Professional Documents
Culture Documents
(ANES) Sat 04 Cardiovascular Drugs For Resuscitation (A2021)
Uploaded by
Ricky Justin NgoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(ANES) Sat 04 Cardiovascular Drugs For Resuscitation (A2021)
Uploaded by
Ricky Justin NgoCopyright:
Available Formats
ANESTHESIOLOGY
CARDIOVASCULAR DRUGS FOR RESUSCITATION
Kristine R. Gonzaga, MD, DPBA, FPSA
First Loop | 1 August 2020
Note. Green – Facilitator’s notes and comments • Oxygenate
TABLE OF CONTENTS
I. Components of Systemic Approach for ACLS • Monitor
A. Conscious and Breathing
B. Unconscious: BLS Survey • IV/IO
C. Simplified ACLS Cardiac Arrest Algorithm • Treat
D. Return of Spontaneous Circulation (ROSC)
1. Oxygenate
• Provide supplemental oxygenation
• If the oxygen is less than 94% (90% for acute coronary syndrome),
provide supplemental oxygen
o Nasal cannula 2-4 LPM
o Simple face mask 6-10 LPM
o Non-rebreather mask 11-15 LPM
▪ Only one that will give you an FiO2 of 100%.
▪ Provides O2 via high flow.
▪ Pressure in the mask is lower than the atmospheric air (21%
O2) pressure. Excess will go out.
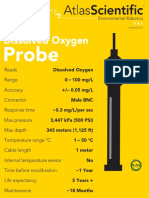
FiO2 of Supplemental Oxygen Delivery
• Nasal cannula – Low flow
• If you want to give higher dose of oxygen, use a nonrebreathing face
(See appendix for clearer view.) mask.
COMPONENTS OF SYSTEMIC APPROACH FOR ACLS Device Flow Rates Delivered O2
Nasal cannula 1 L/min 21%-24%
2 L/min 25%-28%
3 L/min 29%-32%
4 L/min 33%-36%
5 L/min 37%-40%
6 L/min 41%-44%
Simple oxygen 6-10 L/min 35%-60%
face mask
Face mask with O2 6 L/min 60%
reservoir 7 L/min 70%
(nonrebreathing 8 L/min 80%
mask) 9 L/min 90%
10-15 L/min 95%-100%
2. Monitor
• Hook the patient to the cardiac monitor
(See appendix for clearer view.)
• Unconscious, not breathing, and pulseless, do BLS survey.
• Unconscious, not breathing, pale, do BLS survey.
• Conscious, breathing, talking to you, do ACLS Survey.
• Initial Impression
o Consciousness
o Breathing
o Color
• Primary Assessment (ABCDE)
o Airway
o Breathing (Respiratory rate, work of breathing, SpO2, breath
sounds)
o Circulation (Heart rate, blood pressure, central and peripheral 3. IV/IO (Vascular Access)
pulses, CRT) • Establish a vascular access
o Disability (AVPU/GCS, pupillary response, glucose) • Intravenous – Antecubital veins
o Exposure (Temperature, bleeding, burns, trauma, medical alert o Easiest to access
bracelet) o If you cannot insert after 2 attempts in a critically ill patient, do
• Secondary Assessment (SAMPLE, Hs and Ts) intraosseous access since the blood vessels will constrict in a
o Signs and symptoms hypotensive patient.
o Allergies • Intraosseous – Humeral head, sternum, distal femur, proximal tibia,
o Medications distal tibia
o Past medical history o Contraindications: Crush injuries on the site, infections on the
o Last meal site, degenerative bone disorder (osteogenesis imperfecta), if you
o Events have previously inserted on that bone (e.g., If you inserted already
o Hs and Ts but failed on the right proximal tibia, do not attempt to do it in the
right distal tibia. Use the left side instead)
A. Conscious and Breathing
• Visualize, verbalize, vital signs 4. Treat
o Visualize: Is he stable? Is he in cardiorespiratory distress? • Identify and manage the patient’s ECG rhythm
o Verbalize: Ask the patient how he is feeling, his chief complaint.
