Professional Documents
Culture Documents
(OB GRP 2) SGD - Ovarian Cyst in Pregnancy
Uploaded by
Ricky Justin NgoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(OB GRP 2) SGD - Ovarian Cyst in Pregnancy
Uploaded by
Ricky Justin NgoCopyright:
Available Formats
OBSTETRICS ROTATION (FIRST LOOP)
SGD: Ovarian Cyst in Pregnancy
TBM
July 21, 2020
Joint session under TBM
Case: CASE: A 26 y/o G1 P0 consulted because of pain on the right side of the abdomen. One week prior to consult, she noted
intermittent pain that comes and goes on the right side of the abdomen, 2 fingerbreadths below the umbilicus. No consult was
done, because she felt relieved after passing out flatus. She felt the same pain two days ago and resolved spontaneously. A few
hours prior to consult, she was awakened from sleep because of severe pain. She felt nauseous, and reported cold clammy
perspiration. LMP April 12-15, 2020. PMP March 13-25, 2020
On admission,
● VS : BP - 120/80. PR - 90/min. RR - 20 cpm T - 36.8
● HEENT, Chest, lung and heart findings normal
● Abdomen: slightly globular, (+) direct tenderness on the right lower quadrant area, FHR 150 bpm left lower quadrant
● Speculum exam: Cervix - violaceous, minimal discharge, no bleeding
● IE: Cervix - soft, long, closed; Uterus - enlarged to AOG, (+) tenderness right supero-lateral portion of the uterus
Ovarian new growth, right, probably endometrial cyst, located lateral to the uterus.
Unilocular with a cystic mass containing low level echoes, 6.58 x 7.95 x 8.67 (vol: 237.47 cc), with color flow negative
Note the white line/curve on top of the picture: this denotes a transabdominal UTZ was done
1. What is your admitting diagnosis? 2. Give the differential diagnoses
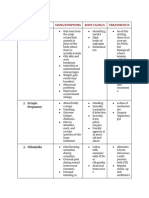
G1P0 * In red are what applies to the patient*
Pregnancy uterine
14-15 weeks AOG Corpus Luteum Cyst
Adnexal Torsion secondary to Ovarian New growth, right ● Present only during the 1st trimester, then regresses
Ovarian cyst (or ovarian new growth, benign), right, ● Maybe asymptomatic
probably in torsion ● Rupture: trauma or spontaneously
● Mild, chronic lower abdominal discomfort that
Torsion suddenly intensifies
● most important symptom of tubal torsion is acute ● Sudden, unilateral, sharp pelvic pain
lower abdominal and pelvic pain accompanied by ● Tachycardia, hypotension
nausea and vomiting ● Moderate to severe unilateral or bilateral lower
● Sonography aids in the diagnosis abdominal tenderness
● Presence of ovarian mass with absent flow
● Pregnancy predisposes to this problem Dermoid Cyst
● Torsion of the fallopian tube is secondary to an ● Found in younger and reproductive age groups
ovarian mass in approximately 50% to 60% of ● Movable mass
patients. ● Unilateral or bilateral
● Nontender
● Some have doughy or both cystic and solid
components
● Majority asymptomatic
● Pressure symptoms
● Abdominal pain
CLINICAL CLERKS 2021 GROUP 2 1 of 4
SGD: Ovarian Cyst in Pregnancy
● Adnexal mass Imaging
● Mass has smooth border Ultrasound
● May present with torsion, rupture, or perforation: on ● initial modality of choice for appendicitis
and off pain, severe pain due to inflammation ● gold standard for the assessment of ovarian cysts
● TVS is preferred
Acute Appendicitis ● IOTA Scoring (for evaluation of possible malignancy)
● Any of the 3 trimesters (highest incidence during 2nd ○ In the patient, only B features is present and
trimester) no M features = benign
● Pain presents initially at the periumbilical area then
localizes to the RLQ MRI, CT Scan
● (+) Abdominal guarding ● if UTZ is inconclusive; CT if MRI is unavailable
● (+)McBurney’s sign
● (+) Rebound tenderness Color Doppler
● Alvarado score: ● detect the movement of blood in vessels
○ RLQ pain migration ● If with ovarian mass and there is absent flow, it is
○ Anorexia usually associated with torsion kasi naiipit yung
○ Nausea and vomiting (1) vessels.
