Professional Documents
Culture Documents
N-WPS Office
Uploaded by
Norhani Panayaman0 ratings0% found this document useful (0 votes)
16 views4 pagesThe spread of COVID-19 has affected the world. While vaccines may not fully protect against COVID-19, vaccination is an important public health intervention as it can help prevent transmission and control deaths. However, vaccine hesitancy, where some people are reluctant or refuse vaccines even when they are available, has become a global concern for COVID-19 vaccines as well as other vaccines. Vaccine hesitancy is influenced by various socioeconomic, psychological, and contextual factors and presents a barrier to successful vaccination programs. To address vaccine hesitancy, health workers and policymakers need to understand its underlying causes in different populations and contexts.
Original Description:
Effec
Original Title
n-WPS Office
Copyright
© © All Rights Reserved
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe spread of COVID-19 has affected the world. While vaccines may not fully protect against COVID-19, vaccination is an important public health intervention as it can help prevent transmission and control deaths. However, vaccine hesitancy, where some people are reluctant or refuse vaccines even when they are available, has become a global concern for COVID-19 vaccines as well as other vaccines. Vaccine hesitancy is influenced by various socioeconomic, psychological, and contextual factors and presents a barrier to successful vaccination programs. To address vaccine hesitancy, health workers and policymakers need to understand its underlying causes in different populations and contexts.
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views4 pagesN-WPS Office
Uploaded by
Norhani PanayamanThe spread of COVID-19 has affected the world. While vaccines may not fully protect against COVID-19, vaccination is an important public health intervention as it can help prevent transmission and control deaths. However, vaccine hesitancy, where some people are reluctant or refuse vaccines even when they are available, has become a global concern for COVID-19 vaccines as well as other vaccines. Vaccine hesitancy is influenced by various socioeconomic, psychological, and contextual factors and presents a barrier to successful vaccination programs. To address vaccine hesitancy, health workers and policymakers need to understand its underlying causes in different populations and contexts.
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 4
n
The spread of coronavirus disease 2019 (COVID-19) has
affected the worldwide (1–3). Although vaccines may not
fully protect from the COVID-19, it is one of the most
important public health interventions as the full range of
vaccination among community people can help protect from
transmission of infection from the infected to the uninfected and
control potential death (4–9). While herd immunity achieved
with vaccination is a potential public health intervention
against COVID-19, vaccine hesitancy (i.e., reluctance in vaccine
acceptance or even delays in refusal amidst the availability
of safety- and effectiveness-assured vaccination facilities) has
become a global public health concern (4–10). COVID-19
vaccine acceptance or hesitancy, like in the case of other
vaccines, is context-specific, varying across the country, time,
and place (8) due to socio-demographic differences, health
conditions, individual cognitive, psychological and behavioral
factors, awareness about vaccines’ safety, effectiveness and
potential side effects, fast development compared to other
vaccines, perceived lack of testing, control of myths, confidence
in the health system, and political and cultural factors. Since
vaccine hesitancy plays a significant barrier to successful
vaccination campaigns, the availability of COVID-19 vaccines
does not solve the issue (4, 7, 11–13). Also, Covid vaccine
hesitancy reflected an interesting public perception that it rose
significantly when new and deadly variants emerged (14). Hence,
health workers and policymakers should address the root cause
of hesitancy to successfully make the global vaccine action plan
(11, 13). The SAGE Working Group on Vaccine Hesitancy
concluded that vaccine hesitancy refers to “delay in acceptance or
refusal of vaccination despite availability of vaccination services.
Vaccine hesitancy is complex and context-specific, varying across
time, place, and vaccines.” Vaccine hesitancy is influenced
by factors such as complacency, convenience, and confidence
(15). Vaccine hesitancy is usually guided by three major
factors: individuals’ perception toward all vaccination programs,
including COVID-19 vaccine peers’ influence, and perceived
behavioral control (7).
