Professional Documents
Culture Documents
Vestibular Migraine: Understanding a Distinct Clinical Entity
Uploaded by
Juan Hernández GarcíaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vestibular Migraine: Understanding a Distinct Clinical Entity
Uploaded by
Juan Hernández GarcíaCopyright:
Available Formats
Review
Vestibular migraine: clinical aspects and pathophysiology
Joseph M Furman, Dawn A Marcus, Carey D Balaban
Lancet Neurol 2013; 12: 706–15 Vestibular migraine is becoming recognised as a distinct clinical entity that accounts for a high proportion of patients
This online publication has with vestibular symptoms. A temporal overlap between vestibular symptoms, such as vertigo and head-movement
been corrected. intolerance, and migraine symptoms, such as headache, photophobia, and phonophobia, is a requisite diagnostic
The corrected version first
criterion. Physical examination and laboratory testing are usually normal in vestibular migraine but can be used to
appeared at thelancet.com/
neurology on September 15, rule out other vestibular disorders with overlapping symptoms. The pathophysiology of vestibular migraine is
2014 incompletely understood but plausibly could include neuroanatomical pathways to and from central vestibular
Department of Otolaryngology structures and neurochemical modulation via the locus coeruleus and raphe nuclei. In the absence of controlled
(Prof J M Furman MD, trials, treatment options for patients with vestibular migraine largely mirror those for migraine headache.
Prof C D Balaban PhD) and
Department of Anesthesiology
(Prof D A Marcus MD),
Introduction appropriately classified as a type of migraine with aura.4
University of Pittsburgh, Although recurrent vertigo in children was known to be In two groups of patients with basilar-type migraine,
Pittsburgh, PA 15213, USA associated with migraine since Basser’s description in 61–63% reported vertigo as a symptom.5,6 However, few
Correspondence to: 1964,1 in 1984 Kayan and Hood2 alerted the clinical migraine patients with vestibular symptoms meet criteria
Prof Joseph M Furman, community to an important association between for basilar-type migraine.7 Additionally, although some
University of Pittsburgh School
of Medicine, Pittsburgh,
vestibular symptoms and migraine in adults. Since that patients with migraine have vertigo as a premonitory
PA 15213, USA time, appreciation of the role of migraine in the dizzy symptom, the vertigo cannot often be characterised as an
furmanjm@upmc.edu patient has grown. In fact, although a migrainous aura because of its duration or temporal association with
aetiology for vestibular symptoms was previously headache. Thus, with present International Headache
unknown or deemed highly speculative, members of the Society classification criteria, the vestibular symptoms of
International Headache Society in collaboration with many patients with migraine would be deemed unrelated
members of the Barany Society have published diagnostic to migraine. However, most migraine patients with
criteria for a disorder called vestibular migraine.3 As vestibular symptoms do not have a recognised
vestibular migraine is rapidly becoming recognised as a independent vestibular disorder such as Ménière’s
common vestibular disorder, and diagnostic criteria have disease, benign paroxysmal positional vertigo, or
been promulgated, the specialty is poised to make vestibular neuritis. As a result, many patients with both
substantial advances in understanding the patho- migraine and vestibular symptoms do not have a specific
physiology of this disorder and improving its diagnosis to account for their vestibular symptoms. In
management. In this Review, we provide an update response to this deficiency when reaching an accurate
regarding both the clinical aspects of vestibular migraine diagnosis in many migraine patients with vestibular
and the neurobiological basis for the disorder. Our symptoms, Neuhauser and colleagues8 developed
current understanding of vestibular migraine is diagnostic criteria for what is now termed vestibular
rudimentary but continues to evolve. We aim to provide migraine, a disorder in which vestibular symptoms are
both clinicians and clinician-scientists with the latest judged as part of the migrainous disorder itself.
relevant information regarding this frequently en- Nearly 1% of the general population meet these criteria,8
countered disorder and with the latest ideas and basic which is five to ten times higher than the prevalence of
science findings germane to the pathophysiology and Ménière’s disease.9
rational treatment of vestibular migraine. Neuhauser and colleagues’8 criteria for vestibular
migraine have been reassessed favourably in a recent
Diagnostic criteria long-term follow-up paper.10 A structured diagnostic
Patients frequently present with a combination of interview using the criteria11 has been used in studies of
migraine and vestibular symptoms.2 The assessment of the clinical features, epidemiology, genetics, patho-
these patients needs to address the association between physiology, and treatment of vestibular migraine. The
these disorders. That is, are the vestibular symptoms most recent diagnostic criteria for vestibular migraine, a
causally related to a migraine subtype; are the vestibular refinement of the 2001 Neuhauser and colleagues
symptoms and the migrainous symptoms simply a criteria, arose from a working group within the Barany
chance co-occurrence, or is there some more complex Society (panel).3 Recently, Cohen and colleagues12
comorbidity association? Currently, the only Inter- advocated the development of diagnostic criteria by the
national Headache Society migrainous disorder that International Headache Society to account for the
includes vertigo in its classification is basilar-type heterogeneity and natural history of vestibular migraine.
migraine, which is characterised by the occurrence of Internationally proposed diagnostic criteria for vestibular
neurological symptoms originating from the brainstem migraine based on those developed by the Barany Society
or both cerebral hemispheres simultaneously. The and the International Headache Society3 will be included
diagnosis of basilar-type migraine might be more in an appendix of the third edition of the International
706 www.thelancet.com/neurology Vol 12 July 2013
Review
Classification of Headache Disorders. This appendix will
suggest that vestibular migraine is a new disorder for Panel: Diagnostic criteria for vestibular migraine
which more research is warranted. Patients need to meet all four of the following criteria:
Vestibular migraine can be thought of as a migraine • At least five episodes with vestibular symptoms* of
variant with vestibular symptoms or a balance disorder moderate or severe intensity† lasting between 5 min and
that includes migraine. Although such a distinction 72 h
might seem to have little clinical relevance, because • Present migraine or previous history of migraine with or
patients with vestibular migraine can present to either without aura according to the International Classification
otolaryngologists or neurologists, patients might receive of Headache Disorders
different care depending on the type of specialist to • One or more migraine features with at least 50% of the
whom they present. A study by Millen and colleagues13 vestibular episodes
shows that specialists have different views regarding the • Headache with at least two of the following
manifestations of vestibular migraine. For example, characteristics: one-sided location, pulsating quality,
more neurologists than otolaryngologists believe that moderate or severe pain intensity, aggravation by
vestibular migraine results from a CNS rather than a routine physical activity
peripheral vestibular abnormality. • Photophobia and phonophobia
• Visual aura
Epidemiology • Not explained by another vestibular disorder
Vestibular migraine is more prevalent than other vestibular
*Vestibular symptoms include: spontaneous vertigo, positional vertigo, visually induced
disorders.14 Lempert and Neuhauser15 report a lifetime
vertigo, head motion-induced vertigo, head motion-induced dizziness with nausea.
prevalence of migraine of 16%, a lifetime prevalence of †Vertigo is rated as moderate if vertigo interferes with but does not prohibit daily
vertigo of 7%, and a comorbidity of 3·2 %, rather than the activities and as severe if daily activities cannot be continued. Modified from Lempert and
colleagues,3 by permission of IOS Press.
1·1% expected by chance alone. Neuhauser and colleagues16
report that vestibular migraine has a 1-year prevalence of
0·89% and accounts for about 10% of patients seen for generally lower in individuals with vestibular migraine,16
dizziness and about 10% of patients seen for migraine.17 including problems with sleep and depression.20
Hsu and colleagues18 report that the 1-year prevalence of
vestibular migraine in women aged 40–54 years is 5%. Physical examination
The physical examination of patients with vestibular
Clinical characteristics migraine is generally normal between episodes. During
Symptoms episodes of vestibular migraine, patients usually manifest
For most patients, vestibular migraine is an episodic a nystagmus that suggests either a central or peripheral
disorder; however, the duration of attacks ranges from vestibular abnormality.21–23 Non-paroxysmal positional
seconds to days. Vestibular migraine has a strong female nystagmus is especially common during attacks of
predominance of up to 5 to 1,11 and vestibular migraine vestibular migraine.
often begins several years after typical migraine. Some
patients can have a headache-free interval of several years Physiological testing
before onset of vestibular migraine. Vestibular migraine Physiological findings alone cannot be used to specifically
might begin in place of headache especially in diagnose patients with vestibular migraine because of
perimenopausal women.19 Vestibular migraine is more their inconsistent pattern and high incidence in patients
common in patients without aura than in patients with with migraine without vestibular complaints.24 However,
aura. The temporal association between the vestibular physiological testing can be used to help rule out other
symptoms and migrainous symptoms such as headache vestibular disorders and to establish the extent of vestibular
is quite variable between patients and the association abnormalities if they exist. Between 10% and 20% of
might be inconsistent in an individual. Furthermore, patients with vestibular migraine have a unilateral
patients might have migraine headache at the same time reduction of vestibular function24–26 and many patients have
as their vestibular symptoms, which include spontaneous a directional preponderance.25 Teggi and colleagues27 and
vertigo—ie, an illusory sensation of motion of self or Celebisoy and co-workers26 found that patients with
surround, dizziness induced by head movement, vestibular migraine had higher postural sway than did
positional vertigo, or gait instability. Other symptoms can patients without vestibular migraine. Two studies have
include visual motion sensitivity and hearing loss, and documented abnormalities of vestibular-evoked myogenic
migrainous symptoms such as photophobia or potentials in patients with vestibular migraine including
phonophobia. Episodes of vestibular migraine can be reduced amplitudes either unilaterally or bilaterally.28,29
brought about by the same triggers as those for migraine
headache, including menstruation, irregular sleep, stress, Genetics
physical exertion, dehydration, food and drinks, and Several studies have investigated the genetics of
intense sensory stimulation.17 Quality of life measures are vestibular migraine. Jen30 concluded that vestibular
www.thelancet.com/neurology Vol 12 July 2013 707
Review
migraine might be monogenic and heterogeneous. Von evidence base is available and no randomised controlled
Brevern and colleagues31 found no evidence of an trials for the treatment of vestibular migraine exist, mainly
association between calcium and sodium channel genes because of the hitherto lack of diagnostic criteria. Instead,
linked to familial hemiplegic migraine and episodic treatments are based on those for migraine headache or
ataxia type 2 and vestibular migraine. Lee and colleagues32 are anecdotal. Avoidance of migraine triggers should
found a region on chromosome 11q that is common in always be the first avenue of treatment. Pharmacotherapy
females in a family with vestibular migraine. Bahmad can be abortive, symptomatic for episodes, and
and colleagues33 located a 12·0 MB interval on prophylactic. Although diagnostic criteria for vestibular
chromosome 5q35 that contained a disease gene for migraine are now available, no randomised treatment
familial vestibular migraine. The pathophysiology of this studies have been done, except for a small inconclusive
disease gene remains unknown. study of zolmitriptan as an abortive agent.46 Symptomatic
treatment for acute episodes of vestibular migraine is
Related disorders similar to treatment for acute vertigo with peripheral
Several balance disorders are related to vestibular vestibular causes, including vestibular suppressants such
migraine. Ménière’s disease, benign paroxysmal positional as promethazine, dimenhydrinate, and meclozine.
