Professional Documents
Culture Documents
MIDTERMS
Uploaded by
Cherish Marie HurbodaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MIDTERMS
Uploaded by
Cherish Marie HurbodaCopyright:
Available Formats
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
ABNORMALITIES OF FECAL ELIMINATION TYPES OF DIARRHEAS
1. Secretory diarrhea
o Usually a high-volume diarrhea
o Often associated with bacterial toxins and
neoplasms
o Caused by increased production and
secretion of water and electrolytes by the
intestinal mucosa into the intestinal lumen
2. Osmotic Diarrhea
o Occurs when water is pulled into the
intestines by the osmotic pressure of
unabsorbed particles, slowing the
reabsorption of water.
o It can be caused by lactase deficiency,
pancreatic dysfunction, or intestinal
hemorrhage.
3. Malabsorptive Diarrhea
o Malabsorptive diarrhea combines
mechanical and biochemical actions,
inhibiting effective absorption of nutrients
manifested by markers of malnutrition that
include hypoalbuminemia.
DIARRHEA 4. Infectious diarrhea
• An increased frequency of bowel movements (more o Infectious diarrhea results from infectious
than three per day) agents invading the intestinal mucosa (Ex:
• An increased amount of stool (more than 200 g/day) Clostridium difficile)
• Altered consistency (ie, increased liquidity) of stool. 5. Exudative diarrhea
• Usually associated with urgency, perianal o Exudative diarrhea is caused by changes
discomfort, incontinence, or a combination of these in mucosal integrity, epithelial loss, or
factors tissue destruction by radiation or
• Can be acute or chronic. chemotherapy
• ETIOLOGY: CLINICAL MANIFESTATIONS
o Certain medications (eg, thyroid hormone • In addition to the increased frequency and fluid
replacement, stool softeners and laxatives, content of stools, the patient usually has:
prokinetic agents, antibiotics, o Abdominal cramps
chemotherapy, antiarrhythmics, o Distention
antihypertensives, magnesium-based o Intestinal rumbling (i.e., borborygmus)
antacids) o Anorexia
o Certain tube-feeding formulas o Thirst
o Metabolic and endocrine disorders (eg, o Painful spasmodic contractions of the anus
diabetes, Addison’s disease, STOOL CHARACTERISTICS
thyrotoxicosis)
• Disorders of the small bowel – watery stools
o Viral or bacterial infectious processes (eg,
• Disorders of the large bowel - Loose, semisolid
dysentery, shigellosis, food poisoning,
stools
Norwalk virus)
o Nutritional and malabsorptive disorders • Intestinal malabsorption - voluminous, greasy stools
ACUTE • Inflammatory enteritis or colitis - presence of blood,
mucus, and pus in the stools
• Most often associated with infection • Pancreatic insufficiency - oil droplets on the toilet
• Usually self-limiting water
• Lasting up to 7-14 days • Diabetic neuropathy – nocturnal diarrhea
CHRONIC
• Persists for more than 2-3 weeks
• May return sporadically
January 30-31, 2023 1
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
ASSESSMENT AND DIAGNOSTIC FINDINGS ETIOLOGY
• When the cause of the diarrhea is not obvious, the • Certain medications (ie, tranquilizers,
following diagnostic tests may be performed: anticholinergics, antidepressants,
o Complete blood cell count antihypertensives, diuretics, opioids, aluminum-
o Serum chemistries based antacids, iron preparations, selected
o Urinalysis antibiotics, and muscle relaxants)
o Routine stool examination • Rectal or anal disorders (eg, hemorrhoids, fissures)
o Stool examination for infectious or parasitic • Obstruction (eg, bowel tumors)
organisms, bacterial toxins, blood, fat, • Metabolic, neurologic, and neuromuscular
electrolytes conditions (eg, Hirschsprung’s disease, Parkinson’s
o White blood cell count disease, multiple sclerosis)
o Endoscopy or barium enema • Endocrine disorders (eg, hypothyroidism,
COMPLICATIONS pheochromocytoma)
• Cardiac dysrhythmias • Lead poisoning
• Urinary output of less than 30mL per hour for 2-3 • Connective tissue disorders (eg, scleroderma,
hours systemic lupus erythematosus).
• Muscle weakness • Weakness
• Paresthesia Hypotension Anorexia • Immobility
• Drowsiness • Debility
• A potassium level of less than 3.5 mEq/L • Fatigue
MEDICAL MANAGEMENT • An inability to increase intraabdominal pressure
• Primary management: • Dietary habits (i.e., low consumption of fiber and
o Controlling symptoms inadequate fluid intake)
o Preventing complications • Lack of regular exercise
o Eliminating or treating the underlying • Stress
disease PATHOPHYSIOLOGY
o Antibiotics and anti-inflammatory agents • Urge to defecate stimulated by rectal distention that
o Antidiarrheals (eg, Loperamide [Imodium], initiates a series of four actions:
Diphenoxylate [Lomotil]) may be used to o Stimulation of the inhibitory rectoanal
reduce the severity of the diarrhea and reflex
treat the underlying disease o Relaxation of the internal sphincter muscle
NURSING RESPONSIBILITIES o Relaxation of the external sphincter
• Monitor characteristics & pattern of diarrhea muscle
• Obtain patient history o Muscles in the pelvic region and increased
• Abdominal auscultation and palpation intraabdominal pressure.
• Inspection of the abdomen, mucous membranes, o Interference with any of these processes
and skin can lead to constipation
• Encourage bed rest and intake of liquids and foods CLINICAL MANIFESTATIONS
low in bulk • Fewer than three bowel movements per week
• Instruct to avoid caffeine, carbonated beverages, • Abdominal distention
and very hot and very cold foods • Pain and pressure
• Restrict milk products, fat, whole-grain products, • Decreased appetite
fresh fruits, and vegetables • Headache
CONSTIPATION • Fatigue
• An abnormal infrequency or irregularity of • Indigestion
defecation • A sensation of incomplete evacuation
• Abnormal hardening of stools that makes their • Straining at stool
passage difficult and sometimes painful • Elimination of small-volume, lumpy, hard, dry stools
• A decrease in stool volume, or retention of stool in
the rectum for a prolonged period often with a
sense of incomplete evacuation after defecation
January 30-31, 2023 2
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
ASSESSMENT AND DIAGNOSTIC FINDINGS PEPTIC ULCER DISEASE (PUD)
• Chronic constipation is usually considered • An ulcerated lesion or excavation that forms in the
idiopathic mucosal wall of the stomach, in the pylorus, in the
• Patient’s history duodenum, or in the esophagus.
• Physical examination • Referred to as gastric, duodenal, or esophageal
• Barium enema or sigmoidoscopy ulcer, depending on its location.
• Fecal occult blood test • Erosion of a circumscribed area of mucous
• Anorectal manometry membrane is the cause that may extend as deeply
as the muscle layers or through the muscle to the
peritoneum.
• Common types: (1) Gastric ulcer and (2) Duodenal
ulcer
• More likely to occur in the duodenum than in the
stomach
• Tend to occur in the lesser curvature of the
stomach, near the pylorus
• Esophageal ulcers occur as a result of the
backward flow of HCl from the stomach into the
esophagus (GERD)
• Occurs in people between 40 and 60 years of age
• Defecography and colonic transit studies
COMPLICATIONS
• Hypertension
• Fecal impaction
• Hemorrhoids (dilated portions of anal veins)
• Fissures (tissue folds)
• Megacolon
• Increased arterial pressure during defecation
• Straining at stool
MEDICAL MANAGEMENT
• Treat underlying cause of constipation and aim to
prevent recurrence
• Education
• Bowel habit training
• Increase fiber and fluid intake
• Judicious use of laxatives
• Daily dietary intake of 25 to 30 g/day of fiber
(soluble and bulk-forming)
• Stool softeners
January 30-31, 2023 3
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
RISK FACTORS o Predisposing factors include smoking,
• Prolong use of steroids alcohol abuse, psychological stress and
• Ellison Zollinger syndrome bacterial infection: Helicobacter pylori.
