Professional Documents
Culture Documents
Bonus - C.P.E - Pregnancy and Lactation
Uploaded by
ali mohammedOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bonus - C.P.E - Pregnancy and Lactation
Uploaded by
ali mohammedCopyright:
Available Formats
C P E Program [PREGNANCY & LACTATION]
Continuing pharmaceutical education (CPE)
program
Alexandria Syndicate of pharmacists
Pregnancy & lactation
Prepared by :
Ph/Esraa nader
Ph/Omnia Abdelrahman
Presented by:
Ph/Ahmed El-Gewily
Alex syndicate of pharmacists Page 1
C P E Program [PREGNANCY & LACTATION]
Pregnancy and lactation
Introduction
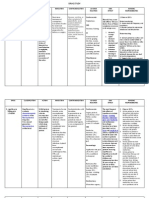
Critical periods in human development
Alex syndicate of pharmacists Page 2
C P E Program [PREGNANCY & LACTATION]
Pharmacokinetics in pregnancy
Physiological changes in pregnancy, beginning during the first trimester, and most
marked during the third trimester; alter the absorption, distribution and clearance of
drugs.
Absorption
Gastric emptying and small intestine motility are reduced in pregnancy due to
elevation of progesterone. This may increase Tmax and reduce Cmax, although
effects on total bioavailability may be relatively minor.
An increase in gastric pH, due to a reduction in H. secretion and an increase in
mucus production may increase the ionization of weak acids, tending to reduce
their absorption more than that of weak bases.
They may, however, reduce the efficacy of a single dose of an oral drug such as
an analgesic or anti-emetic for which Tmax and Cmax are important.
Distribution
During pregnancy there is an expansion of intravascular (plasma volume)
and extra- vascular (breasts, uterus, peripheral edema) water content.
Thus, total body water increases by up to 8 liters, creating a larger space
within which hydrophilic drugs may distribute, i.e. increasing Vd.
Total plasma concentration of albumin-bound drugs decreases as a result of
haemodilution. There is thus the possibility of a rise in free (active) drug
concentration of agents that are normally albumin-bound. This would be
expected to produce an increased drug effect.
distribution for lipophilic drugs, but this has little practical importance.
Alex syndicate of pharmacists Page 3
C P E Program [PREGNANCY & LACTATION]
Metabolism
Some enzymes of the hepatic cytochrome P-450 system are induced by oestrogen/
progesterone, resulting in a higher rate of metabolism (and hence elimination) of
drugs, for example, phenytoin.
Clearance of drugs, such as rifampicin, that are secreted via the biliary system, may
be attenuated due to the cholestatic property of oestrogen.
Elimination
Renal blood flow is increased by 60-80% during pregnancy, and glomerular
normally excreted unchanged, for example, penicillin and digoxin.
Elimination from the fetus is by diffusion back to the maternal com- partment.
Because most drug metabolites are polar, this favours accumulation of
metabolites within the fetus.
FDA pregnancy categories
Category A
Controlled studies in women fail to demonstrate a risk to the
fetus in the first trimester (and there is no evidence of a risk in later trimesters),
and the possibility of fetal harm appears remote.
Category B
Either animal-reproduction studies have not demonstrated a fetal risk but there are no
controlled studies in pregnant women, or animal-reproduction studies have shown an
adverse effect (other than a decrease in fertility) that was not confirmed in controlled
studies in women in the first trimester (and there is no evidence of a risk in later
trimesters).
Category C
Either study in animals has revealed adverse effects on the fetus (teratogenic or
embryocidal or other) and there are no controlled studies in women, or studies in
Alex syndicate of pharmacists Page 4
C P E Program [PREGNANCY & LACTATION]
women and animals are not available. Drugs should be given only if the potential
benefit justifies the potential risk to the fetus.
Category D
There is positive evidence of human fetal risk, but the benefits from use in pregnant
women may be acceptable despite the risk (e.g., if the drug is needed in a life-
threatening situation or for a serious disease for which safer drugs cannot be used or
are ineffective).
Category X
Studies in animals or human beings have demonstrated fetal abnormalities, or there is
evidence of fetal risk based on human experience or both, and the risk of the use of
the drug in pregnant women clearly outweighs any possible benefit. The drug is
contraindicated in women who are or may become pregnant.
Specific drug therapy during pregnancy and lactation
1} headache, migraine & fever
Chronic tension-type headaches often respond to reIaxation exercises and
physical therapy that emphasizes stretching and strengthening of head and neck
muscles.
General treatment measures for migraine include maintaining a regular sleeping
and eating schedule, and practicing methods for coping with stress. Some patients
with migraines benefit from use of ice (ice bags or cold packs) combed with pressure
applied to the forehead to reduce pain associated with acute migraine attack.
Paracetamol/acetaminophen , perhaps combined with caffeine(Panadol® Extra
tab.) is the analgesic and antipyretic of choice.
It can be used at usual dosages and at any stage of pregnancy; paracetamol belongs to
the group of analgesics of choice during breastfeeding.