vertigo, and anxiety are more common in patients with Physical therapy has been reported to improve imbalance
vestibular migraine than would be expected by chance in patients with vestibular migraine in an uncontrolled
alone. The basis for this high comorbidity remains study.47 In general, the scientific literature suggests that
uncertain but might relate to overlaps between the clinical drugs efficacious for prophylaxis of migraine headache
characteristics of these disorders and those of vestibular are also appropriate for prophylaxis of vestibular
migraine, and because vertigo can serve as a migraine migraine.48 On the basis of mainly opinion, and not on
trigger.34 Ménière’s disease and vestibular migraine controlled studies, researchers have advocated β-blockers
overlap extensively in their clinical manifestations, and in such as propranolol or metoprolol; antidepressants such
some patients it might be impossible to establish whether as amitriptyline, nortriptyline, fluoxetine, sertraline, or
they have one or both disorders. Patients with Ménière’s paroxetine; calcium-channel blockers such as verapamil
disease are twice as likely to have migraine as individuals or diltiazem; anticonvulsants such as valproate,
without Ménière’s disease,35 and patients with migraine topiramate, or lamotrigine; and carbonic anhydrase
are more likely to have an earlier onset and bilateral inhibitors such as acetazolamide.49–51
hearing loss with Ménière’s disease.36 Cha and colleagues37
discovered a frequent association among episodic vertigo, Proposed neurobiological bases
migraine, and Ménière’s disease in closely related Present hypotheses of migraine mechanisms are based
individuals. Like patients with Ménière’s disease, patients on results of combined genetic, in-vitro cell biological,
with benign paroxysmal positional vertigo are more likely animal model, and clinical studies in human beings.52–58
to have migraine than patients without benign paroxysmal This well developed published work provides a conceptual
positional vertigo.38 Patients with migraine are also more framework for understanding vestibular migraine as a
likely to have benign paroxysmal positional vertigo than variant produced by the convergence of vestibular
individuals without migraine.39 The highly common information within migraine circuits; therefore, we
finding of persistent rather than paroxysmal positional provide a framework for further development of our
nystagmus in patients with vestibular migraine understanding of vestibular migraine.
complicates this association.22 Psychiatric illness,
especially anxiety and depression, is especially common Vasculature, migraine mechanisms, and the inner ear
in patients with vestibular migraine.40,41 In a prospective The large overlap between migraine pathways and
study of psychiatric illness in vertigo syndromes, only vestibular pathways41,59–61 is consistent with the view that
patients with vestibular migraine had increased rates of vestibular migraine is a migraine variant with vestibular
psychiatric illness 1 year after establishing a vestibular manifestations. Specifically, the vascular, neurogenic
diagnosis.42 Patients with vestibular migraine reported inflammation, and central neural mechanisms that have
more vertigo, more somatic anxiety and autonomic been implicated as peripheral and central triggers of
arousal, and more vertigo-induced handicap than did migraine52–56 are all present in central vestibular pathways
other patients with vertigo.43 Although not strictly a and the inner ear. For example, the trigeminocerebro-
balance disorder, motion sickness susceptibility is more vascular system57 provided a focus to investigate the link
common in patients with migraine in general and patients between vascular responsiveness and pain as a
with vestibular migraine in particular.44,45 physiological consequence of activation of trigeminal
ganglion innervation of cerebral and meningeal
Treatment vasculature. The trigeminovascular system also innervates
Treatment options for patients with vestibular migraine the blood supply of the inner ear.62,63 Iadecola58 provided a
include reduction of triggers, pharmacotherapy, physical more integrative context for migraine mechanisms,
therapy, and mitigation of comorbidities. No dedicated suggesting that a neocortical, extracellular release of
708 www.thelancet.com/neurology Vol 12 July 2013
Review
signals (eg, K+, H+, arachidonic acid, and nitric oxide) animals and human beings.83–86 The central constituents
during cortical spreading depression would activate of the migraine circuit include components of central
trigeminal afferents on cranial blood vessels, which would vestibular pathways. For example, the regions affected by
elicit a trigeminovascular reflex-mediated vasodilation in vestibular stimulation in human functional imaging
the meninges via a parasympathetic relay in the studies include those involved in migraine and pain
sphenopalatine ganglion. Simultaneously, as described by perception, such as the posterior insula, anterior insula,
Moskowitz,54 a sterile inflammatory response is elicited orbitofrontal cortex, and the posterior and anterior
from meningeal vessels by peptide secretion from axon cingulate gyri.87–93 Additionally, because the caudal
collaterals of the trigeminal ganglion cells. parabrachial nucleus receives both trigeminal
Parallel events have been observed in the inner ear of nociceptive94–96 and vestibular inputs in rodents and
animals.64,65 The trigeminal innervation of the inner ear primates,97–100 the related pathways might contribute to
seems to be a component of trigeminal innervation of symptoms of vestibular migraine, including motion
other intracerebral blood vessels,62,63,66 and similar effects sensitivity and its interaction with trigeminal pain in
on inner ear blood perfusion have been seen in animal migraine patients.97–104 Furthermore, the high expression
experiments.67–70 Because the trigeminovascular reflex of stress-response receptors in the amygdala and
innervation of the inner ear is one component of the hypothalamus105 suggests a role of stress interactions with
trigeminovascular reflex system, the innervation is a development of migraine signs and symptoms.77
potential site of action for abortive effects of triptans,
ergots, and calcitonin gene-related peptide antagonists on Vestibular processing and migraine circuits
peripheral triggers in patients with vestibular migraine. Vestibular migraine is an example of the integral overlap
Migraine prophylaxis drugs, such as acetazolamide and between vestibular pathways and migraine circuit
topiramate, have the potential to support endolymph triggers and central mechanisms for premonitory
homoeostasis by inhibition of carbonic anhydrase in the symptom generation (figure). Information transmitted
stria vascularis and supporting cells of the sensory by peripheral vestibular sensory organs and the vestibular
epithelia.71,72 The fact that spiral and vestibular ganglion nerve to the medulla and pons is an external trigger
cells in rodents and primates express the main serotonin within the migraine circuit construct proposed by Ho
receptor targets of the triptans and ergots and colleagues.53 Hence, the abortive effects of drugs in
(5-hydroxytryptamine [5-HT]1A, 5-HT1B, 5-HT1D, and 5-HT1F the inner ear (eg, triptans, ergots, calcitonin gene-related
receptors) is interesting because their binding affinities peptide antagonists, non-steroidal anti-inflammatory
are within the clinical dose-related plasma concentrations drugs, lamotrigine, calcium-channel blockers, and
of the drugs.60,73–75 Hence, actions of ganglion cells might topiramate) can attenuate a peripheral trigger specific for
partly explain the efficacy of these agents in vestibular vestibular migraine, and affect a central migraine circuit.
migraine. Finally, the effects of non-steroidal anti- Similarly, the perceptual and sensorimotor consequences
inflammatory drugs might include a blunting of both the of unilateral or bilateral disruptions of peripheral
inflammation and extravasation responses by vestibular function constitute internal triggers of
cyclooxygenase inhibition. vestibular migraine within their framework because the
migraine circuit overlaps extensively with the vestibular-
Integrative migraine mechanisms and vestibular related pathways that have been discussed in the context
pathways: translational rules from basic research of comorbidity of balance disorders, migraine, and
Because vasodilation is neither necessary nor sufficient anxiety disorders.59–61 The central vestibular pathways that
for perception of headache pain,56–58,76 migraine headache overlap with internal trigger mechanisms for the
pain is attributed mainly to central processing of migraine circuit have been parsed conceptually into a
trigeminal afferent activation in ascending thalamocortical cognitive-behavioural component, a neurological
pathways.53,56,58 Specifically, Ho and colleagues53 expanded sensorimotor performance component, and an
the idea of the migraine circuit from strictly trigeminal interoceptive component, which are each modulated by
pathways for vascular regulation and pain perception to a the dorsal raphe nucleus and locus coeruleus (figure).