• Prolong use of NSAIDS • Clinical manifestations
• Type O blood o Disappearance of pain after eating
o Upper part of the SI is affected
• Infection, intake of spicy food
o Observe for burning pain
• Cigarette smoking
o Decreased appetite
• Use of alcohol o Expected pain 2-4 hours after eating
• Lifestyle o Note for more melena than hematemesis
• Chronic renal and respiratory diseases o A wakens during night d/t pain
• Exposure to irritants o Location of pain – right epigastrium
• Related to the use of mechanical ventilators o Epigastric pain – dull, gnawing, burning
• Stress and anxiety pain in epigastrium
TYPE OF PEPTIC ULCER DISEASE o Epigastric tenderness – gastric: left to
1. Gastric ulcer middle epigastrium; duodenal: middle to
o Ulceration of the mucosal lining of the right epigastrium
stomach, most commonly found in the o Pyrosis – burning sensation; associated
antrum. with belching and sour eructation
o Gastric secretions and stomach emptying o Nausea and vomiting – d/t muscular
rate usually normal spasm or mechanical obstruction
o Rapid diffusion of gastric acid from the o Constipation – iatrogenic side effect
gastric lumen into gastric mucosa,
however; causes an inflammatory reaction
with tissue breakdown
o Also characterized by reflux into the
stomach of bile containing duodenal
contents.
o Occurs often in men in lower
socioeconomic groups, peak age: 40-55
years old
o Predisposing factors include smoking,
alcohol abuse, emotional tension and
drugs (salicylates, steroids, Butazolidin:
NSAIDs)
o Caused by bacterial infection: Helicobacter
pylori
• Clinical manifestations
o Gnawing pain
o Area of pain: left midepigastrium
o Sharp pain
o Time of pain
o Relieved by vomiting
GASTRIC VS DUODENAL PUD
o Increased pain after eating
o Causing more hematemesis rather than
melena
2. Duodenal ulcer
o Most commonly found in the first 2 cm of
the duodenum.
o Occur more frequently than gastric ulcers.
o Characterized by gastric hyperacidity and
a significant increased rate of gastric
emptying.
o Occur more often in younger men, more
women affected after menopause; peak
age 35-45 years.
January 30-31, 2023 4
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
PATHOPHYSIOLOGY ANTI-ULCER MEDICATIONS
• Increased concentration or activity of acid–pepsin / • Antacids
Decreased resistance of the mucosa o Therapeutic effects – neutralize gastric
• A damaged mucosa cannot secrete enough mucus acid secretion
to act as a barrier against HCl o SE/AE: aluminum based antacids:
• The use of NSAIDs inhibits the secretion of mucus constipation; magnesium based antacids:
that protects the mucosa diarrhea
• Damage to the gastroduodenal mucosa results in o Examples: aluminum hydroxide,
decreased resistance to bacteria, and thus infection magnesium hydroxide
from H. pylori bacteria may occur. o Nursing implications: (ANTACIDS)
• Zollinger-Ellison syndrome (ZES) is suspected ▪ Avoid other PO meds within 1-2
when a patient has several peptic ulcers or an ulcer hours
that is resistant to standard medical therapy ▪ Need to shake liquid prep before
• It is identified by the following: hypersecretion of pouring it
gastric juice, duodenal ulcers, and gastrinomas ▪ Taken 1-3 hours after meals
(islet cell tumors) in the pancreas. ▪ Avoid alcohol and products
ASSESSMENT AND DIAGNOSTIC FINDINGS containing aspirin
▪ Chew tablet thoroughly, follow it
• Esopagoduodenoscopy (EGD) with water
o Campylobacter-like organism (CLO) ▪ Instruct to take meds even
biopsy urease test without pain felt
o H. pylori strip ▪ Do report for s/sx of gastric
• H.pylori testing bleeding
o Stool and serum H.Pylori • Anticholinergic
o Urea breath testing o therapeutic effects – inhibit gastric acid
• Barium swallow secretion
o Highlights creates in the GIT o SE/AE
• H.Pylori rapid test kit ▪ Constipation
o The one step H. pylori serum and whole ▪ Urinary retention
blood Rapid Test is a rapid lateral flow, ▪ Hypotension
qualitative immunoassay. ▪ Dry mouth
o It is intended for use at point of care ▪ Blurring of vision
facilities to detect the presence of IgG o Examples: propantheline (Pro Banthine)
antibodies specific to H. pylori in human o Nursing implications:
blood or serum. ▪ Cautiously use in patients with
o It provides an aid in the diagnosis of glaucoma and BPH
infection by H. pylori. ▪ Do not give at the same time with
MANAGEMENT antacids
• Dietary modification • Cytoprotective
• Insertion of NGT – lavage o Therapeutic effects – provides a barrier
• Smoking cessation to the diseased tissue
• Eliminate gastric irritant drugs like ASA and o SE/AE
NSAIDS ▪ Sucralfate (carafate) –
• Antibiotics constipation
• Antacids ▪ Misoprostol (Cytotec) – diarrhea
• Stress reduction o Examples: sucralfate (carafate),
• Eliminate caffeinated drinks and alcohol misoprostol (Cytotec)
• Surgery (vagotomy/gastrectomy) o Nursing implications
▪ Sucralfate – increase OFI and
fiber in the diet
▪ Misoprostol – contraindicated in
pregnancy
January 30-31, 2023 5
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
• Gastrectomy
o Surgical removal of the stomach
I. Total gastrectomy – entire removal of the
stomach
a. Esophagoduodenostomy – esophagus
attach to the duodenum
b. Esophagojenunostomy – esophagus
attach to the jejunum
II. Subtotal gastrectomy – 2/3 of the stomach
was removed
a. Billroth I: gastroduodenostomy –
removal of the lower portion of the
stomach with anastomosis of the
MEDICATION REGIMEN FOR H.PYLORI remaining portion of the duodenum
• Standard triple therapy b. Billroth II: gastrojejunostomy – removal
o 2 antibiotics + 1 proton pump inhibitor of the antrum and distal portion of the
(PPI) stomach and duodenum with anastomosis
o 7-14 days of the remaining portion of the stomach to
• Dual therapy the jejenum
o Antibiotic + PPI • Zollinger-ellison syndrome
o Antibiotic + H2 antagonist o “gastrinoma”
o 7-14 days o Caused by a non–beta islet cell, gastrin-
• Bismuth quadruple therapy (BQT) secreting tumor of the pancreas
o 2 antibiotics + bismuth + H2 antagonist o Stimulates the acid-secreting cells of the
o 10-14 days stomach to maximal activity
SURGICAL MANAGEMENT FOR PUD o Triad findings:
• Vagotomy ▪ Duodenal Ulcers
o Medical intervention to interrupt signals ▪ Gastric hypersecretion
carried by the vagus nerve. ▪ Gastrinoma
o It usually means cutting the branch of the o Etiology:
vagus nerve that sends signal to the ▪ Islet cell tumors in the pancreas
stomach to secrete gastric acid. ▪ Multiple Endocrine Neoplasia 1
o Done to treat severe cases of peptic ulcer (MEN 1)
disease. o Signs and symptoms:
o Surgical division of the vagus nerve -> ▪ Epigastric pain
decrease vagal stimulation -> decrease ▪ Diarrhea
stimulation of HCl Acid ▪ Steatorrhea
January 30-31, 2023 6
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
MANAGEMENT
• Stress reduction and test
o Lifestyle modifications
o Biofeedback therapy, behavior
modification
• Smoking cessation
o Promotes ulcer healing by normalizing HCI
secretions
• Dietary modification
SMALL BOWEL OBSTRUCTION
o Small frequent feeding
o Bland diet; BRAT diet PATHOPHYSIOLOGY
• Medications
o Pain relief
o Eradicate infection
o Promote healing
NURSING DIAGNOSIS
• Pain RT irritated mucosa and muscle spasms
• Altered Nutrition: less than body requirements, RT
discomfort associated with eating
CLINICAL MANIFESTATIONS
• Altered Nutrition: more than body requirements, RT
relief of pain with food intake • Crampy pain (wave-like & colicky)
• Anxiety RT the nature of disease and its long term • May pass blood and mucus but no fecal matter and
management no flatus
• Knowledge deficit regarding the prevention of • Vomiting
symptoms and management of conditions • Vigorous peristaltic waves
NURSING INTERVENTIONS • Intense thirst
• Relieve pain – medications • Drowsiness
• Reduce anxiety – encourage to express fears • Generalized malaise
openly, stress reduction techniques, effective • Aching
coping mechanisms • Parched tongue and mucous membranes
• Maintain nutritional balance – small frequent meals • Distended abdomen
of bland diet CAUSES OF INTESTINAL OBSTRUCTION
• Monitoring for complications – health education on • Intussusception
complications, monitor for development of o A serious condition in which part of the
complications intestine slides into an adjacent part of the
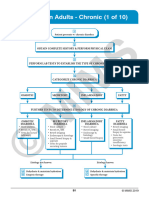
INTESTINAL OBSTRUCTION intestine
• Exists when blockage prevents the normal flow of o This telescoping action often blocks food
intestinal contents through the intestinal tract. or fluid from passing through
• Two types of processes can impede this flow: o Also cuts off the blood supply to the part of
o Mechanical obstruction: An intraluminal the intestine that's affected
obstruction or a mural obstruction from
pressure on the intestinal wall occurs
o Functional obstruction: The intestinal
musculature cannot propel the contents
along the bowel
January 30-31, 2023 7
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
DIAGNOSTICS
• Abdominal x-ray
• CT findings
• Laboratory studies
• Electrolyte studies
• Complete blood cell count
MEDICAL MANAGEMENT
• Decompression of the bowel through a nasogastric
tube
• Surgery depends on the cause of the obstruction.