Dose : Oral(Abimol® tab. ,Tylenol® cap.) , rectal (Acetaminophen® supp.): 325-650 mg
every 4-6 hours or 1000 mg 3-4times/day; do not exceed 4 g/day
Alex syndicate of pharmacists Page 5
C P E Program [PREGNANCY & LACTATION]
Pregnancy risk factor: B
Lactation:
Excreted into milk in small amounts.
Safe in breast feeding but reported single case of maculopapular rash in
exposed infants.
I.V. (Perfalgan® vial):
<50 kg: 15 mg/kg every 6 hours or 12.5 mg/kg every 4 hours; maximum single dose:
750 mg/dose; maximum daily dose: 75 mg/kg/day (≤3.75 g/day)
≥50 kg: 650 mg every 4 hours or 1000 mg every 6 hours; maximum single dose: 1000
mg/dose; maximum daily dose: 4 g/day
Patient Education
Oral: Take with food or milk. While using this medication, do not use other
prescription or OTC medications that contain acetaminophen. This medication will not
reduce inflammation; consult prescriber for anti-inflammatory, if needed.
Pregnancy Risk Factor : C (intravenous)
Lactation: Excretion in breast milk unknown/use caution.
Aspirin is the analgesic and antipyretic of second choice in pregnancy, but this
should not be used from the early third trimester onwards.
Dose: Analgesic and antipyretic:
Oral (Aspocid® tab., chew.tab,): 75-100mg once daily
Pregnancy risk factor: C. Low dose may be used with caution during first and second
trimester. Alternatives should be considered for analgesia. Use not recommended
during third trimester.
Alex syndicate of pharmacists Page 6
C P E Program [PREGNANCY & LACTATION]
Lactation: Enters breast milk
Patient Education
Take with food or milk. The pharmacist should advise patient to stop taking aspirin if
patient experienced ringing in ears, persistent stomach pain, unresolved nausea or
vomiting, respiratory difficulty or shortness of breath, unusual bruising or bleeding
(mouth, urine, stool), or skin rash.
Because of the lack of experience with these substances during pregnancy and
breastfeeding, selective COX-2 inhibitors should be avoided.
Ibuprofen can also be considered, but this should not be used from the early third
trimester onwards.
Dose: Analgesic, antipyretic: Oral (Brufen® tab.): 200-400 mg/dose every 4-6 hours
(maximum daily dose: 1.2 g, unless directed by physician; under physician supervision
daily doses ≤2.4 g may be used)
Pregnancy Risk Factor: C/D ≥30weeks gestation
Lactation : Enters breast milk / not recommended.
Patient Education
prescriber. Take with food or milk.
ketoprofen: pregnancy category B & excreted in breast milk.
Diclofenac: pregnancy category B(The risk category will be D only if used in 3rd
trimester or near delivery) & considered safe in breast feeding
Indomethacin : category B (The risk category will be D only if used longer than 48
Alex syndicate of pharmacists Page 7
C P E Program [PREGNANCY & LACTATION]
Lactation :
Considered safe in breast feeding.
Reported single case of seizures in exposed infants.
Other members mostly category C
If necessary, antiemetics like dimenhydinate, meclizine or metoclopramide should
be given prior to analgesics.
To prevent dehydration, intravenous (i.v.) fluids should be given.
2} Cough:
1-productive cough
N-acetylcysteine, ambroxol and bromhexine are first choice mucolytics during
pregnancy and breastfeeding.
Ambroxol: Dosage Range:
-Oral (Ambroxol® tab., cap.): 60-120 mg/day in 2 divided doses
-In patients with gastric ulceration relative caution should be observed.
Bromhexine: Dosage Range:
-Oral (Bisolvon® tab., drops, syrup): 8-16 mg 3times/day
Iodine-containing mucolytics are contraindicated during lactation and pregnancy,
especially after the first trimester as it may suppress fetal thyroid function.
Carbocisteine (mucolytic) and guaifenesin (expectorant) should be avoided
because of the limited available data.
2- Non-productive cough
In the case of persistent dry cough, codeine and dextromethorphan can be given
in all trimesters of pregnancy and during lactation. Higher doses given for longer
Alex syndicate of pharmacists Page 8
C P E Program [PREGNANCY & LACTATION]
periods, or use near delivery, can cause neonatal withdrawal symptoms and
respiratory depression.
Dextromethorphan :Dosage range:
Oral (Codilar® syrup): 10-20 mg every 4 hours or 30 mg every 6-8 hours; extended
release: 60 mg twice daily; maximum: 120 mg/day
3} Common cold & flu:
Safe & recommended
Acetaminophen
Warm salt/water gargle
Saline nasal drops (Otrivine baby saline ®: 1 drop 3- ) or spray
Most NSAIDs are not preferred during pregnancy and lactation
Diclofenac & ketoprofen: category B
Indomethacin : category B (The risk category will be D only if used longer
Other members mostly category C
The systemic use of ephedrine and other sympathomimetics should be
avoided during pregnancy & lactation
First- -blockers like chlorpheniramine and
dexchlorpheniramine, can be used during pregnancy for the treatment of
allergic conditions.
4} Allergic rhinitis & ashma:
The commonly used drugs for the treatment of asthma do not pose a risk to pregnant
women. These drugs are:
Alex syndicate of pharmacists Page 9
C P E Program [PREGNANCY & LACTATION]
The drugs of first choice during pregnancy:
1-Inhaled selective, short-acting β2-adrenergic agonists Such as salbutamol
(albuterol) and terbutaline.