o Vital signs: HR, BP, RR, T, SpO2
Group 2 Clinical Clerks 1 of 8
ANESTHESIOLOGY CARDIOVASCULAR DRUGS FOR RESUSCITATION
Sinus Bradycardia Supraventricular Tachycardia
• Rhythm is slow (<60/min) • Rhythm is fast (>160/min)
• P waves are present • P waves are absent
• Each P wave is followed by a regularly occurring QRS • QRS is regularly occurring and narrow in configuration
• PR intervals are normal (≤0.2 s)
Treatment for Fast Rhythms (Narrow Complex Tachycardia)
Sinus Bradycardia with 1st Degree AV Block
• All fast rhythms should be treated since the heart cannot go fast for
• Fixed, prolonged PR interval (>0.2 s) too long.
• No dropped beats • Stable
o Physiologic
▪ Vagal maneuver
▪ Carotid massage
• If there are no contraindications (history of coronary artery
disease, coronary bruit), do it unilaterally for 5-10
Sinus Bradycardia with 2nd Degree AV Block Type 1 seconds.
• Dropped beats are present ▪ Cough/strain
• Progressive lengthening of PR interval until dropped beat • If there is a contraindication for carotid massage
o Pharmacologic
▪ If physiologic vagal maneuver is ineffective to convert fast
rhythm.
▪ Adenosine
• Rapid IV bolus (because of its short half-life)
• Initial dose: 6 mg
Sinus Bradycardia with 2nd Degree AV Block Type 2
• Second dose: 12 mg
• Dropped beats are present
• Unstable (SBP < 90 mmHg, stable SVT becomes unresponsive to
• Constant and fixed PR interval until dropped beat
pharmacologic agents)
o Sedate (if time permits)
▪ Diazepam
▪ Midazolam
▪ Etomidate
▪ Propofol
Sinus Bradycardia with 3rd Degree AV Block o Synchronized cardioversion
• Both atrial rhythm and ventricular rhythm are regular but independent ▪ Energy dose
(dissociated) from one other • Atrial fibrillation – 120-200 J
• SVT – 50 J initial (next dose is escalating, 100, 150, 200)
Ventricular Tachycardia with Pulse
• Rhythm is fast (>160/min)
• P waves are absent
• QRS is regularly occurring and wide in configuration
Treatment for Slow Rhythms (Symptomatic and Unstable)
• Do not treat all slow rhythms. In some people, they may have normal
rhythms (athlete, old persons using beta blockers).
• However, if they are symptomatic (dizziness, difficulty of breathing),
have unstable BP (SBP < 90 mm Hg) and have slow rhythms, treat.
• All Trained Dogs Eat
• Atropine sulfate
o Dose: 0.5 mg Treatment for Fast Rhythms (Wide Complex Tachycardia)
o Max: 3 mg
• Stable
o Total: 6 doses
o Seek expert consultation
o Time interval: Every 3 to 5 minutes
o You can try physiologic maneuvers, but usually is ineffective.
o Low degree blocks are responsive to atropine
o Pharmacologic
▪ Sinus bradycardia
▪ Amiodarone infusion
▪ 1st degree AVB
• Dose: 150 mg
▪ 2nd degree AVB Type 1
o Responds by increasing heart rate to achieve an SBP of at least • Duration: 10 mins (for 2 doses)
90 mm Hg • Unstable
o High degree blocks (2nd degree AVP Type 2 and 3rd degree AVB) o Sedate
are unresponsive to atropine and makes the heart more ▪ Diazepam
bradycardic ▪ Midazolam
• Transcutaneous pacing (TCP) ▪ Etomidate
o Put pacer pads ▪ Propofol
o Set rate o Synchronized cardioversion
o Set mAMP ▪ Energy dose
o Pace (achieve complete capture) • V Tach – 100 J initial (if ineffective, give next dose at a
o Confirm pulse higher level, 150, 200)
• Dopamine infusion
o Dose: 2-20 mcg/Kg/min B. Unconscious: BLS Survey
• Epinephrine infusion • Responsiveness: No response?
o Titrate to patient response • Ask for help: Help! Someone, help!