Some people may initially show hesitancy due to less
awareness about vaccination, cost implications, and poor or
substandard health literacy, but later may be interested after
Frontiers in Public Health 02 frontiersin.org
You might also like
- COVID-19 Vaccine Brand Hesitancy and Other Challenges To Vaccination in The Philippines - PLOS Global Public HealthDocument15 pagesCOVID-19 Vaccine Brand Hesitancy and Other Challenges To Vaccination in The Philippines - PLOS Global Public Healthprincess catherine PabellanoNo ratings yet
- Concept Paper For Academic ResearchDocument9 pagesConcept Paper For Academic ResearchMarah Anngelieh TubbaliNo ratings yet
- 13th R.LDocument9 pages13th R.LWilliam Tac anNo ratings yet
- Hesitancy in co-WPS OfficeDocument6 pagesHesitancy in co-WPS OfficeNorhani PanayamanNo ratings yet
- Factors Influencing Public Attitudes Towards COVID-19 Vaccination: A Scoping Review Informed by The Socio-Ecological ModelDocument27 pagesFactors Influencing Public Attitudes Towards COVID-19 Vaccination: A Scoping Review Informed by The Socio-Ecological ModelneneNo ratings yet
- Vaccine Willing-WPS OfficeDocument14 pagesVaccine Willing-WPS OfficeNorhani PanayamanNo ratings yet
- Theoretical FrameworkDocument2 pagesTheoretical FrameworkljgerzonNo ratings yet
- Chelsey (Chapter 2 RRL) LocalDocument3 pagesChelsey (Chapter 2 RRL) LocalChester ArenasNo ratings yet
- Summary of Guidance For Minimizing The Impact of COVID-19 On Individual Persons, Communities, and Health Care Systems - United States, August 2022Document8 pagesSummary of Guidance For Minimizing The Impact of COVID-19 On Individual Persons, Communities, and Health Care Systems - United States, August 2022PANAMA GREEN BUILDING COUNCILNo ratings yet
- ABSTRACTDocument12 pagesABSTRACTAnaliza Dumangeng GuimminNo ratings yet
- Restoring Confidence in Vaccines in The COVID-19 Era: Expert Review of VaccinesDocument4 pagesRestoring Confidence in Vaccines in The COVID-19 Era: Expert Review of VaccinesRaquel CostaNo ratings yet
- What Promotes Cognitive Dissonance Among Anti-Vaccine Members in Indonesia?Document12 pagesWhat Promotes Cognitive Dissonance Among Anti-Vaccine Members in Indonesia?IJPHSNo ratings yet
- May Be hindered-WPS OfficeDocument7 pagesMay Be hindered-WPS OfficeNorhani PanayamanNo ratings yet
- The Impact of Social Media On People Acceptance e of The COVID-19 Vaccine in EgyptDocument20 pagesThe Impact of Social Media On People Acceptance e of The COVID-19 Vaccine in Egyptmohamed elemamNo ratings yet
- 1 s2.0 S2666535222000349 MainDocument7 pages1 s2.0 S2666535222000349 Mainشهد موسىNo ratings yet
- The Vaccine Uptake Continuum: Applying Social Science Theory To Shift Vaccine HesitancyDocument5 pagesThe Vaccine Uptake Continuum: Applying Social Science Theory To Shift Vaccine HesitancyKitKath UwUNo ratings yet
- Hesitancy Towards A COVID-19 Vaccine and Prospects For Herd ImmunityDocument51 pagesHesitancy Towards A COVID-19 Vaccine and Prospects For Herd ImmunityA009Karin Kurniati NurfatmahNo ratings yet
- Ijerph 19 11656 v2Document8 pagesIjerph 19 11656 v2agent purpleNo ratings yet
- Acceptance of COVID-19 Vaccination During The COVID-19 Pandemic in ChinaDocument14 pagesAcceptance of COVID-19 Vaccination During The COVID-19 Pandemic in ChinaMark Nel NuñezNo ratings yet
- DISCUSSION-WPS OfficeDocument11 pagesDISCUSSION-WPS OfficeNorhani PanayamanNo ratings yet
