Professional Documents
Culture Documents
Team Approach: Management of Brachial Plexus Birth Injury
Uploaded by
Sham ObaidatCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Team Approach: Management of Brachial Plexus Birth Injury
Uploaded by
Sham ObaidatCopyright:
Available Formats
|
Team Approach: Management of
Brachial Plexus Birth Injury
Sandra Schmieg, Abstract
MS, OTRL, CHT » Brachial plexus birth injury is an upper-extremity paralysis that occurs
from a traction injury to the brachial plexus during birth. Approx-
Jie C. Nguyen, MD, MS imately 10% to 30% of children with a brachial plexus birth injury have
Meagan Pehnke, residual neurologic deficits with associated impact on upper-limb
function.
MS, OTRL, CHT, CLT
Sabrina W. Yum, MD » Management of brachial plexus birth injuries with a multidisciplinary
team allows optimization of functional recovery while avoiding unnec-
Downloaded from http://journals.lww.com/jbjsreviews by BhDMf5ePHKbH4TTImqenVL8/J7OdHJl5LVzY2uhCL+FUJh7b3e2plafQsRXve7MrUa4U22a2pIs= on 07/03/2020
Apurva S. Shah, MD, MBA essary intervention. Early occupational therapy should be initiated with a
focus on range of motion and motor learning.
Investigation performed at Children’s » The need for microsurgical reconstruction of the brachial plexus can
Hospital of Philadelphia, be predicted based on early physical examination findings, and recon-
Philadelphia, Pennsylvania struction is generally performed at 3 to 9 months of age.
» The majority of children with residual neurologic deficits develop
associated glenohumeral dysplasia. These children may require second-
ary procedures, including botulinum toxin injection, subscapularis and
pectoralis lengthening, shoulder capsular release, shoulder tendon
transfer, and humeral osteotomy.
B
rachial plexus birth injury pseudoparalysis in the setting of a birth
(BPBI) is an upper-extremity fracture or neonatal radial nerve palsy.
paralysis that typically occurs Fractures of the clavicle and the humeral
during vaginal childbirth due shaft are the most common birth fractures
to traction. Shoulder dystocia and macro- but they are not associated with increased
somia are the most common risk factors, risk of BPBI2. In children with an isolated
but breech delivery, instrumented delivery, clavicular fracture, neurologic function
and hypoxia also independently increase improves over the first few weeks of life,
the risk of injury1. The prevalence of suggesting pseudoparalysis that was medi-
BPBI in the United States decreased from ated by pain rather than peripheral nerve
1.7 to 0.9 per 1,000 live births from 1997 to injury. Persistent paralysis beyond fracture-
2012 in the setting of decreasing rates of healing may suggest concurrent BPBI.
macrosomia and increasing rates of multi- Humeral shaft fracture typically occurs on
parity and cesarean section1. Variations in the contralateral side of the BPBI. Neonatal
the reported rate may be attributed to radial nerve palsy should be suspected when
geographic differences in socioeconomic there is absent digital and wrist extension
deprivation, obstetric care, and birth but intact shoulder elevation and elbow
weight. flexion. The presence of ecchymosis or fat
BPBI is typically diagnosed after birth necrosis along the posterolateral aspect of
when there is a lack of spontaneous upper- the brachium is pathognomonic for neo-
extremity movement (Fig. 1). Clinical natal radial nerve palsy3 and is not typically
examination can distinguish BPBI from seen with BPBI.
COPYRIGHT © 2020 BY THE Disclosure: The authors indicated that no external funding was received for any aspect of this work.
JOURNAL OF BONE AND JOINT The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the
SURGERY, INCORPORATED article (http://links.lww.com/JBJSREV/A612).
JBJS REVIEWS 2020;8(7):e19.00200 · http://dx.doi.org/10.2106/JBJS.RVW.19.00200 1
| Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y
is most useful for toddlers and older neurologic recovery is incomplete, 60%
children; it measures gross functional to 80% of children develop some degree
movements (e.g., global shoulder of glenohumeral deformity that may
abduction, global shoulder external benefit from secondary procedures,
rotation, and other movements, in- including subscapularis or pectoralis
cluding hand to mouth, hand to neck, lengthening, shoulder capsular release,
hand to spine, and hand to belly)6. No shoulder tendon transfer, or humeral
scoring system is comprehensive, and osteotomy.
the different systems are difficult to
compare. For example, the modified Case Report
Mallet score does not correlate well with The family was informed that informa-
the AMS or the Toronto Test score tion regarding the case would be sub-
because of its emphasis on shoulder mitted for publication, and they
motion7. Overall, the most important provided consent.
prognostic sign is return of antigravity A boy was delivered vaginally at 39
Fig. 1 elbow flexion since delayed return of weeks of gestation with a birthweight of
Initial presentation of a newborn with a left biceps function has been associated with 3.66 kg. Delivery was complicated by a
upper trunk brachial plexus birth injury (Erb inferior Mallet scores8. left shoulder dystocia and resulted in a
palsy, Narakas type I). The photograph dem-
onstrates the classic “waiter’s tip” positioning While the majority of infants with left upper trunk BPBI and a right
with the shoulder in a position of adduction BPBI have full spontaneous neurologic humeral shaft fracture, which was im-
and internal rotation, the elbow in extension, recovery, 10% to 30% of children are mobilized for 4 weeks in a soft wrap. At
and the wrist in flexion.
left with permanent weakness, contrac- initial presentation, there was no deltoid
ture, and loss of function9,10. The Nar- or biceps activation (Fig. 1). He dem-
Physical examination is the pri- akas classification system stratifies onstrated antigravity elbow, wrist, and
mary assessment tool when evaluating prognosis based on nerve root involve- digital extension. Full passive shoulder
a newborn. With careful examination ment11. Narakas type-I injuries (Erb range of motion was noted. The patient
of specific muscle groups, the physi- palsy) involve the upper trunk (C5-C6) was followed monthly by the multidis-
cian or therapist can determine the and represent 46% of patients. Ap- ciplinary team with serial examinations
pattern of nerve root involvement. proximately 80% of children in this (Tables I and II). Return of biceps and
The clinician also should look for group make a full recovery. Narakas deltoid function was evident at 4
ipsilateral ptosis or miosis to detect type-II injuries involve the upper and months. Clinical examination revealed a
associated Horner syndrome. Serial middle trunk regions (C5-C7) and rep- worsening shoulder internal rotation
evaluation of the newborn allows resent 30% of patients. Only 60% of contracture between 2 and 5 months of
the clinical team to monitor motor these children make a full recovery. age, with no evidence of active shoulder
recovery and formulate a treatment Narakas type-III and IV injuries occur in external rotation. The patient was
plan. 20% of patients. Type-III injuries rep- referred for baseline shoulder ultraso-
Once a diagnosis of BPBI has been resent a global plexopathy (flail limb); nography at 4 months of age and repeat
established, there are multiple scoring type-IV injuries are the most severe and imaging at 5 months, which revealed a
systems available to track neurologic include a flail limb and Horner syn- posterior glenohumeral dislocation
recovery and upper limb function. The drome. The vast majority of children (Figs. 2-A through 2-D). The medical
most commonly used and validated with global injuries do not make a team recommended botulinum toxin
systems include the Active Movement complete recovery. type-A injection in the subscapularis,
Score (AMS), the Toronto Test score, Children with limited neurologic the pectoralis major, and the teres major
and the modified Mallet score. The recovery may be candidates for primary (Fig. 3), along with closed reduction and
AMS comprises 15 spontaneous move- reconstruction of the brachial plexus spica casting with the shoulder in
ments; each score is based on active with nerve-grafting or transfers. Micro- external rotation. This procedure was
movement without gravity and against surgical reconstruction can dramatically completed at 5 months of age, and the
gravity4. The Toronto Test score com- improve strength and limb function. cast was removed after 1 month.
bines 5 essential movements (elbow Developmentally, children with per-
flexion, elbow extension, wrist exten- manent plexopathy experience delayed Team Approach
sion, digital extension, and thumb skeletal maturation, and the affected Surgery
extension) and attempts to prognosti- limb can have smaller dimensions— A multidisciplinary brachial plexus team
cate neurologic recovery with a com- typically 95% of the girth and length of may include orthopaedic surgeons,
posite score5. The modified Mallet score the unaffected extremity12,13. When neurosurgeons, and plastic surgeons.