According to therapy guidelines, their use by inhalation is preferred. The dose may
need to be adjusted. The long- -agonists formoterol and salmeterol should
only be used if they are essential to an optimal treatment.
Salbutamol
(Ventolin® evohaler 100 µgm / actuation , Farcolin®
Patient education:
• Reliever for asthma: can be used to treat an acute attack.
• Inhalation devices should be primed before first use and again if device not used
for two weeks.
• If using salbutamol, ipratropium (or formoterol or
salmeterol) and steroid inhalers, use in that order.
• Can cause tachycardia, tremor and electrolyte disturbances.
• Encourage the development of an asthma management plan.
• If previously effective dose fails to provide at least three hours' relief, seek
medical advice.
• Counsel on technique (spacer, face mask, nebuliser).
• Increasing use to control symptoms indicates deterioration of asthma control;
treatment should be re-assessed.
required.
• Nebuliser solution is stable for one hour once mixed with sodium cromoglycate
or ipratropium.
Pregnancy: C
Breastfeeding: Excretion in breast milk unknown/use caution.
Terbutaline
(Aironyl® tab. ,syrup)
Patient education:
Reliever for asthma or chronic obstructive pulmonary disease; can be used to
treat an acute attack.
• If using terbutaline, ipratropium (or eformoterol,
salmeterol) and steroid inhalers, use in that order.
• Can cause tachycardia, tremor and electrolyte disturbances.
Alex syndicate of pharmacists Page 10
C P E Program [PREGNANCY & LACTATION]
• Encourage the development of an asthma plan.
• Increased reliance on short-acting beta-agonists indicates deterioration of
asthma control; treatment should be reassessed.
Pregnancy: B
Breastfeeding: Enters beast milk/ compatible.
Salmeterol
(Metrovent® 200 doses inhaler 25mg/ dose)
Patient education:
Do not use to treat an acute asthma attack.
• Use regularly, usually twice a day or at least
30 minutes before exercise.
• Encourage the development of an asthma management plan.
• Increased reliance on short-acting beta-agonists indicates deterioration of
asthma control; treatment should be re-assessed.
• Can cause tachycardia and tremor.
• Provide advice on inhaler/accuhaler technique.
• Recommend use of a spacer with an inhaler.
Pregnancy: C
Breastfeeding: Enters breast milk/use caution.
Formoterol
(Berotec® 200 inhaler , Foradil® 12 µgm inh. Cap.)
Patient education:
May be used for symptom relief in patients already receiving inhaled
corticosteroids and regular
formoterol or in combination with budesonide.
• Long acting—use twice a day.
• If paradoxical bronchospasm occurs, seek medical advice.
• May cause tachycardia or tremor.
• Review delivery device technique.
• Counsel on cleaning and disposal of device.
Pregnancy: C
Breastfeeding: Excretion in breast milk unknown/use caution
Alex syndicate of pharmacists Page 11
C P E Program [PREGNANCY & LACTATION]
2-inhaled corticosteroids:
The use of beclomethasone or budesonide is preferred, because these have been
widely used in pregnancy and have a good safety record. Systemic use of the
corticosteroids, prednisone, and its metabolite, prednisolone, is indicated in case of
acute exacerbations of asthma or severe asthma during pregnancy.
For allergic rhinitis, intranasal corticoids may be used.
(Miflonide ® )
Pregnancy risk factor: B
Lactation: Enters breast milk/ use caution.
Patient Education
May take 1-2 weeks or longer before full effects are seen.
Inhaled anticholinergics:
Inhaled ipratropium bromide can be used during pregnancy and breastfeeding if
needed.
Patient education:
If using salbutamol or terbutaline, ipratropium and steroid inhalers, use in that order.
• Not for immediate relief of symptoms, dry mouth common.
• Can be mixed with other beta2 agonists for
nebulised therapy.
• Inquire about eye and vision problems as some may be caused by leakage from
mask.
Changes to urinary system: May induce or aggravate overflow incontinence
(occasionally with nebulised therapy) due to reduced detrusor activity, voiding
difficulty, urinary retention, constipation.
Pregnancy: B.
Breastfeeding: Excretion in breast milk unknown/use caution
Systemic theophylline:
Alex syndicate of pharmacists Page 12
C P E Program [PREGNANCY & LACTATION]
Theophylline may be used during pregnancy and beastfeeding for cases where the
inhaled β2-agonists and corticosteroids are insufficient to control the asthmatic
diseases.
Steady-state serum concentrations should be closely monitored, and
maintained at 8–12 μg/ml.
Theophylline is a medicine of low therapeutic index so monitoring of
plasma theophylline concentration is advisable.
If nausea, palpitations, insomnia, headache or gastrointestinal upsets are
experienced, seek medical advice.
(Quibron-T SR® 300mg tab. , Minophylline® 500mg / 5ml amp.)
Changes to faeces: Black discolouration.
Pregnancy: C
Breastfeeding: Enters breast milk/ compatible.
