of J Palmier-Claus, V Brooks RMN,
three paracetamol tablets in the CBT group). R Byrne, Prof P M Haddad)
Correspondence to:
Interpretation A head-to-head clinical trial of CBT versus antipsychotics versus the combination of the two is feasible Dr Tony Morrison, Psychosis
Research Unit, Greater
and safe in people with first-episode psychosis.
Manchester Mental Health NHS
Foundation Trust, Manchester,
Funding National Institute for Health Research. M25 3BL, UK
tony.morrison@gmmh.nhs.uk
Copyright © 2018 Elsevier Ltd. All rights reserved.
Introduction or other psychoses.1 Many clinical guidelines, therefore,
Schizophrenia and psychosis are associated with sub suggest that people with psychosis should be offered
stantial personal, social, and economic costs. High- both antipsychotics and CBT (as well as family
quality evidence from clinical trials shows that both interventions) and should be involved in collaborative
antipsychotics and cognitive behavioural (CBT) therapy decisions about treatment options.1 However, neither
can be helpful to adults with diagnoses of schizophrenia antipsychotics nor CBT are effective for everyone, and
www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8 1
Articles
Research in context
Evidence before this study randomly assigned to psychological treatment or
We searched PubMed with the terms “schizophrenia”, pharmacological treatment, or both, is possible. Our findings
“psychosis”, “psychological therapy”, “psychosocial suggest that antipsychotics, CBT, and the combination of the
intervention”, “CBT”, “antipsychotic” and “neuroleptic” for two are acceptable, safe, and helpful treatments for people
articles published in any language up to Jan 30, 2018. with early psychosis, but could have different cost–benefit
Although several systematic reviews and meta-analyses have profiles.
shown robust evidence that antipsychotics are superior to
Implications of all the available evidence
placebo and that cognitive behavioural therapy (CBT) for
Our preliminary findings seem consistent with guidelines
psychosis in addition to antipsychotics is superior to
that recommend informed choices and shared decision
treatment as usual, we identified no randomised controlled
making about treatment options for early psychosis on the
trials in which a head-to-head comparison of CBT and
basis of cost–benefit profiles. An adequately powered efficacy
antipsychotics was done. A 2012 Cochrane review concluded
and effectiveness trial is now needed to test hypotheses
that no usable data were available to establish the relative
about superiority (eg, antipsychotics plus CBT vs
efficacy of antipsychotic medication and psychosocial
antipsychotics alone or CBT alone) and non-inferiority
interventions in early episode psychosis.
(eg, antipsychotics vs CBT).
Added value of this study
Our pilot and feasibility trial showed that a methodologically
rigorous clinical trial in which participants with psychosis are
the individual cost–benefit ratios of such treatments concern, in view of the increased cardiovascular mortality
(ie, the balance between efficacy and adverse effects) vary in people with psychosis compared with the general
substantially, both between and within individuals. population.10 Adverse effects of CBT in psychosis have
Meta-analyses2–4 of randomised controlled trials of CBT, not been well studied.2 Potential side-effects, such as
added to antipsychotics, for psychosis have shown effect stigma and deterioration of mental state,11 were not
sizes for both total symptoms and positive symptoms in detected in clinical trials of CBT for people with psychotic
the small-to-moderate range (generally 0·3–0·4 relative to experiences. Rather, CBT resulted in significant
treatment as usual, although the effect size is smaller reductions in the frequency of these side-effects.12,13
when lower quality trials are excluded). Meta-analyses5,6 of However, CBT delivered in the context of a poor
antipsychotics compared with placebo also show therapeutic relationship could be harmful.14
moderate benefits in terms of total and positive Whereas most evidence for the efficacy of CBT for
symptoms. The most comprehensive meta-analysis7 in psychosis is from randomised controlled trials in which
chronic schizophrenia showed a standardised effect size CBT was provided as an adjunct to antipsychotics
for total symptoms of 0·47 (95% CI 0·42–0·51). Although (ie, a combination of both vs antipsychotics alone),
CBT and antipsychotics are better than comparators preliminary evidence suggests that CBT might be helpful
(treatment as usual and placebo, respectively), the for people with psychosis who are not taking anti
proportion of individuals who achieve a clinically psychotics.13 No data for the relative head-to-head efficacy
meaningful benefit is moderate. For example, a meta- or acceptability of CBT and antipsychotics in schizo
analysis7 showed that 51% of multi-episode patients had phrenia are available. We investigated the feasibility of
at least a minimal response (≥20% reduction in symptoms doing a three-group randomised controlled trial of CBT,
as measured on the Positive and Negative Syndrome antipsychotics, and a combination of CBT and anti
Scale [PANSS] or Brief Psychiatric Rating Scale), and psychotics in people with psychosis.
23% had a good response (≥50% reduction in symptoms),
to antipsychotics. By comparison, in first-episode Methods
psychosis, 81% of patients had at least a minimal Study design and participants
response, and 52% had a good response, to antipsychotics.8 We did a single-blind, randomised, controlled pragmatic
The authors of a meta-analysis2 claim that conclusions pilot and feasibility trial between April 1, 2014, and
about the efficacy of CBT have been exaggerated, given June 30, 2017 in four specialist mental health National
that most large, robust trials have not shown significant Health Service trusts in Greater Manchester, UK. Eligible
effects at end of treatment, and that effect sizes are participants were aged 16 years or older; met ICD-10
reduced overall if only studies of high quality are included criteria for schizophrenia, schizoaffective disorder, or
in meta-analyses. delusional disorder, or met the entry criteria for an
Antipsychotics are associated with a wide range of early intervention for psychosis service (operationally
adverse effects.5,9 Metabolic effects are of particular defined with the PANSS), because most individuals with
2 www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8
Articles
first-episode psychosis will receive care from specialist practice, and thus there were no restrictions on the
teams, as recommended by National Institute for Health antipsychotics that could be selected or their doses.
and Care Excellence guidelines; were in contact with Clinicians could switch antipsychotics and adjust doses
mental health services, under the care of a consultant as clinically indicated, but were encouraged to continue
psychiatrist; scored at least 4 on the PANSS delusions or antipsychotic treatment for a minimum of 12 weeks,
hallucinations items, or at least 5 on suspiciousness, and preferably for at least 26 weeks. Participants
persecution, or grandiosity items; and had to have the allocated to the combined treatment group were offered
capacity to consent and also had to be help-seeking. CBT and antipsychotic medications as described for the
Exclusion criteria were receipt of antipsychotic monotherapy groups.
medication or structured CBT with a qualified therapist Clinicians could prescribe drugs other than anti
within the past 3 months, moderate-to-severe learning psychotics, including antidepressants, anxiolytics, and
disabilities, organic impairment, a score of 5 or more on hypnotics, for all participants. Participants were offered
the PANSS conceptual disorganisation item, and a monitoring assessments at 6 weeks, 12 weeks, 24 weeks,
primary diagnosis of alcohol or substance dependence; and 52 weeks. At each assessment, we measured weight,
patients who were an immediate risk to themselves or blood pressure, HbA1c concentrations, fasting glucose
others, and those who did not speak English were also concentrations, and fasting lipids (ie, total cholesterol,
excluded. The PANSS was administered by a research LDL, HDL, triglycerides and prolactin concentrations).
assistant in the participant’s home or a suitable clinical To allay concerns about the safety of withholding
service to establish eligibility, which was confirmed by a antipsychotics medication in the CBT group, trial
qualified clinician. Our trial protocol was approved by the procedures included monitoring for deterioration. Any
National Research Ethics Service of the UK’s National participant randomly assigned to either CBT alone or
Health Service (14/NW/0041). All participants provided antipsychotics alone could be moved to the combined
written informed consent.
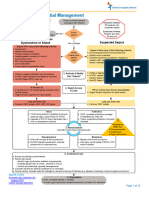
138 people screened for eligibility
Randomisation and masking
Participants were recruited via care coordinators,
consultant psychiatrists, and other mental health staff 63 not eligible
within participating mental health National Health 36 did not meet inclusion criteria
22 declined to participate
Service trusts. Eligible participants were then randomly 5 had other reasons
assigned (1:1:1) to antipsychotics, CBT, or antipsychotics
plus CBT via a secure web-based randomisation system
(Sealed Envelope) operated by the trial administrator. We 75 randomly assigned
used randomised permuted blocks of 4 and 6, stratified
by gender and first episode status. Randomisation at the
individual level was independent and concealed, with all 26 allocated to cognitive 24 allocated to antipsychotics 25 allocated to cognitive
assessors masked to group allocation. Allocation was behavioural therapy behavioural therapy and
subsequently made known to the trial manager, trial antipsychotics
administrator, and therapists. Participants and their care
team were informed of the allocation by letter. 20 completed 6-week assessment 22 completed 6-week assessment 20 completed 6-week assessment
6 missed the assessment 1 missed the assessment 4 missed the assessment
Procedures 1 withdrew 1 withdrew
Participants allocated to CBT were offered up to
26 sessions of therapy based on a specific cognitive 23 completed 12-week 22 completed 12-week 20 completed 12-week
model15 during a 6-month treatment window. Up to assessment assessment assessment
3 missed the assessment 1 missed the assessment 4 missed the assessment
four optional booster sessions were available during 1 withdrew 1 withdrew
the subsequent 6 months. Therapy was individualised
and problem focused. Permissible interventions were
described in the manualised treatment protocol.16 Therapy 22 completed 24-week 22 completed 24-week 20 completed 24-week
assessment assessment assessment
sessions were usually offered weekly and delivered by 3 missed the assessment 1 missed the assessment 1 missed the assessment
appropriately qualified psychological therapists. Fidelity 1 withdrew 1 withdrew 2 withdrew
to protocol was ensured by weekly supervision and
regular rating of recorded sessions with the Cognitive
21 completed 52-week 22 completed 52-week 20 completed 52-week
Therapy Scale–Revised.17 assessment assessment assessment
Participants allocated to antipsychotics were pre 4 missed the assessment 1 missed the assessment 3 missed the assessment
scribed medication by their responsible psychiatrist. 1 withdrew 1 withdrew 2 withdrew
Treatment was begun as soon as possible after
randomisation. Prescribing mirrored standard clinical Figure: Trial profile
www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8 3
Articles
treatment group if deterioration in mental state led to
Antipsychotics (n=24) CBT (n=26) Antipsychotics plus
CBT (n=25) involuntary hospitalisation, or if there was a greater
than 25% deterioration in PANSS scores at the 6-week
Age, years 23·21 (4·97) 23·19 (6·32) 24·44 (6·86)
assessment or a greater than 12·5% deterioration in
Sex
PANSS scores at the 12-week assessment.
