Professional Documents
Culture Documents
WJGS 9 224
Uploaded by
cOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
WJGS 9 224
Uploaded by
cCopyright:
Available Formats
ISSN 1948-9366 (online)
World Journal of
Gastrointestinal Surgery
World J Gastrointest Surg 2017 November 27; 9(11): 215-232
Published by Baishideng Publishing Group Inc
Contents Monthly Volume 9 Number 11 November 27, 2017
ORIGINAL ARTICLE
Clinical Trials Study
215 Laparoscopic complete mesocolic excisions for colonic cancer in the last decade: Five-year survival in a
single centre
Storli KE, Lygre KB, Iversen KB, Decap M, Eide GE
224 Colorectal surgeon consensus with diverticulitis clinical practice guidelines
Siddiqui J, Zahid A, Hong J, Young CJ
WJGS|www.wjgnet.com I November 27, 2017|Volume 9|Issue 11|
Contents World Journal of Gastrointestinal Surgery
Volume 9 Number 11 November 27, 2017
ABOUT COVER Editorial Board Member of World Journal of Gastrointestinal Surgery , Ying Chai,
MD, Chief Doctor, Professor, Surgeon, Chair of Thoracic Surgery, Second Affiliated
Hospital, Zhejiang University School of Medicine, Zhejiang University, Hangzhou
310009, Zhejiang Province, China
AIM AND SCOPE World Journal of Gastrointestinal Surgery (World J Gastrointest Surg, WJGS, online ISSN 1948-9366,
DOI: 10.4240) is a peer-reviewed open access academic journal that aims to guide clinical
practice and improve diagnostic and therapeutic skills of clinicians.
WJGS covers topics concerning micro-invasive surgery; laparoscopy; hepatic, biliary,
pancreatic and splenic surgery; surgical nutrition; portal hypertension, as well as associated
subjects. The current columns of WJGS include editorial, frontier, diagnostic advances,
therapeutics advances, field of vision, mini-reviews, review, topic highlight, medical ethics,
original articles, case report, clinical case conference (Clinicopathological conference),
and autobiography. Priority publication will be given to articles concerning diagnosis and
treatment of gastrointestinal surgery diseases. The following aspects are covered: Clinical
diagnosis, laboratory diagnosis, differential diagnosis, imaging tests, pathological diagnosis,
molecular biological diagnosis, immunological diagnosis, genetic diagnosis, functional
diagnostics, and physical diagnosis; and comprehensive therapy, drug therapy, surgical
therapy, interventional treatment, minimally invasive therapy, and robot-assisted therapy.
We encourage authors to submit their manuscripts to WJGS. We will give priority to
manuscripts that are supported by major national and international foundations and those
that are of great basic and clinical significance.
INDEXING/ABSTRACTING World Journal of Gastrointestinal Surgery is now indexed in Emerging Sources Citation Index
(Web of Science), PubMed, and PubMed Central.
FLYLEAF I-III Editorial Board
Responsible Assistant Editor: Xiang Li Responsible Science Editor: Fang-Fang Ji
EDITORS FOR
Responsible Electronic Editor: Li-Min Zhao Proofing Editorial Office Director: Xiu-Xia Song
THIS ISSUE Proofing Editor-in-Chief: Lian-Sheng Ma
NAME OF JOURNAL World Journal of Gastrointestinal Surgery COPYRIGHT
World Journal of Gastrointestinal Surgery Baishideng Publishing Group Inc © 2017 Baishideng Publishing Group Inc. Articles pub-
7901 Stoneridge Drive, Suite 501, lished by this Open-Access journal are distributed under
ISSN Pleasanton, CA 94588, USA the terms of the Creative Commons Attribution Non-
ISSN 1948-9366 (online) Telephone: +1-925-2238242 commercial License, which permits use, distribution,
Fax: +1-925-2238243 and reproduction in any medium, provided the original
LAUNCH DATE E-mail: editorialoffice@wjgnet.com work is properly cited, the use is non commercial and is
November 30, 2009 Help Desk: http://www.f6publishing.com/helpdesk otherwise in compliance with the license.
http://www.wjgnet.com
FREQUENCY
Monthly SPECIAL STATEMENT
PUBLISHER All articles published in journals owned by the Baishideng
Baishideng Publishing Group Inc Publishing Group (BPG) represent the views and opin-
EDITOR-IN-CHIEF 7901 Stoneridge Drive, Suite 501, ions of their authors, and not the views, opinions or
Timothy M Pawlik, MD, Director, Professor, De-
partment of Surgery, Johns Hopkins University, School Pleasanton, CA 94588, USA policies of the BPG, except where otherwise explicitly
of Medical, Baltimore, MD 21287, United States Telephone: +1-925-2238242 indicated.
Fax: +1-925-2238243
EDITORIAL BOARD MEMBERS E-mail: bpgoffice@wjgnet.com
INSTRUCTIONS TO AUTHORS
All editorial board members resources online at http:// Help Desk: http://www.f6publishing.com/helpdesk
www.wjgnet.com/1948-9366/editorialboard.htm http://www.wjgnet.com/bpg/gerinfo/204
http://www.wjgnet.com
EDITORIAL OFFICE PUBLICATION DATE ONLINE SUBMISSION
Xiu-Xia Song, Director November 27, 2017 http://www.f6publishing.com
WJGS|www.wjgnet.com II November 27, 2017|Volume 9|Issue 11|
Submit a Manuscript: http://www.wjgnet.com World J Gastrointest Surg 2017 November 27; 9(11): 224-232
DOI: 10.4240/wjgs.v9.i11.224 ISSN 1948-9366 (online)
ORIGINAL ARTICLE
Clinical Trials Study
Colorectal surgeon consensus with diverticulitis clinical
practice guidelines
Javariah Siddiqui, Assad Zahid, Jonathan Hong, Christopher John Young
Javariah Siddiqui, Assad Zahid, Jonathan Hong, Christopher Correspondence to: Christopher John Young, MBBS, MS,
John Young, Discipline of Surgery, University of Sydney, FRACS, FACS, FASCRS, Professor, Department of Colorectal
Sydney, NSW 2050, Australia Surgery, Royal Prince Alfred Hospital, Suite 415, 100 Carillon
Ave, Sydney, NSW 2050, Australia. cyoungnsw@aol.com
Assad Zahid, Jonathan Hong, Christopher John Young, Telephone: +61-2-95197576
Department of Colorectal Surgery, Royal Prince Alfred Hospital, Fax: +61-2-95191806
Sydney, NSW 2050, Australia
Received: August 6, 2017
ORCID number: Javariah Siddiqui (0000-0002-2083-258X); Assad Zahid Peer-review started: August 7, 2017
(0000-0002-4401-416X); Jonathan Hong (0000-0003-0404-8979); First decision: September 7, 2017
Christopher John Young (0000-0002-7213-5137). Revised: September 24, 2017
Accepted: October 16, 2017
Author contributions: All authors contributed to the conception, Article in press: October 17, 2017
design, analysis and interpretation of data, as well as drafting and Published online: November 27, 2017
critically revising the manuscript; Siddiqui J was additionally
responsible for the acquisition of data.
Institutional review board statement: The study was reviewed
and approved by the Human and Research Ethics Committee, Abstract
The University of Sydney and the Colorectal Surgical Society of AIM
Australia and New-Zealand for distribution to members. To determine the application of clinical practice guidelines
for the current management of diverticulitis and
Informed consent statement: Submission of the completed colorectal surgeon specialist consensus in Australia and
survey was an indication of the surgeon’s consent to participate
New Zealand.
in the study. This was mentioned in the participant information
sheet (attached) to all members of the Colorectal Surgical Society
of Australia and New Zealand. METHODS
A survey was distributed to 205 colorectal surgeons
Conflict-of-interest statement: Nil conflicts of interests, nil in Australia and New Zealand, using 22 hypothetical
funding from grants. clinical scenarios.