Mast cell stabilizers:
Inhaled cromoglycic acid (sodium cromoglycate) :
Sodium cromoglycate can be safely used in pregnant woman and lactating mother for
the prophylactic treatment of allergic diseases such as asthma and allergic rhinitis.
The use of mast cell inhibitors such as ketotifen, and azelastine should be
avoided during pregnancy.
Antileukotrienes:
Apart from selected cases, antileukotrienes should be avoided in pregnant women.
As the best studied second-generation antihistamine, loratadine can be used
during pregnancy for the treatment of allergic conditions. Cetirizine could be an
acceptable second choice.
Loratadine : Dosing range : Oral (Loratan® tab.): 10 mg/day
Patient Education
You may experience drowsiness, dizziness, dry mouth, or nausea. Report persistent
dizziness or sedation; swelling of face, mouth, lips, or tongue; respiratory difficulty;
lack of improvement; or worsening of condition.
Alex syndicate of pharmacists Page 13
C P E Program [PREGNANCY & LACTATION]
Breast-Feeding Considerations
Small amounts of loratadine and its active metabolite, desloratadine, are excreted into
breast milk.
Cetirizine :Dosing range: Oral (Zyrtic® tab., syrup, drops): 5-10 mg once
daily, depending upon symptom severity
Patient Education
You may experience drowsiness, dizziness, or dry mouth. Report persistent sedation,
confusion, agitation, persistent nausea ,vomiting, blurred vision, or lack of
improvement or worsening of condition.
Breast feeding: Excreted into breast milk.
5} Nausea and vomiting:
-blockers):
First- and second-generation antihistamines are a safe and effective treatment for
NVP. Doxylamine should be the first choice, preferably combined with vitamin B6;
otherwise, second generation antihistamines such as meclizine should be used
because of the sedative effects of the first-generation antihistamines.
Meclizine + pyridoxine: Dosage range: Oral(Navidoxine ®tab.): 1-2 tablets
at bed time.
Pregnancy Risk Factor: B
Lactation : Excretion in breast milk unknown/not recommended
Patient Education
You may experience dizziness, drowsiness, blurred vision, dry mouth, constipation, or
heat intolerance.
Doxylamine: Dosage range:
Oral (Donormyl® tab.): Two delayed release tablets at bedtime.
Alex syndicate of pharmacists Page 14
C P E Program [PREGNANCY & LACTATION]
Pregnancy Risk Factor: A
Lactation : Excretion in breast milk unknown
Patient Education
May cause drowsiness, headache, double vision , gastrointestinal upset, or lack of
appetite.
Dopamine antagonists
Dopamine antagonists are widely used for treatment of NVP. Metoclopramide seems
safe and efficacious; it should probably be first choice among the dopamine
antagonists.
Metoclpramide :Dosing range: Oral (Primperan® tab. ,drops): 10-15
Pregnancy Risk Factor: B
Lactation: Enters breast milk/ use caution.
Patient Education
May cause dizziness, drowsiness, insomnia, or blurred vision.
6} GERD:
Antacids & sucralfate may be used during all phases of pregnancy. The
unrestricted/long-term use of antacids during pregnancy should be avoided. Among
the aluminum-containing antacids, magaldrate and sucralfate may be considered the
drugs of choice because of their apparently limited aluminum absorption.
Antacids and ulcer therapeutics of choice during breastfeeding are the newer
aluminum combinations, such as magaldrate and sucralfate as well as aluminum-free
antacids. It is generally recommended that the serum concentration of aluminum
ormagnesium be monitored.
Alex syndicate of pharmacists Page 15
C P E Program [PREGNANCY & LACTATION]
Antacids : Dosage range: (Acicone® chew.tab. , suspension 15 ml or 1 chew. Tab.
3- )
During pregnancy, H2-receptor antagonists may be prescribed when antacids or
sucralfate have failed. Ranitidine – the best-studied agent – may be preferable to
cimetidine because of a theoretical concern about the anti-androgenic properties of
cimetidine.
Ranitidine: Dosage range: Oral (Ranitak® tab.): Treatment: 150 mg twice daily,
or 300
mg once daily at bedtime
Pregnancy Risk Factor B
Lactation: Enters beast milk/ use caution.
Patient Education
May take several days before you notice relief . May cause drowsiness , dizziness, or
fatigue.
Those with low concentration in breast milk should be preferred – for example,
famotidine or nizatidine.
Famotidine: Dosage range:
Heartburn, indigestion, sour stomach: Oral (Antodine® tab.): 10-20 mg every 12
hours; dose may be taken 15-
heartburn
Pregnancy Risk Factor: B
Lactation: Enters beast milk/ not recommended.
Patient Education
OTC: Do not use for more than 2months unless recommended by prescriber. May
cause drowsiness , dizziness, constipation or diarrhea.
Alex syndicate of pharmacists Page 16
C P E Program [PREGNANCY & LACTATION]
Omeprazole is a drug of choice for reflux esophagitis in pregnancy.
For other treatment indications, proton-pump inhibitors are second-choice drugs
during pregnancy when antacids, sucralfate (Gastrofait® tab.), and ranitidine are not
effective
If proton-pump blockers are indicated during lactation, omeprazole or
pantoprazole should be chosen.