• For hernia and adhesions, surgery involves
repairing the hernia or dividing the adhesion to
which the intestine is attached.
• Portions of affected bowel may be removed, and an
anastomosis is performed.
NURSING RESPONSIBILITIES
• Maintaining the function of the nasogastric tube
• Volvulus • Assessing and measuring the nasogastric output
o When a loop of intestine twists around • Assessing for fluid and electrolyte imbalance
itself and the mesentery that supports it, • Monitoring nutritional status
resulting in a bowel obstruction • Assessing improvement
• Reports discrepancies in intake and output,
worsening of pain or abdominal distention, and
increased nasogastric output.
LARGE BOWEL OBSTRUCTION
• Results in an accumulation of intestinal contents,
fluid, and gas proximal to the obstruction.
• It can lead to severe distention and perforation
unless some gas and fluid can flow back through
the ileal valve.
• If the blood supply is cut off, intestinal strangulation
• Hernia and necrosis occur; this condition is life-threatening.
o The abnormal exit of tissue or an organ, • Adenocarcinoid tumors account for the majority of
such as the bowel, through the wall of the large bowel obstructions.
cavity in which it normally resides.
o Happens when an internal organ pushes
through a weak spot in your muscle or
tissue.
January 30-31, 2023 8
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
CLINICAL MANIFESTATIONS NURSING MANAGEMENT
• Sigmoid colon or the rectum - Constipation • Monitor for symptoms that indicate that the
• Altered shape of stool intestinal obstruction is worsening
• Bloody stool: results to iron deficiency anemia • Administers IV fluids and electrolytes as prescribed.
• Weakness • Prepares the patient for surgery
• Weight loss • Ensure NPO status
• Anorexia • Post surgery, general abdominal wound care
• Distended abdomen HEMORRHOIDS
• Crampy lower abdominal pain • Dilated portions of the veins in the anal canal.
• Fecal vomiting • Shearing of the mucosa during defecation results in
• Symptoms of shock may occur the sliding of the structures in the wall of the anal
canal, including the hemorrhoidal and vascular
tissues
• Types:
o Internal hemorrhoids
o External hemorrhoids
PATHOPHYSIOLOGY
CLINICAL MANIFESTATIONS
• Itching
• Bright red bleeding during defecation
• Pain
o Internal – not usually painful until they
bleed or prolapse occurs
o External – severe pain
DIAGNOSTICS
• Edema
• Abdominal x-ray MEDICAL MANAGEMENT
• Abdominal CT scan or MRI findings
• Good hygiene
• Barium studies are contraindicated
• Avoidance of excessive straining during defecation
MEDICAL MANAGEMENT
• High residue diet
• Restoration of intravascular volume • Hot Sitz Bath
• Correction of electrolyte abnormalities • Cryosurgical Hemorrhoidectomy
• Nasogastric aspiration
• Colonoscopy
• Cecostomy
• Surgical resection of the large intestine
• Temporary or permanent colostomy
• Ileoanal anastomosis
January 30-31, 2023 9
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
NURSING RESPONSIBILITIES CROHN’S DISEASE
• Prevent engorgement: • “Regional Enteritis” or “Granulomatous Enteritis”
o Hydrophilic bulk forming agents • A subacute and chronic inflammation of the GI tract
o (Psyllium) wall that extends through all layers (transmural
o Warm compress & sitz bath lesion).
o Analgesic ointments and suppositories • Can occur anywhere in the GI tract, but commonly
o Astringents (eg, witch hazel) occurs in the distal ileum and, to a lesser degree,
o Bed rest the ascending colon.
• Prevent prolapse: • Extension of inflammation into the mucosa causes:
o Infrared photocoagulation o Abscess formation
o Bipolar diathermy o Fistula
o Laser therapy o Fissures
o Injection of sclerosing agents
SURGICAL TREATMENT
• Rubber-band ligation procedure
• Cryosurgical hemorrhoidectomy
• Stapled hemorrhoidopexy
• Hemorrhoidectomy
INFLAMMATORY BOWEL DISEASE
• 2 types: Crohn’s disease, ulcerative colitis
• The cause of IBD is still unknown
ETIOLOGY
• Ages between 15 30 and 50 70
• (+) Family history: largest
• independent risk factor
• Environmental agents such as pesticides, food
additives, tobacco, and radiation CLINICAL MANIFESTATIONS
• NSAIDs found to exacerbate IBD • RLQ pain
• Diarrhea (unrelieved by defecation)
• Crampy abdominal pain
• Abdominal tenderness & spasm
• Weight loss
• Malnutrition
• Anemia
CHRONIC SYMPTOMS
• Steatorrhea
• Anorexia
• Nutritional deficits
PATHOPHYSIOLOGY
• Begins with edema and thickening of the mucosa
• Ulcers begin to appear on the inflamed mucosa.
• These lesions are not in continuous contact with
one another and are separated by normal tissue
(“cobblestone” appearance)
• Fistulas, fissures, and abscesses form as the
inflammation extends into the peritoneum
• As the disease advances, the bowel wall thickens
and becomes fibrotic, and the intestinal lumen
narrows.
• Diseased bowel loops sometimes adhere to other
loops surrounding them.
January 30-31, 2023 10
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
ASSESSMENT AND DIAGNOSTIC FINDINGS ETIOLOGY
• Proctosigmoidoscopy • Infection
• Fecal Occult Blood Test (FOBT) • Allergy
• Barium study of the upper GI tract • Autoimmune
• Endoscopy • Incidence:
• Colonoscopy o Caucasians
• Intestinal biopsies o Jews
• Barium enema CLINICAL MANIFESTATIONS
• Complete blood count • Diarrhea
• Hematocrit & Hemoglobin (usually decreased) • Passage of mucus and pus
• WBC (usually elevated) • LLQ abdominal pain
• Intermittent tenesmus
• Rectal bleeding
• Anorexia
• Weight loss
• Fever
• Vomiting
• Dehydration
• Cramping pain
• The feeling of an urgent need to defecate
• Passage of 10 to 20 liquid stools each day
• Rebound tenderness may occur in RLQ
• Extraintestinal manifestations:
COMPLICATIONS o Skin lesions (erythema nodosum)
• Intestinal obstruction (stricture formation) o Eye lesions (uveitis)
• Perianal disease o Joint abnormalities (arthritis)
• Fluid and electrolyte imbalance o Liver disease
• Malnutrition from malabsorption
• Fistula (most common: enterocutaneous fistula)
• Abscess formation
ULCERATIVE COLITIS
• Recurrent ulcerative and inflammatory disease of
the mucosal layer of the colon and rectum
• Begins from the rectum and eventually affects entire
colon
• Characteristics:
o Multiple continuous ulcerations PATHOPHYSIOLOGY
o Diffuse inflammations
o Desquamation of colonic epithelium • Ulcerations cause bleeding of the mucosal walls of
the intestine
• Mucosa becomes edematous and inflamed
• Lesions are contiguous, occurring one after the
other fat deposits.