Open-Access: This article is an open-access article which was RESULTS
selected by an in-house editor and fully peer-reviewed by external The response rate was 102 (50%). For 19 guideline-
reviewers. It is distributed in accordance with the Creative based scenarios, only 11 (58%) reached consensus
Commons Attribution Non Commercial (CC BY-NC 4.0) license, (defined as > 70% majority opinion) and agreed with
which permits others to distribute, remix, adapt, build upon this
guidelines; while 3 (16%) reached consensus and did
work non-commercially, and license their derivative works on
different terms, provided the original work is properly cited and not agree with guidelines. The remaining 5 (26%)
the use is non-commercial. See: http://creativecommons.org/ scenarios showed community equipoise (defined
licenses/by-nc/4.0/ as less than/equal to 70% majority opinion). These
included diagnostic imaging where CT scan was
Manuscript source: Invited manuscript contraindicated, management options in the failure
WJGS|www.wjgnet.com 224 November 27, 2017|Volume 9|Issue 11|
Siddiqui J et al . Diverticulitis and guideline consensus
of conservative therapy for complicated diverticulitis, management options including laparoscopic vs open
surgical management of Hinchey grade 3, proximal approach and primary anastomosis vs Hartmann’s
extent of resection in sigmoid diverticulitis and use procedure for Hinchey Grades 3 and 4. An attempt has
of oral mechanical bowel preparation and antibiotics been made by several societies to condense some of
for an elective colectomy. The consensus areas not this into guidelines and practice parameters based on
agreeing with guidelines were management of simple level of evidence .
[2-4]
diverticulitis, management following the failure of Previous surveys
[5-9]
have assessed correlation
conservative therapy in uncomplicated diverticulitis and in their community with these guidelines. However,
follow-up after an episode of complicated diverticulitis. no surveys have been conducted in Australasia
Fifty-percent of rural/regional based surgeons would that evaluates correlation with guidelines for both
perform an urgent sigmoid colectomy in failed the current medical and surgical management of
conservative therapy of diverticulitis compared to
diverticulitis, as well as giving consideration to right-
only 8% of surgeons city-based (Fisher’s exact test P
sided diverticulitis.
= 0.016). In right-sided complicated diverticulitis, a
The aim of our survey was to assess consensus of
greater number of those in practice for more than ten
current colorectal specialist practice within Australia
years would perform an ileocecal resection and ileocolic
anastomosis (79% vs 41%, P < 0.0001). and New Zealand with the clinical practice guidelines
for the management of simple and complicated
CONCLUSION diverticulitis (mainly practice parameters published
While there are areas of consensus in diverticulitis by the Standards Task Force of The American Society
[2]
management, there are areas of community equipoise of Colon and Rectal Surgeons as there are no
for future research, potentially in the form of RCTs. Australasian guidelines on this subject). We also aimed
to highlight areas of community equipoise, to identify
Key words: Diverticulitis; Clinical practice guidelines; areas that will benefit from future research.
Consensus
© The Author(s) 2017. Published by Baishideng Publishing
MATERIALS AND METHODS
Group Inc. All rights reserved. All members of the Colorectal Surgical Society of
Australia and New Zealand (CSSANZ) were mailed
Core tip: This study illustrates colorectal surgeon out an anonymous survey consisting of 22 clinical
specialist consensus with clinical practice guidelines scenarios with multiple choice options (Appendix 1).
for diverticulitis. While consensus occurred with the One reminder mail was sent out after six weeks to non-
majority of guideline recommendations, areas with lack respondents. The University of Sydney Human Ethics
of consensus and even consensus that disagrees with department granted ethical approval and the CSSANZ
guidelines focuses where future research efforts should approved the distribution of the questionnaires.
be placed. Surgeon demographics were collected including
age range, gender, years practicing, the location of
training and current practice, as well as the presence
Siddiqui J, Zahid A, Hong J, Young CJ. Colorectal surgeon of interventional radiology and an Acute Surgical Unit
consensus with diverticulitis clinical practice guidelines. World
(ASU) at the place of practice.
J Gastrointest Surg 2017; 9(11): 224-232 Available from: URL:
The survey was based on clinical scenarios to
http://www.wjgnet.com/1948-9366/full/v9/i11/224.htm DOI:
evaluate the medical and surgical management
http://dx.doi.org/10.4240/wjgs.v9.i11.224
of uncomplicated and complicated diverticulitis.
Nineteen questions were derived from the recently
[2,4]
published guidelines containing an option of 3 to 4
multiple choices, one of which matched the guideline
INTRODUCTION recommendations. The remaining three scenarios
Sigmoid diverticulitis is a common affliction of the were not directly related to the guidelines but were
Western world, and recently, due to migration, there developed to examine surgeon preferences in additional
has been an increase in the incidence of right-sided controversies in diverticulitis management not included
[1]
diverticulitis . Diverticulitis can be divided into the in the guidelines. The areas covered included initial
simple and complicated disease. Complicated disease diagnostic imaging, diagnostic imaging when CT is
includes perforation, obstruction, abscesses, fistula and contraindicated, management of differing size and
stricture formation. With greater understanding of the location of abscesses, management in a medically
pathophysiology of diverticulitis and the advancement complex patient, management upon failure of
of technology, the management of diverticulitis conservative therapy, follow-up options following simple
has been evolving in recent times. There is a greater and complicated diverticulitis, surgical management
push towards the outpatient management of simple options for different Hinchey grades, as well as
diverticulitis and less aggressive initial management for operative considerations and management of right-sided
complicated cases. There is also a change in surgical diverticulitis. The American Society of Anesthesiologists
WJGS|www.wjgnet.com 225 November 27, 2017|Volume 9|Issue 11|
Siddiqui J et al . Diverticulitis and guideline consensus
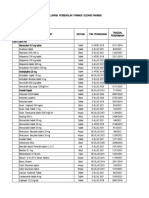
Table 1 Surgeon demographics
Characteristic n (%)
Age range (yr)
30-39 10 (10)
40-49 37 (37)
50-59 40 (40)
Over 60 14 (14)
Gender
Male 90 (89)
Female 11 (11)
Location of current practice
City (tertiary/quaternary referral center) 79 (78)
City (secondary referral) 16 (16)
Rural 6 (6)
Location of subspecialty training1
Australia/New Zealand 66 (65)
Europe 28 (28)
North America 15 (15)
Country of current practice
Australia 84 (83)
New Zealand 17 (17)
ASU present in current practice location 57 (56)
Interventional radiology available 99 (98)
Average years in practice (years ± SD) 14 ± 8.5
1
Total > 100% due to > 1 location of training.
(ASA) grade was provided for reference. Completion recommendation; (3) Equipoise/Agree: scenarios with
of the survey by other colorectal specialists in the ≤ 70% of surgeons choosing an option that agrees
department tested for accuracy and validity before with guideline recommendation; and (4) Consensus/
dissemination to other members of CSSANZ. Agree: scenarios with > 70% surgeons choosing an
option that agrees with guideline recommendations.
Statistical analysis
Statistical analyses were conducted using IBM SPSS
Statistics Version 22. Demographics were tabulated
RESULTS
and descriptive statistics (proportion and mean ± Of 205 members of the CSSANZ, 102 (50%) responded
SD) were calculated. Two groups were formed - by returning the survey, of which one was incomplete
the first compared those that agreed with guideline and excluded from analysis. Surgeon demographics
recommended options and the second compared those are summarized in Table 1. The mean number of
that chose the most popular option among the choices years in practice was 14, with 53% of surgeons aged
provided (i.e., the greatest number of respondents more than 50 years. Sixty-five percent underwent
choosing this option). All demographic data were the majority of their sub-specialty colorectal surgery
tested for their association with these two groups. training in Australia or New Zealand, and 82% are
2
Univariate analysis was carried out using the χ test currently practicing in Australia.
or Fisher’s exact test where appropriate. Multivariate From the 19 guideline based scenarios in the survey,
logistic regression analysis was used to assess 14 (74%) reached consensus. Of these 14, 3 (21%)
associations between covariates. A P-value of less than scenarios disagreed with guideline recommendation.