Male 13 (54%) 16 (62%) 14 (56%)
Female 11 (46%) 10 (38%) 11 (44%)
Outcomes
First-episode psychosis: 24:0 24:2 25:0
multiple episode
The primary outcome was feasibility, which was
psychosis operationalised in terms of referral rates, recruitment,
Duration of untreated 37·33 (44·41) 44·48 (52·30) 39·43 (35·76) retention or attrition, acceptability of treatment,
psychosis, weeks attendance at sessions, adherence to homework, and
PANSS compliance with medication. The primary effectiveness
Total 70·17 (10·12) 70·50 (8·12) 70·76 (8·45) outcome was total score on PANSS18—a 30-item,
Positive 23·04 (4·60) 23·15 (4·63) 21·92 (3·63) semi-structured interview assessing dimensions of
Negative 16·17 (5·72) 15·50 (4·10) 15·24 (5·17) psychosis symptoms rated on a seven-point scale
Disorganised 16·25 (2·60) 17·15 (3·65) 17·8 (4·27) between 1 (absent) and 7 (severe)—which was assessed at
Excitement 18·25 (4·35) 17·85 (3·86) 17·4 (4·14) baseline, 6 weeks, 12 weeks, 24 weeks, and 52 weeks.
Emotional Distress 25·46 (5·00) 25·31 (3·83) 26·28 (3·47) Secondary clinical outcomes were depression and anxiety
Questionnaire about 38·71 (9·23) 40·13 (9·33)* 41·8 (11·79) (assessed with the Hospital Anxiety and Depression
Process of Recovery Scale19), quality of life (assessed with the WHO Quality of
HADS† Life20), social functioning (assessed with the Personal and
Total 41·05 (5·49) 37·54 (5·42) 36·36 (6·76) Social Performance scale21), user-defined recovery
Anxiety 21·96 (2·62) 20·50 (3·32) 19·36 (3·89) (measured with the Questionnaire about the Process of
Depression 19·05 (4·87) 17·38 (3·32) 17·28 (5·55) Recovery22), and results on the Clinical Global
WHO quality of life score‡ 67·03 (14·99) 68·66 (13·41) 70·18 (15·41) Impressions of symptom severity and improvement
Personal and Social 52·67 (13·83) 57·38 (12·04) 58·16 (11·1) scale.23 Instruments were administered by research
Performance Scale assistants trained in their use to achieve a good level
CGI of inter-rater reliability (intraclass correlation
Participant version 4·91 (0·97)§ 4·42 (0·99) 4·38 (1·54) coefficient 0·902).
Clinician version 4·13 (0·74) 4·08 (0·63) 4·04 (0·68) Service use, diagnosis, and antipsychotic prescribing
ANNSERS were recorded via review of case notes. Duration of
Number of side-effects 9·96 (4·72), 24 8·88 (3·77), 26 9·16 (4·69), 25 antipsychotic treatment for each participant was based on
Total 13·92 (7·05), 24 12·12 (6·55), 26 12·28 (6·61), 25 all regular antipsychotics prescribed and was not restricted
Cholesterol to the primary antipsychotic (ie, the antipsychotics
Total (mmol/L) 4·54 (0·91), 20 4·08 (0·82), 15 4·45 (0·93), 16 prescribed for the longest during the study). Non-
HDL (mmol/L) 1·34 (0·35), 20 1·13 (0·30), 15 1·38 (0·40), 15 neurological side-effects were assessed systemically with
Total/HDL 3·57 (0·94), 20 3·5 (0·86), 15 3·35 (0·93), 15 the Antipsychotic Non-neurological Side Effects Rating
LDL (mmol/L) 2·58 (0·78), 15 2·33 (0·67), 12 2·46 (0·68), 14 Scale.24 At 6 months, we obtained self-report data for
Triglycerides (mmol/L) 1·15 (0·39), 16 1·27 (0·64), 12 1·12 (0·45), 14 antipsychotic adherence in the past month on a visual
Prolactin (mU/L) 183·06 (89·71), 17 187·07 (63·33), 15 198·5 (81·78), 14 analogue scale. At the 52-week visit, we surveyed
Glucose (mmol/L) 6·27 (6·96), 18 5·32 (2·41), 15 4·14 (0·55), 15 participants’ opinions on their preferences and views of
measures used in the study to inform choice of measures
Data are mean (SD); mean (SD), number of observations; or n (%), unless otherwise specified. CBT=cognitive for a definitive trial.
behavioural therapy. PANSS=Positive and Negative Syndrome Scale. HADS=Hospital Anxiety and Depression Scale.
CGI=Clinical Global Impressions of Symptom Severity and Improvement Scale. ANNSERS= Antipsychotic After the original ethical approval for the trial in
Non-neurological Side Effects Rating Scale. *n=25. †n=23 in the antipyschotics group and 24 in the CBT group. February, 2014, a substantial protocol amendment was
‡n=25 in the CBT group and 24 in the antipsychotics plus CBT group. §n=22. made (and approved on July 7, 2014): the lower age limit
Table 1: Baseline characteristics was changed from 18 years to 16 years, being an inpatient
was removed as an exclusion criterion, posing an
immediate risk to self or others was introduced as an
treatment group if their mental state declined during exclusion criterion, and the randomisation timeframe
the trial (this procedure was detailed in the standard was amended from 2 working days to 5 working days.
operating procedures for the study and was presented to Other minor amendments included the addition of
the Research Ethics Committee and clinicians who service user and clinician surveys to gather information
referred to the study). Participants who experienced about the feasibility of recruitment. We had originally
such deterioration remained in the trial, and the proposed that the recruitment window would be variable,
assessment schedule was maintained. Participants were with participants recruited in the first 22 months
also given the option to move into the combined receiving a full 6 months’ follow up and participants
4 www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8
Articles
recruited thereafter offered assessments up to the end of
Randomly assigned treatment group Total
treatment. However, we agreed a no-cost extension with
the funder, and were thus able to complete 12-month Antipsychotics CBT Antipsychotics
(n=24) (n=26) plus CBT (n=25)
follow-up visits for all participants. We also originally
proposed that economic analyses would explore the costs Treatment received
of health and social care and quality-adjusted life years Antipsychotics 15 2 4 21
from a broadly societal perspective. However, the EQ5D CBT 0 15 5 20
was erroneously omitted from our assessment battery, Antipsychotics 1 6 14 21
plus CBT
meaning that such analyses were not possible.
Neither 8 3 2 13
Statistical analysis CBT=cognitive behavioural therapy.
The sample size was based on recommendations for
Table 2: Participants’ randomly assigned treatment vs treatment received
obtaining reliable sample size estimates in pilot and
feasibility studies,25 which suggested that 75 patients
would be needed (ie, 25 in each group), with the aim of had multiple previous episodes and were recruited from
achieving usable data for 60 participants across the community mental health services. Most participants did
three groups, allowing for a dropout rate of 20%.26 not have diagnoses in their medical records at baseline.
Primary analysis was by intention to treat. We fitted The most common entry was first-episode psychosis, and
random intercept models with summed scores as the most common formal ICD-10 diagnosis was F29
dependent variables, allowing for attrition and the unspecified non-organic psychosis. Participants from ten
variable follow-up times introduced by trial design. of the 22 participating clinical teams (appendix) were
Covariates were sex, age, time, and the baseline value of randomly assigned. Retention was reasonable, with only
the relevant outcome measure (first episode status, as a four withdrawals and low attrition, which were balanced
stratification factor, should have been included, but across the groups (figure). Nine (12%) partial blind
because only two participants were not having their first breaks (ie, only one treatment was revealed) and
episode of psychosis, age was a more appropriate five (7%) full blind breaks (ie, actual randomly assigned
covariate). The use of these models allowed for analysis group was revealed) were reported by research assistants.
of all available data, on the assumption that data were Four of the full blind breaks were in the antipsychotic
missing at random,27 conditional upon covariates. All arm, and one was in the combined arm. Only 3 (1%) of
treatment effects reported are estimates of the effects 256 follow-up assessments were done by an unmasked
common to all follow-up times (essentially, repeated assessor (the blind was broken during the assessment).
measures ANCOVAs). Because safety and unwanted All three of these assessments were then scored by a
effects should be analysed on the basis of the most masked rater, and consensus was reached on ratings.
accurate information, these results are reported with an Thus, no assessments were done without rater masking
as-treated rather than an intention-to-treat approach. As- Participants who were assigned to CBT (either mono
treated was defined with our predefined minimum therapy or in the combined group) received a mean of
dose criteria for antipsychotics (ie, at least 6 weeks at 14·39 sessions (SD 9·12; range 0–26) within 6 months,
a therapeutic dose) and CBT (at least six sessions). with each session lasting around an hour (additional
We used Stata (version 14.2) for all analyses. This booster sessions were also offered as appropriate).
trial was prospectively registered with ISRCTN 40 (78%) of 51 participants attended six or more sessions,
(number ISRCTN06022197). and only one participant (2%) attended no sessions. Home
work com pliance was good for both participants and
Role of the funding source therapists: 404 (73%) of 557 participant between-session
The funder had no role in study design; data collection, tasks and 396 (89%) of 445 therapist between-session tasks
analysis, or interpretation; or writing of the Article. The were completed.