○ Tenderness in RLQ (2)
○ Rebound pain
○ Elevated temp
○ Leukocytosis
○ WBC shift to the left
● Actually coincides with the presentation of the patient
but is ruled out due to the ultrasound findings.
Adnexal Torsion
● Ovarian mass
● Right > left (3:2) Physiological corpus luteum cyst or benign cystadenoma
● 1st trimester > 2nd trimester > 3rd trimester
● Pain:
○ Moderate to severe
○ Acute, colicky, unilateral
○ Lower abdominal / pelvic
○ Prior intermittent episodes
● Adnexal mass
● Nausea and vomiting
● Low grade fever
3. What ancillary procedures will be requested? Endometrioma or Hemorrhagic corpus luteum cyst
Laboratory Tests Low level echoes (may puti puti, hindi completely black) seen
CBC in the cyst due to the blood present.
● Get the baseline for future management
● Leukocytosis WBC >10,000 with a left shift in the
differential
Fasting Blood Sugar
● Filipinos are at high risk for gestational diabetes
● Done at first prenatal check up
● 75g OGTT - at 24-28 weeks
Urinalysis
● Check for hematuria, pyuria
● Routine screening for STI must be done to the Mature cystic teratoma - m ost common pathologic growth; first
patient, and it is the most cost-effective. thing to think of when there’s pathologic growth in pregnancy
● If, through history we find out that the patient is high hair- linear streaks
risk for other STIs such as HIV, chlamydia, then we Presence of Rokitansky protuberance/nodule — responsible
can do additional serological tests specific to these for acoustic shadowing
(nucleic acid amplification test [chlamydia], rapid
plasma reagin test [syphilis]) 4. What is the management?
Goals of Treatment:
CRP ● Pain relief
● elevated ● Removal of mass
● Monitor the mother and the fetus
Cancer antigen 125 (CA125)
● May be used if there is suspicion of malignancy
CLINICAL CLERKS 2021 GROUP 2 2 of 4
SGD: Ovarian Cyst in Pregnancy
Since the patient is symptomatic already, definitive Postoperative Care
management is surgery. ● Prenatal surveillance
○ Fetal Heart Doppler Ultrasound
■ To confirm fetal well-being
Elective surgery ■ To reassure the mother
● Indicated if highly suspicious of malignancy or
presented with rupture, torsion or hemorrhage MANAGEMENT OF UNCOMPLICATED OVARIAN CYST
○ In torsion, there is necrosis so the ovary ( WITHOUT TORSION)
becomes black-blue color. Grossly, it doesn’t
really look good Pain Relief
○ Normal ovary- looks pearly white ● Rest
● In general, we plan resection at 14 to 20 weeks’ ● Pain Management
gestation because most masses that will regress will
have done so by this time. Conservative Management
○ 2nd trimester is always the best time for ● Intervention should be delayed until 14–16 weeks
surgery to allow spontaneous resolution of functional cysts
○ Patient is 14-15 weeks of gestation, so she ● Usually resolve by the second trimester
can proceed with surgery. ● Usually done in asymptomatic patients or ovarian
● Ovarian cystectomy cysts < 5cm without suspicion of
○ Laparotomy is the standard approach, malignancy/M-features on ultrasound
laparoscopy can be an option
○ Outright oophorectomy is seldom done in Further ultrasound assessment
torsion. Trial of unwinding the torsion is ● Should take place at 4-week intervals
initially done and condition is assessed. ● Monitor the size and condition of the cyst
● Frozen section assessment performed
● Careful examination of contralateral ovary Ultrasound-guided fine needle aspiration
● Preoperatively, prophylactic tocolytics (e.g. ● Persistent, simple, unilocular cysts without any
ixosuprine) are started and continued up to 24 hours solid elements that are larger than 10 cm can be
postoperatively. This is to ensure that maternal stress aspirated
will not cause uterine contractions that may lead to ● Fine needle aspirations should be done after 14
abortion. weeks AOG in order to minimize disturbance to the
○ This is done for all pregnant women corpus luteum
undergoing surgery and not just for torsion ● Useful in relieving acute pain and can reduce the
risk of cyst torsion and rupture
● Prone to recurrence, because the capsule is not
removed
CLINICAL CLERKS 2021 GROUP 2 3 of 4
SGD: Ovarian Cyst in Pregnancy
ALGORITHMS FOR MANAGEMENT
Note: this is just a recommendation
Usually for complex cysts, further measures are done to assess for malignancy (e.g. doppler flow).
