Professional Documents
Culture Documents
Abnormalities of Fecal Elimination Sgmac
Uploaded by
Rachelle DelantarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abnormalities of Fecal Elimination Sgmac
Uploaded by
Rachelle DelantarCopyright:
Available Formats
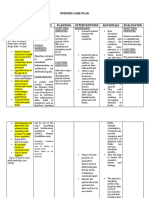
ABNORMALITIES OF FECAL ELIMINATION
Constipation Patients who recently had surgery
Older adults
It is defined as fewer than three bowel
Non-Caucasians
movements weekly or bowel movements that
are hard, dry, small, or difficult to pass People with a history of irritable bowel syndrome
It is a symptom, not a disease
MEDICAL MANAGEMENT
4 CLASSES OF CONSTIPATION
Based upon their underlying pathophysiologic “Treatment targets the underlying cause of
mechanisms constipation and prevention of recurrence.” JIBE
1. Functional constipation Judicious use of laxatives. [If laxative use is
Involves normal transit mechanisms of mucosal necessary, one of the following may be
transport. prescribed: bulk-forming agents (fiber laxatives),
Most common and can be successfully treated saline and osmotic agents, lubricants,
by increasing intake of fiber and fluids. stimulants, or emollient stool softeners]
Increased fiber and fluid intake [Daily dietary
2. Slow-transit constipation intake of 25 to 30 g/day of fiber is
Caused by inherent disorders of the motor recommended. Add fiber to the diet slowly in
function of the colon (e.g., Hirschsprung order to avoid adverse effects such as
disease), abdominal cramping and bloating. Fiber is
Characterized by infrequent bowel movements. increased daily in 5g increments, along with
encouraging fluid intake]
3. Defecatory disorders Bowel habit training
Caused by dysfunctional motor coordination Exercise [Routine exercise to strengthen
between the pelvic floor and anal sphincter. abdominal muscles is encouraged.]
Dyssynergic constipation is a common cause of
chronic constipation and is caused by an To prevent constipation:
inability to coordinate the abdominal, pelvic floor,
and rectoanal muscles to defecate.
Ensure proper dietary habits, such as eating
Anismus is a term used to describe pelvic floor
high-residue, high-fiber foods (e.g., fruits,
dysfunction and constipation.
vegetables); adding fiber to the diet slowly with
adequate fluid intake; choosing dietary sources
4. Opioid-induced constipation of fiber, which are preferred over fiber
Includes new or worsening symptoms that occur supplements; adding bran daily (must be
when opioid therapy is initiated, changed, or introduced gradually); and increasing fluid intake
increased and must include two or more (unless contraindicated) to help prevent
symptoms of functional constipation constipation.
Avoid overuse or long-term use of stimulant
CLINICAL MANIFESTATION
laxatives.
Fewer than three bowel movements per week
Abdominal distention
Abdominal pain and bloating
A sensation of incomplete evacuation
Straining at stool
Elimination of small-volume, lumpy, hard, dry
stools.
The patient may report tenesmus
RISK FACTORS
People more likely to become constipated are:
Women, particularly pregnant women
Page 1 of 4 – EXCLUSIVELY FOR BSN-3A
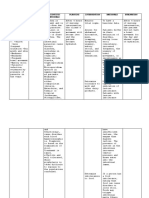
Diarrhea When the cause of the diarrhea is not obvious, the
following diagnostic tests may be performed:
An increased frequency of bowel movements
Complete blood cell count (CBC)
(more than 3 per day) with altered consistency
of stool. Serum chemistries
Can be associated with urgency, perianal Urinalysis
discomfort, incontinence, nausea. Routine stool examination
Stool examinations for infectious or parasitic
DIARRHEA CAN BE CLASSIFIED AS ACUTE, PERSISTENT organisms, bacterial toxins, blood, fat,
OR CHRONIC electrolytes, and white blood cells.