o Dose: 2-10 mcg/min or 0.1-0.5 mcg/Kg/min
Group 2 Clinical Clerks 2 of 8
ANESTHESIOLOGY CARDIOVASCULAR DRUGS FOR RESUSCITATION
• Carotid pulse simultaneously with breathing: 5-10 seconds. No 1. Ventricular Fibrillation
pulse? No or abnormal breathing? • P waves are absent
• Call ERS. Activate emergency response and get an AED/defibrillator. • QRS are present and highly disorganized and chaotic
• Start high quality CPR
1. Critical Elements of a High-Quality CPR
• Push hard: 2-2.4 in (5-6 cm)
• Hand technique: 2 hands (one on top of the other) on the lower half
of the sternum
• Push fast: 100-120/min 2. Pulseless Ventricular Tachycardia
• Allow complete chest recoil. Avoid leaning on the chest between • Rhythm is fast (>160/min)
compressions. • P waves are absent
• Minimize interruptions. Limit to <10 s • QRS is regularly occurring and wide in configuration.
• Avoid excessive ventilation. 2 breaths (using bag-mask device) • Patient is pulseless.
after every 30 compressions
• Priority in cardiac arrest: Compressions (C, then A and B)
Chest Compression Fraction (CCF)
• One of the most important factors for achieving successful outcomes
is to minimize the frequency and duration of interruptions in chest
compressions, thereby maximizing coronary perfusion and blood flow Time-Sensitive Model of Ventricular Fibrillation
during CPR • Electrical Phase
o First 5 minutes of arrest
• When is CPR often interrupted or delayed? o Early defibrillation is critical
o Rescue breaths o High oxygen consumption rapidly depletes myocardial ATP
o Pulse check • Hemodynamic Phase
o Rhythm analysis o Next 5 minutes
o Defibrillation o Perfusing the myocardium and brain with oxygenated blood is
• Measurement of the percentage of time in which chest compressions critical (effective chest compressions help replete or delay
are done by rescuers during a cardiac arrest reductions in ATP by generating adequate coronary perfusion to
restore myocardial blood flow)
𝑇𝑜𝑡𝑎𝑙 𝑡𝑖𝑚𝑒 𝑜𝑓 𝑐ℎ𝑒𝑠𝑡 𝑐𝑜𝑚𝑝𝑟𝑒𝑠𝑠𝑖𝑜𝑛𝑠 (ℎ𝑎𝑛𝑑𝑠 − 𝑜𝑛 𝑡𝑖𝑚𝑒) • Metabolic Phase
𝐶𝐶𝐹 = o Beyond 10 minutes
𝑇𝑜𝑡𝑎𝑙 𝑟𝑒𝑠𝑢𝑠𝑐𝑖𝑡𝑎𝑡𝑖𝑜𝑛 (𝑐𝑜𝑑𝑒) 𝑡𝑖𝑚𝑒
o Ischemic injury to the heart is so great that is not clear what
interventions will be successful
3. Shock First vs CPR First
• Adult witnessed cardiac arrest and AED/defibrillator is immediately
available, shock first. Then, start CPR.
• Adult did not witness cardiac arrest or AED is not immediately
available, start CPR while AED is being retrieved and while it is being
applied to the victim
• Target: 0.6 – 0.8
o In a 10-minute code: 4. Shockable Arrest Rhythms
360 𝑠 480 𝑠 • How much shock you give depends on the defibrillator
0.6 = 0.8 = o Monophasic: 300J
600 𝑠 600 𝑠
o Biphasic: 200J
o In a 2-minute code: • After first shock, do not give any drugs because the primary treatment
72 𝑠 96 𝑠 for shockable rhythms is shock
0.6 = 0.8 =
120 𝑠 120 𝑠 • Epinephrine for its α2 effect for vasoconstriction.
o Diluted for faster delivery to the periphery.
2. CPR with an Advanced Airway (Intubated Patients)
• In the time of COVID, it is recommended to intubate the patients before
you start compressions.
