Professional Documents
Culture Documents
Subjective: CASE 1. STEVE ROGERS (7 Columns)
Uploaded by
Marc PeraltaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Subjective: CASE 1. STEVE ROGERS (7 Columns)
Uploaded by
Marc PeraltaCopyright:
Available Formats
Steve Rogers, an 80-year-old man, was taken to the hospital by his daughter who
stated that her father was
weak, vomited four times, and has pain in his belly. She is also informed that his appetite is poor and he is very
anxious. On assessment of the client, he is lethargic, states his pain is a 9 on a scale of 1-10. He vomited three
times, 100 milliliters each of greenish fluid, and passed approximately 150 milliliters of urine in the urinal. His
temperature is 38.2 C, pulse 80bpm, respiration 22cpm and blood pressure 140/80 mmHg.
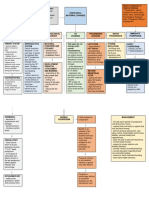
CASE 1. STEVE ROGERS (7 columns)
CUES Nursing Background Planning Interventions Rationale Evaluation
Diagnosis knowledge
Subjective: Risk for Fluid volume Short term: 1.Monitor 1.Fluid loss After 24 hours
“She stated that deficient fluid deficit (also After of 24 active fluid loss from diarrhea patient have
her father felt volume related known as hours nursing from wound and/or achieved the
weak and has to process of hypovolemia) intervention the diarrhea and/or vomiting cause equal of intake
pain in his belly” ageing as describes the patient will vomiting; decreased fluid and output of
as verbalized by manifested by loss of have equal maintain volume and can fluid and his
the relative. patient extracellular intake and accurate input lead to appetite return
vomiting 100 fluid from the output of fluid and output dehydration. to normal.
ml of greenish body. There are as well his record.
fluids 3 times a number ways appetite will 2.Oral fluid Patient
Objective:
the body can return to 2.Persuade the replacement is demonstrates
BP 140/80mmHg
lose fluid. Some normal. patient to drink indicated for the lifestyle to
RR 22cpm
major causes of prescribed mild fluid changes to
HR 80bpm
deficient fluid Long term: amount of fluid deficit and is a progression of
T 38.2C
volume are Patient will cost-effective dehydration.
Lethargic
through demonstrate method for
3.Educate
gastrointestinal lifestyle replacement
Vomited greenish patient about
system: changes to treatment.
fluids possible cause
vomiting and avoid Older patients
and effect of
diarrhea. This is progression of have a
fluid losses or
particularly an dehydration. decreased sense
decreased fluid
issue with infant of thirst and
intake.
and elderly may need
patients. ongoing
Teach family
reminders to
members and
drink. Oral
patient how to
hydrating
monitor output
solutions (e.g.,
in the home.
Oresol,
Instruct them to
Gatorade) can
monitor both
be considered
intake and
as needed.
output.
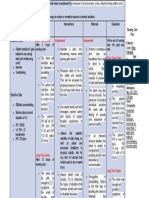
STEVE ROGERS (5 column)
Assessment Diagnosis Planning Intervention evaluation
“She stated her father Acute Pain related to Short term: 1.Teach the use of After 8 hours, patient
has pain in belly and vomiting as After 8 hours of nonpharmacologic vomiting and abdominal
felt very anxious also manifested by patient nursing intervention techniques before, pain has reduced to 4/10
lost his appetite” rating pain 9 on 1-10 patient vomiting and after, and if possible, and his appetite returned to
verbalize by the also scale, active vomiting, abdominal pain will during painful normal.
relative reduce 4/10 as well activities; before pain
his appetite will return occurs or increases; Patient has been feeling
pain scale 9//10 and along with other more energetic than the
Patient will report pain relief measures past 24 hours
feeling less lethargic
within 24 hours. 2.Demonstrate and After 2 days, the patient has
BP 140/80mmHg
practice the relaxation no more pain and afebrile.