2 JULY 2020 · VOLUME 8, ISSUE 7 · e 19.00200
Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y |
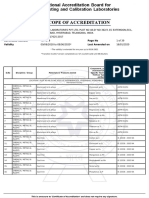
TABLE I Active Movement Scores for the Infant in the Case Report*
Patient Age
Left-Side Movement 1 Month 2 Months 3 Months 4 Months 5 Months 6 Months† 8 Months
Shoulder flexion 0 0 2 2 3 6
Shoulder adduction 7 7 7 7 7 7
Shoulder abduction 0 0 2 2 3 5
Shoulder internal rotation 7 7 7 7 7 7
Shoulder external rotation 0 0 0 0 0 2
Elbow flexion 0 0 2 6 6 6
Elbow extension 7 7 7 7 7 7
Supination 0 0 0 0 0 0
Pronation 7 7 7 7 7 7
Wrist flexion 7 7 7 7 7 7
Wrist extension 6 6 7 7 7 7
Thumb flexion 7 7 7 7 7 7 7
Thumb extension 7 7 7 7 7 7 7
Finger flexion 7 7 7 7 7 7 7
Finger extension 7 7 7 7 7 7 7
*The Active Movement Score (AMS) is completed during all clinical examinations to provide serial tracking of motor recovery and upper-extremity
function. The infant should be positioned to allow observation of the 15 upper-extremity movements, scored first in a gravity-reduced position until full
motion is observed and then progressing to an antigravity plane of movement. Gravity-eliminated score: 0 5 no contraction, 1 5 contraction but no
motion, 2 5 ,50% motion, 3 5 $50% motion, and 4 5 full motion. Antigravity score: 5 5 ,50% motion, 6 5 $50% motion, and 7 5 full motion.
†Immediately after shoulder spica cast removal and 1 month after botulinum injection.
The initial surgeon’s responsibility is to prognosis. Return of partial antigravity recovery and are associated with nerve
confirm the diagnosis of BPBI in con- elbow flexion by 2 months suggests that root avulsion14,15. Phrenic nerve
junction with a neurologist or a physia- the patient will ultimately experience injury results in paralysis of the hem-
trist and to monitor recovery. In many complete spontaneous neurologic idiaphragm and is diagnosed with
multidisciplinary programs, multiple recovery11. However, Waters demon- ultrasonography. Shah et al. demon-
surgeons evaluate the patient because of strated that if antigravity biceps function strated that findings on physical
the complex clinical decision-making. does not return by 3 months, the child examination in the first 3 months of
Due to the variation in severity and the will rarely experience complete recovery life can predict the need for micro-
complexity of the physical examination, and will likely have limitations in surgery, which is useful prognostic
consensus is important. shoulder strength and joint contrac- information for the family16. In their
Because of limitations in diagnos- ture8. Injury to the phrenic nerve and multicenter investigation, 4 early
tic testing, the team must rely on phys- Horner syndrome are individually con- physical examination factors inde-
ical examination to understand the sidered prognostic for poor motor pendently predicted microsurgery,
TABLE II Passive Range of Motion Measurements for the Infant in the Case Report*
Patient Age
Measurement 1 Month 2 Months 3 Months 4 Months 5 Months 6 Months† 8 Months
Scapulohumeral angle (deg) 160 160 150 150 140 110 150
Shoulder external rotation in adduction (deg) 90 80 75 65 30 80 90
Shoulder external rotation in abduction (deg) 110 110 110 110 80 100 100
Elbow extension (deg) 0 0 0 0 0 0 0
*Clinical assessment of joint passive range of motion allows the team to identify onset of joint contractures to provide timely medical or therapeutic
interventions, such as use of orthoses. †Immediately after shoulder spica cast removal and 1 month after botulinum injection.
JULY 2020 · VOLUME 8, ISSUE 7 · e19.00200 3
| Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y
Fig. 2
Figs. 2-A through 2-D Ultrasound assessment of glenohumeral dysplasia. The alpha angle is formed between a line that is drawn along the posterior
scapular margin and another line that is drawn tangential to the humeral head from the posterior margin of the glenoid. An alpha angle of .30° is
abnormal. Humeral head translation is quantified by measuring the percentage of the humeral head that is displaced posterior to the axis of the
scapula, which is abnormal if it measures .50%42. Transverse ultrasound images over the posterior glenohumeral joint in the clinical case report were
obtained at 4 months of age, 5 months of age, and postintervention (9 months of age). Figs. 2-A and 2-B At 4 months, there was an irregular
ossification margin of the left posterior glenoid rim (Fig. 2-A arrowheads) when compared with the normal right glenoid (Fig. 2-B curvy arrow), but
there were normal alpha angles (left, 25°; right, 23°) and a normal PHHD (percentage of the humeral head displaced posterior to the axis of the scapula)
(left, 37%; right, 31%). Fig. 2-C At 5 months of age, the left glenohumeral joint demonstrated an abnormally increased alpha angle (32°) and PHHD
(52%). Fig. 2-D Following intervention, at 9 months of age, there was improved glenohumeral alignment. The PHHD is calculated by dividing the
diameter of the humeral head that is located posterior to the scapular line (short dashes) by the diameter of the entire head (short 1 long dashes) and
multiplying by 100.
including Horner syndrome as well injuries with or without Horner syn- gressive loss of passive shoulder external
lack of antigravity elbow flexion, wrist drome). However, the indications and rotation. As described by Bauer et al.,
extension, and digital and wrist flexion timing for microsurgery for Narakas passive shoulder external rotation of
(Table III). type-I and II injuries (upper trunk or ,60° with the arm at the side can
Microsurgical reconstruction of combined upper and middle trunk indicate posterior dislocation of the
the brachial plexus may be recom- lesions) continue to be deliberated. humeral head17. The dislocation was
mended with nerve-grafting and/or Many surgeons use biceps recovery to confirmed with shoulder ultrasonog-
transfers in infants who do not dem- guide decision-making. The lack of raphy. We recommended botulinum
onstrate adequate neurologic recovery. antigravity biceps function at 6 to 9 toxin type-A injections along with
In most cases, surgical intervention is months has been cited as an indication closed reduction and spica casting with
contraindicated when antigravity for microsurgery16. In the case report the shoulder in external rotation. As
biceps function recovers by 3 months. described above, antigravity biceps reported by Ezaki et al., reduction of
Although evidence-based indications function returned at 4 months, and the shoulder could be maintained in
for reconstruction are lacking, there is reconstruction of the brachial plexus 69% (24 of 35) of infants who undergo
general consensus that microsurgery was not recommended. botulinum toxin injection and spica
is indicated at 3 months of age for On serial examination, the casting18. Greenhill et al. reported
Narakas type-III and IV injuries (global described infant demonstrated pro- higher rates of treatment failure with
4 JULY 2020 · VOLUME 8, ISSUE 7 · e 19.00200
Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y |
to the rotator cuff also can be performed. impairment. Asymmetric chest wall
Although tendon transfers reliably movement or shortness of breath may
improve shoulder strength and motion, indicate diaphragmatic paralysis result-
concurrent reduction of the shoulder ing from phrenic nerve involvement.
joint is required to permit remodeling of The differential diagnosis for arm
the glenohumeral joint. Waters and Bae weakness should include a neonatal or in
demonstrated remodeling of glenohu- utero cerebral infarct, brain malforma-
meral dysplasia in 83% (19 of 23) of tion, or a mass lesion. Since intracranial
patients with combined intra-articular lesions typically present with hypertonia
and extra-articular procedures20. For and/or spasticity, the presence of brisk
older children with severe glenohumeral reflexes in a weak upper limb would
Fig. 3 dysplasia that includes formation of a argue against the diagnosis of BPBI.