corresponding author and RE had access to all study data, Of the 49 participants assigned to antipsychotics (either
and the corresponding author had final responsibility for alone or in combination with CBT), 11 (22%) were not
the decision to submit for publication. prescribed a regular antipsychotic for various reasons,
including five participants who declined to take an
Results antipsychotic despite consenting to enter the trial. The
Between May 1, 2014 and Aug 30, 2016, we recruited primary antipsychotics prescribed most frequently were
75 participants, 26 to CBT, 24 to antipsychotics, and 25 to aripiprazole (n=14), olanzapine (n=10), and quetiapine
antipsychotics plus CBT (figure; table 1). The referral to (n=10), as chosen by the treating psychiatrist in the
recruitment rate was roughly 2:1, with only 22 (16%) of participants’ clinical care team (appendix). 12 (32%) of
138 referred patients declining to participate. 73 patients the 38 participants treated with antipsychotics switched
were experiencing first-episode psychosis and recruited antipsychotics at least once. 34 (92%) of 37 participants
from early-intervention services; the other two patients who commenced antipsychotic treatment were
www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8 5
Articles
Antipsychotics CBT (n=26) Antipsychotics plus Mean difference (SE; 95% CI); p value
(n=24) CBT (n=25)
CBT vs antipsychotics CBT vs antipsychotics Antipsychotics vs
plus CBT antipsychotics plus CBT
Total ·· ·· ·· –1·13 (2·39; –5·81 to –5·65 (2·41; –10·37 to –4·52 (2·44; –9·30 to
3·55); 0·637 –0·93); 0·019 0·26); 0·064
Week 0 70·13 (10·11), 24 70·35 (8·03), 26 70·76 (8·46), 25 ·· ·· ··
Week 6 64·05 (11·39), 22 64·85 (7·85), 20 64·70 (9·74), 20 ·· ·· ··
Week 12 60·81 (16·52), 21 63·74 (7·73), 23 58·40 (14·51), 20 ·· ·· ··
Week 24 61·09 (14·44), 22 60·50 (8·74), 22 53·77 (12·54), 22 ·· ·· ··
Week 52 56·77 (14·10), 22 58·14 (11·68), 21 57·40 (13·58), 20 ·· ·· ··
Positive ·· ·· ·· –1·16 (1·14; –3·40 to –2·02 (1·15; –4·27 to –0·86 (1·17; –3·15 to
1·09); 0·312 0·24); 0·080 1·43); 0·462
Week 0 23·04 (4·60), 24 23·15 (4·63), 26 21·92 (3·63), 25 ·· ·· ··
Week 6 19·36 (5·44), 22 21·00 (4·38), 20 20·10 (4·41), 20 ·· ·· ··
Week 12 19·19 (7·72), 21 21·00 (4·72), 23 17·40 (5·65), 20 ·· ·· ··
Week 24 17·81 (6·85), 21 18·18 (4·81), 22 15·23 (5·31), 22 ·· ·· ··
Week 52 18·18 (6·52), 22 17·90 (5·92), 21 16·80 (6·05), 20 ·· ·· ··
Negative ·· ·· ·· –1·25 (0·78; –2·78 to –2·31 (0·79; –3·85 to –1·06 (0·79; –2·61,
0·28); 0·110 –0·77); 0·003 0·49); 0·178
Week 0 16·17 (5·72), 24 15·50 (4·10), 26 15·24 (5·17), 25 ·· ·· ··
Week 6 14·64 (5·06), 22 15·05 (3·52), 20 13·90 (4·85), 20 ·· ·· ··
Week 12 14·00 (4·32), 21 14·83 (3·10), 23 13·00 (5·23), 20 ·· ·· ··
Week 24 14·14 (5·47), 22 14·91 (4·72), 22 12·41 (4·60), 22 ·· ·· ··
Week 52 12·73 (4·58), 22 14·62 (4·52), 21 12·80 (3·68), 20 ·· ·· ··
Disorganised ·· ·· ·· –0·19 (0·77; –1·69 to –0·85 (0·77; –2·36 to –0·66 (0·80; –2·22 to
1·32); 0·809 0·66); 0·273 0·90); 0·408
Week 0 16·25 (2·59), 24 17·15 (3·65), 26 17·80 (4·27), 25 ·· ·· ··
Week 6 15·77 (3·18), 22 16·8 (2·91), 20 17·50 (4·01), 20 ·· ·· ··
Week 12 15·19 (4·96), 21 16·39 (3·37), 23 16·25 (4·10), 20 ·· ·· ··
Week 24 15·10 (3·86), 21 15·50 (3·53), 22 14·50 (3·78), 22 ·· ·· ··
Week 52 14·82 (3·67), 22 15·67 (3·73), 21 15·80 (4·25), 20 ·· ·· ··
Excitement ·· ·· ·· –0·45 (0·75; –1·91 to –0·80 (0·75; –2·27 to –0·35 (0·76; –1·84 to
1·02); 0·549 0·67); 0·286 1·13); 0·641
Week 0 18·25 (4·35), 24 17·85 (3·86), 26 17·4 (4·14), 25 ·· ·· ··
Week 6 15·95 (4·09), 22 15·90 (3·93), 20 15·75 (4·05), 20 ·· ·· ··
Week 12 15·52 (4·77), 21 15·52 (3·16), 23 14·35 (4·97), 20 ·· ·· ··
Week 24 14·77 (3·37), 22 14·45 (3·40), 22 12·86 (4·36), 22 ·· ·· ··
Week 52 13·41 (4·07), 22 13·62 (2·89), 21 13·80 (4·26), 20 ·· ·· ··
Emotional ·· ·· ·· 0·0 (1·11; –2·17 to –1·93 (1·12; –4·12 to –1·93 (1·13; –4·15 to
distress 2·18); 0·999 0·26); 0·084 0·29); 0·088
Week 0 25·46 (5·00), 24 25·31 (3·83), 26 26·28 (3·47), 25 ·· ·· ··
Week 6 22·55 (5·21), 22 21·50 (4·27), 20 23·10 (3·93), 20 ·· ·· ··
Week 12 21·38 (6·91), 21 22·48 (4·31), 23 19·60 (5·74), 20 ·· ·· ··
Week 24 21·55 (5·75), 22 20·95 (3·70), 22 17·50 (5·49), 22 ·· ·· ··
Week 52 19·86 (6·12), 22 19·10 (5·49), 21 20·10 (5·08), 20 ·· ·· ··
Data are mean (SD), number of observations, unless otherwise specified. The effects are common to all follow-up times and are analysed by intention to treat. CBT=cognitive
behavioural therapy.
Table 3: Outcomes on the Positive and Negative Syndrome Scale
prescribed their primary antipsychotic for 6 weeks or Self-reported data for medication adherence were
more (duration was not captured for one participant). available at 6 months for 42 (86%) of the 49 participants
The median duration of total antipsychotic treatment (86%) assigned to antipsychotics. 29 participants (69%)
was 44·5 weeks (IQR 26–51; range 2–52). 28 (78%) of reported that they were taking an antipsychotic at that
36 participants with accurate duration data were taking timepoint, among whom mean adherence was
antipsychotic medication at the end of the study. 77% (SD 29·19, range 0–100; on a scale on which
6 www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8
Articles
Antipsychotics (n=24) CBT (n=26) Combination (n=25) Mean difference (SE; 95% CI); p value
CBT vs CBT vs antipsychotics Antipsychotics vs
antipsychotics plus CBT antipsychotics plus CBT
QPR ·· ·· ·· –0·93 (2·97; –6·76 4·01 (3·14; –2·15 4·94 (3·05; –1·03 to
to 4·90); 0·754 to 10·17); 0·202 10·91); 0·105
Week 0 38·71 (9·23), 24 40·13 (9·33), 25 41·8 (11·79), 25 ·· ·· ··
Week 24 44·86 (14·99), 22 47·81 (8·86), 21 52 (14·05), 18 ·· ·· ··
Week 52 48·55 (14·73), 22 51·62 (9·25), 21 49·88 (11·04), 17 ·· ·· ··
HADS
Total ·· ·· ·· –0·60 (1·98; –4·48 –2·93 (2·03; –6·90 –2·32 (1·99; –6·22
to 3·27); 0·761 to 1·04); 0·148 to 1·56); 0·241
Week 0 41·05 (5·49), 23 37·54 (5·42), 24 36·36 (6·76), 25 ·· ·· ··
Week 24 35·55 (7·69), 22 35·36 (12·61), 22 30·37 (9·28), 19 ·· ·· ··
Week 52 34·27 (9·08), 22 32·14 (6·96), 21 30·35 (6·98), 17 ·· ·· ··
Anxiety ·· ·· ·· 0·62 (1·28; –1·89 –1·34 (1·32; –3·92 to –1·96 (1·30; –4·50
to 3·14); 0·627 1·25); 0·310 to 0·58); 0·131
Week 0 21·96 (2·62), 23 20·5 (3·32), 24 19·36 (3·89), 25 ·· ·· ··
Week 24 19·36 (4·51), 22 19·18 (10·80), 22 15·65 (5·98), 20 ·· ·· ··
Week 52 18·73 (5·03), 22 17·29 (4·64), 21 15·67 (4·89), 18 ·· ·· ··
Depression ·· ·· ·· –0·14 (1·20; –2·49 –1·60 (1·27; –4·08 to –1·46 (1·20; to –3·82
to 2·20); 0·905 0·88); 0·206 to 0·90); 0·226
Week 0 19·05 (4·87), 23 17·38 (3·32), 24 17·28 (5·55), 25 ·· ·· ··
Week 24 16·27 (5·84), 22 15·18 (3·81), 22 13·42 (5·83), 19 ·· ·· ··
Week 52 14·91 (5·52), 22 14·05 (4·2), 21 14·94 (5·36), 17 ·· ·· ··
WHO quality of ·· ·· ·· 0·62 (3·20; –5·65 5·82 (3·37; –0·78 5·21 (3·39; –1·43
life score to 6·88); 0·847 to 12·42); 0·084 to 11·84); 0·124
Week 0 67·03 (14·99), 24 68·66 (13·41), 25 70·18 (15·41), 24 ·· ·· ··
Week 6 72·5 (19·84), 22 76·78 (14·79), 18 77·82 (14·06), 17 ·· ·· ··
Week 12 77·29 (21·31), 21 79·29 (16·59), 21 85·83 (17·59), 18 ·· ·· ··
Week 24 79·15 (20·95), 20 79·10 (14·03), 21 89·06 (18·87), 18 ·· ·· ··
Week 52 81·36 (20·02), 22 83·81 (15·23), 21 82·93 (19·17), 15 ·· ·· ··
PSP ·· ·· ·· 3·18 (4·18; –5·02 2·17 (4·27; –6·19 –1·01 (4·24; –9·32 to
to 11·38); 0·448 to 10·53); 0·611 7·30); 0·812
Week 0 52·67 (13·83), 24 57·38 (12·04), 26 58·16 (11·1), 25 ·· ·· ··
Week 24 63·95 (18·53), 22 60·05 (10·51), 22 62·48 (17·47), 21 ·· ·· ··
Week 52 60·45 (17·61), 22 60·95 (12·93), 21 61 (16·47), 20 ·· ·· ··
CGI
Clinician ·· ·· ·· –0·16 (0·28; –0·70 –0·64 (0·29; 1·20 –0·48 (0·28; –1·03 to
to 0·38); 0·569 to –0·08); 0·026 0·07); 0·087
Week 0 4·13 (0·74), 24 4·08 (0·63), 26 4·04 (0·68), 25 ·· ·· ··
Week 24 3·32 (1·17), 22 3·45 (0·91), 22 2·86 (1·06), 21 ·· ·· ··
Week 52 3·23 (1·11), 22 3·38 (1·07), 21 3·00 (1·08), 20 ·· ·· ··
Patients ·· ·· ·· 0·35 (0·41; –0·44 –0·29 (0·42; 1·11 –0·65 (0·42; –1·46
to 1·15); 0·385 to 0·52); 0·482 to 0·17); 0·119
Week 0 4·91 (0·97), 22 4·42 (0·99), 26 4·38 (1·54), 25 ·· ·· ··
Week 24 4·33 (1·56), 21 3·71 (1·23), 21 3·20 (1·54), 20 ·· ·· ··
Week 52 3·91 (1·48), 22 3·50 (1·50), 20 3·94 (1·59), 18 ·· ·· ··
Clinician – ·· ·· ·· 0·05 (0·31; –0·56 –0·53 (0·32; –1·16 to –0·58 (0·31; –1·19 to
improvement to 0·65); 0·876 0·10); 0·097 0·03); 0·064
Week 0 ·· ·· ·· ·· ·· ··
Week 24 2·95 (1·21), 22 2·78 (1·23), 22 2·14 (0·91), 21 ·· ·· ··
Week 52 2·45 (1·06), 22 2·50 (1·00), 20 2·25 (1·12), 20 ·· ·· ··
Data are mean (SD), number of observations, unless otherwise specified. The effects are common to all follow-up times and are analysed by intention to treat. CBT=cognitive
behavioural therapy. QPR=Questionnaire about Process of Recovery. HADS=Hospital Anxiety and Depression Scale. PSP=Personal and Social Performance Scale. CGI=Clinical Global
Impressions of Symptom Severity and Improvement Scale.