- KSLING1Document5 pagesKSLING1Clarita BangunNo ratings yet
- Argumentative EssayDocument2 pagesArgumentative Essayjoyce anne GarciaNo ratings yet
- Vaccine Hesitancy Vaccines-09-00160Document14 pagesVaccine Hesitancy Vaccines-09-00160Sundus ShehzadNo ratings yet
- CDC Streamlines COVID-19 GuidanceDocument9 pagesCDC Streamlines COVID-19 GuidanceJessica A. BotelhoNo ratings yet
- COVID-19 Vaccine Hesitancy Among The University Students and PersonnelDocument9 pagesCOVID-19 Vaccine Hesitancy Among The University Students and PersonnelIJPHSNo ratings yet
- COVID-19 Vaccination Intention and Vaccine Characteristics Influencing Vaccination Acceptance: A Global Survey of 17 CountriesDocument14 pagesCOVID-19 Vaccination Intention and Vaccine Characteristics Influencing Vaccination Acceptance: A Global Survey of 17 CountriesManasi PandaNo ratings yet
- Paper RemoladoDocument57 pagesPaper RemoladoJan Michael R. RemoladoNo ratings yet
- Patient Education and Counseling: Haoran Chu, Sixiao LiuDocument9 pagesPatient Education and Counseling: Haoran Chu, Sixiao LiuamalliaNo ratings yet
- Final PaperDocument44 pagesFinal PaperForshia Antonette BañaciaNo ratings yet
- Knowledge and Acceptance of Covid 19 Vaccine Among Nursing Students in Riverside CollegeDocument2 pagesKnowledge and Acceptance of Covid 19 Vaccine Among Nursing Students in Riverside CollegeGLORYLYN ECHOGANo ratings yet
- CHAPTER 1-WPS OfficeDocument5 pagesCHAPTER 1-WPS OfficeAbdulrahman Abarani AdamNo ratings yet
- Review of Related LiteratureDocument18 pagesReview of Related LiteratureAllaiz g.No ratings yet
- Research PaperDocument3 pagesResearch PaperKeitu QuijalvoNo ratings yet
- Psychological, Social, and Situational Factors Associated With COVID-19 Vaccination Intentions: A Study of UK Key Workers and Non-Key WorkersDocument17 pagesPsychological, Social, and Situational Factors Associated With COVID-19 Vaccination Intentions: A Study of UK Key Workers and Non-Key WorkersMónika MikeNo ratings yet
- A Research Proposal On Whether The CovidDocument6 pagesA Research Proposal On Whether The CovidDanielNo ratings yet
- Factors Associated With COVID-19 Vaccine HesitancyDocument14 pagesFactors Associated With COVID-19 Vaccine HesitancyksmidhilaNo ratings yet
- 3rd R.LDocument14 pages3rd R.LWilliam Tac anNo ratings yet
- COVID-19 Vaccine Hesitancy inDocument13 pagesCOVID-19 Vaccine Hesitancy inneneng darliah hermawan putriNo ratings yet
- Healthcare 11 00461 v2 PDFDocument13 pagesHealthcare 11 00461 v2 PDFFaye ToqueroNo ratings yet
- Vaccine Hesitancy and MisinformationDocument2 pagesVaccine Hesitancy and MisinformationJulia Ysabel SañaganNo ratings yet
- Chapter 1 3Document36 pagesChapter 1 3MaximusNo ratings yet
- Aoun Et Al, 2021Document8 pagesAoun Et Al, 2021Oren KatzNo ratings yet
- The Nature and Extent of COVID 19 Vaccination Hesitancy in Healthcare WorkersDocument8 pagesThe Nature and Extent of COVID 19 Vaccination Hesitancy in Healthcare WorkersamiryahiaNo ratings yet
- Review of Related Literature: COVID-19Document17 pagesReview of Related Literature: COVID-19Ed Anthony YubacNo ratings yet
- RRL VaccineDocument6 pagesRRL VaccineAlexandra Mae D. MiguelNo ratings yet
- Badr DKK 2021Document17 pagesBadr DKK 2021WoogyuNo ratings yet
- Chapter I-1Document3 pagesChapter I-1Secret AdmirerNo ratings yet