RR 22cpm
technique with patient
HR 80bpm
T 38.2 C Long term:
Lethargic After 1-2 days of
Vomited greenish nursing intervention
fluids. patient will be pain
free and afebrile
Scenario: Tony Stark is a 36-y/o police officer assigned to a high crime police precinct. One week ago he received a surface
bullet wound to his arm. Today he arrives at the outpatient clinic to have the wound redressed. While speaking with the nurse,
Mr. Stark mentions that he has been promoted to the rank of detective and has assumed new responsibilities. He states that since
his promotion, he has experienced increasing difficulty falling asleep and sometimes staying asleep. He expresses concern over
the danger of his occupation and his desire to do well in his new position. He complains of waking up feeling tired and irritable.
During interview the nurse notes that he is pale, drawn with dark circles under his eyes. Temp: 37.0 C Pulse: 80 bpm, Resp:
18cpm, BP: 140/90mmHg.
TONY STARK (7 COLUMN)
Assessment N. Diagnosis Background Planning Intervention Rationale Evaluation
Knowledge
Subjective: Anxiety related Generalized After 8 hours - Establish a - To establish After 8 hours
“Since the to threat of anxiety of nursing therapeutic the trust and of nursing
promotion I current status disorder is intervention, relationship, show interest. Intervention,
experienced as evidenced characterized the patient will conveying - To avoid the patient is
difficulties by waking up by excessive feel relaxed empathy and confusions. - feeling better
falling asleep feeling tired worry about a and the level of positive To identify and relaxed
and sometimes and irritable, number of anxiety will regards. physical and reduced
staying asleep” difficulty different reduce and - Acknowledge response. - the level of
as verbalized falling asleep events, decrease in to a anxiety fear. May help the anxiety and
by the patient. and stay associated with manageable - Encourage client relax and feel Easily to
asleep. heightened level. the client to feel better fall asleep.
He also tension. A express
expresses the person with feelings.
danger of his generalized - Monitor Vital
of his anxiety signs
occupation. disorder may - Provide
also feel comfort
irritable and - Instructor
Objective:
have physical assess to deep
T 37.0 C
symptoms such breathing and
HR 80bpm
as restlessness, relaxation.
RR 18cpm
feeling easily
BP
tired and
140/90mmHg
having tense
Pale skin
muscles.
Drawn dark
circles
Tony Stark (5 column)
Assessment N. Diagnosis Planning Intervention Evaluation
Subjective: Hypertension related to Patient will maintain Provide calm, restful Maintained the blood
“He states that since lack of sleep as BP within individually surroundings, and pressure at less than
his promotion, he has manifested by acceptable range. minimize 140/90 mmHg with
experienced increasing 140/90mmHg environmental activity lifestyle modifications,
difficulty falling asleep Patient will participate and noise. medications, or both.
and sometimes staying in activities that will
asleep” prevent stress (stress Instruct in relaxation
management, balanced techniques, guided
activities and rest imagery, and
Objective:
plan). distractions.
T 37.0 C
HR 80bpm Monitor response to
RR 18cpm medications to control
BP 140/90mmHg blood pressure.
Pale skin
Drawn dark circles Provide comfort
measures (back and
neck massage, the
elevation of head).
CASE 1. STEVE ROGERS (7 columns)
CUES Nursing Background Planning Interventions Rationale Evaluation
Diagnosis knowledge
Subjective: Risk for Fluid volume Short term: 1.Monitor 1.Fluid loss After 24 hours
“She stated that deficient fluid deficit (also After of 24 active fluid loss from diarrhea patient have
her father felt volume related known as hours nursing from wound and/or achieved the
weak and has to process of hypovolemia) intervention the diarrhea and/or vomiting cause equal of intake
pain in his belly” ageing as describes the patient will vomiting; decreased fluid and output of
as verbalized by manifested by loss of have equal maintain volume and can fluid and his
the relative. patient extracellular intake and accurate input lead to appetite return
vomiting 100 fluid from the output of fluid and output dehydration. to normal.
ml of greenish body. There are as well his record.
fluids 3 times a number ways appetite will 2.Oral fluid Patient
Objective:
the body can return to 2.Persuade the replacement is demonstrates
BP 140/80mmHg
lose fluid. Some normal. patient to drink indicated for the lifestyle to
RR 22cpm
major causes of prescribed mild fluid changes to
HR 80bpm
deficient fluid Long term: amount of fluid deficit and is a progression of
T 38.2C
volume are Patient will cost-effective dehydration.