Table 4: Secondary outcomes
www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8 7
Articles
(p=0·003) groups (table 6). The difference in adverse
Deterioration Improvement
effects between the combined group and the
>25% >50% >25% >50% antipsychotics group was not significant (table 6). In the
Intention-to-treat analysis as-treated analysis, no hospital admissions were recorded
24 weeks among those in the antipsychotics group or those who
CBT 0 2 8 2 received no interventions (appendix). Two participants in
Antipsychotics 0 1 5 3 the CBT group (four admissions) and four people in the
Antipsychotics plus CBT 0 0 11 7 combined group were admitted to hospital (appendix).
52 weeks Only three deteriorations were noted at 6 or 12 weeks in
CBT 0 1 8 4 monotherapy participants (two in the antipsychotics
Antipsychotics 2 0 8 5 group and one in the CBT group).
Antipsychotics plus CBT 0 0 7 6 We recorded another ten potential serious adverse
As-treated analysis events in nine participants (appendix). Only one of these
24 weeks events was thought to be related to the trial (the overdose
CBT 0 1 8 3 of three paracetamol tablets in a participant in the CBT
Antipsychotics 0 1 3 2 group). Only three participants (two in the antipsychotics
Antipsychotics plus CBT 0 1 9 4 group, one in the CBT group) met our deterioration
Neither 0 0 4 3
criteria at 6 or 12 weeks, which prompted an offer to move
52 weeks
into the combined arm.
CBT 0 0 6 6
Antipsychotics 2 0 6 0
Discussion
Our single-blind, randomised, controlled pragmatic
Antipsychotics plus CBT 0 1 8 4
pilot and feasibility trial showed that a study comparing
Neither 0 0 3 5
antipsychotics, CBT, and antipsychotics plus CBT is
Data are n. CBT=cognitive behavioural therapy. possible in people with psychosis. Our trial had low
attrition (<20% at each timepoint) that was balanced
Table 5: Participants with improvements or deteriorations in total
scores on the Positive and Negative Syndrome Scale at 24 and 52 weeks across interventions, and only a small proportion of
participants received an intervention to which they were
not allocated. All three interventions were broadly safe
100% indicates they had taken every dose over the past and acceptable.
month). The mean baseline PANSS total score in the overall
The proportion of patients receiving allocated population was 70·4, which is similar to the baseline
interventions was similar across groups (table 2). PANSS score of 73·8 seen in the CAFÉ study,29 but lower
15 patients (58%) in the CBT group, 15 (63%) in the than the baseline score of 88·5 in EUFEST30 (CAFÉ and
antipsychotics group, and 14 (56%) in the combined EUFEST are large, 1-year randomised controlled trials of
group received the correct allocated intervention. antipsychotics in early psychosis). The mean changes in
Psychiatric symptoms were significantly reduced over PANSS total scores we noted from baseline to 52 weeks
time across all conditions (appendix). The PANSS total (antipsychotics 13·3, CBT 12·3, antipsychotics plus
score differed significantly between the combined group CBT 13·4) were all within the range of those noted with
and the CBT group (p=0·019), but not between the the three antipsychotics in CAFÉ (olanzapine 18·4,
combined group and the antipsychotics group quetiapine 15·6, risperidone 8·4), but lower than those
(p=0·064), or between the CBT group and the in EUFEST (changes of around 35 points with the five
antipsychotics group (p=0·637; table 3). Table 4 shows antipsychotics assessed). The mean PANSS reductions
results for secondary outcomes. PANSS analyses that we noted were less than the 15 points estimated to be
did not include age as a covariate had similar results to equivalent to a rating of minimal improvement on the
the primary analyses (appendix). Clinical Global Impressions scale,31 although the
In the intention-to-treat analysis, the numbers of threshold for minimal improvement could be lower for
participants in each group (completer-only data— patients with less severe symptoms at baseline.31 The
ie, observed cases) achieving 25% and 50% improvements reductions in our trial were larger than the minimal
on adjusted PANSS total scores28 were highest in the clinically important difference in PANSS total score
combined arm at 6 months, and very similar across all estimated to be associated with obtaining employment as
groups at 12 months (table 5). In the as-treated analysis, an objective measure of functioning (8·3 points),32 and
few deteriorations were noted in any groups at both similar to the minimal clinically important difference
6 months and 12 months (table 5). associated with patient-rated improvement (11·2 points).33
Adverse effects (as measured by ANNSERS) were We recorded improvement across measures of symptoms
significantly less common in the CBT group than in the and personal and social recovery, functioning, and quality
antipsychotics (p=0·017) or the antipsychotics plus CBT of life, irrespective of intervention.
8 www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8
Articles
Antipsychotics CBT (n=20) Antipsychotics plus Mean difference (SE; 95% CI); p value
(n=21) CBT (n=21)
CBT vs antipsychotics CBT vs antipsychotics plus CBT Antipsychotics vs
antipsychotics plus CBT
ANNSERS
Number of side-effects ·· ·· ·· 3·22 (1·35; 0·58 to 5·87); 3·99 (1·35; 1·36 to 6·64); 0·78 (1·37; –1·91 to 3·47);
0·017 0·003 0·572
Week 0 8·52 (3·66), 21 8·55 (3·94), 20 10·33 (4·54), 21 ·· ·· ··
Week 24 8·47 (5·62), 17 5·7 (3·23), 20 10·05 (5·35), 19 ·· ·· ··
Week 52 9·06 (5·5), 16 4·74 (3·35), 19 10·42 (5·90), 19 ·· ·· ··
Total score ·· ·· ·· 5·12 (2·05; 1·11 to 9·14); 6·30 (2·03; 2·32 to 10·27); 1·17 (2·07; –2·89 to 5·24);
0·012 0·002 0·571
Week 0 11·57 (5·48), 21 11·7 (6·21), 20 13·62 (6·18), 21 ·· ·· ··
Week 24 11·59 (8·40), 17 7·45 (4·99), 20 14·16 (8·42), 19 ·· ·· ··
Week 52 12·94 (8·77), 16 6·21 (5·07), 19 13·79 (7·63), 19 ·· ·· ··
Cholesterol
HDL (mmol/L) ·· ·· ·· 0·07 (0·09; –0·10 to 0·24); 0·09 (0·09; –0·09 to 0·26); 0·01 (0·08; –0·15 to 0·17);
0·389 0·346 0·893
Week 0 1·37 (0·35), 16 1·21 (0·32), 12 1·37 (0·41), 13 ·· ·· ··
Week 12 1·37 (0·38), 14 1·21 (0·29), 9 1·54 (0·49), 15 ·· ·· ··
Week 52 1·15 (0·36), 8 1·36 (0·31), 6 1·24 (0·21), 7 ·· ·· ··
Total/HDL ratio ·· ·· ·· –0·08 (0·22; –0·50 to 0·35); 0·01 (0·24; –0·45 to 0·48); 0·09 (0·21; –0·33 to 0·51);
0·722 0·950 0·667
Week 0 3·4 (0·85), 16 3·58 (0·66), 12 3·06 (0·81), 13 ·· ·· ··
Week 12 3·63 (1·25), 14 3·64 (0·44), 10 3·23 (0·65), 14 ·· ·· ··
Week 52 4·41 (2·11), 8 3·51 (0·53), 7 3·68 (1·05), 6 ·· ·· ··
LDL (mmol/L) ·· ·· ·· –0·21 (0·28; –0·76 to 0·33); –0·15 (0·29; –0·72 to 0·42); 0·06 (0·26; –0·45 to 0·58);
0·449 0·615 0·809
Week 0 2·42 (0·79), 14 2·44 (0·58), 10 2·34 (0·72), 11 ·· ·· ··
Week 12 2·59 (0·72), 12 2·79 (0·92), 8 2·63 (0·74), 12 ·· ·· ··
Week 52 3·02 (0·84), 6 2·83 (0·59), 6 2·63 (0·90), 6 ·· ·· ··
Triglycerides (mmol/L) ·· ·· ·· 0·08 (0·19; –0·29 to 0·45); –0·27 (0·20; –0·66 to 0·12); –0·35 (0·18; –0·71 to 0·00);
0·659 0·170 0·051
Week 0 1·23 (0·45), 14 1·16 (0·56), 10 1·15 (0·58), 11 ·· ·· ··
Week 12 1·45 (0·75), 12 1·4 (0·63), 8 1·11 (0·63), 13 ·· ·· ··
Week 52 1·62 (1·11), 6 0·97 (0·28), 6 2·57 (4·08), 7 ·· ·· ··
Prolactin (mU/L) ·· ·· ·· 23·12 (26·73; –29·27 to –7·39 (29·00; –64·22 to –30·51 (28·28; –85·94 to
75·50); 0·387 49·44); 0·799 24·93); 0·281
Week 0 162·86 (98·96), 14 188·42 (72·73), 12 221·58 (74·14), 12 ·· ·· ··
Week 12 206·92 (83·76), 13 196·22 (83·08), 9 180 (73·90), 10 ·· ·· ··
Week 52 136·71 (53·84), 7 201·83 (93·32), 6 186·13 (88·69), 8 ·· ·· ··
Glucose (mmol/L) ·· ·· ·· –0·56 (0·50; –1·53 to 0·42); –0·75 (0·52; –1·77 to 0·27); –0·19 (0·45; –1·07 to 0·68);
0·265 0·148 0·662
Week 0 6·6 (7·63), 15 5·04 (2·68), 12 4·72 (0·95), 13 ·· ·· ··
Week 12 4·76 (1·10), 11 5·2 (1·72), 7 4·55 (0·55), 14 ·· ·· ··
Week 52 4·63 (0·65), 8 5·32 (1·81), 6 4·11 (0·76), 7 ·· ·· ··
Weight (kg) ·· ·· ·· 1·80 (1·40; –0·94 to 4·54); 3·70 (1·41; 0·93 to 6·47); 1·90 (1·36; –0·76 to 4·57);
0·198 0·009 0·162
0 75·91 (20·31), 21 73·62 (15·72), 18 70·93 (12·97), 21 ·· ·· ··
6 77·06 (18·20), 16 74·84 (17·27), 15 70·82 (13·56), 18 ·· ·· ··
12 72·87 (13·32), 16 73·58 (15·66), 19 73·86 (14·01), 19 ·· ·· ··
24 78·21 (17·38), 18 72·12 (15·14), 20 75·33 (13·59), 16 ·· ·· ··
52 74·87 (15·34), 16 75·71 (14·88), 15 75·22 (15·07), 18 ·· ·· ··
(Table 6 continues on next page)
www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8 9
Articles
Antipsychotics CBT (n=20) Antipsychotics plus Mean difference (SE; 95% CI); p value
(n=21) CBT (n=21)
CBT vs antipsychotics CBT vs antipsychotics plus CBT Antipsychotics vs
antipsychotics plus CBT
(Continued from previous page)
Systolic blood pressure ·· ·· ·· 1·36 (2·76; –4·06 to 6·78); 0·52 (2·83; –5·04 to 6·07); –0·84 (2·44; –5·61 to 3·93);
(mm Hg) 0·624 0·855 0·730
Week 0 124·12 (12·91), 20 124·05 (15·02), 14 118·98 (11·11), 19 ·· ·· ··
Week 12 124·49 (16·53), 14 122·13 (10·16), 14 123·86 (14·13), 17 ·· ·· ··
Week 52 123·6 (13·28), 16 122·22 (10·67), 10 116·9 (8·47), 18 ·· ·· ··
Data are mean (SD), number of observations on an as-treated basis, unless otherwise specified. CBT=cognitive behavioural therapy. ANNSERS=Antipsychotic Non-neurological Side Effects Rating Scale.
*ANNSERS consists of 43 non-neurological side-effects, each rated as absent (0), mild (1), moderate (2), or severe (3), with a total possible score of 129.