- Org ArabDocument13 pagesOrg Arabandros 77No ratings yet
- C ECH en Group ActivityDocument3 pagesC ECH en Group ActivitySebastianNo ratings yet
- Final Requirement (FINAL EXAM)Document4 pagesFinal Requirement (FINAL EXAM)KATHLEEN JOSOLNo ratings yet
- Vaccine HesitancyDocument12 pagesVaccine HesitancyMhd HidayattullahNo ratings yet
- Degree of Acceptance of Residents Barangay Bibincahan To Vaccination Program of The Philippine GovernmentDocument24 pagesDegree of Acceptance of Residents Barangay Bibincahan To Vaccination Program of The Philippine GovernmentRJ DealcaNo ratings yet
- Preprints202104 0702 v1Document13 pagesPreprints202104 0702 v1JicelleNo ratings yet
- RESEARCH 1 Fi 2Document20 pagesRESEARCH 1 Fi 2Alondra SagarioNo ratings yet
- Acp Statement On Global Covid-19 Vaccine Distribution and Allocation On Being Ethical and Practical 2021Document3 pagesAcp Statement On Global Covid-19 Vaccine Distribution and Allocation On Being Ethical and Practical 2021Suleymen Abdureman OmerNo ratings yet
- My ProjectDocument38 pagesMy ProjectfaizamuhammadaligmlNo ratings yet
- Individual Preferences For COVID-19 Vaccination in ChinaDocument17 pagesIndividual Preferences For COVID-19 Vaccination in ChinaAntonio MoncayoNo ratings yet
- Introduction of VaccineDocument6 pagesIntroduction of VaccineIkra MemonNo ratings yet
- Title: The Acceptance and Attitudes of Students Toward Covid-19 VaccineDocument5 pagesTitle: The Acceptance and Attitudes of Students Toward Covid-19 VaccineJoanah Nichole TinoyNo ratings yet
- Ction Also incr-WPS OfficeDocument7 pagesCtion Also incr-WPS OfficeNorhani PanayamanNo ratings yet
- Hypothesis (H8) - WPS OfficeDocument4 pagesHypothesis (H8) - WPS OfficeNorhani PanayamanNo ratings yet
- DISCUSSION-WPS OfficeDocument11 pagesDISCUSSION-WPS OfficeNorhani PanayamanNo ratings yet
- Makers managed-WPS OfficeDocument9 pagesMakers managed-WPS OfficeNorhani PanayamanNo ratings yet
- Is The deadlies-WPS OfficeDocument8 pagesIs The deadlies-WPS OfficeNorhani PanayamanNo ratings yet
- May Be hindered-WPS OfficeDocument7 pagesMay Be hindered-WPS OfficeNorhani PanayamanNo ratings yet
- Parents Consent-Wps OfficeDocument1 pageParents Consent-Wps OfficeNorhani PanayamanNo ratings yet
- Factors influen-WPS OfficeDocument6 pagesFactors influen-WPS OfficeNorhani PanayamanNo ratings yet
- Vaccine Willing-WPS OfficeDocument14 pagesVaccine Willing-WPS OfficeNorhani PanayamanNo ratings yet
- Studies On COVI-WPS OfficeDocument8 pagesStudies On COVI-WPS OfficeNorhani PanayamanNo ratings yet
- On January 30,-WPS OfficeDocument10 pagesOn January 30,-WPS OfficeNorhani PanayamanNo ratings yet
- Vaccine develop-WPS OfficeDocument9 pagesVaccine develop-WPS OfficeNorhani PanayamanNo ratings yet
- Interview-Questions (ADNOC LNG)Document19 pagesInterview-Questions (ADNOC LNG)Chen XinNo ratings yet
- Angela Shrestha - Written Assessment AnswersDocument3 pagesAngela Shrestha - Written Assessment AnswersAngela ShresthaNo ratings yet
- FAO Ethiopia - Desert Locust Situation UpdateDocument2 pagesFAO Ethiopia - Desert Locust Situation UpdateOsman HassenNo ratings yet
- TOK SampleDocument5 pagesTOK SampleLucianna CheilasNo ratings yet
- Scandinavian Med Sci Sports - 2023 - Nuzzo - Overview of Muscle Fatigue Differences Between Maximal Eccentric andDocument15 pagesScandinavian Med Sci Sports - 2023 - Nuzzo - Overview of Muscle Fatigue Differences Between Maximal Eccentric andcsrpirataNo ratings yet