0.05 was considered significant. Five (26%) scenarios showed community equipoise,
The proportion of surgeons that agreed with the out of which 2 (40%) disagreed with guideline
guideline-recommended option for each scenario was recommendation and 3 (60%) agreed with guidelines
calculated, as well as the proportion forming a majority (Figure 1).
[10,11]
for an option. Evidence suggests community
equipoise is low when more than 70% of respondents Consensus and disagree with guideline recommen-
favored one treatment option. Thus, community dations
equipoise was then assessed by classifying the survey There were three scenarios that reached consensus
scenarios into one of four categories based on the but disagreed with guideline recommendations.
proportion of responses: (1) Consensus/Disagree: These were: (1) Initial management of diverticulitis:
scenarios with > 70% of surgeons choosing an option The consensus being admitting for bowel rest and
that disagrees with guideline recommendation; (2) intravenous antibiotics (76%) as opposed to guideline
Equipoise/Disagree: scenarios with ≤ 70% of surgeons recommendation of outpatient management on
choosing an option that disagrees with guideline oral antibiotics (18%). Four percent would provide
WJGS|www.wjgnet.com 226 November 27, 2017|Volume 9|Issue 11|
Siddiqui J et al . Diverticulitis and guideline consensus
Guideline based
Scenarios
(19)
Consensus Community
(14) equipoise
(5)
Agree with Disagree with Agree with Disagree with
guidelines guidelines guidelines guidelines
(11) (3) (3) (2)
Consensus/Agree Consensus/Disagree Equipoise/Agree Equipoise/Disagree
Figure 1 Summary of survey responses forming the four categories.
supportive care without the use of antibiotics; (2) to conservative management. Univariate analyses
Failure of conservative management for uncomplicated demonstrated that a significantly greater number of
sigmoid diverticulitis: The consensus being to repeat those practicing in a rural/regional or a secondary
CT scan of abdomen (71%, shown by multivariate referral center compared with those in a tertiary or
analysis to be more likely if practicing for greater than quaternary referral center (91% vs 56%, P = 0.002),
10 years - 80% vs 59%, P = 0.043) as opposed to and those practicing for more than 10 years (71%
organizing an emergency sigmoid colectomy (11%, vs 50%, P = 0.047) was associated with this; (2)
more likely if working in a rural/regional center - Hinchey Grade 3 management. Fifty-six percent
50% vs 8%, Fisher’s exact test P = 0.016); and (3) would do a Hartmann’s procedure as opposed to 3%
Management following recovery from an episode of choosing resection with primary anastomosis and
complicated diverticulitis: The consensus being no diverting colostomy and 34% choosing on table colonic
operative management (92%) as opposed to resection lavage and colorectal anastomosis with diverting loop
(7%). ileostomy. A greater proportion of North American sub-
specialty trained surgeons (87% vs 51%, Fisher’s exact
Community equipoise test P = 0.009) and non-Australasian trained surgeons
Equipoise and disagree with guidelines recom (77% vs 46%, P = 0.002) would perform a Hartmann’s
mendations: There were two scenarios with equipoise procedure in this case, as well those practicing for
and disagreed with guideline recommendation. These more than 10 years (67% vs 32%, P = 0.001) and
were: (1) Imaging modality when CT contraindicated. surgeons aged over 50 years old (70% vs 40%, P
The majority opinion was to perform a CT scan (57%), = 0.002); and (3) Proximal extent of resection. The
with some stating without contrast. Only 21% agreed majority (57%) would remove colon where there is
to the alternative of US or MRI. 71 percent of surgeons thickened, inflamed and hypertrophic tissue and resect
practicing less than 10 years vs 48% practicing for the whole sigmoid colon (62% of Australian based
more than 10 years would choose CT scan when CT vs 35% of New Zealand based surgeons, P = 0.04),
was contraindicated (P = 0.03). Choosing US or MRI whereas 14% would only do the former and 24%
was more likely if the surgeon was aged over 50 years would only do the latter.
old (30% vs 11%, Fisher’s exact test P = 0.017); (2)
Use of bowel preparation and antibiotics prior to elective Consensus and agree with guideline recommendations
colectomy. The majority (57%) of respondents would use There were eleven scenarios that reached consensus
oral, mechanical bowel preparation prior to the procedure and agreed with guideline recommendations. These
and Ⅳ antibiotics on induction of general anesthesia. This are summarized in Table 2.
was more likely to be the case if the surgeon was aged The remaining three scenario-based questions that
over 50 years old (67% vs 47%, P = 0.04). did not relate to guidelines were based on surgical
management options. In a patient undergoing resection
Equipoise and agree with guideline recom- of the diseased segment in sigmoid diverticulitis,
mendations: There were three scenarios with 42% would complete the operation via a colorectal
equipoise but agreed with guideline recommendations. anastomosis with diverting loop ileostomy ± on-table
These were: (1) Failed conservative management colonic lavage, 31% would complete it with a colorectal
for complicated diverticulitis. Sixty-three percent of anastomosis ± on-table colonic lavage without diversion
respondents agreed to image guided percutaneous and 18% with an end colostomy construction. For
drainage for a 3 cm mesocolic abscess not responding Hinchey Grade 2, where only surgical management
WJGS|www.wjgnet.com 227 November 27, 2017|Volume 9|Issue 11|
Siddiqui J et al . Diverticulitis and guideline consensus
Table 2 Topics that reached consensus and agree with guideline recommendations
Guideline recommendation In agreement (%) P -value
CT scan as initial diagnostic modality 77
Surgeon North American trained 100 vs 73 0.0151
Surgeon practicing in Australia 81 vs 59 0.047
Right-sided diverticulitis - CT initial imaging 93
Surgeon age < 50 years old 100 vs 89 0.021
Right-sided diverticulitis - Initial management oral/IV antibiotics and bowel 95
rest
Surgeon practicing in Australia 98 vs 82 0.0331
Small diverticular abscess management with antibiotics/bowel rest 77
Surgeon North American trained 100 vs 73 0.0151
Large left-sided diverticular abscess management with percutaneous drainage 81
Large right-sided diverticular abscess - percutaneous drainage 83
Absence of ASU at surgeons place of practice 93 vs 75 0.0161
Hinchey Grade 4 - Hartmann’s procedure 81
Surgeon age > 50 years old 89 vs 72 0.034
Routine elective resection in young patient (< 50 years) NOT recommended 99
For elective anterior resection - extend distal margin to proximal rectum 94
Surgeon Non-European trained 99 vs 82 0.0061
Follow-up for high risk patient with uncomplicated diverticulitis 99
Endoscopic evaluation following acute episode 83
1
Fisher’s exact test P-value. ASU: Acute surgical unit.
options were provided, 48% would resect with primary and occurs when an individual clinician is completely
anastomosis, 20% chose Hartmann’s operation undecided. Community equipoise applies when there
[10]
and 18% chose laparoscopic lavage, with 14% not are differing views among the profession as a whole .
choosing an option and some stating they would not There were three topics with moderate quality
operate and treat conservatively. Multivariate analysis evidence in guideline recommendations; however,
demonstrated that those practicing in a city setting our survey respondents disagreed with these. These
were more likely to choose resection with primary were in the areas of management following failed
anastomosis (55% vs 27%, P = 0.035). In a patient conservative therapy for uncomplicated diverticulitis,
with right-sided diverticulitis with confirmed perforation recovery from an episode of complicated diverticulitis
and a 5 cm abscess formation, 66% would perform and use of bowel preparation and antibiotics for
an ileocecal resection and ileocolic anastomosis. elective resection.