Table 6: Secondary outcomes (adverse effects)
Antipsychotics plus CBT was significantly more weekly contact with trial staff tasked with reporting
efficacious than CBT alone (p=0·019), but the difference adverse effects (the trial therapists). By contrast, patients
between antipsychotics plus CBT and antipsychotics in the antipsychotics group had much less frequent
alone was not significant (p=0·06). However, because contact with trial staff (the trial research assistants).
this study was a pilot and feasibility trial, it was not The number of sessions attended and compliance with
powered to reliably detect differences between groups, homework tasks suggests that CBT was delivered
and any significant differences should be treated with successfully to most participants, although competence of
caution. Efficacy did not differ significantly between the CBT delivery and adherence to the treatment protocol was
CBT group and the antipsychotic group, which is not monitored systematically. Antipsychotics were
noteworthy given that CBT finished after 24 weeks selected on an individual basis, consistent with National
whereas antipsychotic treatment could last 52 weeks Institute for Health and Care Excellence guidance. The
(median duration 44·5 weeks). The absence of any four antipsychotics used most frequently in the study
apparent differences between the three groups at 6 weeks (aripiprazole, olanzapine, quetiapine, and risperidone) are
is also noteworthy (appendix), because 6 weeks is a the four antipsychotics most commonly initiated in
common length for drug trials. The number of routine clinical practice in first-episode services in
participants with PANSS-rated deterioration was low the UK.34 Dose and duration of antipsychotic treatment
across all groups at each timepoint, with no suggestion were at the discretion of the treating clinician and patient
that CBT was worse than antipsychotics or combination wishes. One patient’s primary antipsychotic was pro
treatment. Only three early deteriorations (ie, at 6 or mazine, which is approved to treat agitation but not
12 weeks) were noted, two in the antipsychotics group psychosis; the low dose given was insufficient to be
and one in the CBT group. regarded as an effective antipsychotic dose (appendix).
Fewer side-effects were noted in the CBT group than in The mean modal doses of the other primary antipsychotics
the antipsychotic group or the combined intervention prescribed were at the low end of the dose ranges
group. However, this difference is more accounted for by recommended to treat psychosis, which is probably
reduction in side-effects over time in the CBT group than because participants were recruited almost exclusively
by increases in side-effects in the antipsychotic and from early-intervention services. People with first-episode
combined groups. This decrease in side-effects in the psychosis respond to doses of antipsychotics lower than
CBT group could be related to many ANNSERS items those required for multi-episode schizophrenia,29 and are
being non-specific (eg, sleep problems, memory and more sensitive to side-effects than patients with multi-
attention, loss of libido, loss of energy, and autonomic episode schizophrenia, which has led to guidelines recom
symptoms). Such symptoms could be symptoms of a mending low doses.35,36 Nevertheless, the doses of some of
psychotic disorder or a comorbid illness, or could be the antipsychotics, especially quetiapine, were lower than
antipsychotic side-effects. Some patients in the CBT the corresponding doses used in the CAFÉ and EUFEST
group and the combined group were admitted to hospital, trials in first-episode psychosis. In most cases in our
whereas no patients in the antipsychotic group were. study, when duration of antipsychotic treatment was
Similarly, no serious adverse events were reported to the known, the primary antipsychotic was continued for
ethics committee for the antipsychotics group, compared 6 weeks or longer, suggesting that treatment duration was
with two for the CBT group and four for the combined sufficient to establish effectiveness. 12 (32%) of the
group (although only one was deemed treatment related). 38 participants who started antipsychotic treatment
There is increased opportunity for adverse events to be switched anti psychotic at least once, implying pers
observed in the patients receiving CBT, because they had everance to identify an effective medication. Overall, use
10 www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8
Articles
of antipsychotics was pragmatic and broadly consistent The design of our study (ie, three active intervention
with clinical practice in early-intervention services and arms), combined with the fact that most participants
treatment guidelines. received care from early-intervention services, means that
The study had several limitations. The pilot and we cannot rule out the possibility that recorded benefits
feasibility trial design and small sample size mean that could be attributable to generic factors such as good care
caution should be used when interpreting the statistical coordination, engagement, assertive outreach, and crisis
tests and significance values. Although only 12% of management, rather than the specific active treatments.
participants received an intervention they were not Failure to include the EQ5D means we could not examine
allocated to, a reasonable proportion did not take up the quality-adjusted life-years and cost-effectiveness.
offer of allocated interventions, reflecting that in clinical The main implication of this trial is that an adequately
practice many people do not comply with medication powered efficacy and effectiveness trial is needed to
regimens,34 and some do not engage with talking therapies. provide evidence about relative efficacy of antipsychotics
Such rates of non-adherence are common in drug and and CBT. In our trial, participants were almost exclusively
psychological therapy trials. Operationalisation of experiencing a first episode of psychosis, so a definitive
antipsychotic treatment in terms of target doses, minimal trial should target this population and recruit via early-
duration of trials, and encouraging switching if treatment intervention services (appendix). A trial in people with
was unsatisfactory might have improved the efficacy of multiple episode psychotic disorders would probably not
drug treatment, but higher doses might have led to more be feasible in generic community mental health teams,
side-effects and greater dropout rates. In our trial, mostly because potential participants are already
medication was prescribed and dispensed in accordance prescribed antipsychotics. At present, it seems reasonable
with normal clinical practice, as opposed to delivery of to support people with psychosis (who do not present
medication to patients and use of regular pill counts, both immediate risk to themselves or others) to make informed
of which might improve adherence. The absence of weight choices as outlined in the National Institute for Health
gain in the antipsychotics group casts doubt on adherence. and Care Excellence guidelines,1 which recommend
We did not have a standardised operating procedure for advising people who want to try psychological
weight measurement that emphasised consistency of interventions alone that such inter ventions are more
flooring, and many assessments were done in participants’ effective when delivered in conjunction with antipsychotic
homes. Therefore, weight data could contain errors. medication, but allowing them to try family intervention
Another limitation is that we did not systematically record and CBT without antipsychotics while agreeing a time to
use of other medications such as antidepressants or review treatment options, including introduction of anti
anxiolytics, or measure substance and alcohol use. psychotics.
Response rates on the PANSS and the degree of Contributors
improvement on the Clinical Global Impressions scale All authors were involved in study design, management, and delivery,
were lower in our trial than in previous 52-week and contributed to drafting of this Article. APM was the chief
investigator, conceived the study, prepared the protocol, supervised
randomised controlled trials of antipsychotics in first- researchers, had overall responsibility for day-to-day running of the study,
episode psychosis.29,30 However, data analytic strategies and interpreted data, led writing of the Article, and is the study guarantor.
high attrition in these studies might have increased the APM, PF, EKM, NH, AS, SEB, and JP-C prepared the treatment protocol
risk of bias, which could inflate effects. In EUFEST,30 for and trained and supervised the therapists. APM, HL, MP, and PMH
trained the researchers in use of psychiatric interviews, and supervised
example, data obtained before treatment discontinuation and monitored standards of psychiatric interviewing and assessment
were used in analysis of PANSS outcomes, which was throughout the trial. APM, PF, ARY, and PMH advised on diagnostic
likely to have introduced bias given the high frequency of ratings and inclusion and exclusion criteria. DS, ARY, and PMH advised
discontinuation (33–72%, depending on the specific drug). on medical and pharmacological issues and liaised with prescribers.