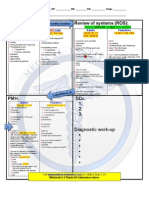
- NCP Head and NeckDocument2 pagesNCP Head and NeckKristine Angie RamosNo ratings yet
- Sonography ProjectDocument9 pagesSonography Projectapi-685351719No ratings yet
- Intraosseous Infusion: by Chisupa EricDocument20 pagesIntraosseous Infusion: by Chisupa EricericNo ratings yet
- Bupa Arabia Health Insurance Company Vs Enaya Health Insurance CompanyDocument7 pagesBupa Arabia Health Insurance Company Vs Enaya Health Insurance CompanygeofreyNo ratings yet
- Linezolid Update. Stable in Vitro Activity Following More Than A Decade PDFDocument12 pagesLinezolid Update. Stable in Vitro Activity Following More Than A Decade PDFsilvia mendez riveraNo ratings yet
- Compatibility and Stability of Diazepam InjectionDocument4 pagesCompatibility and Stability of Diazepam InjectionHanunNo ratings yet
- Q3 WK 3 and 4 Learning Activity Sheets in Plumbing 2021 For 10 and 12Document4 pagesQ3 WK 3 and 4 Learning Activity Sheets in Plumbing 2021 For 10 and 12Mary Rose Hibaya100% (1)
- (Personal Trainer) Justin Price - The Biomechanics Method For Corrective Exercise (2019)Document449 pages(Personal Trainer) Justin Price - The Biomechanics Method For Corrective Exercise (2019)Gustavo Javier Caraballo PeñaNo ratings yet
- SAMDocument108 pagesSAMAlimyon Abilar MontoloNo ratings yet
- Form 4.2 Evidence of Current CompetenciesDocument5 pagesForm 4.2 Evidence of Current CompetenciesvayaNo ratings yet
- A - Pratic Guide Pediatric Wound CareDocument9 pagesA - Pratic Guide Pediatric Wound CareLicia GabrielleNo ratings yet
- Surveying Lab Manual 21cv32 - 2022Document82 pagesSurveying Lab Manual 21cv32 - 2022Tamil Selvi CIVILNo ratings yet
- Going Green With Eco-Friendly Dentistry: Review ArticleDocument4 pagesGoing Green With Eco-Friendly Dentistry: Review ArticleHR LaloNo ratings yet
- MSDS For PVC GlovesDocument2 pagesMSDS For PVC GlovesSebastian CantilloNo ratings yet
- Overseas Registration Exam Application: Dentists Holding Dental Degrees From Outside The UK and EEADocument21 pagesOverseas Registration Exam Application: Dentists Holding Dental Degrees From Outside The UK and EEAPamungkas Dhani100% (2)
- CS Blue Sheet Mnemonics - USMLE Step 2 CS - WWW - MedicalDocument1 pageCS Blue Sheet Mnemonics - USMLE Step 2 CS - WWW - MedicalRavi Parhar75% (4)
- Đề số 1Document5 pagesĐề số 1Thúy NgânNo ratings yet
- Cholinergic Urticaria - Google SearchDocument1 pageCholinergic Urticaria - Google SearchStephanie NhyiraNo ratings yet
- Community Health Planning, Implementation, and EvaluationDocument9 pagesCommunity Health Planning, Implementation, and EvaluationKarl Angelo MontanoNo ratings yet
- Monsieur Pain Roberto BolanoDocument12 pagesMonsieur Pain Roberto BolanoJoseph_McIwan18No ratings yet
- Endo-Perio Dilemma A Brief ReviewDocument10 pagesEndo-Perio Dilemma A Brief ReviewLuisNo ratings yet
- Contoh Judul Jurnal Kesehatan InternasionalDocument3 pagesContoh Judul Jurnal Kesehatan Internasionalnadya100% (1)
- Case Study On Status AsthmaticusDocument129 pagesCase Study On Status AsthmaticusLouie MansaNo ratings yet
- Guide To Nutrigenomic TestingDocument34 pagesGuide To Nutrigenomic Testinggiannidiet100% (1)
- 2ed Y2 72-73 3-9 Hypotheses and SignificanceDocument1 page2ed Y2 72-73 3-9 Hypotheses and SignificancejNo ratings yet