• Chest compressions: Continuous, uninterrupted. At 100-120/min
• Ventilation: 1 breath every 6 seconds (10 breaths/min)
• Why not hyperventilate?
o ↑ Intragastric pressure: Prone to aspiration (BMV)
o ↑ Intrathoracic pressure: ↓ Venous return
o ↓ Carbon dioxide in the brain: Cerebral vasoconstriction (↓ blood
flow)
C. Simplified ACLS Cardiac Arrest Algorithm
(See appendix for clearer view.)
5. 2018 AHA Focused Update on ACLS Use of Antiarrhythmic
Drugs During and Immediately and After Cardiac Arrest
• During resuscitation from adult VF or pulseless VT cardiac arrest
o Amiodarone and lidocaine recommendation
▪ Amiodarone or lidocaine may be considered for VF or
pulseless VT that is unresponsive to defibrillation. These
drugs may be particularly useful for patients with witnessed
arrest, for whom time to drug administration may be shorter
(Class IIb; Level of Evidence B-R).
(See appendix for clearer view.)
Group 2 Clinical Clerks 3 of 8
ANESTHESIOLOGY CARDIOVASCULAR DRUGS FOR RESUSCITATION
• Lidocaine is an alternative.
o First dose: 1-1.5 mg/Kg
o Second dose: 0.5-0.7 mg/Kg
o Magnesium recommendation
▪ The routine use of magnesium for cardiac arrest is not
recommended in adult patients (Class III: No benefit; Level
of Evidence C-LD). Magnesium may be considered for
torsade de pointes (i.e., polymorphic VT associated with
long QT interval) (Class IIb; Level of Evidence C-LD).
1. 5-Point Auscultation
• Primary confirmation of endotracheal tube placement
• Start at epigastric area. There should be no gurgling sounds. If there
are gurgling sounds, the tip of ETT has entered the esophagus or
stomach. Remove and reinsert ETT.
• Equal sounds on the bases and apices.
o If more on the right, it’s on the airway but entered the right main
bronchus. Deflate a little, then pull out a few cm until equal.
(See appendix for clearer view.)
6. Asystole
• Flatline
2. Waveform Capnography
• Secondary confirmation by detecting carbon dioxide
7. Pulseless Electrical Activity (PEA) • Uses:
• Rhythm is regular o Confirms correct placement of advanced airway
• P waves are present o Reflects effectiveness of chest compressions during CPR
• Each P wave is followed by a regularly occurring QRS ▪ Have at least 10 mm Hg
• Patient is pulseless ▪ If 5-8 mm Hg compressions are ineffective
• Any organized rhythm without a pulse ▪ If 35-40 mm Hg, there is ROSC
o Predicts return of spontaneous circulation
Treatment for Asystole and PEA
• Start high-quality CPR
• Give epinephrine (every 3 to 5 minutes or every other cycle)
• Treat reversible causes of cardiac arrests (Hs and Ts)
o The earlier you identify, the greater the chance that the patient will
revive.
Upstroke is exhalation. Downstroke is inhalation.
3. Rescue Breathing
Airway Devices Ventilation during Ventilation during
Cardiac Arrest Respiratory Arrest
Bag-mask 2 ventilations after
every 30 chest
1 ventilation every
compressions
5-6 seconds
Any advanced 1 ventilation every 6
(10-12 breaths/min)
airway seconds
(10 breaths/min)
4. Addressing Circulation
(See appendix for clearer view.) • If there are no contraindications, give fluids first.
o 1-2 PNSS/PLRS
D. Return of Spontaneous Circulation (ROSC) • Monitor VS. If it has not reached at least an SBP of 90 mm Hg or has
• Priorities: renal or cardiac problems, add or start vasopressors.
o Optimize oxygenation and ventilation by managing airway and
breathing
▪ If not breathing spontaneously, give advanced airway.
Group 2 Clinical Clerks 4 of 8
ANESTHESIOLOGY CARDIOVASCULAR DRUGS FOR RESUSCITATION
(See appendix for clearer view.)