Endoscopy or barium enema may assist in
1. Acute diarrhea is self-limiting, lasting 1 or 2 days identifying the cause.
2. Persistent diarrhea typically lasts between 2 and
4 weeks
3. Chronic diarrhea persists for more than 4 weeks
and may return sporadically. This includes FECAL INCONTINENCE
secretory, osmotic, malabsorptive, infectious, AKA Bowel Incontinence
and exudative. Inability to control bowel movements resulting in
involuntary fecal elimination.
Secretory diarrhea is usually high-volume
diarrhea MUST KNOW ------
- associated with bacterial toxins and Can range in severity; from involuntary leakage
chemotherapeutic agents used to treat of small of stool while passing gas to total loss of
neoplasms bowel control
- caused by increased production and It is treatable and not life threatening
secretion of water and electrolytes One of the most socially and psychologically
Osmotic diarrhea occurs when water is pulled debilitating
into the intestines by the osmotic pressure of It is a widespread problem, affecting at least 7
unabsorbed particles, slowing the reabsorption out of 100 non hospitalized adults and at least
of water half of adults who reside in long-term care
- can be caused by lactase deficiency, facilities
pancreatic dysfunction, or intestinal
hemorrhage.
CLINICAL MANIFESTATION
Malabsorptive diarrhea combines mechanical
and biochemical actions, inhibiting effective Patients may have—
absorption of nutrients. minor soiling
- Low serum albumin levels lead to occasional urgency and loss of control, or
intestinal mucosa swelling and liquid complete incontinence.
stool. experience poor control of flatus
- Infectious diarrhea results from diarrhea
infectious agents invading the intestinal constipation.
mucosa.
Exudative diarrhea is caused by changes in
mucosal integrity, epithelial loss, or tissue Passive incontinence occurs without warning; whereas,
destruction by radiation or chemotherapy. patients with urge incontinence have the sensation of
the urge to defecate but cannot reach the toilet in time
Note: Acute and Persistent diarrheas are frequently
caused by viral infections and sometimes drugs such as; Fecal incontinence has many causes and risk factors
some antibiotics (e.g., erythromycin) and magnesium- and may be a symptom of an underlying condition
containing antacids (e.g., magnesium hydroxide).
RISK FACTORS
Note: Chronic diarrhea may be caused by adverse It is less commonly a long-term consequence of
effects of chemotherapy, antihypertensive agents, vaginal childbirth injuries than in years past,
metabolic and endocrine disorders. most likely because of improved delivery
methods,
It is more common with advancing age (i.e.,
weakness or loss of anal or rectal muscle tone)
ASSESSMENT AND DIAGNOSTIC FINDINGS
Page 2 of 4 – EXCLUSIVELY FOR BSN-3A
CAUSES
1. Damage to the anal sphincters - Abdominal pain related to defecation
2. Diarrhea - Abdominal pain associated with a change in
3. Inflammatory Bowel Disease frequency of stool
4. Nerve damage - Abdominal pain associated with a change in
form/appearance of stool.
-
MEDICAL MANAGEMENT
Medical management of fecal incontinence is
directed at correcting the underlying cause.
1. If fecal incontinence is related to diarrhea, the
incontinence may disappear when diarrhea is
successfully treated.
2. If the fecal incontinence is related to the use of
contributory drugs (e.g., laxatives, antacids
containing magnesium), the incontinence may
improve or cease when the drug regimen is
altered. The Bristol Stool Form Scale (BSFS) is used to evaluate
3. When fecal incontinence is related to other bowel movement (BM) habit
disorders, treatments targeted at correcting the
underlying disorder are initiated. Some patients
benefit from the addition of psyllium as a fiber
supplement.
Note: Administering loperamide 30 minutes prior to
meals can be an effective intervention in some patients.