• Abscesses form, and infiltrate is seen in the mucosa
and submucosa, with clumps of neutrophils found in
the lumens of the crypts
• Begins in the rectum and spreads proximally to
involve the entire colon.
• Eventually, the bowel narrows, shortens, and
thickens because of muscular hypertrophy and fat
deposits.
January 30-31, 2023 11
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
ASSESSMENT AND DIAGNOSTIC FINDINGS
• Assess for tachycardia, hypotension, tachypnea,
fever, and pallor
• Assess the level of hydration and nutritional status
• The abdomen is examined for bowel sounds,
distention, and tenderness.
• Laboratory Tests
o Stool Exam
o Fecal Occult Blood Test (FOBT)
• Abdominal X ray Studies
• Sigmoidoscopy or colonoscopy
• Barium enema
COMPLICATIONS
• Toxic megacolon
o Fever NURSING DIAGNOSIS
o Abdominal pain and distention • Diarrhea related to the inflammatory process
o Vomiting • Acute pain related to increased peristalsis and GI
o Fatigue inflammation
• Perforation • Deficient fluid volume related to anorexia, nausea,
• Bleeding and diarrhea
MEDICAL MANAGEMENT • Imbalanced nutrition, less than body requirements,
• Goals: related to dietary restrictions, nausea, and
o Reducing inflammation malabsorption
o Suppressing inappropriate immune • Activity intolerance related to generalized weakness
responses • Risk for impaired skin integrity RT malnutrition and
o Providing rest for a diseased bowel so that diarrhea
healing may take place NURSING INTERVENTIONS
o Improving quality of life • Maintaining Normal Elimination Patterns
o Preventing or minimizing complications • Relieving Pain
• Nutritional therapy • Maintaining Fluid Intake
o Oral fluids and a low residue, high protein, • Maintaining Optimal Nutrition
high calorie diet with supplemental vitamin • Promoting Rest
therapy and iron replacement INFLAMMATORY INTESTINAL DISORDERS
o IV therapy for dehydration and fluid &
APPENDICITIS
electrolyte imbalance
o BRAT diet (Bananas, Rice, Applesauce, • Inflammation of the appendix
Toast) • Most common reason for emergency abdominal
• Pharmacologic therapy surgery
o Antidiarrheals • Can occur at any age, it more commonly occurs
o Antiperistalsis between the ages of 10 and 30 years
o Aminosalicylates (Sulfasalazine)
o Corticosteroids
(Prednisone/Hydrocortisone)
o Immunomodulators (Azathioprine,
Mercaptopurine, Methotrexate,
Cyclosporine)
SURGICAL MANAGEMENT
• Laparoscope-guided strictureplasty
• Intestinal transplant
• Proctocolectomy with ileostomy
• Total Colectomy With Ileostomy
• Continent Ileostomy
• Restorative Proctocolectomy With ileal pouch anal
anastomosis
January 30-31, 2023 12
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
PATHOPHYSIOLOGY MEDICAL MANAGEMENT
• The appendix becomes inflamed and edematous • Appendectomy
• Inflammation increases intraluminal pressure, o May be performed using general or spinal
• Eventually, the inflamed appendix fills with pus. anesthesia with a low abdominal incision
CLINICAL MANIFESTATIONS (laparotomy) or by laparoscopy
• Vague epigastric or periumbilical pain o When perforation occurs, abscess may
form. Treat the abscess initially with
• RLQ pain
antibiotics prior to appendectomy
• Low-grade fever
• Nausea, and sometimes vomiting
• Loss of appetite
• Local tenderness (elicited at McBurney’s point)
• Rebound tenderness
• Rovsing’ssign
• Asymptomatic until the appendix ruptures
o Laparotomy – open surgical exploration of
the abdomen, usually a single large
incision
ASSESSMENT AND DIAGNOSTIC FINDINGS
o Laparoscopy – keyhole surgery; small
• Complete physical examination incision- minimally invasive
• Complete blood count (CBC)
• Abdominal x-ray films
• Ultrasound studies
• CT scans
• Diagnostic laparoscopy
• Pregnancy test
COMPLICATIONS
• Perforation of the appendix, which can lead to:
o Peritonitis
o Abscess formation
• Portal pylephlebitis NURSING MANAGEMENT
• Relieving pain
• Preventing fluid volume deficit
• Reducing anxiety
• Eliminating infection due to the potential or actual
disruption of the GI tract
• Maintaining skin integrity
• Attaining optimal nutrition
• Prepare the patient for surgery (IV access &
antibiotic therapy)
• If there is evidence or likelihood of paralytic ileus, a
nasogastric tube is inserted
• Position patient in a high Fowler’s position post
appendectomy
• Administer Morphine S04 as ordered
January 30-31, 2023 13
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
• Care for the incision and perform dressing changes PATHOPHYSIOLOGY
and irrigations as prescribed • Diverticula form when the mucosa and submucosal
• Avoid heavy lifting post op; May resume normal layers of the colon herniate through the muscular
activity after 2 4 weeks wall because of the ff:
DIVERTICULAR DISEASE o High intraluminal pressure
• A diverticulum is a saclike herniation of the lining o Low volume in the colon (ie, fiber-deficient
of the bowel that extends through a defect in the contents)
muscle layer. o Decreased muscle strength in the colon
• Diverticula may occur anywhere in the small wall (ie, muscular hypertrophy from
intestine or colon but most commonly occur in the hardened fecal masses)
sigmoid colon • Bowel contents can accumulate in the diverticulum
o Diverticulosis –exists when multiple and decompose
diverticula are present without • If obstruction continues, the diverticulum also
inflammation or symptoms. becomes obstructed and then inflamed.
o Diverticulitis – results when food and • The inflammation of the weakened colonic wall of
bacteria retained in a diverticulum produce the diverticulum can cause it to perforate
infection and inflammation that can impede • Abscesses develop and may eventually
drainage and lead to perforation or perforate,leading to peritonitis and erosion of the
abscess formation arterial blood vessels, resulting in bleeding.
• Microperforation of the colon
CLINICAL MANIFESTATIONS
• Diverticulosis
o Bowel irregularity
o Diarrhea
o Nausea
o Anorexia
o Bloating
• Diverticulitis
o Mild to severe pain in LLQ
o Nausea and vomiting
o Fever
o Chills
o Leukocytosis
COMPLICATIONS
• Diverticulosis
o Narrowed large bowel with fibrotic
strictures
o Cramps
o Narrow stools
o Increased constipation
o Intestinal obstruction
• Diverticulitis
o Peritonitis
o Abscess formation
o Bleeding
o Fistulas
o Septicemia
ASSESSMENT AND DIAGNOSTIC FINDINGS
• Colonoscopy
• Abdominal x-ray
• Barium enema
• CBC
• CT scan with contrast
• Erythrocyte sedimentation rate (ESR)
January 30-31, 2023 14
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
MEDICAL MANAGEMENT ETIOLOGY
• Dietary and Pharmacological Management • Bacterial infection
o Initially, clear liquid diet then high-fiber, • Injury or trauma
low-fat diet • Inflammation that extends from an organ outside
o Broad spectrum antibiotics the peritoneal area
o Pain reliever (Opioids) • Appendicitis
o Antispasmodics • Perforated ulcer
• Medical management • Diverticulitis
o Surgery • Bowel perforation
▪ Abscess formation: CT guided PATHOPHYSIOLOGY
percutaneous drainage
▪ One-stage resection/multiple • Leakage of contents from abdominal organs into the
stage resection abdominal cavity
▪ Hartmann’s procedure • Bacterial proliferation occurs
• Edema of the tissue and exudation of fluid develops
• Fluid in the peritoneal cavity becomes turbid with
increasing amounts of protein, white blood cells,
cellular debris, and blood
• An accumulation of air and fluid in the bowel.