HL was the trial manager, supervised and coordinated recruitment,
CAFÉ had very high attrition at 52 weeks (67–73%, contributed to training of research staff, and was responsible for staff
depending on drug), which probably introduced bias.29 management and overall study coordination. HL, LC, RS, and MP were
Response is also dependent on patient and illness responsible for maintaining reliability of assessment procedures and data
characteristics, which vary between studies. Our study collection. RE, the trial statistician, advised on randomisation and all
statistical aspects of the trial, developed the analysis plan, and did the
mostly involved participants who met PANSS-defined statistical analyses. LD was the health economist. RB was a service user
criteria for acceptance into early-intervention services, consultant involved in all aspects of the study.
whereas EUFEST and CAFÉ only included participants Declaration of interests
with schizophrenia spectrum diagnoses. APM, PF, and SEB deliver training workshops and have written textbooks
Our sample was diagnostically heterogeneous: about CBT for psychosis, for which they receive fees. All authors have
done funded research on CBT for psychosis, and RE, ARY, LD, and PMH
73 participants were recruited from early-intervention
have done funded research on antipsychotics. APM, PF, EKM, NH, AS,
services, which operationally define first-episode psych SEB, JP-C, and VB deliver CBT in the National Health Service. DS is an
osis with the PANSS. Therefore, our findings are expert adviser for the National Institute of Health and Care Excellence
generalisable to early-intervention services only, at least Centre for Guidelines and a board member of the National Collaborating
Centre of Mental Health. ARY has received honoraria from Janssen Cilag
in the UK, and should not be generalised to patients
and Sunovion. PMH has received honoraria for lecturing or consultancy
with long-term schizophrenia spectrum diagnoses.
www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8 11
Articles
work from Allergan, Galen, Janssen, Lundbeck, NewBridge 15 Morrison AP. The interpretation of intrusions in psychosis:
Pharmaceuticals, Otsuka, Sunovion, and Teva, plus conference support an integrative cognitive approach to hallucinations and delusions.
from Janssen, Lundbeck and Sunovion. All other authors declare no Behav Cogn Psychother 2001; 29: 257–76.
competing interests. 16 Morrison AP. A manualised treatment protocol to guide delivery
of evidence-based cognitive therapy for people with distressing
Acknowledgments psychosis: learning from clinical trials. Psychosis 2017; 9: 271–81.
This trial was funded by the National Institute for Health Research 17 Blackburn IM, James I, Milne D, Baker CA, Standart S, Garland A.
(NIHR) under its Research for Patient Benefit (RfPB) Programme The revised cognitive therapy scale (CTS-R): psychometric properties.
(Grant Reference Number PB-PG- 1112-29057). The views expressed are Behav Cogn Psychother 2001; 29: 431–46.
those of the authors and not necessarily those of the UK National Health 18 Kay S, Fiszbein A, Opler L. The positive and negative syndrome
Service, NIHR, the Department of Health, the National Institute for scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13: 261–76.
Health and Care Excellence, or the National Collaborating Centre for 19 Zigmond AS, Snaith RP. The hospital anxiety and depression scale.
Mental Health. We thank the Psychosis Research Unit Service User Acta Psychiatrica Scandinavica 1983; 67: 361–70.
Reference Group for their contributions to study design and 20 WHO Quality of Life Group. The World Health Organization
development of study-related materials, the Greater Manchester Clinical quality of life assessment (WHOQOL): development and general
Research Network for their support and assistance, and David Kingdon psychometric properties. Soc Sci Med 1998; 46: 1569–85.
and John Norrie, the independent members of our trial steering and data 21 Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R.
monitoring committee. We also thank Elizabeth Pitt for acting as a Development, reliability and acceptability of a new version of the
service user consultant for the trial (because of unforeseen DSM-IV Social and Occupational Functioning Assessment Scale
circumstances, she could not be contacted about this acknowledgment). (SOFAS) to assess routine social funtioning.
Acta Psychiatrica Scandinavica 2000; 101: 323–29.
References 22 Law H, Neil ST, Dunn G, Morrison AP. Psychometric properties of
1 National Institute for Health and Care Excellence. Psychosis and the Questionnaire about the Process of Recovery (QPR).
schizophrenia in adults: treatment and management. London: Schizophr Res 2014; 156: 184–89.
National Institute for Health and Care Excellence, 2014.
23 Guy W. Assessment manual for psychopharmacology. Rockville:
2 Jauhar S, McKenna PJ, Radua J, Fung E, Salvador R, Laws KR. US Department of Heath, Education, and Welfare Public Health
Cognitive-behavioural therapy for the symptoms of schizophrenia: Service Alcohol, Drug Abuse, and Mental Health Administration, 1976.
systematic review and meta-analysis with examination of potential
24 Ohlsen R, Williamson R, Yusufi B, et al. Interrater reliability of the
bias. Br J Psychiatry 2014; 204: 20–29.
Antipsychotic Non-Neurological Side-Effects Rating Scale measured
3 Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for in patients treated with clozapine. J Psychopharmacol 2008; 22: 323–29.
schizophrenia: effect sizes, clinical models, and methodological rigor.
25 Browne RH. On the use of a pilot sample for sample size
Schizophr Bull 2008; 34: 523–37.
determination. Stat Med 1995; 14: 1933–40.
4 Mehl S, Werner D, Lincoln TM. Does cognitive behavior therapy for
26 Law H, Carter L, Sellers R, et al. A pilot randomised controlled trial
psychosis (CBTp) show a sustainable effect on delusions?
comparing antipsychotic medication, to cognitive behavioural
A meta-analysis. Front Psychol 2015; 6: 1450.
therapy to a combination of both in people with psychosis:
5 Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and rationale, study design and baseline data of the COMPARE trial.
tolerability of 15 antipsychotic drugs in schizophrenia: Psychosis 2017; 9: 193–204.
a multiple-treatments meta-analysis. Lancet 2013; 382: 951–62.
27 Little RJA, Rubin DB. Statistical analysis with missing data.
6 Leucht S, Arbter D, Engel RR, Kissling W, Davis JM. How effective London: John Wiley and Sons, 2002.
are second-generation antipsychotic drugs? A meta-analysis of
28 Leucht S, Kissling W, Davis JM. The PANSS should be rescaled.
placebo-controlled trials. Mol Psychiatry 2009; 14: 429–47.
Schizophr Bull 2010; 36: 461–62.
7 Leucht S, Leucht C, Huhn M, et al. Sixty years of placebo-controlled
29 McEvoy JP, Lieberman JA, Perkins DO, et al. Efficacy and tolerability
antipsychotic drug trials in acute schizophrenia: systematic review,
of olanzapine, quetiapine, and risperidone in the treatment of early
Bayesian meta-analysis, and meta-regression of efficacy predictors.
psychosis: a randomized, double-blind 52-week comparison.
Am J Psychiatry 2017; 174: 927–42.
Am J Psychiatry 2007; 164: 1050–60.
8 Zhu Y, Li C, Huhn M, Rothe P, et al. How well do patients with a first
30 Kahn RS, Fleischhacker WW, Boter H, et al. Effectiveness of
episode of schizophrenia respond to antipsychotics: a systematic
antipsychotic drugs in first-episode schizophrenia and
review and meta-analysis. Eur Neuropsychopharmacology 2017;
schizophreniform disorder: an open randomised clinical trial.
27: 835–44.
Lancet 2008; 371: 1085–97.
9 Haddad P, Sharma S. Adverse effects of atypical antipsychotics:
31 Leucht S, Kane JM, Etschel E, Kissling W, Hamann J, Engel RR.
differential risk and clinical implications. CNS Drugs 2007;
Linking the PANSS, BPRS, and CGI: clinical implications.
21: 911–36.
Neuropsychopharmacol 2006; 31: 2318–25.
10 Correll CU, Solmi M, Veronese N, et al. Prevalence, incidence and
32 Thwin SS, Hermes E, Lew R, et al. Assessment of the minimum
mortality from cardiovascular disease in patients with pooled and
clinically important difference in quality of life in schizophrenia
specific severe mental illness: a large-scale meta-analysis of
measured by the Quality of Well-Being Scale and disease-specific
3 211 768 patients and 113 383 368 controls. World Psychiatry 2017;
measures. Psychiatry Res 2013; 209: 291–96.
16: 163–80.
33 Hermes EDA, Sokoloff DM, Stroup TS, Rosenheck RA.
11 Taylor M, Perera U. NICE CG178 psychosis and schizophrenia in
Minimum clinically important difference in the Positive And Negative
adults: treatment and management—an evidence-based guideline?
Syndrome Scale using data from the CATIE schizophrenia trial.
Br J Psychiatry 2015; 206: 357–59.
J Clin Psychiatry 2012; 73: 526–32.
12 Morrison AP, Birchwood M, Pyle M, et al. Impact of cognitive
34 Whale R, Harris M, Kavanagh G, et al. Effectiveness of antipsychotics
therapy on internalised stigma in people with at-risk mental states.
used in first-episode psychosis: a naturalistic cohort study.
Br J Psychiatry 2013; 203: 140–45.
BJPsych Open 2016; 2: 323–29.
13 Morrison AP, Turkington D, Pyle M, et al. Cognitive therapy for
35 Barnes TR. Evidence-based guidelines for the pharmacological
people with schizophrenia spectrum disorders not taking
treatment of schizophrenia: recommendations from the British
antipsychotic drugs: a single-blind randomised controlled trial.
Association for Psychopharmacology. J Psychopharmacol 2011;
Lancet 2014; 383: 1395–403.
25: 567–620.
14 Goldsmith LP, Lewis SW, Dunn G, Bentall RP. Psychological
36 Gardner DM, Murphy AL, O’Donnell H, Centorrino F,
treatments for early psychosis can be beneficial or harmful,
Baldessarini RJ. International consensus study of antipsychotic
depending on the therapeutic alliance: an instrumental variable
dosing. Am J Psychiatry 2010; 167: 686–93.
analysis. Psychol Med 2015; 45: 2365–73.