IRRITABLE BOWEL SYNDROME
A chronic functional disorder characterized by
recurrent abdominal pain associated with
disordered bowel movements, which may Characteristics of stools as recorded on the BSFS are
include diarrhea, constipation, or both, without then used to determine category of irritable bowel
an identifiable cause syndrome (IBS), where IBS-C (constipation), IBS-D
It is typically diagnosed in adults younger than (diarrhea), IBS-M (mixed), and IBS-U (unclassified)
45 years of age
Note: Recording the quality and quantity of bowel
[Women are affected more often than men, with twice as movements in a stool diary such as the Bristol Stool
many women diagnosed with IBS in the United States Form Scale can be useful in determining the category of
than men.] IBS
MEDICAL MANAGEMENT
CLINICAL MANIFESTATION
Symptoms can vary widely, ranging in intensity and
duration from mild and infrequent to severe and The goals of treatment are to relieve abdominal pain and
continuous. control diarrhea or constipation
The main symptom is an alteration in bowel patterns:
1. constipation (classified as IBS-C),
2. diarrhea (classified as IBS-D)
3. And a combination of both (classified as IBS-M
for “mixed”). 1.Lifestyle modification
- Stress reduction
ASSESSMENT AND DIAGNOSTIC FINDINGS
- Esuring adequate sleep
- Instituting an exercise regimen
The Rome IV criteria define IBS as recurrent abdominal
Can result in symptom improvement.
pain occurring at least once daily during the last 3
months, associated with:
Page 3 of 4 – EXCLUSIVELY FOR BSN-3A
2. The introduction of soluble fiber (e.g., psyllium) to the
diet is important to IBS management.
3.Restriction and then gradual reintroduction of foods
that are possibly irritating may help determine what
types of food are acting as irritants.
4. Low-FODMAP diets, which restrict intake of the
following types of foods, might improve symptoms for
some patients
Fermentable Oligosaccharides (e.g., wheat, rye,
asparagus, legumes, garlic, onions),
Disaccharides (lactose-containing foods such as milk,
yogurt),
Monosaccharides (fructose-containing foods such as
honey, agave nectar, figs, mangoes),
And Polyols (e.g., blackberries, lychee, and low-calorie
sweeteners)
BYE.
Page 4 of 4 – EXCLUSIVELY FOR BSN-3A
You might also like
- GIT DisordersDocument171 pagesGIT DisordersKatrina PonceNo ratings yet
- Obstacles On The Path of YogaDocument5 pagesObstacles On The Path of YogaYogacharya Dr Ananda Balayogi Bhavanani100% (2)
- Foam SclerotherapyDocument30 pagesFoam SclerotherapyRMR100% (1)
- Pranayama & The Art of BreathingDocument16 pagesPranayama & The Art of BreathingAnurrag KumarNo ratings yet
- PHYSIOLOGY AND PATHOLOGY OF DEFECATIONDocument57 pagesPHYSIOLOGY AND PATHOLOGY OF DEFECATIONMonica BellyndaNo ratings yet
- Fecal Elimination EnemaDocument5 pagesFecal Elimination EnemaVia Kristel ZapantaNo ratings yet
- Tips To Diagnose & Address Common Horse AilmentsDocument6 pagesTips To Diagnose & Address Common Horse AilmentsMark GebhardNo ratings yet
- Lecture 15 Bowl EliminationDocument72 pagesLecture 15 Bowl EliminationIsbelNo ratings yet
- Delivering Better Oral HealthDocument102 pagesDelivering Better Oral Healthsavrasx100% (1)
- Standard Treatment GuidelinesDocument468 pagesStandard Treatment GuidelinesHarshit ChempallilNo ratings yet