NURSING MANAGEMENT
• Maintaining Normal Elimination Patterns
o OFI of 2L per day
o High-fiber diet
• Relieving pain
o Opioids
o Antispasmodic agents (Propantheline CLINICAL MANIFESTATIONS
bromide & Oxyphencyclimine) • Depend on the location & extent of the inflammation
• Monitoring and Managing Potential Complications • Diffuse pain (aggravated with movement)
PERITONITIS • Abdominal tenderness and distention
• Inflammation of the peritoneum, the serous • Muscles become rigid
membrane lining the abdominal cavity and covering • Rebound tenderness
the viscera • Paralytic ileus
• Low-grade fever
• Increased pulse rate
• Hypotension
ASSESSMENT AND DIAGNOSTIC FINDINGS
• CBC (WBC is elevated)
• Serum electrolytes (Altered potassium, sodium,
chloride)
• Abdominal X-ray & ultrasound
• CT scan of abdomen
• Magnetic resonance imaging
• Peritoneal aspiration and culture and sensitivity
January 30-31, 2023 15
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
COMPLICATIONS VIRAL HEPATITIS
• Sepsis • A systemic, viral infection in which necrosis and
• Shock inflammation of the liver cells produce a
• Intestinal obstruction characteristic cluster of clinical, biochemical and
MEDICAL MANAGEMENT cellular changes.
• Fluid and electrolyte replacement • A growing global public health concern:
• Analgesics o Easy to transmit
• Antiemetics o High morbidity
o Loss of time from school and work
• Intestinal intubation and suction
• Oxygen therapy HEPATITIS A
• Antibiotic therapy (Broad-spectrum) • Formerly called “Infectious hepatitis”
SURGICAL MANAGEMENT • Causative agent: Hepatitis A Virus
• Excision • Caused by an RNA virus of the Enterovirus family
• Transmission:
• Resection
o Oral-fecal route
• Repair
o Ingestion of food or liquid infected by the
• Drainage
virus
• Fecal diversion
• Incubation period: between 2-6 weeks, lasting to 4-
NURSING MANAGEMENT
8 weeks
• Vital signs monitoring CLINICAL MANIFESTATIONS
• Assessment of pain as well as fluid and electrolytes • Most are anicteric and asymptomatic
• Relieving pain (Analgesics) • When symptoms appear:
• Proper positioning of patient o Mild, flu-like upper respiratory tract
• Strict I&O monitoring infection
DISORDERS OF THE LIVER o Low grade fever
HEPATITIS o Anorexia (often severe)
• Inflammation of the liver cells resulting from: o Indigestion
o Viral agents o Nausea and vomiting
o Exposure to hepatotoxic drugs (drug- • Late onset symptoms:
induced) o Jaundice
o Bacterial infection o Dark-colored urine
ASSESSMENT AND DIAGNOSTIC FINDINGS
• Hepatitis A antigen
• Hepatitis A virus antibodies
• Analysis of subclasses of immunoglobulins
• ALT
• Bilirubin
• Ultrasound of whole abdomen
PREVENTION
• Scrupulous handwashing
• Safe water supplies
• Proper control of sewage disposal
• Effective and safe HAV vaccines include Havrix and
Vaqta
MEDICAL MANAGEMENT
• During acute phase:
o Bed rest
o Dietary modification
• During anorexia stage:
o Small frequent feedings
o IV fluids with glucose
o Food and fluid levels are necessary to
counteract weight loss and to speed
recovery
January 30-31, 2023 16
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
NURSING MANAGEMENT ASSESSMENT AND DIAGNOSTIC FINDINGS
• Proper diet and bed rest • HBcAg
• Small, frequent feeding • HBeAg
• Enteral feeding if N/V persist • HBsAg – Hepatitis B Surface Antigen: Indicates
• Restrict fat intake acute
• Follow-up blood work • or chronic Hepatitis B or carrier state
• Good personal hygiene • Anti-HBc
• Avoiding alcohol • Anti HBs
• Stressing careful handwashing • Anti HBe
• Environmental sanitation PREVENTION
HEPATITIS B • Interrupt chain of transmission
• Causative agent: Hepatitis B Virus • Active and passive immunization
• HBV can be found in blood, saliva, semen, and • Screening of potential blood donors
vaginal secretions • Disposable sharps
• Mode ofTransmission MEDICAL MANAGEMENT
o Parenteral, sexual, perinatal • Interferon
• HBV is also transferred from carrier mothers to their • Bedrest
infants • Adequate Nutrition
• Transmitted primarily through blood (percutaneous HEPATITIS B VACCINATION
and permucosal routes)
• Recommended for high-risk individuals:
• Incubation period: much longer (1-6 months) than
o Health care workers
HAV
o Hemodialysis patients
RISK FACTORS
• Provides 90% active immunity to healthy persons
• Frequent exposure to blood, blood • Not suitable for people already infected with
• products, or other body fluids Hepatitis B
• Health care workers HEPATITIS IMMUNOGLOBULIN
• Hemodialysis • Provides passive immunity
• Male homosexual and bisexual activity • Recommended for those exposed to HBV
• IV/injection drug use • Must not be infected with Hep B and mist not be
• Close contact with carrier of HBV vaccinated with Hep B Vaccine
• Travel to or residence in area with uncertain PROGNOSIS
sanitary conditions
• Mortality – 10%
• Multiple sexual partners
• Carrier state – 10%
• Recent history of sexually transmitted disease
• Chief cause of cirrhosis and hepatocellular
• Receipt of blood or blood products (eg, clotting
carcinoma
factor concentrate)
CLINICAL MANIFESTATIONS HEPATITIS C
• Causative agent: hepatitis C virus
• Loss of appetite
• Mode of transmission – small amounts of blood
• Dyspepsia
(shared needles, sexual contact, needle prick, HD)
• Abdominal pain
• Incubation period – 15-160 days
• Generalized aching
• Occurrence – endemic worldwide
• Body malaise and weakness
• Malignancy risk – high risk with poor management
• Jaundice (May or may not be evident)
RISK FACTORS
• If jaundice occurs:
o Light-colored stools and dark urine • IV or injection drug users
o Liver may be tender and enlarged to 12 to • Sexually active people with multiple partners
14 cm vertically. • Patients receiving frequent transfusions
o Spleen is enlarged and palpable • Hemodialysis patients
o Posterior cervical lymph nodes may also • Health care personnel
be enlarged
January 30-31, 2023 17
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
CLINICAL MANIFESTATIONS PREVENTION
• 80% are asymptomatic • Proper community sanitation
• Symptoms are same with Hepatitis B • Conscientious individual hygiene at all times
• Milder but longer than Hepatitis B • Safe practices for preparing and dispensing food
MEDICAL MANAGEMENT • Effective health supervision in school, dormitories,
• Prolonged low-dose interferon therapy extended care facilities, barracks, and camps
• Ribavirin • Continuous health education program
PREVENTION • Reporting of every case for viral hepatitis to the
local department
• Hepatitis C screening of blood transfusions
HEPATITIS E
HEPATITIS C
• Causative agent – hepatitis E virus
• Causative agent – hepatitis D virus
• Mode of transmission – oral-fecal
• Reservoir – humans, chimpanzee, pigs
• Incubation period – 15-65 days
• Mode of transmission – parenteral, sexual
• Occurrence – endemic worldwide
• Incubation period – 21-140 days
• Course of illness – 2-6weeks
• Occurrence – only in patients with Hepa B
• Malignancy risk – high risk with poor management LIVER CIRRHOSIS
• A chronic disease of the liver d/t destruction of liver
tissues
• Characterized by replacement of normal liver tissue
with diffuse fibrosis that disrupts the structure and
function of the liver.
• 3 Types:
o Alcoholic cirrhosis
o Postnecrotic cirrhosis
o Biliary cirrhosis
• Chiefly involves the portal and periportal spaces,
where bile canaliculi of each lobe communicate to
form the liver bile ducts.