5. Targeted Temperature Management (TTM)
• If patient appears comatose
• Cool down the brain to decrease metabolism, allowing the brain to rest
• Give 30 mL/Kg 4OC PNSS/PLRS for 30 minutes
• Targeted temperature between 32OC and 36OC selected and
achieved, then maintained constantly for at least 24 hours
• Improvement in neurologic outcome for those in whom hypothermia
was induced
• Do post arrest care after
o NGT to decompress the stomach
o Urinary catheter to check for urine output
o ECG
o Chest x-ray
o Insert central line
o Transfer patient to ICU
Group 2 Clinical Clerks 5 of 8
ANESTHESIOLOGY CARDIOVASCULAR DRUGS FOR RESUSCITATION
Group 2 Clinical Clerks 6 of 8
ANESTHESIOLOGY CARDIOVASCULAR DRUGS FOR RESUSCITATION
Group 2 Clinical Clerks 7 of 8
ANESTHESIOLOGY CARDIOVASCULAR DRUGS FOR RESUSCITATION
Group 2 Clinical Clerks 8 of 8
You might also like
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsFrom EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNo ratings yet
- Bantuan Hidup Dasar Dan Lanjut: BHD-BHLDocument38 pagesBantuan Hidup Dasar Dan Lanjut: BHD-BHLIda Benecia DeseNo ratings yet
- Oxygen Therapy BasicsDocument14 pagesOxygen Therapy BasicsCabdiNo ratings yet
- Oxygen TherapyDocument33 pagesOxygen Therapyالغائب الحاضرNo ratings yet
- Oxygen Delivery Systems: Muhimbili National Hospital Critical Care OrientationDocument15 pagesOxygen Delivery Systems: Muhimbili National Hospital Critical Care OrientationfadhiliNo ratings yet
- Oxygen Therapy: Adel Alrihili BSN-RNDocument36 pagesOxygen Therapy: Adel Alrihili BSN-RNmacmohitNo ratings yet
- Terapi Oksigen Dan Tata Laksana Jalan NapasDocument20 pagesTerapi Oksigen Dan Tata Laksana Jalan NapaspiniNo ratings yet
- Terapi Oxygen Pada Pasien Covd-19Document24 pagesTerapi Oxygen Pada Pasien Covd-19normamNo ratings yet
- Ncma113-Finals Modules SummariesDocument3 pagesNcma113-Finals Modules Summariesroldanmarygrace023No ratings yet
- Terapi Oksigen Dan Tata Laksana Jalan NapasDocument23 pagesTerapi Oksigen Dan Tata Laksana Jalan NapasThivyaroobiniNo ratings yet
- Oxygen TherapyDocument2 pagesOxygen TherapyPhilip MusonyeNo ratings yet
- 7-Hypoxia Is A KillerDocument33 pages7-Hypoxia Is A KillerChamindraNo ratings yet
- Oxygen TherapyDocument41 pagesOxygen TherapyYOGAKRISHNANNo ratings yet
- Oxygen Therapy Principles and PracticeDocument34 pagesOxygen Therapy Principles and PracticeMark Anthony AlcantaraNo ratings yet
- DR Lodha Oxygen Therapy in Covid-19 PedsDocument30 pagesDR Lodha Oxygen Therapy in Covid-19 PedsBhoomika PandeyNo ratings yet
- DIXION Practice Anesthesia WorkstationsDocument7 pagesDIXION Practice Anesthesia WorkstationsDharma PoudelNo ratings yet
- Oxygen TherapyDocument59 pagesOxygen TherapyRosi AmaliaNo ratings yet
- Oxygen TherapyDocument33 pagesOxygen TherapySaudah IbrahimNo ratings yet
- Principles of oxygen therapy in the newbornDocument52 pagesPrinciples of oxygen therapy in the newbornKhirzaNo ratings yet
- Мэдээгүйжүүлэх аппаратDocument2 pagesМэдээгүйжүүлэх аппаратЖавхланбаяр ЖаргалсайханNo ratings yet
- Ncma113 Lec & Lab From Dash 10 - Summer Final 2021: Oxygen TherapyDocument12 pagesNcma113 Lec & Lab From Dash 10 - Summer Final 2021: Oxygen TherapyAliyah Julianne PayumoNo ratings yet