- Understanding ConstipationDocument10 pagesUnderstanding ConstipationAndy PurnomoNo ratings yet
- Irritable Bowel SyndromeDocument22 pagesIrritable Bowel SyndromeMarium NabeelNo ratings yet
- Nursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationDocument8 pagesNursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationKrahNo ratings yet
- Cholecystitis and CholelithiasisDocument19 pagesCholecystitis and CholelithiasisChristine Salimbagat100% (1)
- NCM 116 W1 Reading HandoutDocument13 pagesNCM 116 W1 Reading Handoutriza sarmientoNo ratings yet
- ConstipationDocument4 pagesConstipationprincess_bee100% (1)
- NCM 116 - GIT (MODULE 5 Part II)Document6 pagesNCM 116 - GIT (MODULE 5 Part II)Meryville JacildoNo ratings yet
- KONSTIPASIDocument33 pagesKONSTIPASIalhidayahNo ratings yet
- DiareDocument5 pagesDiarefarisNo ratings yet
- Bowel Elimination and Urinary Incontinence ProblemsDocument5 pagesBowel Elimination and Urinary Incontinence ProblemsMegan Rose MontillaNo ratings yet
- 4 NCM+116n+Lecture+Care+of+the+Clients+with+Problems+GI+Function+and+NutritionDocument10 pages4 NCM+116n+Lecture+Care+of+the+Clients+with+Problems+GI+Function+and+NutritionKylle AlimosaNo ratings yet
- A. Related FactorsDocument10 pagesA. Related FactorsEva YuliaNo ratings yet
- Diarrhea (Diare)Document9 pagesDiarrhea (Diare)Eki MegaraniNo ratings yet
- Article 1540977249Document14 pagesArticle 1540977249merissa iglesias100% (1)
- Constipation: Jan M. ShoenbergerDocument5 pagesConstipation: Jan M. ShoenbergerS100% (1)
- Irritable Bowel Syndrome GuideDocument7 pagesIrritable Bowel Syndrome GuideHisyam DinGanuNo ratings yet
- ConstipationDocument22 pagesConstipationOsama ALGabriNo ratings yet
- Nursing management of acute gastrointestinal disordersDocument20 pagesNursing management of acute gastrointestinal disorderswyneNo ratings yet
- (Roselle Balicas) - Chrome - LNKDocument8 pages(Roselle Balicas) - Chrome - LNKRose CasBalNo ratings yet
- Gastrointestinal System: Diseases of The Digestive SystemDocument7 pagesGastrointestinal System: Diseases of The Digestive SystemhadrilkaNo ratings yet
- Constipation Diarrhea Fecal IncontinenceDocument40 pagesConstipation Diarrhea Fecal IncontinenceLiza Marie IgnacioNo ratings yet
- Digestive System DisordersDocument117 pagesDigestive System DisordersSusan Batan BandongNo ratings yet
- 7 - ET - LECT - Dietary ManagementDocument3 pages7 - ET - LECT - Dietary ManagementMa Ellen LumauagNo ratings yet
- Constipation and Bowel Obstructions PP Rat 10.2020Document20 pagesConstipation and Bowel Obstructions PP Rat 10.2020Vaidya M.R. PoornimaNo ratings yet
- Risk For Constipation-Cancer Nursing Care PlanDocument1 pageRisk For Constipation-Cancer Nursing Care PlanRnspeakcomNo ratings yet
- Constipation: Patient Name: Shehzad Age: 45 Ward: Emergency BDocument2 pagesConstipation: Patient Name: Shehzad Age: 45 Ward: Emergency BShafiq Ur RahmanNo ratings yet
- PHCP Lec Topic 4 To 10Document19 pagesPHCP Lec Topic 4 To 10armand bayoranNo ratings yet
- Understanding Medical Surgical Nursing (2) - 0001-0001Document1 pageUnderstanding Medical Surgical Nursing (2) - 0001-0001Anas TasyaNo ratings yet
- Case Study On DiarrheaDocument4 pagesCase Study On DiarrheaDalene Erika GarbinNo ratings yet
- ConstipationDocument12 pagesConstipationfrechel kimNo ratings yet
- Constipation (Sembelit)Document8 pagesConstipation (Sembelit)Eki MegaraniNo ratings yet