ETIOLOGY
• Excessive alcohol consumption
• Nutritional deficiency with reduced protein intake
• Exposure to certain chemicals (carbon tetrachloride,
chlorinated naphthalene, arsenic, or phosphorus)
• Infection (Hepatitis), Exposure to infectious
schistosomiasis
• Drugs (hepatotoxic drugs)
• Biliary obstruction (Biliary Atresia)
• Men are twice to be affected than women; But
women are at greater risk of alcohol-induced liver
disease
• Affects mostly between 40 to 60 years
January 30-31, 2023 18
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
PATHOPHYSIOLOGY • Peritonitis
• Characterized by necrosis involving the liver cells
• Gradually replaced by scar tissue
• Eventually, the amount of scar tissue exceeds the
normal functioning liver tissue
• Gastrointestinal Varices
CLINICAL MANIFESTATIONS
• Liver Enlargement
• Portal Obstruction • Edema
• Vitamin Deficiency and Anemia
• Mental Deterioration
OTHER SIGNS AND SYMPTOMS
• Leukopenia
• Increased susceptibility to infection
• Vomiting and nausea
• Esophageal varices
• Reduced calcium
• Caput medusae
• Increased hormones
• Reduced synthesis of vitamin K
• Reduced potassium
• Ascites • Observe for flapping tremors
• Splenomegaly
• Increased skin pigmentation
• Spider angioma
ASSESSMENT AND DIAGNOSTIC FINDINGS
• Serum albumin – tends to decrease in severe
parenchymal liver dysfunction
• Serum globulin – tends to rise in severe
parenchymal liver dysfunction
• Enzyme test (ALT, ASP, AST, GGT) – tends to
increase
• Serum cholinesterase – tends to decrease
• Bilirubin tests – to measure bile excretion or
retention; tends to increase in liver cirrhosis
• Infection
January 30-31, 2023 19
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
• Prothrombin time – tends to be prolonged TYPES
• Ultrasound – to measure difference in density of 1. Cholesterol stones
parenchymal cells and scar tissue o Oval shaped
• Computed Tomography (CT) Scan o Light yellow to dark green color
• Magnetic Resonance Imaging (MRI) o 2-3cm
• Radioisotope Liver Scans
• Liver Biopsy – confirmatory
• Arterial Blood Gas (ABG) – may reveal a
ventilation-perfusion imbalance and hypoxia
MEDICAL MANAGEMENT
• Medications:
o Antacids / Histamine-2 (H2) Antagonists– 2. Pigment stones
to decrease gastric distress and minimize o Small, dark stones
possibility of GI bleeding o Made of bilirubin and calcium salt and
o Vitamins - promote healing of damaged cholesterol
liver cells and improve the patient’s
general nutritional status.
o Potassium-sparing Diuretics
(spironolactone or triamterene) – to
decrease ascites; minimize fluid and
electrolyte changes
3. Segment stones
• Lifestyle change: o Calcium bilirubinate
o Adequate diet o Radiologically visible
o Avoidance of alcohol
NURSING MANAGEMENT
• Promoting Rest
• Improving Nutritional Status
• Providing Skin Care
• Reducing Risk of Injury (Falls and other Injuries)
• Monitoring for Potential Complications
COMPLICATIONS CHOLECYSTITIS
• Bleeding and Hemorrhage • Acute or chronic inflammation of the gallbladder
• Hepatic Encephalopathy – deteriorating mental • Causes pain, tenderness, andrigidity of the upper
status, dementia, abnormal voluntary and right abdomen that may radiate to the midsternal
involuntary movements area or right shoulder.
• Fluid Volume Excess – develop cardiovascular • An empyema of the gallbladder develops if the
abnormalities gallbladder becomes filled with purulent fluid (pus)
DISORDERS OF THE BILIARY TRACT
CHOLELITHIASIS
• Gallstone formation in the gallbladder
• Presence of calculi or gallstones, usually form in the
gallbladder from the solid constituents of bile.
• Vary greatly in size, shape, and composition
• Uncommon in children and young adults but
become more prevalent with increasing age
• Affecting 30% to 40% of people by the age of 80
years.
January 30-31, 2023 20
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
TYPE OF CHOLECYSTITIS CLINICAL MANIFESTATIONS
1. Calculous cholecystitis • (+) PAIN: Abdominal
o 90% of cases of acute cholecystitis • Location: RUQ that radiates to the back, between
o A gallbladder stone obstructs bile outflow the shoulders or front of the chest
2. Acalculous cholecystitis • Precipitated by: High Fat meal (after eating) → N/V
o Acute inflammation in the absence of • Tachycardia
obstruction by gallstone • Murphy’s Sign
o Occurs after major surgical procedures, • Fever, Leukocytosis
severe trauma, or burns • Palpable gallbladder
• BILE STASIS
• Jaundice
• Pruritus
• Tea colored urine
• Clay colored stool
• Decreased bile in the duodenum
• Indigestion
• Decreased digestion of fat
• Vitamin ADEK deficiency
• Steatorrhea
ASSESSMENT AND DIAGNOSTIC FINDINGS
• Abdominal X-ray
ETIOLOGY • Ultrasonography
• Gallbladder stone – gallstone impacted in the cystic • Radionuclide Imaging or Cholescintigraphy
duct • Cholecystography (Oral)
• Bacteria – secondary infection with e.coli etc • ERCP (Endoscopic Retrograde
• Fluid and electrolyte imbalance – fluids & electrolyte Cholangiopancreatography)
alteration after surgery • Percutaneous Transhepatic Cholangiography
• Bile stasis – lack of gallbladder contraction
• Increased fat intake – supersaturation of bile
• Age & gender – 20-50 years old/women
RISK FACTORS (5Fs)
• Female
• Fat
• Forty and above
• Fertile
• Fair
PATHOPHYSIOLOGY
• Obstruction – gallbladder stone obstructs the bile
outflow
• Chemical reaction – remaining bile initiates a
chemical reaction; autolysis and edema
• Compression – compressed blood vessels
compromise vascular supply
January 30-31, 2023 21
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
MEDICAL MANAGEMENT T-TUBE
• Nutritional and Supportive Therapy • Purpose:
o Low Fat Diet o Preserves the patency of the ducts
o Vitamin ADEK replacement o Promotes drainage of excess bile
• Pharmacologic Therapy o Prevents bile leakage in the peritoneal
o meperidine, Anticholinergics, Antiemetics, cavity
ursodeoxycholic acid/chenodeoxycholic • Nursing Intervention:
acid o Position: semi-fowler’s
• Supportive Management o Measure bile output collected every 24 hrs
o NGT connected to low pressure suction o Normal output within 24 hrs: 300 – 500 ml
o NPO during N/V (brownish red/ greenish brown)
• Nonsurgical Removal of Gallstones o Avoid irrigation or aspiration of T-tube
o Dissolving Gallstones o Clamping of T-tube should be before meal
o Stone Removal by Instrumentation as ordered
o Intracorporeal Lithotripsy o If ambulatory, place drainage bag in the
o Extracorporeal Shock Wave Lithotripsy patient’s pocket
SURGICAL MANAGEMENT o secure connections and avoid kinking
• Laparoscopic Cholecystectomy
• Cholecystectomy
• Choledochostomy
• Choledocholithotomy
• Surgical Cholecystostomy
• Percutaneous Cholecystostomy
COMPLICATIONS
• empyema – an empyema of the bladder develops if
the gallbladder becomes filled with purulent fluid
• gangrene – develops because the tissues do not
receive enough oxygen and nourishment at all
• cholangitis – the infection progresses as it reaches
the bile ducts
NURSING MANAGEMENT UNDERGOING
CHOLECYSTECTOMY
• Inform the patient that a small incision or puncture
at the abdomen