framework that includes circuits for processing triggers The cognitive-behavioural domain encompasses
and premonitory symptoms. External trigger circuits were vestibulo-thalamo-cortical networks that produce
proposed to include visual, auditory, somatosensory, and perceptual responses to vestibular, visual, proprioceptive,
chemical (olfactory and gustatory) sensory pathways, and and somatosensory afferent inputs. The domain also
contributions from vascular phenomena. Internal triggers includes pathways related to premonitory symptoms
include hormonal fluctuations and stress.77 Both internal associated with balance control, such as circuits involving
and external triggers involve structures such as the the ventral lateral prefrontal cortex, orbitofrontal cortex,
hypothalamus and amygdala, which show altered activity and the ventral aspect of the cingulate cortex that
associated with migraine in functional imaging studies,78–82 communicate with the interoceptive domain for regulation
and contain a dense calcitonin gene-related peptide- of affect. The sensorimotor performance component
positive axon plexus among scattered positive neurons in generates somatic and visceral motor responses to afferent
www.thelancet.com/neurology Vol 12 July 2013 709
Review
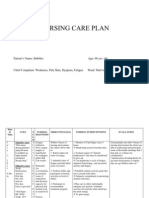
Medulla and pons Midbrain, thalamus, and forebrain
Trigeminovascular reflex Cognition,
Trigeminal pain pathways behaviours
Thalamocortical
processing
Meningeal, brain, and Sensorimotor
labyrinthine vasculature Visceral pathways integration
Amygdala
Vestibular apparatus Vestibular pathways Interoception
Insula Migraine features
Perceptions and sensations
Sensorimotor responses Parabrachial nucleus Premonitory symptoms
• Eye movement
• Head movement
• Postural changes
Autonomic responses Locus coeruleus Dorsal raphe nucleus
Endocrine responses (norepinephrine) (5-hydroxytryptamine)
Figure: Vestibular migraine pathways
Pathways related to sensorimotor performance, interoceptive, and cognitive-behavioural domains within migraine circuits are shown diagrammatically. The boxes
that represent brainstem sensorimotor structures include parallels in peripheral neurochemical organisation between vestibular pathways and migraine
mechanisms.41,106
sensory information. The balance-related sensorimotor intralaminar nuclei including the subparafascicular
component includes brainstem pathways that generate nucleus84,129 and periventricular regions of the
somatic (eg, vestibulo-ocular and vestibulospinal reflexes) hypothalamus. These cells give rise to dense calcitonin
and visceral (vestibulosympathetic and vestibuloparasym- gene-related peptide-immunopositive terminal fields in
pathetic)107,108 motor responses. These vestibular the insular cortex, central amygdaloid nucleus, bed
sensorimotor responses are modulated by the cere- nucleus of the stria terminalis, and the amygdalo-strial
bellum,107,109 which has been activated in human imaging transition region.84 This strong co-localisation of
studies during migraine attacks81,110,111 and shows prominent calcitonin gene-related peptide with central interoceptive
expression of calcitonin gene-related peptide receptors in pathways raises the possibility that central calcitonin
association with Purkinje cells in animals.112 The trigeminal gene-related peptide antagonism is a strategy to both
nociceptive sensorimotor pathways include afferent alter the interpretation of premonitory sensory activity as
sensory thalamocortical pathways, the periaqueductal grey, a symptom and interrupt the progression of external and
and the trigeminovascular reflex circuit. More importantly, internal trigger activity.
neuroanatomical tracing studies have shown extensive The closely connected network between the locus
interconnections among the spinal trigeminal nucleus, coeruleus and dorsal raphe nucleus is a likely target for
vestibular nuclei, and the solitary nucleus100,113–117 and that calcitonin gene-related peptide antagonists and triptans
small cervical dorsal root ganglion cells contribute to in vestibular migraine (figure). This network has the
primary afferent projections to vestibular nuclei.118,119 These potential to modulate vestibular migraine-associated
observations clearly show that the vestibular nuclei premonitory symptoms and triggers of vestibular
contribute to the migraine circuit at the level of the caudal migraine (eg, stress and pain perception) through
brainstem. widespread efferent projections to central migraine and
Interoceptive circuits assess information about present vestibular circuits. The locus coeruleus and the dorsal
sensory and motor processes relative to the physiological raphe nucleus have long been included as modulators of
status of the individual,120 and translate this information both central migraine circuits52,56 and vestibular
into subjective awareness and feelings (often termed the sensorimotor130–134 and interoceptive circuits.59–61 Locus
sentient self).121 Interoceptive circuits for vestibular, coeruleus unit activity in rats and monkeys increases with
visceral sensory, and nociceptive information include a exposure to novel or imperative sensory stimuli,
network that contains the parabrachial nucleus, central particularly during reorientation of attention in contexts
amygdaloid nucleus, and bed nucleus of the stria associated with stress or anxiety.135–137 A large proportion of
terminalis, several posterior thalamic intralaminar nuclei, locus coeruleus neurons are immunoreactive for
the hypothalamus, and the insular cortex. Neuroanatomical calcitonin gene-related peptide in mammals (including
studies have shown that this network is notable for its human beings)84,125,138 and express the stress response-
large concentration of calcitonin gene-related peptide related corticotropin-releasing hormone, glucocorticoid,
immunoreactive neurons,84,122–125 which include regions and mineralocorticoid receptors.105 The dorsal raphe
related to visceral, vestibular, and nociceptive pathways nucleus neurons do not show appreciable calcitonin
in the rostrodorsal and caudoventral parabrachial gene-related peptide expression but do express
nucleus,94,95,97,98,100,126–128 several posterior thalamic corticotrophin-releasing hormone and mineralocorticoid
710 www.thelancet.com/neurology Vol 12 July 2013
Review
receptors highly.105 Raphe neurons and their targets also is plausible for lamotrigine, calcium-channel blockers,
express 5-HT1B and 5-HT1D receptors,139,140 which provide and topiramate153 in the attenuation of peripheral trigger
both presynaptic and postsynaptic targets for triptans. susceptibility in vestibular migraine.
Activity of the dorsal raphe nucleus seems to be associated
with the selection of a behavioural strategy to either act or Conclusions and future directions
orient and gather more information. Activation of the Vestibular migraine is becoming recognised as a highly
dorsal raphe nucleus in rats and monkeys accompanies prevalent vestibular disorder that is a subtype of migraine.
facilitated motor activity, inhibited sensory information Recently developed diagnostic criteria have helped clinical
processing, and concomitant expression of hormonal and research, allowing a more complete understanding of the
neuroendocrine activity.141 During orienting responses, clinical aspects of vestibular migraine. The challenge now
reduced activity of these neurons occurs in conjunction is to better understand the pathophysiology of vestibular
with motor activity disfacilitation and sensory processing migraine from both a clinical and basic science
disinhibition. Hence, the interplay between the locus perspective to enable improved rational management of
coeruleus and dorsal raphe nucleus might modulate this disorder. Recent studies of vestibular psychophysics154
perceptual and trigger-related activity in migraine circuits. and motion sickness susceptibility155–157 in vestibular
migraine are yielding exciting new insights. An expanded
Cav2.1 channels and the sodium–potassium ATPase α2 view of the migraine circuit motivates basic science
subunit studies of the individual and interactive roles of vestibular
In view of the many components of the migraine and and nociceptive mechanisms in vestibular migraine. For
vestibular migraine circuits, it is not surprising that example, studies of the role of inner ear trigeminovascular
identification of one major susceptibility locus has been reflexes in blood flow regulation, endolymph-perilymph
elusive in genetic linkage studies.30,31 However, some homoeostasis, vestibular transduction, and vestibular
candidate mutations from family association studies affect nerve function are needed to develop rules for
molecules in the inner ear (peripheral trigger mechanisms) understanding the different effects of drugs on the
and the brain. For example, functional mutations of a vestibular symptoms and headache. Additionally, basic
neuronal voltage-gated calcium channel (Cav2.1) in studies are needed to elucidate neuronal processing
familial hemiplegic migraine type 1 and the glial catalytic interactions between nociceptive and vestibular
α2 subunit of sodium–potassium ATPase (NaKA α2) in information processing, interactions of nociceptive and
familial hemiplegic migraine type 2 have been discussed vestibular processing with stress-related receptor
in the framework of neuron-glial-vascular contributions mechanisms—eg, arginine vasopressin, corticotrophin-
(neurovascular unit142,143) to cortical spreading depression.144 releasing hormone, glucocorticoid and mineralocorticoid
However, the Cav2.1 (P/Q type) channels have many receptors105 in migraine circuits—and the effects of
potential roles in vestibular migraine. Experiments in antimigraine medications on vestibular nerve and
animals show that these channels are mediators of the vestibular nucleus activity. Finally, in view of the parallel
trigeminovascular reflex145 and they can modulate neurochemical organisation of pain and vestibular
transmission at dural trigeminocervical afferent relays in pathways, it will be fruitful to investigate the common
the spinal cord.146 Additionally, Cav2.1 channels help genetic bases for vestibular migraine, craniofacial pain158
regulate calcitonin gene-related peptide release from and interactions between stress and pain,159 including
neuronal processes in the dura, trigeminal ganglion, and pharmacogenetic features that might affect drug
the spinal trigeminal nucleus.147 The same effect is likely efficacy.160 These studies will provide essential new
in the inner ear trigeminovascular terminals. Other knowledge to guide controlled treatment trials for
mutations of Cav2.1 are associated with vertigo in episodic vestibular migraine.
ataxia type 5 (CACNB4 mutation) or vertigo plus migraine
in episodic ataxia type 2 (CACNA1A mutation).30 Reduced
otolithocular function is also associated with CACNA1A Search strategy and selection criteria
mutations in patients with episodic ataxia type 2 and We searched Medline for articles in English published
spinocerebellar ataxia type 6.30 The trigeminal ganglion,148 between Jan 1, 1980, and Dec 31, 2012, with the search
vestibular ganglion,149 and spiral ganglion150 express Cav2.1 words: “migraine”, “dizziness”, “vertigo”, “vestibular”,
mRNA in rodents, suggesting that mutations can “balance”, and “headache”. Terms were expanded using the
potentially affect both the fifth and eighth cranial nerves. ‘exp’ (explode) function and the Boolean ‘AND’ function was
Immunoreactivity for NaKA α2, on the other hand, is used to select subsets. Studies of human beings and animals
associated with fibrocytes below vestibular sensory were included. Both original research and review articles were
epithelia and in the cochlea.72,151 Hence, the antimigraine included. Additional citations were obtained by searching for
actions of the butterbur root sesquiterpenes S-petasin, iso- additional articles by first authors of articles identified
S-petasin, and eudesmol might show preferential actions through the primary search and by reviewing citation lists
as use-dependent antagonists of the Cav2.1 channel152 in within retrieved papers.
vestibular ganglion cells. A similar mechanism of action
www.thelancet.com/neurology Vol 12 July 2013 711
Review
Contributors 27 Teggi R, Colombo B, Bernasconi L, Bellini C, Comi G, Bussi M.