Lethargic
through demonstrate method for
3.Educate
gastrointestinal lifestyle replacement
Vomited greenish patient about
system: changes to treatment.
fluids possible cause
vomiting and avoid Older patients
and effect of
diarrhea. This is progression of have a
fluid losses or
particularly an dehydration. decreased sense
decreased fluid
issue with infant of thirst and
intake.
and elderly may need
patients. ongoing
4.Teach family
reminders to
members and
drink. Oral
patient how to
hydrating
monitor output
solutions (e.g.,
in the home.
Oresol,
Instruct them to
Gatorade) can
monitor both
be considered
intake and
as needed.
output.
3.Enough
knowledge aids
the patient to
take part in his
or her plan of
care.
4.An accurate
measure of
fluid intake and
output is an
important
indicator of
patient’s fluid
status.
You might also like
- Nursing Care Plan for Carpal Tunnel SyndromeDocument4 pagesNursing Care Plan for Carpal Tunnel SyndromeKiana OcampoNo ratings yet
- Gordon'S Functional Health PatternDocument10 pagesGordon'S Functional Health PatternDave SapladNo ratings yet
- Edited Readiness For Enhanced NutritionDocument4 pagesEdited Readiness For Enhanced NutritionWappy WepwepNo ratings yet
- Bukidnon State University College of NursingDocument5 pagesBukidnon State University College of NursingAIZA MAE BANGGAY100% (1)
- Malabsorption and Elimination DisordersDocument120 pagesMalabsorption and Elimination DisordersBeBs jai SelasorNo ratings yet
- Chapter 36Document7 pagesChapter 36Mariah Jane TaladuaNo ratings yet
- Artapp 1Document40 pagesArtapp 1Dianne LabisNo ratings yet
- Chapter 38Document22 pagesChapter 38Tito, Stephen Gabriel, A.No ratings yet
- Family Nursing Care Plan: Bicol University Tabaco Campus Nursing DepartmentDocument5 pagesFamily Nursing Care Plan: Bicol University Tabaco Campus Nursing DepartmentCelline Isabelle ReyesNo ratings yet
- "Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientDocument2 pages"Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientMussaib Mushtaq100% (1)
- Analyzing Water Rescue and Response SituationDocument3 pagesAnalyzing Water Rescue and Response SituationDIANE FAE FETALVERONo ratings yet
- DDSTDocument61 pagesDDSTji payNo ratings yet
- Acute Pain Related To Frequent As Evidenced by Pain ScaleDocument3 pagesAcute Pain Related To Frequent As Evidenced by Pain ScaledanaNo ratings yet
- Manuscript-research-Impact With CorrectionsDocument88 pagesManuscript-research-Impact With CorrectionsJay VillasotoNo ratings yet
- Religious Beliefs and PracticesDocument3 pagesReligious Beliefs and PracticesLyndonCabilloNo ratings yet
- IDBDocument2 pagesIDBPaulo PolinagNo ratings yet
- NCM 109 Rle Retdems Rational MidtermsDocument35 pagesNCM 109 Rle Retdems Rational MidtermsemilynbernatNo ratings yet
- Osce WrittenDocument6 pagesOsce WrittenNicole NipasNo ratings yet
- Mga NCP For Preterm Birth Case 2Document9 pagesMga NCP For Preterm Birth Case 2John Rendel LopezNo ratings yet
- Assessing Health Problems in FamiliesDocument5 pagesAssessing Health Problems in FamiliesJerson Jeck Salumanda AlcidoNo ratings yet
- Family Case Study-BibliographyDocument1 pageFamily Case Study-BibliographyKatherine 'Chingboo' Leonico LaudNo ratings yet