We do not just wait to rescan in 4 weeks.
CLINICAL CLERKS 2021 GROUP 2 4 of 4
You might also like
- NBME 16 Complete PDFDocument112 pagesNBME 16 Complete PDFSilar Khan67% (18)
- OB-Gyn Case Presentation - BicornuateDocument53 pagesOB-Gyn Case Presentation - BicornuateZari Novela100% (1)
- Inguinal HerniaDocument57 pagesInguinal HerniaIsfahan ⎝⏠⏝⏠⎠No ratings yet
- Hemorrhages in PregnancyDocument153 pagesHemorrhages in PregnancyLisa Kriestanto100% (1)
- Fast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeFrom EverandFast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeNo ratings yet
- AP GeographyDocument95 pagesAP GeographyKhimavathBharathNaik88% (8)
- N Vent Code ENDocument28 pagesN Vent Code ENGwenn LecturaNo ratings yet
- Endorsement Case Discussion JULY 29, 2020 Patient # 39 I. General DataDocument9 pagesEndorsement Case Discussion JULY 29, 2020 Patient # 39 I. General DataChristille Lindy Joyce CaluyoNo ratings yet
- Antepartum Hemorrhage Previa &abruptio PlacentaDocument25 pagesAntepartum Hemorrhage Previa &abruptio PlacentaHannah HalimNo ratings yet
- GYNE SGD - Benign and Ovarian CancerDocument62 pagesGYNE SGD - Benign and Ovarian CancerShia LevyNo ratings yet
- Pregnant Woman Emergency Clinical CaseDocument38 pagesPregnant Woman Emergency Clinical CaseBianca Gallardo AriasNo ratings yet
- OnG Viva Sample Ans Nea 2021 b1Document82 pagesOnG Viva Sample Ans Nea 2021 b1MumtaNo ratings yet
- Endometriosis and FibroidsDocument74 pagesEndometriosis and FibroidsJodi-Ann FletcherNo ratings yet
- Breast Disease WucDocument52 pagesBreast Disease WucOTOH RAYA OMAR100% (1)
- Case Blighted Ovum - Jenni Mutiara Saragih (202006010015)Document28 pagesCase Blighted Ovum - Jenni Mutiara Saragih (202006010015)Jenni SaragihNo ratings yet
- Journal Reading Management of A Pelvic MassDocument40 pagesJournal Reading Management of A Pelvic MassCecilia SalimNo ratings yet
- High Risk PregnancyDocument12 pagesHigh Risk Pregnancyggrrk7100% (2)
- SGD Week 2 - Abnormal Uterine Bleeding Gr4Document39 pagesSGD Week 2 - Abnormal Uterine Bleeding Gr4Andrea GuarinNo ratings yet
- Breast LumpDocument22 pagesBreast LumpEsther KhawlhringNo ratings yet
- ObsGyn - OSCE NotesDocument69 pagesObsGyn - OSCE NotesMatt McCannNo ratings yet
- Diverticulitis ConferenceDocument9 pagesDiverticulitis ConferencemimicamasoNo ratings yet
- Case Study 29-APHDocument31 pagesCase Study 29-APHZarul Naim Mohd TamiziNo ratings yet
- Surger YII Clinic AL Case: Group 4B Bernabe, Bernardo, Bialba, BigorniaDocument39 pagesSurger YII Clinic AL Case: Group 4B Bernabe, Bernardo, Bialba, BigorniaAlloiBialbaNo ratings yet
- Third Trimester Bleeding: Whitney BrantleyDocument17 pagesThird Trimester Bleeding: Whitney BrantleyGeneNo ratings yet
- Surgery 2 - Si & Appendix - D5Document23 pagesSurgery 2 - Si & Appendix - D5Jolaine ValloNo ratings yet
- CMC Abruptio PlacentaDocument76 pagesCMC Abruptio PlacentaNorman Vryne CaduaNo ratings yet