- Easy Oxygen TherapyDocument13 pagesEasy Oxygen TherapyKrizamay Ongat AggerNo ratings yet
- L04 - Part LL Updated Oxygen TherapyDocument12 pagesL04 - Part LL Updated Oxygen TherapyTariku GebreNo ratings yet
- Oxygen Therapy CPG GuideDocument4 pagesOxygen Therapy CPG Guidedragon66No ratings yet
- Spek Vent Vela ComphDocument4 pagesSpek Vent Vela ComphRinawatiNo ratings yet
- Oxygen Delivery Devices: Dr. HimanshuDocument40 pagesOxygen Delivery Devices: Dr. HimanshusnezaimNo ratings yet
- O2 Administration ReviewerDocument5 pagesO2 Administration ReviewerDustin Dela CruzNo ratings yet
- Terapi Oksigen Dan Tata Laksana Jalan NapasDocument23 pagesTerapi Oksigen Dan Tata Laksana Jalan NapasFiyandNo ratings yet
- Eathing IDI 2015Document58 pagesEathing IDI 2015Syamsul Bahri AkhasNo ratings yet
- Medx Anesthesia S6100Document2 pagesMedx Anesthesia S6100Luzon MedicalNo ratings yet
- BASIC OXYGEN RESPINA EditDocument51 pagesBASIC OXYGEN RESPINA EditTheopilus Obed LayNo ratings yet
- Comparison of FFP2, KN95, and N95 and Other Filtering Facepiece Respirator ClassesDocument3 pagesComparison of FFP2, KN95, and N95 and Other Filtering Facepiece Respirator ClassesfaithnicNo ratings yet
- Oxygen TherapyDocument21 pagesOxygen TherapyRaymund Christopher Dela PeñaNo ratings yet
- Terapi Oksigen PDFDocument50 pagesTerapi Oksigen PDFelianamuis100% (1)
- Oxygen Concentrator: Main Technical SpecificationsDocument2 pagesOxygen Concentrator: Main Technical SpecificationsBenn BasilNo ratings yet
- Oxygen AdministrationDocument27 pagesOxygen AdministrationakhilNo ratings yet
- NCM 118 Lec Prelim 2Document13 pagesNCM 118 Lec Prelim 2SammNo ratings yet
- Comparison of FFP2, KN95, and N95 and Other Filtering Facepiece Respirator ClassesDocument3 pagesComparison of FFP2, KN95, and N95 and Other Filtering Facepiece Respirator ClassesRavi S DwivedyNo ratings yet
- Niv HFNCDocument15 pagesNiv HFNCFrank VaronaNo ratings yet
- Oxygen TherapyDocument4 pagesOxygen Therapyharold smithNo ratings yet
- Basics of OxygenDocument78 pagesBasics of OxygenClarisse AcacioNo ratings yet
- Anesthesia System: Technical SpecificationDocument2 pagesAnesthesia System: Technical Specificationasep budiyantoNo ratings yet
- DR Kapil Dev Soni - Oxygen Therapy in AdultsDocument39 pagesDR Kapil Dev Soni - Oxygen Therapy in AdultsBhoomika PandeyNo ratings yet
- Philips Ev300 BrochureDocument2 pagesPhilips Ev300 BrochureErick PGNo ratings yet
- Oxygen Therapy: Dr. Aneela HussainDocument30 pagesOxygen Therapy: Dr. Aneela HussainMohammad AliNo ratings yet
- SBMJ 56Document3 pagesSBMJ 56sherryiqbalNo ratings yet
- Oxygen Therapy: by DR Finny Theo, MBBS, (DNB)Document59 pagesOxygen Therapy: by DR Finny Theo, MBBS, (DNB)The Telugu DoctorNo ratings yet
- 4-Oxygen TherapyDocument31 pages4-Oxygen Therapyabdisalaan hassanNo ratings yet
- Oxygen Therapy Sajoo RTDocument34 pagesOxygen Therapy Sajoo RTsajaNo ratings yet
- Administering Oxygen by Nasal CannulaDocument5 pagesAdministering Oxygen by Nasal CannulaAndrea Bayaga WaganNo ratings yet
- DO ProbeDocument7 pagesDO ProbeasperfudNo ratings yet