- PHYSICAL and FANCAP Assessment FORMAT 1Document1 pagePHYSICAL and FANCAP Assessment FORMAT 1Cheska PalomaNo ratings yet
- Prenatal Care NCPDocument10 pagesPrenatal Care NCPAlex AntipordaNo ratings yet
- Urinary Catheterization RetdemDocument2 pagesUrinary Catheterization RetdemHazel MarananNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation IndependentDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation IndependentAdhaNo ratings yet
- Nursing Care Plan Borderline PD (Client A) NCP #1: Pia Mae D. Buaya N-31Document9 pagesNursing Care Plan Borderline PD (Client A) NCP #1: Pia Mae D. Buaya N-31Pia Mae BuayaNo ratings yet
- Teaching PlanDocument1 pageTeaching PlanUnis OwtwoNo ratings yet
- Completed Teaching Plan To Promote Awareness and Prevention RabiesDocument2 pagesCompleted Teaching Plan To Promote Awareness and Prevention RabiesJm BernardoNo ratings yet
- Case-Scenario-Oxygen Therapy-BuenconsejoDocument6 pagesCase-Scenario-Oxygen Therapy-BuenconsejoCarna BuenconsejoNo ratings yet
- Leptospirosis PamphletDocument2 pagesLeptospirosis PamphletDm KeeNo ratings yet
- Bioethics MidtermsDocument4 pagesBioethics Midtermschanelito rendonNo ratings yet
- Total Population Number of Households A. Family Members and CharacteristicsDocument20 pagesTotal Population Number of Households A. Family Members and CharacteristicsDenvicNo ratings yet
- Pediatric Community Acquired Pneumonia: PresentorsDocument34 pagesPediatric Community Acquired Pneumonia: PresentorsEvelyn MedinaNo ratings yet
- NCP For Parent and Child PDFDocument3 pagesNCP For Parent and Child PDFMariana Mikaela AlagarNo ratings yet
- NCPDocument2 pagesNCPCamille VirayNo ratings yet
- Case Analaysis On infertility-BALLON-Karlo CDocument4 pagesCase Analaysis On infertility-BALLON-Karlo CMelinda Cariño BallonNo ratings yet
- Theory Proposed by Judith Graves and Sheila Corcoran's Model (1989)Document2 pagesTheory Proposed by Judith Graves and Sheila Corcoran's Model (1989)Paul JacksonNo ratings yet
- Cheaper Medicines Act (Revised)Document115 pagesCheaper Medicines Act (Revised)Via H.No ratings yet
- Nursing Care Plan: Lorma Colleges Con Template Related Learning ExperienceDocument4 pagesNursing Care Plan: Lorma Colleges Con Template Related Learning ExperienceMelinda Cariño BallonNo ratings yet
- Cmca Quiz InfancyDocument3 pagesCmca Quiz InfancyEspiritu, ChriscelNo ratings yet
- Socio GramDocument3 pagesSocio GramRomelle Jane M. VelascoNo ratings yet
- Drug Therapeutic Record TemplateDocument1 pageDrug Therapeutic Record TemplateAubrey Justine GaleonNo ratings yet
- Nursing Related Learning Experience ManualDocument11 pagesNursing Related Learning Experience ManualRYAN SAPLADNo ratings yet
- Nutrition and Diet Therapy Menu PlanningDocument51 pagesNutrition and Diet Therapy Menu Planningkaren solibaNo ratings yet
- I. Improper Waste Disposal Actual Scores Justification II. Dog Bites Actual Score JustificationDocument3 pagesI. Improper Waste Disposal Actual Scores Justification II. Dog Bites Actual Score JustificationJanet Ingco San NicolasNo ratings yet
- Now, Try Some Big Leap.: Keep GoingDocument2 pagesNow, Try Some Big Leap.: Keep GoingShyla ManguiatNo ratings yet