- Acute AbdomenDocument71 pagesAcute AbdomenariNo ratings yet
- Benign Ovarian TumoursDocument38 pagesBenign Ovarian TumoursTARAJ MOSTAFA CHERAGHNo ratings yet
- 16.1 - General SurgeryDocument65 pages16.1 - General Surgeryayeshafarooq60No ratings yet
- Abortus: Levina Felicia Supervisor:Dr. Mulyanusa A. Ritonga, Spog (K) ., M.KesDocument27 pagesAbortus: Levina Felicia Supervisor:Dr. Mulyanusa A. Ritonga, Spog (K) ., M.KesIMO UNPADNo ratings yet
- HW1 Ibanez Bio PDFDocument2 pagesHW1 Ibanez Bio PDFBanjo IbañezNo ratings yet
- Placenta PreviaDocument36 pagesPlacenta Previaotartil_nimanNo ratings yet
- Endometrial Hyperplasia Heavy Vaginal BleedingDocument69 pagesEndometrial Hyperplasia Heavy Vaginal BleedingMelcah Marie NacionalesNo ratings yet
- Acute Abdomen Practical Approach FransDocument29 pagesAcute Abdomen Practical Approach FransAbel MncaNo ratings yet
- Placenta Previa TotalisDocument34 pagesPlacenta Previa TotalisRujira Angkinan100% (4)
- AUBNDocument54 pagesAUBNJohn Christopher LucesNo ratings yet
- S0rgical ScibeDocument4 pagesS0rgical ScibeLINDSLEY GONo ratings yet
- Cervical Cancer: Alabe - Aquino - Aquino - Bernardo - BinwagDocument61 pagesCervical Cancer: Alabe - Aquino - Aquino - Bernardo - BinwagApril Mae Magos LabradorNo ratings yet
- 02-03-2021 ADCON (Group 2, DR.)Document43 pages02-03-2021 ADCON (Group 2, DR.)Jolaine ValloNo ratings yet
- Abdome AgudoDocument63 pagesAbdome AgudoAnne Caroline De Morais AlvesNo ratings yet
- Myoma: By: Vabiayu Putri Opponent: Farida Aryani Mariana Ulfah Sandy WijayaDocument37 pagesMyoma: By: Vabiayu Putri Opponent: Farida Aryani Mariana Ulfah Sandy WijayaRaafika StudivianiNo ratings yet
- Presented by Dr. Ayalew ZDocument35 pagesPresented by Dr. Ayalew Zyared getachewNo ratings yet
- OBGYN NotesDocument29 pagesOBGYN NotesavavNo ratings yet
- GTD Hour AprilDocument26 pagesGTD Hour AprilGerben VillanuevaNo ratings yet
- Approach To A Patient With Adenomyosis FINALDocument56 pagesApproach To A Patient With Adenomyosis FINALapi-3700579No ratings yet
- Rehabilitation Post StrokeDocument27 pagesRehabilitation Post StrokeNorNashiraMohdIbrahimNo ratings yet
- Surgical OncologyDocument10 pagesSurgical Oncologysofea zamriNo ratings yet
- SafariViewService - 16 Feb 2019 12.09Document1 pageSafariViewService - 16 Feb 2019 12.09Ngakan Ketut DarmawanNo ratings yet
- Clinical Case PresentationDocument49 pagesClinical Case PresentationRUSSELL CILOTNo ratings yet
- CC C C: June 8, 2011 By: Santos, Edilberto DBDocument63 pagesCC C C: June 8, 2011 By: Santos, Edilberto DBHakugeiNo ratings yet
- 0 - Women Key Words ListDocument7 pages0 - Women Key Words ListamyngaileeNo ratings yet
- Mid Trimester DisorderDocument33 pagesMid Trimester DisorderdhivyadiyaNo ratings yet
- Small Group DiscussionDocument78 pagesSmall Group DiscussionRose PeranteNo ratings yet
- Gastroenterology Case Discussion: JANUARY 07, 2021 Dr. Stephen Wong Indigo and VioletDocument19 pagesGastroenterology Case Discussion: JANUARY 07, 2021 Dr. Stephen Wong Indigo and VioletJolaine ValloNo ratings yet
