Professional Documents
Culture Documents
Cva Concept Map
Cva Concept Map
Uploaded by
Ann Justine OrbetaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cva Concept Map
Cva Concept Map
Uploaded by
Ann Justine OrbetaCopyright:
Available Formats
CEREBROVASCULAR ACCIDENT (STROKE)
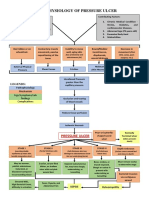
LEGEND PATHOPHYSIOLOGY
Predisposing Factors
Hemorrhagic Stroke
Ischemic stroke
Common path
Clinical Manifestations
Diagnostic Studies
Therapeutic Management
Past history of Transient Ischemic Attack
Nursing Management
Atherosclerosis
NON-MODIFIABLE MODIFIABLE
Hypertension, Diabetes mellitus, Hypertension
age, gender, ethnicity or race,
increase cholesterol, obesity, excessive
and family history or heredity.
alcohol, inflammation,birth control pills
PREDISPOSING FACTORS
thrombus or circulating debris
cerebral aneurysm
Injury to a blood vessel
Thrombosis Emboli Rupture of a blood vessel
partial or complete occlusion of Bleeding into the the cerebrospinal
narrowing of the lumen Bleeding into the brain tissue
a blood vessel fluid?filled space
Hematoma
Ineffective and insufficient cerebral blood flow
blocks the passage
Increased pressure
Anaerobic respiration
Loss of function
Thrombotic Stroke Embolic Stroke Subarachnoid Hemorrhage
Intracerebral Hemorrhage
Infarction
ISCHEM IC STROKE HEM ORRHAGIC STROKE
CLINICAL MANIFESTATIONS
Motor Function Communication Affect Intellectual Function Spatial-Perceptual Alterations Elimination
impairment of mobility, difficulty controlling impaired memory and 4 categories: incorrect perception
aphasia, of self and illness; neglects all frequency, urgency,
respiratory function, emotions- may be exaggerated judgment ; difficulty making
dysphasia, input from the affected side; incontinence, and constipation
swallowing and speech, gag or unpredictable; depression, generalizations, which
dysarthria, agnosia, and apraxia,
reflex, and self-care abilities. frustration interferes with ability to learn.
DIAGNOSTIC STUDIES N U R S I N G M A N A G E M E N T
Diagnosis of Stroke
(Including Extent of Involvement) ASSESSMENT CARE PLAN
- Computed tomography (CT)scan Primary assessment Decreased intracranial adaptive capacity r/t decreased cerebral
- CT angiography (CTA) (1) description of the current illness with attention to initial S/S perfusion pressure
- Magnetic resonance imaging(MRI) (onset and duration, nature -intermittent or continuous,)
- Magnetic resonance angiography (MRA) (2) history of similar symptoms previously experienced; Independent
- CT/MRI perfusion and diffusion imaging (3) current medications Cerebral Perfusion Promotion
(4) history of risk factors
Cerebral Blood Flow (5) family history of CVA - Consult with physician to determine hemodynamic parameters, and
- Cerebral angiography maintain hemodynamic parameters within this range.
- Carotid angiography Secondary assessment - Monitor neurologic status.
- Digital subtraction angiography Acomprehensive neurologic examination guided with NIHSS - Calculate and monitor cerebral perfusion pressure.
- Transcranial Doppler ultrasonography (1) level of consciousness, - Monitor respiratory status (e.g., rate, rhythm, and depth of
- Carotid duplex scanning (2) cognition respirations; PaO2, PaCO2, pH, and bicarbonate levels)
(3) motor abilities - Monitor patient?s ICP and neurologic responses to care.
Cardiac Assessment 4) cranial nerve function - Monitor determinants of tissue oxygen delivery (e.g., PaCO2, SaO2,
- Electrocardiogram (5) sensation hemoglobin levels, and cardiac output)
- Chest x-ray (6) proprioception; - Avoid neck flexion or extreme hip or knee flexion to avoid obstruction
1
- Cardiac markers (troponin, (7) cerebellar function of arterial and venous blood flow.
creatine kinase-MB) 8) deep tendon reflexes.
- Echocardiography Dependent
(transthoracic, ransesophageal) - Administer and titrate vasoactive drugs
Typical Findings
General -lethargy, apathy or combativeness, fever
Respiratory - Loss of cough reflex, labored or irregular respirations,
Risk for aspiration r/t decreased level of consciousness and
THERAPEUTIC MANAGEMENT tachypnea, aspiration, airway occlusion (tongue), apnea
decreased or absent gag and swallowing reflexes
Cardiovascular - Hypertension, tachycardia, carotid bruit
Drug Therapy Aspiration Precautions
Gastrointestinal - Loss of gag reflex, bowel incontinence, decreased
- Platelet inhibitors (e.g., aspirin) - Monitor LOC cough-gag reflex, and swallowing ability.