• Place the patient in low-fowler’s position
• Promote respiratory function
o Encourage DBCE
o Early ambulation
• Relieve post operative pain
o Splint the abdomen using pillow to prevent
discomfort
• Nutritional support
• Inform the patient about the T-tube
January 30-31, 2023 22
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
PANCREATITIS o Bleeding (cullen’s signs and tuner’s sign) –
hypovolemic shock
• inflammation of the pancreas
• caused by hypersecretion of pancreatic enzymes • Clinical manifestations (CHRONIC)
and obstruction of the bile duct o Recurring attacks of severe upper
• types: acute pancreatitis, chronic pancreatitis abdominal and back pain
• Risk factors o Vomiting
o Penetrating peptic ulcers o Anorexia
o Alcoholism o Weight loss
o Neurogenic factors o Malabsorption
o Contraceptive pills o Steatorrhea
o Renal failure and transplantation o Calcification of the gland
o Endoscopic examination • Assessment and diagnostic test (acute)
o Abnormal organ failure o Serum Amylase
o Tract biliary disease o Serum Lipase
o Increased cholesterol o Urinary amylase
o Thyroid problem o Serum calcium
o Infection (bacterial/viral), ischemic disease o UA
o Surgical blunt abdominal trauma o CBC/PC
• Pathophysiology o Abdominal x-ray
o Ultrasound
o CT-scan
o C-reactive protein
• Assessment and diagnostic test (chronic)
o ERCP
o Ultrasound
o CT-Scan
• Clinical manifestations o Glucose tolerance test
o Location – miedepigastrium, radiating on • Medical management (PANCREATITIS)
the back o Pain management, PPI
o Precipitated by eating a heavy meal, o Antacids, avoid alcohol
drinking alcohol, fatty meal, when the o NGT suctioning
patient lies on his back o Cimetidine (H2 blockers)
o Pain is relieved by resting on his knees o Replacement of fluids (IVF)
and upper chest o Eliminate pancreatic secretions (patient on
• Clinical manifestations (ACUTE) strict NPO)
o Abdominal distention o Antibiotics, antiemetics
o Poorly-defined palpable mass o TPN
o Nausea and vomiting o Insulin
o Decreased peristalsis o Transfusion of blood
o Fever o Increase caloric intake
o Jaundice o Surgery
o Pruritus ▪ Laparotomy (acute)
o Vitamin ADEK deficiency ▪ Pancreaticojejunostomy or the
o Mental confusion Roux-en-Y (chronic)
o Hypocalcemia ACUTE PANCREATITIS
o Hyperglycemia – DM • Sudden onset of pancreatic inflammation
o Hypotension
January 30-31, 2023 23
MIDTERMS
2nd Semester
Lecture
Calatrava, Mae Abigael BSN 3
MEDICAL SURGICAL NURSING (NCM 3260)
• Classification:
o Interstitial/Edematous Pancreatitis
o Acute Hemorrhagic Pancreatitis
MILD ACUTE PANCREATITIS
• Characterized by edema and inflammation confined
to the pancreas
• At risk for hypovolemic shock
• Fluid and electrolyte disturbances
• Sepsis
SEVERE ACUTE PANCREATITIS
• More widespread and complete enzymatic digestion
of the gland
• Local blood vessels damage
• Necrotic tissue
• Local complications: pancreatic cysts/abscess,
acute fluid collections
• Systemic complications: organ failure
• Etiology
o Biliary Tract Disease (80%)
o Longterm alcohol use
o Bacterial/Viral Infection
o Blunt Abdominal Tarauma
o Peptic Ulcer Disease (PUD)
o Ischemic Vascular Disease
CHRONIC PANCREATITIS
• Inflammatory disorder characterized by progressive
anatomic and functional destruction of the pancreas
• Pancreatic cells are replaced with fibrous tissue
• Etiology
o Alcohol consumption
o Malnutrition
o Adult men
• Clinical manifestations
o Severe recurrent upper abdominal pain
o Vomiting
o Weight loss
o Frequent, frothy, foul smelling stool
• Assessment and diagnostic findings
o ERCP
o Ultrasound
o CT-Scan
o Glucose Tolerance Test
• Medical management
o Pain Management
o Alcohol Avoidance
o Pancreatojejunostomy
January 30-31, 2023 24
You might also like
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Cqi Indicators As Per Nabh 5Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyDocument3 pagesCqi Indicators As Per Nabh 5Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyNatasha Bhasin91% (11)
- Grand Rounds Amdekar PDFDocument324 pagesGrand Rounds Amdekar PDFBhagyashree SawardekarNo ratings yet
- Diarrhoea - MRCEM SuccessDocument7 pagesDiarrhoea - MRCEM SuccessGazi Sareem Bakhtyar AlamNo ratings yet
- 4 Current Management of Esophageal Atresia and Tracheoesophageal FistulaDocument38 pages4 Current Management of Esophageal Atresia and Tracheoesophageal FistulaTurabayo Jean LéonardNo ratings yet
- Large Bowel Obstruction by Nic MDocument42 pagesLarge Bowel Obstruction by Nic MRisky OpponentNo ratings yet
- Biostat 2020 62 QDocument270 pagesBiostat 2020 62 Q'محمد علي' محمد لافيNo ratings yet
- A Simple Guide to Small Intestinal Bacterial Overgrowth, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Small Intestinal Bacterial Overgrowth, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Drug Study Atropine SulfateDocument1 pageDrug Study Atropine Sulfateirhizzp75% (8)
- NCM 116 W1 Reading HandoutDocument13 pagesNCM 116 W1 Reading Handoutriza sarmientoNo ratings yet
- Nursing Care Plan Nausea & VomitingDocument3 pagesNursing Care Plan Nausea & Vomitingderic87% (47)
- Diarrhea PPTDocument82 pagesDiarrhea PPTIshwar HavaragiNo ratings yet
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesRating: 1 out of 5 stars1/5 (1)
- A Simple Guide to Short Bowel Syndrome, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Short Bowel Syndrome, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Nursing Management of Gastro Intestinal Problem 2Document20 pagesNursing Management of Gastro Intestinal Problem 2wyneNo ratings yet
- Unit Ix: Nursing Management of Patients With Gi Disorders: Topic: DiarrheaDocument13 pagesUnit Ix: Nursing Management of Patients With Gi Disorders: Topic: Diarrheaayushi rainaNo ratings yet
- Abnormalities of Fecal Elimination SgmacDocument4 pagesAbnormalities of Fecal Elimination SgmacRachelle DelantarNo ratings yet
- FecalysisDocument7 pagesFecalysisMiki NishiharaNo ratings yet
- A. Related FactorsDocument10 pagesA. Related FactorsEva YuliaNo ratings yet
- 116 - Alterations in GI EliminationDocument12 pages116 - Alterations in GI EliminationGino-o, KyleNo ratings yet
- GastritisDocument3 pagesGastritisAmoroso, Marian Corneth D.No ratings yet
- Diarrhea (Diare)Document9 pagesDiarrhea (Diare)Eki MegaraniNo ratings yet
- Chronic Diarrhoea SaqlainDocument116 pagesChronic Diarrhoea SaqlainMohammed SaqlainNo ratings yet
- 22 Manuscript Intestinal ObstructionDocument8 pages22 Manuscript Intestinal Obstructionkint manlangitNo ratings yet
- NCM 3260 - Gastro - Intestinal ObstructionDocument36 pagesNCM 3260 - Gastro - Intestinal ObstructionCherish Marie HurbodaNo ratings yet
- (Roselle Balicas) - Chrome - LNKDocument8 pages(Roselle Balicas) - Chrome - LNKRose CasBalNo ratings yet
- Diarrhea NCP Pedia WardDocument4 pagesDiarrhea NCP Pedia WardKyle DapulagNo ratings yet
- DiareDocument5 pagesDiarefarisNo ratings yet
- Understanding Medical Surgical Nursing (2) - 0001-0001Document1 pageUnderstanding Medical Surgical Nursing (2) - 0001-0001Anas TasyaNo ratings yet
- Acute Diarrhoea and VomitingDocument43 pagesAcute Diarrhoea and VomitingAdriana AfiqahNo ratings yet