The patient underwent botulinum toxin type- biconcave glenoid (generally at $4 years With intracranial lesions, careful exam-
A injection of the subscapularis, pectoralis of age), shoulder tendon transfers are ination of ipsilateral lower-extremity
major, and teres major muscles. In this pho-
tograph, the neurologist is performing a bot-
not typically recommended. In these function frequently shows decreased
ulinum toxin injection to the pectoralis major cases, an external rotation humeral movement as well. Central nervous sys-
via palpation that was confirmed with osteotomy can reposition the arc of tem involvement, including neonatal
electromyography.
shoulder rotation and improve hypoxic-ischemic encephalopathy, a
function6. cerebral infarct, or spinal cord injury,
closed reduction and botulinum toxin can occur concurrently with BPBI. MRI
injections, particularly in infants with Neurology of the brain and cervical spinal cord
,15° of passive shoulder external The initial responsibility of a neurologist might be needed to confirm the diag-
rotation19. If closed reduction is per- in the multidisciplinary team is to con- nosis, along with ongoing neurologic
formed, the shoulder should be posi- firm the diagnosis of BPBI. Patients with reexamination.
tioned with the arm close to the side BPBI have lower motor neuron signs on Supplementing the physical
(,15° of abduction) and at .60° of examination, including muscle atrophy, examination with a nerve conduction
external rotation. Casting is typically hypotonia, weakness, and depressed or study (NCS) and electromyography
discontinued after 4 weeks, and therapy absent reflexes. Neurologic examination (EMG) can be helpful to determine the
is reinitiated. While our team recom- is the mainstay of lesion localization, lesion location and the extent and
mended closed shoulder reduction and which has important treatment and severity of the injury, and to detect signs
botulinum toxin injection for the prognostic implications. of reinnervation. An NCS and EMG can
patient described above, other centers Sensory assessment can be chal- support preoperative decision-making
might have recommended subscapu- lenging in neonates, but a global and are predictors of outcome after sur-
laris and pectoralis lengthening and impression can be inferred by the gical repair. For example, the presence of
shoulder tendon transfer given the infant’s facial expression to noxious sensory response in the root(s) inner-
severe loss of passive shoulder external stimulation. Chewing and biting the vating the paretic muscle group is diag-
rotation and the possibility of treat- affected hand can suggest sensory nostic of root avulsion, which typically
ment failure with nonoperative
management.
Despite early recognition and TABLE III Physical Examination Predictors of Microsurgery*
treatment, many infants develop persis-
No. of Early Physical Rate of
tent or progressive glenohumeral dys- Examination Factors Microsurgery
plasia. This can be characterized with
0 0%
magnetic resonance imaging (MRI). For
children with shoulder internal rotation 1 22%
contracture and mild-to-moderate dys- 2 43%
plasia (who are generally ,4 years of 3 76%
age), treatment can include open or 4 93%
arthroscopic anterior capsular release
*In patients with BPBI, early physical examination findings independently predict
and reduction of the shoulder joint with microsurgical intervention. These factors can be used to provide counseling in
subscapularis and/or pectoralis major early infancy for families regarding injury severity and help to plan for potential
lengthening. For children with limita- microsurgical intervention. These findings include the presence of Horner syn-
drome, lack of antigravity elbow flexion, lack of antigravity wrist extension, and
tions in shoulder strength, transfer of the lack of antigravity digital and wrist flexion16.
latissimus dorsi and teres major tendons
JULY 2020 · VOLUME 8, ISSUE 7 · e19.00200 5
| Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y
carries a poor prognosis. However, the ported but typically have been associated functional digit motion29. Limitations
practical utility of an electrophysiologi- with large doses or in the presence of in active shoulder external rotation and
cal study has been controversial because comorbidities. There are 4 different forearm supination can result in com-
the technical difficulty in performing a products that currently are available on pensatory movement patterns, such as
comprehensive examination can be the market, including rimabotulinum trumpeting (compensatory shoulder
considerable and distressing for the toxin B, onabotulinum toxin A, in- abduction), and the forearm can be
patient. The disparity between study cobotulinum toxin A, and abobotuli- supported through the use of a supinator
findings and later prognosis is also num toxin A. The lack of bioequivalence strap that provides a more neutral fore-
sources of concern. Malessy et al. of various proprietary preparations can arm position29. Serial examination of
described a simplified protocol that cause confusion and pose a risk to passive motion should include moni-
showed excellent predictive value21. In a patients. toring of elbow flexion contractures.
prospective study, clinical testing of Serial elbow extension orthoses can be
elbow flexion and extension without Occupational Therapy effective in improving range of motion
performing EMG of the biceps muscle Therapeutic goals for the infant with in the motivated patient with flexion
resulted in a correct prediction rate of BPBI focus on maintaining joint contractures that are .30°30. A SupER
80.8%. Needle EMG increased the motion, maximizing strength, promot- (supination-external rotation) orthosis
percentage of correct predictions by ing sensory awareness, and supporting (University of British Columbia) may be
13%, to 93.6%, at 1 month of age. age-appropriate development23-25. The recommended to passively position the
Interestingly, prediction of severe BPBI occupational therapist plays a role in shoulder in external rotation and fore-
was better at 1 month than at 1 week or 3 assessing active movement in collabora- arm supination in order to address
months of age21. Surface EMG also can tion with the surgeon. The team internal rotation contracture or poste-
help to evaluate for cocontraction, approach to serial examination is crit- rior glenohumeral dislocation. This may
which is believed to occur due to aber- ical for accurate clinical information be indicated when end-range tightness is
rant innervation and/or synkinesis. regarding neurologic recovery during identified or following a procedure to
In the case report described above, time-sensitive surgical decision-making. address glenohumeral dislocation as
we recommended botulinum toxin Examination of the infant is difficult, described in our case report. Pilot study
type-A injection of the subscapularis, the and the occupational therapist may have results suggest that use of this type of
pectoralis major, and the teres major. greater opportunities for interaction to orthosis may have a positive impact on
Botulinum toxin type A blocks the observe new motor activity, providing balanced shoulder growth and muscle
release of acetylcholine at the presynap- key information that may not be function31.
tic neuromuscular junction, resulting in observed by the full team. Strategies to maximize movement
temporary weakness. It has been shown Maintaining passive joint motion and strength in targeted muscles are used
to be an effective adjunctive treatment is the primary initial focus of therapy and during occupational therapy and home
for posterior shoulder subluxation or a home program. The occupational programs. Eccentric contractions are
dislocation when injected into the therapist will instruct the parent on safe first elicited through place-and-hold
shoulder internal rotators. Typically, 2 and effective passive range-of-motion exercises in gravity-reduced planes, with
to 3 U/kg per muscle is injected at (PROM) exercises to complete fre- progression to antigravity concentric
multiple intramuscular points, with a quently throughout the day23. Shoulder contractions. Targeted concentric con-
maximum total dose of 10 U/kg. Botu- stretches are completed both with and tractions and muscle activation can be
linum toxin injections also have been without scapular stabilization to maxi- achieved through developmental posi-
reported with variable effectiveness for mize glenohumeral joint motion26,27. tioning17. Kinesiology taping tech-
triceps or biceps cocontraction or pro- Caregiver comfort with completing niques can be used to target specific
nator contracture in retrospective stud- PROM exercises routinely is critical to muscle facilitation or inhibition23,32.
ies22. Although botulinum toxin type A maintain joint integrity. Sensory strategies are used to
has been approved by the U.S. Food and Orthotic intervention may be address altered cortical representation
Drug Administration for treatment of indicated to maintain joint integrity, and awareness of the affected limb17.