- Anticoagulation therapy for patients or absent bowel sounds, constipation - Avoid liquids or use thickening agent to facilitate swallowing.
with atrial fibrillation Urinary - Frequency, urgency, incontinence - Feed in small amounts until patient is no longer at risk for aspiration.
- Offer foods/ liquids that can be formed into a bolus before swallowing.
Neurologic - Contralateral motor and sensory deficits, paresis,
Surgical Therapy
- Carotid endarterectomy paralysis, anesthesia; unequal pupils, akinesia, aphasia, dysarthria Airway Management
- Stenting of carotid artery (slurred speech), agnosias, apraxia, visual deficits, perceptual or - Auscultate breath sounds, noting areas of decreased or absent
- Transluminal angioplasty spatial disturbances, altered LOC, and Babinski?s sign?, ? deep ventilation and presence of adventitious sounds
2
- Extracranial-intracranial bypass tendon reflexes, flaccidity, spasticity, amnesia, ataxia, personality - Remove secretions by encouraging coughing or by suctioning.
- Surgical interventions for change, nuchal rigidity, seizures. - Encourage slow, deep breathing; turning; and coughing.
aneurysms at risk of bleeding - Assist with incentive spirometer.
Possible Diagnostic Findings - Positive CT, CTA, MRI, MRA, or - Keep patient NPO until swallow evaluation completed.
other neuroimaging scans showing size, location, and type of lesion;
positive Doppler ultrasonography and angiography indicating stenosis
Impaired physical mobility r/t neuromuscular and cognitive
impairment and decreased muscle strength and control
HEALTH PROMOTION General Intervention
Exercise Therapy: Muscle Control
- Health teaching (healthy lifestyle, balanced diet) - Collaborate with physical, occupational, and recreational
- Involved in BP screening, stroke risk screening. therapists in developing and executing exercise program
- Ensuring that patients adhere to medications (antihypertensive, - Determine patient?s readiness to engage in activity or exercise
anticoagulants etc.) protocol
- Inform patients and families about early symptoms associated with - Apply splints to achieve stability of proximal joints involved with
stroke or be guided with the FAST acronym. fine motor skills to prevent contractures.
- Encourage patient to practice exercises independently.
- Reinforce instructions provided to patient about the proper way
3
to perform exercises.
- Provide restful environment for patient after periods of exercise
Acronym ?FAST? helps to detect common S/S to facilitate recuperation.
Face: Does one side of the face droop?
Arm: If a person holds both arms out, does one drift downward?
Speech: Is their speech abnormal or slurred?
Time: Time to call 911 if any of these symptoms are present. Impaired verbal communication r/t aphasia as evidenced by
refusal or inability to speak, difficulty forming words and
inappropriate verbalization
Communication Enhancement: Speech Deficit
- Listen attentively to convey the importance of patient?s thoughts
and to promote a positive environment for learning.
4
- Provide positive reinforcement and praise.
- Use simple words and short sentences.
- Perform prescriptive speech-language therapies.
- Provide verbal prompts and reminders.
Impaired urinary elimination related to impaired impulse to void
or manage tasks of voiding as evidenced by loss of urinary
control
Urinary Habit Training
- Keep a continence specification record.
- Establish interval of initial toileting schedule.
- Assist patient to toilet and prompt to void at prescribed intervals.
- Teach patient to consciously hold urine until the scheduled toileting
time.
5
- Discuss daily record of continence with staff and encourage
compliance with toileting schedule.
- Give positive feedback or positive reinforcement to patient when he
or she voids at scheduled toileting times.
Situational low self-esteem related to actual or perceived loss of
function and altered body image
Self-Esteem Enhancement
- Monitor patient?s statements of self-worth to determine effect of
stroke on self-esteem.
- Encourage patient to identify strengths.
6
- Assist in setting realistic goals.
- Reward or praise patient?s progress toward reaching goals.
- Encourage increased responsibility for self.
- Monitor levels of self-esteem over time.