All authors contributed equally in literature searches, writing, and Migrainous vertigo: results of caloric testing and stabilometric
creation of figures. findings. Headache 2009; 49: 435–44.
28 Boldingh MI, Ljostad U, Mygland A, Monstad P. Vestibular
Conflicts of interest sensitivity in vestibular migraine: VEMPs and motion sickness
We declare that we have no conflicts of interest. susceptibility. Cephalalgia 2011; 31: 1211–19.
References 29 Baier B, Stieber N, Dieterich M. Vestibular-evoked myogenic
1 Basser L. Benign paroxysmal vertigo of childhood. Brain 1964; potentials in vestibular migraine. J Neurol 2009; 256: 1447–54.
87: 141–52. 30 Jen JC. Recent advances in the genetics of recurrent vertigo and
2 Kayan A, Hood JD. Neuro-otological manifestations of migraine. vestibulopathy. Curr Opin Neurol 2008; 21: 3–7.
Brain 1984; 107: 1123–42. 31 von Brevern M, Ta N, Shankar A, et al. Migrainous vertigo:
3 Lempert T, Olesen J, Furman J, et al. Vestibular migraine: mutation analysis of the candidate genes CACNA1A, ATP1A2,
diagnostic criteria. J Vestib Res 2012; 22: 167–72. SCN1A, and CACNB4. Headache 2006; 46: 1136–41.
4 Kaniecki RG. Basilar-type migraine. Curr Pain Headache Rep 2009; 32 Lee H, Sininger L, Jen JC, Cha YH, Baloh RW, Nelson SF.
13: 217–20. Association of progesterone receptor with migraine-associated
5 Sturzenegger MH, Meienberg O. Basilar artery migraine: a vertigo. Neurogenetics 2007; 8: 195–200.
follow-up study of 82 cases. Headache 1985; 25: 408–15. 33 Bahmad F Jr, DePalma SR, Merchant SN, et al. Locus for familial
6 Kirchmann M, Thomsen LL, Olesen J. Basilar-type migraine: migrainous vertigo disease maps to chromosome 5q35.
clinical, epidemiologic, and genetic features. Neurology 2006; Ann Otol Rhinol Laryngol 2009; 118: 670–76.
66: 880–86. 34 Murdin L, Davies RA, Bronstein AM. Vertigo as a migraine trigger.
7 Eggers SD. Migraine-related vertigo: diagnosis and treatment. Neurology 2009; 73: 638–42.
Curr Pain Headache Rep 2007; 11: 217–26. 35 Radtke A, Lempert T, Gresty MA, Brookes GB, Bronstein AM,
8 Neuhauser H, Leopold M, von Brevern M, Arnold G, Lempert T. Neuhauser H. Migraine and Meniere’s disease: is there a link?
The interrelations of migraine, vertigo, and migrainous vertigo. Neurology 2002; 59: 1700–04.
Neurology 2001; 56: 436–41. 36 Shepard NT. Differentiation of Meniere’s disease and migraine-
9 Neuhauser HK, Lempert T. Vertigo: epidemiologic aspects. associated dizziness: a review. J Am Acad Audiol 2006; 17: 69–80.
Semin Neurol 2009; 29: 473–81. 37 Cha YH, Kane MJ, Baloh RW. Familial clustering of migraine,
10 Radtke A, Neuhauser H, von Brevern M, Hottenrott T, Lempert T. episodic vertigo, and Meniere’s disease. Otol Neurotol 2008;
Vestibular migraine—validity of clinical diagnostic criteria. 29: 93–96.
Cephalalgia 2011; 31: 906–13. 38 Ishiyama A, Jacobson KM, Baloh RW. Migraine and benign
11 Neuhauser H, Lempert T. Vestibular migraine. Neurol Clin 2009; positional vertigo. Ann Otol Rhinol Laryngol 2000; 109: 377–80.
27: 379–91. 39 Lempert T, Leopold M, von Brevern M, Neuhauser H. Migraine and
12 Cohen JM, Bigal ME, Newman LC. Migraine and vestibular benign positional vertigo. Ann Otol Rhinol Laryngol 2000; 109: 1176.
symptoms—identifying clinical features that predict “vestibular 40 Eckhardt-Henn A, Best C, Bense S, et al. Psychiatric comorbidity in
migraine”. Headache 2011; 51: 1393–97. different organic vertigo syndromes. J Neurol. 2008; 255: 420–28.
13 Millen SJ, Schnurr CM, Schnurr BB. Vestibular migraine: perspectives 41 Furman JM, Balaban CD, Jacob RG, Marcus DA. Migraine-anxiety
of otology versus neurology. Otol Neurotol 2011; 32: 330–37. related dizziness (MARD): a new disorder?
14 Cherchi M, Hain TC. Migraine-associated vertigo. J Neurol Neurosurg Psychiatry 2005; 76: 1–8.
Otolaryngol Clin North Am 2011; 44: 367–75. 42 Best C, Eckhardt-Henn A, Tschan R, Dieterich M. Psychiatric
15 Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and morbidity and comorbidity in different vestibular vertigo
vestibular migraine. J Neurol 2009; 256: 333–38. syndromes. Results of a prospective longitudinal study over one
year. J Neurol 2009; 256: 58–65.
16 Neuhauser HK, Radtke A, von Brevern M, et al. Migrainous vertigo:
prevalence and impact on quality of life. Neurology 2006; 43 Best C, Tschan R, Eckhardt-Henn A, Dieterich M. Who is at risk for
67: 1028–33. ongoing dizziness and psychological strain after a vestibular
disorder? Neuroscience 2009; 164: 1579–87.
17 Neuhauser H, Lempert T. Vertigo and dizziness related to migraine:
a diagnostic challenge. Cephalalgia 2004; 24: 83–91. 44 Cuomo-Granston A, Drummond PD. Migraine and motion
sickness: what is the link? Prog Neurobiol 2010; 91: 300–12.
18 Hsu LC, Wang SJ, Fuh JL. Prevalence and impact of migrainous
vertigo in mid-life women: a community-based study. Cephalalgia 45 Jeong SH, Oh SY, Kim HJ, Koo JW, Kim JS. Vestibular dysfunction
2011; 31: 77–83. in migraine: effects of associated vertigo and motion sickness.
J Neurol 2010; 257: 905–12.
19 Park JH, Viirre E. Vestibular migraine may be an important cause
of dizziness/vertigo in perimenopausal period. Med Hypotheses 46 Neuhauser H, Radtke A, Von Brevern M, Lempert T. Zolmitriptan
2010; 75: 409–14. for treatment of migrainous vertigo: a pilot randomized
placebo-controlled trial. Neurology 2003; 60: 882–83.
20 Salhofer S, Lieba-Samal D, Freydl E, Bartl S, Wiest G, Wober C.
Migraine and vertigo: a prospective diary study. Cephalalgia 2010; 47 Whitney SL, Wrisley DM, Brown KE, Furman JM. Physical therapy
30: 821–28. for migraine-related vestibulopathy and vestibular dysfunction with
history of migraine. Laryngoscope 2000; 110: 1528–34.
21 von Brevern M, Zeise D, Neuhauser H, Clarke AH, Lempert T.
Acute migrainous vertigo: clinical and oculographic findings. Brain 48 Maione A. Migraine-related vertigo: diagnostic criteria and
2005; 128: 365–74. prophylactic treatment. Laryngoscope 2006; 116: 1782–86.
22 von Brevern M, Radtke A, Clarke AH, Lempert T. Migrainous 49 Fotuhi M, Glaun B, Quan SY, Sofare T. Vestibular migraine: a
vertigo presenting as episodic positional vertigo. Neurology 2004; critical review of treatment trials. J Neurol 2009; 256: 711–16.
62: 469–72. 50 Bisdorff AR. Management of vestibular migraine.
23 Polensek SH, Tusa RJ. Nystagmus during attacks of vestibular Ther Adv Neurol Disord 2011; 4: 183–91.
migraine: an aid in diagnosis. Audiol Neurootol 2009; 15: 241–46. 51 Baier B, Winkenwerder E, Dieterich M. “Vestibular migraine”:
24 Casani AP, Sellari-Franceschini S, Napolitano A, Muscatello L, effects of prophylactic therapy with various drugs. A retrospective
Dallan I. Otoneurologic dysfunctions in migraine patients with or study. J Neurol 2009; 256: 436–42.
without vertigo. Otol Neurotol 2009; 30: 961–67. 52 Goadsby PJ, Lipton RB, Ferrari MD. Migraine: current
25 Cass SP, Furman JM, Ankerstjerne K, Balaban C, Yetiser S, understanding and treatment. N Engl J Med 2002; 346: 257–70.
Aydogan B. Migraine-related vestibulopathy. 53 Ho TW, Edvinsson L, Goadsby PJ. CGRP and its receptors provide
Ann Otol Rhinol Laryngol 1997; 106: 182–89. new insights into migraine pathophysiology. Nat Rev Neurol 2010;
26 Celebisoy N, Gokcay F, Sirin H, Bicak N. Migrainous vertigo: 6: 573–82.
clinical, oculographic and posturographic findings. Cephalalgia 54 Moskowitz MA. Neurogenic inflammation in the pathophysiology
2008; 28: 72–77. and treatment of migraine. Neurology 1993; 43: 16–20.