[2]
This was more likely if a surgeon was in practice for The ASCRS practice parameters recommends
more than 10 years (78% vs 41%, P < 0.0001) or an urgent sigmoid colectomy for those in whom non-
based in Australia compared to New Zealand (71% vs operative management of acute diverticulitis fails. This
41%, P = 0.016). By multivariate analysis, practicing includes those who have continued abdominal pain or
for more than 10 years was found to be significant cannot tolerate enteral nutrition secondary to a bowel
for performing an ileocecal resection and ileocolic obstruction or ileus. In our survey, 71% opted for a
anastomosis (P = 0.001) (Figure 2). repeat CT scan instead. This may be a reasonable
The responses to the 19 guideline-based scenario option in order to exclude possible abscess formation
questions are summarized in Figure 3 according to avoiding the need for surgery. The urgency to operate
the sixteen clinically based diverticulitis management should be assessed on a case by case basis depending
topics that they fit into. This is due to the eleven on patient factors.
scenarios that reached consensus and agree scenarios Despite the recommendation of an elective colectomy
in Table 2 being able to coalesce into eight topics. following recovery from an acute episode of complicated
diverticulitis, only 7% of respondents in our survey
[2]
chose this for an ASA grade 2 patient. The ASCRS ,
DISCUSSION [12] [4]
The Netherland , WGO and German guidelines
[13]
Our survey is the first to evaluate both medical and recommend elective colectomy following recovery from
surgical management decisions of simple and complicated an episode of complicated diverticulitis. However, there
diverticulitis within Australasia. It shows there remain is still a need for further research in terms of resection
areas of community equipoise, approximately in a third criteria for this group of patients, which may explain
of the guideline related topics in our survey, and where why Australasian colorectal specialists are still acting
[14]
consensus does exist, it is not always in agreement with conservatively. In contrast, the Danish guidelines
accepted guidelines. Some management decisions were do not recommend elective resection unless it is for
[3]
found to be dependent on duration of practice. patients with fistula or stenosis. Vennix et al concluded
Individual equipoise measures clinical uncertainty in their systematic review of guidelines that surgery
WJGS|www.wjgnet.com 228 November 27, 2017|Volume 9|Issue 11|
Siddiqui J et al . Diverticulitis and guideline consensus
Practicing > 10 years Practicing < 10 years
90
80 79
80
71 71
67
70
Percentage (%)
59
60 50
48
50 41
40 32
30
20
10
0
Use CT for diagnosis Repeat CT for failed Percutaneous Hartmann's Ileocecal resection
when CT conservative drainage for failed operation for and ileocolic
contraindicated therapy of conservative Hinchey grade 3 anastamosis for
(P = 0.030) uncomplicated therapy of abscess (P = 0.001) complicated right
diverticulitis (P = 0.047) sided diverticulitis
(P = 0.024) (P = 0.0001)
Figure 2 Areas of significance when considering duration of colorectal surgeons practice. All P values are from χ 2 test.
is not required in the case of conservatively treated in patients with no systemic manifestations of
[18-21]
abscess, however, if it is a pelvic abscess then this can infection, recent studies have pushed towards
[15]
be justified. Recently, a population-based analysis the outpatient management of simple diverticulitis
also showed a decline in elective colectomy following utilizing oral antibiotics. The recommendation is based
an episode of diverticulitis. This was most pronounced on the belief that the body’s host defense mechanisms
in those younger than 50 years old (17% to 5%) and can manage the inflammation without antibiotics if
with complicated disease states (21% to 8%, P < the patient is otherwise well and immunocompetent.
[22]
0.0001). Chabok et al conducted a randomized control trial
[2]
The ASCRS practice parameters state that (RCT) that showed that treatment with antibiotics did
for elective colon resection, oral mechanical bowel not accelerate recovery nor prevent complications
preparation is not required; however, oral antibiotics or recurrence when compared to treatment without
given pre-operatively may reduce surgical site infections. antibiotics. Similar results were reported in a recent
[23]
Recently the use of oral, mechanical bowel preparation Cochrane review of 3 RCTs . Many of the more recent
has been questioned prior to elective colectomy and guidelines have moved towards advising outpatient
the ASCRS guidelines recommend the use of oral treatment for those with minimal comorbidities and
[24]
antibiotics to reduce surgical site infections (SSI). A otherwise well. Jackson et al published a systematic
large systematic review found no statistically significant review on this showing that 97% of patients were
evidence that patients undergoing colonic surgery successfully treated in an outpatient type setting. The
[25]
benefit from mechanical bowel preparation. Guenaga DIVER trial also demonstrated this, where patients
et al [16] conducted a meta-analysis showing there was received a dose of Ⅳ antibiotics in the emergency
no benefit of mechanical bowel preparation in terms department and then were randomized to being
of reduced rates of wound infection or anastomotic hospitalized or discharged for management. The Delphi
[17] [8]
failure. Bellows’s et al meta-analysis showed that study demonstrated international acceptance of this
[5,6]
use of oral and IV antibiotics reduced risk of surgical as well as other survey studies . Contrary to this, the
wound infection (RR 0.57, 95%CI: 0.43-0.76, P = majority (76%) of respondents in our study elected
0.0002), but had no effect on organ space infections to admit for bowel rest and Ⅳ antibiotics. Whether
or risk of anastomotic leak. There is still lack of high- this view may change with a high-quality study being
grade research looking specifically at diverticulitis and conducted in Australasia needs to be seen.
[5-8]
colonic surgery. Our survey showed that surgeons In keeping with other survey studies and with
[2]
aged over 50 years old were more likely to use oral, current guidelines , the majority (77%) of surgeons
mechanical bowel preparation and IV antibiotics on GA opted for CT scan as initial diagnostic modality.
induction compared to those under 50 years. However, only 21% would utilize an US or MRI where
There were two topics with low quality evidence in CT was contraindicated, with some stating they would
guideline recommendations that our survey respondents perform a CT without contrast. This is despite the
disagreed with. This included initial management of fact that US has been shown to have a comparable
[2,26]
uncomplicated diverticulitis and initial diagnostic modality diagnostic accuracy to CT . Nevertheless, US does
when CT contraindicated. have its limitations and is inferior when considering
[27]
For management of simple, uncomplicated diverticulitis diagnosis of alternative diseases .
WJGS|www.wjgnet.com 229 November 27, 2017|Volume 9|Issue 11|
Siddiqui J et al . Diverticulitis and guideline consensus
Consensus/Agree
Initial diagnostic modality (left and right-sided diverticulitis)
Equipoise/Agree
Imaging
Equipoise/Disagree Imaging modality when CT contraindicated
Consensus/Disagree
Simple, left sided diverticulitis
Initial
Simple, right-sided diverticulitis
management
Complicated, left and right-sided diverticulitis
Simple, diverticulitis
Failure of initial
management
Complicated, diverticulitis
Hinchey grade 3 management
Topics
Hinchey grade 4 management
Proximal extent of resection
Surgical therapy
Extent of distal margin
Bowel prep and antibiotics
Elective resection young age
High risk patient management
Follow-up Post recovery from complicated diverticulitis
Endoscopic evaluation post acute episode
Figure 3 Summary by topic (responses agree/disagree with guidelines, consensus or equipoise).