- NIV and HFNCDocument16 pagesNIV and HFNCMarceline GarciaNo ratings yet
- OKSIGENDocument51 pagesOKSIGENlNo ratings yet
- Anaesthesia DFX WorkbookDocument10 pagesAnaesthesia DFX WorkbookSaurav SinghNo ratings yet
- Ventilation Modes and Parameters of Anesthesia MachineDocument2 pagesVentilation Modes and Parameters of Anesthesia MachineLuis RodriguezNo ratings yet
- Post Arrest CareDocument23 pagesPost Arrest CareMohamed RasoolNo ratings yet
- Dr. Subhasis Roy: Consultant, Sisu Sanjiban Hospital, Salt Lake, KolkataDocument19 pagesDr. Subhasis Roy: Consultant, Sisu Sanjiban Hospital, Salt Lake, Kolkatacy_alcantaraNo ratings yet
- Case Study AssigmentDocument8 pagesCase Study AssigmentArvin LabradaNo ratings yet
- Oxygen Therapy For NurseDocument46 pagesOxygen Therapy For NurseselviiNo ratings yet
- (ANES) Sat 05 Pharmacology of Inhalational Anesthetics (A2021)Document3 pages(ANES) Sat 05 Pharmacology of Inhalational Anesthetics (A2021)Ricky Justin NgoNo ratings yet
- (ANES) Sat 01 Ambulatory Anesthesia (A2021)Document3 pages(ANES) Sat 01 Ambulatory Anesthesia (A2021)Ricky Justin NgoNo ratings yet
- Adrenal Crisis Workup in ERDocument16 pagesAdrenal Crisis Workup in ERRicky Justin NgoNo ratings yet
- (ANES) Sat 02 Anesthesia Machine and Equipment (A2021)Document3 pages(ANES) Sat 02 Anesthesia Machine and Equipment (A2021)Ricky Justin NgoNo ratings yet
- MEDICINE 2 – NEPHRO: GENERAL LECTUREDocument13 pagesMEDICINE 2 – NEPHRO: GENERAL LECTURERicky Justin NgoNo ratings yet
- MED NE 1 14 Water-Metabolism-Hypernatremia-HyponatremiaDocument12 pagesMED NE 1 14 Water-Metabolism-Hypernatremia-HyponatremiaRicky Justin NgoNo ratings yet
- MED - IR.L3.MDR Organisms and Antibiotic StewardshipDocument6 pagesMED - IR.L3.MDR Organisms and Antibiotic StewardshipRicky Justin NgoNo ratings yet
- MED - EN.CCD4.When Acute Is Not CuteDocument9 pagesMED - EN.CCD4.When Acute Is Not CuteRicky Justin NgoNo ratings yet
- (OB GRP 2) SGD - Ovarian Cyst in PregnancyDocument4 pages(OB GRP 2) SGD - Ovarian Cyst in PregnancyRicky Justin NgoNo ratings yet
- Cholera Mindmap: Understanding The Disease, Symptoms, and PreventionDocument1 pageCholera Mindmap: Understanding The Disease, Symptoms, and PreventionUlysse BerraNo ratings yet
- Colquitt, LePine, & Noe (2000) JAP PDFDocument30 pagesColquitt, LePine, & Noe (2000) JAP PDFMeyrina PronityastutiNo ratings yet
- Pub Family Practice Examination and Board ReviewDocument937 pagesPub Family Practice Examination and Board ReviewMohammad PharaonNo ratings yet
- Critical Thinking, Clinical Reasoning, and Clinical Judgment, 7eDocument274 pagesCritical Thinking, Clinical Reasoning, and Clinical Judgment, 7eBrianna DoyleNo ratings yet
- Ca Print 1Document134 pagesCa Print 1Kyoko ANo ratings yet
- المعدات وغرف الانتاج والتنظيف والصيانة دليل الطالبDocument56 pagesالمعدات وغرف الانتاج والتنظيف والصيانة دليل الطالبbionorluxeNo ratings yet
- Vital-Action LevelsDocument34 pagesVital-Action LevelsLuis GallegosNo ratings yet
- 818503r10 Manual TAT2000 PDFDocument12 pages818503r10 Manual TAT2000 PDFadrian alonsoNo ratings yet
- G08 Water1 Report 202Document7 pagesG08 Water1 Report 202notmuappleNo ratings yet