You might also like
- Concept Map Worksheet Mary Richards Heart Failure Jasgou1752Document3 pagesConcept Map Worksheet Mary Richards Heart Failure Jasgou1752Jasmyn Rose100% (1)
- VSIM Clinical Worksheet 07.16.2020Document6 pagesVSIM Clinical Worksheet 07.16.2020Jackie GriffisNo ratings yet
- Hypertension Pathophysiology and Treatment PDFDocument6 pagesHypertension Pathophysiology and Treatment PDFBella TogasNo ratings yet
- NCP CvaDocument4 pagesNCP CvaMariquita BuenafeNo ratings yet
- Stroke PathoDocument15 pagesStroke PathoWiljohn de la CruzNo ratings yet
- Concept Map AAADocument6 pagesConcept Map AAASandrine BarredoNo ratings yet
- Pathophysiology AHS HTN EDocument1 pagePathophysiology AHS HTN Erod navalesNo ratings yet
- Schematic Diag DMDocument1 pageSchematic Diag DMReynaKatNo ratings yet
- Diabetes PathoDocument2 pagesDiabetes Pathodrewcel100% (1)
- Schematic Diagram Pathophysiology (Book-Based) COPD and TuberculosisDocument1 pageSchematic Diagram Pathophysiology (Book-Based) COPD and Tuberculosispragna novaNo ratings yet
- Schematic Diagram: Signs and Symptoms: Headache, Unconsciousness, Nausea and Vomiting, Visual DisturbancesDocument3 pagesSchematic Diagram: Signs and Symptoms: Headache, Unconsciousness, Nausea and Vomiting, Visual DisturbancesJosett RomanoNo ratings yet
- Acute Rheumatic Fever PathophysiologyDocument1 pageAcute Rheumatic Fever PathophysiologyMoonyeen Jann Casera BalicNo ratings yet
- Schistosomiasis (From Anatomy To Pathophysiology)Document10 pagesSchistosomiasis (From Anatomy To Pathophysiology)Tiger Knee100% (1)
- Cues Nursing Diagnosis Background Knowledge Goals and Objectives Nursing Interventions and Rationale Evaluation Subjective: NOC: Swallowing Status Goal: NIC: SwallowingDocument10 pagesCues Nursing Diagnosis Background Knowledge Goals and Objectives Nursing Interventions and Rationale Evaluation Subjective: NOC: Swallowing Status Goal: NIC: SwallowingSkyla FiestaNo ratings yet
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Client Centered PathophysiologyDocument3 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Client Centered PathophysiologyCarl Elexer Cuyugan Ano50% (2)
- ESRD PathophysiologyDocument2 pagesESRD Pathophysiologynursing concept mapsNo ratings yet
- Open I Tibia Fibula (R) Lacerated Wounded Leg: Our Lady of Fatima UniversityDocument21 pagesOpen I Tibia Fibula (R) Lacerated Wounded Leg: Our Lady of Fatima UniversityPOTENCIANA MAROMANo ratings yet
- PPPDocument3 pagesPPPJack BangcoyoNo ratings yet
- CASE STUDY PheumoniaDocument5 pagesCASE STUDY PheumoniaEdelweiss Marie CayetanoNo ratings yet
- 4th Yr. Med Cardio Module Question - Copy-1Document11 pages4th Yr. Med Cardio Module Question - Copy-1Sheda BondNo ratings yet
- NCP OsteosarcomaDocument6 pagesNCP OsteosarcomaNiksNo ratings yet
- A Subdural HematomaDocument12 pagesA Subdural HematomaGina Irene IshakNo ratings yet
- Annotated Group 2 Impetigo Concept Mapping 1Document30 pagesAnnotated Group 2 Impetigo Concept Mapping 1DHANE ANN CAMPOSANONo ratings yet
- Pathophysiology HeadinjuryDocument1 pagePathophysiology HeadinjuryK.b. Dequiña100% (1)
- Pathophysiology Diagram of Congestive Heart FailureDocument3 pagesPathophysiology Diagram of Congestive Heart FailureLeng Royo BrionesNo ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- Tatz Pa ToolDocument23 pagesTatz Pa Toolian_mendoza_3No ratings yet
- Pathophysiology of Pressure UlcersDocument1 pagePathophysiology of Pressure UlcersSTORAGE FILENo ratings yet
- Pathophysiology-Kni Ns PLZZZDocument8 pagesPathophysiology-Kni Ns PLZZZAnna Lira Manluyang MungcalNo ratings yet
- Cerebrovascular DiseaseDocument4 pagesCerebrovascular DiseasekathyfacaNo ratings yet
- DB13 - Pathophysiology of AtherosclerosisDocument2 pagesDB13 - Pathophysiology of Atherosclerosisi_vhie03No ratings yet
- HPN Patopisyo!Document1 pageHPN Patopisyo!Raprap TristanNo ratings yet