- Antepartum Haemorrhage PolicyDocument5 pagesAntepartum Haemorrhage PolicyubayyumrNo ratings yet
- 1 - Abdomen 1Document23 pages1 - Abdomen 1noushad aminNo ratings yet
- Obstetricsafetyprotocols PDFDocument10 pagesObstetricsafetyprotocols PDFLoraine CastilloNo ratings yet
- Case NoDocument22 pagesCase NoBella DirkNo ratings yet
- Breast MassDocument107 pagesBreast MassISFAHAN MASULOTNo ratings yet
- OPD Orientation (July 26, 2021)Document7 pagesOPD Orientation (July 26, 2021)Jennifer HerediaNo ratings yet
- Ectopic PregnancyDocument44 pagesEctopic Pregnancygea pandhita sNo ratings yet
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicFrom EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicRating: 5 out of 5 stars5/5 (1)
- Fast Facts: Enfermedad inflamatoria intestinal Para Pacientes y las Personas que los Apoyan: Colitis ulcerativa y enfermedad de Crohn Información + Tomar el control = El mejor resultadoFrom EverandFast Facts: Enfermedad inflamatoria intestinal Para Pacientes y las Personas que los Apoyan: Colitis ulcerativa y enfermedad de Crohn Información + Tomar el control = El mejor resultadoNo ratings yet
- (ANES) Sat 05 Pharmacology of Inhalational Anesthetics (A2021)Document3 pages(ANES) Sat 05 Pharmacology of Inhalational Anesthetics (A2021)Ricky Justin NgoNo ratings yet
- (ANES) Sat 04 Cardiovascular Drugs For Resuscitation (A2021)Document8 pages(ANES) Sat 04 Cardiovascular Drugs For Resuscitation (A2021)Ricky Justin NgoNo ratings yet
- (ANES) Sat 02 Anesthesia Machine and Equipment (A2021)Document3 pages(ANES) Sat 02 Anesthesia Machine and Equipment (A2021)Ricky Justin NgoNo ratings yet
- (ANES) Sat 01 Ambulatory Anesthesia (A2021)Document3 pages(ANES) Sat 01 Ambulatory Anesthesia (A2021)Ricky Justin NgoNo ratings yet
- MED2 B3 FC2 - AdrenalDocument16 pagesMED2 B3 FC2 - AdrenalRicky Justin NgoNo ratings yet
- MED - NE.1.18.Potassium Disorders (A2023)Document13 pagesMED - NE.1.18.Potassium Disorders (A2023)Ricky Justin NgoNo ratings yet
- MED NE 1 14 Water-Metabolism-Hypernatremia-HyponatremiaDocument12 pagesMED NE 1 14 Water-Metabolism-Hypernatremia-HyponatremiaRicky Justin NgoNo ratings yet
- MED - EN.CCD4.When Acute Is Not CuteDocument9 pagesMED - EN.CCD4.When Acute Is Not CuteRicky Justin NgoNo ratings yet
- MED - IR.L3.MDR Organisms and Antibiotic StewardshipDocument6 pagesMED - IR.L3.MDR Organisms and Antibiotic StewardshipRicky Justin NgoNo ratings yet
- Cosmetic Surgery EssayDocument7 pagesCosmetic Surgery Essayalisharenee0550% (2)
- OptoPrep Part1 StudyCalendar 3-MonthDocument4 pagesOptoPrep Part1 StudyCalendar 3-MonthmelanieNo ratings yet
- EnSURE Touch - F&BDocument6 pagesEnSURE Touch - F&BfaradillafattaNo ratings yet
- The Danger of Microwave TechnologyDocument16 pagesThe Danger of Microwave Technologyrey_hadesNo ratings yet