12 www.thelancet.com/psychiatry Published online March 28, 2018 http://dx.doi.org/10.1016/S2215-0366(18)30096-8
You might also like
- Your Examination for Stress & Trauma Questions You Should Ask Your 32nd Psychiatric Consultation William R. Yee M.D., J.D., Copyright Applied for May 31st, 2022From EverandYour Examination for Stress & Trauma Questions You Should Ask Your 32nd Psychiatric Consultation William R. Yee M.D., J.D., Copyright Applied for May 31st, 2022No ratings yet
- PIIS2215036618300968Document13 pagesPIIS2215036618300968zuhrul_baladNo ratings yet
- 1 s2.0 S0140673613622461 MainDocument9 pages1 s2.0 S0140673613622461 MainFrancisco Javier RamosNo ratings yet
- Clinical Effectiveness and Acceptability of StructDocument10 pagesClinical Effectiveness and Acceptability of StructArthur AlvesNo ratings yet
- Cognitive Behavioural Therapy in Clozapine-Resistant Schizophrenia (FOCUS) : An Assessor-Blinded, Randomised Controlled TrialDocument11 pagesCognitive Behavioural Therapy in Clozapine-Resistant Schizophrenia (FOCUS) : An Assessor-Blinded, Randomised Controlled TrialRabiatul AdawiyahNo ratings yet
- Background: Lancet Psychiatry 2017Document11 pagesBackground: Lancet Psychiatry 2017Manya DhuparNo ratings yet
- Pi Is 2215036616303789Document11 pagesPi Is 2215036616303789U of T MedicineNo ratings yet
- Goldstein 2010Document10 pagesGoldstein 2010esckere papas fritasNo ratings yet
- Sustained Benefit of Cognitive Behaviour Therapy For Health Anxiety in Medical Patients (CHAMP) Over 8 Years A Randomised-Controlled TrialDocument9 pagesSustained Benefit of Cognitive Behaviour Therapy For Health Anxiety in Medical Patients (CHAMP) Over 8 Years A Randomised-Controlled TrialJan LAWNo ratings yet
- Paroxetine, Cognitive Therapy or Their Combination in The Treatment of Social Anxiety Disorder With and Without Avoidant Personality Disorder: A Randomized Clinical TrialDocument11 pagesParoxetine, Cognitive Therapy or Their Combination in The Treatment of Social Anxiety Disorder With and Without Avoidant Personality Disorder: A Randomized Clinical TrialAdm Foto MahniteseNo ratings yet
- RCT - Telemedicine-Based Collaborative Care For Posttraumatic Stress Disorder - 2017Document10 pagesRCT - Telemedicine-Based Collaborative Care For Posttraumatic Stress Disorder - 2017RayssaNo ratings yet
- Špela PDFDocument11 pagesŠpela PDFŠpela MiroševičNo ratings yet
- 2022 de VriesDocument8 pages2022 de Vriesmvillar15_247536468No ratings yet
- Comparison of Clinical Significance of Cognitive-Behavioral Therapy and Psychodynamic Therapy For Major Depressive DisorderDocument8 pagesComparison of Clinical Significance of Cognitive-Behavioral Therapy and Psychodynamic Therapy For Major Depressive DisorderAnanda Amanda cintaNo ratings yet
- Jiwa 1Document9 pagesJiwa 1Hamidah S.No ratings yet
- Rector Et Al-2019-British Journal of Clinical PsychologyDocument18 pagesRector Et Al-2019-British Journal of Clinical PsychologyJulia DGNo ratings yet
- Pilot Randomised Controlled Trial of Culturally Adapted Cognitive Behavior Therapy For Psychosis (Cacbtp) in PakistanDocument8 pagesPilot Randomised Controlled Trial of Culturally Adapted Cognitive Behavior Therapy For Psychosis (Cacbtp) in Pakistanzuhrul_baladNo ratings yet
- Comparative Efficacy and Tolerability of 32 Oral Antipsychotics For The Acute Treatment of Adults With Multi-Episode Schizophrenia PDFDocument13 pagesComparative Efficacy and Tolerability of 32 Oral Antipsychotics For The Acute Treatment of Adults With Multi-Episode Schizophrenia PDFfrancesca_valdiviaNo ratings yet
- Anti Dep and Alzheimers Lancet 2011Document9 pagesAnti Dep and Alzheimers Lancet 2011bcy123No ratings yet
- Gloster Et Al., (2019)Document15 pagesGloster Et Al., (2019)Jonathan PitreNo ratings yet
- Physical Exercise and iCBT in Treatment of DepressionDocument9 pagesPhysical Exercise and iCBT in Treatment of DepressionCarregan AlvarezNo ratings yet
- Artikel InternasionalDocument15 pagesArtikel InternasionalFitriatul MunawarohNo ratings yet
- Depression TreatmentDocument8 pagesDepression TreatmentAkshay HegdeNo ratings yet
- We Therell 2009Document10 pagesWe Therell 2009Oslo SaputraNo ratings yet
- On Predicting Improvement and Relapse in Generalized Anxiety Disorder Following PsychotherapyDocument19 pagesOn Predicting Improvement and Relapse in Generalized Anxiety Disorder Following PsychotherapyElizaIancuNo ratings yet
- Internet-Versus Group-Administered Cognitive Behaviour Therapy For Panic Disorder in A Psychiatric Setting: A Randomised TrialDocument10 pagesInternet-Versus Group-Administered Cognitive Behaviour Therapy For Panic Disorder in A Psychiatric Setting: A Randomised TrialSophi RetnaningsihNo ratings yet
- Cuijpers Et Al., (2021)Document11 pagesCuijpers Et Al., (2021)Jonathan PitreNo ratings yet
- Birchwood 2014Document11 pagesBirchwood 2014Lisa MaghfirahNo ratings yet
- Eca MBCT en TocDocument11 pagesEca MBCT en TocMiriam JaraNo ratings yet
- Artículo Grupo 3Document11 pagesArtículo Grupo 3pepeluchovelezquezadaNo ratings yet
- Articles: BackgroundDocument11 pagesArticles: BackgroundNurul AhdiahNo ratings yet
- A Systematic Scoping Review of Psychological Therapies For Psychosis Within Acute Psychiatric In-Patient Settings.Document8 pagesA Systematic Scoping Review of Psychological Therapies For Psychosis Within Acute Psychiatric In-Patient Settings.Eric KatškovskiNo ratings yet
- The Role of CBT in Relapse Prevention of SchizophreniaDocument2 pagesThe Role of CBT in Relapse Prevention of SchizophreniaKorn IbraNo ratings yet
- Treatment of Acute Stress DisorderDocument11 pagesTreatment of Acute Stress DisorderKusnanto Penasehat Kpb RyusakiNo ratings yet
- Effectiveness of Videoconference-Delivered Cognitive Behavioral Therapy For Adults With Psychiatric Disorders: Systematic and Meta-Analytic ReviewDocument16 pagesEffectiveness of Videoconference-Delivered Cognitive Behavioral Therapy For Adults With Psychiatric Disorders: Systematic and Meta-Analytic ReviewlaiaNo ratings yet
- Edited By: Dr. Javaid Akhtar, MCPS, FCPS, Head Of: Search StrategyDocument3 pagesEdited By: Dr. Javaid Akhtar, MCPS, FCPS, Head Of: Search StrategyKaram Ali ShahNo ratings yet
- (Stanley) Joc90025 - 1460 - 1467Document8 pages(Stanley) Joc90025 - 1460 - 1467niia kurniiasihNo ratings yet
- Bryant20et20al20 20additive20benefit20of20hypnosis20and20cbtDocument8 pagesBryant20et20al20 20additive20benefit20of20hypnosis20and20cbtita elizabethNo ratings yet
- Meta-Analysis of The Efficacy of Treatments For PTSDDocument10 pagesMeta-Analysis of The Efficacy of Treatments For PTSDJulianaNo ratings yet
- Metanalisis Comparacion de La Eficacia de de La Psicoterapia en Pacientes DeprimidosDocument17 pagesMetanalisis Comparacion de La Eficacia de de La Psicoterapia en Pacientes DeprimidosDulce HerreraNo ratings yet
- A Meta-Analysis of The Effects of Cognitive Therapy in Depressed PatientsDocument14 pagesA Meta-Analysis of The Effects of Cognitive Therapy in Depressed PatientsDragan DjundaNo ratings yet
- Evid Based Mental Health 2001 Therapeutics 82Document2 pagesEvid Based Mental Health 2001 Therapeutics 82Fernanda Avila CastroNo ratings yet
- 2014 TMO en Dolores de Cabeza, Revisión SistemáticaDocument8 pages2014 TMO en Dolores de Cabeza, Revisión Sistemáticaignacio quirogaNo ratings yet
- Jamapsychiatry Breedvelt 2021 Oi 210022 1628043342.75801Document8 pagesJamapsychiatry Breedvelt 2021 Oi 210022 1628043342.75801Jonathan PitreNo ratings yet
- PIIS2215036623002584Document12 pagesPIIS2215036623002584Dr. Nivas SaminathanNo ratings yet
- Managing Antidepressant Discontinuation A Systematic ReviewDocument9 pagesManaging Antidepressant Discontinuation A Systematic ReviewAlejandro Arquillos ÁlvarezNo ratings yet
- May 09 Journals (Mostly) : 63 AbstractsDocument14 pagesMay 09 Journals (Mostly) : 63 AbstractssunkissedchiffonNo ratings yet
- Depresia CazDocument19 pagesDepresia CazBetu SasuNo ratings yet
- BrueraDocument21 pagesBrueraThatiana GimenesNo ratings yet
- Jurnal JiwaDocument6 pagesJurnal JiwaoldDEUSNo ratings yet
- Artigo InglesDocument11 pagesArtigo InglesEllen AndradeNo ratings yet
- Artículo Terapia EsquemasDocument24 pagesArtículo Terapia EsquemasAna Salvador CastellanoNo ratings yet
- Metaanalisis Psicoterapia Resultados PPLDocument20 pagesMetaanalisis Psicoterapia Resultados PPLXavierBilbaoNo ratings yet