Omeprazole: Dosage range :Oral (Omepac® cap.): 40 mg once daily for 4-8
weeks
Pregnancy Risk Factor: C
Lactation: Enters beast milk/ not recommended.
Patient Education
Take ½ hour before eating.
Bismuth salts are relatively contraindicated during pregnancy.
Eat a high fiber diet: Ideally, you will consume 25 to 30 grams per day of dietary
fiber from fruits, vegetables, breakfast cereals, whole grain breads, prunes and
bran.
Drink a lot of fluids: Drinking plenty of fluids is important, particularly with your
increase of fiber. Drink 10 to 12 cups of fluids each day.
Exercise routinely: If you are inactive, you have a greater chance of
constipation.
Reduce or eliminate iron supplements: Iron supplements may contribute to
constipation. Good nutrition can often meet your iron needs during pregnancy.
Alex syndicate of pharmacists Page 17
C P E Program [PREGNANCY & LACTATION]
After stool-bulking agents, lactulose (Lactulose® susp.) is the first-choice laxative
in pregnancy. Lactitol, mannitol, and sorbitol can also be used as laxatives during
pregnancy.
When constipation needs to be treated with medication and neither bulk nor
osmotic laxatives like lactulose work effectively enough, bisacodyl is the drug
of choice throughout the entire pregnancy.
Bisacodyl : Dosage range:
Oral (Bisadyl® tab.): 5-15 mg as single dose (up to 30 mg when complete
evacuation of bowel is required)
Rectal (Bisadyl® supp.): Suppository: 10 mg as single dose
Pregnancy Risk Factor: C
Castor oil should not be used during pregnancy because it may stimulate uterine
contraction.
Mineral oil is contraindicated during pregnancy
Senna (can be used as last choice in pregnancy but when physician assess the
case)
If a change in dietary habits is not successful, bulking agents, senna
preparations, bisacodyl, and both saline and osmotic agents may be taken
during breastfeeding.
8} Chronic inflammatory bowel diseases:
Mesalazine is the drug of choice for treatment of chronic inflammatory bowel
disease during pregnancy and lactation. Sulfasalazine may also be used if necessary.
Alex syndicate of pharmacists Page 18
C P E Program [PREGNANCY & LACTATION]
Mesalazine: Dosage range:
Capsule (salazine®): 1 g 4times/day.
Tablet (Salofalk®): Initial:
Pregnancy Risk Factor: B/C (product specific)
Lactation: Enters breast milk/ use caution.
Corticosteroids may also be used, locally as well as systemically, when indicated.
Immunosuppressive agents such as azathioprine should only be used when
compellingly indicated. Methotrexate should not be prescribed.
9} Flatulence:
Dimeticon/simethicone and the plant-based substances which contain anise,
caraway, or peppermint, may be used throughout the pregnancy as
carminatives.
Simethicone (Luftal® chew. Tab.): Dosage range: Oral: 40-
meals and at bedtime, as needed
10} Hemorrhoids:
lie on your side when reading or watching TV
Dietary fiber & fluids
Sitz baths
Topical anesthetics(eg: lidocaine)
Skin protectants & astringents
# Sitz baths (hip bath) is a type of bath in which only the hips and buttocks are soaked
in water or saline solution. Its name comes from the German verb "sitzen," meaning
"to sit."
Alex syndicate of pharmacists Page 19
C P E Program [PREGNANCY & LACTATION]
Contraindicated:
Sitting for long periods(which puts pressure on the veins in your anus and rectum)
11} Urinary tract infection:
Cephalexin can be used safely during pregnancy
Oral (Ceporex® tab.): 250-1000 mg every 6 hours (maximum: 4 g/day)
Pregnancy Risk Factor: B
Lactation: Enters breast milk (small amounts)/ use caution.
Patient Education
Take at regular intervals around-the-clock, with or without food. Maintain adequate
hydration, unless instructed to restrict fluid intake.
Nitrofurantoin (Macrofuran® cap.)(but should not be used after ninth month
because it may cause hemolytic anemia in the newborn)
Sulfa-containing drugs , folate antagonists such as trimethoprim ,
fluoroquinolones and tetracyclines are contraindicated during pregnancy
12} Gestational diabetes:
Eating a balanced diet. After you find out that you have gestational diabetes, you
will meet with a registered dietitian to create a healthy eating plan.
Getting regular exercise. Try to do at least 2½ hours a week of moderate exercise.
Checking blood sugar levels. An important part of treating gestational diabetes is
checking your blood sugar level at home every day.
Monitoring fetal growth and well-being.
Getting regular medical checkups. Having gestational diabetes means regular
visits to your doctor.
Alex syndicate of pharmacists Page 20
C P E Program [PREGNANCY & LACTATION]
Pregnant women gestational diabetes should have regular insulin, if diet alone is
insufficient for control.
14} Minerals use during pregnancy:
Folic acid supplements:
For the protective action of folic acid against open neural tube defects to be effective,
–0.8 mg folic acid per day should begin as early as possible
pregnancy. Pregnant women should also be encouraged to consume foods high in
folate, such as green leafy vegetables, and fruit.
Iron supplements:
Iron supplementation during pregnancy is indicated if the hemoglobin level is 100 g/l.