- Drug Study AzathioprineDocument3 pagesDrug Study AzathioprineBunnie AlphaNo ratings yet
- Nutrition Care Plan for Severe MalnutritionDocument3 pagesNutrition Care Plan for Severe Malnutritioncharles estradaNo ratings yet
- Post-Op Pain Management Nursing InterventionsDocument4 pagesPost-Op Pain Management Nursing InterventionsAllen Vincent Cauton TulaganNo ratings yet
- Homework 1: Developing A Health Teaching Program 1. What Insights and Reflections Do You Have Based On Your Understanding of The EssentialDocument2 pagesHomework 1: Developing A Health Teaching Program 1. What Insights and Reflections Do You Have Based On Your Understanding of The EssentialRianne BaetiongNo ratings yet
- Concept Map 4Document2 pagesConcept Map 4Daniela Claire FranciscoNo ratings yet
- Physics Lab Report 1Document7 pagesPhysics Lab Report 1Liana BelleNo ratings yet
- Nursing Care PlanDocument1 pageNursing Care PlanMikki lor PuaganNo ratings yet
- LP2 ncm105Document8 pagesLP2 ncm105Margarette GeresNo ratings yet
- CHN 2 Session 3 SASDocument5 pagesCHN 2 Session 3 SASrica sebabillonesNo ratings yet
- FyhffDocument44 pagesFyhffRico Torregosa Jr.No ratings yet
- Nursing Care for a Toddler with Accidental Burn InjuryDocument16 pagesNursing Care for a Toddler with Accidental Burn InjuryJiezl Abellano AfinidadNo ratings yet
- Resource Unit On Common Drugs (LRDR Rotation)Document37 pagesResource Unit On Common Drugs (LRDR Rotation)kiamoiNo ratings yet
- NPR Deficient FluidDocument4 pagesNPR Deficient FluidDj KurtNo ratings yet
- NCP Deficient Fluid VolumeDocument3 pagesNCP Deficient Fluid VolumeDoneva Lyn MedinaNo ratings yet
- JusticeDocument5 pagesJusticeIVERSON ESTILLORENo ratings yet
- Family Health ProfileDocument8 pagesFamily Health ProfileMarc PeraltaNo ratings yet
- Family Health ProfileDocument8 pagesFamily Health ProfileMarc PeraltaNo ratings yet
- 5 Yrs Old BelowDocument8 pages5 Yrs Old BelowMarc PeraltaNo ratings yet
- Introduction Family Case Study HypertensionDocument5 pagesIntroduction Family Case Study HypertensionMarc PeraltaNo ratings yet
- Request to retake midterm exam due to family obligationsDocument1 pageRequest to retake midterm exam due to family obligationsMarc PeraltaNo ratings yet
- Theory of Justice 1Document22 pagesTheory of Justice 1Marc PeraltaNo ratings yet
- 5 Yrs Old BelowDocument8 pages5 Yrs Old BelowMarc PeraltaNo ratings yet
- Finals ActivitytfnDocument1 pageFinals ActivitytfnMarc PeraltaNo ratings yet
- CRWT111 - WEEK 2 - Introduction To Critical ReadingDocument41 pagesCRWT111 - WEEK 2 - Introduction To Critical ReadingMarc PeraltaNo ratings yet
- Phed 214 Week 2-3Document5 pagesPhed 214 Week 2-3Marc PeraltaNo ratings yet
- Genital Care (Male)Document2 pagesGenital Care (Male)Marc PeraltaNo ratings yet
- Family Service Record Details ToothacheDocument8 pagesFamily Service Record Details ToothacheMarc PeraltaNo ratings yet
- BJMP and BuCor Release Procedure AssignmentDocument1 pageBJMP and BuCor Release Procedure AssignmentMarc PeraltaNo ratings yet
- Turn Anxiety Into AdvantageDocument26 pagesTurn Anxiety Into AdvantageIgnacio Andrés Torres NeiraNo ratings yet
- PBL Mental Health Questions - HTRHDocument3 pagesPBL Mental Health Questions - HTRHHellguz ArtNo ratings yet