712 www.thelancet.com/neurology Vol 12 July 2013
Review
55 Moskowitz MA. Pathophysiology of headache—past and present. 80 Denuelle M, Fabre N, Payoux P, Chollet F, Geraud G. Hypothalamic
Headache 2007; 47 (suppl 1): 58–63. activation in spontaneous migraine attacks. Headache 2007;
56 Pietrobon D, Striessnig J. Neurobiology of migraine. 47: 1418–26.
Nat Rev Neurosci 2003; 4: 386–98. 81 Stankewitz A, May A. Increased limbic and brainstem activity
57 May A, Goadsby PJ. The trigeminovascular system in humans: during migraine attacks following olfactory stimulation. Neurology
pathophysiologic implications for primary headache syndromes of 2011; 77: 476–82.
the neural influences on the cerebral circulation. 82 Mainero C, Boshyan J, Hadjikhani N. Altered functional magnetic
J Cereb Blood Flow Metab 1999; 19: 115–27. resonance imaging resting-state connectivity in periaqueductal gray
58 Iadecola C. From CSD to headache: a long and winding road. networks in migraine. Ann Neurol 2011; 70: 838–45.
Nat Med 2002; 8: 110–12. 83 Skofitsch G, Jacobowitz DM. Calcitonin gene-related peptide:
59 Balaban CD, Jacob RG, Furman JM. Neurologic bases for detailed immunohistochemical distribution in the central nervous
comorbidity of balance disorders, anxiety disorders and migraine: system. Peptides 1985; 6: 721–45.
neurotherapeutic implications. Expert Rev Neurother 2011; 11: 379–94. 84 de Lacalle S, Saper CB. Calcitonin gene-related peptide-like
60 Balaban CD. Migraine, vertigo and migrainous vertigo: links between immunoreactivity marks putative visceral sensory pathways in
vestibular and pain mechanisms. J Vestib Res 2011; 21: 315–21. human brain. Neuroscience 2000; 100: 115–30.
61 Balaban CD, Thayer JF. Neurological bases for balance-anxiety 85 Kawai Y, Takami K, Shiosaka S, et al. Topographic localization of
links. J Anxiety Disord 2001; 15: 53–79. calcitonin gene-related peptide in the rat brain: an
62 Vass Z, Dai CF, Steyger PS, Jancso G, Trune DR, Nuttall AL. immunohistochemical analysis. Neuroscience 1985; 15: 747–63.
Co-localization of the vanilloid capsaicin receptor and substance P 86 Takahashi K, Mouri T, Sone M, et al. Calcitonin gene-related
in sensory nerve fibers innervating cochlear and vertebro-basilar peptide in the human hypothalamus. Endocrinol Jpn 1989;
arteries. Neuroscience 2004; 124: 919–27. 36: 409–15.
63 Vass Z, Shore SE, Nuttall AL, Miller JM. Direct evidence of 87 Dieterich M, Brandt T. Functional brain imaging of peripheral and
trigeminal innervation of the cochlear blood vessels. Neuroscience central vestibular disorders. Brain 2008; 131: 2538–52.
1998; 84: 559–67. 88 Suzuki M, Kitano H, Ito R, et al. Cortical and subcortical vestibular
64 Koo JW, Balaban CD. Serotonin-induced plasma extravasation in response to caloric stimulation detected by functional magnetic
the murine inner ear: possible mechanism of migraine-associated resonance imaging. Brain Res Cogn Brain Res 2001; 12: 441–49.
inner ear dysfunction. Cephalalgia 2006; 26: 1310–19. 89 Bucher SF, Dieterich M, Wiesmann M, et al. Cerebral functional
65 Vass Z, Steyger PS, Hordichok AJ, Trune DR, Jancso G, Nuttall AL. magnetic resonance imaging of vestibular, auditory, and nociceptive
Capsaicin stimulation of the cochlea and electric stimulation of the areas during galvanic stimulation. Ann Neurol 1998; 44: 120–25.
trigeminal ganglion mediate vascular permeability in cochlear and 90 Lobel E, Kleine JF, Bihan DL, Leroy-Willig A, Berthoz A. Functional
vertebro-basilar arteries: a potential cause of inner ear dysfunction MRI of galvanic vestibular stimulation. J Neurophysiol 1998;
in headache. Neuroscience 2001; 103: 189–201. 80: 2699–2709.
66 Smith D, Hill RG, Edvinsson L, Longmore J. An immunocytochemical 91 Fasold O, von Brevern M, Kuhberg M, et al. Human vestibular
investigation of human trigeminal nucleus caudalis: CGRP, substance cortex as identified with caloric stimulation in functional magnetic
P and 5-HT1D-receptor immunoreactivities are expressed by resonance imaging. Neuroimage 2002; 17: 1384–93.
trigeminal sensory fibres. Cephalalgia 2002; 22: 424–31. 92 Emri M, Kisely M, Lengyel Z, et al. Cortical projection of peripheral
67 Burgio DL, Hazra AS, Komjathy DA, Quirk WS. Guinea pig vestibular signaling. J Neurophysiol 2003; 89: 2639–46.
vestibular blood flow in response to calcitonin-gene related peptide. 93 Eickhoff SB, Weiss PH, Amunts K, Fink GR, Zilles K. Identifying
Acta Otolaryngol 1997; 117: 819–24. human parieto-insular vestibular cortex using fMRI and
68 Herzog M, Scherer EQ, Albrecht B, Rorabaugh B, Scofield MA, cytoarchitectonic mapping. Hum Brain Mapp 2006; 27: 611–21.
Wangemann P. CGRP receptors in the gerbil spiral modiolar artery 94 Bernard JF, Bester H, Besson JM. Involvement of the
mediate a sustained vasodilation via a transient cAMP-mediated spino-parabrachio -amygdaloid and -hypothalamic pathways in the
Ca2+-decrease. J Membr Biol 2002; 189: 225–36. autonomic and affective emotional aspects of pain. Prog Brain Res
69 Quirk WS, Seidman MD, Laurikainen EA, Nuttall AL, Miller JM. 1996; 107: 243–255.
Influence of calcitonin-gene related peptide on cochlear blood flow 95 Feil K, Herbert H. Topographic organization of spinal and
and electrophysiology. Am J Otol 1994; 15: 56–60. trigeminal somatosensory pathways to the rat parabrachial and
70 Scherer EQ, Herzog M, Wangemann P. Endothelin-1-induced Kolliker-Fuse nuclei. J Comp Neurol 1995; 353: 506–28.
vasospasms of spiral modiolar artery are mediated by rho-kinase- 96 Jasmin L, Burkey AR, Card JP, Basbaum AI. Transneuronal labeling
induced Ca(2+) sensitization of contractile apparatus and reversed of a nociceptive pathway, the spino-(trigemino-)parabrachio-
by calcitonin gene-related Peptide. Stroke 2002; 33: 2965–71. amygdaloid, in the rat. J Neurosci 1997; 17: 3751–65.
71 Lim DJ, Karabinas C, Trune DR. Histochemical localization of 97 Balaban CD. Vestibular nucleus projections to the parabrachial
carbonic anhydrase in the inner ear. Am J Otolaryngol 1983; nucleus in rabbits: implications for vestibular influences on the
4: 33–42. autonomic nervous system. Exp Brain Res 1996; 108: 367–81.
72 Spicer SS, Schulte BA, Adams JC. Immunolocalization of 98 Balaban CD, McGee DM, Zhou J, Scudder CA. Responses of
Na+,K(+)-ATPase and carbonic anhydrase in the gerbil’s vestibular primate caudal parabrachial nucleus and Kolliker-fuse nucleus
system. Hear Res 1990; 43: 205–17. neurons to whole body rotation. J Neurophysiol 2002; 88: 3175–93.
73 Tfelt-Hansen P, De Vries P, Saxena PR. Triptans in migraine: 99 McCandless CH, Balaban CD. Parabrachial nucleus neuronal
a comparative review of pharmacology, pharmacokinetics and responses to off-vertical axis rotation in macaques. Exp Brain Res
efficacy. Drugs 2000; 60: 1259–87. 2010; 202: 271–90.
74 Ahn SK, Balaban CD. Distribution of 5-HT1B and 5-HT1D 100 Porter JD, Balaban CD. Connections between the vestibular nuclei
receptors in the inner ear. Brain Res 2010; 1346: 92–101. and brain stem regions that mediate autonomic function in the rat.
75 Ferrari A, Tiraferri I, Neri L, Sternieri E. Why pharmacokinetic J Vestib Res 1997; 7: 63–76.
differences among oral triptans have little clinical importance: a 101 Drummond PD. Motion sickness and migraine: optokinetic
comment. J Headache Pain 2011; 12: 5–12. stimulation increases scalp tenderness, pain sensitivity in the
76 Goadsby PJ. The vascular theory of migraine—a great story wrecked fingers and photophobia. Cephalalgia 2002; 22: 117–24.
by the facts. Brain 2009; 132: 6–7. 102 Drummond PD. Triggers of motion sickness in migraine sufferers.
77 Sauro KM, Becker WJ. The stress and migraine interaction. Headache 2005; 45: 653–56.
Headache 2009; 49: 1378–86. 103 Drummond PD, Granston A. Facial pain increases nausea and
78 Stankewitz A, Aderjan D, Eippert F, May A. Trigeminal nociceptive headache during motion sickness in migraine sufferers. Brain 2004;
transmission in migraineurs predicts migraine attacks. J Neurosci 127: 526–34.
2011; 31: 1937–43. 104 Marano E, Marcelli V, Di Stasio E, et al. Trigeminal stimulation
79 Alstadhaug KB. Migraine and the hypothalamus. Cephalalgia 2009; elicits a peripheral vestibular imbalance in migraine patients.
29: 809–17. Headache 2005; 45: 325–31.
www.thelancet.com/neurology Vol 12 July 2013 713
Review
105 Joels M, Baram TZ. The neuro-symphony of stress. 127 Cechetto DF, Standaert DG, Saper CB. Spinal and trigeminal dorsal
Nat Rev Neurosci 2009; 10: 459–66. horn projections to the parabrachial nucleus in the
106 Marcus DA, Furman JM, Balaban CD. Motion sickness in migraine rat. J Comp Neurol 1985; 240: 153–60.
sufferers. Expert Opin Pharmacother 2005; 6: 2691–97. 128 Saxon DW, Hopkins DA. Efferent and collateral organization of
107 Balaban C, Yates BJ. Vestibulo-autonomic interactions: a teleologic paratrigeminal nucleus projections: an anterograde and retrograde
perspective. In: Highstein SN, Fay RR, Popper AN, eds. Springer fluorescent tracer study in the rat. J Comp Neurol 1998; 402: 93–110.
handbook of auditory research: the vestibular system. New York: 129 Shiroyama T, Kayahara T, Yasui Y, Nomura J, Nakano K. Projections
Springer-Verlag, 2004: 286–342. of the vestibular nuclei to the thalamus in the rat: a Phaseolus
108 Holstein GR, Friedrich VL Jr, Kang T, Kukielka E, Martinelli GP. vulgaris leucoagglutinin study. J Comp Neurol 1999; 407: 318–32.