Controversy remains regarding the best surgical option favored over Hartmann’s procedure. However, a number
for Hinchey Grades 3 and 4 diverticulitis. Like previous of limitations were identified following publication. Binda
[6,8]
surveys , the majority opted for Hartmann’s procedure et al [30] brought to attention a number of issues with
for Hinchey Grade 4. However, there remains a divide the trial, including selection bias, surgeons refusing to
between Hartmann’s and primary anastomosis with randomize certain patients, the inclusion of patients with
diverting loop ileostomy for Hinchey Grade 3. A perforation not secondary to diverticulitis and failure
[28]
systematic review showed that patients undergoing to base conclusions on the pre-planned endpoint. The
[31]
primary anastomosis had lower mortality; however, LOLA arm (laparoscopic lavage with sigmoidectomy)
[32]
the studies included were low quality with selection of the LADIES trial was prematurely terminated
[29]
bias. A recent multi-center RCT concluded that following increased adverse events post laparoscopic
primary anastomosis with diverting ileostomy is lavage compared with sigmoidectomy. However, we
WJGS|www.wjgnet.com 230 November 27, 2017|Volume 9|Issue 11|
Siddiqui J et al . Diverticulitis and guideline consensus
still await the results of the DIVA arm comparing Applications
Hartmann’s procedure with sigmoidectomy plus Areas of further research identified include initial management of simple
primary anastomosis. This will provide randomized, diverticulitis, failure of conservative management for diverticulitis, whether
recovery following complicated diverticulitis requires operative intervention, use
controlled evidence for this controversial issue.
of bowel preparation and proximal extent of resection for elective resection and
We did not use previous surveys that are already surgical management of Hinchey Grade 3 diverticulitis. Higher quality evidence
published and then compare our responses to them. to back up recommendations for these will result in better outcomes for patients
This is because previous surveys did not cover as and given the increasing disease burden, will also help reduce the future
many aspects of diverticulitis management and did not financial burden on health care organizations dealing with this.
focus as much, if at all, on surgical management. Also,
previously published surveys are heterogeneous in Terminology
terms of areas covered when compared to each other. Evidence suggests community equipoise is low when more than 70% of
respondents favor one treatment option. Thus, community equipoise was
Weaknesses in our study include a suboptimal
assessed by classifying the survey scenarios into one of four categories based
response rate. This may be due in part to the length of on the proportion of responses: (1) Consensus/Disagree: scenarios with > 70%
the survey, which was necessary to explore the topic. of surgeons choosing an option that disagrees with guideline recommendation;
Also, we do not have data on the non-responders (2) Equipoise/Disagree: scenarios with ≤ 70% of surgeons choosing an option
and whether they differed markedly from responders. that disagrees with guideline recommendation; (3) Equipoise/Agree: scenarios
with ≤ 70% of surgeons choosing an option that agrees with guideline
Furthermore, only subspecialty colorectal surgeons
recommendation; and (4) Consensus/Agree: scenarios with > 70% surgeons
were invited to complete this survey in an effort choosing an option that agrees with guideline recommendations.
to maximize the response rate. We acknowledge
that many general surgeons also treat diverticulitis. Peer-review
These factors limit the generalizability of the results. It is an interesting piece to read and publish. It provides very good overview of
Furthermore, responses to clinical scenarios may be Australian surgeons’ opinions on diverticulitis guidelines.
constrained by the multiple choice options, which may
have varied from the respondents’ true preference.
Never-the-less, the survey results are still useful in
REFERENCES
highlighting current practices and areas of equipoise. 1 Cristaudo A, Pillay P, Naidu S. Caecal diverticulitis: Presentation
and management. Ann Med Surg (Lond) 2015; 4: 72-75 [PMID:
In conclusion, this survey has identified areas of
25830021 DOI: 10.1016/j.amsu.2015.02.002]
community equipoise and areas of clinical practice 2 Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD,
that disagree with guideline recommendations in the Rafferty JF. Practice parameters for the treatment of sigmoid
management of diverticulitis. It has also demonstrated diverticulitis. Dis Colon Rectum 2014; 57: 284-294 [PMID:
that despite the availability of guidelines, some areas 24509449 DOI: 10.1097/DCR.0000000000000075]
3 Vennix S, Morton DG, Hahnloser D, Lange JF, Bemelman WA;
in clinical practice reach consensus contrary to these
Research Committee of the European Society of Coloproctocology.
recommendations. In order for guidelines to become Systematic review of evidence and consensus on diverticulitis: an
more widely acceptable, further higher quality research analysis of national and international guidelines. Colorectal Dis
is necessary in these areas. 2014; 16: 866-878 [PMID: 24801825 DOI: 10.1111/codi.12659]
4 Murphy T, Hunt RH, Fried M, Krabshuis JH. World Gastroenterology
Organisation Practice Guidelines. Diverticular Disease, 2007. Available
COMMENTS
COMMENTS from: URL: http://www.worldgastroenterology.org/UserFiles/file/
guidelines/diverticular-disease-english-2007.pdf
Background 5 Schechter S, Mulvey J, Eisenstat TE. Management of uncomplicated acute
Diverticular disease carries a significant disease burden. It ranges from diverticulitis: results of a survey. Dis Colon Rectum 1999; 42: 470-475;
presence of diverticula to simple inflammation to more complex disease discussion 475-476 [PMID: 10215046 DOI: 10.1007/BF02234169]
processes. There are established guidelines with regards to initial investigations 6 de Korte N, Klarenbeek BR, Kuyvenhoven JP, Roumen RM,
and management options for varying severity of disease. It is unclear whether Cuesta MA, Stockmann HB. Management of diverticulitis: results of a
current clinical practice in Australia and New Zealand is in consensus to survey among gastroenterologists and surgeons. Colorectal Dis 2011; 13:
established guidelines. The aim of this study was to determine the application e411-e417 [PMID: 21819518 DOI: 10.1111/j.1463-1318.2011.02744.x]
of clinical practice guidelines for the current management of diverticulitis and 7 Munikrishnan V, Helmy A, Elkhider H, Omer AA. Management
colorectal surgeon specialist consensus in Australia and New Zealand. of acute diverticulitis in the East Anglian region: results of a United
Kingdom regional survey. Dis Colon Rectum 2006; 49: 1332-1340
[PMID: 16897334 DOI: 10.1007/s10350-006-0594-2]
Research frontiers 8 O’Leary DP, Lynch N, Clancy C, Winter DC, Myers E.
There remains disagreement in areas of diverticulitis management including the
International, Expert-Based, Consensus Statement Regarding
move to outpatient management and treatment without antibiotics for simple
the Management of Acute Diverticulitis. JAMA Surg 2015; 150:
diverticulitis; and operative strategies for Hinchey grade 3 and 4 diverticulitis.
899-904 [PMID: 26176318 DOI: 10.1001/jamasurg.2015.1675]
This, together with low quality evidence for some guideline recommendations,
9 Jaung R, Robertson J, Rowbotham D, Bissett I. Current
means that guidelines need to be reviewed and revised with more recent
management of acute diverticulitis: a survey of Australasian
studies.
surgeons. N Z Med J 2016; 129: 23-29 [PMID: 27005870]
10 Johnson N, Lilford RJ, Brazier W. At what level of collective
Innovations and breakthroughs equipoise does a clinical trial become ethical? J Med Ethics 1991;
The achievement of this study is in highlighting areas of equipoise and 17: 30-34 [PMID: 2033628 DOI: 10.1136/jme.17.1.30]
consensus, albeit not with guideline recommendations, to be areas of future 11 Young J, Harrison J, White G, May J, Solomon M. Developing
research to provide better quality evidence so that guidelines may be adopted. measures of surgeons’ equipoise to assess the feasibility of
WJGS|www.wjgnet.com 231 November 27, 2017|Volume 9|Issue 11|
Siddiqui J et al . Diverticulitis and guideline consensus
randomized controlled trials in vascular surgery. Surgery 2004; 136: 775-781 [PMID: 24859874 DOI: 10.1007/s00384-014-1900-4]
1070-1076 [PMID: 15523403 DOI: 10.1016/j.surg.2004.04.012] 25 Biondo S, Golda T, Kreisler E, Espin E, Vallribera F, Oteiza
12 Andeweg CS, Mulder IM, Felt-Bersma RJ, Verbon A, van der Wilt F, Codina-Cazador A, Pujadas M, Flor B. Outpatient versus
GJ, van Goor H, Lange JF, Stoker J, Boermeester MA, Bleichrodt hospitalization management for uncomplicated diverticulitis: a
RP; Netherlands Society of Surgery; Working group from prospective, multicenter randomized clinical trial (DIVER Trial).