spasticity, the off-label nature of its use prevent contracture, and promote Provision of sensory experiences
with BPBI should be disclosed to par- function. In the infant with limited through touch, gentle massage, and
ents, and informed consent should be active wrist or digital extension, a resting texture rubs are initiated early in care and
obtained. With correct technique, bot- orthotic is indicated to support the hand used throughout recovery. Positioning
ulinum toxin type-A injection appears to in an extended position overnight23,28. of the involved hand in the infant’s visual
be safe and well tolerated. Serious side A dorsal wrist extension orthosis may be field during developmental activities is
effects, including profound weakness, used during the day to support a wrist recommended. Gentle joint compres-
dysphagia, and death, have been re- drop and provide a position for more sion and weight-bearing promote joint
6 JULY 2020 · VOLUME 8, ISSUE 7 · e 19.00200
Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y |
proprioception33. The use of sensory or surgeon to assess the need for a second- nerve root avulsion, its use in children
motor-level electrical stimulation does ary shoulder intervention is indicated if is hindered by the need for sedation
require future research but it can be used the patient is not being actively followed and the use of ionizing radiation.
as an adjunct to therapy to improve by a multidisciplinary team. Children MRI with 3-dimensional (3D) fluid-
cortical representation and muscle acti- who are not candidates for surgical sensitive sequences to optimize the
vation in poorly innervated muscles34. intervention may benefit from episodic visualization of exiting cervicothoracic
Sensory-level stimulation can be used therapy to address motion, strength, nerve roots is becoming the preferred
to optimize the activation of spared activity adaptation, and motor training alternative36,37. In a cohort of 13
nerves to enhance cortical awareness. to minimize habitual compensatory patients with BPBI who later under-
Motor-level stimulation may be used movements23. went reconstructive surgery, Soma-
when active muscle movement is shekar et al. found high-resolution 3D
demonstrated35. Radiology MRI to be 75% sensitive and 82%
Rehabilitation after nerve recon- Differentiation between neurapraxia specific for nerve root avulsion36.
struction follows the principles outlined or mild axonotmesis and neurotmesis Indirect features of nerve injury
above. Parents’ expectations for recovery or nerve root avulsion is critically include the presence of a pseudome-
must be managed as nerve regeneration important as the former diagnoses ningocele, asymmetric periscalene soft-
occurs at approximately 1 in (2.54 cm) have potential for spontaneous recov- tissue edema, and downstream muscle
per month, and no change in movement ery while the latter require early sur- denervation changes38. Pseudome-
is typically expected before 6 months. As gical intervention because treatment ningocele is a contained cerebrospinal
children with BPBI enter school age and effectiveness declines with time. Many fluid leak that surrounds the injured
adolescence, they may experience experts rely on physical examination to nerve root sleeve (Figs. 4-A and 4-B). In
changes in muscle length and strength determine injury severity, but some children who are ,18 months old, a
during periods of growth, which may also utilize noninvasive imaging early pseudomeningocele is highly specific
impact function17. Progression of joint after birth to complement the clinical for underlying nerve injury but lacks
contractures, loss of active movement, assessment and help define injury sensitivity36,39. Asymmetric peri-
and development of pain due to com- severity36. Although computed scalene soft-tissue edema may be more
pensatory movement patterns may tomography (CT) myelography is sensitive for nerve injury and may
develop. Evaluation by an orthopaedic widely accepted for the evaluation of represent a posttraumatic scar or a
Fig. 4
Figs. 4-A and 4-B MRI-based detection of a
pseudomeningocele. Coronal (Fig. 4-A) and
axial (Fig. 4-B) reformatted 3D high-resolution
fluid-sensitive images of a 3-month-old girl
showed a small right pseudomeningocele
(arrowheads) and no identifiable exiting
nerves. Note the appearance of normal exiting
ventral and dorsal nerves on the normal left
side (arrows).
JULY 2020 · VOLUME 8, ISSUE 7 · e19.00200 7
| Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y
Fig. 5
Figs. 5-A and 5-B MRI assessment of glenohumeral dysplasia. Three-dimensional dual echo steady state (DESS) cartilage-sensitive axial images of a
20-month-old girl with right BPBI show abnormally increased glenoid retroversion (236°) and decreased PHHA (percentage of the humeral head
anterior to the scapular axis) (25%) when compared with the normal left shoulder (211° and 50%, respectively). The PHHA is calculated by dividing the
diameter of the humeral head that is located anterior to the scapular axis (short dashes) by the diameter of the entire head (short 1 long dashes) and
multiplying by 100.
reparative neuroma, but it does not facing away from the sonographer. On hypoplasia, and dysplasia remodeling of
allow the identification of the exact ultrasonography, glenohumeral align- the posterior glenoid can be observed52.
level of involvement40. In a retro- ment is defined by the alpha angle and Humeral head coverage is quantified by
spective MRI review of a cohort of 37 humeral head translation (Figs. 2-A measuring the percentage of the humeral
patients with BPBI, Wandler et al. through 2-D). head that is anterior to the axis of the
found periscalene soft-tissue edema in MRI remains the noninvasive ref- scapula, which is normal when it is
95% of the patients and a pseudome- erence standard for the comprehensive between 40% and 55% and abnormal if
ningocele in 40% of the patients41. assessment of glenohumeral alignment it measures ,35%52,53. These mea-
Muscle denervation changes include and the characterization of glenoid dys- surements can be used to classify the
muscle edema during the active phase plasia, particularly in older children in severity of glenohumeral dysplasia using
and atrophy during the late phase38. whom ultrasonography may be less the criteria described by Waters et al.53.
Given the rapid neurologic recovery reliable due to formation of the humeral
of the patient in our case report, head ossification centers40,43 (Figs. 5-A Overview
MRI of the brachial plexus was not and 5-B). Features of unresolved BPBI Optimal management of a patient with
recommended. include posterior humeral head transla- BPBI involves a multidisciplinary
Accurate clinical characterization tion and glenoid retroversion, which can approach and can include evaluation
of glenohumeral dysplasia in children appear in infants as young as 3 months and treatment by orthopaedic sur-
with BPBI can be challenging42. old40,46. On MRI, proton-density- gery, plastic surgery, neurosurgery,
Ultrasonography and MRI are becom- weighted sequences are preferred; they neurology, physiatry, occupational/
ing increasingly utilized to complement provide the highest signal-to-noise physical therapy, and radiology person-
the clinical assessment, to monitor ratio47. Axial images are most useful for nel. Our patient received coordinated
treatment response, and to determine the evaluation of glenoid morphology care from all disciplines through serial
optimal timing for intervention. and glenohumeral alignment48,49. Gle- examinations, medical interventions,
Ultrasonography is the preferred initial noid version is measured between a line and therapeutic interventions. Because
imaging modality to screen for sus- drawn along the scapular axis and of shoulder internal rotation contracture
pected glenohumeral malalignment another line drawn parallel to the surface and progressive posterior humeral head
(posterior subluxation or dislocation) of the glenoid. Mild physiological dislocation that was demonstrated on
and glenoid dysplasia42-45. Ultraso- glenoid retroversion decreases with ultrasonography between 4 and 5
nography is performed using a high- time (26.3 6 6.5 in children who are months of age, our patient was sched-
frequency linear transducer (9 to 15 ,2 years old and 22.1 6 5.9 in children uled for botulinum toxin injection of the
MHz) and a posterior approach. The who are $2 years old)50,51, but with pectoralis major, subscapularis, and teres
infant often is seated on the parent’s lap BPBI, progressive glenoid retroversion, major muscles with concurrent closed
8 JULY 2020 · VOLUME 8, ISSUE 7 · e 19.00200
Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y |
shoulder reduction and shoulder spica 3. Monica JT, Waters PM, Bae DS. Radial nerve subluxation in neonatal brachial plexus palsy. J
palsy in the newborn: a report of four cases and Bone Joint Surg Am. 2010 Sep 15;92(12):2171-7.