Direct projections from the caudal vestibular nuclei to the 130 Cuccurazzu B, Halberstadt AL. Projections from the vestibular
ventrolateral medulla in the rat. Neuroscience 2011; 175: 104–17. nuclei and nucleus prepositus hypoglossi to dorsal raphe nucleus in
109 Ito M. The cerebellum and neural control. New York: Raven Press, rats. Neurosci Lett 2008; 439: 70–74.
1984. 131 Halberstadt AL, Balaban CD. Organization of projections from the
110 Afridi SK, Giffin NJ, Kaube H, et al. A positron emission raphe nuclei to the vestibular nuclei in rats. Neuroscience 2003;
tomographic study in spontaneous migraine. Arch Neurol 2005; 120: 573–94.
62: 1270–75. 132 Halberstadt AL, Balaban CD. Serotonergic and nonserotonergic
111 Afridi SK, Matharu MS, Lee L, et al. A PET study exploring the neurons in the dorsal raphe nucleus send collateralized projections
laterality of brainstem activation in migraine using glyceryl to both the vestibular nuclei and the central amygdaloid nucleus.
trinitrate. Brain 2005; 128: 932–39. Neuroscience 2006; 140: 1067–77.
112 Edvinsson L, Eftekhari S, Salvatore CA, Warfvinge K. Cerebellar 133 Halberstadt AL, Balaban CD. Anterograde tracing of projections
distribution of calcitonin gene-related peptide (CGRP) and its from the dorsal raphe nucleus to the vestibular nuclei. Neuroscience
receptor components calcitonin receptor-like receptor (CLR) and 2006; 143: 641–54.
receptor activity modifying protein 1 (RAMP1) in rat. 134 Schuerger RJ, Balaban CD. Organization of the coeruleo-vestibular
Mol Cell Neurosci 2011; 46: 333–39. pathway in rats, rabbits, and monkeys. Brain Res Rev 1999; 30: 189–217.
113 Buisseret-Delmas C, Compoint C, Delfini C, Buisseret P. 135 Aston-Jones G, Chiang C, Alexinsky T. Discharge of noradrenergic
Organisation of reciprocal connections between trigeminal and locus coeruleus neurons in behaving rats and monkeys suggests a
vestibular nuclei in the rat. J Comp Neurol 1999; 409: 153–68. role in vigilance. Prog Brain Res 1991; 88: 501–20.
114 Diagne M, Valla J, Delfini C, Buisseret-Delmas C, Buisseret P. 136 Foote SL, Berridge CW, Adams LM, Pineda JA. Electrophysiological
Trigeminovestibular and trigeminospinal pathways in rats: evidence for the involvement of the locus coeruleus in alerting,
retrograde tracing compared with glutamic acid decarboxylase and orienting, and attending. Prog Brain Res 1991; 88: 521–32.
glutamate immunohistochemistry. J Comp Neurol 2006; 137 Bremner JD, Krystal JH, Southwick SM, Charney DS.
496: 759–72. Noradrenergic mechanisms in stress and anxiety: I. Preclinical
115 Menetrey D, Basbaum AI. Spinal and trigeminal projections to the studies. Synapse 1996; 23: 28–38.
nucleus of the solitary tract: a possible substrate for somatovisceral 138 Tiller-Borcich JK, Capili H, Gordan GS. Human brain calcitonin
and viscerovisceral reflex activation. J Comp Neurol 1987; gene-related peptide (CGRP) is concentrated in the locus caeruleus.
255: 439–50. Neuropeptides 1988; 11: 55–61.
116 Balaban CD, Beryozkin G. Vestibular nucleus projections to 139 Sari Y. Serotonin 1B receptors: from protein to physiological
nucleus tractus solitarius and the dorsal motor nucleus of the vagus function and behavior. Neurosci Biobehav Rev 2004; 28: 565–82.
nerve: potential substrates for vestibulo-autonomic interactions. 140 Sari Y, Miquel MC, Brisorgueil MJ, et al. Cellular and subcellular
Exp Brain Res 1994; 98: 200–12. localization of 5-hydroxytryptamine1B receptors in the rat central
117 Yates BJ, Grelot L, Kerman IA, Balaban CD, Jakus J, Miller AD. nervous system: immunocytochemical, autoradiographic and lesion
Organization of vestibular inputs to nucleus tractus solitarius and studies. Neuroscience 1999; 88: 899–915.
adjacent structures in cat brain stem. Am J Physiol 1994; 267: 974–83. 141 Jacobs BL, Fornal CA. 5-HT and motor control: a hypothesis.
118 Bankoul S, Goto T, Yates B, Wilson VJ. Cervical primary afferent Trends Neurosci 1993; 16: 346–52.
input to vestibulospinal neurons projecting to the cervical dorsal 142 Hawkins BT, Davis TP. The blood-brain barrier/neurovascular unit
horn: an anterograde and retrograde tracing study in the cat. in health and disease. Pharmacol Rev 2005; 57: 173–85.
J Comp Neurol 1995; 353: 529–38.
143 Lecrux C, Hamel E. The neurovascular unit in brain function and
119 Neuhuber WL, Zenker W. Central distribution of cervical primary disease. Acta Physiol (Oxf) 2011; 203: 47–59.
afferents in the rat, with emphasis on proprioceptive projections to
144 Moskowitz MA, Bolay H, Dalkara T. Deciphering migraine
vestibular, perihypoglossal, and upper thoracic spinal nuclei.
mechanisms: clues from familial hemiplegic migraine genotypes.
J Comp Neurol 1989; 280: 231–53.
Ann Neurol 2004; 55: 276–80.
120 Craig AD. How do you feel? Interoception: the sense of the
145 Akerman S, Williamson DJ, Goadsby PJ. Voltage-dependent
physiological condition of the body. Nat Rev Neurosci 2002;
calcium channels are involved in neurogenic dural vasodilatation
3: 655–66.
via a presynaptic transmitter release mechanism. Br J Pharmacol
121 Craig AD. How do you feel–now? The anterior insula and human 2003; 140: 558–66.
awareness. Nat Rev Neurosci 2009; 10: 59–70.
146 Shields KG, Storer RJ, Akerman S, Goadsby PJ. Calcium channels
122 Kruger L, Sternini C, Brecha NC, Mantyh PW. Distribution of modulate nociceptive transmission in the trigeminal nucleus of the
calcitonin gene-related peptide immunoreactivity in relation to the cat. Neuroscience 2005; 135: 203–12.
rat central somatosensory projection. J Comp Neurol 1988;
147 Amrutkar DV, Ploug KB, Olesen J, Jansen-Olesen I. Role for voltage
273: 149–62.
gated calcium channels in calcitonin gene-related peptide release in
123 Kruger L, Mantyh PW, Sternini C, Brecha NC, Mantyh CR. the rat trigeminovascular system. Neuroscience 2011; 172: 510–17.
Calcitonin gene-related peptide (CGRP) in the rat central nervous
148 Pietrobon D. Insights into migraine mechanisms and CaV2.1
system: patterns of immunoreactivity and receptor binding sites.
calcium channel function from mouse models of familial
Brain Res 1988; 463: 223–44.
hemiplegic migraine. J Physiol 2010; 588: 1871–78.
124 Yasui Y, Saper CB, Cechetto DF. Calcitonin gene-related peptide
149 Eatock RA, Xue J, Kalluri R. Ion channels in mammalian vestibular
immunoreactivity in the visceral sensory cortex, thalamus, and
afferents may set regularity of firing. J Exp Biol 2008; 211: 1764–74.
related pathways in the rat. J Comp Neurol 1989; 290: 487–501.
150 Chen WC, Xue HZ, Hsu YL, Liu Q, Patel S, Davis RL. Complex
125 Tajti J, Uddman R, Edvinsson L. Neuropeptide localization in the
distribution patterns of voltage-gated calcium channel alpha-
“migraine generator” region of the human brainstem. Cephalalgia
subunits in the spiral ganglion. Hear Res 2011; 278: 52–68.
2001; 21: 96–101.
151 Peters TA, Kuijpers W, Curfs JH. Occurrence of NaK-ATPase
126 Balaban CD. Projections from the parabrachial nucleus to the
isoforms during rat inner ear development and functional
vestibular nuclei: potential substrates for autonomic and limbic
implications. Eur Arch Otorhinolaryngol 2001; 258: 67–73.
influences on vestibular responses. Brain Res 2004; 996: 126–37.
714 www.thelancet.com/neurology Vol 12 July 2013
Review
152 Horak S, Koschak A, Stuppner H, Striessnig J. Use-dependent 157 Furman JM, Marcus DA, Balaban CD. Rizatriptan reduces
block of voltage-gated Cav2.1 Ca2+ channels by petasins and vestibular-induced motion sickness in migraineurs. J Headache Pain
eudesmol isomers. J Pharmacol Exp Ther 2009; 330: 220–26. 2011; 12: 81–88.
153 Shank RP, Maryanoff BE. Molecular pharmacodynamics, clinical 158 Fillingim RB, Wallace MR, Herbstman DM, Ribeiro-Dasilva M,
therapeutics, and pharmacokinetics of topiramate. Staud R. Genetic contributions to pain: a review of findings in
CNS Neurosci Ther 2008; 14: 120–42. humans. Oral Dis 2008; 14: 673–82.
154 Lewis RF, Priesol AJ, Nicoucar K, Lim K, Merfeld DM. Abnormal 159 Mogil JS, Sorge RE, LaCroix-Fralish ML, et al. Pain sensitivity and
motion perception in vestibular migraine. Laryngoscope 2011; vasopressin analgesia are mediated by a gene-sex-environment
121: 1124–25. interaction. Nat Neurosci 2011; 14: 1569–73.