- Alwyn Naicker - Research Proposal Assignment 2 PDFDocument15 pagesAlwyn Naicker - Research Proposal Assignment 2 PDFAlwyn NaickerNo ratings yet
- Delirium Using The 4AT AssessmentDocument10 pagesDelirium Using The 4AT AssessmentAna KmaidNo ratings yet
- Tdiagnostics - Telangana.gov - in ViewFiles - Aspx ReportId p1s0K7qAzHwmL8S2z98THgDocument3 pagesTdiagnostics - Telangana.gov - in ViewFiles - Aspx ReportId p1s0K7qAzHwmL8S2z98THgyesawovNo ratings yet
- Mastoiditis - B.MDocument25 pagesMastoiditis - B.MBwalya MunjiliNo ratings yet
- Conflict or Consensus - An Investigation of Stakeholder Concerns DuringDocument10 pagesConflict or Consensus - An Investigation of Stakeholder Concerns DuringhohoexeNo ratings yet
- Chemistry, Manufacturing and ControlDocument11 pagesChemistry, Manufacturing and ControlHk HkNo ratings yet
- Tonometry and Care of Tonometers PDFDocument7 pagesTonometry and Care of Tonometers PDFAnni MuharomahNo ratings yet
- Freud's Psychosexual Stages of DevelopmentDocument30 pagesFreud's Psychosexual Stages of DevelopmentjessaNo ratings yet
- Republic Act No. 11210 - 105-Day Expanded Maternity Leave LawDocument4 pagesRepublic Act No. 11210 - 105-Day Expanded Maternity Leave LawRaymond CruzinNo ratings yet
- Personal Finance Canadian 2nd Edition Madura Test BankDocument48 pagesPersonal Finance Canadian 2nd Edition Madura Test Bankannabellaauroravb5cf100% (22)
- DNAlysis MygeneRx Sample ReportDocument13 pagesDNAlysis MygeneRx Sample ReportTrustNo ratings yet
- Health and Wellness Programs For CVommercial Truck Drivers 144 PagesDocument91 pagesHealth and Wellness Programs For CVommercial Truck Drivers 144 PagesDenise Mathre100% (1)
- 2016 Article InternationalEcoHealthOneHealtDocument139 pages2016 Article InternationalEcoHealthOneHealtMauricio FemeníaNo ratings yet
- IntroductionDocument9 pagesIntroductionMarc Harold FloresNo ratings yet
- 19-CPS Student Induction Presentation-RAZAK FinalDocument18 pages19-CPS Student Induction Presentation-RAZAK FinalbaderNo ratings yet
- CertificateDocument1 pageCertificateriteshNo ratings yet
- Stress Management Stress Management: NptelDocument99 pagesStress Management Stress Management: NptelDKNo ratings yet
- Blue Modern Medical Center Z-Fold BrochureDocument2 pagesBlue Modern Medical Center Z-Fold BrochureAngela Shaine CruzNo ratings yet
- Risk Assessment: Severity (1, 2 or 3)Document1 pageRisk Assessment: Severity (1, 2 or 3)Ulviyye ElesgerovaNo ratings yet
- Journal of Public Procurement: Article InformationDocument38 pagesJournal of Public Procurement: Article Informationwalelgn eyayuNo ratings yet
- Trainee's CharacteristicDocument3 pagesTrainee's CharacteristicRoldan EstibaNo ratings yet
- Overconfidence As A Cause of Diagnostic Error in Medicine PDFDocument22 pagesOverconfidence As A Cause of Diagnostic Error in Medicine PDFIulianZaharescuNo ratings yet
- Fall Prevention: How Can Older Adults Prevent Falls?Document4 pagesFall Prevention: How Can Older Adults Prevent Falls?Amalina ZahariNo ratings yet