Netherlands Societies of Internal Medicine, Gastroenterologists, Ann Surg 2014; 259: 38-44 [PMID: 23732265 DOI: 10.1097/
Radiology, Health echnology Assessment and Dieticians. SLA.0b013e3182965a11]
Guidelines of diagnostics and treatment of acute left-sided colonic 26 Laméris W, van Randen A, Bipat S, Bossuyt PM, Boermeester
diverticulitis. Dig Surg 2013; 30: 278-292 [PMID: 23969324 DOI: MA, Stoker J. Graded compression ultrasonography and computed
10.1159/000354035] tomography in acute colonic diverticulitis: meta-analysis of test
13 Kruis W, Germer CT, Leifeld L; German Society for Gastroenterology, accuracy. Eur Radiol 2008; 18: 2498-2511 [PMID: 18523784 DOI:
Digestive and Metabolic Diseases and The German Society for 10.1007/s00330-008-1018-6]
General and Visceral Surgery. Diverticular disease: guidelines of the 27 Flor N, Maconi G, Cornalba G, Pickhardt PJ. The Current Role of
german society for gastroenterology, digestive and metabolic diseases Radiologic and Endoscopic Imaging in the Diagnosis and Follow-
and the german society for general and visceral surgery. Digestion Up of Colonic Diverticular Disease. AJR Am J Roentgenol 2016;
2014; 90: 190-207 [PMID: 25413249 DOI: 10.1159/000367625] 207: 15-24 [PMID: 27082846 DOI: 10.2214/AJR.16.16138]
14 Andersen JC, Bundgaard L, Elbrønd H, Laurberg S, Walker LR, 28 Constantinides VA, Tekkis PP, Athanasiou T, Aziz O, Purkayastha
Støvring J; Danish Surgical Society. Danish national guidelines S, Remzi FH, Fazio VW, Aydin N, Darzi A, Senapati A. Primary
for treatment of diverticular disease. Dan Med J 2012; 59: C4453 resection with anastomosis vs. Hartmann’s procedure in nonelective
[PMID: 22549495] surgery for acute colonic diverticulitis: a systematic review. Dis
15 Li D, Baxter NN, McLeod RS, Moineddin R, Nathens AB. Colon Rectum 2006; 49: 966-981 [PMID: 16752192 DOI: 10.1007/
The Decline of Elective Colectomy Following Diverticulitis: A s10350-006-0547-9]
Population-Based Analysis. Dis Colon Rectum 2016; 59: 332-339 29 Oberkofler CE, Rickenbacher A, Raptis DA, Lehmann K, Villiger
[PMID: 26953992 DOI: 10.1097/DCR.0000000000000561] P, Buchli C, Grieder F, Gelpke H, Decurtins M, Tempia-Caliera
16 Güenaga KF, Matos D, Wille-Jørgensen P. Mechanical bowel AA, Demartines N, Hahnloser D, Clavien PA, Breitenstein S. A
preparation for elective colorectal surgery. Cochrane Database Syst multicenter randomized clinical trial of primary anastomosis or
Rev 2011: CD001544 [PMID: 21901677 DOI: 10.1002/14651858. Hartmann’s procedure for perforated left colonic diverticulitis
CD001544.pub4] with purulent or fecal peritonitis. Ann Surg 2012; 256:
17 Bellows CF, Mills KT, Kelly TN, Gagliardi G. Combination of 819-826; discussion 826-827 [PMID: 23095627 DOI: 10.1097/
oral non-absorbable and intravenous antibiotics versus intravenous SLA.0b013e31827324ba]
antibiotics alone in the prevention of surgical site infections after 30 Binda GA, Serventi A, Puntoni M, Amato A. Primary anastomosis
colorectal surgery: a meta-analysis of randomized controlled trials. versus Hartmann’s procedure for perforated diverticulitis with
Tech Coloproctol 2011; 15: 385-395 [PMID: 21785981 DOI: peritonitis: an impracticable trial. Ann Surg 2015; 261: e116-e117
10.1007/s10151-011-0714-4] [PMID: 24441815 DOI: 10.1097/SLA.0000000000000536]
18 Al-Sahaf O, Al-Azawi D, Fauzi MZ, El-Masry S, Gillen P. Early 31 Vennix S, Musters GD, Mulder IM, Swank HA, Consten EC,
discharge policy of patients with acute colonic diverticulitis Belgers EH, van Geloven AA, Gerhards MF, Govaert MJ, van
following initial CT scan. Int J Colorectal Dis 2008; 23: 817-820 Grevenstein WM, Hoofwijk AG, Kruyt PM, Nienhuijs SW,
[PMID: 18443803 DOI: 10.1007/s00384-008-0492-2] Boermeester MA, Vermeulen J, van Dieren S, Lange JF, Bemelman
19 Alonso S, Pera M, Parés D, Pascual M, Gil MJ, Courtier R, WA; Ladies trial colloborators. Laparoscopic peritoneal lavage
Grande L. Outpatient treatment of patients with uncomplicated or sigmoidectomy for perforated diverticulitis with purulent
acute diverticulitis. Colorectal Dis 2010; 12: e278-e282 [PMID: peritonitis: a multicentre, parallel-group, randomised, open-
19906059 DOI: 10.1111/j.1463-1318.2009.02122.x] label trial. Lancet 2015; 386: 1269-1277 [PMID: 26209030 DOI:
20 Etzioni DA, Chiu VY, Cannom RR, Burchette RJ, Haigh PI, 10.1016/S0140-6736(15)61168-0]
Abbas MA. Outpatient treatment of acute diverticulitis: rates and 32 Swank HA, Vermeulen J, Lange JF, Mulder IM, van der Hoeven
predictors of failure. Dis Colon Rectum 2010; 53: 861-865 [PMID: JA, Stassen LP, Crolla RM, Sosef MN, Nienhuijs SW, Bosker
20484998 DOI: 10.1007/DCR.0b013e3181cdb243] RJ, Boom MJ, Kruyt PM, Swank DJ, Steup WH, de Graaf EJ,
21 Mizuki A, Nagata H, Tatemichi M, Kaneda S, Tsukada N, Ishii H, Weidema WF, Pierik RE, Prins HA, Stockmann HB, Tollenaar
Hibi T. The out-patient management of patients with acute mild-to- RA, van Wagensveld BA, Coene PP, Slooter GD, Consten EC, van
moderate colonic diverticulitis. Aliment Pharmacol Ther 2005; 21: Duijn EB, Gerhards MF, Hoofwijk AG, Karsten TM, Neijenhuis
889-897 [PMID: 15801924 DOI: 10.1111/j.1365-2036.2005.02422.x] PA, Blanken-Peeters CF, Cense HA, Mannaerts GH, Bruin SC,
22 Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K; AVOD Eijsbouts QA, Wiezer MJ, Hazebroek EJ, van Geloven AA, Maring
Study Group. Randomized clinical trial of antibiotics in acute JK, D’Hoore AJ, Kartheuser A, Remue C, van Grevenstein HM,
uncomplicated diverticulitis. Br J Surg 2012; 99: 532-539 [PMID: Konsten JL, van der Peet DL, Govaert MJ, Engel AF, Reitsma JB,
22290281 DOI: 10.1002/bjs.8688] Bemelman WA; Dutch Diverticular Disease (3D) Collaborative
23 Shabanzadeh DM, Wille-Jørgensen P. Antibiotics for uncomplicated Study Group. The ladies trial: laparoscopic peritoneal lavage
diverticulitis. Cochrane Database Syst Rev 2012; 11: CD009092 or resection for purulent peritonitis and Hartmann’s procedure
[PMID: 23152268 DOI: 10.1002/14651858.CD009092.pub2] or resection with primary anastomosis for purulent or faecal
24 Jackson JD, Hammond T. Systematic review: outpatient management peritonitis in perforated diverticulitis (NTR2037). BMC Surg 2010;
of acute uncomplicated diverticulitis. Int J Colorectal Dis 2014; 29: 10: 29 [PMID: 20955571 DOI: 10.1186/1471-2482-10-29]
P- Reviewer: Isik A, Kirshtein B, Lo ZJ, Nah YW, Rubbini M, Wu ZQ,
Zhu WM S- Editor: Ji FF L- Editor: A E- Editor: Zhao LM
WJGS|www.wjgnet.com 232 November 27, 2017|Volume 9|Issue 11|
Published by Baishideng Publishing Group Inc
7901 Stoneridge Drive, Suite 501, Pleasanton, CA 94588, USA
Telephone: +1-925-223-8242
Fax: +1-925-223-8243
E-mail: bpgoffice@wjgnet.com
Help Desk: http://www.f6publishing.com/helpdesk
http://www.wjgnet.com
© 2017 Baishideng Publishing Group Inc. All rights reserved.