- Jamapsychiatry Papola 2023 Oi 230080 1697118575.84256Document11 pagesJamapsychiatry Papola 2023 Oi 230080 1697118575.84256Renan CruzNo ratings yet
- Patients SchizofreniaDocument3 pagesPatients SchizofreniaArinaDogaruNo ratings yet
- And Behavioural Stress Management For Severe Health Anxiety: Internet-Delivered Exposure-Based Cognitive-Behavioural TherapyDocument9 pagesAnd Behavioural Stress Management For Severe Health Anxiety: Internet-Delivered Exposure-Based Cognitive-Behavioural TherapyRoxana MălinNo ratings yet
- A Study of Depression and Anxiety in Cancer Patients PDFDocument34 pagesA Study of Depression and Anxiety in Cancer Patients PDFIrdha Nasta KurniaNo ratings yet
- Jamapsychiatry Stroup 2019 Oi 180113Document8 pagesJamapsychiatry Stroup 2019 Oi 180113opanocayNo ratings yet
- Efficacy For Treatment Anxiety DisordersDocument10 pagesEfficacy For Treatment Anxiety DisordersAnderson GaldinoNo ratings yet
- Depression and Anxiety - 2022 - Gutner - A Pilot Randomized Effectiveness Trial of The Unified Protocol in Trauma ExposedDocument11 pagesDepression and Anxiety - 2022 - Gutner - A Pilot Randomized Effectiveness Trial of The Unified Protocol in Trauma ExposedCristina Alarcón RuedaNo ratings yet
- Sexual and Physical Abuse and Depressive Symptoms in The UK BiobankDocument10 pagesSexual and Physical Abuse and Depressive Symptoms in The UK BiobankDewi NofiantiNo ratings yet
- Experimental Methods Induce Basic EmotionDocument11 pagesExperimental Methods Induce Basic EmotionDewi NofiantiNo ratings yet
- Yoa70030 1115 1122Document8 pagesYoa70030 1115 1122Dewi NofiantiNo ratings yet
- Genetic Developmental DisabilityDocument5 pagesGenetic Developmental DisabilityDewi NofiantiNo ratings yet
- Jurnal 37Document5 pagesJurnal 37Dewi NofiantiNo ratings yet
- Depression and HivDocument6 pagesDepression and HivDewi NofiantiNo ratings yet
- School Child EmotionalDocument15 pagesSchool Child EmotionalDewi NofiantiNo ratings yet
- The Biopsychology of Emotion Current Theoretical eDocument4 pagesThe Biopsychology of Emotion Current Theoretical eDewi NofiantiNo ratings yet
- Neuroinflammation in Schizophrenia - Erlynlimoa - InternasionalDocument5 pagesNeuroinflammation in Schizophrenia - Erlynlimoa - InternasionalDewi NofiantiNo ratings yet
- 1 DiagnosisRosenDSM5NCD AR4Document44 pages1 DiagnosisRosenDSM5NCD AR4Мануель Антоніо Бенавенте ⃝⃤No ratings yet
- Evidence That Neuropsychological de Ficits Following Early Life Adversity May Underlie Vulnerability To DepressionDocument8 pagesEvidence That Neuropsychological de Ficits Following Early Life Adversity May Underlie Vulnerability To DepressionJeanYanNo ratings yet
- 2020 Latest Impact Factor Clarivate Analytics Journal Citation Reports Releaseof JCRThomson ReutersDocument355 pages2020 Latest Impact Factor Clarivate Analytics Journal Citation Reports Releaseof JCRThomson ReutersDewi NofiantiNo ratings yet
- Young People's Trauma-Related Cognitions BeforeDocument12 pagesYoung People's Trauma-Related Cognitions BeforeDewi NofiantiNo ratings yet
- RANZCP Practice ExamDocument50 pagesRANZCP Practice ExamDewi NofiantiNo ratings yet
- Perinatal Depression: A ReviewDocument5 pagesPerinatal Depression: A ReviewDewi NofiantiNo ratings yet
- Perinatal Depression: A ReviewDocument5 pagesPerinatal Depression: A ReviewDewi NofiantiNo ratings yet
- DialoguesClinNeurosci 19 93Document15 pagesDialoguesClinNeurosci 19 93DAVI VIANANo ratings yet
- Var WWW HTML Wp-Content Uploads 2021-02-16131 Postpartum-Mood-Disorders-Diagnosis-Treatment-GuidelinesDocument7 pagesVar WWW HTML Wp-Content Uploads 2021-02-16131 Postpartum-Mood-Disorders-Diagnosis-Treatment-GuidelinesDewi NofiantiNo ratings yet
- Correll 2008Document15 pagesCorrell 2008Dewi NofiantiNo ratings yet
- Molyneaux Et Al-2014-Cochrane Database of Systematic ReviewsDocument4 pagesMolyneaux Et Al-2014-Cochrane Database of Systematic ReviewsDewi NofiantiNo ratings yet
- Oamjms 9t3 288Document6 pagesOamjms 9t3 288Dewi NofiantiNo ratings yet
- JWH 2010 2485Document10 pagesJWH 2010 2485Dewi NofiantiNo ratings yet
- Tuthill 2016Document8 pagesTuthill 2016Dewi NofiantiNo ratings yet
- Article AntipsychoticPolypharmacyPrescDocument9 pagesArticle AntipsychoticPolypharmacyPrescDina IslamiNo ratings yet
- CGJ02Document7 pagesCGJ02Dewi NofiantiNo ratings yet
- CGJ 03Document9 pagesCGJ 03Dewi NofiantiNo ratings yet
- Be Bbing Ton 1999Document7 pagesBe Bbing Ton 1999Dewi NofiantiNo ratings yet
- Cap 2017 0120Document8 pagesCap 2017 0120Dewi NofiantiNo ratings yet
- CGJ01Document8 pagesCGJ01Dewi NofiantiNo ratings yet
- Thiacloprid Draft Assessment ReportDocument109 pagesThiacloprid Draft Assessment ReportTomás Afonso CavacoNo ratings yet
- What Does TOTAPS Stand For? Touch, ObserveDocument4 pagesWhat Does TOTAPS Stand For? Touch, ObserveMohd Shafuan33% (3)
- Mais IndiaDocument12 pagesMais Indiavc_mpNo ratings yet
- The Beauty of DentistryDocument5 pagesThe Beauty of DentistryMorosanu Diana GeorgianaNo ratings yet
- Committee 2020, Reporter, May Edition 2020, April 24, 2020Document32 pagesCommittee 2020, Reporter, May Edition 2020, April 24, 2020ucopresident_2130533No ratings yet
- Maravilla, Dessa Fe N. BSN 3Y1-2S: Health Problem Health-RelatedDocument4 pagesMaravilla, Dessa Fe N. BSN 3Y1-2S: Health Problem Health-RelatedALIANA KIMBERLY MALQUESTONo ratings yet
- A Key To Occlusion: Spencer R. Atkinson, D.D.S Pasadena, CalifDocument17 pagesA Key To Occlusion: Spencer R. Atkinson, D.D.S Pasadena, CalifMazhalai SelvaNo ratings yet
- Five Times Sit To Stand (5Tsts) : InstructionsDocument2 pagesFive Times Sit To Stand (5Tsts) : InstructionsNovinna KusumawatiNo ratings yet
- The Role of Health and Education and Economic Growth of PakistanDocument68 pagesThe Role of Health and Education and Economic Growth of PakistankamilbismaNo ratings yet
- CAS PLAN 2021 TemplateDocument4 pagesCAS PLAN 2021 TemplateTunchanok TrangansriNo ratings yet
- Classroom AbusesDocument6 pagesClassroom AbusesJulius de la CruzNo ratings yet
- 813-Article Text-1261-1-10-20180214Document5 pages813-Article Text-1261-1-10-20180214dwiky ramaNo ratings yet
- Research Methods For The Behavioral Sciences 4th Edition Gravetter Test BankDocument20 pagesResearch Methods For The Behavioral Sciences 4th Edition Gravetter Test Bankmilterjubilatepo8y1b100% (20)
- Chapter 25Document27 pagesChapter 25Kriana RosalesNo ratings yet
- SepsisDocument10 pagesSepsisJessa MaeNo ratings yet
- Positive Intelligence Book (HP Internal Use)Document238 pagesPositive Intelligence Book (HP Internal Use)Ana-Maria NuţăNo ratings yet
- Harvard Referencing Style SpecificDocument16 pagesHarvard Referencing Style SpecificHJames SmithNo ratings yet
- Oral and Naso Pharyngeal SuctioningDocument10 pagesOral and Naso Pharyngeal SuctioningMa. Ferimi Gleam BajadoNo ratings yet
- Presentation PathophysiologyDocument11 pagesPresentation PathophysiologyJade DeopidoNo ratings yet
- Laboratory Test Report: Test Name Result Serum HCG (Human Chorionic Gonadotropin)Document1 pageLaboratory Test Report: Test Name Result Serum HCG (Human Chorionic Gonadotropin)rbitNo ratings yet
- Chest Wall DeformitiesDocument25 pagesChest Wall DeformitiesRaghu NadhNo ratings yet
- Rajiv Gandhi University of Health Sciences, Bangalore, KarnatakaDocument13 pagesRajiv Gandhi University of Health Sciences, Bangalore, KarnatakaAmit TamboliNo ratings yet
- The PACE Trial: Radiotherapy Planning and Delivery Guidelines (Pace-A and Pace-C)Document33 pagesThe PACE Trial: Radiotherapy Planning and Delivery Guidelines (Pace-A and Pace-C)Анастасия АнохинаNo ratings yet
- Risk Assessment No. 42 WORKING OVER-SIDE Rev. 02 28.12.09Document2 pagesRisk Assessment No. 42 WORKING OVER-SIDE Rev. 02 28.12.09Devi Ratna Pratiwi80% (5)
- Master Youtube: WorkbookDocument64 pagesMaster Youtube: WorkbookLucian TrandafirNo ratings yet
- Efficacy of The Combination of Teriparatide Andn Denosumab in The Treatment of Postmenopausal SymptomsDocument11 pagesEfficacy of The Combination of Teriparatide Andn Denosumab in The Treatment of Postmenopausal Symptomsitsjustmee03No ratings yet
- Fire Stop Final Inss2460 Inss2460 Us en Sds 180808Document7 pagesFire Stop Final Inss2460 Inss2460 Us en Sds 180808Jamile Santos AraujoNo ratings yet
- Fundamentals Mt1 Nov 2023Document16 pagesFundamentals Mt1 Nov 2023Rika MaeNo ratings yet
- Neil HillDocument32 pagesNeil HillAndrés Felipe100% (1)
- Discharge PlanDocument9 pagesDischarge PlanRheynel NietesNo ratings yet