cast application. The cast was removed literature review. J Pediatr Orthop. 2008 Jun; 19. Greenhill DA, Wissinger K, Trionfo A, Solarz
1 month later, and the patient wore a 28(4):460-2. M, Kozin SH, Zlotolow DA. External rotation
SupER orthosis at night and during nap 4. Curtis C, Stephens D, Clarke HM, Andrews D. predicts outcomes after closed glenohumeral
The Active Movement Scale: an evaluative tool joint reduction with botulinum toxin type A in
time, with weekly therapy to maximize for infants with obstetrical brachial plexus brachial plexus birth palsy. J Pediatr Orthop.
the strength of the posterior shoulder palsy. J Hand Surg Am. 2002 May;27(3):470-8. 2018 Jan;38(1):32-7.
and scapular muscles. Repeat ultraso- 5. Michelow BJ, Clarke HM, Curtis CG, Zuker RM, 20. Waters PM, Bae DS. The early effects of
Seifu Y, Andrews DF. The natural history of tendon transfers and open capsulorrhaphy on
nography at 3 months after cast removal obstetrical brachial plexus palsy. Plast Reconstr glenohumeral deformity in brachial plexus
revealed improved glenohumeral align- Surg. 1994 Apr;93(4):675-80; discussion 681. birth palsy. J Bone Joint Surg Am. 2008 Oct;
6. Abzug JM, Chafetz RS, Gaughan JP, Ashworth 90(10):2171-9.
ment. Substantially improved passive S, Kozin SH. Shoulder function after medial 21. Malessy MJ, Pondaag W, Yang LJ, Hofstede-
and partial recovery of active shoulder approach and derotational humeral osteotomy Buitenhuis SM, le Cessie S, van Dijk JG. Severe
in patients with brachial plexus birth palsy. J obstetric brachial plexus palsies can be
external rotation also were noted. The Pediatr Orthop. 2010 Jul-Aug;30(5):469-74. identified at one month of age. PLoS One. 2011;
patient will be followed by the multi- 7. Greenhill DA, Lukavsky R, Tomlinson-Hansen 6(10):e26193. Epub 2011 Oct 17.
disciplinary team periodically through- S, Kozin SH, Zlotolow DA. Relationships 22. Gobets D, Beckerman H, de Groot V, Van
between 3 classification systems in brachial Doorn-Loogman MH, Becher JG. Indications
out childhood to monitor his progress. plexus birth palsy. J Pediatr Orthop. 2017 Sep; and effects of botulinum toxin A for obstetric
MRI of the shoulder may be indicated in 37(6):374-80. brachial plexus injury: a systematic literature
8. Waters PM. Comparison of the natural review. Dev Med Child Neurol. 2010 Jun;52(6):
the future to better characterize residual 517-28. Epub 2010 Feb 12.
history, the outcome of microsurgical repair,
glenohumeral dysplasia and determine and the outcome of operative reconstruction in 23. Nelson VS, Justice D, Rasmussen L,
the potential need for secondary shoul- brachial plexus birth palsy. J Bone Joint Surg Popadich MG. Rehabilitation concepts for
Am. 1999 May;81(5):649-59. pediatric brachial plexus palsies. In: Chung KC,
der surgery. The need for subscapularis Yang LJS, McGillicuddy JE, editors. Practical
9. Hoeksma AF, ter Steeg AM, Nelissen RG, van
or pectoralis major tendon lengthening, Ouwerkerk WJ, Lankhorst GJ, de Jong BA. management of pediatric and adult brachial
Neurological recovery in obstetric brachial plexus palsies. Philadelphia: W.B. Saunders;
capsular release, or shoulder tendon 2012. p 143-56.
plexus injuries: an historical cohort study. Dev
transfer remains a distinct possibility in Med Child Neurol. 2004 Feb;46(2):76-83. 24. Abid A. Brachial plexus birth palsy:
management during the first year of life. Orthop
this case scenario, particularly given the 10. Pondaag W, Malessy MJ, van Dijk JG,
Traumatol Surg Res. 2016 Feb;102(1)(Suppl):
Thomeer RT. Natural history of obstetric
lack of antigravity shoulder external brachial plexus palsy: a systematic review. Dev S125-32. Epub 2016 Jan 7.
rotation. Med Child Neurol. 2004 Feb;46(2):138-44. 25. Hale HB, Bae DS, Waters PM. Current
11. Narakas AO. [Injuries of the brachial plexus concepts in the management of brachial plexus
and neighboring peripheral nerves in vertebral birth palsy. J Hand Surg Am. 2010 Feb;35(2):
Sandra Schmieg, MS, OTRL, CHT1, 322-31.
fractures and other trauma of the cervical
Jie C. Nguyen, MD, MS1, spine]. Orthopade. 1987 Feb;16(1):81-6. 26. Abzug JM, Kozin SH. Evaluation and
Meagan Pehnke, MS, OTRL, CHT, CLT1, German. management of brachial plexus birth palsy.
Sabrina W. Yum, MD1, 12. Oktay F, Cömert D, Gökkaya NKO, Özbudak Orthop Clin North Am. 2014 Apr;45(2):225-32.
Epub 2014 Jan 29.
Apurva S. Shah, MD, MBA1 SD, Uysal H. Bone age in children with
obstetrical brachial plexus palsy: effect of 27. Russo SA, Killelea CM, Zlotolow DA, Kozin
1Children’s peripheral nerve injury on skeletal maturation. J SH, Rodriguez LM, Chafetz RS, Richards JG.
Hospital of Philadelphia, Child Neurol. 2014 Feb;29(2):203-9. Epub 2013 Scapular stabilization limits glenohumeral
Philadelphia, Pennsylvania Apr 22. stretching in children with brachial plexus
13. Bae DS, Ferretti M, Waters PM. Upper injuries. J Hand Surg Am. 2019 Jan;44(1):63.e1-
Email address for A.S. Shah: extremity size differences in brachial plexus 9. Epub 2018 Jun 20.
shaha6@email.chop.edu birth palsy. Hand (N Y). 2008 Dec;3(4):297-303. 28. Dorich JM, Shotwell C. Orthotics and
Epub 2008 Apr 25. casting. In: Abzug JM, Kozin SH, Zlotolow DA,
14. Yoshida K, Kawabata H. The prognostic editors. The pediatric upper extremity. New
ORCID iD for S. Schmieg: York: Springer; 2015. p 141-69.
value of concurrent phrenic nerve palsy in
0000-0001-8744-8788 newborn babies with neonatal brachial plexus 29. Ashworth S, Estilow T, Humpl D.
ORCID iD for J.C. Nguyen: palsy. J Hand Surg Am. 2015 Jun;40(6):1166-9. Occupational therapy evaluation and
0000-0002-6257-6860 Epub 2015 Mar 21. treatment. In: Abzug JM, Kozin SH, Zlotolow DA,
ORCID iD for M. Pehnke: 15. El-Sayed AA. The prognostic value of editors. The pediatric upper extremity. New
concurrent Horner syndrome in extended Erb York: Springer; 2015. p 171-95.
0000-0001-7863-0991
ORCID iD for S.W. Yum: obstetric brachial plexus palsy. J Child Neurol. 30. Ho ES, Roy T, Stephens D, Clarke HM. Serial
2014 Oct;29(10):1356-9. Epub 2014 Jan 21. casting and splinting of elbow contractures in
0000-0002-5243-5546 children with obstetric brachial plexus palsy. J
16. Shah AS, Kalish LA, Bae DS, Peljovich AE,
ORCID iD for A.S. Shah: Cornwall R, Bauer AS, Waters PM; Treatment Hand Surg Am. 2010 Jan;35(1):84-91. Epub 2009
0000-0002-9597-5665 and Outcomes of Brachial Plexus Injuries (TOBI) Dec 3.