- NCP 2 CabalunaDocument7 pagesNCP 2 CabalunaIrene Grace BalcuevaNo ratings yet
- Multiple Sclerosis PDFDocument1 pageMultiple Sclerosis PDFAcey TfNo ratings yet
- Communicating Pathophysiology: Impaired Absorption of The CSF in The Arachnoid SpaceDocument2 pagesCommunicating Pathophysiology: Impaired Absorption of The CSF in The Arachnoid SpaceAyaBasilioNo ratings yet
- Cva PathoDocument2 pagesCva Pathokriska_ortizNo ratings yet
- Cerebrovascular Disease (Emphasis On CVA)Document29 pagesCerebrovascular Disease (Emphasis On CVA)OlynsieMorrisNo ratings yet
- CVA PathophysiologyDocument3 pagesCVA Pathophysiologyshmily_0810No ratings yet
- NCP CKDDocument3 pagesNCP CKDRiel TumandaNo ratings yet
- V. Pathophysiology Modifiable: Non - ModifiableDocument2 pagesV. Pathophysiology Modifiable: Non - ModifiableMary Grace BanezNo ratings yet
- Cerebrovascular Disease (Bleed)Document25 pagesCerebrovascular Disease (Bleed)Margaret Jenaw JenawNo ratings yet
- Age Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat IntakeDocument3 pagesAge Greater Than 60 Y/o Hereditary Precipitating Factors: Hypertension Increase Protein and Fat Intakenursing concept mapsNo ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPRomel BaliliNo ratings yet
- Acute Head InjuryDocument5 pagesAcute Head InjuryRitesh KumarNo ratings yet
- Pathophysiology of Pressure UlcerDocument1 pagePathophysiology of Pressure UlcerSTORAGE FILENo ratings yet
- Pathophysiology of Hypertension, Diabetes, Ubm, BPHDocument3 pagesPathophysiology of Hypertension, Diabetes, Ubm, BPHCarly Beth Caparida LangerasNo ratings yet
- Traumatic Brain Injury PathophysiologyDocument2 pagesTraumatic Brain Injury PathophysiologyJane VargasNo ratings yet
- Assess For Signs of HyperglycemiaDocument9 pagesAssess For Signs of HyperglycemiaSheril Sularte CasanesNo ratings yet
- Angina Pectoris PathophysiologyDocument2 pagesAngina Pectoris PathophysiologyALIANA KIMBERLY MALQUESTONo ratings yet
- Introduction - MIDocument10 pagesIntroduction - MIkhimiiiNo ratings yet
- PathophysiologyDocument1 pagePathophysiologyHazel PalomaresNo ratings yet
- Case Study 1 FinalDocument28 pagesCase Study 1 Finalapi-3905968320% (1)
- Hypertensive Cardiovascular DiseaseDocument5 pagesHypertensive Cardiovascular DiseaseAna Katrina OcanaNo ratings yet
- Ineffective Tissue Perfusion PDFDocument4 pagesIneffective Tissue Perfusion PDFgcodouganNo ratings yet
- BSN4D-SG2 DM Type2Document201 pagesBSN4D-SG2 DM Type2Charisse CaydanNo ratings yet
- Tuberculous MeningitisDocument23 pagesTuberculous MeningitisAsma KhmNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument3 pagesAssessment Diagnosis Planning Implementation Rationale EvaluationHanz AlecNo ratings yet
- Nursing Care Plan On Platelet DisordersDocument8 pagesNursing Care Plan On Platelet DisordersbhavanaNo ratings yet
- Disseminated Intravascular CoagulationDocument1 pageDisseminated Intravascular CoagulationAnn Justine OrbetaNo ratings yet
- Physrev 00004 2019Document57 pagesPhysrev 00004 2019Ann Justine OrbetaNo ratings yet
- Maternal, Child Health Prog-Part 1Document25 pagesMaternal, Child Health Prog-Part 1Ann Justine OrbetaNo ratings yet
- NCM 32 LAB A1 Lesson 1 NotesDocument14 pagesNCM 32 LAB A1 Lesson 1 NotesAnn Justine OrbetaNo ratings yet
- Maternal, Child Health Prog-Part 2Document23 pagesMaternal, Child Health Prog-Part 2Ann Justine OrbetaNo ratings yet
- Town and Country Lovers by Nadine GordimerDocument2 pagesTown and Country Lovers by Nadine GordimerAnn Justine OrbetaNo ratings yet
- 2 RJ Town and Country LoversDocument1 page2 RJ Town and Country LoversAnn Justine OrbetaNo ratings yet
- Urine AnalysisDocument9 pagesUrine AnalysisAnn Justine OrbetaNo ratings yet
- Short Story Response 2 Town and Country Lovers 1 2Document3 pagesShort Story Response 2 Town and Country Lovers 1 2Ann Justine OrbetaNo ratings yet