It should be given orally, using an iron (II) preparation. If for some reason parenteral
iron supplementation is necessary, this should be given intravenously with an iron (III)
preparation.
Calcium supplements:
It makes sense to take 500 mg of calcium per day orally, or to drink a liter of milk. The
milk has the advantage that it supplies not only the calcium but also the daily vitamin
D requirement.
Normal vaginal discharge during pregnancy called leukorrhea is thin,
white, milky and mild smelling.
If the vaginal discharge is green or yellowish, strong smelling, and/or
accompanied by redness or itching, you may have a vaginal infection.
One of the most common vaginal infections during pregnancy is
candidiasis, also known as a yeast infection.
Alex syndicate of pharmacists Page 21
C P E Program [PREGNANCY & LACTATION]
Vaginal yeast infections:
These infections are a common problem during pregnancy, likely caused by
high estrogen levels.
During pregnancy do not:
Use tampons (they can introduce new germs into the vagina)
Douche (this can interrupt the normal balance and lead to a vaginal
infection)
Assume that it is a vaginal infection and treat it yourself
Only vaginal medicines, such as creams or vaginal suppositories, should be
used for yeast infection treatment. Oral medicines are not recommended
for women who are pregnant.
Nonprescription medicines include clotrimazole: (Candistan® cream
and miconazole :(Gyno-daktarin® vaginal
cream2%: , Gyno-daktarin® vaginal
supp. 200 mg: Insert 1 suppository at )
References:
Sites :
Online.lexi.com
www.drugs.com
www.safefetus.com
Books :
Drugs during pregnancy and lactation
st
Edition
Drugs for pregnant and lactating women
th
Edition
Alex syndicate of pharmacists Page 22
You might also like
- Clinical Obstetrics/Gynecology Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2From EverandClinical Obstetrics/Gynecology Review 2023: For USMLE Step 2 CK and COMLEX-USA Level 2Rating: 4 out of 5 stars4/5 (1)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Pregnancy and Lactation LabDocument39 pagesPregnancy and Lactation LabAoiNo ratings yet
- Some Issues To Consider While Prescribing Medications For : Pregnant and Lactating PatientsDocument25 pagesSome Issues To Consider While Prescribing Medications For : Pregnant and Lactating PatientsKishor Bajgain100% (1)
- Pregnancy and Lactation AnswersDocument8 pagesPregnancy and Lactation AnswersAoiNo ratings yet
- Lecturer Department of Pharmacy Practice SRM College of PharmacyDocument12 pagesLecturer Department of Pharmacy Practice SRM College of PharmacyRobert Selvin MNo ratings yet
- Drug Treatment To Increase Milk Supply in Lactatin-4Document4 pagesDrug Treatment To Increase Milk Supply in Lactatin-4leslieNo ratings yet
- Unit IV Drugs Used in PregnancyDocument32 pagesUnit IV Drugs Used in PregnancySuvinder singh PannuNo ratings yet
- Drugs and X-Rays For Pregnant and Breastfeeding Women During Dental TreatmentDocument5 pagesDrugs and X-Rays For Pregnant and Breastfeeding Women During Dental TreatmentArief BudimanNo ratings yet
- Anaesthetic of Choice During Pregnancy and LactationDocument5 pagesAnaesthetic of Choice During Pregnancy and LactationDegefu TadesseNo ratings yet
- Gamma-Hydroxybutyric Acid: Controlled Drug SubstancesDocument5 pagesGamma-Hydroxybutyric Acid: Controlled Drug SubstancesAngelica Charisse BuliganNo ratings yet
- 39 Hormonal ContraceptionDocument36 pages39 Hormonal ContraceptionaweleNo ratings yet
- My Sls Breast Complications in PureperiumDocument20 pagesMy Sls Breast Complications in Pureperiummarina_shawky100% (1)
- Drug Use During Pregnancy and LactationDocument50 pagesDrug Use During Pregnancy and LactationchintyamontangNo ratings yet
- Module Obsterics DrugsDocument5 pagesModule Obsterics Drugsjanina mykaNo ratings yet
- What Is The Appendix?: Symptoms of AppendicitisDocument6 pagesWhat Is The Appendix?: Symptoms of AppendicitisVonn Bryan CalumiaNo ratings yet
- Marlent Report Final-1 (3) 7aleemDocument29 pagesMarlent Report Final-1 (3) 7aleemOmarElmasryNo ratings yet
- St. Paul University Dumaguete St. Paul University System College of Nursing ISO 9001Document16 pagesSt. Paul University Dumaguete St. Paul University System College of Nursing ISO 9001Dinarkram Rabreca EculNo ratings yet