Study Group. Early predictors of microsurgical 31. Verchere C, Durlacher K, Bellows D, Pike J,
reconstruction in brachial plexus birth palsy. Bucevska M. An early shoulder repositioning
References Iowa Orthop J. 2019;39(1):37-43. program in birth-related brachial plexus injury:
1. DeFrancesco CJ, Shah DK, Rogers BH, Shah 17. Bauer AS, Morehouse S, Waters PM. Brachial a pilot study of the Sup-ER protocol. Hand (N Y).
AS. The epidemiology of brachial plexus birth plexus injuries. In: Trumble TE, Rayan GM, Baratz 2014 Jun;9(2):187-95.
palsy in the United States: declining incidence ME, Budoff JE, Slutsky DJ, editors. Principles of 32. Walsh SF. Treatment of a brachial plexus
and evolving risk factors. J Pediatr Orthop. 2019 hand surgery and therapy. 3rd ed. Philadelphia: injury using Kinesiotape and exercise.
Feb;39(2):e134-40. Elsevier; 2017. p 322-38. Physiother Theory Pract. 2010 Oct;26(7):490-6.
2. Gandhi RA, DeFrancesco CJ, Shah AS. The 18. Ezaki M, Malungpaishrope K, Harrison RJ, 33. Ramos LE, Zell JP. Rehabilitation program
association of clavicle fracture with brachial Mills JK, Oishi SN, Delgado M, Bush PA, Browne for children with brachial plexus and peripheral
plexus birth palsy. J Hand Surg Am. 2019 Jun; RH. Onabotulinum toxinA injection as an nerve injury. Semin Pediatr Neurol. 2000 Mar;
44(6):467-72. Epub 2019 Jan 23. adjunct in the treatment of posterior shoulder 7(1):52-7.
JULY 2020 · VOLUME 8, ISSUE 7 · e19.00200 9
| Te a m A p p r o a c h : M a n a g e m e n t o f B r a c h i a l P l e x u s B i r t h I n j u r y
34. Justice D, Awori J, Carlson S, Chang KWC, shoulder abnormalities in children. AJR Am J imaging without sedation correlates with injury
Yang LJS. Use of neuromuscular electrical Roentgenol. 2015 Feb;204(2):W199-206. severity in brachial plexus birth palsy. J Hand
stimulation in the treatment of brachial plexus 41. Wandler E, Lefton D, Babb J, Shatzkes D. Surg Am. 2017 May;42(5):335-43. Epub 2017
palsy: a literature review. Open J Occupational Periscalene soft tissue: the new imaging Mar 17.
Therapy. 2018 Jul;6(3):1-11. hallmark in Erb palsy. AJNR Am J Neuroradiol. 48. Lippert WC, Mehlman CT, Cornwall R, Foad
35. Berggren J, Baker LL. Therapeutic 2010 May;31(5):882-5. Epub 2009 Dec 17. MB, Laor T, Anton CG, Welge JA. The intrarater
application of electrical stimulation and 42. Bauer AS, Lucas JF, Heyrani N, Anderson RL, and interrater reliability of glenoid version and
constraint induced movement therapy in Kalish LA, James MA. Ultrasound screening for glenohumeral subluxation measurements in
perinatal brachial plexus injury: a case report. J posterior shoulder dislocation in infants with neonatal brachial plexus palsy. J Pediatr
Hand Ther. 2015 Apr-Jun;28(2):217-20; quiz persistent brachial plexus birth palsy. J Bone Orthop. 2012 Jun;32(4):378-84.
221. Epub 2014 Dec 17. Joint Surg Am. 2017 May 3;99(9):778-83. 49. Reading BD, Laor T, Salisbury SR, Lippert
36. Somashekar D, Yang LJ, Ibrahim M, Parmar 43. Donohue KW, Little KJ, Gaughan JP, Kozin WC, Cornwall R. Quantification of humeral head
HA. High-resolution MRI evaluation of neonatal SH, Norton BD, Zlotolow DA. Comparison of deformity following neonatal brachial plexus
brachial plexus palsy: a promising alternative to ultrasound and MRI for the diagnosis of palsy. J Bone Joint Surg Am. 2012 Sep 19;94(18):
traditional CT myelography. AJNR Am J glenohumeral dysplasia in brachial plexus birth e136.
Neuroradiol. 2014 Jun;35(6):1209-13. Epub palsy. J Bone Joint Surg Am. 2017 Jan 18;99(2): 50. Mintzer CM, Waters PM, Brown DJ. Glenoid
2013 Dec 19. 123-32. version in children. J Pediatr Orthop. 1996 Sep-
37. Lutz AM, Gold G, Beaulieu C. MR imaging of 44. Moukoko D, Ezaki M, Wilkes D, Carter P. Oct;16(5):563-6.
the brachial plexus. Neuroimaging Clin N Am. Posterior shoulder dislocation in infants with 51. Friedman RJ, Hawthorne KB, Genez BM. The
2014 Feb;24(1):91-108. Epub 2013 May 16. neonatal brachial plexus palsy. J Bone Joint use of computerized tomography in the
38. Dsouza AP, Tandon S, Gundogan M, Abdalla Surg Am. 2004 Apr;86(4):787-93. measurement of glenoid version. J Bone Joint
AA. Adding value to the magnetic resonance 45. Hunter JD, Franklin K, Hughes PM. The Surg Am. 1992 Aug;74(7):1032-7.
examination in a case of brachial plexus birth ultrasound diagnosis of posterior shoulder 52. Chagas-Neto FA, Dalto VF, Crema MD,
palsy. J Clin Imaging Sci. 2018 Aug 24;8:38. dislocation associated with Erb’s palsy. Pediatr Waters PM, Gregio-Junior E, Mazzer N,
39. Medina LS, Yaylali I, Zurakowski D, Ruiz J, Radiol. 1998 Jul;28(7):510-1. Nogueira-Barbosa MH. Imaging assessment of
Altman NR, Grossman JA. Diagnostic performance 46. Eismann EA, Laor T, Cornwall R. Three- glenohumeral dysplasia secondary to brachial
of MRI and MR myelography in infants with a dimensional magnetic resonance imaging of plexus birth palsy. Radiol Bras. 2016 May-Jun;
brachial plexus birth injury. Pediatr Radiol. 2006 glenohumeral dysplasia in neonatal brachial 49(3):144-9.
Dec;36(12):1295-9. Epub 2006 Oct 7. plexus palsy. J Bone Joint Surg Am. 2016 Jan 20; 53. Waters PM, Smith GR, Jaramillo D.
40. Menashe SJ, Tse R, Nixon JN, Ishak GE, 98(2):142-51. Glenohumeral deformity secondary to brachial
Thapa MM, McBroom JA, Iyer RS. Brachial plexus 47. Bauer AS, Shen PY, Nidecker AE, Lee PS, plexus birth palsy. J Bone Joint Surg Am. 1998
birth palsy: multimodality imaging of spine and James MA. Neonatal magnetic resonance May;80(5):668-77.