- PBL 6 (ALS) - Food PoisoningDocument9 pagesPBL 6 (ALS) - Food Poisoningfarah fadzilNo ratings yet
- PHCP Lec Topic 4 To 10Document19 pagesPHCP Lec Topic 4 To 10armand bayoranNo ratings yet
- 9 Intestinal ObstructionDocument7 pages9 Intestinal ObstructionMAH pedNo ratings yet
- GastroenteritisDocument20 pagesGastroenteritisSuresh ThanneruNo ratings yet
- 62 DiarrheaChronic MGHG MIMG MFM 20161229Document10 pages62 DiarrheaChronic MGHG MIMG MFM 20161229Wei HangNo ratings yet
- Management of Patients With Intestinal and RectaldisordersDocument16 pagesManagement of Patients With Intestinal and RectaldisordersintotheunknownNo ratings yet
- Pathophysiology: Etiology: Salmonella, Shigella, Staphylococcus, Campylobacter Jejuni, ClostridiumDocument5 pagesPathophysiology: Etiology: Salmonella, Shigella, Staphylococcus, Campylobacter Jejuni, ClostridiumHanna La MadridNo ratings yet
- Gastroenteritis - J.J. Kambona (Compatibility Mode)Document43 pagesGastroenteritis - J.J. Kambona (Compatibility Mode)shibutaNo ratings yet
- Chronic Diarrhea-HTKDocument63 pagesChronic Diarrhea-HTKcerenblgstrNo ratings yet
- Irritable Bowel Syndrome (IBS)Document7 pagesIrritable Bowel Syndrome (IBS)Hisyam DinGanuNo ratings yet
- Pathology: One By: Bdulrahman Aljadoa & Anar AljebreenDocument7 pagesPathology: One By: Bdulrahman Aljadoa & Anar AljebreenRizki WahyuniNo ratings yet
- Diarrhea PDFDocument7 pagesDiarrhea PDFLhie SamaNo ratings yet
- INTESTINEDocument98 pagesINTESTINEDeepika LingamNo ratings yet
- Bowel ObstructionsDocument14 pagesBowel ObstructionsDicky Aditya DwikaNo ratings yet
- Diarrhea 2Document20 pagesDiarrhea 2Amisalu NigusieNo ratings yet
- Artikel Diare Wakhidah Umi SDocument13 pagesArtikel Diare Wakhidah Umi SWakhidah Umi SholikhahNo ratings yet
- Fecal AnalysisDocument23 pagesFecal AnalysisBabylene MamauagNo ratings yet
- Constipation Diarrhea Fecal IncontinenceDocument40 pagesConstipation Diarrhea Fecal IncontinenceLiza Marie IgnacioNo ratings yet
- Alterations in Nutrition, Elimination and Sexuality - Large Bowel DysfunctionDocument9 pagesAlterations in Nutrition, Elimination and Sexuality - Large Bowel DysfunctionjazmemonNo ratings yet
- Acute If 4 Weeks in DurationDocument9 pagesAcute If 4 Weeks in DurationSalsabila Rahma FadlillahNo ratings yet
- Irritable Bowel Syndrome Malabsorption SyndromeDocument29 pagesIrritable Bowel Syndrome Malabsorption SyndromeLiza Marie IgnacioNo ratings yet
- MS Lec Ibs and MSDocument3 pagesMS Lec Ibs and MSTrishia Camille GuillermoNo ratings yet
- Persistent Diarrhea-Sept2009Document43 pagesPersistent Diarrhea-Sept2009Mega Dwi PutriNo ratings yet
- 4 NCM+116n+Lecture+Care+of+the+Clients+with+Problems+GI+Function+and+NutritionDocument10 pages4 NCM+116n+Lecture+Care+of+the+Clients+with+Problems+GI+Function+and+NutritionKylle AlimosaNo ratings yet
- Principles of Alimentary Tract Dysfunction: Internal Medicine - Part I - 4 Year 2019Document3 pagesPrinciples of Alimentary Tract Dysfunction: Internal Medicine - Part I - 4 Year 2019EhanghariEl-hanghariNo ratings yet
- Diet in Gastro Intestinal and Liver Disorders: ObjectivesDocument19 pagesDiet in Gastro Intestinal and Liver Disorders: ObjectivesIyappan SubramaniNo ratings yet
- Intestinal ObstructionDocument42 pagesIntestinal ObstructionSaurabh SharmaNo ratings yet
- Problem 5 GIT Kelompok 16Document116 pagesProblem 5 GIT Kelompok 16Andreas AdiwinataNo ratings yet
- Intestinal Diseases in Cattle 2023Document30 pagesIntestinal Diseases in Cattle 2023Krystyna WędrychowskaNo ratings yet
- Osmotic Diarrhoea: Difficile)Document4 pagesOsmotic Diarrhoea: Difficile)Marwan M.No ratings yet
- BSN 3e Concept PaperDocument29 pagesBSN 3e Concept PaperCherish Marie HurbodaNo ratings yet
- NCM 3260 - Gastro - Intestinal ObstructionDocument36 pagesNCM 3260 - Gastro - Intestinal ObstructionCherish Marie HurbodaNo ratings yet
- Gastro Inflammatory Bowel DiseasesDocument39 pagesGastro Inflammatory Bowel DiseasesCherish Marie HurbodaNo ratings yet
- BSN 3e Concept PaperDocument29 pagesBSN 3e Concept PaperCherish Marie HurbodaNo ratings yet
- Testing For Tuberculosis (TB) : Tuberculin Skin Test (TST)Document2 pagesTesting For Tuberculosis (TB) : Tuberculin Skin Test (TST)Aluh L DiniNo ratings yet
- Thromboembolic Disease PDFDocument5 pagesThromboembolic Disease PDFBáĦẳá Y. Ẳl-mársǾúmiNo ratings yet
- Otovent Patient BrochureDocument2 pagesOtovent Patient BrochureAleksandar MojićNo ratings yet
- Extreme Preterm Premature Rupture of Membranes: KSM Obstetri Dan Ginekologi Rumah Sakit Umum Pusat PersahabatanDocument27 pagesExtreme Preterm Premature Rupture of Membranes: KSM Obstetri Dan Ginekologi Rumah Sakit Umum Pusat Persahabatanrilla saeliputriNo ratings yet
- Appendix DuplicationDocument3 pagesAppendix DuplicationMario TrejoNo ratings yet
- Drugs of ChoiceDocument2 pagesDrugs of ChoiceGian Carla SoNo ratings yet
- Abdominal Pain in Children - Dr. Hermanto SP - BaDocument41 pagesAbdominal Pain in Children - Dr. Hermanto SP - Bajimmy_junNo ratings yet
- Pain Terms: A Current List With Definitions and Notes On UsageDocument9 pagesPain Terms: A Current List With Definitions and Notes On UsagealexandruNo ratings yet
- Sepsis Bundle by DR - ZakiDocument3 pagesSepsis Bundle by DR - Zakizaki ansariNo ratings yet
- Pediatrics RemarksDocument62 pagesPediatrics RemarksGÖKSU SAYGILINo ratings yet
- Association Between Liver Cirrhosis and Diabetes Mellitus: A Review On Hepatic OutcomesDocument15 pagesAssociation Between Liver Cirrhosis and Diabetes Mellitus: A Review On Hepatic Outcomesdoremi miredoNo ratings yet
- Aanjan LabsDocument33 pagesAanjan LabsMeghanath PandhikondaNo ratings yet
- Immune Responses, and TransplantationDocument7 pagesImmune Responses, and TransplantationJoyzoeyNo ratings yet
- Leg English PDFDocument1 pageLeg English PDFBracelethNicole E. NicolasNo ratings yet
- Bepen VKDocument5 pagesBepen VKelcapitano vegetaNo ratings yet
- Name of The Course:-M.Phil, Economics: Result of Delhi University Entrance Test (DUET) - 2018Document5 pagesName of The Course:-M.Phil, Economics: Result of Delhi University Entrance Test (DUET) - 2018Saiganesh RameshNo ratings yet
- Investigations For PneumoniaDocument27 pagesInvestigations For PneumoniaRoshana Mallawaarachchi0% (1)
- Parameatal Cyst :A Case ReportDocument3 pagesParameatal Cyst :A Case ReportDr.ankit AnandNo ratings yet
- CCL 029 029a Child Medical Record Immunization History Health AssessmentDocument3 pagesCCL 029 029a Child Medical Record Immunization History Health Assessmentapi-311935573No ratings yet
- Plasma ExpandersDocument4 pagesPlasma ExpandersNix EnarioNo ratings yet
- Neurosurgery Lecture Notes: Abdul Gofar SastrodiningratDocument14 pagesNeurosurgery Lecture Notes: Abdul Gofar SastrodiningratAnggita Setya LudtianingmaNo ratings yet
- Document PDFDocument11 pagesDocument PDFYANDA PELIA ANo ratings yet
- Milia AriaDocument8 pagesMilia AriaAtsabitFarisNo ratings yet
- Goljan Errata SheetDocument11 pagesGoljan Errata SheetVishala MishraNo ratings yet
- NR 325 Diabetes Power-Student Copy1118Document39 pagesNR 325 Diabetes Power-Student Copy1118John MixerNo ratings yet