155 Marcus DA, Furman JM. Prevention of motion sickness with 160 Chan A, Pirmohamed M, Comabella M. Pharmacogenomics in
rizatriptan: a double-blind, placebo-controlled pilot study. neurology: current state and future steps. Ann Neurol 2011;
Med Sci Monit 2006; 12: 1–7. 70: 684–97.
156 Furman JM, Marcus DA. A pilot study of rizatriptan and visually-
induced motion sickness in migraineurs. Int J Med Sci 2009;
6: 212–17.
www.thelancet.com/neurology Vol 12 July 2013 715
You might also like
- FDARDocument33 pagesFDARRaquel M. Mendoza100% (7)
- Science 9 Q1 Module 1 Respiratory and Circulatory With Key AnswerDocument42 pagesScience 9 Q1 Module 1 Respiratory and Circulatory With Key AnswerJan Ice90% (128)
- New England Journal of Medicine Volume 383 Issue 19 2020 (Doi 10.1056 - NEJMra1915327) Ropper, Allan H. Ashina, Messoud - MigraineDocument11 pagesNew England Journal of Medicine Volume 383 Issue 19 2020 (Doi 10.1056 - NEJMra1915327) Ropper, Allan H. Ashina, Messoud - MigraineMarija Sekretarjova100% (1)
- L95 NecropsyDocument7 pagesL95 NecropsyKING 5 News100% (1)
- Journal of Neurology Volume 256 Issue 3 2009 (Doi 10.1007/s00415-009-0149-2) T. Lempert H. Neuhauser - Epidemiology of Vertigo, Migraine and Vestibular MigraineDocument6 pagesJournal of Neurology Volume 256 Issue 3 2009 (Doi 10.1007/s00415-009-0149-2) T. Lempert H. Neuhauser - Epidemiology of Vertigo, Migraine and Vestibular MigraineDevi Arnes SimanjuntakNo ratings yet
- Migraine Associated Vertigo Review Highlights Link Between ConditionsDocument6 pagesMigraine Associated Vertigo Review Highlights Link Between ConditionsnoraNo ratings yet
- Migraña Vestibular Actualizacion-BaranyDocument6 pagesMigraña Vestibular Actualizacion-Baranyjuanm.maciasNo ratings yet
- Migraine Pathophysiology Advances Implications for Clinical ManagementDocument9 pagesMigraine Pathophysiology Advances Implications for Clinical ManagementAzam alausyNo ratings yet
- 2016 Epidemiologia Da Migrânea VestibularDocument6 pages2016 Epidemiologia Da Migrânea VestibularGloria CantoNo ratings yet
- Vestibular Migraine Episodic VertigoDocument9 pagesVestibular Migraine Episodic VertigoDanielNo ratings yet
- Charles 2017Document9 pagesCharles 2017Aldebaran LadoNo ratings yet
- The Migraine Syndrome in Children 2022 Paediatrics and Child HealthDocument6 pagesThe Migraine Syndrome in Children 2022 Paediatrics and Child HealthEduardo Rios DuboisNo ratings yet
- Mikulec Faraji Kinsella. Evaluation of The Efficacy of Caffeine Cessation, Nortriptyline, and Topiramate Therapy in Vestibular Migraine and Complex Dizziness of Unknown Etiology .Document7 pagesMikulec Faraji Kinsella. Evaluation of The Efficacy of Caffeine Cessation, Nortriptyline, and Topiramate Therapy in Vestibular Migraine and Complex Dizziness of Unknown Etiology .HelderSouzaNo ratings yet
- Challenges for Epidemiological Research on Vertigo and DizzinessDocument6 pagesChallenges for Epidemiological Research on Vertigo and DizzinessKim AntelNo ratings yet
- Contents 2019 Neurologic-ClinicsDocument4 pagesContents 2019 Neurologic-ClinicsAghie vlogNo ratings yet
- Interdisciplinary Care Improves Outcomes for Headache PatientsDocument14 pagesInterdisciplinary Care Improves Outcomes for Headache PatientsareteusNo ratings yet
- Karsan2018 Premonitory SymptomsDocument12 pagesKarsan2018 Premonitory SymptomsPAULINA OSPINA BARRIENTOSNo ratings yet
- Artigo InsoniaDocument9 pagesArtigo InsoniaLaizyCoelhoNo ratings yet
- Egurgel 2007 - Dizzines Associates With Panic Disorder and AgoraphobiaDocument4 pagesEgurgel 2007 - Dizzines Associates With Panic Disorder and AgoraphobiaJuan Hernández GarcíaNo ratings yet
- Guidelines VertigoDocument16 pagesGuidelines VertigoririnNo ratings yet
- Gadingzhr, ARTIKEL 7Document6 pagesGadingzhr, ARTIKEL 7NqbilNo ratings yet
- Involucrar A Los Pacientes en El TratamientoDocument5 pagesInvolucrar A Los Pacientes en El TratamientoluciaNo ratings yet
- Anxiety, Mood, and Personality Disorders in Patients With Benign Paroxysmal Positional VertigoDocument5 pagesAnxiety, Mood, and Personality Disorders in Patients With Benign Paroxysmal Positional VertigoOkim NawarNo ratings yet
- The Natural History of Epilepsy: An Epidemiological View: ReviewDocument6 pagesThe Natural History of Epilepsy: An Epidemiological View: ReviewDiana LeonNo ratings yet
- Kapfhammer 1997 PPV Vs AgorafobiaDocument6 pagesKapfhammer 1997 PPV Vs AgorafobiaJuan Hernández GarcíaNo ratings yet
- Review of Vestibular Migraine: Current Understanding and Future DirectionsDocument15 pagesReview of Vestibular Migraine: Current Understanding and Future DirectionsSerdar MeteNo ratings yet
- Flunarizine Effective Migrainous Vertigo PreventionDocument6 pagesFlunarizine Effective Migrainous Vertigo PreventionNanda WtNo ratings yet
- Initial Evaluation VertigoDocument8 pagesInitial Evaluation VertigoTanri Hadinata WiranegaraNo ratings yet
- Vestibular MigraineDocument8 pagesVestibular MigraineYayatRuslanNo ratings yet
- Chronic Fatigue Syndrome From Chronic Fatigue To More Specific SyndromesDocument5 pagesChronic Fatigue Syndrome From Chronic Fatigue To More Specific SyndromesArgenis SalinasNo ratings yet
- Evaluation and Management of The Dizzy PatientDocument9 pagesEvaluation and Management of The Dizzy Patientsara mohamedNo ratings yet
- Behavsci 12 00065 v2Document8 pagesBehavsci 12 00065 v2Dina Saka IINo ratings yet
- Episodic Migraine (S Nahas, Section Editor)Document8 pagesEpisodic Migraine (S Nahas, Section Editor)Loida CamargoNo ratings yet
- Dizziness 1 PDFDocument7 pagesDizziness 1 PDFShruthi IyengarNo ratings yet
- BPPV LabuguenDocument8 pagesBPPV LabuguenMuhammad Furqon FahlulyNo ratings yet
- Chronic Migraine Pathophysiology and Treatment: A Review of Current PerspectivesDocument15 pagesChronic Migraine Pathophysiology and Treatment: A Review of Current PerspectivesJorge ZegarraNo ratings yet
- Is This Just A: Headache?Document6 pagesIs This Just A: Headache?agirl_9807No ratings yet
- Medscape NeurologyDocument54 pagesMedscape NeurologyShannon RamsumairNo ratings yet
- Ioi80105 2118 2124Document8 pagesIoi80105 2118 2124AlishaNo ratings yet
- Migrain TreatmentDocument10 pagesMigrain TreatmentveNo ratings yet
- Facts and Myths Pertaining To FibromyalgiaDocument11 pagesFacts and Myths Pertaining To FibromyalgiaZélia TeixeiraNo ratings yet
- Benign Paroxysmal Vertigo of ChildhoodDocument6 pagesBenign Paroxysmal Vertigo of ChildhoodWhilliamharveyNo ratings yet
- Nej MR A 1915327Document11 pagesNej MR A 1915327Noel Saúl Argüello SánchezNo ratings yet
- 2019 - 08 - 05 Essential TremorDocument16 pages2019 - 08 - 05 Essential TremorstaseaditNo ratings yet
- Vertigo and Dizziness in ChildrenDocument5 pagesVertigo and Dizziness in ChildrenPablo Antonio AntonioNo ratings yet
- Migraine Headaceh Treated With FamciclovirDocument2 pagesMigraine Headaceh Treated With FamciclovirReani ZulfaNo ratings yet
- Maju Jurnal MigrainDocument7 pagesMaju Jurnal MigrainRosyid PrasetyoNo ratings yet
- Chronic Insomnia: Matt T. Bianchi, MD, PHDDocument6 pagesChronic Insomnia: Matt T. Bianchi, MD, PHDAlex BorroelNo ratings yet
- Baldwin2014 PDFDocument12 pagesBaldwin2014 PDFSamuel Bayona MendozaNo ratings yet
- Pato Insomnia PDFDocument14 pagesPato Insomnia PDFdilaNo ratings yet
- Clinical Research: Facts and Myths Pertaining To FibromyalgiaDocument10 pagesClinical Research: Facts and Myths Pertaining To FibromyalgiaArief HidayatNo ratings yet
- Causes of Migraine PDFDocument7 pagesCauses of Migraine PDFJohn Christopher LucesNo ratings yet
- The Spectrum of Vestibular MigraineDocument14 pagesThe Spectrum of Vestibular MigraineRudolfGerNo ratings yet
- BMJ l4485 FullDocument16 pagesBMJ l4485 FullJennifer AlmeidaNo ratings yet
- Headache - Seminars in NeurologyDocument7 pagesHeadache - Seminars in NeurologyandreaNo ratings yet
- Review of Migraine Pathophysiology, Diagnosis, and ManagementDocument6 pagesReview of Migraine Pathophysiology, Diagnosis, and ManagementNurul Fadilah SariNo ratings yet