10 JULY 2020 · VOLUME 8, ISSUE 7 · e 19.00200
You might also like
- Operative Brachial Plexus Surgery: Clinical Evaluation and Management StrategiesFrom EverandOperative Brachial Plexus Surgery: Clinical Evaluation and Management StrategiesAlexander Y. ShinNo ratings yet
- US For Glenohumeral DysplasiaDocument10 pagesUS For Glenohumeral DysplasiaTeoNo ratings yet
- Jurding AmeliaDocument42 pagesJurding AmeliaBenk Setsuna F. SeieiNo ratings yet
- Original ResearchDocument7 pagesOriginal ResearchMitsury Jacqueline Flores C.No ratings yet
- Assessment and Treatment of Children With Cerebral PalsyDocument13 pagesAssessment and Treatment of Children With Cerebral PalsyLizza Mora RNo ratings yet
- Case Study HydrocephalusDocument19 pagesCase Study HydrocephalusJane Mae JesoroNo ratings yet
- Anterior JigDocument6 pagesAnterior Jig박소영No ratings yet
- Rehabilitation in Transverse MyelitisDocument15 pagesRehabilitation in Transverse MyelitisGabi NacuNo ratings yet
- Proximal Humerus and Humeral Shaft Fractures in Children: M. Wade Shrader, MDDocument5 pagesProximal Humerus and Humeral Shaft Fractures in Children: M. Wade Shrader, MDRoyman MejiaNo ratings yet
- An Update On The Management of Neonatal Brachial Plexus PalsyDocument7 pagesAn Update On The Management of Neonatal Brachial Plexus PalsyAgustinus HuangNo ratings yet
- Spatial Compounding 2Document14 pagesSpatial Compounding 2عامر العليNo ratings yet
- Medical Decision Making Among Adolescents With Neonatal Brachial Plexus Palsy and Their Families: A Qualitative StudyDocument8 pagesMedical Decision Making Among Adolescents With Neonatal Brachial Plexus Palsy and Their Families: A Qualitative StudyPaoloLansangNo ratings yet
- Does Corticospinal Tract Connectivity Influence The Response To Intensive Bimanual Therapy in Children With Unilateral Cerebral Palsy?Document11 pagesDoes Corticospinal Tract Connectivity Influence The Response To Intensive Bimanual Therapy in Children With Unilateral Cerebral Palsy?Ana paula CamargoNo ratings yet
- Rehabilitation of Ataxic Gait Following Cerebellar LesionsDocument9 pagesRehabilitation of Ataxic Gait Following Cerebellar LesionsresidenciailianatulaNo ratings yet
- 10 1097@MD 0000000000020653Document6 pages10 1097@MD 0000000000020653CamilaVegaNo ratings yet
- Implications For Neuroplasticity in Physical RehabilitationDocument8 pagesImplications For Neuroplasticity in Physical RehabilitationHanine HassanNo ratings yet
- Prigatano 1987Document11 pagesPrigatano 1987andromeda.godoyNo ratings yet
- Maturation of MSKDocument12 pagesMaturation of MSKVinay KumarNo ratings yet
- Brain: Do Children Really Recover Better? Neurobehavioural Plasticity After Early Brain InsultDocument25 pagesBrain: Do Children Really Recover Better? Neurobehavioural Plasticity After Early Brain InsultDana DumitruNo ratings yet
- Lectura Bio (Ingles)Document5 pagesLectura Bio (Ingles)Valeria RengifoNo ratings yet
- Acute Exercise Improves Prefrontal Cortex But Not Hippocampal Function in Healthy AdultsDocument11 pagesAcute Exercise Improves Prefrontal Cortex But Not Hippocampal Function in Healthy AdultsAlexander ElkoninNo ratings yet
- Postsurgical Physical Therapy Management of.16OledzkaSuhr2017Document8 pagesPostsurgical Physical Therapy Management of.16OledzkaSuhr2017naeemullahNo ratings yet
- Nelson Et Al. - 2023Document7 pagesNelson Et Al. - 2023bade tunayNo ratings yet
- Facial Paralysis Reconstruction in Children and Adolescents With Central Nervous System TumorsDocument12 pagesFacial Paralysis Reconstruction in Children and Adolescents With Central Nervous System TumorsCarlos Ageno AlemánNo ratings yet
- Down 1Document7 pagesDown 1Lusy Jimenez OrtizNo ratings yet
- Effects of Osteopathic Manipulative Treatment On Children With Plagiocephaly in The Context of Current Pediatric Practice - A Retrospective Chart Review StudyDocument7 pagesEffects of Osteopathic Manipulative Treatment On Children With Plagiocephaly in The Context of Current Pediatric Practice - A Retrospective Chart Review StudymireliNo ratings yet
- The Pediatric Mandible II. Management of Traumatic Injury or FractureDocument14 pagesThe Pediatric Mandible II. Management of Traumatic Injury or FractureJulián David Ríos ZuluagaNo ratings yet
- Journal AnesthesiaDocument9 pagesJournal AnesthesiaoliviafabitaNo ratings yet
- Guerra Carrillo2014Document12 pagesGuerra Carrillo2014GsNo ratings yet
- Article RNO 1Document7 pagesArticle RNO 1dra.merchealbaNo ratings yet
- Develop Med Child Neuro - 2016 - Cioni - Early Intervention in Neurodevelopmental Disorders Underlying Neural Mechanisms PDFDocument6 pagesDevelop Med Child Neuro - 2016 - Cioni - Early Intervention in Neurodevelopmental Disorders Underlying Neural Mechanisms PDFRenan MelloNo ratings yet
- Zbojniewicz Sorger 2014 Posttreatment Imaging of Pediatric Musculoskeletal TumorsDocument18 pagesZbojniewicz Sorger 2014 Posttreatment Imaging of Pediatric Musculoskeletal Tumorsdinda indah AsmaraNo ratings yet
- OB 3rd Year 4 TH ClassDocument40 pagesOB 3rd Year 4 TH ClassShadow TiNo ratings yet
- The Importance of Anatomy in Health Professions.8Document3 pagesThe Importance of Anatomy in Health Professions.8Dr Dhiren Kumar PandaNo ratings yet
- Neurogenic BladderDocument8 pagesNeurogenic BladderrafendyfendyNo ratings yet
- Child Article 1Document19 pagesChild Article 1Juliana AndradeNo ratings yet
- Bhat - Pediatric TraumaDocument13 pagesBhat - Pediatric TraumaRicardo GrilloNo ratings yet
- The Potential of Endogenous Neurogenesis For BrainDocument5 pagesThe Potential of Endogenous Neurogenesis For BrainConstantinos ChristodoulidesNo ratings yet
- Periosteum Classification and Flap AdvancementDocument9 pagesPeriosteum Classification and Flap AdvancementAlNo ratings yet
- Congenital Muscular Torticollis: Bridging The Gap Between Research and Clinical PracticeDocument10 pagesCongenital Muscular Torticollis: Bridging The Gap Between Research and Clinical PracticeMuiz SaddozaiNo ratings yet
- Congenital Deformities of The Upper LimbsDocument8 pagesCongenital Deformities of The Upper LimbsEric Yesaya TanNo ratings yet
- Neuroanatomical Correlation of The House-Brackmann Grading System in The Microsurgical Treatment of Vestibular SchwannomaDocument23 pagesNeuroanatomical Correlation of The House-Brackmann Grading System in The Microsurgical Treatment of Vestibular SchwannomaAskarNo ratings yet
- Swallowing and DysphagiaDocument25 pagesSwallowing and DysphagiaFernanda BecerraNo ratings yet
- Care Pathways Early Diagnosis PrintDocument5 pagesCare Pathways Early Diagnosis PrintiannikkiNo ratings yet
- Artigo - NeuroplasticidadeDocument26 pagesArtigo - NeuroplasticidadeGesiane SantosNo ratings yet
- Artículo Efectos Del EjercicioDocument11 pagesArtículo Efectos Del EjercicioMeredick SotomayorNo ratings yet
- Resultados Do Neurodesenvolvimento e Comorbidades de Crianças Com Torcicolo Muscular Congênito, Avaliação Usando o Banco de Dados Do National Health Screening Program For Infants and ChildrenDocument8 pagesResultados Do Neurodesenvolvimento e Comorbidades de Crianças Com Torcicolo Muscular Congênito, Avaliação Usando o Banco de Dados Do National Health Screening Program For Infants and ChildrenYesenia PaisNo ratings yet