- Attachment and Mind Theory in Psychotherapy and Psychopathology of SchizophreniaDocument11 pagesAttachment and Mind Theory in Psychotherapy and Psychopathology of SchizophreniaIris Druț-PerianNo ratings yet
- DR Barbara StarfieldDocument37 pagesDR Barbara StarfieldSuyanto SuyantoNo ratings yet
- Sop For Facility and Equipment Maintenance Management in Primary Health Care Clinic in IraqDocument79 pagesSop For Facility and Equipment Maintenance Management in Primary Health Care Clinic in IraqticoNo ratings yet
- Manual Therapy Interventions For Carpal Tunnel Syndrome A ReviewDocument10 pagesManual Therapy Interventions For Carpal Tunnel Syndrome A ReviewlathifatulNo ratings yet
- HHA - X-MET8000 Optimum + Expert Performance Document (Alloy) - Thin Window - V1-3Document5 pagesHHA - X-MET8000 Optimum + Expert Performance Document (Alloy) - Thin Window - V1-3Paula InesNo ratings yet
- OpenLMIS: Open Source Software for Managing Health Supply ChainsDocument4 pagesOpenLMIS: Open Source Software for Managing Health Supply Chainschibwe chatamaNo ratings yet
- Massive Hemoptysis An Update On The Role of Bronchoscopy in Diagnosis and Management PDFDocument21 pagesMassive Hemoptysis An Update On The Role of Bronchoscopy in Diagnosis and Management PDFdoc_next_doorNo ratings yet
- PDF097Document1 pagePDF097Hao LuoNo ratings yet
- Wahyu Agung Kenworth Motors Case StudyDocument2 pagesWahyu Agung Kenworth Motors Case StudyWahyu Utama100% (1)
- Quantum Academies Program OverviewDocument234 pagesQuantum Academies Program OverviewThomas Marti100% (1)
- Positioning A Client in BedDocument32 pagesPositioning A Client in BedGrape JuiceNo ratings yet
- Indian Journal of Public Health Research and DevelopmentDocument1 pageIndian Journal of Public Health Research and DevelopmentNusa karya engineeringNo ratings yet
- Mental Health DepressionDocument4 pagesMental Health DepressionKAIZEN KINGZNo ratings yet
- Case Study The Teaching HospitalDocument4 pagesCase Study The Teaching HospitalDerick DarkZide100% (4)
- 5 6136226561843528157Document15 pages5 6136226561843528157Om Prakash RajNo ratings yet
- Policy Paper-Bpa108Document6 pagesPolicy Paper-Bpa108Aripin SangcopanNo ratings yet
- Call For Papers: Innovations in Glaucoma Surgery: Improving The ResultsDocument1 pageCall For Papers: Innovations in Glaucoma Surgery: Improving The ResultsYulias YoweiNo ratings yet
- Shapiro (1992) A Preliminary Study of The Long Term MeditatorsDocument18 pagesShapiro (1992) A Preliminary Study of The Long Term MeditatorsMichel AngersNo ratings yet
- Penerapan Model Pembelajaran Problem Based Learning Untuk Meningkatkan Hasil Belajar Siswa Mata Pelajaran PAK Di Kelas V SDN 003 Bintan TimurDocument12 pagesPenerapan Model Pembelajaran Problem Based Learning Untuk Meningkatkan Hasil Belajar Siswa Mata Pelajaran PAK Di Kelas V SDN 003 Bintan Timurrony carolesNo ratings yet
- Chloe Ting - 2 Weeks Shred Challenge - Free Workout ProgramDocument5 pagesChloe Ting - 2 Weeks Shred Challenge - Free Workout ProgramIndecisiveGurl100% (2)
- MR No. Urine Test ResultsDocument1 pageMR No. Urine Test Results112345678900No ratings yet