- MIDTERMSDocument24 pagesMIDTERMSCherish Marie HurbodaNo ratings yet
- Constipation and Bowel Obstructions PP Rat 10.2020Document26 pagesConstipation and Bowel Obstructions PP Rat 10.2020Osman Bin SaifNo ratings yet
- Unit Ix: Nursing Management of Patients With Gi Disorders: Topic: DiarrheaDocument13 pagesUnit Ix: Nursing Management of Patients With Gi Disorders: Topic: Diarrheaayushi rainaNo ratings yet
- Healthful Practices That Affect The Digestive System andDocument16 pagesHealthful Practices That Affect The Digestive System andNovie Jane HontiverosNo ratings yet
- Management of Patients With Intestinal and RectaldisordersDocument16 pagesManagement of Patients With Intestinal and RectaldisordersintotheunknownNo ratings yet
- Chronic Diarrhoea SaqlainDocument116 pagesChronic Diarrhoea SaqlainMohammed SaqlainNo ratings yet
- Nutrition Imbalance NCPDocument1 pageNutrition Imbalance NCPmawelNo ratings yet
- Constipation LeukemiaDocument1 pageConstipation LeukemiamawelNo ratings yet
- 22 Manuscript Intestinal ObstructionDocument8 pages22 Manuscript Intestinal Obstructionkint manlangitNo ratings yet
- p2277 PDFDocument8 pagesp2277 PDFGoran TomićNo ratings yet
- 9 Intestinal ObstructionDocument7 pages9 Intestinal ObstructionMAH pedNo ratings yet
- Daud Khan 1045Document31 pagesDaud Khan 1045Iqra BatoolNo ratings yet
- Diarrhea NCP Pedia WardDocument4 pagesDiarrhea NCP Pedia WardKyle DapulagNo ratings yet
- Consti Pati On: Evaluati On and Management: by Bhairvi Jani, MD & Elizabeth Marsicano, MDDocument5 pagesConsti Pati On: Evaluati On and Management: by Bhairvi Jani, MD & Elizabeth Marsicano, MDsavitri geminiNo ratings yet
- Pathophysiology of Acute DiarrheaDocument3 pagesPathophysiology of Acute DiarrheaFabiana TorresNo ratings yet
- NCM116 Prelim Week 1Document15 pagesNCM116 Prelim Week 1Loungayvan BatuyogNo ratings yet
- New Intestinal ObstructionDocument12 pagesNew Intestinal Obstructionmustafalotfy01No ratings yet
- Fecal EliminationDocument4 pagesFecal EliminationEzra MaeNo ratings yet
- Group 4 Case Presentation DiarrheaDocument46 pagesGroup 4 Case Presentation DiarrheaEphraim John QuichoNo ratings yet
- Age NCPDocument3 pagesAge NCPMartin Allen ClaudioNo ratings yet
- GI SlidesDDM1Document39 pagesGI SlidesDDM1Anonymous d3qpXcm4xVNo ratings yet
- Childhood Constipation: BackgroundDocument5 pagesChildhood Constipation: BackgroundJihan FaadhilahNo ratings yet
- CONTENTDocument17 pagesCONTENTEromobor OnobunNo ratings yet
- Constipation: How To Treat Constipation: How To Prevent Constipation: Along With Nutrition, Diet, And Exercise For ConstipationFrom EverandConstipation: How To Treat Constipation: How To Prevent Constipation: Along With Nutrition, Diet, And Exercise For ConstipationNo ratings yet
- Midterms - Electrolyte Renal DisordersDocument40 pagesMidterms - Electrolyte Renal DisordersRachelle DelantarNo ratings yet
- SummerTerm TopicOutline1Document20 pagesSummerTerm TopicOutline1Rachelle DelantarNo ratings yet
- Research BSN3G SetA Group1FINALDocument75 pagesResearch BSN3G SetA Group1FINALRachelle DelantarNo ratings yet
- NCM 116 G.I Trans Group 2Document30 pagesNCM 116 G.I Trans Group 2Rachelle DelantarNo ratings yet
- NCM116 Finals Assessment of The Nervous SystemDocument9 pagesNCM116 Finals Assessment of The Nervous SystemRachelle DelantarNo ratings yet