You might also like
- Erba Lisawash Service ManualDocument9 pagesErba Lisawash Service ManualEricj Rodríguez100% (1)
- ASCO-SEP Medical Oncology Self-Evaluation Program, 7e by ASCODocument730 pagesASCO-SEP Medical Oncology Self-Evaluation Program, 7e by ASCOandrei vladNo ratings yet
- Diverticulitis AGA CPGDocument7 pagesDiverticulitis AGA CPGImam WakedNo ratings yet
- GastrointestinalDocument13 pagesGastrointestinalIndra D. KristionoNo ratings yet
- WJGS 10 6Document11 pagesWJGS 10 6WILLIAM RICARDO EFFIO GALVEZNo ratings yet
- WJH 9 1001Document11 pagesWJH 9 1001titis dwi tantiNo ratings yet
- Gastrointestinal Pathophysiology: World Journal ofDocument20 pagesGastrointestinal Pathophysiology: World Journal ofMagdalila Pua RosalesNo ratings yet
- Aki 2Document14 pagesAki 2fahad nokiaNo ratings yet
- Pityriasis Rosea: A Comprehensive ClassificationDocument13 pagesPityriasis Rosea: A Comprehensive ClassificationaaNo ratings yet
- Diabetes: World Journal ofDocument15 pagesDiabetes: World Journal ofAnca LunguNo ratings yet
- 2018 Role Endoscopy Caustik TraumaDocument14 pages2018 Role Endoscopy Caustik Traumasolikin ikinNo ratings yet
- Qol JournalDocument14 pagesQol JournalAgus Tamil ArifinNo ratings yet
- WJGS 11 143Document16 pagesWJGS 11 143fikriafisNo ratings yet
- WJGPT 8 90 1 PDFDocument13 pagesWJGPT 8 90 1 PDFAngga Aryo LukmantoNo ratings yet
- Bariatric Surgery and Long-Term Nutritional IssuesDocument15 pagesBariatric Surgery and Long-Term Nutritional IssuesfabiolaNo ratings yet
- WJG 25 2058Document18 pagesWJG 25 2058Ummul HayatiNo ratings yet
- WJCC 7 1535Document24 pagesWJCC 7 1535Patty Alarcón ParraNo ratings yet
- WJCC 6 322Document18 pagesWJCC 6 322Intan PermatasariNo ratings yet
- Gastroenterology: World Journal ofDocument19 pagesGastroenterology: World Journal ofRengganis PutriNo ratings yet
- WJG-25-1640 2Document18 pagesWJG-25-1640 2Francisco Javier Mercado SánchezNo ratings yet
- Doctor FishDocument39 pagesDoctor Fishzagad04No ratings yet
- WJG 25 2863Document20 pagesWJG 25 2863Pilar AufrastoNo ratings yet
- Microembolic Signal Detection by Transcranial Doppler Old Method With A New IndicationDocument8 pagesMicroembolic Signal Detection by Transcranial Doppler Old Method With A New IndicationSombat MuengtaweepongsaNo ratings yet
- WJGPT 10 1 PDFDocument25 pagesWJGPT 10 1 PDFayleen rivera tenorioNo ratings yet
- Gastroenterology: World Journal ofDocument18 pagesGastroenterology: World Journal ofHana Nuraisa BasyaNo ratings yet
- WJG RegoDocument32 pagesWJG Regojesus llumpoNo ratings yet
- WJG 25 3787Document16 pagesWJG 25 3787St. Nur SyamsiahNo ratings yet
- WJN 8 1Document14 pagesWJN 8 1AmeldaNo ratings yet
- WJN 8 44Document19 pagesWJN 8 44Dokdem AjaNo ratings yet
- WJN 7 148Document11 pagesWJN 7 148AmeldaNo ratings yet
- Wjcid 7 46Document8 pagesWjcid 7 46aalmadasalazarNo ratings yet
- WJCC 7 1206Document12 pagesWJCC 7 1206Grace Bella NovaliaNo ratings yet
- WJGS 12 9Document12 pagesWJGS 12 9Hector ReinozoNo ratings yet
- WJCC 8 1172Document13 pagesWJCC 8 1172johoba5344No ratings yet
- Impact of A Simulation-Based Induction Programme IDocument18 pagesImpact of A Simulation-Based Induction Programme ISohaib Mohammad KhanNo ratings yet
- WJH-11-421 2Document25 pagesWJH-11-421 2HNINNo ratings yet
- WJG 23 6137Document16 pagesWJG 23 6137MUHAMMAD09No ratings yet
- WJG 23 7765Document16 pagesWJG 23 7765Pierre GonzalesNo ratings yet
- Inflam&fibrosis Rev WJG-2020Document29 pagesInflam&fibrosis Rev WJG-2020Banchob SripaNo ratings yet
- Radiology: World Journal ofDocument20 pagesRadiology: World Journal ofFitrah AfdhalNo ratings yet
- Vargaz 2017 - Role of Interleukin-1-Family Cytokines On Effector CD4 T Cell DifferentiationDocument12 pagesVargaz 2017 - Role of Interleukin-1-Family Cytokines On Effector CD4 T Cell DifferentiationYoerizta RatuNo ratings yet
- Perforated Peptic Ulcer - An Update: ArticleDocument14 pagesPerforated Peptic Ulcer - An Update: ArticleMuhammad ibnu kaesar PurbaNo ratings yet
- How To Perform Gastrointestinal Ultrasound AnatomyDocument17 pagesHow To Perform Gastrointestinal Ultrasound AnatomyElisabeth PermatasariNo ratings yet
- WJH 11 250Document15 pagesWJH 11 250HNINNo ratings yet
- Handbook of Hepato-Pancreato-Biliary Surgery PDFDocument469 pagesHandbook of Hepato-Pancreato-Biliary Surgery PDFRisyad Ibrahim Pradana100% (1)
- WJN 7 155Document10 pagesWJN 7 155AmeldaNo ratings yet
- Download Bone 2Nd Edition G Petur Nielsen full chapterDocument67 pagesDownload Bone 2Nd Edition G Petur Nielsen full chapterdorothy.carr400100% (3)
- Gastroenterology: World Journal ofDocument23 pagesGastroenterology: World Journal ofLarissa MeloNo ratings yet
- NASH - Non-Alcoholic Fatty Liver Disease and Atherosclerosis at A Crossroad The Overlap of A Theory of Change and BioinformaticsDocument11 pagesNASH - Non-Alcoholic Fatty Liver Disease and Atherosclerosis at A Crossroad The Overlap of A Theory of Change and BioinformaticsntnquynhproNo ratings yet
- Gastrointestinal Pharmacology and Therapeutics: World Journal ofDocument24 pagesGastrointestinal Pharmacology and Therapeutics: World Journal ofDwi atikaNo ratings yet
- Complementary Roles of Interventional Radiology and Therapeutic Endoscopy in GastroenterologyDocument16 pagesComplementary Roles of Interventional Radiology and Therapeutic Endoscopy in GastroenterologyMANGNo ratings yet
- 09 Antigen Cancer 2017 DecDocument12 pages09 Antigen Cancer 2017 DecGabriela MilitaruNo ratings yet