- Fifteen-Minute Consultation: Point of Care Ultrasound in The Management of Paediatric ShockDocument6 pagesFifteen-Minute Consultation: Point of Care Ultrasound in The Management of Paediatric ShockÄfťæb AliNo ratings yet
- Grapefruit Model For Deep Cerebral BypassDocument13 pagesGrapefruit Model For Deep Cerebral BypassIevgenii IarmoliukNo ratings yet
- Intramedullary Nailing of Pediatric Femoral Shaft FractureDocument10 pagesIntramedullary Nailing of Pediatric Femoral Shaft FractureJayNo ratings yet
- Cervical Spine Injuries.4Document2 pagesCervical Spine Injuries.4tri ananda adi pranotoNo ratings yet
- Spatial Neglect Spacial DisordeesDocument13 pagesSpatial Neglect Spacial DisordeesKarol MorenoNo ratings yet
- The Floppy Infant Contribution of Genetic and MetaDocument21 pagesThe Floppy Infant Contribution of Genetic and MetaMagdaLena02No ratings yet
- Torticollis, Facial Asymmetry and Plagiocephaly in Normal NewbornsDocument6 pagesTorticollis, Facial Asymmetry and Plagiocephaly in Normal NewbornsJuan Pablo PérezNo ratings yet
- (The Clinics - Radiology) Noam Lazebnik-Advanced Obstetrical Ultrasound - Fetal Brain, Spine, and Limb Abnormalities, An Issue of Ultrasound Clinics-Saunders (2008) PDFDocument122 pages(The Clinics - Radiology) Noam Lazebnik-Advanced Obstetrical Ultrasound - Fetal Brain, Spine, and Limb Abnormalities, An Issue of Ultrasound Clinics-Saunders (2008) PDFAndres PengNo ratings yet
- Pone 0253963Document15 pagesPone 0253963Aroa BermudezNo ratings yet
- Impaired Interneuron Development in A Novel Model of Neonatal Brain InjuryDocument17 pagesImpaired Interneuron Development in A Novel Model of Neonatal Brain InjurySamara Braga Do NascimentoNo ratings yet
- Depressed Skull Fracture in A Term Newborn Infant 2161 0665 1000i109Document2 pagesDepressed Skull Fracture in A Term Newborn Infant 2161 0665 1000i109Andrei GheorgheNo ratings yet
- Subaxial Cervical Spine Trauma JAAOSDocument12 pagesSubaxial Cervical Spine Trauma JAAOSAzmi FarhadiNo ratings yet
- TBICossu GDocument13 pagesTBICossu GKapil LakhwaraNo ratings yet
- The Role of Physical Therapy and Occupational Therapy in The Treatment of Amyotrophic Lateral SclerosisDocument11 pagesThe Role of Physical Therapy and Occupational Therapy in The Treatment of Amyotrophic Lateral SclerosisSham ObaidatNo ratings yet
- Torticollis and Your BabyDocument14 pagesTorticollis and Your BabySham ObaidatNo ratings yet
- Spina BifidaDocument3 pagesSpina BifidaSham ObaidatNo ratings yet
- A Theoretical Model To Measure The Appraisal and Coping Response To Hassles in Outdoor Recreation SettingDocument24 pagesA Theoretical Model To Measure The Appraisal and Coping Response To Hassles in Outdoor Recreation SettingSham ObaidatNo ratings yet
- Coping and Care-Related Stress in Parents of A Child With Autism Spectrum DisorderDocument15 pagesCoping and Care-Related Stress in Parents of A Child With Autism Spectrum DisorderSham ObaidatNo ratings yet
- The stress can be unbearable, but the good times are like finding gold”: A phase one modelling survey to inform the development of a self-help positive reappraisal coping intervention for caregivers of those with autism spectrum disorderDocument18 pagesThe stress can be unbearable, but the good times are like finding gold”: A phase one modelling survey to inform the development of a self-help positive reappraisal coping intervention for caregivers of those with autism spectrum disorderSham ObaidatNo ratings yet
- Material - 5. Injection Moulding Technology Part 3 - 3Document127 pagesMaterial - 5. Injection Moulding Technology Part 3 - 3Sachin KumarNo ratings yet
- Grease Select Guide PDFDocument12 pagesGrease Select Guide PDFeng13No ratings yet
- MorphineDocument3 pagesMorphineAizat KamalNo ratings yet
- Yellow Book (Analysis of Rate)Document161 pagesYellow Book (Analysis of Rate)antt phweNo ratings yet
- Instant Russia 6 NightsDocument7 pagesInstant Russia 6 Nightsshivam vermaNo ratings yet
- SOCIALISATIONDocument8 pagesSOCIALISATIONAdityaNo ratings yet
- Construction Technology 3Document41 pagesConstruction Technology 3苇菱100% (3)
- Molecular Basis of InheritanceDocument37 pagesMolecular Basis of Inheritancechristopher lopezNo ratings yet
- Design of Columns, BeamsDocument7 pagesDesign of Columns, BeamsAbdulaashik AbdulkareemNo ratings yet
- Britain Food and DrinksDocument15 pagesBritain Food and DrinksAnny NamelessNo ratings yet
- Aneurisma de La Arteria HumeralDocument3 pagesAneurisma de La Arteria HumeralcastillojessNo ratings yet
- Part3 Icho 11 15 PDFDocument124 pagesPart3 Icho 11 15 PDFManuel GuilhermeNo ratings yet
- Ch1 MCQDocument3 pagesCh1 MCQAnuj PalNo ratings yet
- PriapismDocument36 pagesPriapismShih Hsun Lin100% (1)
- 17 Proven Instant Cost Reduction Ideas Chandan GoyalDocument56 pages17 Proven Instant Cost Reduction Ideas Chandan GoyalvedanshanaghNo ratings yet
- Class 9 Science Annual Paper 2 Prince Public SchoolDocument3 pagesClass 9 Science Annual Paper 2 Prince Public SchoolSHAURYA VARDHANNo ratings yet
- All CodesDocument279 pagesAll CodesiceyrosesNo ratings yet
- Essentials of Orthognathic Surgery, 3eDocument14 pagesEssentials of Orthognathic Surgery, 3epaolacsuarezaNo ratings yet
- Daalchini Value Proposition - Ver 18.11Document13 pagesDaalchini Value Proposition - Ver 18.11Amit SaxenaNo ratings yet
- English - JapanDocument2 pagesEnglish - JapanJoseNo ratings yet
- Crackdown 15 ECDocument6 pagesCrackdown 15 ECSadhana SentosaNo ratings yet
- Science Quarter 1 Module 6Document44 pagesScience Quarter 1 Module 6shang121194% (32)
- SANRAYDocument39 pagesSANRAYgopinadh57No ratings yet
- Ztipc 2019Document86 pagesZtipc 2019Journal of Pharmacy & Pharmacognosy ResearchNo ratings yet
- Chapter 4 & 5Document12 pagesChapter 4 & 5endalkachewNo ratings yet
- HUBUNGAN STRUKTUR, Ikatan Kimia Dan Aktivitas Fisiologis CompleteDocument67 pagesHUBUNGAN STRUKTUR, Ikatan Kimia Dan Aktivitas Fisiologis Completedatin suhaellaNo ratings yet
- Chapter 2 Multiple 200 300 PDFDocument17 pagesChapter 2 Multiple 200 300 PDFRajeswari Rajarammurthy R0% (1)
- Eocr-Pfz: Digital Over Current RelayDocument1 pageEocr-Pfz: Digital Over Current RelayFaris RasyadiNo ratings yet
- Staining in Microscopy - Stains and Techniques From WikipediaDocument321 pagesStaining in Microscopy - Stains and Techniques From WikipediaDan Johnson100% (5)
- Climate Change BrochureDocument2 pagesClimate Change BrochureNicole Natcher Gallego100% (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (2)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (38)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (83)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionFrom EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (267)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (255)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingFrom EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingRating: 1 out of 5 stars1/5 (2)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)