- Guide assess candidates 49 questionsDocument26 pagesGuide assess candidates 49 questionsMoumita RoyNo ratings yet
- Al G. DavenDocument2 pagesAl G. DaventhecutealNo ratings yet
- Buspirone Hydrochloride (Drug Study)Document2 pagesBuspirone Hydrochloride (Drug Study)Franz.thenurse6888100% (1)
- 01-John Assaraf S M A MindsetDocument11 pages01-John Assaraf S M A MindsetYash SNo ratings yet
- PSYCHIATRIC NURSING PNLE REVIEW (MAY 2022Document9 pagesPSYCHIATRIC NURSING PNLE REVIEW (MAY 2022Justine CagatanNo ratings yet
- Psychological Responses To Injury in SportsDocument7 pagesPsychological Responses To Injury in SportsWasuki UpadhyayaNo ratings yet
- Terrorist NegotiationDocument64 pagesTerrorist NegotiationSherlyn Mendez Irinco0% (2)
- Worked: Prishila MuraDocument9 pagesWorked: Prishila MuraGabriel MuraNo ratings yet
- Negative Effects of Social Media AddictionDocument2 pagesNegative Effects of Social Media AddictionTubagus Fikih AriansyahNo ratings yet
- How To Cope With Toxic RelationshipDocument2 pagesHow To Cope With Toxic Relationshipveky61No ratings yet
- Stress Management ProjectDocument53 pagesStress Management ProjectwestmkingNo ratings yet
- A Guide To Crisis Intervention 5th Edition Kanel Test BankDocument12 pagesA Guide To Crisis Intervention 5th Edition Kanel Test BankChuck Simmons100% (26)
- Client Satisfaction Safety Final HAHAHAAHDocument21 pagesClient Satisfaction Safety Final HAHAHAAHDonna Mae VasquezNo ratings yet
- How To Center Yourself Within 60 SecondsDocument5 pagesHow To Center Yourself Within 60 Secondskabshiel100% (1)
- PDEV 111 Answer 2nd QuarterDocument30 pagesPDEV 111 Answer 2nd QuarterChan-Chan Matamorosa50% (2)
- Nursing Case Study: Psychiatric Mental Health PracticumDocument2 pagesNursing Case Study: Psychiatric Mental Health Practicumleen276781% (31)
- BPRS-C 9item PDFDocument2 pagesBPRS-C 9item PDFPriyashree RoyNo ratings yet
- Psychological Domain - Nursing Care PlanDocument1 pagePsychological Domain - Nursing Care PlanPussykate DollNo ratings yet
- Ted Talk Essay 1Document7 pagesTed Talk Essay 1api-665638494No ratings yet
- ĐỀ THI THỬ SỐ 38-KHÓA 9+ BIÊN SOẠN CÔ PHẠM LIỄUDocument7 pagesĐỀ THI THỬ SỐ 38-KHÓA 9+ BIÊN SOẠN CÔ PHẠM LIỄUMai KateNo ratings yet
- Psychological Disorders: Quick ReviewDocument5 pagesPsychological Disorders: Quick Reviewshah FahadNo ratings yet
- Group Process Term ProjectDocument26 pagesGroup Process Term ProjecthancidiousNo ratings yet
- Social AnxietygtdgnDocument40 pagesSocial AnxietygtdgnRanjit MoreNo ratings yet
- Anxiety Disorder - DSM 5Document57 pagesAnxiety Disorder - DSM 5Rizky Indah Soraya100% (1)
- Herman & Polivy, 1975Document7 pagesHerman & Polivy, 1975Ana Sofia AlmeidaNo ratings yet
- Importance of A Positive Attitude in Customer ServiceDocument8 pagesImportance of A Positive Attitude in Customer ServiceEL FuentesNo ratings yet
- 8 Ways To Stop Over-Thinking and Find Peace in The Present MomentDocument6 pages8 Ways To Stop Over-Thinking and Find Peace in The Present MomentBadri VrsnprasadNo ratings yet
- Upper Gastrointestinal - Esophageal BleedingDocument15 pagesUpper Gastrointestinal - Esophageal Bleedingmardsz100% (9)