- Drugs in PregnancyDocument33 pagesDrugs in PregnancyserbalexNo ratings yet
- Antibiotics and Other Antimicrobial Agents in Pregnancy andDocument38 pagesAntibiotics and Other Antimicrobial Agents in Pregnancy andrina gustutiNo ratings yet
- OtcdrugDocument2 pagesOtcdrugDaffodil PearlNo ratings yet
- Intended Learning Objectives: Unit 3: Drugs Affecting The Body System Week 1: Reproductive System Cardiovascular SystemDocument27 pagesIntended Learning Objectives: Unit 3: Drugs Affecting The Body System Week 1: Reproductive System Cardiovascular SystemThrecia RotaNo ratings yet
- Unit: 6 Pharmacology For Midwives: Prepared By: Anita Khadka M.SC Nursing 4 BatchDocument244 pagesUnit: 6 Pharmacology For Midwives: Prepared By: Anita Khadka M.SC Nursing 4 BatchAnita KhadkaNo ratings yet
- Gyn AsDocument2 pagesGyn AsJamal kenasaNo ratings yet
- Clin Pharm - Handbook Pharmacotherapy 9thDocument10 pagesClin Pharm - Handbook Pharmacotherapy 9thstella.gillesania.chenNo ratings yet
- Liver Problems in Pregnancy - 27 To 40 WeeksDocument9 pagesLiver Problems in Pregnancy - 27 To 40 WeeksJing CruzNo ratings yet
- Prot 9 Galactogogues EnglishDocument5 pagesProt 9 Galactogogues EnglishGary YuenNo ratings yet
- DrugsDocument81 pagesDrugsrevathidadam55555100% (1)
- Drug StudyDocument14 pagesDrug StudyAthena Irish LastimosaNo ratings yet
- Health ArticlesDocument5 pagesHealth Articlesprashant_shivdas_1No ratings yet
- Client Profile Log Antenatal - CompleteDocument5 pagesClient Profile Log Antenatal - CompleteLinea GreeneNo ratings yet
- The Effects of Immunosuppressive and Anti-Inflammatory Medications On Fertility, Pregnancy, and LactationDocument10 pagesThe Effects of Immunosuppressive and Anti-Inflammatory Medications On Fertility, Pregnancy, and LactationBamdad KhomaarNo ratings yet
- Kuliah 3 Obat-Obat TeratogenikDocument38 pagesKuliah 3 Obat-Obat TeratogenikMuhammad AidilNo ratings yet
- Pregnancy and LactationDocument42 pagesPregnancy and LactationnabilaNo ratings yet
- Angeliq PM enDocument45 pagesAngeliq PM enTomacho HitachiNo ratings yet
- OknotokDocument6 pagesOknotokBeau PhatruetaiNo ratings yet
- Pharmacotherapeutics in ObstetricsDocument14 pagesPharmacotherapeutics in ObstetricsmercyNo ratings yet
- Do Not Copy Penalties Apply: Safety of Topical Dermatologic Medications in PregnancyDocument5 pagesDo Not Copy Penalties Apply: Safety of Topical Dermatologic Medications in Pregnancypipim septianaNo ratings yet
- 9 Antepartum CareDocument24 pages9 Antepartum CareFlowerer ShafaaNo ratings yet
- MisoprostolDocument3 pagesMisoprostolMichael Aditya LesmanaNo ratings yet
- Family Planning Methods Contraceptive Implants: Who Can Use Implantable Contraception?Document5 pagesFamily Planning Methods Contraceptive Implants: Who Can Use Implantable Contraception?Cindy MaslagNo ratings yet
- Antibiotic GuidelinesDocument38 pagesAntibiotic GuidelinesKomang Adhi AmertajayaNo ratings yet
- Drugs & Pregnancy: Table 1. Principles of Classifying Drugs Into Various CategoriesDocument5 pagesDrugs & Pregnancy: Table 1. Principles of Classifying Drugs Into Various CategoriesMuhammad GoharNo ratings yet
- Lipincott Answer KeyDocument3 pagesLipincott Answer KeyKelly Queenie AndresNo ratings yet
- Final Maternal Physiology in Pregnancy and Fetal CirculationDocument87 pagesFinal Maternal Physiology in Pregnancy and Fetal Circulationmonaalzoubi02No ratings yet
- NCP - Diabetes Mellitus Prepregnancy/GestationalDocument13 pagesNCP - Diabetes Mellitus Prepregnancy/GestationalClaudine Christophe100% (1)
- ZegenDocument6 pagesZegenainvenNo ratings yet
- Oral Health Care For The Pregnant PatientDocument6 pagesOral Health Care For The Pregnant PatientDominique Harz FresnoNo ratings yet
- Nursing Management of PreeclampsiaDocument2 pagesNursing Management of PreeclampsiaMary Shane MoraldeNo ratings yet
- Eluxadoline-100mg TabletDocument8 pagesEluxadoline-100mg TabletMd. Abdur RahmanNo ratings yet
- ContraceptionDocument33 pagesContraceptionShams AtrashNo ratings yet
- Amoxicillin and Clavulanate PotassiumDocument6 pagesAmoxicillin and Clavulanate PotassiumPascalis AyukNo ratings yet
- Drugs Affecting The Myometrium (Stimulants and Relaxants of The Uterus)Document25 pagesDrugs Affecting The Myometrium (Stimulants and Relaxants of The Uterus)soumyajitchakraborty0238No ratings yet