- Neuropalliative Care: A Practical Guide For The Neurologist: K. Brizzi, MD C. J. Creutzfeldt, MDDocument7 pagesNeuropalliative Care: A Practical Guide For The Neurologist: K. Brizzi, MD C. J. Creutzfeldt, MDjumabarrientosNo ratings yet
- Migraine Review Article: April 2017Document6 pagesMigraine Review Article: April 2017Ahmad BaihaqiNo ratings yet
- Chest 147 4 1179Document14 pagesChest 147 4 1179Albert TandyNo ratings yet
- Rana2013 2Document14 pagesRana2013 2Shaun TylerNo ratings yet
- 5ch Izoph Ren Ia: Key ConceptsDocument24 pages5ch Izoph Ren Ia: Key ConceptsNAURA ARNEITA AN-NAJLANo ratings yet
- Egurgel 2007 - Dizzines Associates With Panic Disorder and AgoraphobiaDocument4 pagesEgurgel 2007 - Dizzines Associates With Panic Disorder and AgoraphobiaJuan Hernández GarcíaNo ratings yet
- Vertigo 2 PDFDocument7 pagesVertigo 2 PDFyolan ariyanaNo ratings yet
- Mast 2014 Spactial Cognition Body Representation and Affective ProcessesDocument15 pagesMast 2014 Spactial Cognition Body Representation and Affective ProcessesJuan Hernández GarcíaNo ratings yet
- Space and Motion Discomfort Questionnaire ValidityDocument26 pagesSpace and Motion Discomfort Questionnaire ValidityJuan Hernández GarcíaNo ratings yet
- Sansone 2009 Panic Disorder Subtypes - Deceptive Somatic ImpersonatorsDocument5 pagesSansone 2009 Panic Disorder Subtypes - Deceptive Somatic ImpersonatorsJuan Hernández GarcíaNo ratings yet
- Furman 2014 MARDDocument10 pagesFurman 2014 MARDJuan Hernández GarcíaNo ratings yet
- Furman - 2007 Vestibo Ocular Function in Anxiety DisordersDocument8 pagesFurman - 2007 Vestibo Ocular Function in Anxiety DisordersJuan Hernández GarcíaNo ratings yet
- Carmeli 2015 Anxiety in The Elderly Can Be A Vestibular ProblemDocument2 pagesCarmeli 2015 Anxiety in The Elderly Can Be A Vestibular ProblemJuan Hernández GarcíaNo ratings yet
- Kolev 2014 Anxiety Changes DespersonalizationDocument10 pagesKolev 2014 Anxiety Changes DespersonalizationJuan Hernández GarcíaNo ratings yet
- Balaban 2011Document16 pagesBalaban 2011Juan Hernández GarcíaNo ratings yet
- Jacob 2001 Psychiatric Consequences of Vestibular DysfunctionDocument6 pagesJacob 2001 Psychiatric Consequences of Vestibular DysfunctionJuan Hernández GarcíaNo ratings yet
- Nagaratnam - 2004 Vestibular Dysfunction and Anxiety Disorder Interface - ElderlyDocument13 pagesNagaratnam - 2004 Vestibular Dysfunction and Anxiety Disorder Interface - ElderlyJuan Hernández GarcíaNo ratings yet
- Tecer 2004 Audiovestibular Functioning in Patients With Panic DisorderDocument6 pagesTecer 2004 Audiovestibular Functioning in Patients With Panic DisorderJuan Hernández GarcíaNo ratings yet
- Emotional Aspects of Vestibular Disorders - Part2 - 57Document4 pagesEmotional Aspects of Vestibular Disorders - Part2 - 57Juan Hernández GarcíaNo ratings yet
- Pascal 2019 Ooperation of The Vestibular and Cerebellar Networks in Anxiety Disorders and DepressionDocument56 pagesPascal 2019 Ooperation of The Vestibular and Cerebellar Networks in Anxiety Disorders and DepressionJuan Hernández GarcíaNo ratings yet
- Hoffman 1994Document11 pagesHoffman 1994Juan Hernández GarcíaNo ratings yet
- Frank 1984 The Boulder ModelDocument19 pagesFrank 1984 The Boulder ModelJuan Hernández GarcíaNo ratings yet
- Brandt and Dieterich 2020 Excess Anxiety' and Less Anxiety' Both Depend o 1Document6 pagesBrandt and Dieterich 2020 Excess Anxiety' and Less Anxiety' Both Depend o 1Juan Hernández GarcíaNo ratings yet
- Yardley 1995Document5 pagesYardley 1995Juan Hernández GarcíaNo ratings yet
- Medicine as Social Political Science in Spain c. 1920Document16 pagesMedicine as Social Political Science in Spain c. 1920Juan Hernández GarcíaNo ratings yet
- Amiaz 2021 Responses To Balance Challenges in Persons With Panic Disorder A Pilot Study ofDocument12 pagesAmiaz 2021 Responses To Balance Challenges in Persons With Panic Disorder A Pilot Study ofJuan Hernández GarcíaNo ratings yet
- (2006-04) Moynihan, R. y Henry, D. - The Fight Against Disease Mongering Generating Knowledge For ActionDocument4 pages(2006-04) Moynihan, R. y Henry, D. - The Fight Against Disease Mongering Generating Knowledge For ActionCarlos IslasNo ratings yet
- The History of Clinical PsychologyDocument33 pagesThe History of Clinical PsychologyJuan Hernández GarcíaNo ratings yet
- Function and Training of The Clinical PsychologistDocument17 pagesFunction and Training of The Clinical PsychologistJuan Hernández GarcíaNo ratings yet
- El Sector Inmobiliario en España - Evolución y AnálisisDocument26 pagesEl Sector Inmobiliario en España - Evolución y AnálisisJuan Hernández GarcíaNo ratings yet
- The Liberal Temper in Greek Politics - HavelockDocument452 pagesThe Liberal Temper in Greek Politics - HavelockJuan Hernández GarcíaNo ratings yet
- ProQuestDocuments 2023-01-23Document11 pagesProQuestDocuments 2023-01-23Juan Hernández GarcíaNo ratings yet
- Kapfhammer 1997 PPV Vs AgorafobiaDocument6 pagesKapfhammer 1997 PPV Vs AgorafobiaJuan Hernández GarcíaNo ratings yet
- Bation 2016 Transcranial Direct Current Stimulation in Treatment Resistant OCDDocument5 pagesBation 2016 Transcranial Direct Current Stimulation in Treatment Resistant OCDJuan Hernández GarcíaNo ratings yet
- Pharmacology MnemonicsDocument17 pagesPharmacology MnemonicsKrizzia SuñerNo ratings yet
- Finasteride in Men With BPHDocument3 pagesFinasteride in Men With BPHmonia agni wiyatamiNo ratings yet
- @MBS MedicalBooksStore 2020 HeadDocument238 pages@MBS MedicalBooksStore 2020 HeadtamiNo ratings yet
- Reca Op Claim Form 12-11-0Document25 pagesReca Op Claim Form 12-11-0Ehren OertellNo ratings yet
- Midwifery Pharmacology-7Document1 pageMidwifery Pharmacology-7georgeloto12No ratings yet
- Probe Guide: Logiq P9 and LOGIQ P7Document3 pagesProbe Guide: Logiq P9 and LOGIQ P7Shantanu Mandal100% (1)
- Thyroid DiseasesDocument44 pagesThyroid DiseasesPLDT HOMENo ratings yet
- Il Gem 4000 Operating and Maintenance ProcedureDocument15 pagesIl Gem 4000 Operating and Maintenance ProcedureHfsh OmerNo ratings yet
- LIOFeron®TB-LTBI EN Tube-IDocument4 pagesLIOFeron®TB-LTBI EN Tube-ITuấn Minh PhùngNo ratings yet
- Skills Fair Agenda 2014Document3 pagesSkills Fair Agenda 2014api-211571782No ratings yet
- Hereditary SpherocytosisDocument39 pagesHereditary SpherocytosisjoannaNo ratings yet
- Wheezing From PCODocument23 pagesWheezing From PCOShan KaiNo ratings yet
- 4th Annual Pediatric Echocardiography Review BrochureDocument4 pages4th Annual Pediatric Echocardiography Review Brochuremadimadi11No ratings yet
- Approach To Unknown Drug OverdoseDocument3 pagesApproach To Unknown Drug OverdoseRobert So JrNo ratings yet
- Physical Health and Mental HealthDocument2 pagesPhysical Health and Mental HealthLuise MauieNo ratings yet
- Current U.S. Military Fluid Replacement GuidelinesDocument6 pagesCurrent U.S. Military Fluid Replacement Guidelines"Rufus"No ratings yet
- Questions from the Ministry of Health for Residency and Fellowship Programs (2013-2018Document68 pagesQuestions from the Ministry of Health for Residency and Fellowship Programs (2013-2018Ahmad HamdanNo ratings yet
- DiabetesDocument170 pagesDiabetesKoRnflakesNo ratings yet
- Antenatal CareDocument12 pagesAntenatal CarefiramnNo ratings yet
- Gordon's 11 Functional Health PatternDocument2 pagesGordon's 11 Functional Health PatternWendell AcuñaNo ratings yet
- Effects of Hypoxia on Health ConditionsDocument36 pagesEffects of Hypoxia on Health ConditionsVeres András100% (2)
- Nursing Care PlanDocument10 pagesNursing Care PlanSittie Rohaina SabanNo ratings yet
- Tennis Elbow Bill 2015 PDFDocument8 pagesTennis Elbow Bill 2015 PDFDiegoKosiakNo ratings yet
- Guide to Neurology ClerkshipDocument63 pagesGuide to Neurology ClerkshipShane AllenNo ratings yet
- Handling Wounded in Counter-Guerrilla Wars: Soviet/Russian Lessons from Afghanistan and ChechnyaDocument8 pagesHandling Wounded in Counter-Guerrilla Wars: Soviet/Russian Lessons from Afghanistan and ChechnyaMarco TulioNo ratings yet
- Pathologt of The HeartDocument40 pagesPathologt of The HeartJudithNo ratings yet
- Deep Fungal InfectionsDocument33 pagesDeep Fungal Infectionstummalapalli venkateswara raoNo ratings yet