- Download ebook Bone Pdf full chapter pdfDocument67 pagesDownload ebook Bone Pdf full chapter pdfjean.ransdell165100% (22)
- Gastroenterology: World Journal ofDocument18 pagesGastroenterology: World Journal ofDeasy PutriNo ratings yet
- Diarrhea After Bariatric Procedures: Diagnosis and TherapyDocument13 pagesDiarrhea After Bariatric Procedures: Diagnosis and TherapyAndrei SarmientoNo ratings yet
- 4 2 KdigoDocument242 pages4 2 KdigoPatricia Denise Tome MagisaNo ratings yet
- Hepatology: World Journal ofDocument18 pagesHepatology: World Journal ofHNINNo ratings yet
- Guide to Managing Post-Op PainDocument28 pagesGuide to Managing Post-Op Painnijad jabrNo ratings yet
- 10.1177 2192568217701914Document14 pages10.1177 2192568217701914richardson.gabrielNo ratings yet
- Use of Sodium Bicarbonate and Blood Gas Monitoring in Diabetic KetoacidosisDocument11 pagesUse of Sodium Bicarbonate and Blood Gas Monitoring in Diabetic Ketoacidosisdchh096No ratings yet
- Epidemiology of Viral Hepatitis in SomaliaDocument36 pagesEpidemiology of Viral Hepatitis in SomaliaDr Mohamed KadleNo ratings yet
- Clinical Endocrine OncologyFrom EverandClinical Endocrine OncologyIan D. HayRating: 5 out of 5 stars5/5 (1)
- SAGES Consent 2019 2023Document16 pagesSAGES Consent 2019 2023cNo ratings yet
- DiverticulitisDocument18 pagesDiverticulitisTom BiusoNo ratings yet
- Diverticulita Cu Aer OlandaDocument6 pagesDiverticulita Cu Aer OlandacNo ratings yet
- AntiagreganteDocument19 pagesAntiagregantecNo ratings yet
- Coronary Chronic Total Occlusion CTO A ReviewDocument8 pagesCoronary Chronic Total Occlusion CTO A ReviewcNo ratings yet
- A. Gudang Farmasi 2023 (Feni Dwi) UpdateDocument882 pagesA. Gudang Farmasi 2023 (Feni Dwi) UpdatehefikurniasariNo ratings yet
- Continual Improvement ProcedureDocument6 pagesContinual Improvement ProcedureRonald Sarillana100% (1)
- Before - During - After A Volcano EruptionDocument3 pagesBefore - During - After A Volcano EruptionVaughn Jay GonzalesNo ratings yet
- Wa0002.Document9 pagesWa0002.SojiNo ratings yet
- Retinol in CosmeticsDocument204 pagesRetinol in CosmeticsMarrauNo ratings yet
- Long-Term Mortality After The Blood Pressure and Lipid-Lowering Treatment in Hypertensive Patients: 16-Year Follow-Up of The ASCOT Legacy StudyDocument22 pagesLong-Term Mortality After The Blood Pressure and Lipid-Lowering Treatment in Hypertensive Patients: 16-Year Follow-Up of The ASCOT Legacy StudyFlore HountondjiNo ratings yet
- 의약품동등성시험기준 해설서 요약Document137 pages의약품동등성시험기준 해설서 요약Travis JeonNo ratings yet
- Adaptive Community for Continuity of EducationDocument2 pagesAdaptive Community for Continuity of EducationAina Gail LontocNo ratings yet
- General Topics: Anesthesia, Analgesia, and Sedation of Small MammalsDocument23 pagesGeneral Topics: Anesthesia, Analgesia, and Sedation of Small Mammalsdoja catNo ratings yet
- Research ProjectDocument6 pagesResearch Projectapi-357418960No ratings yet
- Material Safety Data Sheet for York L Synthetic LubricantDocument8 pagesMaterial Safety Data Sheet for York L Synthetic LubricantGabriel VoglarNo ratings yet
- Townshend - Effectivness of Mindful Parents ProgramsDocument40 pagesTownshend - Effectivness of Mindful Parents ProgramsDavid ZNo ratings yet
- Career ObjectivesDocument4 pagesCareer ObjectivesJennifer Davis CondimanNo ratings yet
- CHAPTER 1 Nursing As A ProfessionDocument3 pagesCHAPTER 1 Nursing As A ProfessionKarl ZacariasNo ratings yet
- Resona r9 Platinum Multi Parametric Breast SolutionDocument2 pagesResona r9 Platinum Multi Parametric Breast SolutionXing LuNo ratings yet
- LanoLip Power Point PresentationDocument12 pagesLanoLip Power Point PresentationWalter Sanchez EscobarNo ratings yet
- IntelliSort HDS Maintenance ManualDocument118 pagesIntelliSort HDS Maintenance ManualJulio César HernándezNo ratings yet
- Week 4 English 9: Judging The Validity of The Evidence From A TextDocument4 pagesWeek 4 English 9: Judging The Validity of The Evidence From A TextMaria Carmela ArellanoNo ratings yet
- IBPS Prelims CallDocument5 pagesIBPS Prelims CallPrakash RajNo ratings yet
- Power of Play An Evidence BaseDocument64 pagesPower of Play An Evidence BaseIsaiNo ratings yet
- Covid MemoDocument4 pagesCovid Memocharlie malalangNo ratings yet
- 6 135Document6 pages6 135Ashok LenkaNo ratings yet
- Frist Aid PPT For Pharm PDFDocument257 pagesFrist Aid PPT For Pharm PDFAbdulwhab MohammedNo ratings yet
- Cancer and Its Easy Treatment in Homeopathy - Bashir Mahmud ElliasDocument5 pagesCancer and Its Easy Treatment in Homeopathy - Bashir Mahmud ElliasBashir Mahmud ElliasNo ratings yet
- Kindly Read and Check For The Correctness of The Answers Provided As Well As Providing Answers To The Asteriks Numbers Which Are Represented in RedDocument4 pagesKindly Read and Check For The Correctness of The Answers Provided As Well As Providing Answers To The Asteriks Numbers Which Are Represented in RedHilary AnozieNo ratings yet
- Exerciții Pe TEXT 2Document27 pagesExerciții Pe TEXT 2Balanean TatianaNo ratings yet
- Systematic Literature Review Thematic AnalysisDocument4 pagesSystematic Literature Review Thematic Analysishyz0tiwezif3100% (1)
- Behavioral Perspective On Mental Health and IllnessDocument12 pagesBehavioral Perspective On Mental Health and IllnessMonisha LakshminarayananNo ratings yet
- Chemistry Lesson PlanDocument6 pagesChemistry Lesson Planapi-509031396No ratings yet