- Breast-Feeding Reduced Risk For ER/PR-Negative Breast CancerDocument5 pagesBreast-Feeding Reduced Risk For ER/PR-Negative Breast CancerpreciouscamilleNo ratings yet
- Presentation Dyspepsia Medications in PregnancyDocument25 pagesPresentation Dyspepsia Medications in Pregnancyelly_k4443244No ratings yet
- Pregnancy and OmfsDocument29 pagesPregnancy and OmfsbbilaspaNo ratings yet
- Journal at Iba PaDocument5 pagesJournal at Iba PaMIkahell CaszxyNo ratings yet
- Oxytocics and TocolyticsDocument6 pagesOxytocics and TocolyticsFarheen khanNo ratings yet
- Drugs in Pregnancy and Lactation 2021Document51 pagesDrugs in Pregnancy and Lactation 2021LU'LUIL MUNIROHNo ratings yet
- Review Article The Management of Heartburn in PregnancyDocument9 pagesReview Article The Management of Heartburn in PregnancyBeatriz SSNo ratings yet
- Controlling Sexual UrgeDocument10 pagesControlling Sexual UrgeRajan Kumar SinghNo ratings yet
- Dulcolax PDFDocument12 pagesDulcolax PDFAnica BesmonteNo ratings yet
- 4 ConstipationDocument58 pages4 ConstipationPonkiya Ankit100% (1)
- Diareea Cronica Constipatia Cronica: Prof. Dr. Mircea DiculescuDocument33 pagesDiareea Cronica Constipatia Cronica: Prof. Dr. Mircea Diculescuasum_1987No ratings yet
- Adobe Scan 01-Dec-2020Document4 pagesAdobe Scan 01-Dec-2020Saiman Ranjan TripathyNo ratings yet
- N C by Dr. Mohamed Baraka: Ausea AND Vomiting Onstipation AND DiarrheaDocument72 pagesN C by Dr. Mohamed Baraka: Ausea AND Vomiting Onstipation AND DiarrheaIbrahim Mahmoud AliNo ratings yet
- GIT AgentsDocument51 pagesGIT AgentsEimhie Lee CasiNo ratings yet
- DiseasesDocument8 pagesDiseasesBulcio Reed NaxilaNo ratings yet
- Drug Study - BisacodylDocument4 pagesDrug Study - BisacodylKyla CastroNo ratings yet
- Abnormalities of Fecal Elimination SgmacDocument4 pagesAbnormalities of Fecal Elimination SgmacRachelle DelantarNo ratings yet
- PDDS Laboratory Midterms ReviewerDocument5 pagesPDDS Laboratory Midterms ReviewerStephanie AlyssonNo ratings yet
- Test Bank For Understanding Motivation and Emotion 7th Edition Johnmarshall ReeveDocument24 pagesTest Bank For Understanding Motivation and Emotion 7th Edition Johnmarshall ReeveJulieCooperb25om100% (38)
- Eat A BananaDocument3 pagesEat A Bananamehima10No ratings yet
- Module Gastrointestinal AgentsDocument6 pagesModule Gastrointestinal AgentsKim JunkyuNo ratings yet
- Dosi MetricsDocument282 pagesDosi MetricsMark GarciaNo ratings yet
- Chapter V Gastrointestinal AgentsDocument5 pagesChapter V Gastrointestinal AgentsArantxa ElepañoNo ratings yet
- Fundamentals of Nursing Transes 1Document4 pagesFundamentals of Nursing Transes 1Louise Torres88% (8)
- Drugs Affecting The G.I.T.Document11 pagesDrugs Affecting The G.I.T.Mona MahfouzNo ratings yet
- Laxative Guidelines Nov 2013Document2 pagesLaxative Guidelines Nov 2013Purim KTshipNo ratings yet
- Katzung LaxativesDocument6 pagesKatzung LaxativesLonnieAllenVirtudesNo ratings yet
- Alternative and Complementary Medicine: AlterativeDocument9 pagesAlternative and Complementary Medicine: AlterativemuhammadriazNo ratings yet
- Gastrointestinal Pharmacotherapy: Sarah Nelson, Pharm.D. March 3, 2009Document45 pagesGastrointestinal Pharmacotherapy: Sarah Nelson, Pharm.D. March 3, 2009YainPanggaloNo ratings yet
- DIARE Pharmacotherapy Handbook 9th Edition 200 205 INGDocument6 pagesDIARE Pharmacotherapy Handbook 9th Edition 200 205 INGNyoman WiraNo ratings yet
- Test Bank For Principles of Supply Chain Management A Balanced Approach 3rd Edition by WisnerDocument24 pagesTest Bank For Principles of Supply Chain Management A Balanced Approach 3rd Edition by WisnerDestinyDickersoncfws100% (42)
- Drug StudyDocument6 pagesDrug StudyRyan BancoloNo ratings yet
- Extend Fast HugDocument4 pagesExtend Fast HugSyahrul Mubarak Danar SumantriNo ratings yet
- DocusateDocument3 pagesDocusateAaliyah OralloNo ratings yet
- Epsom Salt Benefits, Uses and Side Effects - Dr. AxeDocument9 pagesEpsom Salt Benefits, Uses and Side Effects - Dr. AxeJames MukhwanaNo ratings yet
- Anti EmeticsDocument112 pagesAnti Emeticsjoel david knda mjNo ratings yet
- Constac For Constipation Treatment by Healing Hands HerbsDocument25 pagesConstac For Constipation Treatment by Healing Hands HerbsHealing Hands Clinic PuneNo ratings yet