- Hemorraghic StrokeDocument4 pagesHemorraghic StrokeRachelle Delantar100% (1)
- Effectiveness of thoracic-abdominal rebalancing technique for acute viral bronchiolitisDocument9 pagesEffectiveness of thoracic-abdominal rebalancing technique for acute viral bronchiolitisrebeca paulinoNo ratings yet
- Liver Case - Hepatic ToxicologyDocument2 pagesLiver Case - Hepatic Toxicologysaya001No ratings yet
- Peripheral Vascular System Anatomy Exam TechniquesDocument2 pagesPeripheral Vascular System Anatomy Exam TechniquesAngelica Mae Dela CruzNo ratings yet
- One Form Should Be Completed by An Adult Member of Each Family. Print in Capital (UPPERCASE) Letters. Leave Blank Boxes For SpacesDocument1 pageOne Form Should Be Completed by An Adult Member of Each Family. Print in Capital (UPPERCASE) Letters. Leave Blank Boxes For SpacesDiana CharvinskayaNo ratings yet
- Chapter 6 - Nutrition (Part 1)Document41 pagesChapter 6 - Nutrition (Part 1)Ema FatimahNo ratings yet
- Genetic Analysis An Integrated Approach 2nd Edition Sanders Test BankDocument15 pagesGenetic Analysis An Integrated Approach 2nd Edition Sanders Test Bankjenniferedwardsmpnidwyjkb100% (48)
- Freelesson1endhairloss EulastversionDocument7 pagesFreelesson1endhairloss EulastversionDezant MiradzNo ratings yet
- Vitamins enable body processes and energy useDocument70 pagesVitamins enable body processes and energy usecon_orenseNo ratings yet
- AHP Matlab software calculates weights for network analysisDocument9 pagesAHP Matlab software calculates weights for network analysisAllahyarNo ratings yet
- Instructional PlanningDocument3 pagesInstructional PlanningRadino Bryan C. SardidoNo ratings yet
- Respiratory Effects of Amyotrophic Lateral Sclerosis, Problems and SolutionsDocument14 pagesRespiratory Effects of Amyotrophic Lateral Sclerosis, Problems and SolutionsMarcelaNo ratings yet
- Vet Pathol 2011 2011 ACVP Annual Meeting E1 E51Document52 pagesVet Pathol 2011 2011 ACVP Annual Meeting E1 E51Haroon RashidNo ratings yet
- The Design and Synthesis of Novel BarbituratesDocument333 pagesThe Design and Synthesis of Novel BarbituratesLucas Timmer100% (1)
- Conservative TreatmentDocument30 pagesConservative TreatmentAlessandro AnceschiNo ratings yet
- 3 Steps To Reverse Aging 1Document3 pages3 Steps To Reverse Aging 1santosh MaliNo ratings yet
- Mercaptan Fact SheetDocument6 pagesMercaptan Fact SheetPravin GowardunNo ratings yet
- EM200 Clerkship Packet - November, 2012Document139 pagesEM200 Clerkship Packet - November, 2012jtsk2No ratings yet
- A Project Report On Banana PlantationDocument10 pagesA Project Report On Banana Plantationkim shinNo ratings yet
- Tuesday, December 09, 2014 EditionDocument16 pagesTuesday, December 09, 2014 EditionFrontPageAfricaNo ratings yet
- Adaptation For Life After Birth A Review of Neonatal PhysiologyDocument9 pagesAdaptation For Life After Birth A Review of Neonatal PhysiologyGrifanda HumairahNo ratings yet
- Ectopic Pregnancy - CSDocument14 pagesEctopic Pregnancy - CSMASII100% (1)
- Infant Formulas. Pediatr Rev 2011Document13 pagesInfant Formulas. Pediatr Rev 2011Zeniff ArciveNo ratings yet
- COVID-19 Reflection - Pengosro, YzahDocument5 pagesCOVID-19 Reflection - Pengosro, Yzahyzah graceNo ratings yet
- Utah KidneyDocument16 pagesUtah KidneyChristineGonzalesNo ratings yet